Abstract
The provision of comprehensive cancer care in an increasingly complex landscape necessitates that oncology providers familiarize themselves with the application of palliative care. Palliative care is a learnable skill. Recent endeavors in this arena have demonstrated that providing palliative care is part and parcel with providing compassionate and high-quality cancer care, specifically as it pertains to physical and emotional outcomes for patients and their caregivers alike. The basic tenets of providing palliative care emphasize: frequent and honest communication, routine and systematic symptom assessment, integration of spiritual assessments, and early integration of specialized hospice and palliative care resources as a patient’s circumstances evolve. This article will endeavor to review and synthesize recent developments in the palliative care literature, specifically as they pertain to the oncologist as a primary palliative care provider.
Keywords: Palliative care, end of life care, hospice care, advance care planning, prognostication
Oncologists are increasingly faced with the challenge of providing comprehensive care to patients in an evolving landscape. Of all patients diagnosed with metastatic cancer, current treatment will permit nearly half to continue living for a period of years after their initial diagnosis.1 We must use our growing arsenal to provide personalized,2 compassionate, and cost-effective care that translates into better outcomes and quality of life (QOL) for our patients.
Palliative care, which is a distinct medical specialty that is often included within the continuum of comprehensive cancer care, is “specialized medical care for people with serious illnesses, focused on providing patients with relief from the symptoms, pain, and stress of a serious illness”—whatever the diagnosis and regardless of the prognosis.3 “The goal is to improve quality of life for both patient and family.”3 This must necessarily be distinguished from end of life or hospice care. Medicare defines the latter as “care of patients with a physician-estimated life expectancy of 6 months or less.”4
Palliative care is part of best practice in oncology, as endorsed by the American Society of Clinical Oncology (ASCO), European Society for Medical Oncology, the National Comprehensive Cancer Network (NCCN), and the Society for Surgical Oncology.1,5 Many oncologists agree that integrating palliative care at the time of an advanced cancer diagnosis enhances patient care and complements their practice.6 However, although most oncologists believe that they already practice palliative care, recent studies suggest that our performance in this regard is in need of significant improvement.7,8
What Kinds of Palliative Care Exist?
Palliative care is a resource provided by a team of doctors, nurses, and other specialists who are (or work along with) the patient’s longitudinal care providers to provide an added layer of support. As such, palliative care can be meaningfully used at any stage of a serious illness—including circumstances where it is provided concomitantly with curative therapy. Primary palliative care9 is provided on a regular basis by the longitudinal oncologist and care team. Secondary palliative care is provided by teams of individuals with dedicated expertise in this discipline. This resource can be provided either in outpatient programs or in an inpatient unit. Tertiary palliative care is provided by specialized teams of providers with advanced expertise in the management of symptoms and pain, including but not limited to implantable drug delivery systems, palliative sedation, and management of advanced delirium. This article will emphasize the rationale behind and methods/resources for providing quality primary palliative care for the medical oncologist.
What Is the Best Model?
We do not know what the core or essential elements of palliative care when provided alongside primary oncology care are, but there are good models. Capital Caring and Hospice has partnered with US Oncology to provide palliative care doctors and advance practice nurses in the private practice oncology office. This model was based on what services were reimbursable. Patient symptoms were reduced by 21%, with high provider satisfaction and remarkable time savings of almost 4 weeks for the practice by shifting symptom management to the palliative care provider.10 Similar models of “modified” palliative care have been successfully integrated into usual oncology practice at numerous other centers, including academic centers in the United States and Canada.11
Why Does Providing Palliative Care Matter?
In recent years, there has been a growing body of academic scholarship investigating the impact of early and/or integrated palliative care. Several of the recently published studies have offered more modern, consistent, comprehensive, and carefully controlled investigations of palliative care interventions. Improvements in QOL,12,13 symptoms,12–14 mood,12–14 patient satisfaction,15,16 caregiver burden,17 and completion of advance directives13,14,16 have been demonstrated. Decreased utilization of clinical and financial resources,13,15,16 decreased treatment toxicity,18 and improved survival have also been observed.13 We have listed some of the consistent findings in Table 1.
TABLE 1.
Outcomes From Randomized Trials of Palliative Care Performed in the Last 10 Years
| First Author, Year | Outcomes
|
||||||
|---|---|---|---|---|---|---|---|
| Symptoms | Quality of Life | Mood | Satisfaction | Resource Use | Advance Care Planning | Survival | |
| Bakitas et al. (2009),12 nurse-led intervention | Improved, P = 0.06 | Improved, P = 0.02 | Improved, P = 0.02 | Not measured | No difference | No difference | No difference |
| Brumley et al. (2007),15 team intervention | Not measured | Not measured | Not measured | Improved, P < 0.05 | Cost $7500 less, P = 0.03, hospital days reduced by 4.36 (P < 0.001) ED visits reduced by 0.35 (P = 0.02) | Not measured | No difference |
| Gade et al. (2008),16 team intervention | No difference | No difference | No difference | IPCS greater satisfaction with care (P = 0.04) and communication (P = 0.0004) | Costs $6766 less P < 0.001). Net cost savings of $4855 (P < 0.001); longer median hospice stays (24 vs 12 d, P = 0.04) | IPCS patients had more ADs at discharge than UC patients (91.1% vs 77.8%; P < 0.001) | No difference |
| Temel et al. (2010)13 | Improved, P = 0.04 | Improved, P = 0.03 | Less depression, P = 0.01 | Not measured | Less aggressive care, P = 0.05, $2200 per person savings | More ADs documented in PC group, P = 0.05 | 11.6 vs 8.9 mo, P = 0.02 |
ED indicates emergency department; IPCS, interdisciplinary palliative care service; UC, usual care; AD, advance directive; PC, palliative care.
Palliative care provided concomitantly with standard oncologic care in patients with advanced cancer results in noninferior—and often superior—outcomes with regard to QOL, symptom relief, mood, patient satisfaction, advance care planning, and survival. This is despite the decreased intensity and use of medical and financial resources at the end of life in patients receiving palliative care. Moreover, no studies have demonstrated harm associated with early or integrated palliative care. These findings have been validated in several recently published systematic reviews of the palliative care literature.19–21
How Do I Provide Primary Palliative Care in the Oncology Office?
We have listed some of the most important parts of primary palliative care in Table 2.
TABLE 2.
Components of Office-Based Primary Oncology Palliative Care
|
Communicate Honestly and Effectively: Ask, Tell, Ask… and Listen
Honest and effective communication with cancer patients and their families regarding diagnosis, prognosis, and likely treatment outcomes and toxicities remains a central tenet in the oncology care continuum. Yet, even so, studies have shown that patients with advanced cancers commonly share an inaccurate perception of treatment effect, goals, and outcomes—often overestimating survival. In a recently published study by Weeks et al.,22 nearly 80% of patients with metastatic lung and colo-rectal cancer reported that chemotherapy was “very/somewhat/a little likely to be curative.” Patients with advanced-stage disease operating with a belief in a high likelihood of survival greater than 6 months were 2.6 times more likely to favor life-extending therapy over comfort measures—but without any improvement in survival.22 Physicians caring for such patients can be similarly challenged in their efforts to accurately prognosticate—and have been shown to overestimate prognosis by a factor of 5.23 Thus, providers, patients, and families with inaccurate perceptions of treatment outcomes may opt for therapies that incur significant risk with only modest potential for benefit.
Several prognostic scales have been developed for and validated in cancer patients to aid providers in having frank discussions about prognosis and treatment outcomes.24–26 Such efforts are important to patients and families and can contribute to better outcomes. Temel and colleagues27 have previously demonstrated that a better understanding of the incurable nature of their disease is associated with improved survival in lung cancer patients. This is possibly due to less use of ineffective and toxic fourth- and fifth-line chemotherapy. We have listed some helpful prognostic tools in Table 3.
TABLE 3.
Prognostic Tools Available to Oncologists
| Tool | Usefulness | Actions That Oncologists Can Take |
|---|---|---|
| Performance status (PS) | Decline in PS predicts worse response to chemotherapy and shortened survival | “Ask, tell, ask” about the level of information requested; advance care planning; hospice information visits |
| Clinical characteristics | Reliable predictors of survival <6 mo
|
With a few exceptions such as gastrointestinal stromal tumor (GIST) and human epidermal receptor (HER)-2 positive/amplified breast cancer, these always indicate mean survival of <6 mo and can lead to the actions above while pursuing treatment. |
| Palliative Performance Scale | Reliably predicts survival in days, weeks, or months with bedside observations | Available with interpretation at End of Life/Palliative Education Resource Center (EPERC) http://www.eperc.mcw.edu/EPERC/FastFactsIndex/ff_125.htm |
| Palliative prognostic score | Reliably predicts survival into 3 categories based on clinical observations, white count, and lymphocyte count | Available with interpretation at EPERC http://www.eperc.mcw.edu/EPERC/FastFactsIndex/ff_124.htm |
Such discussions should necessarily occur on a repeating basis.28 Poignant triggers for such conversations include when the disease progresses, when medical complications of the cancer occur, and when the performance status declines. We let the natural history of the disease prompt us to have these conversations (as shown in Figure 1). Emphasis should be placed on negotiating the content and pace of the discussion to best meet the patient and family’s needs, that is, ask, tell, then ask again. “How much would you like to know?” “What kind of information would be most useful to you?” We should always be sure to confirm comprehension. “Can you tell me what you are taking away from this discussion?”
FIGURE 1.
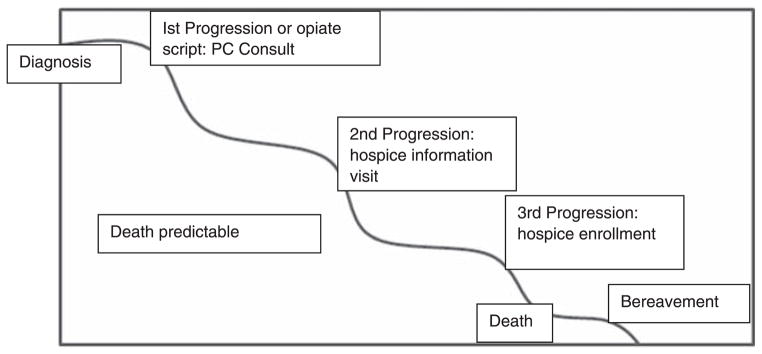
Using the natural history of advanced cancer to guide palliative care involvement.
Although such skills do not necessarily evolve with time and/or experience,29 they can be learned.30–37 In recent years, specific workshops and longitudinal programs such as Oncotalk have been developed and effectively implemented. After participation, providers were much more likely to use skills useful in discussing end-of-life issues and breaking bad news.30
These conversations are critically important, but we do not have them or document them often or well enough. In the most recent nationwide survey of lung cancer patients, only half had any mention of hospice 2 months before death—by any physician.38 Only 22% had a doctor tell them about impending death, and when it did occur (in many cases only a month before death), it was often not the primary oncologist who had the conversation.39 The data are clear that many oncologists prefer not to have these conversations until “there are no more treatment options left”40—when often, it is too late to plan.
We recommend the use of the decision aid and prompts from the ASCO lung cancer guideline,41 which gives the oncologist a script to use for advance care planning.
Assess Symptoms Consistently, Then Intervene
That patients with advanced cancer experience multiple concurrent symptoms has been well demonstrated in the literature.42 Several symptom assessment tools are currently in existence. What matters is not so much which tool is used, but that a tool is used consistently and the results documented. Their value is not simply in the 1-time assessment, but also in the evolution over time. Symptom assessment is more than just an evaluation of pain and performance status. Delirium, nausea (with or without vomiting), constipation, anorexia, insomnia/fatigue, anxiety, depression, and dyspnea are among the other considerations that significantly impact patients’ QOL. Such assessments not only facilitate meaningful therapeutic interventions, but may also assist in improving the accuracy of providers’ survival predictions. In multivariate analyses, confusion, anorexia, fatigue, cachexia, weight loss, dyspnea, and dysphagia all served as independent predictors of survival.43
We use a simple rounding tool available from the Center to Advance Palliative Care (Table 4) to assess for the most common symptoms.
TABLE 4.
The Memorial Symptom Assessment Scale Condensed Rounding Tool*
| Reported by: □ Patient □ Caregiver □ RN □ MD. Ask: “Are you Bothered by…?”
| ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unable to Respond: □ Yes □ No
| ||||||||||
| Delirium: □ Yes □ No | ||||||||||
| Pain (or 0–10) | Tiredness | Nausea | Depression | Anxiety | Drowsiness | Anorexia | Constipation | Dyspnea | Secretions | |
| 0 | ||||||||||
| 1 | ||||||||||
| 2 | ||||||||||
| 3 | ||||||||||
| 4 | ||||||||||
| 7 | ||||||||||
Scoring: 0 = none, 1 = a little bit, 2 = somewhat, 3 = quite a lot, 4 = very much, 7 = refused.
Help Patients and Families Prepare With Purpose: Advance Directives and Addressing Spiritual and Family Needs
As of 1991, the Patient Self-determination Act passed by the US Congress mandated that health care institutions provide information about advance directives to adult patients upon admission to their facility. Advance directives are legal documents that communicate a patient’s preferences about his/her medical care (what to do/what not to do, and who will perform decision making) in the event that the patient becomes incapacitated and is unable to make such decisions for himself/herself. Important components include the living will and medical power of attorney. In a living will, a patient specifically outlines his/her decisions about future medical care, including (but not limited to) do-not-resuscitate or do-not-intubate orders, use of life-sustaining equipment (dialysis machines, ventilators), placement of enteral feeding tubes, and organ donation. The medical power of attorney is the component of the advance directive that specifies another individual who is empowered to make decisions about the patient’s medical care if the patient is otherwise unable to do so. Since passage of the Patient Self-determination Act, completion of advance care plans has increased from 21% of patients hospitalized with serious illness to nearly 40%.44,45
Completing an advance directive is an integral component of oncology care, because at least half of our patients will die, and nearly all those with metastatic cancer will die. Studies indicate that patients view completion of the advance directive as a way of preparing for future uncertainty and incapacity by minimizing the burden of death on loved ones.46 However, in a 2003 report from the Agency for Healthcare Research and Quality, less than 50% of severely/terminally ill patients had an advance directive in their medical record.47 Recent studies have indicated that access to early and/or integrated palliative care significantly increases the frequency with which advance directives are completed by patients with advanced illness, with reported completion rates as high as 91% in those groups where a formal palliative care intervention was involved.13,14,16
Help Patients and Families With Their Spiritual Needs
Recent data show that 86% of our patients want us to be aware of their spirituality and think it is an important part of cancer care.48 There is accumulating evidence that programs that do spiritual assessments and have active chaplaincy programs have better satisfaction49 and fewer in-hospital deaths.50 In fact, if spiritual care is provided by the medical team, in distinction to community services, patients with terminal illness are more likely to use hospice and have better QOL scores.51 We use the FICA52 (F—faith, I—importance, C—community, A—address) Spiritual History Tool (www.gwumc.edu/gwish/clinical/fica.cfm) or simply ask: “Is religion or spirituality important to you?” (and have established links to chaplains when the person says “Yes… I have neglected that part of my life….”). Key elements of palliative care include knowing that patients want us to address these issues and to have predetermined resources to address these issues.
Facilitate Hospice Referrals Early
In current practice, hospice care is often initiated too late for patients and their families to derive maximal benefit. Nearly 30% of cancer patients in the United States enter hospice with less than 1 week to live.53 On average, most patients spend less than 20 days in hospice care,53 and less than 55% of Medicare cancer patients ever use hospice.54 Many oncologists view the optimal timing for hospice referral as that when “there are no treatment options left.” However, as the evidence for early and integrated palliative care continues to rise (reviewed previously here), our professional societies (ASCO, NCCN, European Society for Medical Oncology, and others) are increasingly encouraging primary cancer providers to reconsider the optimal timing and utilization of resources such as hospice at the end of life.1,5 Several investigators have now demonstrated increased use of hospice resources when referrals are made early,55 and there is a 10-fold increase in referrals when palliative care is consulted.56
Initiating a hospice referral when a patient still has 3 to 6 months to live can provide patient, family, and providers alike the opportunity to maximally understand, accept, and utilize this resource at the end of life. Indeed, although accurate forecasting in cancer patients is often considered more art than science, certain clinical features are reliable in identifying patients with less than 6 months to live.24 The development of malignant hypercalcemia (excluding patients with newly diagnosed breast cancer and multiple myeloma), malignant ascites, malignant pleural/pericardial effusion, and malignant bowel obstruction are among these tell-tale scenarios.57
How Can I Access Resources to Help Me?
Primary palliative care should be part of most oncology practices now, but the practice patterns observed in studies such as the Temel lung cancer study suggest it is not being done.7,13 The NCCN has readily available guidelines that detail the components of palliative care. ASCO University has excellent tools on palliative care (http://university.asco.org/palliative-care-review), as does the Center to Advance Palliative Care Web site (http://www.capc.org/). We use the natural history of the illness as prompts to remember to deliver the best palliative care at the most meaningful intervals. An up-to-date list of providers is available at www.getpalliativecare.org.
What Are the Barriers to Accessing and Integrating Palliative Care?
First, we need more clinic- and community-based nonhospice palliative care programs. The pioneering programs of Capital Caring and US Oncology suggest that such programs are productive and self-sustaining. Second, we need more dedicated secondary/tertiary palliative care providers to meet the growing demand, as there is a workforce shortage in both oncology and palliative care. Finally, we need better financial support/reimbursement infrastructure to support early palliative care interventions—most resources in this regard are available only in the hospice/end-of-life setting. The available data show that provision of “expanded access” programs, such as the Aetna Compassionate Care program of allowing hospice to be involved with concurrent chemotherapy, showed that hospice days were increased, hospital days at the end of life were reduced 7-fold, and intensive care days reduced nearly 10-fold.58 Based on the equal survival and better end-of-life care with earlier hospice involvement and a 22% savings in the last 40 days of life, Aetna has made this routinely available.59
CONCLUSIONS
With recent advances in diagnostic, therapeutic, and supportive care strategies for our cancer patients, we as oncologists and longitudinal care providers must empower ourselves to offer comprehensive, compassionate, and high-quality care to a growing population of medically complex patients. Early and effective integration of palliative care into our daily best practice means that we recognize, understand, and are agile with the opportunities to meaningfully intervene and resources that will help us to do so. The provision of primary palliative care is learnable and dependent on patient-centered communication occurring at regular/disease-prompted intervals, routine and systematic use and documentation of symptom assessments, completion of spiritual assessments, and early involvement of specialized hospice and palliative care providers.
Acknowledgments
No specific grant funding for this project.
The authors thank Nancy Cisar for expert administrative and secretarial assistance.
Footnotes
The authors have disclosed that they have no significant relationships with, or financial interest in, any commercial companies pertaining to this article.
References
- 1.Smith TJ, Temin S, Alesi E, et al. American Society of Clinical Oncology Provisional Clinical Opinion: the integration of palliative care into standard oncology care. J Clin Oncol. 2012;30:880–887. doi: 10.1200/JCO.2011.38.5161. [DOI] [PubMed] [Google Scholar]
- 2.Peppercorn JM, Smith TJ, Helft PR, et al. American Society of Clinical Oncology Statement: toward individualized care for patients with advanced cancer. J Clin Oncol. 2011;29:755–760. doi: 10.1200/JCO.2010.33.1744. [DOI] [PubMed] [Google Scholar]
- 3.Center to Advance Palliative Care. What is palliative care? 2012 Available at: http://www.getpalliativecare/org/whatis.
- 4.Center for Medicare and Medicaid Services. Medicare hospice benefits. US Department of Health and Human Services; 2012. Available at: http://www.medicare.gov/publications/pubs/pdf/02154.pdf. [Google Scholar]
- 5.Levy M, Benedetti C, Billings JA, et al. NCCN clinical practice guidelines in oncology: palliative care. J Natl Compr Canc Netw. 2009;7:436–473. doi: 10.6004/jnccn.2009.0031. [DOI] [PubMed] [Google Scholar]
- 6.Bakitas M, Lyons KD, Helgel MT, et al. Oncologists’ perspectives on concurrent palliative care in a National Cancer Institute–designated comprehensive cancer center. Palliat Support Care. 2012:1–9. doi: 10.1017/S1478951512000673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abram JL. Integrating palliative care into comprehensive cancer care. J Natl Compr Canc Netw. 2012;20:1192–1198. doi: 10.6004/jnccn.2012.0126. [DOI] [PubMed] [Google Scholar]
- 8.Blaney DW, Severson J, Martin CJ, et al. Michigan oncology practices showed varying adherence rates to practice guidelines, but quality interventions improved care. Health Aff (Millwood) 2012;31:718–728. doi: 10.1377/hlthaff.2011.1295. [DOI] [PubMed] [Google Scholar]
- 9.Weismann DE. Identifying patients in need of a palliative care assessment in a hospital setting: a concensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14:17–23. doi: 10.1089/jpm.2010.0347. [DOI] [PubMed] [Google Scholar]
- 10.Muir JC, Daly F, Davis MS, et al. Integrating palliative care into the outpatient, private practice oncology setting. J Pain Symptom Manage. 2010;40:126–135. doi: 10.1016/j.jpainsymman.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 11.Alesi E, Fletcher DS, Muir C, et al. Palliative care and oncology partnerships in real practice. Oncology (Williston Park) 2011;25:1287–1290. 1292–1293. [PubMed] [Google Scholar]
- 12.Bakitas M, Lyons KDSO, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA. 2009;302:741. doi: 10.1001/jama.2009.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non small-cell lung cancer. N Engl J Med. 2010;363:733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 14.Rabow MW, Dibble SL, Pantilat SZ, et al. The comprehensive care team: a controlled trial of outpatient palliative medicine consultation. Arch Intern Med. 2004;164:83–91. doi: 10.1001/archinte.164.1.83. [DOI] [PubMed] [Google Scholar]
- 15.Brumley R, Enguidanos S, Jamison P, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007;55:993–1000. doi: 10.1111/j.1532-5415.2007.01234.x. [DOI] [PubMed] [Google Scholar]
- 16.Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11:180–190. doi: 10.1089/jpm.2007.0055. [DOI] [PubMed] [Google Scholar]
- 17.Meyers FJ, Carducci M, Loscalzo MJ, et al. Effects of a problem-solving intervention (COPE) on quality of life for patients with advanced cancer on clinical trials and their caregivers: Simultaneous Care Educational Intervention (SCEI): linking palliation and clinical trials. J Palliat Med. 2011;14:465–473. doi: 10.1089/jpm.2010.0416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Molassiotis A, Brearley S, Saunders M, et al. Effectiveness of a home care nursing program in the symptom management of patients with colorectal and breast cancer receiving oral chemotherapy: a randomized, controlled trial. J Clin Oncol. 2009;27:6191–6198. doi: 10.1200/JCO.2008.20.6755. [DOI] [PubMed] [Google Scholar]
- 19.El-Jawahri A, Greer JA, Temel J. Does palliative care improve outcomes for patients with incurable illness? A review of the evidence. J Support Oncol. 2012;9:87–94. doi: 10.1016/j.suponc.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Higginson IJ, Evans CJ. What is the evidence that palliative care teams improve outcomes for cancer patients and their families? Cancer J. 2010;16:423–435. doi: 10.1097/PPO.0b013e3181f684e5. [DOI] [PubMed] [Google Scholar]
- 21.Zimmermann C, Riechelmann R, Krzyzanowska M, et al. Effectiveness of specialized palliative care: a systematic review. JAMA. 2008;299:1698–1709. doi: 10.1001/jama.299.14.1698. [DOI] [PubMed] [Google Scholar]
- 22.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279:1709–1714. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 23.Christakis NA, Lamont EB, Smith JL, et al. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study/commentaries. Br Med J. 2000;320:469–472. doi: 10.1136/bmj.320.7233.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salpeter SR, Malter DS, Luo EJ, et al. Systematic review of cancer presentations with a median survival of six months or less. J Palliat Med. 2012;15:175–185. doi: 10.1089/jpm.2011.0192. [DOI] [PubMed] [Google Scholar]
- 25.Morita T, Tsunoda J, Inoue S, et al. The Palliative Prognostic Index: a scoring system for survival prediction of terminally ill cancer patients. Support Care Cancer. 1999;7:128–133. doi: 10.1007/s005200050242. [DOI] [PubMed] [Google Scholar]
- 26.Pirovano M, Maltoni M, Nanni O, et al. A new palliative prognostic score: a first step for the staging of terminally ill cancer patients. An Italian Multicenter and Study Group on Palliative Care. J Pain Symptom Manage. 1999;17:231–239. doi: 10.1016/s0885-3924(98)00145-6. [DOI] [PubMed] [Google Scholar]
- 27.Temel JS, Greer JA, Admane S, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non–small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol. 2011;29:2319–2326. doi: 10.1200/JCO.2010.32.4459. [DOI] [PubMed] [Google Scholar]
- 28.Smith TJ, Longo DL. Talking with patients about dying. N Engl J Med. 2012;367:1651–1652. doi: 10.1056/NEJMe1211160. [DOI] [PubMed] [Google Scholar]
- 29.Ford S, Fallowfield L, Lewis SN. Doctor-patient interactions in oncology. Soc Sci Med. 1996;42:1511–1519. doi: 10.1016/0277-9536(95)00265-0. [DOI] [PubMed] [Google Scholar]
- 30.Back AL, Arnold RM, Aile WF. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med. 2007;167:453–460. doi: 10.1001/archinte.167.5.453. [DOI] [PubMed] [Google Scholar]
- 31.Barth J, Lannen P. Efficacy of communication skills training courses in oncology: a systematic review and meta-analysis. Ann Oncol. 2011;22:1030–1040. doi: 10.1093/annonc/mdq441. [DOI] [PubMed] [Google Scholar]
- 32.Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet. 2004;363:312–319. doi: 10.1016/S0140-6736(03)15392-5. [DOI] [PubMed] [Google Scholar]
- 33.Moore PM, Rivera Mercado S, Grez Artigues M, Lawrie TA. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev. 2013 Mar 28;3:CD003751. doi: 10.1002/14651858.CD003751.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kissane DW, Bylund CL, Banerjee SC, et al. Communication skills training for oncology professionals. J Clin Oncol. 2012;30:1242–1247. doi: 10.1200/JCO.2011.39.6184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maerkert I, Libert Y, Razavi D. Communication skills training in cancer care: where are we and where are we going? Curr Opin Oncol. 2005;17:319–330. doi: 10.1097/01.cco.0000167737.72196.f9. [DOI] [PubMed] [Google Scholar]
- 36.Ptacek JT, Eberhardt TL. Breaking bad news: a review of the literature. JAMA. 1996;276:496–502. [PubMed] [Google Scholar]
- 37.Uitterhoeve R, Bensing J, Grol R, et al. The effect of communication skills training on patient outcomes in cancer care: a systematic review of the literature. Eur J Cancer Care. 2010;19:442–457. doi: 10.1111/j.1365-2354.2009.01082.x. [DOI] [PubMed] [Google Scholar]
- 38.Huskamp HA, Keating NL, Malin JL, et al. Discussions with physicians about hospice among patients with metastatic lung cancer. Arch Intern Med. 2009;169:954–962. doi: 10.1001/archinternmed.2009.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mack JW, Cronin A, Taback N, et al. End-of-life care discussions among patients with advanced cancer. Ann Intern Med. 2012;156:204W–220W. doi: 10.1059/0003-4819-156-3-201202070-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Keating NL, Landrum MB, Rogers SO, et al. Physician factors associated with discussions about end-of-life care. Cancer. 2010;116:998–1006. doi: 10.1002/cncr.24761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.American Society of Clinical Oncology. Decision aid—stage IV non-small cell lung cancer (NSCLC) third-line and fourth-line chemotherapy. 2004 Serial online. Available at: http://www.asco.org/sites/www.asco.org/files/nsclc_third_and_forth_line_decision_aid_11.12.09_1.pd.
- 42.Gilbertson-White S, Aouizerat BE, Jahan T, et al. A review of the literature on multiple symptoms, their predictors, and associated outcomes in patients with advanced cancer. Palliat Support Care. 2011;9:81–102. doi: 10.1017/S147895151000057X. [DOI] [PubMed] [Google Scholar]
- 43.Trajkovic-Vidakovic M, de Graeff A, Voest EE, et al. Symptoms tell it all: a systematic review of the value of symptom assessment to predict survival in advanced cancer patients. Crit Rev Oncol Hematol. 2012;84:130–148. doi: 10.1016/j.critrevonc.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 44.Teno J, Wenger N, Phillips RS, et al. Advance directives for seriously ill hospitalized patients: effectiveness with the patient self-determination act and the SUPPORT intervention. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc. 1997;45:500–507. doi: 10.1111/j.1532-5415.1997.tb05178.x. [DOI] [PubMed] [Google Scholar]
- 45.Degenholtz HB, Rhee Y, Arnold RM. Brief communication: the relationship between having a living will and dying in place. Ann Intern Med. 2004;141:113–117. doi: 10.7326/0003-4819-141-2-200407200-00009. [DOI] [PubMed] [Google Scholar]
- 46.Singer PA, Martin DK, Lavery JV, et al. Reconceptualizing advance care planning from the patient’s perspective. Arch Intern Med. 1998;158:879–884. doi: 10.1001/archinte.158.8.879. [DOI] [PubMed] [Google Scholar]
- 47.Kass-Bartelms BL, Hughes R. Advance care planning: preferences for care at the end of life. J Pain Palliat Care Pharmacother. 2004;18:87–109. [PubMed] [Google Scholar]
- 48.Balboni MJ, Sullivan A, Amobi A, et al. Why is spiritual care infrequent at the end of life? spiritual care perceptions among patients, nurses, and physicians and the role of training. J Clin Oncol. 2013;31:461–467. doi: 10.1200/JCO.2012.44.6443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Williams JA, Meltzer D, Arora V, et al. Attention to inpatients’ religious and spiritual concerns: predictors and association with patient satisfaction. J Gen Intern Med. 2011;26:1265–1271. doi: 10.1007/s11606-011-1781-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.El Nawawi NM, Balboni MJ, Balboni TA. Palliative care and spiritual care: the crucial role of spiritual care in the care of patients with advanced illness. Curr Opin Support Palliat Care. 2012;6:269–274. doi: 10.1097/SPC.0b013e3283530d13. [DOI] [PubMed] [Google Scholar]
- 51.Balboni TA, Paulk ME, Balboni MJ, et al. Provision of spiritual care to patients with advanced cancer: associations with medical care and quality of life near death. J Clin Oncol. 2010;28:445–452. doi: 10.1200/JCO.2009.24.8005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Borneman T, Ferrell B, Puchalski CM. Evaluation of the FICA tool for spiritual assessment. J Pain Symptom Manage. 2010;40:163–173. doi: 10.1016/j.jpainsymman.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 53.NHPCO Facts and Figures: Hospice Care in America. Alexandria, VA: National Hospice and Palliative Care Organization; Oct, 2012. Available at: http://www.nhpco.org/sites/default/files/public/Statistics_Research/2012_Facts_Figures.pdf. [Google Scholar]
- 54.Morden NE, Chang CH, Jacobson JO, et al. End-of-life care for Medicare beneficiaries with cancer is highly intensive overall and varies widely. Health Aff. 2012;31:786–796. doi: 10.1377/hlthaff.2011.0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pitorak E, Armor M, Sivec H. Project Safe Conduct integrates palliative goals into comprehensive cancer care: an interview with Elizabeth Ford Pitorak and Meri Armour. Innov End of Life Care. 2002;4(4) doi: 10.1089/109662103768253812. serial online. [DOI] [PubMed] [Google Scholar]
- 56.Morrison RS, Dietrich J, Ladwig S, et al. Palliative care consultation teams cut hospital costs for Medicaid beneficiaries. Health Aff. 2011;30:454–463. doi: 10.1377/hlthaff.2010.0929. [DOI] [PubMed] [Google Scholar]
- 57.Ryan NM, Birring SS, Gibson PG. Gabapentin for refractory chronic cough: a randomised, double-blind, placebo-controlled trial. Lancet. 2012;380:1583–1589. doi: 10.1016/S0140-6736(12)60776-4. [DOI] [PubMed] [Google Scholar]
- 58.Spettell CM, Rawlins WS, Krakauer R, et al. A comprehensive case management program to improve palliative care. J Palliat Med. 2009;12:827–832. doi: 10.1089/jpm.2009.0089. [DOI] [PubMed] [Google Scholar]
- 59.Krakauer R, Spettell CM, Reisman L, et al. Opportunities to improve the quality of care for advanced illness. Health Aff. 2011;28:1357–1359. doi: 10.1377/hlthaff.28.5.1357. [DOI] [PubMed] [Google Scholar]


