Abstract
Acute thyroiditis is an extremely rare complication of nocardiosis. We report a patient with hyperthyroidism due to suppurative thyroiditis caused by Nocardia brasiliensis. A 38-year-old Black male presented with features of thyrotoxicosis, sepsis and airway obstruction. He had no evidence of underlying thyroid disease, but was severely immunocompromised as a result of acquired immunodeficiency syndrome. He had previously been diagnosed with pulmonary nocardiosis and also had nocardial abscesses on his anterior chest wall. Investigations revealed thyrotoxicosis, with a FT4 of 43.2 pmol/l and a suppressed TSH <0.01 mIU/l. Serum anti-thyroperoxidase and anti-thyroglobulin antibodies were absent. Computed tomography scan showed a large abscess in the anterior neck involving the left lobe and isthmus, as well as inhomogeneous changes in the right lobe of the thyroid. The radioisotopic scan showed absent uptake of tracer in keeping with thyroiditis. Although the initial presentation was that of hyperthyroidism, destruction of the gland later resulted in sustained hypothyroidism, necessitating thyroid hormone supplementation. The hyperthyroidism can be explained by the release of presynthesized and stored thyroid hormone into the circulation as a result of inflammation and disruption of the thyroid follicles, and the subsequent hypothyroidism by the fact that much of the gland was destroyed by the abscess and the extensive inflammatory process. This is the first documented case of hyperthyroidism in a patient with acute suppurative thyroiditis caused by Nocardia.
Key Words : Suppurative thyroiditis, Nocardiosis, Hyperthyroidism, Human immunodeficiency virus, Acquired immunodeficiency syndrome
What Is Known about This Topic
• Acute suppurative thyroiditis due to nocardiosis is extremely rare, with only 8 cases caused by Nocardia asteroidies or Nocardia farcinica having been reported. The only thyroid hormone abnormality documented prior to this report was subclinical hypothyroidism in 1 patient.
What This Case Report Adds
• This is the first documented case of acute suppurative thyroiditis due to Nocardia presenting with hyperthyroidism which, in addition, was followed by persistent hypothyroidism as a result of extensive gland destruction. This is also the first report of Nocardia thyroiditis caused by the species Nocardia brasiliensis.
Introduction
Acute suppurative thyroiditis is rare, being far less common than the non-suppurative post-viral variety, de Quervain's disease. It occurs mainly in immunocompromised and elderly patients [1]. Possible reasons for the infrequency of suppurative infections of the thyroid include the gland's abundant blood supply and lymphatic drainage, and the antimicrobial action of iodine [2]. Most patients have a preexistent thyroid disorder, especially multinodular goiter [1,2,3]. Most infections are bacterial, but opportunistic infections also occur. Typically, patients are acutely ill with fever, dysphagia, and a tender thyroid mass, but presentation may be insidious in patients with opportunistic infections [1]. Management includes the administration of appropriate antibiotics and drainage of any abscesses [1,2].
Nocardia are aerobic, branching, filamentous, Gram-positive actinomycetes. Human nocardiosis occurs most commonly in immunocompromised hosts including acquired immunodeficiency syndrome (AIDS) [4]. The most frequent route of entry for Nocardia is the respiratory tract. Most organs can be affected [4,5]. Infection due to Nocardia brasiliensis occurs less frequently than that caused by Nocardia asteroides, and commonly affects skin and soft tissue [5,6]. Hematogenous seeding leading to disseminated disease is uncommon [6]. Therapy requires prolonged antibiotic administration, together with surgical intervention when indicated [4].
Thyroiditis caused by Nocardia is extremely rare and only 8 cases have been described in the literature [5,7,8,9,10,11,12,13]. Of these, N. asteroides was cultured in 7 cases and N. farcinica in 1 case. Most of the reports made no mention of abnormal thyroid function at the time of presentation. Subclinical hypothyroidism developed in only 1 patient after 12 weeks [8]. Outcomes were poor and half of the patients demised [7,10,11,12].
Case Report
A 38-year-old Black male presented to Chris Hani Baragwanath Academic Hospital with a 3-day history of a rapidly enlarging neck mass, dysphagia, dysphonia, and difficulty breathing. He complained of recent-onset diarrhea, significant weight loss, productive cough and night sweats. He had been managed by the hospital for AIDS as well as pulmonary nocardiosis. Non-compliance with medication had resulted in persistently low CD4 counts and a high viral load. The Nocardia infection had not improved despite the prescription of prolonged courses of appropriately selected antibiotics to which the organism was sensitive.
Physical examination revealed a wasted, pale, pyrexial patient with a hoarse voice and labored respiration. He had florid oropharyngeal candidiasis. A large, tender, fluctuant mass was noted on the left anterior aspect of his neck with overlying induration of the skin and displacement of the trachea to the right. There were bilateral crackles on auscultation of his chest. Two large abscesses on the upper aspect of his anterior chest wall were draining pus. The patient had a fine tremor and displayed generalized weakness, most pronounced in the proximal limb musculature.
Initial testing revealed a free thyroxine (FT4) of 43.2 pmol/l (normal 12.0-22.0), a suppressed TSH <0.01 mIU/l (normal 0.27-4.20) and a free triiodothyronine (FT3) of 3.1 pmol/l (normal 2.8-7.1). Serum anti-thyroperoxidase and anti-thyroglobulin antibodies were negative. Inflammatory markers were elevated with a leukocytosis of 13.7 × 109/l and a C-reactive protein of 179.9 mg/l. CD4 count was 142 cells/µl and viral load, 69,064 RNA copies/ml.
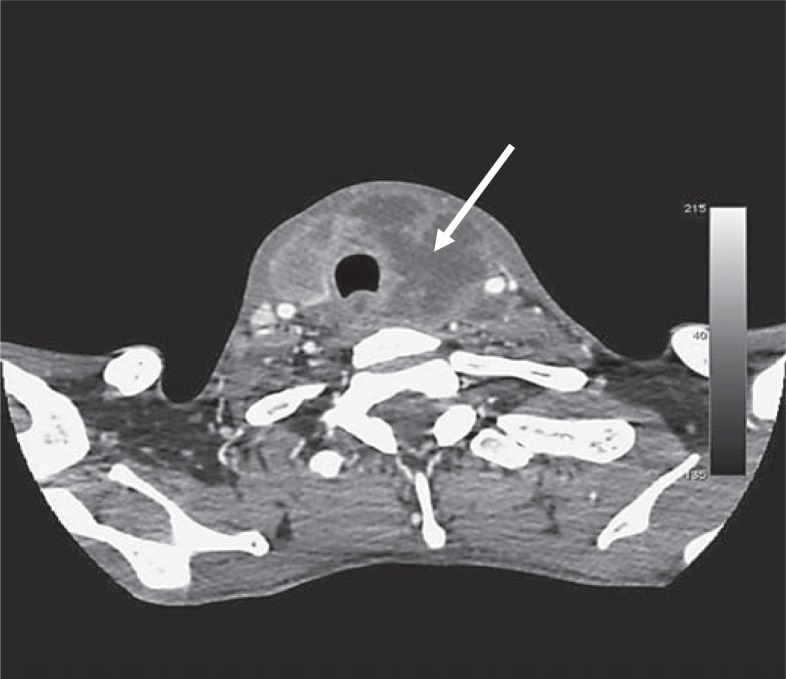
The patient's chest radiograph showed bilateral infiltrates. Ultrasound revealed a large abscess in the anterior neck, shown by computed tomography to involve the left lobe and isthmus of the thyroid (fig. 1). The right lobe showed inhomogeneous changes. A technetium thyroid scan showed absent tracer uptake, in keeping with thyroiditis.
Fig. 1.
Computed tomography scan of the patient's neck showing a large rim-enhancing collection (45 × 45 × 52 mm) in the left lobe and isthmus of the thyroid (arrow). The abscess extended around the trachea, compressing the esophagus. The right lobe showed an inhomogeneous pattern. There were significant paratracheal and jugular lymph nodes.
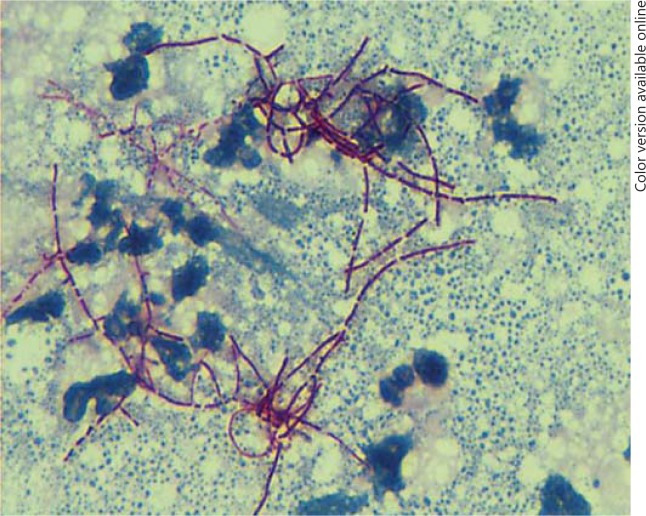
Aspiration of the abscess yielded purulent material, microscopy of which displayed branching filamentous Gram-positive organisms (fig. 2). N. brasiliensis was subsequently cultured and demonstrated extensive antibiotic resistance. Blood cultures and sputum microscopy and culture yielded no organisms. Tests for active tuberculosis were negative.
Fig. 2.
Smear of abscess aspirate showing Nocardia species. Note the branching filamentous Gram-positive organisms. Kinyoun stain. ×100.
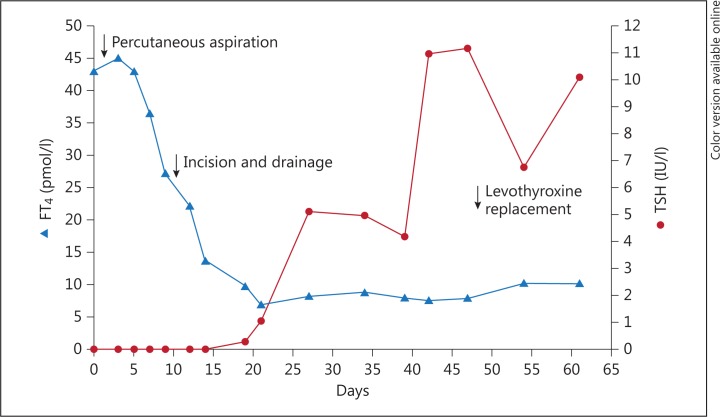
The patient was treated with targeted intravenous antibiotics. Aspiration of the abscess was followed by surgical drainage on the tenth hospital day, and the hyperthyroidism progressively abated. By day 19, the FT4 had fallen to subnormal levels and was followed by a gradual rise in TSH levels. Hypothyroidism persisted and levothyroxine replacement was commenced on day 48 post-admission (fig. 3).
Fig. 3.
FT4 and TSH levels from admission (day 0) to day 61. Levothyroxine replacement therapy was commenced on day 48.
Discussion
This is the first documented case of hyperthyroidism in a patient with acute suppurative thyroiditis caused by N. brasiliensis. Our patient had no evidence of underlying thyroid disease, but was immunocompromised as a result of AIDS. Hyperthyroidism in an AIDS patient can be attributed to a number of processes including Graves' disease in the setting of the immune reconstitution syndrome, various antiretroviral drugs and complicating infections, such as cytomegalovirus. The absence of tracer uptake on the scan, his non-compliance with antiretroviral treatment, the presence of Nocardia cultured from thyroid abscess, and the absence of any other organism on culture all support the diagnosis of Nocardia thyroiditis in our patient.
While the initial presentation was that of hyperthyroidism, destruction of the gland subsequently resulted in hypothyroidism, requiring thyroxine supplementation. The majority of patients presenting with suppurative thyroiditis have normal thyroid functions in the absence of preexistent thyroid disease, but both hypothyroidism and hyperthyroidism have been reported [1,2]. The mechanism of hyperthyroidism is probably similar to that occurring in subacute thyroiditis, in which presynthesized stored thyroid hormone is released into the circulation as a result of inflammation and disruption of the thyroid follicles [14]. Even when only part of the gland is affected, radioactive iodine uptake may be suppressed due, in part at least, to the inhibition of TSH secretion by the elevated circulating thyroid hormone [15]. As in our patient, the predominant hormone elevated is T4. The normal T3 levels are likely due to the effects of non-thyroidal illness on type 1 deiodinase (i.e. sick hyperthyroid). Following abscess drainage and resolution of the inflammation, the FT4 level fell below normal and persisted without recovery, in contrast to the usual situation in non-suppurative de Quervain's thyroiditis. The reason for the failure to return to the euthyroid state in our patient can be explained by the fact that much of the thyroid gland was destroyed by the large abscess and the surrounding severe inflammatory process.
Disclosure Statement
The authors have no conflicts of interest to disclose.
Acknowledgements
The authors thank Dr. Sharona Seetharam, Department of Microbiology, and Dr. Stephen Mphomane, Department of Radiology, Chris Hani Baragwanath Academic Hospital for their assistance.
References
- 1.Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003;348:2646–2655. doi: 10.1056/NEJMra021194. [DOI] [PubMed] [Google Scholar]
- 2.Berger SA, Zonszein J, Villamena P, Mittman N. Infectious diseases of the thyroid gland. Rev Infect Dis. 1983;5:108–122. doi: 10.1093/clinids/5.1.108. [DOI] [PubMed] [Google Scholar]
- 3.Farwell AP, Braverman LE. Inflammatory thyroid disorders. Otolaryngol Clin North Am. 1996;4:541–556. [PubMed] [Google Scholar]
- 4.Lerner PI. Nocardiosis. Clin Infect Dis. 1996;22:891–903. doi: 10.1093/clinids/22.6.891. quiz 904-905. [DOI] [PubMed] [Google Scholar]
- 5.Vandôme A, Pageaux GP, Bismuth M, Fabre JM, Domergue J, Perez C, Makeieff M, Mourad G, Larrey D. Nocardiosis revealed by thyroid abscess in a liver-kidney transplant recipient. Transpl Int. 2001;14:202–204. doi: 10.1007/s001470100308. [DOI] [PubMed] [Google Scholar]
- 6.Smego RA, Gallis HA. The clinical spectrum of Nocardia brasiliensis infection in the United States. Rev Infect Dis. 1984;6:164–180. doi: 10.1093/clinids/6.2.164. [DOI] [PubMed] [Google Scholar]
- 7.Balikian JP, Herman PG, Kopit S. Pulmonary nocardiosis. Radiology. 1978;126:569–573. doi: 10.1148/126.3.569. [DOI] [PubMed] [Google Scholar]
- 8.Lewin SR, Street AC, Snider J. Suppurative thyroiditis due to Nocardia asteroides. J Infect. 1993;26:339–340. doi: 10.1016/0163-4453(93)95937-e. [DOI] [PubMed] [Google Scholar]
- 9.Carriere C, Marchandin H, Andrieu JM, Vandome A, Perez C. Nocardia thyroiditis: unusual location of infection. J Clin Microbiol. 1999;37:2323–2325. doi: 10.1128/jcm.37.7.2323-2325.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leong KP, Tee NWS, Yap WM, Chee TS, Koh ET. Nocardiosis in patients with systemic lupus erythematosus. J Rheumatol. 2000;27:1306–1312. [PubMed] [Google Scholar]
- 11.Severo CB, Oliveira FM, Cunha L, Cantarelli V, Severo LC. Disseminated nocardiosis due to Nocardia farcinica: diagnosis by thyroid abscess culture. Rev Inst Med Trop Sao Paulo. 2005;47:355–358. doi: 10.1590/s0036-46652005000600009. [DOI] [PubMed] [Google Scholar]
- 12.Indumathi VA, Shivakumar NS. Disseminated nocardiosis in an elderly patient presenting with prolonged pyrexia: diagnosis by thyroid abscess culture. Indian J Med Microbiol. 2007;25:294–296. doi: 10.4103/0255-0857.34781. [DOI] [PubMed] [Google Scholar]
- 13.Su B, Ko W, Chuang Y, Tang HJ. Disseminated nocardiosis with thyroid involvement: a case report. J Microbiol Immunol Infect. 2011;44:238–240. doi: 10.1016/j.jmii.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 14.Nieuwland Y, Tan KY, Elte JWF. Miliary tuberculosis presenting with thyrotoxicosis. Postgrad Med J. 1992;68:677–679. doi: 10.1136/pgmj.68.802.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewitus Z, Rechnic J, Lubin E. Sequential scanning of the thyroid as an aid in the diagnosis of subacute thyroiditis. Isr J Med Sci. 1967;3:847–854. [PubMed] [Google Scholar]