Abstract
Aim:
To study long term outcome of bilateral congenital and developmental cataract surgery.
Subjects:
258 pediatric cataract operated eyes of 129 children.
Materials and Methods:
Children who underwent pediatric cataract surgery in 2004-8 were traced and examined prospectively in 2010-11. Demographic and clinical factors were noted from retrospective chart readings. All children underwent visual acuity estimation and comprehensive ocular examination in a standardized manner. L. V. Prasad Child Vision Function scores (LVP-CVF) were noted for before and after surgery.
Statistics:
Statistical analysis was done with SPSS version 16 including multi-variate analysis.
Results:
Children aged 9.1 years (std dev 4.6, range 7 weeks-15 years) at the time of surgery. 74/129 (57.4%) were boys. The average duration of follow-up was 4.4 years (stddev 1.6, range 3-8 years). 177 (68.6%) eyes had vision <3/60 before surgery, while 109 (42.2%) had best corrected visual acuity (BCVA) >6/18 and 157 (60.9%) had BCVA >6/60 3-8 years after surgery. 48 (37.2%) had binocular stereoacuity <480 sec of arc by TNO test. Visual outcome depended on type of cataract (P = 0.004), type of cataract surgery (P < 0.001), type of intra-ocular lens (P = 0.05), age at surgery (P = 0.004), absence of post-operative uveitis (P = 0.01) and pre-operative vision (P < 0.001), but did not depend on delay (0.612) between diagnosis and surgery. There was a statistically significant improvement for all the 20 questions of the LVP-CVF scale (P < 0.001).
Conclusion:
Pediatric cataract surgery improved the children's visual acuity, stereo acuity and vision function. Developmental cataract, use of phacoemulsification, older children and those with better pre-operative vision had betterlong-termoutcomes.
Keywords: Congenital cataract, developmental cataract, outcome, vision function
Recent studies from India and other parts of the world have demonstrated pediatric cataract to be a significant cause of severe visual impairment and blindness in children.[1,2,3,4] ORBIS International, an international non-governmental developmental organisation had helped set up 29 tertiary pediatric eye care centres in India with the aim to combat avoidable childhood blindness. Pediatric cataracts are a surgically treatable cause of blindness. There have been few reports of outcomes of pediatric cataract from South Asia, but most were limited to one week to six weeks follow up.[5,6,7] However, outcomes of pediatric cataract vary with time as a child grows and develops, unlike that of an adult. South Asia has the largest number of children affected with pediatric cataracts but there have been few studies in published literature regarding long term follow-up of one year or more in these children.[8] While improvement in visual acuity have been documented; there are few reports on how the intervention affects the child's vision function and ability to negotiate with the environment, his/her peers and participate in educational and vocational activities.[9] The aim of our study was to gauge the 3-8 year follow up of congenital and developmental cataracts operated in India; and to find how visual acuity, vision function and stereo-acuity of a child changed after pediatric cataract surgery.
Materials and Methods
The study was completed in July 2010-July 2011 in a pediatric ophthalmology department of a comprehensive eye care centre. It was a retrospective-prospective, longitudinal, interventional study. Permission was sought for and obtained from the ethical committee of the Lions NAB Eye Hospitall (LNEH). From the medical record section of LNEH, the case records of all children who were operated for cataract surgery from 2004-2008 were collated and studied. They had been operated under the ORBIS International, India country office's childhood blindness initiative. Detailed case records had been maintained for reporting and monitoring. The children had undergone cataract surgery with intra-ocular lens (IOL) implantation, the power of which had been calculated using Dahan's formula.[10] Surgeons had implanted the IOL in the bag wherever possible. Primary posterior capsulotomy (PPC) and anterior vitrectomy (AV) was performed till age of six years. They had been prescribed topical steroid-antibiotic drops for six weeks in tapering doses along with a non-steroidal anti-inflammatory agent locally. Cycloplegic eye drops were used for first two weeks. Amblyopia treatment and spectacle correction had been prescribed at the one week follow-up. The children were to have a six weeks, six m and then at least an annual follow-up.[11]
The addresses of each and every child along with the phone numbers had been carefully recorded. The children were then grouped according to talukas (sub-districts in Indian administration) and villages. These children were identified in their villages and towns and were visited by a medical social worker. Demographic data was recorded. The children who could be identified were transported in a vehicle to the hospital along with their parents for an eye examination during the period. They underwent a comprehensive ocular examination comprising slit lamp examination, orthoptic evaluation, tonometry, fundoscopy and cycloplegic refraction. Visual acuity was measured by the Snellen's chart, intra-ocular pressure (IOP) by a non-contact tonometer (Air puff tonometer, Nidek KLB instruments) stereoacuity with TNO charts. If any treatment was needed, be it spectacles, Nd: YAG laser posterior capsulotomy, surgery or low vision aids, the parents were informed, and relevant treatment provided free of cost to the children. The parents and children were also counselled during this visit about the importance of follow-up.
In spite of house visits and counselling, some children did not visit the examination centre. A detailed programme was made for house visits of these children. Apediatric ophthalmologist, an optometrist and a community worker visited these children at their home with the required portable equipments like visual acuity charts, slit lamp, keratometer and A-scan to examine these children in their homes.
Only those in whom a reliable history was available were classified as having congenital (opacity detected within first six m of life) or developmental (opacity detected after seven m of age) cataract. ‘Congenital/developmental’ cataracts were completely white and mature cataracts in which no reliable history or morphology was available as to whether they were developmental or congenital cataracts. Cataracts with signs of uveitis before surgery were termed complicated cataracts. Cataracts that had a confirmed delay between diagnosis of the disease and surgery of > 18 m were considered as delayed presenting cataracts.[9,12] This cut-off of 18 m was taken as reports from the developing world showed that delay of about a year between diagnosis and treatment was usual.[9,12] Children in whom this delay could not be verified with certainty, depending on case records and parents’ interviews, were classified as otherwise.
The L. V. Prasad Child Vision Function (LVP-CVF) questionnaire had been validated and used to gauge vision function of children in India.[13] The questionnaire was translated into Marathi, the regional language and back translated into English by three independent translators each way to validate the translation. The counsellors - cum - social worker who interviewed and counselled the child were trained to impart the questionnaire. It had 20 questions, 19 of which was scored 0 to 4; 0 - no difficulty at all to four - maximum difficulty and unable to perform the task due to impaired vision. The Likert scale was used in a manner that the counsellors would ask the parent/child about no difficulty (0%), little difficulty (25%, ‘chaaranna’), some difficulty (50%, ‘aathanna’), great difficulty (75%, ‘baraanna’) and unable to perform the task (100% difficulty, ‘purnarupaya’, scored 4).[13] Children over 12 years of age were encouraged to complete the questionnaire on their own and to take help from the counsellor only when required. For younger children, the questions were directed to the parents, especially the mother, with the child also participating in the semi-structured interviewing. For those questions which were inappropriate or not valid for that age group, a score of ‘9’ was taken and that score not considered for analysis. The post operative vision function scores were recorded as per the current vision function, while the preoperative ones were recorded after interview with parents and the child. The questionnaire is enclosed as Appendix A.
Statistical analysis was done using the SPSS version 19 software including multi-variate analysis with binary logistic regression.
Results
This study presents the results of 258 bilateral congenital and developmental cataracts of 129 children operated in 2004-8 and reassessed in 2010-11. At the time of surgery in 2004-8, the average age of the child was 9.1 years (std dev 4.6). 18 (14%) children aged 0-2 year; 18 (14%) aged 3-5 years, 55 (42.6%) aged 6-10 years, 27 (20.9%) aged 10-15 years and 10 (7.8%) aged 16 years, details regarding age were not clear for one child. The average age of the child at the time of assessment was 12.5 years (std dev 4.9). Of those examined 10 (7.8%) children were up to 5 years of age, 31 (24%) 6-10 years of age, 50 (35.9%) 11-15 years of age and 38 (29.4%) aged 16 years or more during the final assessment. 74/129 (57.4%) were boys. The average duration of follow-up between surgery and final assessment was 4.4 years (range 3 to 8 years, standard deviation 1.6 years).
Of the 258 cataracts, 32 (12.4%) were congenital, 98 (38%) were developmental, 4 (1.6%) were subluxated, 8 (3.1%) were complicated and 116 (45%) were ‘congenital/developmental’ cataracts. 204 (79%) surgeries had been performed by pediatric ophthalmologists, and 54 (21%) by general ophthalmologists. There was no statistically significant difference between the visual outcomes of pediatric and general ophthalmologists, in uni and multi variate analysis.
The mean preoperative visual acuity by decimal notation was 0.061 (SD 0.139), while mean post-operative visual acuity was 0.376 (SD 0.403) (P < 0.001 by paired t-test). 177 (68.6%) eyes had vision < 3/60 before surgery. 109 (42.2%) eyes had best corrected visual acuity (BCVA) > 6/18 at the 3-8 year follow-up, while 149 (57.8%) had it < 6/18. 157 (60.9%) eyes had BCVA > 6/60, while 101 (39.1%) had BCVA < 6/60. Amongst the type of surgery performed: 7 eyes underwent aspiration (all in year 2004), 22 underwent cataract aspiration with primary posterior capsulotomywith anterior vitrectomy (PPC + AV), 3 had manual small incision cataract aspiration with PPC + AV and posterior chamber IOL implantation (SICS + PPC + AV + PCIOL), another 3 phacoemulsification aspiration (Phaco) +PPC + AV + PCIOL, 61 had SICS + PCIOL and 99 were Phaco + PCIOL, 5 surgeries were with scleral fixated PCIOLs (SFIOL);13 underwent membranectomy (for cataracts that were membrane like), 9 had cataract surgery and then secondary PCIOL implants while 12 underwent cataract + PPC + AV and then secondary PCIOL implants. Details about surgery were not clear from the surgical notesof 24 operated eyes.
10 (3.9%) pseudophakic eyes had postoperative IOP > 20 mm of Hg, while 6 (2.3%) had signs of post-operative uveitis. 48 (37.2%) had binocular stereo acuity < 480 sec of arc by TNO test. One had 60 sec of arc stereopsis, 17 (13.2%) had 240 arc30 (23.9%) had binocular stereo acuity of 480 sec of arc stereopsis.
Table 1 demonstrates the various factors associated with visual outcome after surgery. Visual outcome depended on type of cataract (P = 0.004), type of surgery (P < 0.001), type of intra-ocular lens (P = 0.05), age at surgery (P = 0.003), absence of post-operative uveitis (P = 0.041) and pre-operative vision (P < 0.001).
Table 1.
Association of clinical and demographic factors with long term visual outcome
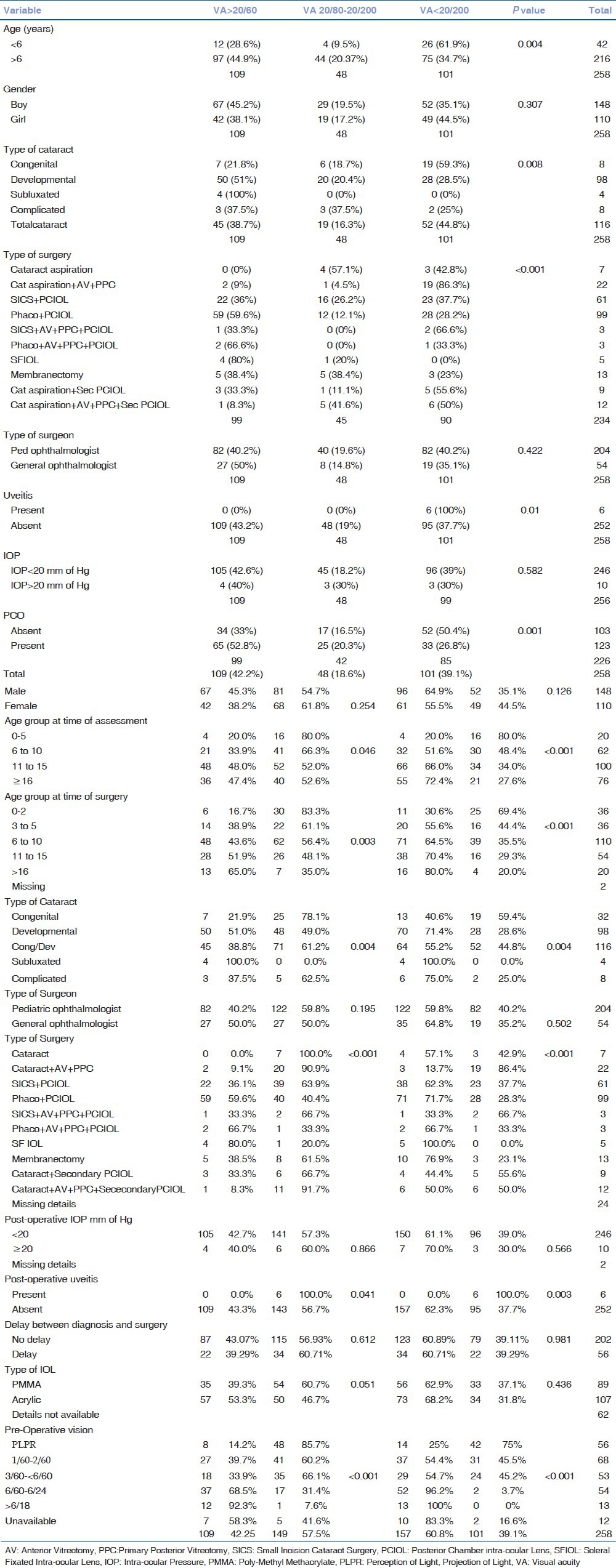
56/258 (21.7%) cataracts had a confirmed history of delay between diagnosis and surgery. The mean delay in these eyes was 4.9 years (SD 3.2, range 2-14 years). There was no significant difference in those cataracts that were operated after a delay between diagnosis and surgery and those that did not have such a delay (P = 0.062). Gender (P = 0.254) and type of operating surgeon (P = 0.502) did not affect visual acuity, but older children did better in terms of post-operative vision (P < 0.001). Eyes with better preoperative vision fared better after surgery (p < 0.001). Surgeries in which the phacoemulsification technique was used had a mean acuity of 0.51 (SD 0.39) compared to mean acuity of 0.31 (SD 0.35) in which it was not used (P < 0.01).
On binary logistic regression by backward elimination method, the odds ratio of age of surgery, pre-operative vision and type of surgery, phaco or SICS were the chief factors found significant.
Table 2 demonstrates the factors associated with raised IOP after surgery. The type of surgery performed (anterior vitrectomy and primary posterior capsulotomy) and male gender were significant variables. Similarly, table 3 illustrates factors responsible for post-operative posterior capsular opacification (PCO). The type of surgery performed, with specific reference to those in whom primary posterior capsulotomy was not performed and older age groups were significant variables for the occurrence of PCOs.
Table 2.
Variables associated with post-operative raised intra-ocular pressure
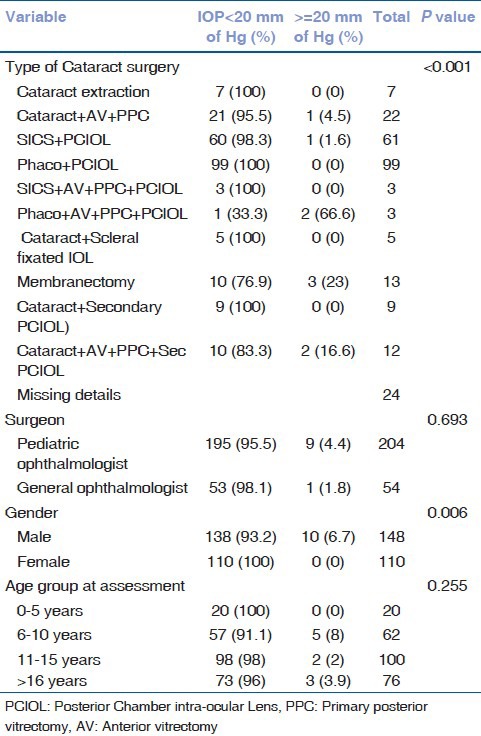
Table 3.
Variables associated with posterior capsular opacification
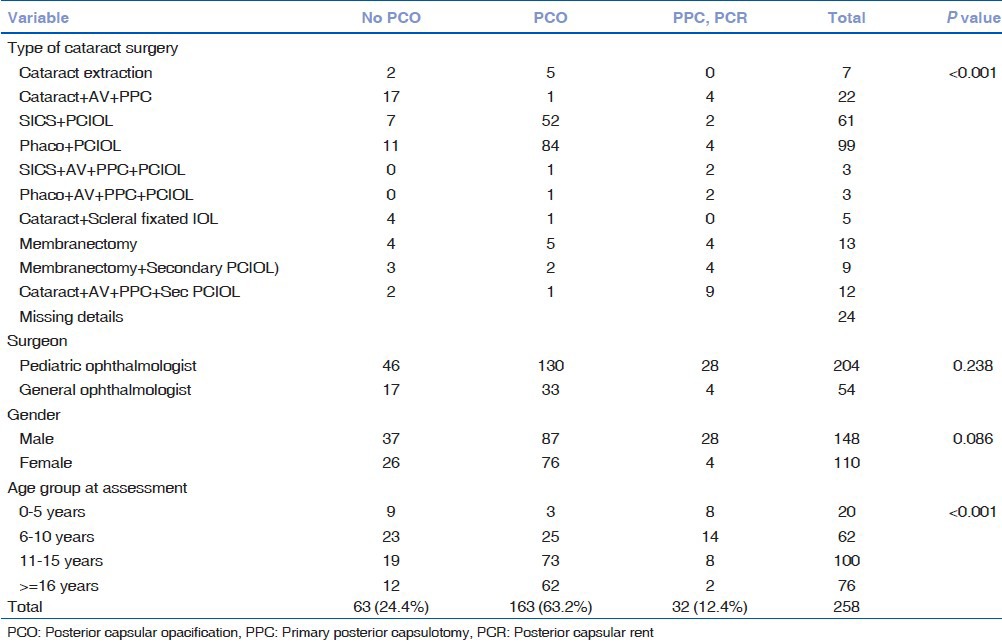
Significant posterior capsular opacificationwas seen in 163 (63.2%) eyes and absent (< grade 1) in 63 (24.4%) eyes who did not undergo primary posterior capsulotomy, while another 32 (11.2%) eyes had primary posterior capsulotomy performed or had posterior capsular rent (PCR). PCO was observed in childrenwith a longer follow-up. 65 eyes underwent Nd: YAG LASER capsulotomyunder topical anesthesia and another 5 under general anaesthesia.
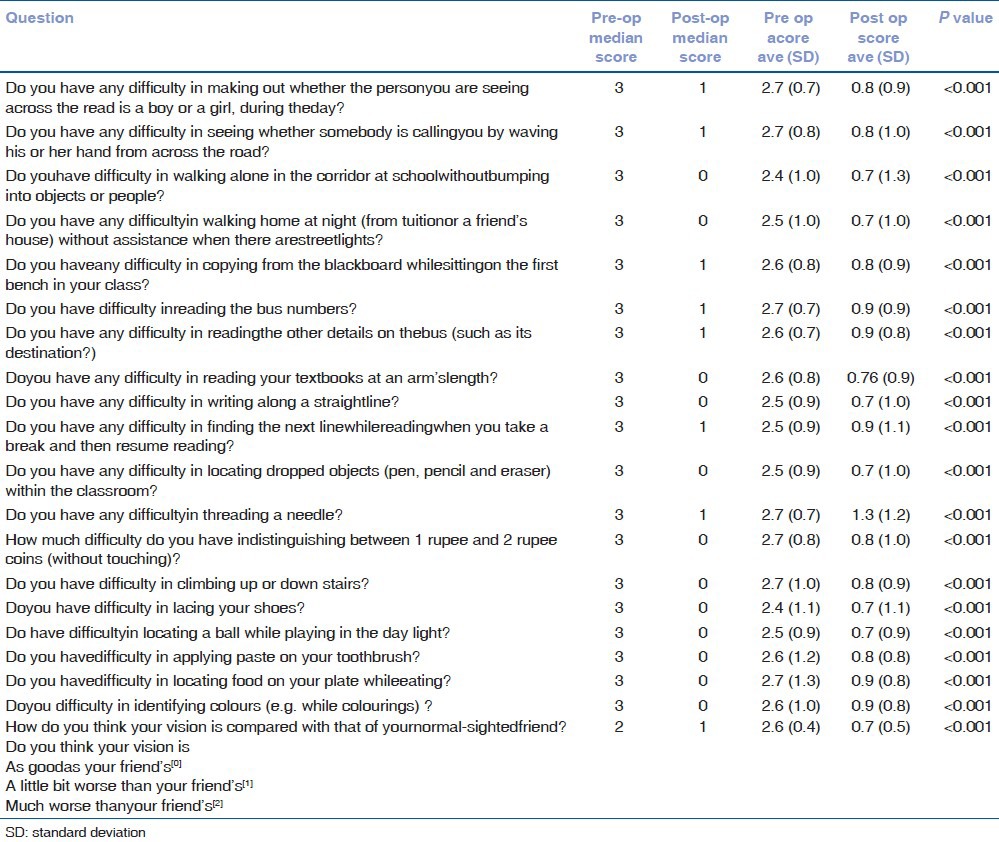
Table 4 demonstratesvisual function scores using the LVP-CVF before and after cataract surgery. There was a statistically significant difference in scores for all the questions before and after surgery, those related to distant vision, near vision, colour vision and field of vision.
Table 4.
Vision function scores before and after surgery (L.V.Prasad child vision function questionnaire used)
Discussion
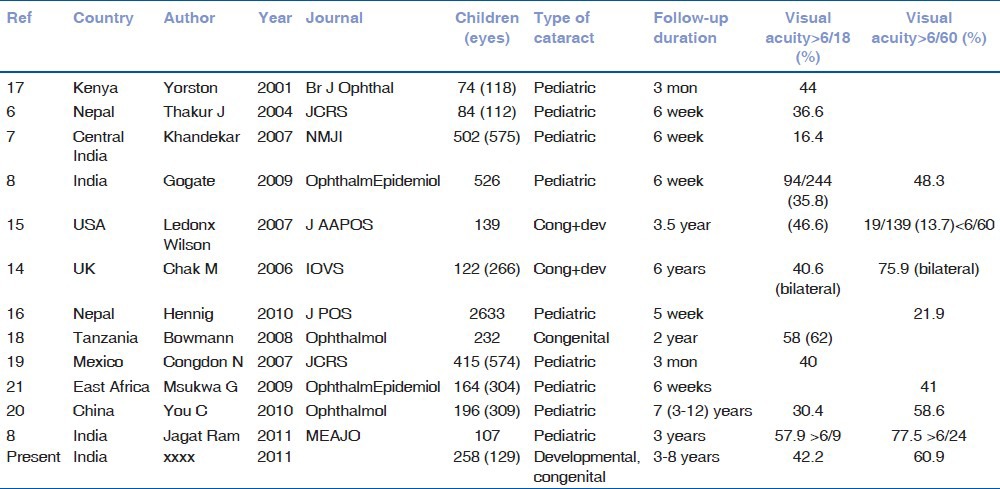
The series demonstrated that long term outcomes of development and congenital cataracts in India were good and improved the child's functioning, but were poorer compared to series from the UK and the US.[14,15] The outcomes were better than those reported from previousstudies fromIndia and Nepal, presumably because this study had a longer follow-up, and appropriaterefractive correction and amblyopia treatment had been started.[5,6,7,16] The visual outcomes of pediatric cataracts are compared in table 5.[5,6,7,8,14,15,16,17,18,19,20,21]
Table 5.
Comparison with other studies
Congenital cataracts had a poorer outcome, 44% children nonetheless demonstrated best corrected visual acuity (BCVA) of > 6/60. Congenital/developmental cataracts (which could be either developmental or congenital) followed with 51.4% children demonstrating visual acuity of > 6/60. This was similar to results from Nepal where most cataracts were mature and etiologically indistinguishable by morphological evaluation.[16] Cataracts which developed later in life after some visual maturation had occurred, be it complicated, sub-luxated or developmental fared better[7] with the older children demonstratinga better visual outcome. The poorer outcomes of cataract extraction with AV and PPC compared tophacoemulsification or SICS without AV and PPC done in children > 6 years of age may be due to this as AV and PPC was performedmostly in younger children with congenital cataracts. However, if the younger cohort with congenital cataracts who underwent AV and PPC versus those who did not (historically the earliest patients operated in 2004 before advent of necessary equipment and expertise) were compared, it was observed that eye that did not undergo AV with PPV uniformly fared poorly. This is similar to results reported forvery young children with cataract in studies from India and USA.[22,23]
Postoperative uveitis and rise in IOP affected the visual potential of these paediatric eyes. This again underlines the importance of a regular and repeated follow-ups of such cataract operated eyes. As mentioned previously, the type of surgery also affected outcome but age was a confounder as younger children needed AV and PPC and were more likely to have congenital cataracts.[9,14] Older children reported better outcomes. Cataracts operated by the phacoemulsification techniques had better results presumably because the automated irrigation aspiration may have ensured a more diligent cortical clean-up and better polishing of the residual posterior capsule. Use of phacoemulsification for pediatric cataract surgery is to be recommended wherever phacoemulsification machines and trained surgeons are available. As foldable acrylic lenses were used with phacoemulsification technique, compared to poly-methly-methacrylate (PMMA) with SICS, they may be associated with better outcomes. A study from north India reported equally good outcomes for PCO with PMMA and hydrophilic acrylic lenses while another had similar outcome with silicone and hydrophobic acrylic lenses.[22,24]
Posterior capsular opacification affected nearly half the pediatric cataract operated eyes and was a cause of poor postoperative visual acuity. Posterior capsular management should be more aggressive-PPC + AV should be performed till older age groups or early post-operative Nd: YAG LASER capsulotomy should be encouraged.[7,15,17,18,22,23] PCO was associated with older age group (in which AV + PPC was not performed) and longer duration of follow-up but not with gender of childor type of operating surgeon. Another study demonstrated hydrophobic acrylic lenses were associated with least PCO.[25]
The incidence of secondary glaucoma was much lesser than otherstudies from India and Arabia.[26,27,28,29] Reasons for this may be older age of children at the time of surgery and sparse use of high viscosity ophthalmic viscous devices.
Delay between diagnosis of cataract and cataract surgery was not a statistically significant variable affecting visual rehabilitation in this study unlike aseries from China, which comprised both unilateral and bilateral cataracts.[20] The cataract was recognized within 6 m of age in 46 children (40.7%) with bilateral cataract and 10 children (12.0%) with unilateral cataract.[20] Among these children, only 18 (15.9%) with bilateral cataract and 1 (1.2%) with unilateral cataract underwent surgery between 3 and 6 m of age. The outcomes were poorer in unilateral cataracts, visual impairment and blindness occurred 35.4% of eyes with bilateral cataract, and 74.7% of eyes with unilateral cataract.[20] Series from US and UK had better visual outcomes, possibly due to earlier detection and more aggressive and diligent follow-up.[14,15]
This study shows that outcomes of paediatric cataract surgery in India are comparableto those performed indeveloped countries, if proper surgical techniques and post-operative care protocols are followed, even though the cataracts may have been operated later in life. Paediatric cataract surgery, if properly performed is a boon to children blind with cataract, and no cost should deter the implementation of the same.[30]
Post-operatively, it was observed that not only had the children's vision improved their ability to learn and negotiate with the environment improved also. The assessedvision function data had two major limitations which were firstly, a recall bias as the pre-operative scores were calculated from parental memory and secondly because as the child grew older, cognitive functioning due to better BCVA was correspondingly different like for example an older child was capable of performing finer functions, like tying shoe laces or putting tooth paste on a tooth brush, which may not necessarily be related to better visual functions. There may also be a ‘floor’ and ‘ceiling’ effect in recording the scores. However, this is the first large long-term study, which documents the importance of pediatric cataract surgery on the child's life and functioning. Maximum efforts were made to keep the data unbiased. Ophthalmologists who operated and later evaluated the patients were not involved in the data collection. Social workers who were specially trained in interview skills and who were not part of the initial pediatric eye surgery team were recruited to minimize interviewer bias.
Acknowledgement
The clinical examination protocol was validated by Dr. Joan McLeod-Omnawale, ORBIS Director of Monitoring and Evaluation, Professor Clare Gilbert, International Centre for Eye Health, London School of Hygiene and Tropical Medicine, Dr. Rupal Trivedi, Associate Professor, Storm Eye Institute, South Carolina, Dr. H. Kishore, senior pediatric ophthalmologist, Al-Nahda Hospital, Muscat, Oman and Dr. Milind Killedar, pediatric ophthalmologist from Sangli, India. The final version was in concurrence of the authors with Dr. G. V. Rao, Rishi Raj Bora, Dr.Lutful Hussain (all from ORBIS India, Bangladesh) and Dr. A. H. Mahadik (from Lions NAB Eye Hospital, Miraj). Faiz Mushrif and Poonam Shinde helped in data collection; Shrivallabh Sane of Data Clinic in data analysis. We thank Dr. Mukesh Pariyani for helping with the vision function questionnaire, Dr. Bageshri Gogate, Madhuri Gogate, Dr. Meena Kharat and Shital Ghorpade for translating, back translating and validating it.
Appendix A. L.V.Prasad Child Vision Function Questionnaire
Name of Child:
Responses for each item rated on a 5-pointLikert scale.
0 = No difficulty
1 = Little difficulty (25%, char anna)
2 = Some difficulty (50%, aathanna)
3 = Great difficulty (75%, baraanna)
4 = Unable to perform the task due to visual reasons (100%, rupayya)
9 = Not applicable
-
Do you have any difficulty in making out whether the personyou are seeing across the read is a boy or a girl, during the day?
0 1 2 3 4
-
Do you have any difficulty in seeing whether somebody is callingyou by waving his or her hand from across the road?
0 1 2 3 4
-
Do youhave difficulty in walking alone in the corridor at schoolwithoutbumping into objects or people?
0 1 2 3 4
-
Do you have any difficultyin walking home at night (from tuitionor a friend's house) without assistance when there arestreetlights?
0 1 2 3 4
-
Do you haveany difficulty in copying from the blackboard whilesittingon the first bench in your class?
0 1 2 3 4
-
Do you have difficulty inreading the bus numbers?
0 1 2 3 4
-
Do you have any difficulty in readingthe other details on thebus (such as its destination?)
0 1 2 3 4
-
Doyou have any difficulty in reading your textbooks at an arm'slength?
0 1 2 3 4
-
Do you have any difficulty in writing along a straightline?
0 1 2 3 4
-
Do you have any difficulty in finding the next linewhilereadingwhen you take a break and then resume reading?
0 1 2 3 4
-
Do you have any difficulty in locating dropped objects (pen, pencil, eraser) within the classroom?
0 1 2 3 4
-
Do you have any difficultyin threading a needle?
0 1 2 3 4
-
How much difficulty do you have indistinguishing between 1 rupee and 2 rupee coins (without touching)?
0 1 2 3 4
-
Do you have difficulty in climbing up or down stairs?
0 1 2 3 4
-
Doyou have difficulty in lacing your shoes?
0 1 2 3 4
-
Do have difficultyin locating a ball while playing in the daylight?
0 1 2 3 4
-
Do you havedifficulty in applying paste on your toothbrush?
0 1 2 3 4
-
Do you havedifficulty in locating food on your plate whileeating?
0 1 2 3 4
-
Doyou difficulty in identifying colors (e.g., while coloring)?
0 1 2 3 4
-
How do you think your vision is compared with that of yournormal-sightedfriend? Do you think your vision is: As goodas your friend's
0
-
A little bit worse than your friend's 1Much worse thanyour friend's
2
End of Questionnaire
The questionnaire was based on four parameters: Distance vision (Q 1,2,4,5,6,7), near vision (Q 8,9,10,12,13,15), colour vision (Q 17,19), field of vision (Q 3,11,14,16,18)
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gilbert C, Foster A. Childhood blindness in the context of VISION 2020: The right to sight. Bull World Health Organ. 2001;79:227–32. [PMC free article] [PubMed] [Google Scholar]
- 2.Gogate P, Muhit M. Childhood blindness and cataract in developing countries. J Community Eye Health. 2009;22:4–5. [PMC free article] [PubMed] [Google Scholar]
- 3.Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert C. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. doi: 10.1136/bjo.2006.094433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gogate P, Kishore H, Dole K, Shetty J, Gilbert C, Ranade S, et al. The pattern of childhood blindness in Karnataka, South India. Ophthalmic Epidemiol. 2009;16:212–7. doi: 10.3109/09286580902999405. [DOI] [PubMed] [Google Scholar]
- 5.Thakur J, Reddy H, Wilson ME, Jr, Paudyal G, Gurung R, Thapa S, et al. Pediatric cataract surgery in Nepal. J Cataract Refract Surg. 2004;30:1629–35. doi: 10.1016/j.jcrs.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 6.Khandekar R, Sudhan A, Jain BK, Shrivastav K, Sachan R. Pediatric cataract and surgery outcomes in Central India: A hospital based study. Indian J Med Sci. 2007;61:15–22. [PubMed] [Google Scholar]
- 7.Gogate P, Khandekar R, Srisimal M, Dole K, Taras S, Kulkarni S, et al. Cataracts with delayed presentation- Are they worth operating upon? OphthalmicEpidemiol. 2010;17:25–33. doi: 10.3109/09286580903450338. [DOI] [PubMed] [Google Scholar]
- 8.Ram J, Sukhija J, Thapa BR, Arya VK. Comparison of hospital versus rural eye camp based pediatric cataract surgery. Middle East Afr J Ophthalmol. 2012;19:141–6. doi: 10.4103/0974-9233.92131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilbert CE, Rahi JS, Quinn GE. Visual impairment and blindness in children. In: Johnson GJ, Weale R, Minassian DC, West SK, editors. The Epidemiology of Eye Disease. 2nd ed. London: Arnold; 2003. [Google Scholar]
- 10.Dahan E, Drusedau MU. Choice of lens and dioptric power in pediatricpseudophakia. JCataract Refract Surg. 1997;23:618–23. doi: 10.1016/s0886-3350(97)80043-0. [DOI] [PubMed] [Google Scholar]
- 11.Gogate P, Patil S, Kulkarni A, Mahadik A, Tamboli R, Mane R, et al. Barriers to follow-up for pediatric cataract surgery in Maharashtra, India. How regular follow-up is important for good outcome. Indian J Ophthalmol. 2013 doi: 10.4103/0301-4738.116465. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mwende J, Bronsard A, Mosha M, Bowman R, Geneau R, Courtright P. Delay in presentation to hospital for surgery for congenital and developmental cataract in Tanzania. Br J Ophthalmol. 2005;89:1478–82. doi: 10.1136/bjo.2005.074146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gothwal VK, Lovie-Kitchin JE, Nutheti R. The development of the LV Prasad-Functional Vision Questionnaire: A measure of functional vision performance of visually impaired children. Invest Ophthalmol Vis Sci. 2003;44:4131–9. doi: 10.1167/iovs.02-1238. [DOI] [PubMed] [Google Scholar]
- 14.Chak M, Wade A, Rahi JS British Congenital Cataract Interest Group. Long-term visual acuity and its predictors after surgery for congenital cataract: Findings of the British congenital cataract study. Invest Ophthalmol Vis Sci. 2006;47:4262–9. doi: 10.1167/iovs.05-1160. [DOI] [PubMed] [Google Scholar]
- 15.Ledoux DM, Trivedi RH, Wilson ME, Payne JF. Pediatric cataract extraction with IOL: Visual acuity outcome when measured at age 4 years and older. J AAPOS. 2007;11:218–24. doi: 10.1016/j.jaapos.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Wilson ME, Hennig A, Trivedi RH, Thomas BJ, Singh SK. Clinical characteristics and early postoperative outcomes of pediatric cataract surgery with IOL implantation from Lahan, Nepal. J PediatricOphthalmol Strabismus. 2011;48:286–91. doi: 10.3928/01913913-20100920-03. [DOI] [PubMed] [Google Scholar]
- 17.Yorston D, Wood M, Foster A. Results of cataract surgery in young children in east Africa. Br J Ophthalmol. 2001;85:267–71. doi: 10.1136/bjo.85.3.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bowman R, Karibu J, Negretti G, Wood M. Outcome of bilateral cataract surgery in Tanzanian children. Ophthalmology. 2007;114:2287–92. doi: 10.1016/j.ophtha.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 19.Congdon NG, Ruiz S, Suzuki M, Herrera V. Determinants of pediatric cataract program outcomes and follow up in a large series in Mexico. J Cataract Refract Surg. 2007;33:1775–80. doi: 10.1016/j.jcrs.2007.06.025. [DOI] [PubMed] [Google Scholar]
- 20.You C, Wu X, Zhang Y, Dai Y, Huang Y, Xie L. Visual impairment and delay in presentation for surgery in Chinese pediatric patients with cataract. Ophthalmology. 2011;118:17–23. doi: 10.1016/j.ophtha.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 21.Msukwa G, Ninguna M, Tumweisgye C, Shilo B, Courtright P, Lewallen S. Cataracts in children attending schools for the blind and resource centres in Eastern Africa. Ophthalmic Epidemiol. 2009;16:1009–12. doi: 10.1016/j.ophtha.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 22.Ram J, Brar GS, Kaushik S, Gupta A, Gupta A. Role of posterior capsulotomy with vitrectomy and intraocular lens design and material in reducing posterior capsule opacification after pediatric cataract surgery. J Cataract Refract Surg. 2003;29:1579–84. doi: 10.1016/s0886-3350(03)00231-1. [DOI] [PubMed] [Google Scholar]
- 23.Wilson ME, Trivedi RH, Bartholomew LR, Pershing S. Comparison of anterior vitrectorhexis and continuous curvilinear capsulorhexis in pediatric cataract and intraocular lens implantation surgery: A 10-year analysis. J AAPOS. 2007;11:443–6. doi: 10.1016/j.jaapos.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 24.Bhusal S, Ram J, Sukhija J, Pandey S, Kaushik SS. Comparison of the outcome of implantation of hydrophobic acrylic versus silicone intraocular lenses in pediatric cataract: prospective randomized study. Can J Ophthlamol. 2010;45:531–6. doi: 10.3129/i10-045. [DOI] [PubMed] [Google Scholar]
- 25.Trivedi RH, Wilson ME, Vasavada AR, Shah SK, Vasavada V, Vasavada VA. Visual axis opacification after cataract surgery and hydrophobic acrylic intraocular lens implantation in the first year of life. J Cataract Refract Surg. 2011;37:83–7. doi: 10.1016/j.jcrs.2010.07.036. [DOI] [PubMed] [Google Scholar]
- 26.Astle WF, Alewenah O, Ingram AD, Paszuk A. Surgical outcomes of primary foldable intra-ocular lens implantation in children: Understanding posterior capsular opacification and absence of glaucoma. J Cataract Refract Surg. 2009;35:1216–22. doi: 10.1016/j.jcrs.2009.02.028. [DOI] [PubMed] [Google Scholar]
- 27.Mandal A, Netland PA. Glaucoma in aphakia and pseudophakia after congenital cataract surgery. Indian J Ophthalmol. 2004;52:185–98. [PubMed] [Google Scholar]
- 28.Al-Dahmash S, Khan AO. Pediatricpseudophakic glaucoma following surgery for isolated childhood cataract. Ophthalmic Lasers Imaging. 2010;41:463–6. doi: 10.3928/15428877-20100525-01. [DOI] [PubMed] [Google Scholar]
- 29.Swamy BN, Billson F, Martin F, Donaldson C, Hing S, Jamieson R, et al. Secondary glaucoma after pediatric cataract surgery. Br J Ophthalmol. 2007;91:1627–30. doi: 10.1136/bjo.2007.117887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gogate P, Dole K, Ranade S, Deshpande M. Cost of pediatric cataract in Maharashtra, India. Int J Ophthalmol. 2010;10:1248–52. doi: 10.3980/j.issn.2222-3959.2010.02.22. [DOI] [PMC free article] [PubMed] [Google Scholar]


