Abstract
Stigmatizing beliefs about mental illness can be a daily struggle for people with schizophrenia. While investigations into the impact of internalizing stigma on negative symptoms have yielded mixed results, resistance to stigmatizing beliefs has received little attention. In this study, we examined the linkage between internalized stigma, stigma resistance, negative symptoms, and social power, or perceived ability to influence others during social interactions among people with schizophrenia. Further, we sought to determine whether resistance to stigma would be bolstered by social power, with greater power in relationships with other possibly buffering against motivation/pleasure negative symptoms. Fifty-one people with schizophrenia or schizoaffective disorder completed measures of social power, internalized stigma, and stigma resistance. Negative symptoms were assessed using the Clinical Assessment Interview for Negative Symptoms (CAINS). Greater social power was associated with less internalized stigma and negative symptoms as well as more stigma resistance. Further, the relationship between social power and negative symptoms was partially mediated by stigma resistance. These findings provide evidence for the role of stigma resistance as a viable target for psychosocial interventions aimed at improving motivation and social power in people with schizophrenia.
Keywords: Internalized stigma, Stigma resistance, Motivation/pleasure
1. Introduction
Two of the biggest barriers and unmet treatment needs in schizophrenia are stigma and negative symptoms. Despite attempts to debunk common misconceptions, the general public often view people with mental illness as violent, incompetent, and responsible for their illness (Corrigan and Kleinlein, 2005). Unfortunately, people with schizophrenia often come to believe that these stigmatizing conceptions about mental illness apply to themselves. Indeed, a survey of over 1300 mental health consumers, including people with schizophrenia, conducted by the National Institute of Mental Health, 60% reported the experience of being avoided or shunned because of their illness and 74% reported having avoided telling people outside of their immediate family about their illness (Wahl, 1999). Furthermore, as many as three-quarters of people with schizophrenia have negative symptoms (Fenton and McGlashan, 1991), and current treatments have limited effects on negative symptom (Leucht et al., 2009; Buchanan, et al., 2010; Elis et al., 2013). In the present study, we examined the linkages between the internalization of and resistance to such stigmatizing beliefs and negative symptoms. We also considered whether social power, or one’s perceived control and influence in relationships, may be associated with the ability to resist such stigma in people with schizophrenia.
Internalization of stigmatizing beliefs involves applying the negative beliefs to oneself, resulting in feelings of shame and devaluation (Corrigan, 1998; Ritsher and Phelan, 2004). This concept is distinct from other stigma-related constructs, such as anticipated discrimination, which focuses on changes in behavior due to the expectation of being discriminated against (Thornicroft et al., 2009; Ucok et al., 2013). Although some studies have found a relationship between internalized stigma and negative symptoms (Lysaker et al., 2009; Hill and Startup, 2013), others have not (Lysaker et al., 2007; Kleim et al., 2008; Park et al., 2012), perhaps reflecting the variety of negative symptom measures used in these studies. The negative symptoms of schizophrenia are most parsimoniously explained by two independent factors: motivation/pleasure and emotional expressivity (Blanchard and Cohen, 2006; Foussias and Remington, 2010; Kring et al., 2013), Motivation/pleasure encompasses the engagement in and pleasure derived from goal-directed behavior across social, vocational, and recreational domains, while expressivity includes the outward expression of emotion via the face and voice (e.g., Kring and Elis, 2013). To date, no study has investigated the relationship between internalized stigma and the two negative symptom domains. However, theoretical and empirical work by Corrigan and colleagues suggests that stigma is associated with motivated behavior (e.g., pursuing a job or educational goals), suggesting a possible link between internalized stigma and the negative symptom domain of motivation/pleasure.
Considerably less is known about stigma resistance, or the experience of being unaffected by stigmatizing attitudes (Sibitz et al., 2011a), in people with schizophrenia. While stigma resistance and internalized stigma might appear to be the opposite poles of the same dimension, the only study that compared the relationship between internalized stigma and stigma resistance found only weak relationships between the two domains (Sibitz et al., 2011a). Even though increasing stigma resistance may not reduce internalized stigma (or vice-versa), bolstering skills to help buffer against stigma may nevertheless help diminish negative outcomes. While no study has directly investigated the relationship between stigma resistance and negative symptoms, the act of resisting stigma could itself be considered a motivated behavior. Indeed, stigma resistance is theorized to involve actively confronting and/or deflecting negative beliefs associated with having mental illness (Thoits, 2011). Further, resistance may help to counteract social isolation common among people who internalized stigma, paving the way for greater motivation and engagement across the different life domains (e.g. work, social relationships).
1.1. Linking stigma and negative symptoms: the role of social power
Sense of power is conceptualized as the perceived ability to control one’s own life. Among people with mental illness, sense of power is related to improved quality of life (Sibitz et al., 2011b), illness recovery (Corrigan et al., 1999), stigma resistance (Lysaker et al., 2008; Sibitz et al., 2011a), and internalized stigma (Vauth et al., 2007; Brohan et al., 2010; Livingston & Boyd, 2010). To our knowledge, only one study has investigated the relationship between sense of power and negative symptoms in people with schizophrenia, finding a non-significant relationship (Vauth et al., 2007), perhaps because the power measure was not sensitive to the contexts associated with negative symptoms, such as social relationships. Indeed, greater sense of power is associated with a larger social network among people with schizophrenia (Rogers et al., 1997; Lundberg et al., 2008). In the present study, we adopted a social conceptualization of power as “the perception of one’s ability to influence another person or other people” (Anderson et al., 2012), what we will refer to as “social power.” This conceptualization focuses sense of power to the social domain, in relation to the other people.
Studies in healthy people suggest that social power is associated with the processes underpinning the negative symptom domains of motivation/pleasure and expressivity (Keltner et al., 2003). That is, healthy people with high social power engage in greater levels of motivated behavior and pursuit of rewards compared to people with low social power (Anderson and Berdahl, 2002). Further, higher social power is associated with greater risk-taking and optimism (Anderson and Galinsky, 2006), which may facilitate goal pursuit. Higher social power is also associated with greater expression and experience of positive emotion (Berdahl and Martorana, 2006), as well as greater production of non-verbal behaviors indicative of social engagement, such as gesturing and eye gaze (Carney et al., 2005).
Investigating the relationship between social power and the internalization of and resistance to stigma may help to elucidate deficits associated with negative symptoms. Indeed, Corrigan et al. (2009) posited that power might mediate the relationship between internalized stigma and motivated pursuit of life goals. That is, people experiencing internalized stigma may be more likely to pursue life goals if they have a greater sense of power. Unpacking the relationship between social power and stigma resistance may further our understanding of the motivation/pleasure domain in schizophrenia. Thoits (2011) hypothesized stigma resistance, regardless of the outcome, increases sense of power. However, might it be the case that having power can increase the ability to resist stigma. That is, in addition to the mediation model proposed by Corrigan and colleagues, stigma resistance may mediate the relationship between social power and motivation/pleasure negative symptoms in people with schizophrenia.
1.2. Present study
Using a multi-method approach, we tested three hypotheses about the linkages between social power, internalized stigma, stigma resistance, and negative symptoms in people with schizophrenia or schizoaffective disorder: (1) greater social power will be associated with lower internalized stigma but greater stigma resistance, (2) greater social power will be associated with fewer motivation/pleasure and expressivity negative symptoms, and (3) greater stigma resistance and lower internalized stigma will be associated with fewer motivation/pleasure and expressivity negative symptoms.
We also sought to test two mediation models based on the results obtained from correlational analyses. First, in line with Corrigan et al. (2009), we tested whether social power would mediate the relationship between internalized stigma and motivation/pleasure negative symptoms. Second, we tested whether stigma resistance would mediate the relationship between social power and motivation/pleasure negative symptoms.
2. Methods
2.1. Participants
Fifty-one people meeting DSM-IV criteria for schizophrenia (n=34) or schizoaffective disorder (n=17) were recruited from outpatient mental health clinics and community advertisements. Participants were between the ages of 18 and 60, had no history of neurological disorders or serious head trauma, were fluent in English, had an estimated IQ 70, and did not meet criteria for depression, mania, hypomania, or substance abuse in the past month or substance dependence in the last six months. Forty-seven people were taking medications; of these, forty-one were taking atypical anti-psychotics.
Trained interviewers confirmed diagnoses using the Structured Clinical Interview for DSM-IV (SCID; First et al., 1996). General symptoms were assessed using the 24-item Brief Psychotic Rating Scale (BPRS; Lukoff et al., 1986). A full-scale IQ estimate was obtained from the Wechsler Test of Adult Reading (WTAR; Wechsler, 2001). Demographic and clinical data are presented in Table 1.
Table 1.
Demographic and clinical variables (n=51).
| Mean (S.D.) | |
|---|---|
| Age | 45.92 (10.6) |
| Education | 14.39 (2.5) |
| Parental education | 14.37 (3.1) |
| Sex (M/F) | 27/24 |
| Number of hospitalizations | 6.98 |
| Duration of illness (years) | 21.85 |
| WTAR FSIQ | 103.83 (15.3) |
| BPRS total score | 43.89 (12.0) |
| CAINS | |
| MAP scale | 14.39 (5.3) |
| EXP scale | 5.80 (3.9) |
| SPS | 34.98 (9.2) |
| ISMIS | |
| Internalized stigma | 2.08 (0.6) |
| Stigma resistance | 2.90 (0.5) |
WTAR=Wechsler Test of Adult Reading, BPRS=Brief Psychotic Rating Scale; CAINS=Clinical Assessment Inventory for Negative Symptoms; MAP=Motivation and Pleasure; EXP=Expression; SPS=Sense of Power Scale; and ISMIS=Internalized Stigma of Mental Illness Scale.
2.2. Measures
2.2.1. Clinical Assessment Interview for Negative Symptoms (CAINS)
We measured negative symptoms with the Clinical Assessment Interview for Negative Symptoms (CAINS; Kring et al., 2013). Interviewers rated engagement in motivated behavior as well as pleasure derived from social, vocational, and recreational activities over the past week using the CAINS Motivation and Pleasure (MAP) scale. The nine MAP items were rated using a 0–4 scale, with higher scores reflecting greater impairment. Interviewers also rated changes in expressivity using the CAINS Expression (EXP) scale. The four EXP items were rated using a 0–4 scale, with higher scores reflecting greater impairment. Internal consistency was good for both scales (MAP: α=0.70; EXP α=0.84).
2.2.2. Internalized Stigma of Mental Illness Scale (ISMIS)
The Internalized Stigma of Mental Illness Scale (ISMIS; Ritsher et al., 2003; Ritsher and Phelan, 2004) is a 29-item self-report questionnaire that assesses self-identification with negative beliefs about mental illness and contains five sub-scales: Alienation, Stereotype Endorsement, Social Withdrawal, Discrimination Experience, and Stigma Resistance. Sample items include: “I feel inferior to others who do not have a mental illness,” and “People can tell that I have a mental illness by the way I look.” Items are rated on a 1 (strongly disagree) to 4 (strongly agree) Likert scale. Sibitz et al., (2011a) found two independent factors for the ISMIS: (1) internalized stigma, which is a composite total of the first four subscales, and (2) stigma resistance. We computed these two scores rather than the individual subscales, with higher scores reflecting great internalized stigma or stigma resistance. Both the internalized stigma (α=0.92) and stigma resistance (α=0.72) scales showed good internal consistency. One person chose not to complete the ISMIS, so analyses involving this scale have a sample of fifty people.
2.2.3. Sense of Power Scale (SPS)
The Sense of Power Scale (SPS; Anderson et al., 2012) is an 8-item questionnaire that assesses perceived social power in the context of relationships with the other people. Sample items include: “I can get others to listen to what I say,” and “If I want to, I get to make decisions.” Participants rated each item on a 1 (disagree strongly) to 7 (agree strongly) Likert scale. The SPS demonstrated good internal consistency (α=0.74).
2.3. Statistical analyses
To test our three hypotheses about the relationships between stigma, social power, and negative symptoms, we computed correlations between Internalized Stigma, Stigma Resistance, SPS, CAINS MAP, and CAINS EXP. Because our data were all collected at the same time point, we were not able to determine temporal precedence of our predictor or mediator variables as is necessary for a true mediation model (Kraemer et al., 2001). We thus conducted mediated path analyses, and following the criteria outlined by Baron and Kenny (1986), we report direct, indirect, and total effects as unstandardized regression coefficients with standard error estimates. Direct effects refer to the effect of the independent variable (X) on the dependent variable (Y); indirect effects refer to the product of the relationship between X and the mediator (M) and the relationship between M and Y; and total effects refer to the sum of the direct and indirect effects. We used 10,000 bootstrap samples to compute bias-corrected 95% confidence intervals for all indirect effects (Preacher and Hayes, 2004). We computed the ratio of indirect to total effect as an indicator of the amount of variance accounted for by the mediator (Shrout and Bolger, 2002).
3. Results
Social power, internalized stigma, and stigma resistance were not significantly related to age, education, duration of illness, number of hospitalizations, or BPRS total scores. There were no differences in any clinical or demographic variables between people with schizophrenia and people with schizoaffective disorder. Thus, in the service of being concise, we will refer to the participants in this study as people with schizophrenia. In addition, men and women did not differ on internalized stigma, stigma resistance, social power, CAINS MAP, or CAINS EXP.
We found support for our first hypothesis (see Table 2). Greater social power was associated with both lower internalized stigma, r (50)= −0.53, p 0.01, and greater stigma resistance, r(50)=0.33 p=0.02. Thus, people with schizophrenia who reported having a greater sense of influence in their relationships with others also reported less internalization of stigma and greater resistance to stigma. We also found support for our second hypothesis. Greater social power was associated with lower scores on the CAINS MAP, r(51)= −0.32, p=0.02 and CAINS EXP scales, r(51)= −0.28, p=0.05 indicating that people who reported more social power had fewer motivation/pleasure and expressivity negative symptoms.
Table 2.
Correlation between social power, internalized stigma, stigma resistance, and negative symptoms.
SPS=Sense of Power Scale; IS=Internalized Stigma; SR=Stigma Resistance; MAP=Motivation and Pleasure; and EXP=Expression.
p 0.05.
p 0.01.
We found partial support for our third hypothesis. Internalized stigma was not associated with either CAINS scale; however, stigma resistance was significantly correlated with the CAINS MAP, r(50)= −0.40, p 0.01, and CAINS EXP scales, r(50)= −0.40, p=0.01. These results suggest that greater resistance to stigma is related to both fewer motivation/pleasure and expressivity negative symptoms in people with schizophrenia.
3.1. Mediated path analyses
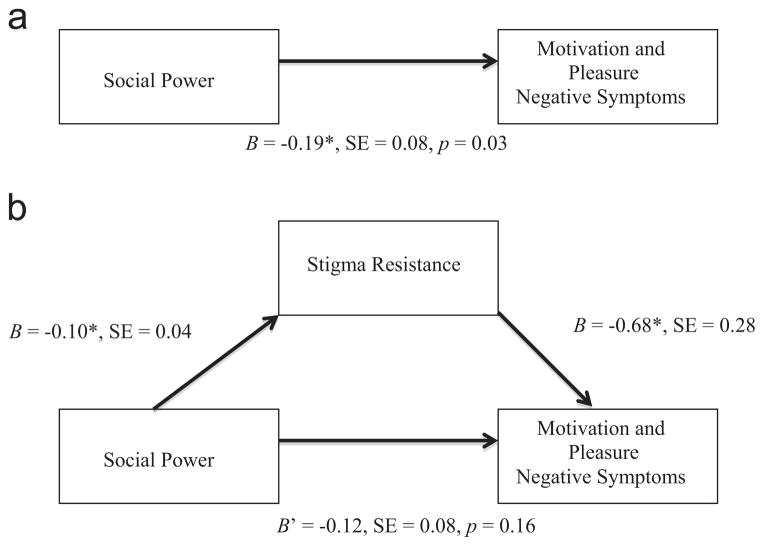
Because internalized stigma was not related to CAINS MAP, we were not able to test whether social power mediated the relationship between internalized stigma and motivation/pleasure negative symptoms as proposed by Corrigan et al. (2009). However, we were able to test whether stigma resistance mediated the relationship between social power and motivation/pleasure negative symptoms. Fig. 1a depicts the significant, direct effect of social power on CAINS MAP scores without stigma resistance in the model. Fig. 1b shows the mediated path analysis with stigma resistance in the model. The coefficient and bootstrap confidence interval for the indirect effect of social power on CAINS MAP scores were B= −0.07, SE=0.04, CI [−0.16 to −0.01]. The ratio of indirect to total effect was 0.37, indicating that stigma resistance accounted for close to half of the effect of social power on motivation/pleasure negative symptoms in people with schizophrenia. Further, the amount of variance explained by the model increased from 0.10 to 0.20 with the addition of stigma resistance, which was significant, F-change(1,48)=5.99, p=0.02.
Fig. 1.
(a) Direct effect of social power (X) on motivation and pleasure negative symptoms (Y). (b) Mediated path model, with the stigma resistance (M) mediating the relationship between social power and motivation and pleasure negative symptoms.
4. Discussion
In this study, we examined the relationship between internalized stigma, stigma resistance, social power, and negative symptoms in people with schizophrenia using both interview and self-report measures. We found four main results. First, greater social power was associated with greater stigma resistance and lower internalized stigma. Second, greater social power was associated with fewer negative symptoms. Third, stigma resistance, but not internalized stigma, was associated with fewer negative symptoms. Fourth, the relationship between social power and motivation/pleasure negative symptoms was partially mediated by reported resistance to stigmatizing beliefs.
Although we adopted a social conceptualization of power (Anderson et al., 2012), our results are consistent with previous studies that found greater reported power was associated with less reported stigma in people with schizophrenia (Lysaker et al., 2008; Brohan et al., 2010; Livingston and Boyd, 2010). Thus, our results add to the existing literature on power and stigma by showing that both the internalization of and resistance to stigmatizing beliefs are linked with power, specifically in the context of social relationships. Having a sense of control in social relationships is beneficial for all the people, but this may be particularly important for people with schizophrenia who often have interpersonal difficulties for a variety of reasons (e.g., poor social skills, anxiety, and isolation).
We further extend the literature by showing that greater social power is associated with fewer motivation/pleasure and expressivity negative symptoms, which is broadly consistent with previous findings in healthy people, at least within the domains of motivated behavior and expression of positive emotion (Anderson and Berdahl, 2002; Keltner et al., 2003; Anderson and Galinsky, 2006;). Previous research has linked decreased expressivity in schizophrenia to interpersonal relationship difficulties (see Kring and Moran, 2008 for review). Our results show that social power is a psychological correlate of expressivity and future studies might test whether social power mediates the relationship between expressivity and relationship quality in people with schizophrenia. The relationship between social power and the motivation/pleasure domain of negative symptoms is particularly noteworthy and has implications for our understanding of decreased social engagement among people with schizophrenia. Specifically, these findings suggest that one possible reason people with schizophrenia do not frequently seek out social interactions is because of a perceived inability to be heard in social relationships or to influence other people. Thus, skills related to confidence and even assertiveness during social interactions (e.g. Bellack et al., 2004) may not only help to promote social engagement in people with schizophrenia, but also help to reduce motivation/pleasure negative symptoms.
Contrary to expectations, we did not find a significant relationship between internalized stigma and negative symptoms in people with schizophrenia. While this is consistent with previous studies (Lysaker et al., 2007; Kleim et al., 2008; Park et al., 2012), others have reported a significant positive relationship between internalized stigma and negative symptoms (Lysaker et al., 2009; Hill and Startup, in press). In addition, unlike Sibitz et al. (2011a) who found a weak, but significant relationship between internalized stigma and stigma resistance, we found no relationship between these factors. Taken together, these findings suggest that stigma resistance may be a separate and distinct intervention target from internalized stigma. Further, by distinguishing stigma resistance and internalized stigma, we were able to demonstrate that only stigma resistance is associated with fewer negative symptoms – both motivation/pleasure and expressivity. Taken together, our results help to clarify the relationship between stigma and negative symptoms and point to the potential of stigma resistance as an intervention target in people with schizophrenia (Sibitz et al., 2011a), an area that up until now has received little attention.
While previous theoretical models have conceptualized power as a potential mediator between internalized stigma and pursuit of life goals (Corrigan et al., 2009), our results suggest that the relationship between social power and motivation/pleasure negative symptoms in people with schizophrenia is at least partially explained by resistance to stigmatized beliefs. In people with mental illness, resistance to stigmatizing beliefs can occur in the form of actively challenging or deflecting these negative beliefs (Thoits, 2011). While avoidance and withdrawal are common maladaptive coping strategies for dealing with stigma (Ritsher and Phelan, 2004), one in five mental health consumers reported actively challenging people who make disparaging remarks about mental illness, and 18% of those surveyed indicated that challenging stigmatized beliefs increased their feelings of power (Wahl, 1999). Thus, interventions aimed at increasing stigma resistance techniques (e.g., challenge not withdrawal) have the potential to increase feelings of social power by helping consumers take control of their interpersonal lives and promote greater engagement in everyday activities by helping to debunk negative beliefs about mental illness.
Interventions aimed at reducing internalized stigma among people with schizophrenia have had limited success. Indeed, a recent review found that only 2 of the 7 interventions targeting stigma in people with schizophrenia showed significant decreases in reported internalized stigma post-treatment (Mittal et al., 2012). However, as our and other findings (Sibitz et al., 2011a) have suggested, internalized stigma and stigma resistance are independent, which leaves open the possibility that interventions seeking to bolster stigma resistance may succeed. Given the relationship between stigma resistance and both negative symptom domains, this appears to be a valuable intervention target. That is, increasing the use of stigma resistance may help to mitigate both motivation/pleasure and expressivity negative symptoms common among people with schizophrenia. To our knowledge, there have been no interventions that have specifically targeted improving stigma resistance among people with schizophrenia, or mental illness in general. While survey results suggest that about 1 in 5 people with mental illness may already actively resist stigma, our findings provide an initial framework for interventions aimed at increasing resistance. For example, increasing feelings of social power among people with schizophrenia may help to increase stigma resistance. While measures of power have been used as treatment outcomes, stigma interventions have yet to specifically target feelings of power in general, or more specifically in the context of social relationships.
As with any study, it is important to acknowledge some limitations. First, our study is the first to adopt the construct of social power for investigations into people with schizophrenia. While our measure showed strong internal consistency, future studies should seek to replicate our findings regarding social power. Second, since our sample size was just short of the established convention of having a 20:1 participant to model parameter ratio (Kline, 2005), we limited our path analyses to three parameters. Thus, it remains unclear if including other variables would have increased the explanatory ability of our model. Finally, while we chose to focus our investigation on negative symptoms, particularly in the motivation/pleasure domain, some studies have also found significant relationships between internalized stigma and positive symptoms (e.g. Lysaker et al., 2007), though our study and others (e.g. Vauth et al., 2007) have not. These mixed findings suggest the need for further research on linkages between internalized stigma, stigma resistance, and all types of schizophrenia symptoms.
In summary, we found that greater social power was associated with less internalized stigma, fewer negative symptoms, and greater stigma resistance in people with schizophrenia. Further, we found that stigma resistance partially mediated the relationship between social power and motivation/pleasure negative symptoms, such that people with schizophrenia who have more social power will exhibit fewer motivation/pleasure negative symptoms if they report greater stigma resistance. Taken together, our findings point to stigma resistance as a possible intervention target to help ameliorate negative symptoms in schizophrenia.
Acknowledgments
Funding
US National Institutes of Mental Health Grant 5T32MH089919 to TRC and 1R01MH082890 to AMK.
We would like to thank Ori Elis, Erin Moran, and Jasmine Mote for their assistance in data collection. We would also like to thank the people who participated in the study.
References
- Anderson C, Berdahl JL. The experience of power: examining the effects of power on approach and inhibition tendencies. Journal of Personality and Social Psychology. 2002;83:1362–1377. [PubMed] [Google Scholar]
- Anderson C, Galinsky AD. Power, optimism, and risk-taking. European Journal of Social Psychology. 2006;36:511–536. [Google Scholar]
- Anderson C, John OP, Keltner D. The personal sense of power. Journal of Personality. 2012;80 (2):313–344. doi: 10.1111/j.1467-6494.2011.00734.x. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bellack AS, Mueser KT, Gingerich S, Agresta J. Social Skills Training for Schizophrenia: A Step-by-Step Guide. Guilford Press; New York: 2004. [Google Scholar]
- Berdahl JL, Martorana P. Effects of power on emotion and expression during a controversial group discussion. European Journal of Social Psychology. 2006;36:497–509. [Google Scholar]
- Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophrenia Bulletin. 2006;32:238–245. doi: 10.1093/schbul/sbj013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brohan E, Elgie R, Sartorius N, Thornicroft G. Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophrenia Research. 2010;122:232–238. doi: 10.1016/j.schres.2010.02.1065. [DOI] [PubMed] [Google Scholar]
- Buchanan RW, Kreyenbuhl J, Kelly DL, Noel JM, Boggs DL, Fischer BA, Himelhoch S, Fang B, Peterson E, Aquino PR, Keller W. The 2009 PORT psychopharmacological treatment recommendations and summary statements. Schizophrenia Bulletin. 2010;36:71–93. doi: 10.1093/schbul/sbp116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney DR, Hall JA, LeBeau LS. Beliefs about the nonverbal expression of social power. Journal of Nonverbal Behavior. 2005;29:105–123. [Google Scholar]
- Corrigan PW. The impact of stigma in severe mental illness. Cognitive and Behavioral Practice. 1998;5:201–222. [Google Scholar]
- Corrigan PW, Giffort D, Rashid F, Leary M, Okeke I. Recovery as a psychological construct. Community Mental Health Journal. 1999;35:231–239. doi: 10.1023/a:1018741302682. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Kleinlein P. The impact of mental illness stigma. In: Corrigan PW, editor. On the Stigma of Mental Illness: Implications for Research and Social Change. The American Psychological Association; Washington: 2005. [Google Scholar]
- Corrigan PW, Larson JE, Rüsch N. Self-stigma and the “why try” effect: impact on life goals and evidence-based practices. World Psychiatry. 2009;8:75–81. doi: 10.1002/j.2051-5545.2009.tb00218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elis O, Caponigro JM, Kring AM. Psychosocial treatments for negative symptoms in schizophrenia: current practices and future directions. Clinical Psychology Reviews. 2013;33:914–928. doi: 10.1016/j.cpr.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenton WS, McGlashan TH. Natural history of schizophrenia subtypes II: positive and negative symptoms and long-term course. Archives of General Psychiatry. 1991;48:978–986. doi: 10.1001/archpsyc.1991.01810350018003. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. Biometrics Research; New York: 1996. Patient Edition. [Google Scholar]
- Foussias G, Remington G. Negative symptoms in schizophrenia: avolition and Occam’s razor. Schizophrenia Bulletin. 2010;36:359–369. doi: 10.1093/schbul/sbn094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill K, Startup M. The relationship between internalized stigma, negative symptoms and social functioning in schizophrenia: the mediating role of self-efficacy. Psychiatry Research. 2013;206:151–157. doi: 10.1016/j.psychres.2012.09.056. [DOI] [PubMed] [Google Scholar]
- Keltner D, Gruenfeld DH, Anderson C. Power, approach, and inhibition. Psychological Review. 2003;110:265–284. doi: 10.1037/0033-295x.110.2.265. [DOI] [PubMed] [Google Scholar]
- Kleim B, Vauth R, Adam G, Stieglitz RD, Hayward P, Corrigan P. Perceived stigma predicts low self-efficacy and poor coping in schizophrenia. Journal of Mental Health. 2008;17:482–491. [Google Scholar]
- Kline RB. Principles and Practices of Structural Equation Modeling. Guilford Press; New York: 2005. [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Kring AM, Elis O. Emotion deficits in people with schizophrenia. Annual Review of Clinical Psychology. 2013;9:409–433. doi: 10.1146/annurev-clinpsy-050212-185538. [DOI] [PubMed] [Google Scholar]
- Kring AM, Gur R, Blanchard J, Horan WP, Reise S. The clinical assessment interview for negative symptoms (CAINS): final development and validation. American Journal of Psychiatry. 2013;170:165–172. doi: 10.1176/appi.ajp.2012.12010109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Moran EK. Emotional response deficits in schizophrenia: Insights from affective science. Schizophrenia Bulletin. 2008;34:819–834. doi: 10.1093/schbul/sbn071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Social Science and Medicine. 2010;71:2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. The Lancet. 2009;373:31–41. doi: 10.1016/S0140-6736(08)61764-X. [DOI] [PubMed] [Google Scholar]
- Lundberg B, Hansson L, Wentz E, Björkman T. Stigma, discrimination, empowerment and social networks: a preliminary investigation of their influence on subjective quality of life in a Swedish sample. International Journal of Social Psychiatry. 2008;54:47–55. doi: 10.1177/0020764007082345. [DOI] [PubMed] [Google Scholar]
- Lukoff D, Nuechterlein KH, Ventura J. Manual for the expanded Brief Psychotic Rating Scale. Schizophrenia Bulletin. 1986:594–602. [Google Scholar]
- Lysaker PH, Roe D, Yanos PT. Toward understanding the insight paradox: internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophrenia Bulletin. 2007;33:192–199. doi: 10.1093/schbul/sbl016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lysaker PH, Vohs JL, Tsai J. Negative symptoms and concordant impairments in attention in schizophrenia: associations with social functioning, hope, self-esteem and internalized stigma. Schizophrenia Research. 2009;110:165–172. doi: 10.1016/j.schres.2009.01.015. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Tsai J, Yanos P, Roe D. Associations of multiple domains of self-esteem with four dimensions of stigma in schizophrenia. Schizophrenia Research. 2008;98:194–200. doi: 10.1016/j.schres.2007.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal D, Sullivan G, Chekuri L, Allee E, Corrigan PW. Empirical studies of self-stigma reduction strategies: a critical review of the literature. Psychiatric Services. 2012;63:974–981. doi: 10.1176/appi.ps.201100459. [DOI] [PubMed] [Google Scholar]
- Park SG, Bennett ME, Couture SM, Blanchard JJ. Internalized stigma in schizophrenia: relations with dysfunctional attitudes, symptoms, and quality of life. Psychiatry Research. 2012;205:43–47. doi: 10.1016/j.psychres.2012.08.040. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Research. 2003;121:31–49. doi: 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Research. 2004;129:257–265. doi: 10.1016/j.psychres.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatric Services. 1997;48:1042–1047. doi: 10.1176/ps.48.8.1042. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Sibitz I, Unger A, Woppmann A, Zidek T, Amering M. Stigma resistance in patients with schizophrenia. Schizophrenia Bulletin. 2011a;37:316–323. doi: 10.1093/schbul/sbp048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibitz I, Amering M, Unger A, Seyringer ME, Bachmann A, Schrank B, Benesch T, Schulze B, Woppmann A. The impact of the social network, stigma and empowerment on the quality of life in patients with schizophrenia. European Psychiatry. 2011b;26:28–33. doi: 10.1016/j.eurpsy.2010.08.010. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Resisting the stigma of mental illness. Social Psychology Quarterly. 2011;74:6–28. [Google Scholar]
- Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. The Lancet. 2009;373:408–415. doi: 10.1016/S0140-6736(08)61817-6. [DOI] [PubMed] [Google Scholar]
- Üçok A, Karadayı G, Emirolu B, Sartorius N. Anticipated discrimination is related to symptom severity, functionality and quality of life in schizophrenia. Psychiatry Research. 2013;209:333–339. doi: 10.1016/j.psychres.2013.02.022. [DOI] [PubMed] [Google Scholar]
- Vauth R, Kleim B, Wirtz M, Corrigan PW. Self-efficacy and empowerment as outcomes of self-stigmatizing and coping in schizophrenia. Psychiatry Research. 2007;150:71–80. doi: 10.1016/j.psychres.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Wahl OF. Mental health consumers’ experience of stigma. Schizophrenia Bulletin. 1999;25:467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Test of Adult Reading. Psychological Corporation; London: 2001. [Google Scholar]