Abstract
Background:
Considering the prevalence and associated burden of disease due to bronchial asthma, it is mandatory to obtain an optimal control of the disease and to improve outcomes for these patients. But it has been observed that there is very poor adherence to the inhalational therapy which leads to the suboptimal control of the disease.
Objectives of the Study:
To study the adherence for aerosol therapy in bronchial asthma patients and to assess the impact of health education and self-action plan in improving the compliance to the therapy.
Methodology:
A prospective study was done in a total of 500 bronchial asthma patients over a period of 2 years. Once included in the study, the patients were followed-up for a total of 12 weeks for calculation of nonadherence to the aerosol therapy. In nonadherent patients, we employed various health education strategies to improve the compliance in these cases.
Results:
A total of 500 patients of bronchial asthma who were started on aerosol therapy over duration of 2 years were included in the study. At the end of 12 weeks, it was observed that, only 193 patients (38.6%) had regular compliance and 307 patients (61.4%) were noncompliant to aerosol therapy as prescribed for bronchial asthma. Factors that were associated with poor compliance were: Lower educational level status, poor socioeconomic status, cumbersome regimens, dislike of medication, and distant pharmacies. Nondrug factors that reduced the compliance were: Fears about side effects, anger about condition or its treatment, forgetfulness or complacency, and patient's ill attitudes toward health. After employing the various strategies for improving the compliance in these patients, the compliance increased in 176 patients (57.3%) among the earlier defaulted patients, while the remaining 131 patients (42.7%) were found to be noncompliant even after various educational techniques.
Conclusion:
Noncompliance in asthma management is a fact of life and no single compliance improving strategy probably will be as effective as a good physician-patient relationship. Optimal self-management allowing for optimization of asthma control by adjustment of medications may be conducted by either self-adjustment with the aid of a written action plan or by regular medical review. Individualized written action plans based on peak expiratory flow are equivalent to action plans based on symptoms.
Keywords: Bronchial asthma, compliance, health education, nonadherence, self-action plan
Introduction
Bronchial asthma is a major public health problem affecting a large number of individuals of all ages. Globally, 100-150 million people suffer from asthma. India has 20-28 million asthmatics and the prevalence amongst children (5-11 years) is 10-15%. Being a chronic medical condition, management of bronchial asthma requires continuous medical care. Modern management of bronchial asthma requires prolonged medications. A key issue in proper management of bronchial asthma is adherence to treatment. Poor compliance to prescribed therapy increases morbidity and mortality and it is increasingly being documented that long-term compliance or adherence to prescribed therapy is difficult to attain.[1] Studies have reported that 50% of patients with a chronic disease do not use their medication at all or do not use it as prescribed.[2] Important reason for poor compliance is that patients with a chronic disease do not have a satisfactory understanding of their condition. The economic burden of bronchial asthma to the society is well-documented in industrialized countries,[3] and is a great burden to the health services. Poor asthma control is responsible for a large proportion of the total cost of the disease, for the patient as well as to the society, and thus responsible for the both direct and indirect cost of therapy.
The present study was undertaken to study the factors that influence patient's compliance with prescribed medications, and to assess the impact of health education and self-action plan in improving the compliance in bronchial asthma patients.
Materials and Methods
The present study was a prospective study done at a tertiary care hospital over a period of 2 years from June 2010 to May 2012. Children above 10 years of age and adults with the diagnosis of bronchial asthma as per Global Initiative for Asthma (GINA) guidelines[4] were included in the study. Patients with acute severe asthma, chronic obstructive pulmonary disease (COPD), and cardiac asthma were excluded. All patients were interviewed using a standard interview schedule and requested to maintain a diary regarding the dosing of aerosol therapy. Apart from a detailed history, physical examination, pulmonary function test, and peak expiratory flow rate were measured during the first visit. All the patients were treated according to GINA guidelines under the supervision of chest physicians. Regarding the use of medications, the choice was left to the treating chest physician. All patients were followed-up every 15 days for 12 weeks. At the end of 12 weeks, compliance to treatment was calculated after studying the patient diary noting and frequency of the hospital visits. Control of the disease was assessed by pulmonary function testing and peak expiratory flow rate measurements. Compliant day was defined as one in which the prescribed number of puffs (metered dose inhalers (MDI)) or dry powder inhalation capsules were taken each day. Patient was said to be compliant if he/she had taken more than 80% of the prescribed medicines during the study period.
Second step in this study was to impart health education in the nonadherent patients. We tried to improve the compliance by imparting the patient education program with the help of health educator. Various strategies which were employed for the patient education included verbal praise, interactive communication skills, tailoring the medications to the patient's routine, conducting asthma awareness camps for the defaulted patients, distribution of literature regarding asthma, and its consequences in the local languages and answering to the family's worries regarding bronchial asthma. At this stage, all the nonadherent patients were given detail health education regarding bronchial asthma, its allergy status, chronicity of the disease, and duration of treatment, nature of quick relief and long term medications, and preventive aspects of the disease with the help of health educator. All the patients were asked to keep a diary of any symptoms occurring during this period. Also an action plan was provided by the treating physician for all the noncompliant cases, explaining what to do in case of increase in the symptoms, or during any exacerbations, when to take oral steroids, and when to call the doctor. This will help the patient to be more interactive and be more communicable with the doctor. In the second step, all the patients were followed-up for another 12 weeks. Final assessment was done at the end of this period only. The study was approved by the Institutional Ethical Board.
The economic status was classified as per modified B. G. Prasad classification.[5] Income levels initially proposed by Prasad can be converted into currently applicable levels by multiplying with a factor of 0.0493 × prevailing level of All India Consumer Price Index (AICPI). The average AICPI during the study period was 26. Hence, the per capita income in class I was Rs. 2,600 per head per month, in class II it was Rs. 1,300-2,340 per head per month, in class III it was between Rs. 780 and 1,274 per head per month, in class IV it was Rs. 390-754 per head per month, and class V less than Rs. 390 per head per month.
Statistical analysis
Data are expressed as the mean (standard deviation (SD)). Comparison of parameters between two groups was done by Student's t-test. Comparisons among three groups were done by one-way analysis of variance (ANOVA) with Bonferroni's multiple comparison tests. Differences in frequency between compliance and noncompliance patients were assessed by the Chi-square test. A P value of less than 0.05 was considered significant.
Results
A total of 500 patients were studied during the period. The majority of the patients (39%) were in the age group of 21-40 years. The male: female ratio was 3:2. Majority of patients 290 (58%) had either primary or secondary education and 10% were illiterate. The majority of the patients belonged to middle socioeconomic status [Table 1].
Table 1.
Baseline characteristics of the patients
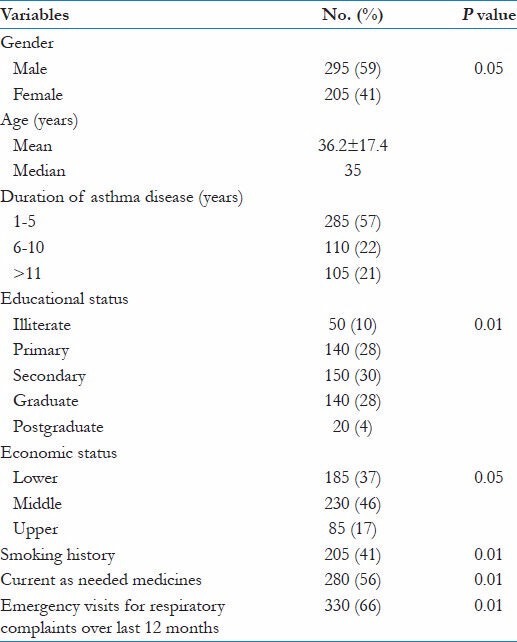
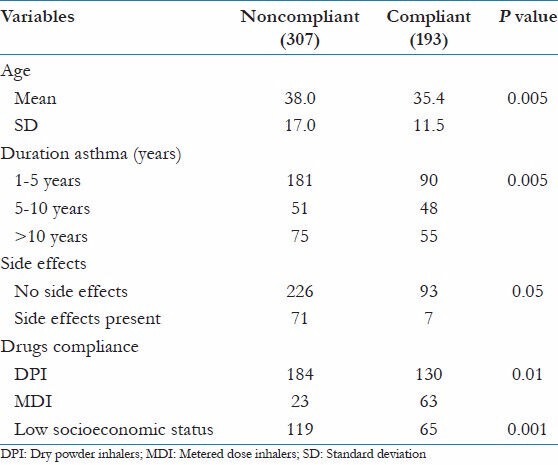
Nearly one-third of the patients (193 patients, 38.6%) were regular to aerosol therapy and did not miss a single dose and the remaining 61.4% were noncompliant. Among male patients, regular compliance was observed in 121 patients, while 72 female patients were regular to therapy. A higher number of male patients missed more than 20 doses over duration of 12 weeks (56.6%) as compared to female patients (43.3%). There was significant correlation between the educational status and the compliance to the therapy. Socioeconomic status of the patient was a significant risk factor associated with the noncompliance to the therapy. More than two-third of patients (80%) were using dry powder inhalers (DPI), and 20% were using MDI, and remaining 18 patients (6%) used combination of the drugs [Table 2].
Table 2.
Factors affecting compliance for aerosol therapy
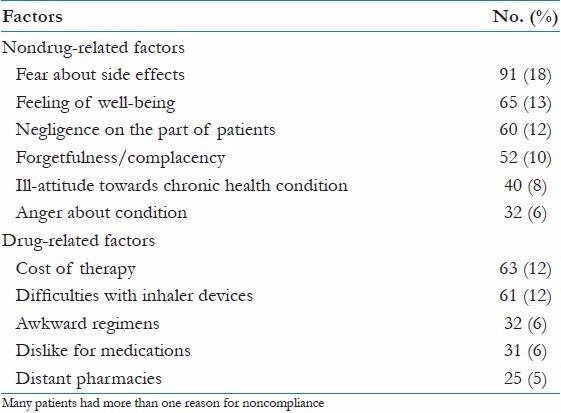
Nondrug factors were the key reasons for nonadherent to the aerosol therapy [Table 3]. The major nondrug factors associated with poor compliance were: Fear about side effects to the medications (18%), higher cost of the therapy (10%), feeling of well-being on therapy (8%), and negligence on the part of the patients (7%). Other reasons included forgetfulness or complacency and attitudes toward ill-health, anger about condition, etc., Drug-related reasons for noncompliance included difficulties with inhaler devices, awkward regimes (e.g. four times daily or multiple drugs), dislike of medications, and distant pharmacies.
Table 3.
Causes for non-adherence for asthma therapy
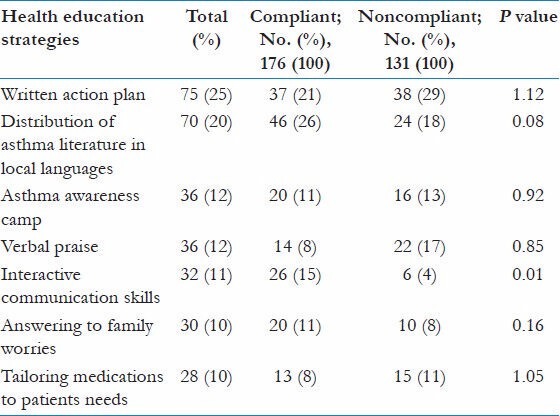
Various strategies were employed with the help of a health educator after 12 weeks of therapy to improve the patient's compliance to the aerosol therapy, and these patients were followed-up for a further duration of 12 weeks to evaluate the response to the intervention. We have tried to educate these bronchial asthma patients in different ways, so that it will help in improving the adherence to the therapy. These different ways included: Verbal praise (12%), interactive communication skills (11%), tailoring the medications to the patient's routine (10%), conducting asthma awareness camps for the defaulted patients (12%), distribution of literature regarding asthma and its consequences in local languages (20%), answering to the family's worry (10%), and written self-action plan (25%) [Table 4]. After 12 weeks of therapy, it was observed that the compliance improved in additional 176 patients (57.3%) who had defaulted earlier. The remaining 131 patients (42.7%) were found to be still nonadherent to the therapy. The improvement in the compliance was observed to be better in female patients (48.1%) as compared to male patients (26%). It was also observed that direct interaction with the patients or with the parents of asthma patients improved the compliance to a significant level.
Table 4.
Strategies employed for health education and its impact on compliance
Discussion
Bronchial asthma, a chronic lung disease that affects people of all ages, races, and ethnic groups, is a growing concern throughout the world. There is a need for educating the patient about asthma disease and medications used like DPI/MDI to be taken on regular basis as prescribed. In the study[6] conducted in Trinidad regarding the understanding and use of inhaler medication by asthmatics, it was observed that educating patients with a focus on children and the elderly, inhaler techniques, and reinforcing understanding of asthma medications could improve asthma management to a great extent.
Noncompliance to treatment programs is common in patients with bronchial asthma. Noncompliance is more common than usually suspected and rates vary from 20% to 80%.[7] True rates of noncompliance are hard to come by because patients do not accurately report and physicians often do not inquire critically. The rule-of-thumb in chronic nonlethal disease (i.e., asthma, hypertension, etc.) is that one-third of patients are compliant, one-third are somewhat compliant, and one-third are noncompliant. This is important because compliant patients are significantly less likely to experience exacerbations than less compliant patients.[8] A real problem is that although there is much known about why so many patients do not take their medicine, there is less solid information on how to actually improve compliance. Methods to improve compliance must be validated with objective data and outcome measurements before they can be recommended with confidence.[9] A word about compliance versus adherence, for mixed reasons, adherence seems to have become the preferred word.[10]
The present study was conducted to know compliance with aerosol therapy in bronchial asthma patients and reasons for noncompliance. An effort was also made to improve the patient compliance via the patient education program. In the present study a total of 307 patients (69%) were observed to be noncompliant to the asthma therapy. Noncompliance rates were more in male patients as compared to female patients. Rhodes et al.,[11] observed higher prevalence of asthma in female patients as compared to males. Females with current asthma, reported adult onset of asthma more often, and males reported childhood onset of symptoms more often. Gibson et al.,[12] conducted a study to study the compliance with inhaled asthma medications in preschool children. In preschool children, the parents supervise and are responsible for drug administration. In this study it was observed that parental supervision would result in good compliance. It was concluded that compliance with inhaled prophylactic therapy is poor in preschool children with asthma whose medication is administrated under parental supervision. Lewis and Lewis[13] investigated the consequences of empowering children to care for themselves.
Noncompliance depends on many factors and they are difficult to sort out.[14] Beliefs, perceptions, and experience constitute some of the variables associated with compliant medication taking behavior.[9] It had been suggested that race, crime, age, and other environmental factors are associated with compliance and noncompliance; but these are speculative.[15] Lindberg et al.,[16] studied various factors affecting the compliance in asthma patients and have identified five important factors regarding self-reported compliance with prescribed medications in patients with asthma: Age, gender, length of time with airway problems, whether the staff listen and take into account the patient's views concerning his/her asthma, and whether the patient has received information and education concerning asthma.
Educational status
There were 20 patients with higher education (postgraduation) and all these patients had regular compliance with the therapy. Patients having graduation degree (140 patients) also had better compliance (78%) with the medications. Patients having secondary education had a default rate of 60%, patients having primary education had a high default rate of 71.4%, while illiterate patients had a higher default rate 100%. Education status was thus a significant factor for the noncompliance to the therapy for asthma medications.
Valid educational program for asthmatics can improve the knowledge of the disease and to understand how they look after themselves by careful evaluation of their own symptoms and respiratory function. Patients attending two lessons with helpful training tools can increase significantly asthma knowledge, treatment compliance, and patient self-management.[17] In the present study economic status was significant and there was moderate correlation to compliance and low socioeconomic status. It was observed that there were higher default rates among lower socioeconomic class patients. Length of stay (LOS) and costs per discharge were studied from the Taiwan National Health Insurance Research Database covering the period from 1997 to 2001.[18] Study subjects were identified from the database by principal diagnosis of asthma or asthmatic bronchitis, with a total of 139,630 cases being included in the study. Multiple regression analyses were performed to explore the relationship between LOS, costs per discharge and hospital characteristics, adjusting for age, gender, and discharge status of patients, as well as complications or comorbidities. The regression analyses showed that, compared with district hospitals, medical centers and regional hospitals have longer and more statistically significant LOS, as well as higher costs. This study shows the existence of wide variations in LOS and costs per discharge for asthma hospitalizations, between the various types of hospitals.
Patient education in bronchial asthma is to provide the patient and the patient's family with suitable information and training so that the patient can keep well and adjust according to a planned medication. The factors involved in noncompliance in the present study are multifactorial. A total of 307 patients (69%) defaulted to the aerosol therapy; the default rate was higher (41% ) among female patients, while it was 59% among male patients. The most common reasons for the higher noncompliance rates were side effects to the medications (18%), higher cost of the therapy (10%), feeling of well-being on therapy (8%), and negligence on the part of the patients (7%). Other causes for noncompliance for therapy are drug factors which includes difficulties with inhaler devices, awkward regimes (e.g. four times daily or multiple drugs), and dislike for medication and distant pharmacies. Nondrug factors include fear about side effects (18%), anger about condition or its treatment (3%), forgetfulness or complacency (5%), and attitudes toward ill-health (5%).
Adherent patients had greater understanding about their illness and the options for managing the illness. They also had greater confidence that current management would keep their illness under control. Dowell and Hudson[19] concluded that accepting the recommended treatment, especially long-term treatment perceived as powerful, requires an acceptance of the illness. Recently, a study by George et al.,[20] observed suboptimal adherence for inhalation therapy to be 63% in patients with COPD. Adherent patients had greater understanding about their illness and options for managing the illness. They also had greater confidence that current management would keep their illness under control. Satisfaction with and faith in the treating physicians were found to be low among the less adherent group compared to highly adherent group.[17]
Differences in both intentional and unintentional health behaviors were observed between the two groups by George et al.[20] Adherent patients were less likely to be confused about their medications, which might have been result of their greater medication knowledge. “Routinization”, that is, the ability to fit to a medication regimen to one's daily routine, has been recognized as a major determinant of improved adherence.[20] Associated comorbid condition is also one of the important factors responsible for the noncompliance in therapy. Depression is known to be a risk factor for the nonadherene.[21] In the present study, any specific questions about depression in the questionnaire were avoided due to the sensitivity of the topic and concerns about patient nonresponse. Patient's acceptance of the disease process and recommended treatment, knowledge about and faith in the treatment, effective patient-clinician interaction, and routinization of drug therapy are critical for optional medication adherence in bronchial asthma patients. In early consultation; for example, different inhaler devices should be demonstrated and patients should take part in a decision as to which is most suitable for them. In the present study, strategies to improve patients compliance was undertaken like tailoring the medications to patients routine (10%), review the patients self-management plan (8%), patients were given special attention and encouragement (8 + 8%), they were praised for their inhaler techniques (12%), some of the patients' family worries were answered (10%). and there was use of interactive communications techniques (11%). A detailed written action plan was also given for all the defaulted patients. This enumerated what action to be taken in certain situations. A separate asthma awareness camp was also conducted for these nonadherent patients. Patient education program was organized for the noncompliant patients with the help of a psychologist regarding adherence to the therapy was reiterated again and again. Patients were given adequate opportunity to express their expectation of both the asthma and its treatment. In a study conducted in Sweden on compliance with medications in asthma patients, the important factors that resulted in noncompliance were: Age, gender, duration of the disease, and patients' view on asthma.[22]
The major methods that have been proposed and tried to improve compliance include improved dosing schedules, patient education, and improved communication between physician and the patient. It has been well-established that less frequent dosing and simple schedules works best.[23] It is less certain that patient education and/or provider involvement by themselves make a significant difference in the long run.[24] The following are thought to improve compliance: Specific patient written instructions, patient diaries, physician/provider interest, less frequent dosing, long-acting drugs, a simplified dose schedule, pro re nata (p.r.n.) dosing, self-management, and shorter course of therapy. Patient education plays an important role in improving the adherence in such a chronic disease like bronchial asthma. Hence, every effort should be made to motivate these patients at every visit. Motivational interviewing (MI) is one approach to building patient motivation for adherence.[25] MI is a patient-centered style of communication specifically geared toward resolving ambivalence and building motivation for change. It focuses on creating a comfortable atmosphere without pressure or coercion to change. MI was originally described by Miller,[26] and the theory and practice of MI has been expanded upon in several seminal texts and in several hundred peer-reviewed papers. MI views ambivalence as part of the natural process of change—a phase that people must go through before fully committing to a decision.[27]
Although extensive research has been done in efforts to understand and improve compliance in asthma, little progress has been made in cutting the rate of noncompliance.[28] It is frustrating and goes against our intuition and training that spending time and effort, interacting with patients, and building rapport does not seem to be very effective in improving compliance.[29] It is better to design programs that are more convenient and comfortable. Patients take drugs only if they agree that these agents are more beneficial than disruptive.[30]
Conclusion
The percentage of regular compliance on aerosol therapy in bronchial asthma is 31%, and noncompliance is 69% which is significantly high. Regular compliance is an important aspect in the management and control of bronchial asthma, so patients should be advised to take regular and long-term aerosol therapy for reducing the acute attacks of asthma and maintaining the disease state. Patients who have faith in the physician and the prescribed method of treatment are more likely to adhere to the treatment than patients who have a negative attitude toward treatment. The same is true of the parents of children with asthma. People with asthma should be offered education and written asthma action plans that focus on their individual needs-this is a reinforcement of earlier advice.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Chochrane GM. Compliance and outcomes in patients with asthma. Drugs. 1996;52:S12–9. doi: 10.2165/00003495-199600526-00004. [DOI] [PubMed] [Google Scholar]
- 2.Antonello N. The problem of adherence in the management of bronchial asthma: An educational ambulatory course called “The School of Asthma”. Tanaffos. 2009;8:14–8. [Google Scholar]
- 3.Barnes PJ, Jonsson B, Klim JB. The costs of asthma. Eur Respir J. 1996;9:636–42. doi: 10.1183/09031936.96.09040636. [DOI] [PubMed] [Google Scholar]
- 4.Global Initiative for Asthma (GINA) Global strategy for Asthma Management and Prevention. Bethesda, National Institute of Health, (Revised 2011) 2011. [Last accessed on 2012 Dec 20]. Available from: http://www.ginasthma.com .
- 5.Prasad BG. Changes proposed in the social classification of Indian families. J Indian Med Assoc. 1970;55:198–9. [PubMed] [Google Scholar]
- 6.Pinto Pereira LM, Clement Y, Da Silva CK, McIntosh D, Simeon DT. Understanding and use of inhaler medication by asthmatics in specialty care in Trinidad: A study following development of Caribbean guidelines for asthma management and prevention. Chest. 2002;121:1833–40. doi: 10.1378/chest.121.6.1833. [DOI] [PubMed] [Google Scholar]
- 7.Rand CS, Wise RA. Measuring adherence to asthma medication regimens. Am J Respir Crit Care Med. 1994;149:S69–S76. doi: 10.1164/ajrccm/149.2_Pt_2.S69. [DOI] [PubMed] [Google Scholar]
- 8.Stern L, Berman J, Luwry W, Katz L, Wang L, Rosenblatt L, et al. Medication compliance and disease exacerbation in patients with asthma: A retrospective study of managed care data. Ann Allergy Asthma Immunol. 2006;97:402–8. doi: 10.1016/S1081-1206(10)60808-3. [DOI] [PubMed] [Google Scholar]
- 9.Fernando GN, De Silva KH. Adherence to the National Guidelines on the management of bronchial asthma: A cross-sectional study in Medical Clinics in Teaching Hospital, Karapitiya. Galle Med J. 2010;15:8–13. [Google Scholar]
- 10.Kaisar HB. Compliance and noncompliance in asthma. Allergy Asthma Proc. 2007;28:514–6. doi: 10.2500/aap2007.28.3040. [DOI] [PubMed] [Google Scholar]
- 11.Rhodes L, Moorman JE, Redd SC. Sex differences in asthma prevalence and other diseases characteristics in eight states. J Asthma. 2005;42:772–82. doi: 10.1080/02770900500308387. [DOI] [PubMed] [Google Scholar]
- 12.Gibson NA, Ferguson AE, Aitchson TC, Patson JY. Compliance with inhaled asthma medication in preschool children. Thorax. 1995;50:1274–9. doi: 10.1136/thx.50.12.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lewis MA, Lewis CE. Consequences of empowering children to care for themselves. Pediatrician. 1990;17:63–7. [PubMed] [Google Scholar]
- 14.Juniper EF. The impact of patient compliance on effective asthma management. Curr Opin Pulm Med. 2003;9(Suppl 1):S8–10. doi: 10.1097/00063198-200304001-00003. [DOI] [PubMed] [Google Scholar]
- 15.Williams LK, Joseph CL, Peterson EL, Moon C, Xi H, Krajenta R, et al. Race-ethnicity, crime, and other factors associated with adherence to inhaled corticosteroids. J Allergy Clin Immunol. 2007;119:168–75. doi: 10.1016/j.jaci.2006.09.029. [DOI] [PubMed] [Google Scholar]
- 16.Lindberg M, Estrom J, Moller M, Ahlner J. Asthma care and factors affecting medication compliance: The patient's point of view. Int J Qual Health Care. 2001;13:375–83. doi: 10.1093/intqhc/13.5.375. [DOI] [PubMed] [Google Scholar]
- 17.Cegala DJ, Marinelli T, Post D. The effects of patient communication skills training on compliance. Arch Fam Med. 2000;9:57–64. doi: 10.1001/archfami.9.1.57. [DOI] [PubMed] [Google Scholar]
- 18.Lin HC, Kao S, Wen HC, Wu CS, Chung CL. Length of stay and costs for asthma patients by hospital characteristics: A five-year population-based analysis. J Asthma. 2005;42:537–42. doi: 10.1080/02770900500214783. [DOI] [PubMed] [Google Scholar]
- 19.Dowell J, Hudson H. A qualitative study of medication-taking behaviour in primary care. Fam Pract. 1997;14:369–75. doi: 10.1093/fampra/14.5.369. [DOI] [PubMed] [Google Scholar]
- 20.George J, Kong DC, Thoman R, Stewart K. Factors associated with medication non-adherence in patients with COPD. Chest. 2005;128:3198–204. doi: 10.1378/chest.128.5.3198. [DOI] [PubMed] [Google Scholar]
- 21.Dimatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 22.Ryan GW, Wagne GJ. Pill taking “routinization”: A critical factor to understanding episodic medication adherence. AIDS Care. 2003;15:795–806. doi: 10.1080/09540120310001618649. [DOI] [PubMed] [Google Scholar]
- 23.Riekert KA, Butz AM, Eggleston PA, Huss K, Winkelstein M, Rand CS. Caregiver-physician medication concordance and undertreatment of asthma inner-city children. Pediatrics. 2003;111:E214–20. doi: 10.1542/peds.111.3.e214. [DOI] [PubMed] [Google Scholar]
- 24.Abudahish A, Bella H. Adherence of primary care physicians in Aseer region, Saudi Arabia to the National protocol for the Management of Asthma. East Mediterr Health J. 2010;16:171–5. [PubMed] [Google Scholar]
- 25.Alex J. Med Perception of primary care physicians about guidelines of bronchial asthma. 2013. [Last accessed on 2012 Dec 22]. Available from: http://dx.doi.org/10.1016/j.ajme . 2013.05.002.
- 26.Miller WR. Motivational interviewing with problem drinkers. Behav Psychother. 1983;11:147–72. [Google Scholar]
- 27.Treharne GJ. Adherence to medication (letter) N Engl J Med. 2005;353:1973. [PubMed] [Google Scholar]
- 28.Bender BG, Bender SE. Patient-identified barriers to asthma treatment adherence: Response to interviews, focus groups, and questionnaires. Immunol Allergy Clin North Am. 2005;25:107–30. doi: 10.1016/j.iac.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Brown MD, Reeves MJ, Meyerson K, Korzeniewski SJ. Randomized trial of a comprehensive asthma education program after an emergency department visit. Ann Allergy Asthma Immunol. 2006;97:44–51. doi: 10.1016/S1081-1206(10)61368-3. [DOI] [PubMed] [Google Scholar]
- 30.Gillissen A, Buschi K, Juergens U. Adherence to therapy in bronchial asthma. Dtsch Med Wochenschr. 2007;132:1281–6. doi: 10.1055/s-2007-982028. [DOI] [PubMed] [Google Scholar]


