Abstract
Objectives
To examine the association of anxiety and depression with pulmonary-specific symptoms of Chronic Obstructive Pulmonary Disease (COPD), and to determine the extent to which disease severity and functional capacity modify this association.
Method
Patients (N = 162) enrolled in the INSPIRE-II study, an ongoing randomized, clinical trial of COPD patients and their caregivers who received either telephone-based coping skills training or education and symptom monitoring. Patients completed a psychosocial test battery including: Brief Fatigue Inventory, St. George’s Respiratory Questionnaire, UCSD Shortness of Breath Questionnaire, State-Trait Anxiety Inventory, and Beck Depression Inventory. Measures of disease severity and functional capacity (i.e., FEV1 and six-minute walk test) were also obtained.
Results
After covariate adjustment, higher anxiety and depression levels were associated with greater fatigue levels (ps < .001, ΔR2 = 0.16 and 0.29, respectively), shortness of breath (ps < .001, ΔR2 = 0.12 and 0.10), and frequency of COPD symptoms (ps < .001, ΔR2 = 0.11 and 0.13). In addition, functional capacity was a moderator of anxiety and pulmonary-specific COPD symptoms. The association between anxiety and shortness of breath (p = 0.009) and frequency of COPD symptoms (p = 0.02) was greater among patients with lower functional capacity.
Conclusions
Anxiety and depression were associated with higher levels of fatigue, shortness of breath, and frequency of COPD symptoms. It is important for clinicians to be aware of the presence of anxiety and depression in COPD patients, which appears to correlate with pulmonary-specific COPD symptoms, especially in patients with lower functional capacity. Prospective design studies are needed to elucidate the causal relationships between anxiety and depression and pulmonary-specific symptoms in COPD patients.
Keywords: anxiety, depression, COPD
INTRODUCTION
Chronic Obstructive Pulmonary Disease (COPD) is a progressive airway disease marked by symptoms of dyspnea, sputum production, wheezing, coughing, chest tightness, and fatigue [1]. The morbidity associated with these symptoms is substantial as patients often report a significant degree of disability and restriction in daily activities, decreased quality of life, and psychological distress [2]. Not surprisingly, two of the most common co-morbidities in COPD are anxiety and depression [3]. Prevalence rates of elevated depressive symptoms have been reported to be as high as 80% [4–6] and rates of elevated anxiety symptoms may exceed 90% [5, 7]. The presence of anxiety and depression in COPD is also associated with increased COPD exacerbations, COPD-related hospitalizations, and mortality [6]. Despite their negative influence on quality of life and medical outcomes [3], anxiety and depression often go undetected in clinical practice due to variations in the frequency and type of diagnostic assessment, variability in clinical presentation, and the significant overlap between co-morbid pulmonary symptoms [7].
In recent years, there has been a growing literature on the impact of psychological distress on medical factors such as pulmonary function, exercise capacity, and pulmonary-specific symptoms of COPD [8–11]. Several studies have now shown an association between elevated levels of depression and greater pulmonary symptoms (e.g., fatigue or dyspnea) [12–19]. Few studies have assessed the association between anxiety and pulmonary symptoms [15, 16] despite the complex, bidirectional relationship between anxiety and pulmonary-specific symptoms in COPD patients. Anxiety is often associated with exacerbated pulmonary symptoms such as coughing and dyspnea, which can also be potent stimuli for greater levels of anxiety [20, 21]. In addition, some therapies for COPD, such as short-acting beta agonist medications, may increase symptoms of anxiety as a result of side effects [20].
Health status, including disease severity and functional capacity, may also modify the association between anxiety and depression and pulmonary-specific symptoms in COPD, yet research on this topic is limited [22, 23]. To date, no investigation has examined the association of functional capacity on symptoms of anxiety and depression in COPD. The primary aim of this study was to determine the association between anxiety and depression and pulmonary-specific symptoms within COPD patients. We also sought to examine disease severity and functional capacity as potential moderators of this association.
METHODS
Study Design
Participants were enrolled in the INSPIRE-II study [24], an ongoing randomized, clinical trial of COPD patients and their caregivers who received either telephone-based coping skills training or an education control condition. Eligibility requirements included ≥ 21 years of age, a diagnosis of COPD (i.e., FEV1/FVC < 70%; forced expiratory volume/forced vital capacity, which are standard measurements used in spirometry testing), FEV1 > 25%, and capacity to give informed consent and follow study procedures. Exclusion criteria included dementia, psychosis, acute suicide or homicide risk, other medical illnesses (e.g., cancer) that could likely cause death within 3 years, lack of ambulatory function, unstable angina, congestive heart failure (stage III or IV), and active involvement in a pulmonary rehabilitation or a formal exercise program. All patients provided written informed consent to participate. The consent form and all study procedures were approved by the institutional review board at Duke University Medical Center.
Procedure
Participants completed a psychosocial test battery that included self-reported measures of pulmonary-specific COPD symptoms, anxiety, and depression. Demographic, medical, disease severity, and functional capacity variables were also obtained including the six minute walk test (6MWT) and pulmonary functioning (i.e., forced expiratory volume; FEV1 % predicted value).
Psychosocial Measures
Brief Fatigue Inventory (BFI) [25]
The BFI is a nine-item scale that measures the level of current, worst, and usual fatigue and interference due to fatigue. Respondents are asked to rate each item on a scale that ranges from 0 to 10. An average score from these nine items is calculated with scores (≥ 7) indicating clinically significant levels of fatigue [25].
St. George’s Respiratory Questionnaire (SGRQ)–Symptom Component [26, 27]
The SGRQ is a standardized, disease-specific measure used to assess patients with mild to severe airway disease. The SGRQ consists of 50 items that produce three domain scores and one overall score measuring: symptoms, activities, and impact. The symptom component consists of eight items that assess the frequency over the last year of coughing, sputum production, dyspnea, wheezing, and number of respiratory attacks. Responses to these items are rated on four or five possible levels of frequency of occurrence [26]. A higher score indicates a greater frequency of symptom occurrence.
University of California at San Diego Shortness of Breath Questionnaire (SOBQ) [28]
The SOBQ is a 24-item measure that assesses the occurrence of shortness of breath on a 6-point scale (0 to 5) during 21 activities of daily living associated with varying levels of exertion. The SOBQ items are summed with total scores ranging from 0 to 120 [28]. Higher scores indicate greater perceptions of dyspnea.
Beck Depression Inventory (BDI-II) [29]
The BDI-II is a standardized 21-item self-report questionnaire assessing symptoms and attitudes related to depression. The items are summed with total scores ranging from 0 to 63 with higher scores indicating higher levels of depression [29].
State-Trait Anxiety Inventory (STAI) [30]
The STAI consists of two separate self-report inventories, one measuring state anxiety and the other trait anxiety. The STAI was developed as a tool for investigating anxiety in normal (non-psychiatric) adults, but has been used in assessing anxiety in neuropsychiatric, medical, and surgical patients.
Demographic, Medical, Disease Severity, and Functional Capacity Variables
Demographics and medical characteristics were collected using self-report questionnaires that assessed age, gender, height, weight, ethnicity, marital status, education level, smoking status, medical comorbidities (as measured by the Charlson Comorbidity Index [31]), short-acting beta agonist medication usage, and anti-depressant and anxiolytic medication usage. Patients also performed the Six Minute Walk Test (6MWT), a self-paced, timed test of the total distance that a patient is able to walk in 6 minutes [32]. Further, patients also underwent standard spirometry testing according to the American Thoracic Society guidelines, which provided information on forced vital capacity and FEV1 [33]. These measurements are useful in evaluating the severity of obstruction or the presence and severity of restrictive lung disease [33].
Data Analyses
Statistical analyses were conducted using SAS [34]. Models were examined for normality, skewedness, kurtosis, multicollinearity, and homoscedasticity of the residuals prior to analysis. Because fatigue was measured twice during this investigation (i.e., once using the BFI as an outcome measure and again as an item assessed on the BDI-II), a new variable was calculated for depression which excluded fatigue from the BDI-II. Use of this strategy minimized the overlapping measurement of fatigue since it could artificially inflate the likelihood of detecting a significant correlation between depression scores and BFI outcomes. The new depression variable, which excluded fatigue, was used in all regression analyses.
Hierarchical Regression Analyses
The primary data analysis strategy was to conduct separate hierarchical regression analysis models on the BFI, SOBQ, and SGRQ (Symptom Component) scales. Each model was adjusted for age, gender, BMI, smoking status, FEV1, medical comorbidities, 6MWT, short-acting beta agonist, anti-depressant, and anxiolytic medications. Following covariate adjustment, anxiety and depression symptoms were entered into the models separately.
Associations with Disease Severity and Functional Capacity
Hierarchical regression analyses with product terms were used to examine the associations of anxiety and depression on BFI, SOBQ, and SGRQ (Symptom Component) scales at varying levels of disease severity and functional capacity (i.e., 6MWT and FEV1). Scores for anxiety, depression, 6MWT, and FEV1 were mean-centered to enhance interpretation of model estimates. All models were adjusted for age, gender, BMI, smoking status, medical comorbidities, short-acting beta agonist, anti-depressant, and anxiolytic medication usage. Following covariate adjustment (Step 1), anxiety or depression main effects and 6MWT or FEV1 main effects were entered into the models separately (Step 2), followed by corresponding product terms (e.g., anxiety by 6MWT; Step 3). A total of 12 models were constructed in order to test each product term separately.1 In the presence of a significant interaction, simple slopes were generated to examine the effect of anxiety or depression symptoms on BFI, SOBQ, and SGRQ (Symptom Component) at one standard deviation above and below the centered mean of either 6MWT or FEV1.
RESULTS
Participant Characteristics
One hundred sixty-two participants were included in this study. The mean age for the overall sample was 67 ± 8 years. As shown in Table 1, the majority of patients were Caucasian, married, and had at least a high school education. On average, participants were overweight [35], reported a history of lung disease for 3.8 ± 2 years, and had at least two comorbid medical conditions. Approximately 16% of participants were current smokers. The average FEV1 (% predicted value) in the sample was 46.5% ± 17.1%, indicating that participants demonstrated moderate levels of pulmonary obstruction. Participants walked an average of 346 ± 106 feet during the six minute walk test, which is considered low based on age-adjusted normative data [36], suggesting a lower functional capacity level, consistent with their diagnosis of COPD. Approximately 53% of participants reported the use of short-acting beta agonist medications (e.g., albuterol). More than one-quarter of participants in our sample (27%) were taking anti-depressant medications and 12% were taking anxiolytic medications.
Table 1.
Background Characteristics
| Variable | Mean | SD |
|---|---|---|
| Age (years) | 67.1 | 8.3 |
| Men, n (%) | 100 (61.7) | |
| BMI | 28.9 | 6.4 |
| Ethnicity, n (% Whites) | 146 (90.1) | |
| Education, n (% beyond high school) | 94 (58.0) | |
| Married, n (%) | 105 (64.8) | |
| Lung disease duration (years) | 3.8 | 2.1 |
| Current smoker, n (%) | 26 (16.0) | |
| CCI | 2.1 | 1.7 |
| 6MWT – Total distance (in feet) | 345.9 | 106.3 |
| FEV1 (% predicted value) | 46.5 | 17.1 |
| Short-acting beta agonist medication, n (%) | 85 (52.5) | |
| Anti-depressant medication, n (%) | 43 (26.5) | |
| Anxiolytic medication, n (%) | 20 (12.3) |
Notes: Data are given as number (%) unless otherwise indicated. SD = standard deviation; BMI = Body Mass Index; CCI = Charlson Comorbidity Index; 6MWT = 6 Minute Walk Test; FEV1 = Forced Expiratory Volume.
Anxiety, Depression, and COPD Symptoms
Approximately 27.8% of the sample had elevated levels of depressive symptoms according to the BDI-II (cut-score ≥ 14) [29] while 58% of participants endorsed medium to high levels of anxiety symptoms according to the STAI (cut-score ≥ 31) [30, 37].
After covariate adjustment, main effects models demonstrated that higher reported levels of anxiety were associated with higher levels of fatigue (ΔR2 = 36%; ΔF[1, 150] = 35.8, p < .0001) and shortness of breath (ΔR2 = 12%; ΔF[1, 149] = 34.7, p < .0001), and greater frequency of COPD symptoms (ΔR2 = 11%; ΔF[1, 150] = 22.9, p < .0001; Table 2).
Table 2.
Association of Anxiety and Depression with Pulmonary-Specific Symptoms of COPD
| Predictors | ||||||
|---|---|---|---|---|---|---|
| Anxiety | Depression | |||||
| Outcomes | B | S.E. | β | B | S.E. | β |
| Fatigue | 0.10 | 0.02 | 0.43** | 0.17 | 0.02 | 0.59** |
| Shortness of breath | 0.81 | 0.14 | 0.36** | 1.00 | 0.18 | 0.35** |
| COPD symptoms | 0.88 | 0.18 | 0.35** | 1.29 | 0.24 | 0.40** |
p < .001.
Similarly, after covariate adjustment, main effects models showed that higher levels of depression were associated with higher levels of fatigue (ΔR2 = 29%; ΔF[1, 150] = 77.6, p < .0001), shortness of breath (ΔR2 = 10%; ΔF[1, 149] = 30.1, p < .0001), and greater frequency of COPD symptoms (ΔR2 = 13%; ΔF[1, 150] = 29.2, p < .0001; Table 2).
Association of Functional Capacity on Anxiety, Depression, and COPD Symptoms
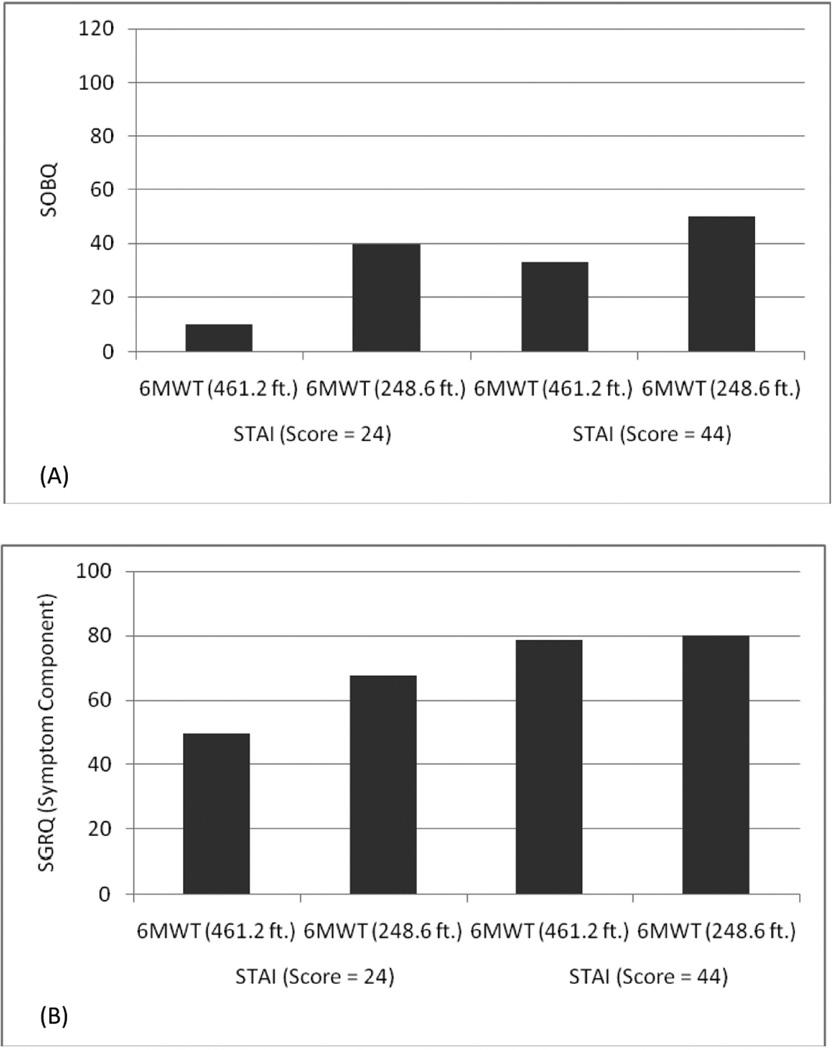
After adjustment for covariates, there was a significant anxiety by 6MWT interaction on shortness of breath (p = 0.009; ΔR2 = 0.02). Figure 1(A) shows that the association between anxiety and shortness of breath was greater among patients with lower functional capacity compared to patients with higher functional capacity. Patients with low performance on the 6MWT and higher levels of anxiety were more likely to exhibit greater symptoms of shortness of breath.
Figure 1.
Panel A – Association between High (+1 SD) and Low (−1 SD) Levels of Anxiety (STAI) and Shortness of Breath Questionnaire (SOBQ) at High (+1 SD) & Low (−1 SD) Levels of Functional Capacity (6MWT); Panel B – Association between High (+1 SD) and Low (−1 SD) Levels of Anxiety (STAI) and St. George’s Respiratory Questionnaire (Symptom Component) at High (+1 SD) and Low (−1 SD) Levels of Functional Capacity (6MWT).
Similarly, after covariate adjustment, there was a significant anxiety by 6MWT interaction on frequency of COPD symptoms (p = 0.02; ΔR2 = 0.03). Figure 1(B) shows that higher levels of anxiety were associated with greater frequency of COPD symptoms at both high and low levels of functional capacity. At higher levels of anxiety, patients demonstrated more frequent COPD symptoms regardless of their level of functional capacity.
There was not a significant anxiety by 6MWT interaction on fatigue (p = .13). In addition, all depression by 6MWT interactions on fatigue (p = 0.19), shortness of breath (p = 0.20), and frequency of COPD symptoms (p = 0.55) were non-significant. Finally, FEV1 did not affect the relationship between anxiety, depression, and COPD symptoms as all interactions between these variables were non-significant.
DISCUSSION
Higher levels of anxiety and depression are associated with elevated levels of pulmonary-specific symptoms among individuals with COPD, including fatigue, shortness of breath, and frequency of COPD symptoms. These associations remained significant even after adjustment for background characteristics and potential confounders, such as age, gender, BMI, smoking status, medical comorbidities, and short-acting beta agonist, anti-depressant, and anxiolytic medications. Although the causal direction of these findings cannot be determined, as heightened anxiety and depression could be a cause or consequence of elevated pulmonary symptoms, the results are consistent with several prior investigations that examined the association between higher depression scores and elevated levels of fatigue or dyspnea [12–14, 17–19]. However, unlike previous studies [15, 16], we examined the associations between both anxiety and depression across multiple measures of pulmonary symptoms. Demonstrating that both anxiety and depression were significantly related to pulmonary-specific COPD symptoms is clinically relevant as it reinforces the need to assess for these psychological comorbidities to improve pulmonary symptom management and increase quality of life among patients [38]. Several studies have shown that pulmonary-specific COPD symptoms are predictive of outcomes such as increased risk of hospitalization [39], failure after treatment of exacerbations [40], and early mortality [41]. In this context, identifying and treating modifiable factors such as anxiety and depression could potentially result in improved COPD outcomes.
Another important finding from this study is that the strength of the association between anxiety and pulmonary-specific COPD symptoms appears to vary by functional capacity. The association of anxiety on shortness of breath and frequency of COPD symptoms was greater among patients who demonstrated lower functional capacity. However, at higher levels of anxiety, patients reported a greater frequency of COPD symptoms regardless of their functional capacity. The cross-sectional nature of this study did not allow us to determine if lower functional capacity increased anxiety symptoms or if anxiety symptoms reduced functional capacity. Nonetheless, it may be that identifying and treating anxiety in patients at earlier stages of COPD, particularly among individuals with lower functional capacity, could help to improve pulmonary-specific COPD symptom management. This is particularly important as nearly 60% of participants in our sample reported elevated levels of anxiety and more than 25% reported taking psychotropic medications.
To our knowledge, only two prior investigations have shown that disease severity (as measured by FEV1) modifies the association between psychological distress and pulmonary-specific COPD symptoms [22, 23]. Balcells and colleagues [23] showed that the association between anxiety and depressive symptoms on health-related quality of life (as measured by the St. George’s Respiratory Questionnaire) was stronger among patients with severe to very severe COPD than among those with mild to moderate COPD symptoms. In another study, Hajiro and colleagues [22] showed that anxiety was correlated with health-related quality of life only among patients with moderate to severe COPD symptoms. However, in contrast to these studies [22, 23], we did not find that FEV1 modified the association between anxiety and pulmonary symptoms. This may suggest that COPD severity as measured by FEV1 is not differentially related to anxiety or depressive symptoms. It could also be that our lack of findings are explained by the fact that patients were only included in this study if they had a FEV1 > 25%. The exclusion of patients with more severe COPD may have precluded our ability to observe a significant association between FEV1, anxiety, and pulmonary symptoms.
Given that anxiety and depressive symptoms are both correlated to pulmonary-specific symptoms among patients with COPD and that functional capacity appears to moderate the association between anxiety and pulmonary symptoms, there is a need for treatments that reduce the anxiety characteristic of many COPD patients. Evidence is available for the efficacy of both pharmacological and non-pharmacological treatments of anxiety in COPD [38].
Limitations
The cross-sectional design of the study does not allow us to determine if a causal relationship between anxiety and depression and pulmonary-specific symptoms of COPD exists since increased anxiety and depression could be a cause or consequence of elevated pulmonary symptoms among patients with COPD. The exclusion of patients with more severe COPD (i.e., FEV1 ≤ 25%) may have precluded our ability to observe a relationship between FEV1, anxiety, and pulmonary-specific symptoms. The extent to which FEV1 impacts the relationship between anxiety and pulmonary symptoms among those with more severe COPD warrants further investigation.
CONCLUSIONS
Findings from this study suggest that co-morbid anxiety and depression are associated with increased fatigue, shortness of breath, and frequency of pulmonary-specific symptoms in COPD. The extent to which anxiety and depression exacerbate pulmonary symptoms could not be determined, as heightened anxiety and depression could be a cause or consequence of elevated pulmonary symptoms. Patients with low performance on the 6MWT and higher levels of anxiety were more likely to exhibit greater symptoms of shortness of breath. Furthermore, the association between increased anxiety and frequency of COPD symptoms appears to be strongest among patients with impaired functional capacity. At higher levels of anxiety, patients demonstrated more frequent COPD symptoms regardless of their level of functional capacity. A prospective design study is needed to better understand the temporal association between anxiety symptoms and functional capacity.
ACKNOWLEDGMENTS
The authors wish to thank Tamara Green, Amelia Hoyle, Virginia O’Hayer, and Francis Keefe for their research assistance with this article.
Footnotes
This study was performed at Duke University Medical Center and was supported by National Heart, Lung, and Blood Institute grant 5R01-HL065503.
The authors recognize that conducting multiple tests could artificially inflate the Type I error rate. However, several analytic strategies were considered (e.g., MANCOVA) to address this potential problem and the study results remained the same regardless of the strategy used. As a result, the findings are described using hierarchical regression analyses in order to highlight the significant results for each outcome measure separately.
Contributor Information
Todd Doyle, Duke University Medical Center, Durham, North Carolina
Scott Palmer, Duke University Medical Center, Durham, North Carolina.
Julie Johnson, Duke University Medical Center, Durham, North Carolina.
Michael A. Babyak, Duke University Medical Center, Durham, North Carolina
Patrick Smith, Duke University Medical Center, Durham, North Carolina
Stephanie Mabe, Duke University Medical Center, Durham, North Carolina.
Karen Welty-Wolf, Duke University Medical Center, Durham, North Carolina and Durham Veterans Administration Medical Center, North Carolina.
Tereza Martinu, Duke University Medical Center, Durham, North Carolina.
James A. Blumenthal, Duke University Medical Center, Durham, North Carolina
REFERENCES
- 1.National Heart Lung and Blood Institute. COPD. [Retrieved on May 22, 2012];2010 from http://www.nhlbi.nih.gov/health/health-topics/topics/copd.
- 2.Pommer AM, Pouwer F, Denollet J, Pop VJM. Managing co-morbid depression and anxiety in primary care patients with asthma and/or chronic obstructive pulmonary disease: Study protocol for a randomized controlled trial. Trials. 2012;13:6–13. doi: 10.1186/1745-6215-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parekh PI, Blumenthal JA, Babyak MA, Merrill K, Carney RM, Davis RD, Palmer SM. Psychiatric disorder and quality of life in patients awaiting lung transplantation. Chest. 2003;124:1682–1688. doi: 10.1378/chest.124.5.1682. [DOI] [PubMed] [Google Scholar]
- 4.Kunik ME, Roundy K, Veazey C, Souchek J, Richardson P, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127:1205–1211. doi: 10.1378/chest.127.4.1205. [DOI] [PubMed] [Google Scholar]
- 5.Hynninen KMJ, Breitve MH, Wiborg AB, Pallesen S, Nordhus IH. psychological characteristics of patients with chronic obstructive pulmonary disease: A review. Journal of Psychosomatic Research. 2005;59:429–443. doi: 10.1016/j.jpsychores.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 6.Lacasse Y, Rousseau L, Maltais F. Prevalence of depressive symptoms and depression in patients with severe oxygen-dependent chronic obstructive pulmonary disease. Journal of Cardiopulmonary Rehabilitation. 2001;21:80–86. doi: 10.1097/00008483-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Borak J, Sliwinski P, Piasecki Z, Zielinski J. Psychological status of COPD patients on long term oxygen therapy. European Respiratory Journal. 1991;4:59–62. [PubMed] [Google Scholar]
- 8.Ferrer M, Alonso J, Morera J, Marrades RM, Khalaf A, Aguar C, et al. Chronic obstructive pulmonary disease stage and health-related quality of life. Annals of Internal Medicine. 1997;127:1072–1079. doi: 10.7326/0003-4819-127-12-199712150-00003. [DOI] [PubMed] [Google Scholar]
- 9.Ketelaars CA, Schlosser MA, Mostert R, Huyer Abu-Saad H, Halfens RJ, Wouters EF. Determinants of health-related quality of life in patients with chronic obstructive pulmonary disease. Thorax. 1996;51:39–43. doi: 10.1136/thx.51.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wijnhoven HA, Kriegsman DM, Hesselink AE, de Haan M, Schellevis FG. The influence of co-morbidity on health-related quality of life in asthma and COPD patients. Respiratory Medicine. 2003;97:468–475. doi: 10.1053/rmed.2002.1463. [DOI] [PubMed] [Google Scholar]
- 11.Wijnhoven HA, Kriegsman DM, Hesselink AE, Pennix BW, de Haan M. Determinants of different dimensions of disease severity in asthma and COPD. Chest. 2001;119:1034–1042. doi: 10.1378/chest.119.4.1034. [DOI] [PubMed] [Google Scholar]
- 12.Xu W, Collet JP, Shapiro S, Lin Y, Yang T, Platt RW, Wang C, Bourbeau J. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. American Journal of Respiratory and Critical Care Medicine. 2008;178(9):913–920. doi: 10.1164/rccm.200804-619OC. [DOI] [PubMed] [Google Scholar]
- 13.Stanley MA, Veazey C, Hopko D, Diefenbach G, Kunik ME. Anxiety and depression in chronic obstructive pulmonary disease: A new intervention and case report. Cognitive and Behavioral Practice. 2005;12:424–436. [Google Scholar]
- 14.Small SP, Graydon JE. Perceived uncertainty, physical symptoms, and negative mood in hospitalized patients with chronic obstructive pulmonary disease. Heart & Lung. 1992;21:568–574. [PubMed] [Google Scholar]
- 15.Graydon JE, Ross E. Influence of symptoms, lung function, mood, and social support on level of functioning of patients with COPD. Research in Nursing & Health. 1995;18:525–533. doi: 10.1002/nur.4770180608. [DOI] [PubMed] [Google Scholar]
- 16.Kapella MC, Larson JL, Patel MK, Covey MK, Berry JK. Subjective fatigue, influencing variables, and consequences in chronic obstructive pulmonary disease. Nursing Research. 2006;55(1):10–17. doi: 10.1097/00006199-200601000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Regvat J, Zmitek A, Vegnuti M, Kosnik M, Suskovic S. Anxiety and depression during hospital treatment of exacerbation of chronic obstructive pulmonary disease. The Journal of International Medical Research. 2011;39:1028–1038. doi: 10.1177/147323001103900338. [DOI] [PubMed] [Google Scholar]
- 18.Neuman A, Gunnbjornsdottir M, Tunsater A, Nystrom L, Franklin KA, et al. Dyspnea in relation to symptoms of anxiety and depression: A prospective population study. Respiratory Medicine. 2006;100:1843–1849. doi: 10.1016/j.rmed.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 19.Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease. Archives of Internal Medicine. 2007;167:60–67. doi: 10.1001/archinte.167.1.60. [DOI] [PubMed] [Google Scholar]
- 20.Eisner MD, Blanc PD, Yelin EH, Katz PP, Sanchez G, et al. The influence of anxiety on health outcomes in COPD. Thorax. 2010;65:229–234. doi: 10.1136/thx.2009.126201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill K, Geist R, Goldstein RS, Lacasse Y. Anxiety and depression in end-stage COPD. European Respiratory Journal. 2008;31:667–677. doi: 10.1183/09031936.00125707. [DOI] [PubMed] [Google Scholar]
- 22.Hajiro T, Nishimura K, Tsukino M, Ikeda A, Oga T. Stages of disease severity and factors that affect the health status of patients with chronic obstructive pulmonary disease. Respiratory Medicine. 2000;94:841–846. doi: 10.1053/rmed.2000.0804. [DOI] [PubMed] [Google Scholar]
- 23.Balcells E, Gea J, Ferrer J, Serra I, Orozco-Levi M, de Batlle J, et al. Factors affecting the relationship between psychological status and quality of life in COPD patients. Health and Quality of Life Outcomes. 2010;8:108–116. doi: 10.1186/1477-7525-8-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blumenthal JA, Keefe FJ, Babyak MA, Fenwick CV, Johnson JM, Scott K, et al. Caregiver-assisted coping skills training for patients with COPD: Background, design, and methodological issues for the INSPIRE-II study. Clinical Trials. 2009;6:172–184. doi: 10.1177/1740774509102565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mendoza TR, Wang SX, Cleland CS, Morrissey M, Johnson BA, Huber SL. The rapid assessment of fatigue severity in cancer patients: Use of the Brief Fatigue Inventory. Cancer. 1999;85:1186–1196. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 26.Jones PW, Quirk FH, Baveystock CM. The St. George’s Respiratory Questionnaire. Respiratory Medicine. 1991;85(Supplement):25–31. doi: 10.1016/s0954-6111(06)80166-6. [DOI] [PubMed] [Google Scholar]
- 27.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. American Review of Respiratory Disease. 1992;145:1321–1327. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 28.Eakin EG, Resnikoff PM, Prewitt LM, Ries AL, Kaplan RM. Validation of a new dyspnea measure: The UCSD Shortness of Breath Questionnaire. University of California, San Diego. Chest. 1998;113:619–624. doi: 10.1378/chest.113.3.619. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Steer RA, Brown GK. Beck depression inventory manual. 2nd ed. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- 30.Speilberger CD. Manual for the state-trait anxiety inventory (Form Y) Palo Alto, CA: Consulting Psychologists; 1983. [Google Scholar]
- 31.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 32.American Thoracic Society. ATS statement: Guidelines for the six-minute walk test. American Journal of Respiratory and Critical Care Medicine. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 33.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardization of spirometry. European Respiratory Journal. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 34.SAS Institute. Version 9.03e. Cary, North Carolina: 2003. [Google Scholar]
- 35.World Health Organization. [Retrieved August 7, 2012];Obesity and overweight. 2012 May; from http://www.who.int/mediacentre/factsheets/fs311/en/index.html.
- 36.Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. American Journal of Respiratory and Critical Care Medicine. 1998;158:1384–1387. doi: 10.1164/ajrccm.158.5.9710086. [DOI] [PubMed] [Google Scholar]
- 37.Antunes HKM, Stella SG, Santos RF, Bueno OFA, de Mello MT. Depression, anxiety and quality of life scores in seniors after an endurance exercise program. Brazilian Journal of Psychiatry. 2005;27:266–271. doi: 10.1590/s1516-44462005000400003. [DOI] [PubMed] [Google Scholar]
- 38.Carfarella PA, Effing TW, Usmani ZA, Frith PA. Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: A literature review. Respirology. 2012;17:627–638. doi: 10.1111/j.1440-1843.2012.02148.x. [DOI] [PubMed] [Google Scholar]
- 39.Paddison JS, Effing TW, Quinn S, Frith PA. Fatigue in COPD: Association with functional status and hospitalizations. European Respiratory Journal. 2013;41:565–570. doi: 10.1183/09031936.00021412. [DOI] [PubMed] [Google Scholar]
- 40.Miravitlles M, Izquierdo I, Herrejon A, Torres JV, Bario E, Borja J. COPD severity score as a predictor of failure in exacerbations of COPD. The ESFERA study. Respiratory Medicine. 2011;105:740–747. doi: 10.1016/j.rmed.2010.12.020. [DOI] [PubMed] [Google Scholar]
- 41.Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patient with COPD. Chest. 2002;121:1434–1440. doi: 10.1378/chest.121.5.1434. [DOI] [PubMed] [Google Scholar]