Abstract
Splenic artery aneurysm (SAA) is a rare and potentially life-threatening clinical entity that carries a risk of rupture and peritoneal hemorrhage. When ruptured, it typically manifests as abdominal pain with hemodynamic instability. This is a report about a 29-year-old male admitted for evaluation of recentonset ascites following the spontaneous resolution of a transient episode of severe epigastric and left upper quadrant pain with syncope the preceding day. Paracentesis revealed bloody fluid. Abdominal computed tomographic angiography (CTA) and magnetic resonance venography (MRV) showed a three centimeter SAA. During admission, prompt exploratory laparotomy was performed that revealed excessive intraperitoneal hemorrhage due to a ruptured SAA. The pathology report confirmed that the SAA had developed secondary to atherosclerosis. Careful history taking together with appropriate imaging tests and emergent surgical intervention led to a timely diagnosis and the patient’ s survival.
Keywords: Splenic artery aneurysm, Abdominal pain, Hypotension, Computed tomographic angiography, Magnetic resonance venography
INTRODUCTION
Splenic artery aneurysm (SAA) is an uncommon cause of abdominal pain.1 It is reported to have an incidence rate of 0.7% in the normal population, even though rates as high as 10% have been found on necropsy studies.2 If intact, SAAs are typically asymptomatic but may be associated with manifestations such as epigastric pain or obstructive jaundice.3-6 Fatal hemorrhage, however, commonly occurs subsequent to aneurysm rupture – the only significant reported complication of SAA. The rupture typically presents with abdominal pain and hemodynamic instability.7 Reports of rupture rates are inconsistent and vary from 5%-10% to as high as 46%, with the highest incidence reported in young pregnant females.5,8-10, Mortality rates range from 10%-25% in non-pregnant patients and may reach 56% in pregnant females.
The incidental diagnosis of SAA is becoming increasingly more frequent with the increase in use of cross-sectional imaging modalities (e.g., computed tomography and magnetic resonance imaging) for the investigation of abdominal pain.11
The cause of SAA is not clearly identified, yet the increased volume of blood flowing through the splenic artery can contribute to its formation.12 It has also been associated with hypertension, portal hypertension, cirrhosis and liver transplantation.13
The following is a case presentation of a patient with SAA as a rare cause of abdominal pain and ascites. The diagnostic approach, including appropriate imaging tests, and the management steps taken are discussed below along with a review of the literature.
CASE REPORT
A 29-year-old male was admitted to Ghaem Hospital, Mashad, Iran in June 2013 with complaints of a transient episode of severe epigastric pain and syncope which had occurred the previous day. On admission, he had intermittent abdominal pain in the epigastric and periumbilical regions without any other associated symptoms. His past medical history was unremarkable.
On the physical examination, he had a blood pressure of 100/70 mmHg and a pulse rate of 100 beats per minute, with normal body temperature recordings and blood oxygen saturation levels. On the abdominal examination, a symmetric distention was noted with mild tenderness in the epigastrium without any evidence of peritoneal irritation (e.g., abdominal guarding or rebound tenderness) or a pulsatile mass. No further abnormalities were found on physical examination.
The complete blood count revealed a white blood cell (WBC) count of 16700/mm3 and a left shift without any abnormal hemoglobin levels or platelet counts. The lactate dehydrogenase levels had increased to approximately six times that of the upper limit of normal. The liver function and all biochemical tests were normal. Abdominal and erect chest radiographs were without any significant findings. Emergency abdominal ultrasound (U/S) showed mild ascites with bloody paracentesis indicative of a high serum-ascites albumin gradient (2.2 g/dL) and high ascites protein (2.7 g/dL). In addition, the ascites analysis demonstrated 5630 WBCs/mm3, with a predominance of polymorphonuclear cells, numerous red blood cells, and negative bacterial smears and cultures.
Based on the symptom of abdominal pain and a high-gradient-high-protein abdominal fluid analysis Doppler ultrasonography of the inferior vena cava (IVC) and the hepatic and portal veins were performed to evaluate for intra-abdominal vein thromboses, which included Budd-Chiari syndrome. With normal Doppler results the patient was scheduled to undergo magnetic resonance venography (MRV) for better assessment of the IVC. However, prior to further imaging, a repeat episode of acute severe generalized abdominal pain and hypotension occurred, which lasted approximately three minutes. Subsequent emergency abdomino-pelvic computed tomography scan showed thick collections in the pelvic area with a similar high albumin-gradient and protein results on repeat paracentesis.
A ruptured abdominal vascular aneurysm was suspected with a repeat bloody paracentesis and the impression was strengthened by the falling hemoglobin levels, which declined from the initial normal value to levels as low as 8.7 g/dL. Therefore, after hemodynamic stabilization, the patient underwent an urgent abdominal computed tomographic angiography (CTA) and MRV, both of which detected a 3 cm splenic aneurysm in the distal part of the splenic artery near the pancreas with small amounts of fluid that surrounded the defect (Figures 1, 2).
Fig. 1 .
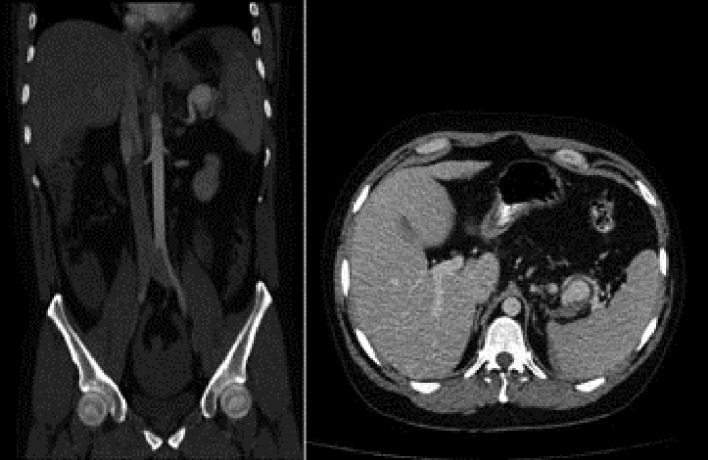
IV contrast-enhanced axial and coronal multiplanar reformation CT images of a 29-year -old man with abdominal pain showing a 3cm aneurysm located near the splenic hilum, with adjacent retroperitoneal hemorrhage.
Fig. 2 .

A three-dimensional MR angiographic arterial-phase image with maximum intensity projection performed in the coronal oblique view after enhancement with gadolinium in a29-year-old man with abdominal pain revealing an aneurysm in the splenic artery.
At two hours prior to the planned exploratory laparotomy the patient’s condition suddenly deteriorated with progressive abdominal distention, hypotension and confusion. Despite aggressive resuscitation with intravenous crystalloid fluids, the patient’s mental status quickly deteriorated leading to complete loss of consciousness. He was immediately taken to the operating room, where an exploratory laparotomy revealed approximately three liters of blood in the peritoneal cavity and blood filling the lesser sac. The pancreas appeared slightly edematous in the region of the aneurysm. With a rupture detected in the SAA and adhesions surrounding the area, we performed a ligation of the proximal portion of the artery together with resection of the aneurysm and spleen. Later, histologic examination of the vessel wall showed a perforated arteriosclerotic aneurysm of the splenic artery with normal spleen pathology. There were no complications after the surgical operation and the patient was discharged from the hospital in good condition ten days later.
DISCUSSION
SAA are the second most common intra-abdominal aneurysms after those of the aortoiliac arteries.3-5 With a mean size of 2.1 cm, SAAs are rarely larger than 3 cm. Therefore, giant aneurysms are extremely rare and previous reports of aneurysms ≥8 cm have not exceeded ten cases.6,8,14,15 The exact etiology of SAA is not known, but risk factors for the disease include arterial fibro dysplasia, multiparity, arteriosclerosis, pancreatitis, trauma, chronic liver disease and portal hypertension, with the latter two considered the most common etiologies.13
SAA is a rare, typically asymptomatic clinical entity with only 27% of inflicted patients presenting with abdominal pain. Nevertheless, the condition is increasingly being recognized due to the availability of advanced imaging techniques.5 Rupture of the aneurysm is the main complication seen in 3.0%-9.6% of cases.9,16 The risk for rupture, however, reaches 50% in pregnant patients in whom 65% of all SAAs occur.17-22 Therefore, since SAAs have been largely described in females the occurrence of such a condition in a young healthy male with no associated medical history, especially that of trauma or portal hypertension, is rare with only a handful of case reports reporting similar presentations.23-25
An acute-onset pain in the left upper quadrant is usually indicative of rupture which may be associated with hypotension or only significantly delayed signs of hemorrhage. Such a “double rupture” phenomenon (e.g., acute pain followed by delayed signs of hemorrhage) is reflective of an initial bleeding episode confined to the lesser sac which, approximately 6-96 hours later, is followed by free intraperitoneal hemorrhage and shock, eventuating in the collapse of the patient.6,8,16 This two-phase phenomenon, which has been reported in 25% of cases, provides an invaluable opportunity for the attending clinician to make a proper diagnosis and timely intervention.1,26,27 In the present case, a similar pattern of presentation, with two episodes of sudden abdominal pain and mild hypotension provided sufficient time for diagnostic workup prior to emergency laparotomy. However, an unnecessary delay in the decision to perform surgery put the patient at a higher risk of mortality due to serious intraperitoneal hemorrhage. Available evidence has suggested that painful or symptomatic aneurysms, an aneurysm of any diameter in a pregnant female, following liver transplantation, and an aneurysm more than 2 cm should be operated as soon as possible.3,5,14,17,28 Therefore, it is highly recommended that in such cases, as soon as a diagnosis of SAA with leakage is made, immediate surgical operation be performed prior to the completion of the “double rupture” phenomenon.
There are basically two approaches to the treatment of SAAs – endovascular or surgical. For elective cases of unruptured true aneurysms the more common method used is the endovascular approach which is also less invasive.29 However, laparoscopic surgery is indicated for more complicated cases and aggressive surgical operations for ruptured SAAs.1,3,17 Surgical treatment consists of aneurysmectomy with or without splenectomy.13,30-32, Preservation of the spleen is desirable yet difficult in the case of rupture.
Finally, although fortunately rare, SAAs are associated with high mortality rates and thus a high clinical suspicion is vital in avoiding a misdiagnosis. The diagnosis of SAA should be contemplated in any patient with sudden-onset pain in the upper abdomen with or without hypotension, especially when falling hemoglobin levels and new-onset ascites complicate the clinical picture. Timely detection of a ruptured SAA and emergent surgical management significantly improves the patient’s chances of survival, particularly in the presence of the “double rupture” phenomenon.
ACKNOWLEDGEMENTS
We would like to thank the Vascular Surgery Department at Emamreza Hospital and the medical team at Ghaem Hospital. This study has no conflict of interest.
CONFLICT OF INTEREST
The authors declare no conflict of interest related to this work.
Please cite this paper as:
Goshayeshi L, Vosoghinia H, Rajabzadeh F, Sakhmaresi AM, Farzanehfar MR. Splenic Artery Aneurysm as an Unusual Cause of New Onset Ascites: A Case Report. Middle East J Dig Dis 2014;6:37-41.
References
- 1.Manjula D, Al Mashini S, Golash V. Rupture of splenic artery aneurysm during pregnancy: a report of two cases. Oman Med J. 2011;26:1–3. doi: 10.5001/omj.2011.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Vries JE, Schattenkerk ME, Malt RA. Complications of the splenic artery aneurysm other than intraperitoneal rupture. Surgery. 1982;91:200. [PubMed] [Google Scholar]
- 3.Matsumoto K, Ohgami M, Shirasugi N, Nohga K, Kitajima M. A first case report of the successful laparoscopic repair of a splenic artery aneurysm. Surgery. 1997;121:462. doi: 10.1016/s0039-6060(97)90318-4. [DOI] [PubMed] [Google Scholar]
- 4.Reidy JF, Rowe PH, Ellis FG. Splenic artery aneurysm embolisation—the preferred technique to surgery. Clin Radiol. 1990;41:281–2. doi: 10.1016/s0009-9260(05)81667-8. [DOI] [PubMed] [Google Scholar]
- 5.Algudkar A. Unruptured splenic artery aneurysm presenting as epigastric pain . JRSM Short Rep. 2010;1:24. doi: 10.1258/shorts.2010.010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coulier B, Mairy Y, Broze B, Ramboux A. Giant splenic artery aneurysm presenting as an unusual cause of obstructive jaundice. JBR-BTR. 2006;89:201–3. [PubMed] [Google Scholar]
- 7.Mattar SG, Lumsden AB. The management of splenic artery aneurysms: experience with 23 cases. Am J Surg. 1995;169:580–584. doi: 10.1016/s0002-9610(99)80225-6. [DOI] [PubMed] [Google Scholar]
- 8.Long CD, Bakshi KR, Kahn MB, Roberts AB. Giant splenic artery aneurysm. Ann Vasc Surg. 1993;7:474–478. doi: 10.1007/BF02002133. [DOI] [PubMed] [Google Scholar]
- 9.Lee SY, Florica O. Laparoscopic resection of splenic artery aneurysm with preservation of splenic function. Singapore Med J. 2008;49:e303–e304. [PubMed] [Google Scholar]
- 10.Tochii M, Ogino H, Sasaki H, Matsuda H, Minatoya K, Yagihara T, Kitamura S. Successful surgical treatment for aneurysm of splenic artery with anomalous origin. Ann Thorac Cardiovasc Surg. 2005;11:346–9. [PubMed] [Google Scholar]
- 11.Agrawal GA, Johnson PT, Fishman EK. Splenic artery aneurysms and pseudoaneurysms: clinical distinctions and CT appearances. AJR Am J Roentgenol. 2007;188:992–9. doi: 10.2214/AJR.06.0794. [DOI] [PubMed] [Google Scholar]
- 12.Ayalon A, Wiesner RH, Perkins JD, Tominaga S, Hayes DH, Krom RA. Splenic artery aneurysms in liver transplant patients. Transplantation. 1998;45:386–9. doi: 10.1097/00007890-198802000-00028. [DOI] [PubMed] [Google Scholar]
- 13.Manjunatha YC, Prasad KN, Beeregowda YC, Bhaskaran A. Multiple splenic artery aneurysms secondary to extra hepatic portal vein obstruction . J Clin Diagn Res. 2013;7:401–402. doi: 10.7860/JCDR/2013/4087.2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kehagias DT, Tzalonikos MT, Moulopoulos LA, Gouliamos AD, Mourikis DA, Vlahos LJ. MRI of a giant splenic artery aneurysm. Brit J Radiol. 1998;71:444–446. doi: 10.1259/bjr.71.844.9659140. [DOI] [PubMed] [Google Scholar]
- 15.Bornet P, Medjoubi SA, Tissot A, Jurado A, Hibon J, Terris C. Giant aneurysm of the splenic artery: a case report. Angiology. 2000;51:343–347. doi: 10.1177/000331970005100411. [DOI] [PubMed] [Google Scholar]
- 16.Deshpande AA, Kulkarni VM, Rege S, Dalvi AN, Hardikar JV. Ruptured true aneurysm of the splenic artery: an unusual cause of haemoperitoneum. J Postgrad Med. 2000;46:191–2. [PubMed] [Google Scholar]
- 17.Kim Y, Johna S. Laparoscopic excision of splenic artery aneurysm. JSLS. 2013;17:132–134. doi: 10.4293/108680812X13517013317392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benali M, Charrada H, Bouassida M, Bahloul A, Jmal K, Dhouib F. et al. Splenic rtery aneurysm rupture in late pregnancy: a case report. Ann Fr Anesth Reanim. 2013;32:721–2. doi: 10.1016/j.annfar.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 19.Boufettal H, Moussaïd I, Salmi S, Mahdaoui S, Hermas S, Samouh N. Spontaneous rupture of a splenic artery aneurysm in peri-partum. Ann Fr Anesth Reani. 2013;32:722. doi: 10.1016/j.annfar.2013.07.799. [DOI] [PubMed] [Google Scholar]
- 20.Holdsworth RJ, Gunn A. Ruptured splenic artery aneurysm in pregnancy: a review. Br J Obstet Gynaecol. 1992;99:595–7. doi: 10.1111/j.1471-0528.1992.tb13828.x. [DOI] [PubMed] [Google Scholar]
- 21.De Vries JE, Schattenkerk ME, Malt RA. Complications of splenic artery aneurysm other than intraperitoneal rupture. Surgery. 1982;91:200–4. [PubMed] [Google Scholar]
- 22.O’Grady JP, Day EJ, Toole AL, Paust JC. Splenic artery aneurysm rupture in pregnancy: a review and case report. Obstet Gynecol. 1977;50:627–30. [PubMed] [Google Scholar]
- 23.Mattick A, Gawthorpe I. Splenic artery aneurysm rupture: a case report of this uncommon presentation. Emerg Med J. 2007;24:863. doi: 10.1136/emj.2007.048637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sarikaya S, Ecki B, Aktas C, Cetin A, Ay D, Demirag A. A rare clinical presentation of abdominal pain: rupture of splenic artery aneurysm: a case report. Cases j. 2009;2:148. doi: 10.1186/1757-1626-2-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Green A, Bowman-Burns C, Cumberbatch G. Abdominal pain and collapse in the emergency department. BMJ Case Rep. 2013;2013:bcr2013009925. doi: 10.1136/bcr-2013-009925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mattar SG, Lumsden AB. The management of splenic artery aneurysms: experience with 23 cases. Am J Surg. 1995;169:580–4. doi: 10.1016/s0002-9610(99)80225-6. [DOI] [PubMed] [Google Scholar]
- 27.Remy D, Linder JL. Splenic aneurysm rupture: case report and review of the literature. Acta Chir Belg. 1993;93:54–7. [PubMed] [Google Scholar]
- 28.Al-Habbal Y, Christophi C, Muralidharan V. Aneurysms of the splenic artery: a review. Surgeon. 2010;8:223–31. doi: 10.1016/j.surge.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 29.Arepally A, Dagli M, Hofmann LV, Kim HS, Cooper M, Klein A. Treatment of splenic artery aneurysm with use of a stent-graft. J Vasc Interv Radiol. 2002;13:631–3. doi: 10.1016/s1051-0443(07)61659-5. [DOI] [PubMed] [Google Scholar]
- 30.Holdsworth RJ, Gunn A. Ruptured splenic artery aneurysm in pregnancy: A review. Br J Obstet Gynaecol. 1992;99:595–7. doi: 10.1111/j.1471-0528.1992.tb13828.x. [DOI] [PubMed] [Google Scholar]
- 31.Barrett JM, Van Hooydonk JE, Boehm FH. Pregnancy-related rupture of arterial aneurysms. Obstet Gynecol Surv. 1982;37:557–66. doi: 10.1097/00006254-198209000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Qiu JF, Xu L, Wu ZY. Diagnosis and surgical treatment of giant splenic artery aneurysms with portal hypertension: a report of 4 cases. Hepatobiliary Pancreat Dis Int. 2004;3:526–9. [PubMed] [Google Scholar]


