Abstract
Natural eye lens is a crystalline substance to produce a clear passage for light. Cataract is opacity within the clear lens of the eye and is the dominant cause of socio-medical problem i.e., blindness worldwide. The only available treatment of cataract is surgery. However, insufficient surgical facilities in poor and developing countries and post-operative complications inspire researchers to find out other modes of treatment for cataract. In this review, an attempt has been made to appraise various etiological factors of cataract to make their perception clear to build up counterpart treatment. Present study is an assortment of various available literatures and electronic information in view of cataract etiopathogenesis. Various risk factors have been identified in development of cataracts. They can be classified in to genetic factors, ageing (systemic diseases, nutritional and trace metals deficiencies, smoking, oxidative stress etc.), traumatic, complicated (inflammatory and degenerative diseases of eye), metabolic (diabetes, galactosemia etc.), toxic substances including drugs abuses, alcohol etc., radiation (ultraviolet, electromagnetic waves etc.) are implicated as significant risk factors in the development of cataract.
Keywords: Blindness, cataract, eye lens, risk factors, treatment of cataract
Cataract is defined as opacity within the clear lens inside the eye that reduces the amount of incoming light and results in deterioration of vision. Natural lens is a crystalline substance and a precise structure of water and protein to create a clear passage for light. Cataract is often described as being similar to looking through a waterfall or waxed paper.[1]
Blindness causes human suffering is economically devastating, and many early deaths.[2] According to WHO, one-third of the world's 45 million blind and half of the world's 1.5 million blind children live in South-East Asia region. The blind persons are often leading a miserable life and are disenfranchised.[2] Three national surveys in India have extrapolated the survey result to project that number of people affected with cataract will reach to 8.25 million by 2020.[3] Currently available treatment is surgical extraction of the cataractous lens. Reports say that all cataract surgeries in India are not sight-restoring.[4] Blindness due to cataract is terrific challenge for ophthalmologists on public health stance. It imposes great economic burden on people and surfeit to be handled by surgery alone. Alternatively, the preventive ophthalmology offers another approach to tackle the problem to identify factors, which might modify or simply delay the onset and progression of cataract by a period of 10 years, the number of cataract surgeries would drastically decrease by 45% or more.[5] Therefore, identifying modifiable risk factors is of great importance from a public health perspective. The better understanding of causes can definitely have great impact in its management, as elimination of causes is the main key to eradicate any disease. The present study recapitulated after reviewing various literatures, research articles, reviews, and internet data associated with etiopathogenesis of cataract.
Risk factors of cataract
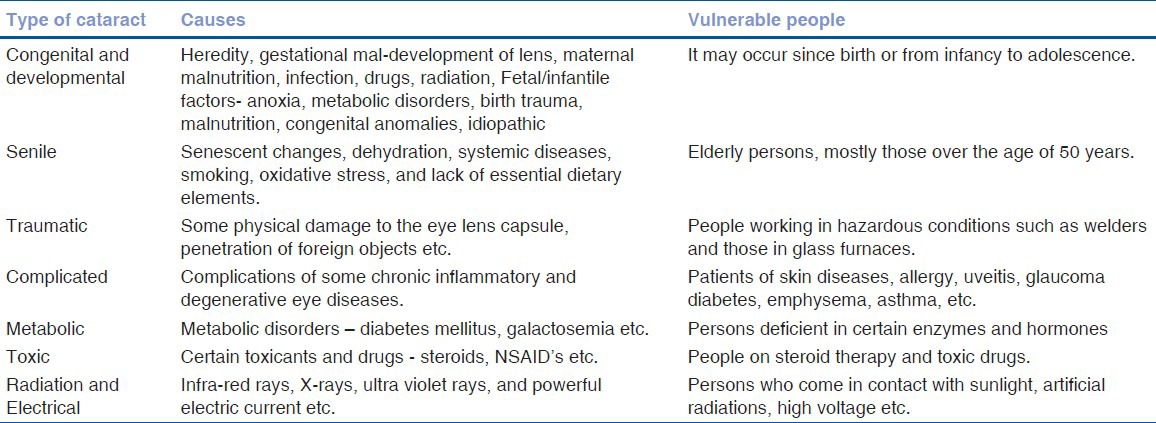
Cataract develops from a variety of reasons. Human cataract formation is mostly considered to be a multifactorial disease. Most of them develop with their specific etiologies and can be diagnosed through it, e.g., posterior (classically due to steroid use) and anterior (common senile cataract).[6] Table 1 represents the cataracts with their causes and vulnerable persons.
Table 1.
Various types of cataract, their causes, and persons at risks
Congenital
Following factors are generally involved in the development of the congenital cataracts.
Genetic factors
Genetically determined cataract is due to an anomaly in the chromosomal pattern of the individual. About one third of all congenital cataracts are hereditary.[7] It may occur with or without microphthalmia, aniridia, anterior chamber developmental anomalies, retinal degenerations, other multisystem genetic disorders such as chromosome abnormalities, Lowe syndrome or neurofibromatosis type.[8] PITX3 gene are reported to be responsible for some inherited cataracts in anterior segment mesenchymal dysgenesis.[9] Hereditary Mendelian cataract is inherited autosomal-dominant and autosomal-recessive or X-linked traits. Phenotypically, identical cataracts can result from mutations at different genetic loci and may have different inheritance patterns.[8]
Maternal and fetal factors
Malnutrition during pregnancy or in early infancy has been associated with non-familial zonular cataract. Maternal infections like rubella, toxoplasmosis, and cytomegalo-inclusion etc., are also associated with congenital cataracts.[10] Endocrine disturbance,[8] abuses of alcohol or drugs (thalidomide, corticosteroids etc.) as well as exposure of radiation during pregnancy increases the risk of cataracts in their infants.[10] Intrauterine hypoxia in the last trimester of pregnancy, Lowe's syndrome, myotonia dystrophica, congenital icthyosis etc., are infantile factors to cause cataract in infants.[8,10] The Osaka variant of galactokinase with an A198V substitution was shown to be associated with bilateral cataract in adults.[11]
Gender
Women have a higher incidence and risk for most types of cataracts than men,[7] probably due to lack of estrogen in post-menopausal years. An experimental study suggested the protective effects of estradiol or estrone treatment against cataractous eyes up to 25%, in the MNU-treated, ovariectomized rats.[12]
Race and ethnicity
African-Americans and Hispanic Americans seem to have nearly twice the risk of developing cataracts than Caucasians. This difference may be due to other medical illnesses, particularly diabetes, and due to lack of treatment.[7]
Ageing
Age-related (or senile) cataract is defined as cataract occurring in people >50 years of age, unrelated to known mechanical, chemical, or radiation trauma. It becomes progressively more severe and frequent in elderly[13] and is responsible for 48% of world blindness.[14] Breakdown and aggregation of protein, damage to fiber cell membranes, deficiency of glutathione, oxidative damage, elevated calcium, abnormal lens epithelial cell migration etc., are some specific mechanisms responsible for senile cataract. Some of the following factors may provoke the above mechanisms for cataract.
Diarrhea/dehydrational crisis
Minassian et al.[15] reported that one episode of severe diarrhea is 4.1 times more likely to cause cataract. The risk rose to 21% with two or more episodes of diarrhea and was still higher in those with history of both severe diarrhea and heatstroke. Harding[16] summarizes that the diarrhea, malnutrition, acidosis, dehydration, high level of urea in the body, and associated osmotic imbalance lead to accumulation of cyanate, thus adversely affect the glutathione level, which causes cataract.
Hypertension
Early clinical studies of cataract formation in diabetes mellitus noted a high prevalence of arterial hypertension.[17] Decreased lenticular ionic transport resulting from a specific decrease in Na+ K+ Adenosine Triphosphatase (ATPase) activity in the lens epithelium leads to cataract formation in the Nakano mouse.[18] Some in vitro studies with Na+ K+ ATPase inhibitors also results in lens opacification.[18] Low Na+ K+ ATPase activity has been reported in renal microsomal preparations from hypertensive Dahl salt-sensitive rats.[19,20]
Smoking
The role of smoking in cataractogenesis has been highlighted in various studies.[21,22,23] These studies have shown 2-3 fold increased risk of cataract in smokers. The increase in smoking dose was associated with increasing severity of nuclear opacities. Aromatic compounds present in the inhaled smoke oxidatively modify lenticular components.[24]
Oxidative stress - oxygen-free radicals (Oxidants)
It is widely accepted that oxidative stress is a significant factor in the genesis of cataract, both in experimental animals[25,26] and in cultured lens models.[27,28] The oxidative processes rise with age in the human lens, and concentration of proteins found significantly higher in cataractous lenses.[29] The overproduction of oxidants is very harmful that they can even affect genetic material.[30] One theory postulated that in the aging eye, barriers develop that prevent glutathione and other protective antioxidants from reaching the nucleus in the lens, thus making it vulnerable to oxidation.[7]
Lipid content and cholesterol
The composition and metabolism of membrane lipids may affect the formation of various types of cataracts.[31] Lens membrane contains the highest cholesterol content of any known membrane.[32] The development of cataract is associated with increased accumulation and re-distribution of cholesterol inside these cells. The Smith-Lemli-Opitz syndrome, mevalonic aciduria, and cerebrotendinous xanthomatosis all involve mutations in enzymes of cholesterol metabolism, and affected patients can develop cataracts. Hypocholesterolemic drugs like statins can block cholesterol accumulation by these lenses and can produce cataracts.[31,33]
Traumatic
A cataract can form after blunt or penetrating injuries to the eye and entry of a difficult-to-remove foreign object, leads to physical damage and discontinuation of the eye lens capsule. When the outer lens capsule breaks, the inner lens swells with water and turns white due to denaturation of lens proteins. Concussion of the lens without rupture of the capsule may result in a cataract that is initially sub-capsular and commonly has a star-shaped appearance.[34] These injuries typically occur in young men, and the lenses are very soft and easy to suck out. People working in hazardous conditions such as welders and those in glass furnaces are more susceptible to this kind of injury-induced cataract.
Complicated
This term refers to cataracts that are secondary to local eye as well as systematic inflammatory and degenerative diseases.
Skin diseases and allergy
Lens opacities associated with cutaneous diseases are termed syndromatotic cataracts, occur at young age and are bilateral.[10] Atopic cataract is most common condition associated with atopic dermatitis (AD), especially in children.[35] The mechanism is not known; however, habitual tapping and rubbing of the face in pruritic conditions may play a role.[36] Patients with AD have been found to have higher levels of protein flare in the aqueous humor.[37] Other skin disorders associated with cataract include poikiloderma, vascular atrophicus, scleroderma, and keratotis follicularis.[10]
Eye conditions
Glaucoma and its treatments, including certain drugs (notably miotics viz; demecarium, isoflurophate, and echothiophate) and filtering surgery, posing a high risk for cataracts.[7] Inflammatory conditions of eye viz. uveitis caused by an autoimmune disease or response, including Fuch's heterochromic cyclitis and Still's disease, hypoyon corneal ulcer, endophthalmitis, myopic chorioretinal degeneration, retinitis pigmentosa and other pigmentary retinal dystrophies, retinoblastoma or melanoma (complicated last stages) are the other factors.[10] The myopic change also precedes the development of cataract.[38] Nuclear cataract is associated with presumed acquired myopia.[39,40] Posterior sub-capsular cataract reported as significantly associated with myopic refraction.[41,42]
Metabolic
These cataracts occur due to endocrine disorders and biochemical abnormalities. Galactosemic and diabetic cataracts are common example of this kind of cataract.
Galactosemia
Galactosemia is associated with inborn error of galactose metabolism, which can occur due to deficiency of galactose-1 phosphate uridyl-transferase (GPUT) and due to deficiency of galactokinase (GK). Development of bilateral cataract in the form of oil droplet central lens opacities is characteristic feature of galactosemia.[10]
Diabetes
Poor control of diabetes mellitus (DM) is linked to the formation of several systemic and ocular complications included vision loss.[43,44] Evidently, direct in vivo and in vitro experimental studies suggest that diabetes is a cause of cataract. Uncontrolled DM results in hyperglycemia, which is associated in ocular tissues with non-enzymatic protein glycation,[45] osmotic stress,[46] and oxidative stress.[47]
Insulin therapy, strict control of blood glucose levels, exercise, anorexia as well as ischemia-induced hypoglycemia leads to unfolded protein response (UPR),[48,49] lens epithelial cell (LEC) death[50] through activation of specific death pathways, and apoptosis.[51]
Hypocalcemia
Cataractous changes may be associated with parathyroid tetany, which may occur due to atrophy or inadvertent removal (during thyroidectomy) of parathyroid glands. Multicolored crystals or small discreet white flacks of punctate opacities are formed in the sub-capsular region of lens, which seldom matures.[37]
Hypothyroidism
Cataract is not a common feature of hypothyroidism or cretinism; however, an association has been claimed,[52] and the described opacities resemble those seen in hypoparathyroidism. Thyroidectomy without interference with the parathyroids has also been stated to cause cataract, usually a blue dot type.
Error of copper metabolism
Inborn error of copper metabolism results in Wilson's disease (hepatolenticular degeneration) may develop a characteristic opacity in the anterior capsular region brightly-colored sunflower pattern, green-colored, and has negligible effect on vision. The more commonly observed feature is ‘Kayser-Fleischer ring’ in the cornea.[10,53]
Nutritional
Animal studies and in vitro investigations have shown that nutritional deficiencies of micronutrients are associated with cataract.
Aldose reductase (for reduction of sugars) is the basis for the formation of cataracts related to abnormalities in sugar metabolism.[54,55] Studies suggested that poor nutritional status of cataract patients accelerates protein insolubilization in the lens of most types of human and experimentally induced animal cataracts.[56] Tryptophan deficiency-induced cataract has consistently been documented.[57] Cataracts have also been produced in experimental animals on a diet low in folic acid.[58] Study published recently shows that regular intake of multivitamin supplement decreases the risk for all types of cataracts.[59,60,61]
There are many evidences suggesting that the trace elements, especially zinc and copper in nutrition, may play a role in the formation of human cataract. Animal and human studies have reported the involvement of various inorganic minerals linked to cataract formation.[60,62] These elements have recently attracted much attention as possible causative factors in development of cataract.[63,64,65]
Neonatal hypoglycemia, aminoaciduria, homocystinuria, Fabry's disease, Hurler's disease, Lowe's syndrome are other metabolic conditions, which lead to cataract development.
Toxic cataracts
Drug abuses
Many drugs can contribute to cataracts, including corticosteroids (such as prednisolone and cortisone),[66] tranquilizers, radiomimetic drugs,[67] quinoline, methotrexate, oral contraceptives, miotics, ergot, sulfanilamide, streptozotocin, methoxsalen, accutane, epinephrine psoralen, thiazide etc.[68]
Steroid use is the fourth leading risk factor for secondary cataract and accounts for 4.7% of all cataract extractions.[69] In addition to systemic steroids, cataracts have also been associated with ocular topical steroids, inhaled steroids, and topical steroid creams.[70,71] Steroids, such as prednisone, block normal metabolism of connective tissue, of which the lens is composed. Even low potency steroid creams applied to the eyelids may result in increased intra-ocular pressure and cataract.[72] The mechanism of corticosteroid-induced cataract is not known but may be due to osmotic imbalance, oxidative damage, or disrupted lens growth factors.[70]
Thiazolidinediones is major new therapy for non-insulin-dependent diabetes.[73,74] On oral administration, it was associated with the formation of lenticular opacities during non-clinical safety assessment studies conducted in rats.[75]
An asymptomatic anterior sub-capsular lens opacities and keratopathy characterized by sub-epithelial corneal whorls similar to those noted in Fabry's disease are well documented as ophthalmic side-effects of Amiodorone (anti-arrhythmic drug).[76]
Neuroleptic drugs are used in the treatment of various psychiatric disorders.[77] Chlorpromazine (CPZ) therapy is associated with anterior capsular lens pigmentation, followed by corneal endothelial pigmentary changes.[78,79] During carbamazepine therapy, blurred vision, transient diplopia, and conjunctivitis, in addition to lens opacities, have been reported.[80,81] Such visual disturbances are reversible and respond to decrease in dose.
The eye's lens consists of serotonin receptors and has shown that excess serotonin lead to cataract formation in animal studies.[82]
Long-term use of miotics, particularly long acting cholinesterase inhibitors such as echothiophate, demecarium bromide, disopropyl fluorophosphate (DFP) etc., may induce reversible anterior sub-capsular granular type of cataract.[10]
Many others drugs are weakly associated with cataracts including busulfan, gold, allopurinol, potassium-sparing diuretics, thyroid hormone, tetracyclines, sulfamidase, tomoxifen, naphthalene, simvastatin etc. A significant interaction between simultaneous statin and erythromycin use is reported with the development of cataract.[32,83,84,85]
Toxins
Many toxins, including synthetic chemicals and pharmaceuticals, are known to trigger cataract. They include: acetone, dinitrophenol, cresol, and paradichlorobenzol as well as numerous chemicals and solvents. Heavy metals like mercury are found at increasing levels in the lens with aging and cataractogenesis. Cadmium, bromine, cobalt, iridium, and nickel are one of the important co-factors of lipid peroxidation process and potentially deactivating antioxidant functions.[86,87,88] Additional minerals thallium, zinc sulfate, cobalt chloride, sodium selenite etc., in certain forms and dosages can become toxic and cause cataract.[89,90]
Hormonal replacement therapy
Cataract is more prevalent in post-menopausal women than in men at similar ages; this implies that hormonal differences are involved and suggests a possible role for estrogen. Estrogen receptors have been detected in the cataractous eye's lens. Naturally occurring (endogenous) estrogen appears to protect the eye from cataract, along with cardiovascular and other body systems before menopause. A prospective study on post-menopausal Swedish women found that HRT may also raise risk.[91]
Alcohol consumption
Alcohol increases the risk of nuclear, cortical, and posterior sub-capsular cataracts (PSC). The lens is sensitive to oxidative stress and directs toxic effects of alcohol.[92,93] The lowest level that showed an effect in the studies was 91 g pure ethanol per week, (seven-nine) standard drinks were 4.6 times more likely to suffer from PSC when compared with non-drinkers.[94]
Radiation and electromagnetic waves
The radiation may be of any kind viz; ultra-violet rays, infrared, or electromagnetic waves. Ultra-violet-radiation has been linked with senile cataract in many studies. Duke-Elder had opined that the fundamental cause of cataract in all its forms may be traced to the incidence of radiant energy directly on the lens itself.[10,95] Data from the HANES survey have shown higher ratio of cataract to non-cataractous diseases in areas with high numbers of annual sunlight hours.[96] In Australia, areas of higher UV irradiation were shown with higher prevalence and early onset of cataract.[97] Cataract prevalence reported 3.8 times higher in areas with an average of 12 hours of daily sunlight exposure compared to areas with only 7 hours of exposure in Nepal.[98] Interestingly, cataract was reported more common in cloudier areas of India.[99] Both epidemiological and experimental evidence indicates maximum lens sensitivity to UVR-B with wavelengths around 300 nm.[100,101,102] Until today, little is known how the genome modulates the lens sensitivity to oxidative stress from UVR. Electromagnetic radiation with longer wavelengths, e.g., UVR-A also contributes to adverse biological effects, but as in DNA damage, the contribution is small, even though UVR-A in sunlight is nearly a thousand-fold more intense than UVR-B.[103,104] Several epidemiological studies have consistently demonstrated the correlation between cortical cataract and exposure to solar UVR.[105,106,107] Widmark (1901) described[108] lens epithelial damage, swollen lens fibers, but no damage on the lens equator in rabbit lenses following controlled exposure to UVR. Small fraction of high energetic UVR-B 300 nm passing cornea is absorbed by lens epithelium, which is, therefore, the primary target for damage.[109,110]
Prolonged exposure to infrared rays may cause discoid posterior sub-capsular opacities and true exfoliation of the anterior capsule (Exfoliation syndrome) as typically seen in workers of glass industries. Exposure to microwave radiation can cause cataracts.[10] Exposure to X-rays, gamma rays or neutrons may be associated with irradiation cataract. There is usually a latent period ranging from 6 months to a few years to the development of cataract. Inadequately protected technicians, patients treated for malignant tumors, and workers of atomic energy plants are prone to this.[10]
Discussion
Clinically, cataract patients can be classified into morphological groups viz. nuclear, sub-capsular or cortical for studying the risk factors. Most case-control studies have been on pooled cataracts. This approach has been strongly criticized by some authors on the basis that different morphological types have different risk factors.[16] Since cataract is a major cause of avoidable blindness in the developing countries, the key to the success of the Global Vision 2020: The right to sight initiative is a special effort to tackle cataract blindness by finding out precise cause. Even though effective surgical procedures are available for treatment, the problem of post-operative complications, cost of surgery, and high number of people requiring surgery pose a substantial economic burden. It has been estimated that delaying cataract onset by 10 years could reduce the need for surgery by as much as half.[111] The respective causes of different type of cataracts must be known in order to understand the patho-physiology of disease and its management. However, risk factors for cataracts summarized above cannot be comprehended this way, but they may help to confer the matter with new approaches.
Inherited disorders are often involved in the development of congenital cataracts in children with ratio of 1:10,000 births.[7] Such cataracts are most often due to inborn abnormalities in the structure or shape of the lens capsule. PITX3 gene has been reported as responsible for some inherited cataracts. The role of Osaka variant is new interest of point at present. Infantile cataracts, those developing within the first year of life, are frequently associated with a metabolic or systemic disease.[112] The role of gender and race or community could not be made clear in the development of cataract. Age-related cataracts are mostly developed due to increase in oxidative stress in lens due to various systemic diseases or imbalance in pro and anti-oxidants in body particularly eyes. Trauma has direct impact to induce denaturation processes in eye lenses. Removal and implant placement can be complicated in these cases though, as the blunt force often tears the zonular support.[113] Complications of untreated systemic as well as local conditions are well-elaborated in development of cataract, though their mechanism is still unclear. Cataracts, those precede by metabolic abnormalities, are mostly associated with congenital aberrations. Most of them are having peculiar diagnostic characters like oil droplet type of opacity appearance in galactosemia,[10] multicolored crystals-like opacities can be seen in hypocalcemia,[10] and sunflower-like appearance in copper metabolic error.[53] The deficiencies of micronutrients directly affect the antioxidant systems in eyes lens.[114,115] The role of nutrition in cataract formation in developing countries is perhaps closely linked with diarrhea and poverty, all of which are closely interrelated.[116] Many drug abuses as well as various toxins may cause oxidative damage and interrupt the lens growth. They bind to sulfhydryl groups, including glutathione peroxidase and Na+ K+ ATPase, along with super oxide dismutase and catalase, which are responsible for the maintenance of clarity of the lens during oxidative stress.[69] Most of them are reversible in nature. Radiation stimulates the senile changes in eye lenses. Radiation or electromagnetic waves can rouse the exfoliation process in lens that leads to disturbance in protein arrangement and oxidative systems. Experimental evidence indicates maximum lens sensitivity to UVR-B in the wavelength region around 300 nm.[101,102] ROS are mediators of damage induced by UVR[117] and can trigger alteration in growth factors- and cytokine-mediated signal transduction pathways, leading to aberrant gene expression.[118]
Elimination of causes of cataract which were described above may reverse the cataractous changes in the initial stage. Nutritional supplements and balancing antioxidants during old age and malnutrition and in condition of diarrhea are reported in preventing senile cataract.[119] Correction of transient metabolic defects e.g., treatment of galactosemia, copper metabolism etc., are also found useful in the prevention of cataract. Eluding factors affecting congenital defects like consanguineous marriage, galactosemic diet, medication and radiation during pregnancy can be helpful in preventing development of congenital cataract.[120,121,122] Prescription of alternate medications for steroid and other drugs prone to cataract formation can be used to prevent cataractous changes.[123] Many studies reported that antioxidants (Vit E, Vit C, thiamine, riboflavin, lutein, flavonoids, carotenoids etc.)[28,124,125] can effectively prevent and cure UVB-induced protein oxidation and photo-peroxidation of lipids in lens. Local protective measures like use of UV-protected sun glasses as well as use of UV-absorbing hydrogel polymers also can be useful in this way.[126] Though many of the factors identified are responsible for the development of cataract, but their mechanism of action is still unclear. There is much space to work in this direction.
Conclusion
Present review summarizes the various etiopathogenesis of cataract. Senile cataract due to aging is more common than other types of cataract. Apart from aging, various risk factors of cataract like: Nutritional inadequacy, metabolic and inherited defects, ultraviolet radiation, and smoking have been implicated as significant risk factors in development of cataract. Most of the risk factors are mingled with other factors and leads to unavoidable progression of the disease. It is today's need to categorize the causative factors according to the nature of cataract appropriately and incorporate with the diagnosis, which may be helpful in the treatment of cataract.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Robert S, Randall LK, editors. Cataracts-Overview (Internet) Life Extension. [Last accessed on 08.09.10]. Available from: http://www.garynullforum.com/articles/pdf/foundarticles1/lef/CATARACTS.pdf .
- 2.World Health Organization. Strategic Plan for Vision 2020: The Right to Sight. Elimination of Avoidable Blindness in the South-East Asia Region, SEA-Ophthal-117, World Health Organization Regional Office for South-East Asia New Delhi. 2000. [Last accessed on 27.3.11]. p. 6. Available from: http://www.searo.who.int/LinkFiles/Publications_SEA-Ophthal-117.pdf .
- 3.Murthy G, Gupta SK, John N, Vashist P. Current status of cataract blindness and Vision 2020: The right to sight initiative in India. Indian J Ophthalmol. 2008;56:489–94. doi: 10.4103/0301-4738.42774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Limburg H, Foster A, Vaidyanathan K, Murthy GV. Monitoring visual outcome of cataract surgery in India. Bull WHO. 1999;77:455–60. [PMC free article] [PubMed] [Google Scholar]
- 5.Kupfer C. The conquest of cataract: A global challenge. Trans Ophthalmol Soc UK. 1985;104:01–10. [PubMed] [Google Scholar]
- 6.Greiner J, Chylack L. Posterior subcapsular cataracts: Histopathologic study of steroid-associated cataracts. Arch Ophthalmol. 1979;97:135–44. doi: 10.1001/archopht.1979.01020010069017. [DOI] [PubMed] [Google Scholar]
- 7.Harvey Simon, David Zieve., editors. New York: Time Health Guide; [Last updated and reviewed on 2010 June 23, Last accessed on 16.4.11]. Cataract-Risk factors (Internet) Available from: http://health.nytimes.com/health/guides/disease/cataract/risk-factors.html . [Google Scholar]
- 8.Hejtmancik JF, Kaiser-Kupfer MI, Piatigorsky J. Molecular biology and inherited disorders of the eye lens. In: Scriver CR, Beaudet AL, Valle D, editors. The Metabolic and Molecular Basis of Inherited Disease. 8th ed. New York: McGraw Hill; 2001. pp. 6033–62. [Google Scholar]
- 9.Semina EV, Ferrell RE, Mintz-Hittner HA. A novel homeobox gene PITX3 is mutated in families with autosomal-dominant cataracts and ASMD. Nat Genet. 1998;19:167–70. doi: 10.1038/527. [DOI] [PubMed] [Google Scholar]
- 10.Khurana AK. 4th ed. New Delhi: New Age International (P) Ltd; 2007. Diseases of the lens, Comprehensive Ophthalmology; pp. 167–204. [Google Scholar]
- 11.Okano Y, Asada M, Fujimoto A, Ohtake A, Murayama K, Hsiao KJ, et al. A genetic factor for age-related cataract: Identification and characterization of a novel galactokinase variant, “Osaka,” in Asians. Am J Hum Genet. 2001;68:1036–42. doi: 10.1086/319512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robert MB, Horacio C, Andrea CG, Clinton JG. Protective effect of estrogen in age related cataracts. Proc Natl Acad Sci. 1999;96:9328–32. doi: 10.1073/pnas.96.16.9328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klaus GB, James EF, Wolfgang L. The role of ascorbic acid in senile cataract. Proc Natl Acad Sci USA. 1985;82:7193–96. doi: 10.1073/pnas.82.21.7193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Causes of blindness and visual impairment. Prevention of blindness and visual impairment. [Last accessed on 27.3.11]. Available from: http://www.who.int/blindness/causes/priority/cataract-magnitude/en/index.html .
- 15.Minassian DC, Mehra V, Jones BR. Dehydrational crisis from severe diarrhoea or heatstroke and risk of cataract. Lancet. 1984;1:751–53. doi: 10.1016/s0140-6736(84)91274-1. [DOI] [PubMed] [Google Scholar]
- 16.Harding J. London: Chapman - Hall; 1991. Cataract: Biochemistry, Epidemiology and Pharmacology; pp. 83–124. [Google Scholar]
- 17.Kirby DB. Cataract and diabetes. Arch Ophthalmol. 1932;8:966–73. [Google Scholar]
- 18.Miller D, Tijerine ML, Mayman C. In vitro production of steroid cataract in bovine lens: Part I. Measurement of optical changes. Acta Ophthalmol. 1979;7:1101–6. doi: 10.1111/j.1755-3768.1979.tb00544.x. [DOI] [PubMed] [Google Scholar]
- 19.Rodriguez SC, Cangiano JL, Opava-Stitzer S, Martfnez MM. Renal Na+K+ ATPase in Okamoto and Dahl hypertensive rats. Hypertension. 1981;3(Suppl 2):S86–91. doi: 10.1161/01.hyp.3.6_pt_2.ii-86. [DOI] [PubMed] [Google Scholar]
- 20.McPartland RP, Rapp JP. Na+, K+ Activated adenosine triphosphate and hypertension in Dahl salt-sensitive and resistant rats. Clin Exp Hypertens. 1982;A4:379–91. doi: 10.3109/10641968209060750. [DOI] [PubMed] [Google Scholar]
- 21.West S, Munoz B, Emmett EA. Cigarette smoking and risk of nuclear cataract. Arch Ophthalmol. 1989;107:1166–69. doi: 10.1001/archopht.1989.01070020232031. [DOI] [PubMed] [Google Scholar]
- 22.Christen WG, Manson JE, Seddon JM. A prospective study of cigarette smoking and risk of cataract in men. JAMA. 1992;268:989–93. [PubMed] [Google Scholar]
- 23.Hankinson SE, Willett WC, Colditz GA. A prospective study of cigarette smoking and risk of cataract in women. JAMA. 1992;268:994–98. [PubMed] [Google Scholar]
- 24.West S, Munoz B, Vitale S. Waterman study II Smoking and nuclear opacities. Invest Ophthalmol Vis Sci. 1992;33:2023. [Google Scholar]
- 25.Truscott RJ. Age-related nuclear cataract-oxidation is the key. Exp Eye Res. 2005;80:709–25. doi: 10.1016/j.exer.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 26.Varma SD, Devamanoharan PS, Morris SM. Prevention of cataracts by nutritional and metabolic antioxidants. Crit Rev Food Sci Nutr. 1995;35:111–29. doi: 10.1080/10408399509527691. [DOI] [PubMed] [Google Scholar]
- 27.Spector A, Wang GM, Wang RR. A brief photochemically induced oxidative insult causes irreversible lens damage and cataract. II. Mechanism of action. Exp Eye Res. 1995;60:483–93. doi: 10.1016/s0014-4835(05)80063-6. [DOI] [PubMed] [Google Scholar]
- 28.Gupta SK, Trivedi D, Srivastava S. Lycopene attenuates oxidative stress induced experimental cataract development: An in vitro and in vivo study. Nutrition. 2003;19:794–9. doi: 10.1016/s0899-9007(03)00140-0. [DOI] [PubMed] [Google Scholar]
- 29.Boscia F, Grattagliano I, Vendemiale G. Protein oxidation and lens opacity in humans. Invest Ophthalmol Vis Sci. 2000;41:2461–5. [PubMed] [Google Scholar]
- 30.Lou MF. Redox regulation in the lens. Prog Retin Eye Res. 2003;22:657–82. doi: 10.1016/s1350-9462(03)00050-8. [DOI] [PubMed] [Google Scholar]
- 31.Zelenka PS. Lens lipids. Curr Eye Res. 1984;3:1337–59. doi: 10.3109/02713688409007421. [DOI] [PubMed] [Google Scholar]
- 32.Cenedella RJ. Cholesterol and cataracts. Surv Ophthalmol. 1996;40:320–37. doi: 10.1016/s0039-6257(96)82007-8. [DOI] [PubMed] [Google Scholar]
- 33.David S. Antibiotic use with cholesterol lowering drugs may increase risk of cataracts. [Last accessed on 15.09.11];Br Med J. 2002 325:1194–4. Available from http://www.bmj.com/content/325/7374/1194.4.long . [Google Scholar]
- 34.Davidson M. Lens lesion in contusion: A medico-legal case study. Am J Ophthalmol. 1940;23:252. [Google Scholar]
- 35.Chen CC, Huang JL, Yang KD, Chen HJ. Atopic cataracts in a child with atopic dermatitis: A case report and review of the literature. Asian Pac J Allergy Immunol. 2000;18:69–71. [PubMed] [Google Scholar]
- 36.Nagaki Y, Hayasaka S, Kadoi C. cataract progression in patients with atopic dermatitis. J Cataract Refract Surg. 1999;25:96–99. doi: 10.1016/s0886-3350(99)80018-2. [DOI] [PubMed] [Google Scholar]
- 37.Matsuo T, Saito H, Matsuo N. cataract and aqueous flare levels in patients with atopic dermatitis. Am J Ophthalmol. 1997;124:36–39. doi: 10.1016/s0002-9394(14)71641-1. [DOI] [PubMed] [Google Scholar]
- 38.Brown NA, Hill AR. Cataract: The relation between myopia and cataract morphology. Br J Ophthalmol. 1987;71:405–14. doi: 10.1136/bjo.71.6.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Panchapakesan J, Rochtchina E, Mitchell P. Myopic refractive shift caused by incident cataract: The Blue Mountains Eye Study. Ophthalmic Epidemiol. 2003;10:241–47. doi: 10.1076/opep.10.4.241.15911. [DOI] [PubMed] [Google Scholar]
- 40.Lim R, Mitchell P, Cumming RG. Refractive associations with cataract: The Blue Mountains Eye Study. Invest Ophthalmol Vis Sci. 1999;40:3021–26. [PubMed] [Google Scholar]
- 41.Chang MA, Congdon NG, Bykhovskaya I, Munoz B, West SK. The association between myopia and various subtypes of lens opacity: Salisbury Eye Evaluation project. Ophthalmology. 2005;112:1395–401. doi: 10.1016/j.ophtha.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 42.Wong TY, Foster PJ, Johnson GJ, Seah SK. Refractive errors, axial ocular dimensions, and age-related cataracts: The Tanjong Pagar Survey. Invest Ophthalmol Vis Sci. 2003;44:1479–85. doi: 10.1167/iovs.02-0526. [DOI] [PubMed] [Google Scholar]
- 43.Brian G, Taylor H. cataract blindness: Challenges for the 21 st century. Bull World Health Organ. 2001;79:249–56. [PMC free article] [PubMed] [Google Scholar]
- 44.Delcourt C, Carriere I, Ponton-Sanchez A, Lacroux A, Covacho MJ, Papoz L. Light exposure and the risk of cortical, nuclear and posterior subcapsular cataracts: The Pathologies Oculaires Liees a l’Age (POLA) study. Arch Ophthalmol. 2000;118:385–92. doi: 10.1001/archopht.118.3.385. [DOI] [PubMed] [Google Scholar]
- 45.Derham BK, Harding JJ. Alpha-crystallin as a molecular chaperone. Prog Retin Eye Res. 1999;18:463–509. doi: 10.1016/s1350-9462(98)00030-5. [DOI] [PubMed] [Google Scholar]
- 46.Kador PF, Robison WG, Jr, Kinoshita JH. The pharmacology of aldose reductase inhibitors. Annu Rev Pharmacol Toxicol. 1985;25:691–714. doi: 10.1146/annurev.pa.25.040185.003355. [DOI] [PubMed] [Google Scholar]
- 47.Kowluru RA, Kennedy A. Therapeutic potential of anti-oxidants and diabetic retinopathy. Exp Opin Investig Drugs. 2001;10:1665–76. doi: 10.1517/13543784.10.9.1665. [DOI] [PubMed] [Google Scholar]
- 48.Heller SR. Diabetic hypoglycaemia. Baillieres Best Pract Res Clin Endocrinol Metab. 1999;13:279–94. doi: 10.1053/beem.1999.0020. [DOI] [PubMed] [Google Scholar]
- 49.Vignesh JP, Mohan V. Hypoglycaemia unawareness. J Assoc Physicians India. 2004;52:727–32. [PubMed] [Google Scholar]
- 50.Ikesugi K, Yamamoto R, Mulhern ML, Shinohara T. Role of the unfolded protein response (UPR) in cataract formation. Exp Eye Res. 2006;83:508–16. doi: 10.1016/j.exer.2006.01.033. [DOI] [PubMed] [Google Scholar]
- 51.Benavides A, Pastor D, Santos P, Tranque P, Calvo S. CHOP plays a pivotal role in the astrocyte death induced by oxygen and glucose deprivation. Glia. 2005;52:261–75. doi: 10.1002/glia.20242. [DOI] [PubMed] [Google Scholar]
- 52.Mahto RS. Ocular features of hypothyroidism. Br J Ophthalmol. 1977;56:546. doi: 10.1136/bjo.56.7.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Duke-Elder S. London: Kimpton; 1954. Textbook of Ophthalmology; p. 1693. [Google Scholar]
- 54.Bhat KS, Rao PV. International Symposium on Biological oxidation systems. Bangalore, India: 1989. Lens oxidant scavenger system in rats with galactose induced cataract; p. 48. [Google Scholar]
- 55.Kador PF, Kinoshita JH. Diabetic and galactosemic cataracts. In: Nugent J, Whelan J, editors. Human cataract Formation. Ciba Foundation Symposium 106. London: Pitman; 1984. pp. 110–31. [DOI] [PubMed] [Google Scholar]
- 56.Mandal K, Kono M, Bose SK. Structure and stability of gammacrystallins-IV. Aggregation and structural destabilization in photosensitized reactions. Photochem Photobiol. 1988;47:583–91. doi: 10.1111/j.1751-1097.1988.tb08848.x. [DOI] [PubMed] [Google Scholar]
- 57.Bunce GE. Nutrition and cataract. In: Tobin BB, Mehlman MA, editors. Advances in Modern Human Nutrition. Illinois: Pathotox Publishers Inc; 1980. pp. 01–31. [Google Scholar]
- 58.Borkman RF. Catarcts and Photochemical damage in the lens. In: Nugent J, Whelan J, editors. Human cataract formation. Ciba Foundation Symposium 106. London: Pitman; 1984. pp. 88–109. [DOI] [PubMed] [Google Scholar]
- 59.Leske MC, Chylack LT, Wu SY The lens opacities case-control study group. The lens opacities case control study: Risk factors for cataract. Arch Ophthalmol. 1991;109:244–51. doi: 10.1001/archopht.1991.01080020090051. [DOI] [PubMed] [Google Scholar]
- 60.Bunce GE, Kinoshita JH, Horwitz J. Nutritional factors in cataract. Annu Rev Nutr. 1990;10:233–54. doi: 10.1146/annurev.nu.10.070190.001313. [DOI] [PubMed] [Google Scholar]
- 61.Balasubramanian D, Bhat KS, Rao GN. Factors in the prevalence of cataract in India: Analysis of the recent Indian-US study of age-related cataracts. Curr Sci. 1990;59:498–505. [Google Scholar]
- 62.Leske MC, Suh-Yuh W, Hyman L, Sperduto R, Underwood B, Chylack LT, et al. The lens opacities case-controls study group. Biochemical factors in the lens opacities case-control study. Arch Ophthalmol. 1995;113:1113–19. doi: 10.1001/archopht.1995.01100090039020. [DOI] [PubMed] [Google Scholar]
- 63.Akyol N, Deger O, Keha EE, Kilic S. Aqueous humour and serum zinc and copper concentrations of patients with glaucoma and cataract. Br J Ophthalmol. 1990;74:661–62. doi: 10.1136/bjo.74.11.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rasi V, Costantini S, Moramarco A, Giordano R, Giustolisi R, Balacco Gabrieli C. Inorganic element concentrations in cataractous human lenses. Ann Ophthalmol. 1992;24:459–64. [PubMed] [Google Scholar]
- 65.Srivastava VK, Varshney N, Pandey DC. Role of trace elements in senile cataract. Acta Ohthalmologica. 1992;70:839–41. doi: 10.1111/j.1755-3768.1992.tb04898.x. [DOI] [PubMed] [Google Scholar]
- 66.Spencer R, Andelman S. Steroids are bad cataracts. Posterior subcapsular cataract formation in rheumatoid arthritis patients on long term steroid therapy. Arch Ophthalmol. 1965;74:38–41. doi: 10.1001/archopht.1965.00970040040009. [DOI] [PubMed] [Google Scholar]
- 67.Lerman S. Balasubramanian D, Bansal AK, Basti S, Bhatt KS, Murthy JS, Rao CM, editors. Potential ocular complications of psoralen UV-A therapy. The biology of cataract. The Hyderabad cataract research group. Indian J Ophthalmol. 1993;41:153–71. [PubMed] [Google Scholar]
- 68.Andrew T. Atopic dermatitis, cutaneous steroids and cataracts in children: Two case reports. J Med Case Rep. 2008;2:124. doi: 10.1186/1752-1947-2-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jobling AI, Augusteyn RC. What causes steroid cataracts? A review of steroid-induced posterior subcapsular cataracts. Clin Exp Optom. 2002;85:61–75. doi: 10.1111/j.1444-0938.2002.tb03011.x. [DOI] [PubMed] [Google Scholar]
- 70.McLean CJ, Lobo RF, Brazier DJ. Cataracts, glaucoma and femoral avascular necrosis caused by topical corticosteroid ointment. Lancet. 1995;345:330. doi: 10.1016/s0140-6736(95)90324-0. [DOI] [PubMed] [Google Scholar]
- 71.Cumming RG, Mitchell P, Leeder SR. Use of inhaled corticosteroids and the risk of cataracts. N Engl J Med. 1997;337:08–14. doi: 10.1056/NEJM199707033370102. [DOI] [PubMed] [Google Scholar]
- 72.Garrott HM, Walland MJ. Glaucoma from topical corticosteroids to the eyelids. Clin Exp Ophthalmol. 2004;32:224–26. doi: 10.1111/j.1442-9071.2004.00787.x. [DOI] [PubMed] [Google Scholar]
- 73.Aoun P, Simpkins JW, Agarwal N. Role of PPAR-gamma ligands in neuroprotection against glutamate-induced cytotoxicity in retinal ganglion cells. Invest Ophthalmol Vis Sci. 2003;44:2999–3004. doi: 10.1167/iovs.02-1060. [DOI] [PubMed] [Google Scholar]
- 74.Murata T, He S, Hangai M, Ishibashi T, Xi XP, Kim S, et al. Peroxisome proliferator-activated receptor-gamma ligands inhibit choroidal neovascularization. Invest Ophthalmol Vis Sci. 2000;41:2309–17. [PubMed] [Google Scholar]
- 75.Michael DA, Colleen MD, Kimberly AN. Ciglitazone-induced lenticular opacities in rats: In vivo and whole lens explant culture evaluation. J Pharmacol Exp Ther. 2005;312:1027–33. doi: 10.1124/jpet.104.076950. [DOI] [PubMed] [Google Scholar]
- 76.Steven P, Steven K, Robert H, Judy H. Amiodarone Corneal Topography. Digital J Ophthalmol. 1997;3:03. [Google Scholar]
- 77.Alexender LJ, Bowerman L, Thompson LR. The prevalance of the ocular side effects of chlorpromazine in the Tuscaloosa Veterens Administration patient population. J Am Optom Assoc. 1985;56:872–76. [PubMed] [Google Scholar]
- 78.Greiner AC, Berry K. Skin pigmentation and corneal and lens opacities with prolonged chlorpromazine therapy. Can Med Assoc J. 1964;90:663–65. [PMC free article] [PubMed] [Google Scholar]
- 79.Subhashini K, Rao VA. Chlorpromazine induced cataract and corneal pigmentation: Case report. Indian J Pharmacol. 2004;30:323–24. [Google Scholar]
- 80.Fukuo Y, Abe T, Hayasaka S. Acute comitant esotropia in a boy with head trauma and convulsions receiving carbamazepine. Ophthalmologica. 1998;212:61–62. doi: 10.1159/000027262. [DOI] [PubMed] [Google Scholar]
- 81.Fraunfelder FT, Meyer SM. 2th ed. Philadelphia: Lea and Febiger; 1982. Drug induced ocular side effects and drug interactions. [Google Scholar]
- 82.Etminan M, Mikelberg FS, Brophy JM. Selective Serotonin reuptake inhibitors and the risk of cataracts: A nested case-control study. Ophthalmology. 2010;117:1251–55. doi: 10.1016/j.ophtha.2009.11.042. [DOI] [PubMed] [Google Scholar]
- 83.Xu GT, Zigler JS, Lou MF. The possible mechanism of naphthalene cataract in rat and its prevention by an aldose reductase inhibitor. Exp Eye Res. 1992;54:63–72. doi: 10.1016/0014-4835(92)90070-9. [DOI] [PubMed] [Google Scholar]
- 84.Zhang JJ, Jacob TJ, Valverde MA, Hardy SP, Mintenig GM, Sepulveda FV, et al. Tamoxifen blocks chloride channels: A possible mechanism for cataract formation. J Clin Investig. 1994;94:1690–97. doi: 10.1172/JCI117514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mayo GL. Chandler DA, editor. Richmond Eye Associates, PC [Internet]. Ophthalmic Side Effects of Drugs. Ophthalmology Update. 2003. [Last accessed on 11.4.11]. pp. 01–04. Available from: http://www.richmondeye.com/newsletter/Ophthalmology_Update_15_sep03.pdf .
- 86.Kinter WD, Pritchard D. Altered permeability of cell membrane. In: Lee SD, Falh HL, Murphy SD, Gieger SR, editors. Handbook of Physiology Sect-9. Reactions to environmental agent. American Physiological Society; 1977. p. 563. [Google Scholar]
- 87.Stacey NH, Contilena LR, Jr, Klassen D. Cadmium toxicity and lipid peroxidation in isolated rat hepatocytes. Toxicol Appl Pharmacol. 1980;53:470. doi: 10.1016/0041-008x(80)90359-2. [DOI] [PubMed] [Google Scholar]
- 88.Dwivedi RS, Kaur G, Srivastava RC, Krishnamurti CR. Lipid peroxidation in tin intoxicated partially hepatectomized rats. Bull Environ Contamn Toxicol. 1984;33:200–09. doi: 10.1007/BF01625531. [DOI] [PubMed] [Google Scholar]
- 89.Grubb BR, DuVal GF, Morris JS, Bentley Accumulation of cadmium by the eye with special reference to the lens. Toxicol Appl Pharmacol. 1985;77:444–50. doi: 10.1016/0041-008x(85)90184-x. [DOI] [PubMed] [Google Scholar]
- 90.Jacob JC, Duncan CT. The role of divalent cations in controlling amphibian lens membrance permeability: The mechanism of toxic cataract. Exp Eye Res. 1983;36:595–606. doi: 10.1016/0014-4835(83)90053-2. [DOI] [PubMed] [Google Scholar]
- 91.Science Daily; 2010. [Last accessed on 160411]. American Academy of Ophthalmology. Does HRT use raise women's cataract risk? Available from: http://www.sciencedaily.com¬/releases/2010/03/100301122326.htmArticle . [Google Scholar]
- 92.Harding JJ, van Heyningen R. Beer, cigarettes and military work as risk factors for cataract. Dev Ophthalmol. 1989;17:13–16. doi: 10.1159/000416990. [DOI] [PubMed] [Google Scholar]
- 93.Jacques PF, Chylack LT, Jr, McGandy RB, Hartz SC. Antioxidant status in persons with and without senile cataract. Arch Ophthalmol. 1988;106:337–40. doi: 10.1001/archopht.1988.01060130363022. [DOI] [PubMed] [Google Scholar]
- 94.Modern Brewery Age. FindArticles.com (Internet). Study says alcohol raises cataract risk. 22 February. 1993. [Last accessed on 16.04.11]. Available from: http://findarticles.com/p/articles/mi_m3469/is_n8_v44/ai_13661584 .
- 95.Duke ES. The pathological action of light upon the eye. Lancet. 1926;1:1188–91. [Google Scholar]
- 96.Hiller R, Giacometti L, Yuen K. Sunlight and cataract: An epidemiological investigation. Am J Epidemiol. 1977;105:450–59. doi: 10.1093/oxfordjournals.aje.a112404. [DOI] [PubMed] [Google Scholar]
- 97.Hollows F, Moran D. cataract-the ultraviolet risk factor. Lancet. 1981;11:1249–50. doi: 10.1016/s0140-6736(81)91490-2. [DOI] [PubMed] [Google Scholar]
- 98.Brilliant LB, Grasset NC, Pokhrel RP. Association among cataract prevalence, sunlight hours and altitude in the Himalayas. Am J Epidemiol. 1983;118:250–64. doi: 10.1093/oxfordjournals.aje.a113632. [DOI] [PubMed] [Google Scholar]
- 99.Wright RE. The possible influence of solar radiation on the production of cataract in certain districts of Southern India. Indian J Med Res. 1937;24:917–20. [Google Scholar]
- 100.Bachem A. Ophthalmic ultraviolet action spectra. Am J Ophthalmol. 1956;41:969–75. doi: 10.1016/0002-9394(56)91044-3. [DOI] [PubMed] [Google Scholar]
- 101.Pitts DG, Cullen AP, Hacker PD. Ocular effects of ultraviolet radiation from 295 to 365 nm. Invest Ophthalmol Vis Sci. 1977;16:932–39. [PubMed] [Google Scholar]
- 102.Merriam J, Lofgren S, Michael R, Soderberg PG, Dillon J, Zheng L, et al. An action spectrum for UV-B radiation in the rat lens. Invest Ophthalmol Vis Sci. 2000;41:2642–47. [PubMed] [Google Scholar]
- 103.Godar D, Wengraitis S, Shreffler J, Sliney D. UV doses of Americans. Photochem Photobiol. 2001;73:621–29. doi: 10.1562/0031-8655(2001)073<0621:udoa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 104.Sliney DH. How light reaches the eye and its components. Int J Toxicol. 2002;21:501–09. doi: 10.1080/10915810290169927. [DOI] [PubMed] [Google Scholar]
- 105.Taylor HR, West SK, Rosenthal FS, Munoz B, Newland HS, Abbey H, et al. Effect of ultraviolet radiation on cataract formation. N Engl J Med. 1988;319:1429–33. doi: 10.1056/NEJM198812013192201. [DOI] [PubMed] [Google Scholar]
- 106.Delcourt C, Carriere I, Ponton Sanchez A, Lacroux A, Caovacho MJ, Papoz L. Light exposure and the risk of cortical, nuclear and posterior subcapsular cataracts: Pathologies Oculaires Liees a I’Age (POLA) study. Arch Ophthalmol. 2000;118:385–92. doi: 10.1001/archopht.118.3.385. [DOI] [PubMed] [Google Scholar]
- 107.McCarty CA, Nanjan MB, Taylor HR. Attributable risk estimates for cataract to prioritize medical and public health action. Invest Ophthalmol Vis Sci. 2000;41:3720–25. [PubMed] [Google Scholar]
- 108.Widmark J. Ueber den Einfluss des Lichtes auf die Linse. In: Widmark J, editor. Mitteilungen aus der Augenklink des Carolinischen Medico-chirugischen Instituts zu Stockholm. Jena: Verlag von Gustav Fischer; 1901. pp. 135–49. [Google Scholar]
- 109.Soderberg PG. Acute cataract in the rat after exposure to radiation in the 300 nm wavelength region. Acta Ophthalmol. 1988;66:141–52. doi: 10.1111/j.1755-3768.1988.tb04001.x. [DOI] [PubMed] [Google Scholar]
- 110.Boettner EA, Wolter JR. Transmission of ocular media. Invest Ophthalmol Vis Sci. 1962;1:776–83. [Google Scholar]
- 111.Suryanarayana P, Saraswat M, Mrudula T, Krishna TP, Krishnaswamy K, Reddy GB. Curcumin and turmeric delay streptozotocin-induced diabetic cataract in rats. Invest Ophthalmol Vis Sci. 2005;46:2092–99. doi: 10.1167/iovs.04-1304. [DOI] [PubMed] [Google Scholar]
- 112.Brian BB, Jared EM, Nicholas BV, Doanald SR, Gholam AP. The lens, cataract and its management. In: Peyman GA, Sander DR, Goldberg MF, editors. Principles and Practice of Ophthalmology. Vol. 1. New Delhi, India: Jaypee Brothers; 1987. pp. 489–510. [Google Scholar]
- 113.Root T. OphthoBook.com (Internet). Introduction to the lens and cataract surgery. July. 2008. [Last accessed on 08.09.10]. Available from: http://www.ophthobook.com/chapters/cataract.pdf .
- 114.Bhat KS. Nutrition and cataract. Bulletin Nutr Fond India. 1993;14:01–03. [Google Scholar]
- 115.Shearer TR, David LL, Anderson RS. Review of selenite cataract. Curr Eye Res. 1992;11:357–69. doi: 10.3109/02713689209001789. [DOI] [PubMed] [Google Scholar]
- 116.Balasubramanian D, Bansal AK, Basti S, Bhatt KS, Murthy JS, Rao CM. The biology of cataract. The Hyderabad cataract research group. Indian J Ophthalmol. 1993;41:153–71. [PubMed] [Google Scholar]
- 117.Lou M. Redox regulation in the lens. Prog Retinal Eye Res. 2003;22:657–82. doi: 10.1016/s1350-9462(03)00050-8. [DOI] [PubMed] [Google Scholar]
- 118.Heck D, Gerecke D, Vetrao A, Laskin J. Solar ultraviolet radiation is a trigger of cell signal transduction. Toxicol Appl Pharmacol. 2004;195:288–97. doi: 10.1016/j.taap.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 119.Kathleen A. Natural therapies for ocular disorders. Part two: Cataract and Glaucoms. Altern Med Rev. 2001;6:141–66. [PubMed] [Google Scholar]
- 120.Prasad LV. Eye Institute (Internet). Blindness due to consanguineous marriages. [Last accessed on 12.07.12]. Available from: http://www.lvpei.org/resources/eye-faq/blindnessdue.html .
- 121.Narchi H. C-1 Causes of Birth defects. In: Engels JV, editor. Birth defects: New Reaserch. New York: Nova Publishers; 2006. p. 208. [Google Scholar]
- 122.Bosch AM. Classical galactosaemia revisited. J Inherit Metab Dis. 2006;29:516–25. doi: 10.1007/s10545-006-0382-0. [DOI] [PubMed] [Google Scholar]
- 123.Mohan R, Muralidharan AR. Steroid induced glaucoma and cataract. Indian J Ophthalmol. 1989;37:13–16. [PubMed] [Google Scholar]
- 124.Wang J, Lofgren S, Dong X, Galichanin K, Soderberg PG. Dose-response relationship for α-tocopherol prevention of ultraviolet radiation induced cataract in rat. Exp Eye Res. 2011;93:91–97. doi: 10.1016/j.exer.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 125.Ray Sahelian. (Internet) Cataract prevention and treatment with natural supplements, herbs and vitamins. [Last accessed on 12.07.12]. Available from: http://www.raysahelian.com/cataract.html .
- 126.Chandler HL, Reuter KS, Sinnott LT, Nichols JJ. Prevention of UV-Induced Damage to the Anterior Segment Using Class I UV-Absorbing Hydrogel Contact Lenses. Invest Ophthalmol Vis Sci. 2010;51:172–78. doi: 10.1167/iovs.09-3996. [DOI] [PubMed] [Google Scholar]


