Abstract
Context:
The provision of ocular surgical interventions for poorer, less educated populations is increasing as a result of increased globalization and outreach. However, these populations still have trouble understanding surgical concepts and are not always fully informed decision makers.
Aims:
We aimed to test the effect that a multimedia addition to a traditional verbal informed consent would have on patient comprehension of relatively difficult cataract surgical concepts.
Settings and Design:
We conducted a randomized controlled trial with relatively uneducated patients reporting to a private surgical hospital in Chennai, India. 47 patients were placed into the intervention group and 50 patients were placed into the control group.
Materials and Methods:
The intervention group was presented with a scripted verbal informed consent as well as a 3-fold pamphlet and a presentation with a 3-dimensional model of the eye. The control group was only presented with a scripted verbal informed consent. The two groups were tested using an 11 item “True/False/I don’t know” quiz directly before the informed consent, directly after the informed consent, and one-day postoperatively.
Statistical Analysis Used:
Scores on the quiz were compared across groups and time-points using paired t-tests.
Results:
Patients in the both groups showed a significant improvement in scores between pre- and post-informed consent quizzes (P value on the order of 10-6) and the improvement in scores was significantly greater in the intervention group than the control group (P value on the order of 10-16). There was no significant difference observed in either group with regards to the change in scores between post-informed consent and post-operative quizzes.
Conclusion:
Multimedia aids in addition to a standard informed consent process are effective in improving patient comprehension even for patients with low literacy and limited knowledge of surgical interventions.
Keywords: Cataract surgery, education, informed consent, multimedia, rural health
Proper informed consent is an ethical imperative that is meant to protect patients who elect to undergo invasive medical procedures. Despite attention directed towards the informed consent process, patients undergoing surgical procedures may not comprehend up to 50% of the information presented and have low rates of post-operative retention of information.[1,2] The informed consent process can be especially challenging for indigent patients in developing countries who may have limited formal education, high rates of illiteracy, and incorrect ideas about medical interventions.[3,4,5]
Consenting a patient for cataract surgery may be particularly challenging due to the complexity of ocular anatomy and the often misunderstood nature of ocular surgery.[6,7] The cognitive theory of multimedia learning, which has been applied to improving medical education for professionals, posits that people have two separate channels for processing verbal and pictorial material, and that learners can only process a limited amount of information in any one channel at any one point in time.[8] By activating both channels, such as utilizing a visual aid during a verbal informed consent, a larger amount of information may be communicated. Many reports have identified that the comprehension of a written consent is improved by adding a verbal component, and both comprehension and retention are further improved with the use of multimedia components.[9,10,11,12,13,14] On the contrary, other reports on patient populations in the western world have not shown multimedia based informed consent procedures to consistently improve understanding more than simple paper based methods.[15,16,17] Similar to studies in the western world, there are mixed reports regarding the value of verbal interactions and multimedia elements to the informed consent process seen in the developing world.[4,18] In a previous smaller study, we found that using a visual diagram improved retention of information for indigent patients undergoing surgery at a South Indian cataract surgery camp.[19]
In this randomized controlled trial, we examined whether using multiple multimedia resources in addition to a verbal informed consent would improve patient comprehension of cataract surgery in a group of indigent patients presenting for cataract surgery in rural South India.
Materials and Methods
All the participants who were considered for participation in our study were patients from rural villages and slums around Chennai, India and were evaluated at eye care camps organized by a local non-governmental organization (Unite for Sight), and scheduled for cataract surgery per the usual routine of the eye care camps. Patients, who presented for cataract surgery during July and August 2010, were approached to participate in the study. Not all patients who presented for surgery were approached to participate in the study, but recruitment for this study was based entirely on the resources and availability of study personnel and not based on any selection bias or prior knowledge of patient demographics. Exclusion criteria included not being able to see more than 1 meter in at least one eye, having any significant hearing impairment, or any obvious mental condition that would adversely affect comprehension of materials. Verbal informed consent to participate in the study was obtained from all participants.
Participants were blinded to the study design and objectives to prevent undue concentration on the study material. Patients participated in the study individually, in a closed room, where other participants could not observe the informed consent process. Patients were allotted to the control or intervention group based on when they presented for surgery. The first 50 participants were placed into the control group and the next 47 were placed into the intervention group. Randomization was retrospectively confirmed as patients were evenly matched in demographic categories. To obtain a power of 0.8 at a minimum significance level of 0.01 and a large effect size (Cohen's d = 0.8), each group would require at least 38 patients.[20] A total of 47 patients were placed in the intervention group and 50 patients served as controls.
An 11-question true-false quiz regarding the risks, benefits, alternatives, and procedural components of cataract surgery was created by two of the authors (HRM and AK) to concisely cover key components of the nature of cataracts, generalities regarding the cataract surgical procedure, and significant risks and benefits of cataract surgery. All items on the quiz were addressed in the scripted verbal informed consent [Fig. 4]. An “I don’t know” option was offered as an attempt to reduce guessing by the study participants. The questionnaire was translated by two local ophthalmologists, as well as an optometrist working for the NGO (Unite for Sight) and they verified the level of complexity to be appropriate for the study population. The quiz was first validated by 100% correct answers by 4 practicing ophthalmologists and 4 resident ophthalmologists in a U.S.-based university. The questionnaire was then tested for face validity in a previous study by the authors and was deemed culturally appropriate and understandable for use in this population.[19]
Figure 4.
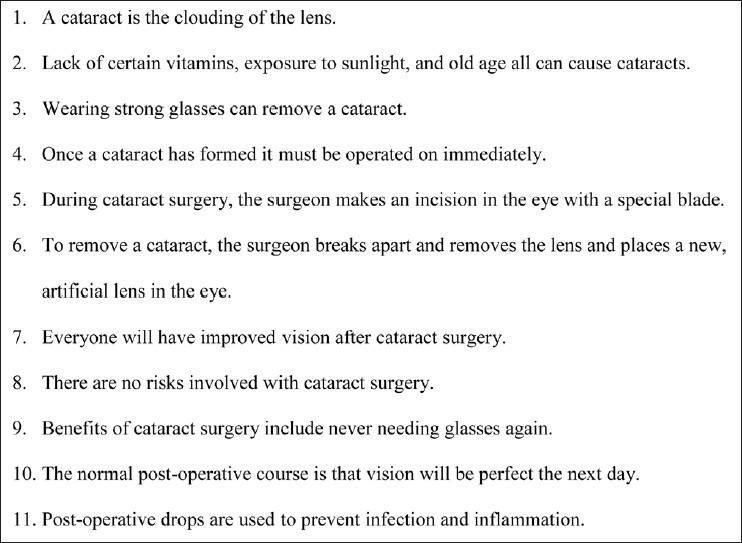
Informed consent T/F quiz
All participants in both groups were first given the quiz immediately after agreement to participate in the study. The quiz experience was tightly regulated and if necessary, patients were dissuaded from asking questions that may have biased the quiz results. Participants in both groups were then presented with a verbal informed consent read from a script by a native Tamil-speaking interviewer in a rehearsed, unbiased voice. Only one interviewer was used in this study to reduce interviewer bias. The recitation of this script took roughly 2-3 minutes per patient. In addition to the verbal informed consent, patients in the intervention group were presented with pamphlets [Figs. 1 and 2] outlining the surgical and post-operative procedure and general information regarding cataracts. These pamphlets were designed by the NGO (Unite for Sight), an ophthalmologist at the partner eye clinic in Chennai, and a team of visual communication specialists at a U.S.-based university. Patients in the intervention group were also shown a three-dimensional model of the eye and a short, scripted demonstration of cataract formation in reference to opacification of the ocular lens. This demonstration took roughly 10 minutes per participant in the intervention group. The pamphlet was presented first (and eventually taken home), followed by the scripted presentation of the three-dimensional model. Immediately after informed consent, participants in both groups were re-administered the quiz. All patients underwent cataract surgery the same day. One day post-operatively, patients were re-administered the same quiz.
Figure 1.
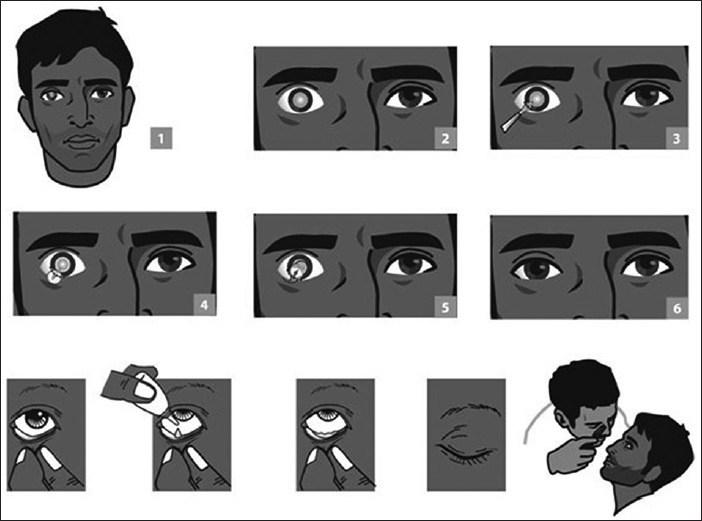
Cataract surgical procedure
Figure 2.
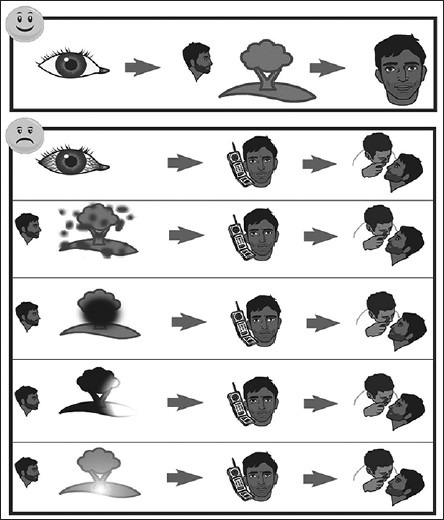
Post-operative complications
Using the R-programming language, the average number of questions answered correctly was compared within the control and intervention groups across the three time points as well as between groups for the pre-informed consent scores using a paired t-test. The difference in scores across the time points was compared between the control and intervention groups using paired t-tests as well. We did not use a repeated measure ANOVA because this experiment was primarily focused on a single intervention as the lapse in time between the 2nd and 3rd quiz scores did not appear to have any significant effect and was, thus, not a conceptually critical aspect of the study.
Results
Participants in both groups were evenly matched in demographic characteristics including age, gender, education level, literacy, hearing disability, presence of a caretaker, previous eye surgery, number of friends with previous eye surgery, past problems with eye surgery, and fear of eye surgery (all P > 0.10).
The quiz was scored by the number of questions correct out of 11. If a participant answer incorrectly or “I don’t know,” it was counted as a 0 toward the final score. Initial pre-informed consent quiz scores were not significantly different in the control and intervention groups [Table 1, 2], confirming the absence of any initial grouping bias (P = 0.84).
Table 1.
Sample mean proportion of questions answered correctly, mean (standard deviation)
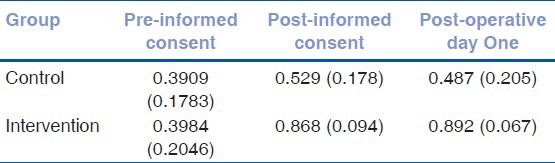
Table 2.
Sample mean number of questions answered correctly out of 11
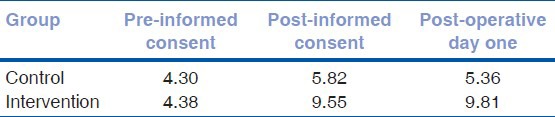
Patients in the both groups showed a significant improvement in scores between pre- and post-informed consent quizzes (P value on the order of 10-6) [Table 3 and Fig. 3]. The improvement in scores from before and after the informed consent process was significantly greater in the intervention group than the control group (P value on the order of 10-16) [Table 3 and Fig. 3]. There was no significant difference observed in either group with regards to the change in scores between post-informed consent and post-operative quizzes.
Table 3.
Average difference in scores between testing sessions
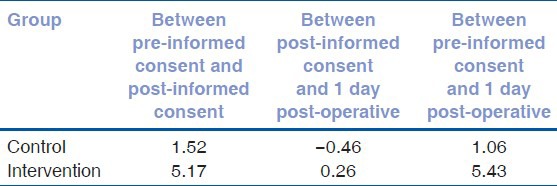
Figure 3.
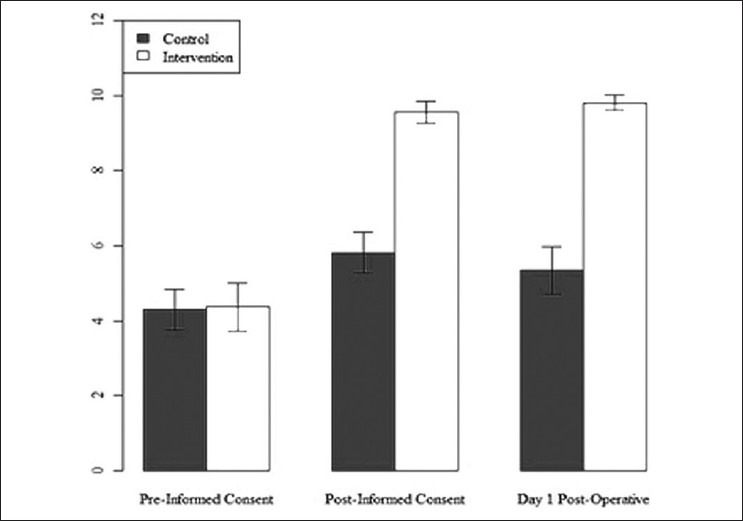
Number of correct responses
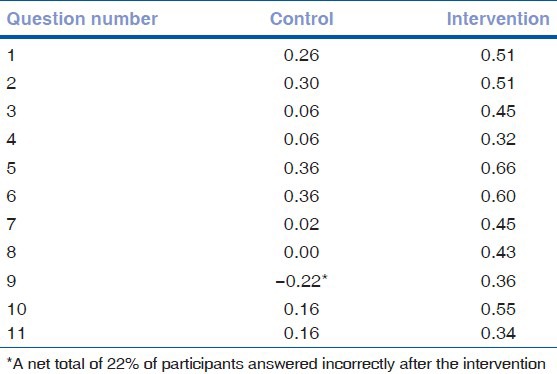
Table 4 displays the net improvement on individual questions by group. If a patient changed an answer from an incorrect response or “I don’t know” to the correct response, this was marked as “+1”, whereas if the patient changed an answer from the correct answer or “I don’t know” to the incorrect response, this was marked as “−1”. The net totals were taken among all patients and divided by the number of patients in the group to obtain the rate of improvement. Only one question showed a net decrease in the rate of change (question 8 in the control group). In both groups, the greatest improvement was seen on questions 5 and 6, both of which involved cataract surgical procedure that was presented in the handouts and demonstrated with the eye model. Patients in the intervention group had a higher rate of improvement on each individual question when compared to the control group.
Table 4.
Net rate of improvement per question between pre- and post-informed consent groups
Discussion
Consistently effective methods of informed consent have been a challenge to implement in the developed world.[21] Impediments to an effective informed consent may be even greater in developing countries where many research trials and medical procedures involve patients who often have little formal education and few socioeconomic resources, among other challenges.[3,22] Despite the barriers, studies have shown that patients in developing countries place a high value on the informed consent.[23,24,25] Unfortunately, patients in the developing world are often be subjected to paternalistic attitudes from practitioners who underestimate the value of informed consent.[25,26,27,28] In a previous study of similar design with a smaller patient population, we found that patients presented with a poster intervention during the informed consent process for cataract surgery had significantly greater retention of information on post-operative day one.[19]
This study demonstrated that in this rural, indigent South Indian population, a verbal informed consent alone or a verbal informed consent in combination with multimedia resources significantly increases understanding of cataracts and cataract surgery. In addition, this study identified that a verbal informed consent augmented with multimedia resources, in this case a pamphlet with pictures and a 3-dimensional eye model, improves comprehension significantly more than a verbal informed consent alone, as expected by the cognitive theory of multimedia learning.[8] Furthermore, improvements on individual questions were higher for the questions that had images directly associated to information in the pamphlets. This study also demonstrated improved retention of subject matter one day post-operatively in both groups, with significantly higher scores maintained in the intervention group. Interestingly, the multimedia demonstration, unlike the scripted verbal informed consent, was not tailored towards the quiz. It is possible that the improved scores were a result of a greater general sense of understanding regarding cataracts and cataract surgery, as opposed to patients reiterating answers to specific questions.
While improved informed consent provision is crucial in all populations, from an ethical standpoint, the findings concerning the efficacy of a multimedia approach have broader implications for education regarding complex medical procedures that are now more commonly being performed on previously neglected populations in developing countries.[27] In addition to improving informed consent, multimedia aids could improve the quality of post-operative care and surgical outcomes as well as education on preventative healthcare. We encourage further research into the value of multimedia presentations in various types of patient education scenarios, as well as investigation into optimal multimedia images and models for various target populations.
Our study included a number of limitations. There was a lack of true randomization of the control and intervention groups. However, there were no significant demographic differences between the groups, in part validating our efforts to create a non-biased patient selection process that was feasible based on the limited number of investigative resources in the face of a large patient population. Greater test subject numbers may have allowed for more subtle data analysis, such as differences between ages, educational status, or gender, but our current sample size met the statistical criteria for an appropriately powered study for the conclusions drawn. A subsequent testing session at a later time-point, such as one week or one month after the initial intervention, may have elucidated information about longer-term retention of information. Finally, it was difficult to ensure complete standardization of a clinically-practical informed consent experience. We chose not to use a recording for the verbal consent as we felt this may introduce unforeseen biases, such as ill-fitting headphones or inappropriate patient attention. We tried to improve standardization by using a single, native Tamil speaking researcher and a scripted informed consent process.
In this rural, indigent South Indian population, an informed consent improved patients’ understanding of the risks, benefits, alternatives, and side effects of cataract surgery, as seen in previous informed consent studies in the developed world. In this study population, the addition of visual aids during the informed consent process significantly improved comprehension of information more than a verbal informed consent alone, and improvement in comprehension persisted one day after the informed consent.
Acknowledgment
The authors would like to acknowledge the Unite for Sight NGO and its affiliated staff for helping in the logistical demands of this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Fink AS, Prochazka AV, Henderson WG, Bartenfeld D, Nyirenda C, Webb A, et al. Predictors of comprehension during surgical informed consent. J Am Coll Surg. 2010;210:919–26. doi: 10.1016/j.jamcollsurg.2010.02.049. [DOI] [PubMed] [Google Scholar]
- 2.Morgan LW, Schwab IR. Informed consent in senile cataract extraction. Arch Ophthalmol. 1986;104:42–5. doi: 10.1001/archopht.1986.01050130052018. [DOI] [PubMed] [Google Scholar]
- 3.Krogstad DJ, Diop S, Diallo A, Mzayek F, Keating J, Koita OA, et al. Informed consent in international research: The rationale for different approaches. Am J Trop Med Hyg. 2010;83:743–7. doi: 10.4269/ajtmh.2010.10-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fitzgerald DW, Marotte C, Verdier RI, Johnson WD, Jr, Pape JW. Comprehension during informed consent in a less-developed country. Lancet. 2002;360:1301–2. doi: 10.1016/S0140-6736(02)11338-9. [DOI] [PubMed] [Google Scholar]
- 5.Mystakidou K, Panagiotou I, Katsaragakis S, Tsilika E, Parpa E. Ethical and practical challenges in implementing informed consent in HIV/AIDS clinical trials in developing or resource-limited countries. SAHARA J. 2009;6:46–57. doi: 10.1080/17290376.2009.9724930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson GJ. Improving outcome of cataract surgery in developing countries. Lancet. 2000;355:158–9. doi: 10.1016/S0140-6736(99)00404-3. [DOI] [PubMed] [Google Scholar]
- 7.Abbott RL. Informed consent for cataract surgery. Curr Opin Ophthalmol. 2009;20:52–5. doi: 10.1097/ICU.0b013e32831b6dcf. [DOI] [PubMed] [Google Scholar]
- 8.Mayer RE. Applying the science of learning to medical education. Med Educ. 2010;44:543–9. doi: 10.1111/j.1365-2923.2010.03624.x. [DOI] [PubMed] [Google Scholar]
- 9.Moseley TH, Wiggins MN, O’Sullivan P. Effects of presentation method on the understanding of informed consent. Br J Ophthalmol. 2006;90:990–3. doi: 10.1136/bjo.2006.092650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scanlan D, Siddiqui F, Perry G, Hutnik CM. Informed consent for cataract surgery: What patients do and do not understand. J Cataract Refract Surg. 2003;29:1904–12. doi: 10.1016/s0886-3350(03)00234-7. [DOI] [PubMed] [Google Scholar]
- 11.Wanzer MB, Wojtaszczyk AM, Schimert J, Missert L, Baker S, Baker R, et al. Enhancing the “informed” in informed consent: A pilot test of a multimedia presentation. Health Commun. 2010;25:365–74. doi: 10.1080/10410231003775198. [DOI] [PubMed] [Google Scholar]
- 12.Beamond BM, Beischer AD, Brodsky JW, Leslie H. Improvement in surgical consent with a preoperative multimedia patient education tool: A pilot study. Foot Ankle Int. 2009;30:619–26. doi: 10.3113/FAI.2009.0619. [DOI] [PubMed] [Google Scholar]
- 13.Bollschweiler E, Apitzsch J, Obliers R, Koerfer A, Mönig SP, Metzger R, et al. Improving informed consent of surgical patients using a multimedia-based program? Results of a prospective randomized multicenter study of patients before cholecystectomy. Ann Surg. 2008;248:205–11. doi: 10.1097/SLA.0b013e318180a3a7. [DOI] [PubMed] [Google Scholar]
- 14.Panton RL, Downie R, Truong T, Mackeen L, Kabene S, Yi QL, et al. A visual approach to providing prognostic information to parents of children with retinoblastoma. Psychooncology. 2009;18:300–4. doi: 10.1002/pon.1397. [DOI] [PubMed] [Google Scholar]
- 15.Agre P, Campbell FA, Goldman BD, Boccia ML, Kass N, McCullough LB, et al. Improving informed consent: The medium is not the message. IRB. 2003;25:S11–S19. [PubMed] [Google Scholar]
- 16.Agre P, Rapkin B. Improving informed consent: A comparison of four consent tools. IRB. 2003;25:1–7. [PubMed] [Google Scholar]
- 17.Weston J, Hannah M, Downes J. Evaluating the benefits of a patient information video during the informed consent process. Patient Educ Couns. 1997;30:239–45. doi: 10.1016/s0738-3991(96)00968-8. [DOI] [PubMed] [Google Scholar]
- 18.Joseph P, Schackman BR, Horwitz R, Nerette S, Verdier RI, Dorsainvil D, et al. The use of an educational video during informed consent in an HIV clinical trial in Haiti. J Acquir Immune Defic Syndr. 2006;42:588–91. doi: 10.1097/01.qai.0000229998.59869.05. [DOI] [PubMed] [Google Scholar]
- 19.Karan A, Campbell D, Mayer HR. The effect of a visual aid on the comprehension of cataract surgery in a rural, indigent South Indian population. Digital J Ophthalmol. 2011;17:3. doi: 10.5693/djo.01.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen J. A power primer. Psychol Bull. 1992;112:155–9. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 21.Flory J, Emanuel E. Interventions to improve research participants’ understanding in informed consent for research: A systematic review. JAMA. 2004;292:1593–601. doi: 10.1001/jama.292.13.1593. [DOI] [PubMed] [Google Scholar]
- 22.O’Donnell O. Access to health care in developing countries: Breaking down demand side barriers. Cad Saude Publica. 2007;23:2820–34. doi: 10.1590/s0102-311x2007001200003. [DOI] [PubMed] [Google Scholar]
- 23.Humayun A, Fatima N, Naqqash S, Hussain S, Rasheed A, Imtiaz H, et al. Patients’ perception and actual practice of informed consent, privacy and confidentiality in general medical outpatient departments of two tertiary care hospitals of Lahore. BMC Med Ethics. 2008;9:14. doi: 10.1186/1472-6939-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yousuf RM, Fauzi AR, How SH, Rasool AG, Rehana K. Awareness, knowledge and attitude toward informed consent among doctors in two different cultures in Asia: a cross-sectional comparative study in Malaysia and Kashmir, India. Singapore Med J. 2007;48:559–65. [PubMed] [Google Scholar]
- 25.Sanwal AK, Kumar S, Sahni P, Nundy S. Informed consent in Indian patients. J R Soc Med. 1996;89:196–8. doi: 10.1177/014107689608900406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luna F. Paternalism and the argument from illiteracy. Bioethics. 1995;9:283–90. doi: 10.1111/j.1467-8519.1995.tb00363.x. [DOI] [PubMed] [Google Scholar]
- 27.Isaacson G, Drum ET, Cohen MS. Surgical missions to developing countries: Ethical Conflicts. Otolaryngol Head Neck Surg. 2010;143:476–9. doi: 10.1016/j.otohns.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 28.Saleem T, Khalid U. Informed consent in developing countries: Dilemmas and deliberations. J Pak Med Assoc. 2009;59:805. [PubMed] [Google Scholar]


