Abstract
Purpose:
The purpose of this study is to evaluate the lateral rectus periosteal fixation and partial vertical rectus transpositioning (VRT) as treatment modalities to correct exotropic Duane retraction syndrome (Exo-DRS).
Materials and Methods:
Prospective interventional case study of cases of Exo-DRS with limitation of adduction. A total of 13 patients were subdivided into two groups. Six patients underwent only lateral rectus periosteal fixation (group A) and seven patients also underwent partial VRT (group B). Assessment involved prism bar cover test, abduction and adduction range, extent of binocular single visual field and exophthalmometry. These tests were repeated at 1 week, 1 month and 3 months post-operatively and data analyzed.
Results:
The pre-operative mean values and ranges were 26.2Δ (22-35) exotropia for group A and −21.3Δ (14-30) exotropia for group B. The post-operative mean and range was +0.6Δ esotropia (+20 to −8) for group A and 8Δ (−2 to −20) exotropia for group B. Mean grade of limitation of abduction changed from −3.8 to −3.6 versus −3.6 to −2.8 and mean grade of limitation of adduction changed from −1.9 to −0.7 versus −1.5 to −0.5 in the groups A and B respectively. Mean binocular single visual field changed from 14.7° to 23.3° in group A and 11.8° to 26.4° in the group B respectively.
Conclusion:
Lateral rectus periosteal fixation is an effective surgery to correct the exodeviation, anomalous head posture and improving adduction in Exo-DRS and partial VRT in addition is effective in improving abduction and binocular single visual fields.
Keywords: Exotropic Duane retraction syndrome, periosteal fixation, strabismus surgery, vertical rectus transposition
Several surgical options have been described to tackle the problems of exotropic Duane retraction syndrome (Exo-DRS) type II These have ranged from differential recession of both lateral and medial recti of the affected eye, Y splitting of the lateral rectus with or without recession and supramaximal recession of the lateral rectus.[1,2,3] While these procedures have corrected the exodeviation in the primary position with resultant correction of the head posture, the problem of co-contraction in adduction and subsequently the retraction and upshoot or downshoot of the globe persisted, even if diminished to some extent. Theoretically unless the misdirected innervation to lateral rectus is tackled effectively, the above mentioned procedures are but a partial or temporary reprieve as the lateral rectus recovers its ability to contract during adduction. Therefore, some authors have suggested doing a periosteal fixation or extirpation of the lateral rectus.[4,5] In addition, to improve the abduction forces the use of full thickness vertical rectus transpositioning (VRT), has also been suggested.[5] We prospectively evaluated the effect of periosteal fixation of the lateral rectus alone and periosteal fixation with the partial VRT (using just the temporal halves of vertical recti to reduce the risk of anterior segment ischemia) in Exo-DRS.
Materials and Methods
The study was approved by the Ethics Committee and the Institutional Review Board of our Institute. We included 13 patients of Exo-DRS in our study. We randomized the patients by simple draw of chits and assigned them into two groups, one treated with periosteal fixation of the lateral rectus alone (n = 6) and the other in which split VRT was done in addition to periosteal fixation of the lateral rectus, (n = 7). All the cases had no prior surgery done, except the case A1 who had supramaximal lateral rectus recession done in the right eye and periosteal fixation of the lateral rectus done in the left eye.
At the initial visit complete ocular motility workup was done for each patient including Prism bar cover test, nine gaze measurements as well as grading for underaction of abduction and adduction. This was graded on the scale of 0,−1 through−4, by two separate examiners and the mean of the two grades taken. The scale was; Full rotation upto the canthus: 0, slight limitation−1, half of the range from midline to canthus; −2, slight movement not upto halfway: −3, no movement from midline: −4. Extent of binocular single visual field, wherever measurable, was assessed by Lister's perimetry. Exophthalmometry measurements were recorded using Hertel's exophthalmometer. Patients were followed-up at 1 week, 1 month and 3 months post-operatively with the above parameters repeated at each visit.
Periosteal fixation of the lateral rectus of involved eye was done in all the patients of the two groups. Surgery was done by the same surgeon (PS). Surgical steps were as follows.
Under general or local anesthesia, passive forced duction test was performed. Two 4-0 cotton sutures were placed at the limbal area. A limbal conjunctival incision was fashioned and the lateral rectus was dissected from the surrounding intermuscular membrane and Tenon's capsule and isolated on a muscle hook. The insertion of the rectus muscle was sutured by non-absorbable 5-0 Ethibond sutures and detached from the globe using Westcott scissors. The adjacent periosteum, approximately 5 mm posterior to the orbital rim, was exposed lateral to the lateral rectus after applying an epinephrine soaked swab stick. The lateral rectus muscle was fixed by a periosteal bite to the orbital wall. The cut edges of the intermuscular membrane were sutured together over the sclera with 8-0 polyglactin 910 sutures to avoid adherence of the muscle to the sclera. The conjunctival incision was closed by interrupted 8-0 vicryl sutures and recessed if the conjunctiva was found to be short.
In the group B of Duane retraction syndrome, partial VRT was done in addition to lateral rectus periosteal fixation. The surgery was performed as mentioned below.
The same lateral limbal conjunctival incision was used. Superior and inferior rectus muscles were cleaned carefully and isolated from surroundings. The lateral one half of each vertical muscle was separated from the nasal portion with a split from the insertion to 9.0 mm posteriorly. Care was taken to preserve the nasal anterior ciliary vessel in each remaining portion. One single double-armed 6-0 polyglactin 910 Suture was woven through the lateral portion on the vertical rectus muscles and then the muscle was disinserted for transposition and reattachment to the corresponding superior or inferior border of the lateral rectus 7 mm from the limbus at the original insertion of the lateral rectus. Intraoperative ductions were done to avoid leaving any restriction of movement or any obvious vertical incomitance.
Observations
The pre-operative and post-operative parameters of the two groups A and B are shown in Tables 1 and 2 respectively in our study, among 13 Exo-DRS subjects, 7 had left eye involvement, 4 bilateral and two right eye involvement. 6 were females and 7 males. The 6 cases of group A included 3 cases of unilateral left eye, 1 right eye and 2 cases of bilateral Duane syndrome. Among bilateral cases case A1 underwent lateral rectus recession in the right eye and periosteal fixation of the lateral rectus in the left eye while the other case had periosteal fixation of the lateral rectus in each eye. The 7 cases of group B included 4 left, 1 right sided and 2 bilateral case. The bilateral cases had the same surgery done on each side.
Table 1.
Pre-operative and post-operative parameters of group A of Exo-DRS operated by LR periosteal fixation alone
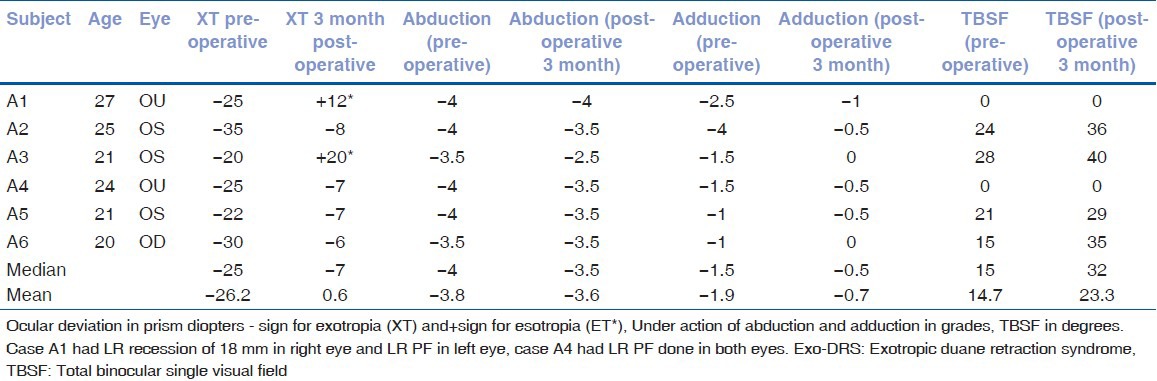
Table 2.
Pre-operative and post-operative parameters of group B of Exo-DRS operated by LR periosteal fixation and partial VRT
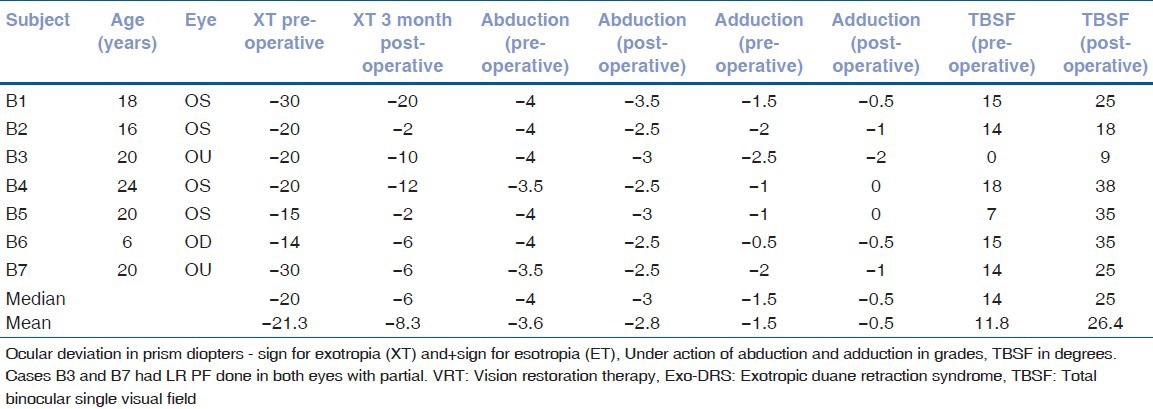
We assessed the outcome of surgery in terms of ocular alignment in primary gaze as well as improvement in limitation of adduction and abduction and the binocular fields of fixation. The pre-operative mean values and ranges were 26.2Δ (22-35) exotropia for group A and 21.3Δ (14-30) exotropia for group B The post-operative mean and the range was +0.6Δ esotropia (+20Δ to −8Δ) for group A (Note that two cases had esotropia of 12Δ and 20Δ) and 8.3Δ exotropia (−2 to −20) for group B (Note that none of the cases had esotropia). Median change of exotropia was from 25Δ to 7Δ in group A and from 20Δ to 6Δ in patients who underwent partial VRT. The pre-operative and post-operative deviations in the three horizontal gazes are shown in Figs. 1 and 2.
Figure 1.

Case A6: Right exotropic Duane retraction syndrome before (top) and after (bottom) right lateral rectus periosteal fixation showing the correction of exotropia, improvement in adduction and better retraction control
Figure 2.

Case B2: Left exotropic Duane retraction syndrome before (top) and after (bottom) left lateral rectus periosteal fixation and partial Vertical Rectus Transposition showing the correction of exotropia, improvement in adduction and also abduction and better retraction control
Abduction and adduction improved significantly in both groups. For abduction in group 1 the mean abduction changed from −3.8 to −3.6 P = 0.007 (median changed from−4 to−3.5) and mean adduction changed from−1.9 to−0.7, P = 0.002 (median changed from −1.5 to −0.5). In group 2, the mean abduction changed from −3.6 to −2.8 P = 0.001 (median changed from−4 to−3) and mean adduction changed from −1.5 to −0.7 (median changed from−1.5 to−0.5) P = 0.001. The improvement in abduction was better in group having undergone partial VRT.
Total binocular single visual field also improved significantly in both groups of Exo-DRS. In group 1 the mean binocular single visual field changed from 14.7° to 23.3° (median changed from 15° to 32°). In group 2, the Mean binocular single visual field changed from 11.8° to 26.4° (median changed from 14° to 25°.
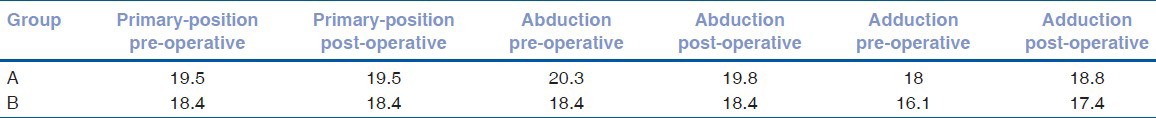
The mean exophthalmometry (Hertel) in the primary position, abduction and adduction before and after 3 months of surgery for groups A and B are shown in Table 3. A change of about 1 mm was seen in the adduction in both groups.
Table 3.
Mean exophthalmometry (Hertel) in different gazes pre-operative and post-operative in the two groups
Discussion
The average correction of exotropia in our cases at 3 months post-operation was 72% and 70% of the pre-operative XT for periosteal fixation of the lateral rectus alone (group A) and for periosteal fixation with partial VRT (group B) respectively. Kubota et al.[6] reported satisfactory ocular alignment (considered up to 12Δ XT) in 119 of the 124 cases (89%) of Duane syndrome, including 40 of 48 (83.3%) of Exo-DRS cases. A retrospective case series by Barbe et al.[7] which included 8 unilateral and 3 bilateral Exo-DRS subjects to evaluate unilateral or bilateral lateral rectus recessions, described a mean correction of exotropia from 16Δ to 6.25Δ in unilateral cases, while in bilateral cases, it changed from the mean value 32Δ exotropia pre-operative to 11.6Δ exotropia post-operatively. Among the three bilateral cases 1 required resurgery. The difficulty in the surgical treatment of Duane's Type II patients with exotropia has been well recognized. A case series of five patients of Exo-DRS in whom lateral rectus recession with Y-split was done showed a change from the mean value 16Δ of exotropia pre-operatively to small residual exotropia. In one patient, medial rectus recession 5 mm was also done[8] for the consecutive esotropia. In our cases, we had consecutive esotropia in 2 of the 6 cases with periosteal fixation, while none of the 7 cases with additional partial VRT had consecutive esotropia. This residual exotropia in the 4 cases of group A could be due to other exotropic forces in the orbit or some indirect action of the lateral rectus, though the post-operative forced duction test was negative in all cases. The partial VRT group however had better control and this could be more predictable if this was done on adjustable sutures as we have subsequently started to do.
Patients of Exo-DRS included in our study had significant pre-operative globe retraction, upshoot and/or downshoot, which significantly improved after periosteal fixation of the lateral rectus in all the 13 cases except one of the cases which had partial improvement. This can be attributed to the perisoteal fixation, which eliminates the abnormal innervations of the lateral rectus during adduction causing co-contraction. This is evident in case 1 of group 1 in which the right eye underwent a lateral rectus recession of 18 mm and still had retraction and limited adduction, whereas the left eye which had periosteal fixation done had better adduction and no significant retraction [Fig. 3]. This is because even after the supramaximal recession of the lateral rectus, it still retains enough co-contraction to prevent adduction and cause retraction. Andalib and Javadzadeh[9] reported a 7-year-old left Exo-DRS subject with 30Δ XT operated previously by lateral rectus recession who after lateral rectus periosteal fixation was aligned to 6Δ exotropia at 1 year follow-up, with a marked decrease in globe retraction and upshoot. They concluded that even a large recession of the lateral rectus could not eliminate the anomalous eye movement and suggested inactivating the muscle to decrease or eliminate the mechanical effects of the aberrant innervations. Jampolsky has highlighted the “contracture propensity” of the misinnervated lateral rectus and the surgeons’ tendency to under correct and have recurrence or residual Exo-DRS.[10]
Figure 3.
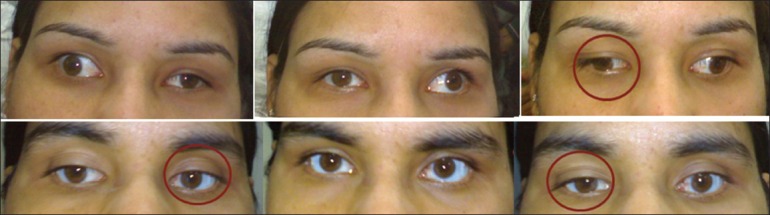
Case A1: Bilateral exotropic Duane retraction syndrome after right lateral rectus supramaximal recession done (top) same after (bottom) left lateral rectus periosteal fixation showing the better retraction control after the latter surgery
Limited or minimal abduction has been observed consistently in most of the cases of DRS. Partial or full thickness VRT was first described by Gobin.[11] This was reported successfully by several surgeons.[12,13,14] However, the problem of worsening of the retraction was also observed. The full thickness vertical rectus muscle transpositions that had been used to increase abduction strength in Duane syndrome resulted in worsening co-contraction in the presence of an aberrantly acting lateral rectus. A precautionary note was aired that vertical rectus transpositoning should only be done once the anomalous innervations of the lateral rectus had been confirmed to be absent by electromyography.[15] Or we may say that a prerequisite to VRT should be the elimination of misinnervation of the lateral rectus by a procedure like periosteal fixation.
A retrospective review of five patients including 1 with Exo-DRS and 4 with third nerve palsy in whom lateral rectus periosteal fixation was done, showed that stable and satisfactory ocular alignment was achieved post-operatively.[16] In this case of Duane syndrome patient, partial vertical rectus transpositoning and medial rectus resection was also done as he had previously undergone large lateral rectus recession and had come with 15Δ exotropia. However, we would like to suggest that the resection of the medial rectus is unwarranted and the adduction improves significantly just by being relieved of the co-contraction of the anomalous lateral rectus. Resections of horizontal muscles of the involved eye should be avoided because the effect of this procedure is unpredictable and because of the underlying innervational abnormality, the co-contraction would become more evident.
Parsa[17] found in their case series of three cases of different phenotypic forms of Duane retraction syndrome that lateral rectus periosteal fixation accompanied by full tendon VRT using ciliary vessel sparing technique resulted in marked improvement in globe retraction, upshoot and downshoot which was stable until 3 years of follow-up. Anterior segment ischemia has also been reported after full width vertical rectus muscle transposition procedures in Duane syndrome as the horizontal recti are also operated upon.[18] Hummelscheim introduced partial width rectus muscle transposition, a procedure with advantage to allow surgery on multiple ipsilateral rectus muscles without risk of anterior segment ischemia. We preferred to rely on the partial sparing of the half muscle to scaffold its anterior ciliary vessels rather than the vessel sparing technique, where a possibility of the stretched unsupported vessels to collapse or shrink in the long run exists.
To conclude the paradoxic innervation of lateral rectus during adduction can be effectively eliminated by periosteal fixation. This improves the exodeviation in primary position and thus the anomalous head posture, as well as the adduction range. The abduction can be improved by doing partial vertical rectus transpositoning after periosteal fixation of lateral rectus.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Sprunger DT. Recession of both horizontal rectus muscles in Duane syndrome with globe retraction in primary position. J AAPOS. 1997;1:31–3. doi: 10.1016/s1091-8531(97)90020-3. [DOI] [PubMed] [Google Scholar]
- 2.Jampolsky A. A new surgical procedure for upshoots and downshoots in Duane syndrome: The Y-splitting of the lateral rectus as cited by Jampolsky A, Duane syndrome. In: Rosenbaum AL, Santiago AP, editors. Clinical Strabismus Management. Philadelphia: WB Saunders; 1999. pp. 325–46. [Google Scholar]
- 3.Freedman HL, Kushner BJ. Congenital ocular aberrant innervation–New concepts. J Pediatr Ophthalmol Strabismus. 1997;34:10–6. doi: 10.3928/0191-3913-19970101-04. [DOI] [PubMed] [Google Scholar]
- 4.Carlson MR, Jampolsky A. An adjustable transposition procedure for abduction deficiences. Am J Ophthalmol. 1979;87:382–7. doi: 10.1016/0002-9394(79)90081-3. [DOI] [PubMed] [Google Scholar]
- 5.Velez FG, Thacker N, Britt MT, Alcorn D, Foster RS, Rosenbaum AL. Rectus muscle orbital wall fixation: A reversible profound weakening procedure. J AAPOS. 2004;8:473–80. doi: 10.1016/j.jaapos.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Kubota N, Takahashi H, Hayashi T, Sakaue T, Maruo T. Outcome of surgery in 124 cases of Duane's retraction syndrome (DRS) treated by intraoperatively graduated recession of the medial rectus for esotropic DRS, and of the lateral rectus for exotropic DRS. Binocul Vis Strabismus Q. 2001;16:15–22. [PubMed] [Google Scholar]
- 7.Barbe ME, Scott WE, Kutschke PJ. A simplified approach to the treatment of Duane›s syndrome. Br J Ophthalmol. 2004;88:131–8. doi: 10.1136/bjo.88.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rao VB, Helveston EM, Sahare P. Treatment of upshoot and downshoot in Duane syndrome by recession and Y-splitting of the lateral rectus muscle. J AAPOS. 2003;7:389–95. doi: 10.1016/s1091-8531(03)00213-1. [DOI] [PubMed] [Google Scholar]
- 9.Andalib D, Javadzadeh A. Lateral rectus muscle disinsertion and reattachment to the lateral orbital wall in exotropic Duane syndrome: A case report. J Med Case Rep. 2008;2:253. doi: 10.1186/1752-1947-2-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jampolsky A. A functional classification of retraction syndromes: The 19 th Jules Stein lecture: As cited by Jampolsky A, Duane syndrome. In: Rosenbaum AL, Santiago AP, editors. Clinical Strabismus Management. Philadelphia: WB Saunders; 1999. pp. 325–46. [Google Scholar]
- 11.Gobin MH. Surgical management of Duane's syndrome. Br J Ophthalmol. 1974;58:301–6. doi: 10.1136/bjo.58.3.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Velez FG, Foster RS, Rosenbaum AL. Vertical rectus muscle augmented transposition in Duane syndrome. J AAPOS. 2001;5:105–13. doi: 10.1067/mpa.2001.112677. [DOI] [PubMed] [Google Scholar]
- 13.Molarte AB, Rosenbaum AL. Vertical rectus muscle transposition surgery for Duane's syndrome. J Pediatr Ophthalmol Strabismus. 1990;27:171–7. doi: 10.3928/0191-3913-19900701-03. [DOI] [PubMed] [Google Scholar]
- 14.Britt MT, Velez FG, Velez G, Rosenbaum AL. Vertical rectus muscle transposition for bilateral Duane syndrome. J AAPOS. 2005;9:416–21. doi: 10.1016/j.jaapos.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 15.Souza-Dias C. Congenital VI nerve palsy is Duane syndrome until disproven. Binocul Vis Strabismus Q. 1992;7:70. [Google Scholar]
- 16.Morad Y, Kowal L, Scott AB. Lateral rectus muscle disinsertion and reattachment to the lateral orbital wall. Br J Ophthalmol. 2005;89:983–5. doi: 10.1136/bjo.2004.051219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parsa CF. A practical and theoretically optimal surgical approach to Duane syndrome. In: de Faber JT, editor. Rio de Janeiro, Brazil: Strabismus 2006; Proceedings of the Joint Congress of the International Strabismological Association, ISA and the First Extraordinary Meeting of the Latin American Council of Strabismus, CLADE. Cultura Medica; 2006. pp. 315–20. [Google Scholar]
- 18.Saunders RA, Sandall GS. Anterior segment ischemia syndrome following rectus muscle transposition. Am J Ophthalmol. 1982;93:34–8. doi: 10.1016/0002-9394(82)90695-x. [DOI] [PubMed] [Google Scholar]


