Abstract
Protein energy malnutrition (PEM) is a major public health problem in India. This affects the child at the most crucial period of time of development, which can lead to permanent impairment in later life. PEM is measured in terms of underweight (low weight for age), stunting (low height for age) and wasting (low weight for height). The prevalence of stunting among under five is 48% and wasting is 19.8% and with an underweight prevalence of 42.5%, it is the highest in the world. Undernutrition predisposes the child to infection and complements its effect in contributing to child mortality. Lalonde model (1974) is used to look into the various determinants of PEM in under five children and its interrelation in causation of PEM. The determinants of PEM are broadly classified under four distinct categories: Environmental factors including the physical and social environment, behavioral factors, health-care service related and biological factors. The socio-cultural factors play an important role wherein, it affects the attitude of the care giver in feeding and care practices. Faulty feeding practice in addition to poor nutritional status of the mother further worsens the situation. The vicious cycle of poor nutritional status of the mother leading to low birth weight child further exposes the child to susceptibility to infections which aggravates the situation. However, it is seen that percapita income of the family did not have much bearing on the poor nutritional status of the child rather lack of proper health-care services adversely contributed to poor nutritional status of the child. PEM is a critical problem with many determinants playing a role in causing this vicious cycle of undernutrition. With almost half of under five children undernourished in India, the Millennium Development Goal (MDG) of halving the prevalence of underweight by 2015 seems a distant dream.
Keywords: India, protein energy malnutrition, under five children, undernutrition
Introduction
According to World Health Organization, protein energy malnutrition (PEM) refers to “an imbalance between the supply of protein and energy and the body's demand for them to ensure optimal growth and function”.[1] It is a major public health problem in India. It affects particularly the preschool children (<6 years) with its dire consequences ranging from physical to cognitive growth and susceptibility to infection. This affects the child at the most crucial period of time of development which can lead to permanent impairment in later life.[2,3]
PEM is measured in terms of underweight (low weight for age), stunting (low height for age) and wasting (low weight for height). The prevalence of stunting among under five is 48% (moderate and severe) and wasting is 20% (moderate and severe) and with an underweight prevalence of 43% (moderate and severe),[4] it is the highest in the world. The majority of children suffering from undernutrition (80%) are the mild and the moderate forms which go unnoticed[3] and the early ages are affected more which makes the process irreversible. In comparison to the global reference standards, the weight for age distribution of Indian children falls to the left of the curve [Figure 1].
Figure 1.
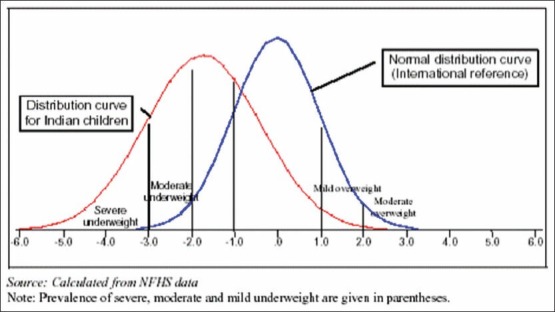
Weight-for-age distribution: Children under three in India compared to the global reference population
Undernutrition makes the child susceptible to infection and complements its effect in contributing to child mortality. This accounts for 22% of the burden of disease in India and adversely affects the economic growth of the country with an estimated adult productivity loss of 1.4% of gross domestic product (GDP).[2]
In order to ensure that adequate amount of food is available to the household, it is necessary for the family to be food secure.[5] The National Food Security Bill, 2010 Launched by the Government of India is a step forward in sustaining food availability to marginalized groups who are at a vulnerable position to be worst hit by food insecurity. According to the bill, “legal entitlement to subsidized food grains to be extended to at least 75% of the country's population 90% in rural areas and 50% in urban areas”.[6] It is seen that food unavailability, inadequate purchasing power or inappropriate utilization at household level contributes to food insecurity.[7] However, though the per capita food production increased by 75% in the past two decades, ironically this has not reflected in nutrition and food security, which still remains high.[8] The disturbing fact is that income, poverty and nutritional deprivation is not moving in the same direction. Despite an increase in per capita food production and decline in poverty, India continues to feature increased rates of undernutrition.[8] Therefore, it becomes necessary to distinguish the determinants responsible for persisting high undernutrition in the light of improvement in poverty status and food availability.
With an annual per capita growth rate of 3% (1990-2002), the reduction in underweight prevalence to 39% among children under three is estimated by the year 2015, but is “still short of the MDG” and even if India achieves the MDG goal, the prevalence will still be higher than the Sub Saharan African region.[2] PEM is a critical problem with many determinants playing a role in causing this vicious cycle of undernutrition.
This paper looks into the various determinants of PEM in under five children and its interrelation in causation of PEM using the Lalonde model[9] [Figure 2].
Figure 2.
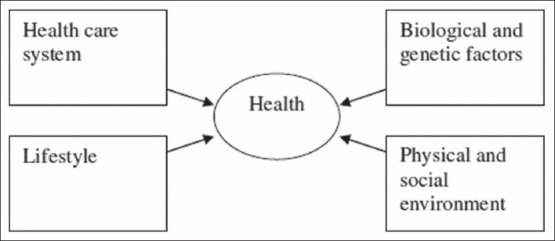
Lalonde basic health field model
Determinants of PEM
Environment
Socio-cultural factors affecting feeding practices
Appropriate child feeding behavior goes a long way in preventing and overcoming malnutrition and determining a child's growth.[2] As feeding practice changes with age, a fourfold increase in the prevalence of undernutrition is seen from 15.4% (0-6 months) to 52.6% (12-23 months).[10] This can be attributed to early initiation of complementary feeds in the earlier months and late weaning and inadequate amount of complementary feeds in the later months.[11] A delay in the initiation of breast feeding, lack of colostrum and inappropriate complementary feeding were significantly associated with underweight and stunting.[12]
Inappropriate feeding practices are closely related to cultures and beliefs. Mothers feed their children with prelacteal feeds to cleanse their intestines and did not initiate complementary feeds thinking that it will lead to infections.[13] Beliefs like considering colostrums as witch's milk and cultural practices of prelacteal feeds exposed the child to infections which contributes to undernutrition.[14] The feeding practices come up as a major concern in combating undernutrition with hidden cultural values and beliefs.
Maternal nutrition
Maternal nutritional status has a direct relation to the child's nutritional status.[15] An undernourished mother gives birth to a low birth weight baby who grows up with compromised feeding and infections to a stunted child and adolescent and carries this vicious life cycle approach by giving birth to an underweight child.[16] Women with height <145 cm and body mass index <18.5 are likely to give birth to low birth weight children.[15] With a low birth weight prevalence of 28%, these children are already compromised before birth.
Infection
The vicious cycle of infection and undernutrition go hand in hand. With inadequate dietary intake, the immune response gets weaker and increases susceptibility to infections. A single episode of infection is easy to regain but if the child suffers from repeated infections without adequate dietary intake, it becomes difficult to regain normal growth. Infection was commonly diagnosed in children suffering from undernutrition.[17] One of the first studies to associate infection and malnutrition was cited from India where children developed diarrhea during the weaning period which resulted in growth faltering (Gordon et al., 1964; Scrimshaw et al., 1968 cited in Gragnolati et al.[2]). 46.8% of infants suffering from acute diarrhea were underweight and it was worse for those children having persistent diarrhea (83.35%).[18] Respiratory infections were found to be the second common infection.[19] Measles and helminthic infections too contribute to undernutrition by increasing demand for proteins and calories but reducing its absorption and utilization.[3] It shows that infection and undernutrition complements the effect of each other and cannot be managed separately.
Gender
National Family Health Survey II (NFHS II) reported an underweight prevalence of 48.9% among girls compared with boys (45.5%). Even the proportion of severe underweight was higher for girls (18.9%) than boys (16.9%) (NFHS II, 1998-99 cited in Gragnolati et al.[2]). Similar findings were noticed in West Bengal where undernutrition among girls (54.8%) exceeded those of boys (46.8%) and the difference was higher for moderate and severe forms.[20] However, these differences are not merely biological but the care and feeding practices makes up for the difference. Timely feeding and continuation of breast feeding was seen more among boys than girls.[21] The median duration of breast feeding was 2 months longer for boys than girls. Early weaning of the girl child was done to increase chances of having a boy in the next pregnancy.[15] Therefore, the gender inequality of male preference over female among the care givers is responsible for the difference in prevalence of undernutrition.
Mother's literacy status
A decreasing trend in all forms of undernutrition is observed where the literacy status of mother increased.[22] Children of illiterate women were twice as likely to show signs of underweight and stunting as those who had at least completed high school. Children whose mothers were illiterate showed 3 times higher prevalence of wasting than literate mothers.[15,23,24] Increasing literacy status of a mother has a positive effect in reducing undernutrition since she is the first contact of care for the child and a more informed and literate mother is at a better position to take care of her child.
Poverty and income
Undernutrition is more common in the lower income groups and even if malnutrition is present in the upper income group, it is limited to the milder forms.[22] There is over representation of “backward” caste and socially excluded groups in the society among the poor people, which exposes them to further disadvantages of poverty, food insecurity and undernutrition.[25] NFHS II findings suggest a twofold increase in undernutrition among children belonging to households with low standard of living than with a high standard of living.[15] Though 26% of people live below the poverty line in India, 46% of under three children are suffering from undernutrition.[26] This shows that the prevalence of poverty solely cannot be responsible for undernutrition but is an underlying cause of factors like inadequate dietary intake, large family, infection, unhygienic environment and illiteracy which contributes to undernutrition among low income group.
Urban-rural difference
NFHS data shows that except Tripura, the prevalence of undernutrition is higher in rural than urban children in all states.[10] The urban and rural variations are large with prevalence of 50% in rural when compared with 38% in urban children.[2] Stunting was seen more among the rural children (74.5%), but undernutrition was lower among urban children, majority were wasted (30.3%).[27] It shows that rural undernutrition is related more towards food insecurity whereas the problem of undernutrition is more acute in urban areas.[28] However with 26% below the poverty line in urban areas, it is catching up with the rural areas (29%) and undernutrition might not remain only a rural problem.[29]
Life-style and behavior
The life-style and behavior of the child itself does not contribute to undernutrition, but the child feeding practices of the mother and care givers affect the dietary intake of the child. Since the care givers and mother belong to the environment of the child, the feeding practices have been discussed in the environment section.
Health-care services
The Integrated Child Development Services (ICDS) scheme has an empirical role in combating undernutrition whose services include supplementary nutrition, health checkups and growth monitoring. But even after 35 years of its initiation, the problem of undernutrition still persists and the decrease in the prevalence is relatively low.
The program has given more attention to coverage rather than quality-of-care. It has neglected aspect of educating parents on improving nutrition through proper child care and feeding behavior within the family budget, but focused more on food distribution. Even when the ICDS coverage is as high as 90% in few states, the utilization is limited to 28% among under six children.[23] In addition to it, inadequate skills of the staff, lack of logistics and poor supervision has added to the problem.[2]
However, there are examples of good implementation of services for e.g. States like Kerala and Tamil Nadu with a low per capita income still have low undernutrition prevalence (Kerala: 23% and Tamil Nadu: 30%) due to good health services. States where the ICDS enrolment is lower show a higher prevalence of undernutrition. Bihar with prevalence of 55% has very low ICDS beneficiaries of 1.5%, whereas the north eastern states with a fairer picture of undernutrition (20-30%) have the highest ICDS beneficiaries.[2] Therefore, access and quality-of-care are both important features of a good health-care service.
Biological
Age
The prevalence of underweight rapidly increased from 11.9% (<6 months) to 37.5% (6-11 months) to 58.5% among 12-23 months old children. Stunting prevalence also rose from 15.4% (<6 months) to 57.5% among 12-23 months.[15] A study in Jhansi found an increase in undernutrition from 52.3% (0-1 years) to 80.9% among 1-3 years children.[30] These variations are not just due to increasing age, but the dietary changes have a positive role in affecting nutritional status.
Birth order and birth interval
The proportion of undernutrition in higher birth order (>3) was more at risk of undernutrition than those with first birth order.[22] NFHS II observed that lower birth orders were an advantage.[15] The prevalence of undernutrition declined from a birth order of 3 (48.5%) to 1 (20.38%). Severe undernutrition was not seen in children with first birth order.[22]
A decrease in the prevalence of underweight is seen when the birth interval widens from 24 months (52.2%) to 47 months (45.1%) as well as for stunting with an 8% decrease with increasing interval. Mothers belonging to households with many children did not have time to care and feed each one of them.[31] Frequent childbirth at short interval does not allow the mother to regain her heath for the next pregnancy resulting in a low birth weight child and short intervals of childbirth results in early weaning of the earlier child from breast milk.
Conclusion
India stands at a very vulnerable position with one of the highest prevalence of undernutrition in the world in spite of improvement in food availability and poverty alleviation. In addition to it, numerous determinants play a role in its causation. The interplay of these determinants and their complementary effect makes it difficult to isolate one key factor in causing undernutrition.
For example, age cannot be dealt in isolation since faulty feeding practices have a complementary effect in causing undernutrition. The socio-cultural factors play an important role wherein, it affects the attitude of the care giver in feeding and care practices. The compromised nutritional status of the mother comes up as a direct determinant in producing a low birth weight baby, worse if the child is born to a large and poor family. This further worsens the condition with susceptibility to infections and lack of health care services. Evidence shows that states with low percapita income have better undernutrition figures as compared with the richer states due to better implementation of health care services, which shows that low income capability of the family is not always responsible for undernutrition.
The MDG goal of halving the prevalence of underweight by 2015 seems a distant target if the determinants are dealt in isolation. It requires a holistic approach due to the complex interrelation of factors in causation of PEM, which has continued to haunt India as a silent crisis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Onis MD, Blossner M. WHO global database on child growth and malnutrition. WHO. 1997. [Last retrieved on 2010 Oct 01]. Available from: http://whqlibdoc.who.int/hq/1997/WHO_NUT_97.4.pdf .
- 2.Gragnolati M, Shekar M, Gupta MD, Bredenkamp C, Lee YK. India's Undernourished Children: A Call for Reform and Action. Washington, DC: World Bank; 2005. [Google Scholar]
- 3.Park K. Parks Textbook of Preventive and Social Medicine. 19th ed. Jabalpur: Banarsidas Bhanot; 2007. Nutrition and health; p. 507. [Google Scholar]
- 4.UNICEF. The state of the world's children. Adolescence: Children with disabilities. 2013. [Last retrieved on 2013 Aug 10]. Available from: http://www.unicef.org/sowc2011/
- 5.UNICEF. Underlying causes of undernutrition: Food insecurity. Food insecurity. [Last retrieved on 2013 Aug 11]. Available from: http://www.unicef.org/nutrition/training/2.5/9.html .
- 6.NFSB. Report of the expert committee on national food security bill. 2010. [Last retrieved on 2013 Aug 16]. Available from: http://eac.gov.in/reports/rep_nfsb.pdf .
- 7.FAO. Hunger portal. 2013. [Last retrieved on 2013 Aug 11]. Available from: http://www.fao.org/hunger/en/
- 8.Chand R, Jumrani J. Food security and undernourishment in India: Assessment of alternative norms and the income effect. Indian J Agric Econ. 2013;68:39–53. [Google Scholar]
- 9.Lalonde M. A new perspective on the health of Canadians: Working document. 1974. [Last retrieved on 2010 Oct 07]. Available from: http://www.hc-sc.gc.ca/hcs-sss/alt_formats/hpb-dgps/pdf/pubs/1974-lalonde/lalonde-eng.pdf .
- 10.Nutritional status in infancy and early childhood. 2008. [Last retrieved on 2010 Oct 02]. Available from: http://wcd.nic.in/research/nti1947/7.5%20iycn%203.2.2008%20prema.pdf .
- 11.Ramachandran P, Gopalan HS. Undernutrition and risk of infections in preschool children. Indian J Med Res. 2009;130:579–83. [PubMed] [Google Scholar]
- 12.Kumar D, Goel NK, Mittal PC, Misra P. Influence of infant-feeding practices on nutritional status of under-five children. Indian J Pediatr. 2006;73:417–21. doi: 10.1007/BF02758565. [DOI] [PubMed] [Google Scholar]
- 13.Hasan J, Khan Z, Sinha SN. Socio-cultural factors influencing nutritional status of infants - A longitudinal study. Indian J Matern Child Health. 1991;2:84–6. [PubMed] [Google Scholar]
- 14.Deshpande JD, Giri PA, Phalke DB, Phalke VD, Kalakoti P, Syed M. Socio-cultural practices in relation to breast feeding, weaning and child rearing among Indian mothers and assessment of nutritional status of children under five in rural India. Australas Med J. 2010;3:618–24. [Google Scholar]
- 15.National Family Health Survey (NFHS) II Report (1998-1999) Ministry of Health and Family Welfare India. [Last retrieved on 2010 Oct 01]. Available from: http://www.nfhsindia.org/india1.html .
- 16.Christian P. Maternal height and risk of child mortality and undernutrition. JAMA. 2010;303:1539–40. doi: 10.1001/jama.2010.469. [DOI] [PubMed] [Google Scholar]
- 17.National Nutrition Monitoring Bureau (NNMB) Diet and nutritional status of rural population, Technical report 21, India. 2002. [Last retrieved on 2010 Oct 03]. Available from: http://www.nnmbindia.org/NNMBREPORT2001.web.pdf .
- 18.Umamaheswari B, Biswal N, Adhisivam B, Parija SC, Srinivasan S. Persistent diarrhea: Risk factors and outcome. Indian J Pediatr. 2010;77:885–8. doi: 10.1007/s12098-010-0125-y. [DOI] [PubMed] [Google Scholar]
- 19.Sharma ML. A study of malnutrition and associated infection in children in an urban private hospital in India. Malnutrition and Infection. 2001. [Last retrieved on 2010 Oct 03]. Available from: http://www.capgan.org/malinf.htm .
- 20.Banerjee B, Mandal ON. An intervention study in malnutrition among infants in a tribal community of West Bengal. Indian J Community Med. 2005;30:27–9. [Google Scholar]
- 21.Pal I, Chaudhuri RN. Gender inequalities while rearing of children under 5 years in a rural area of West Bengal. Indian J Community Med. 2007;32:215–6. [Google Scholar]
- 22.Harishankar, Dwivedi S, Dabral SB, Walia DK. Nutritional status of children under 6 years of age. Indian J Prev Soc Med. 2004;35:156–62. [Google Scholar]
- 23.National Family Health Survey (NFHS) III Report (2005-2006) Ministry of Health and Family Welfare India. [Last retrieved on 2010 Oct 01]. Available from: http://www.nfhsindia.org/NFHS.../NFHS 3%20Nutritional%20Status%20of%20Children.ppt .
- 24.National Family Health Survey (NFHS) I Report (1992-1993) Infant feeding and child nutrition. [Last retrieved on 2010 Oct 01]. Available from: http://www.nfhsindia.org/india1.html .
- 25.Cohen M, Tirado C, Aberman NL, Thompson B. World Food Insecurity and Malnutrition: Scope, Trends, Causes and Consequences. Rome: International Food Policy Research Institute (IFPRI), Food and Agriculture Organization of the United Nations (FAO) 2008 [Google Scholar]
- 26.Mendelson S, Chaudhuri S. Child malnutrition in India: Why does it persist? Child in Need Institute (CINI) [Last retrieved on 2010 Oct 07]. Available from: http://www.cini.org.uk/childmalutrition.pdf .
- 27.Jha R, Gaiha R, Kulkarni VS. Child undernutrition in India. ASARC working paper. 2010. [Last retrieved on 2010 Oct 16]. Available from: http://rspas.anu.edu.au/papers/asarc/WP2010_11.pdf .
- 28.Haddad L, Ruel MT, Garrett JL. Are urban poverty and undernutrition growing. Some newly assembled evidence? World Dev. 1999;27:1891–904. [Google Scholar]
- 29.Haub C, Sharma OP. What is poverty, really? The case of India. Population Reference Bureau. 2010. [Last retrieved on 2010 Oct 15]. Available from: http://www.prb.org/articles/2010/indiapoverty.aspx .
- 30.Chakraborty S, Gupta SB, Chaturvedi B, Chakraborty SK. A study of protein energy malnutrition (PEM) in children (0.6 year) in a rural population of Jhansi district (U.P.) Indian J Community Med. 2006;31:291–2. [Google Scholar]
- 31.Svedberg P. Why malnutrition in shining India persists. 2008. [Last retrieved on 2010 Oct 03]. Available from: http://www.isid.ac.in/~pu/conference/dec_08_conf/Papers/PeterSvedberg.pdf .


