Abstract
Background
Previous studies assessing the validity of adolescent self-reported height and weight for estimating obesity prevalence have not accounted for potential bias due to non-response in self-reports.
Objectives
The purpose of this study was to assess the implications of selective non-response in self-reports of height and weight for estimates of adolescent obesity.
Methods
The authors analyzed 613 adolescents ages 12-17 from the 2006-08 Los Angeles Family and Neighborhood Survey, a longitudinal study of Los Angeles County households with an oversample of poor neighborhoods. Obesity prevalence estimates based on (1) self-report, (2) measured height and weight for those who did report, and (3) measured height and weight for those who did not report were compared.
Results
Among younger teens, measured obesity prevalence was higher for those who did not report height and weight compared to those who did (40% vs. 30). Consequently, obesity prevalence based on self-reported height and weight underestimated measured prevalence by 12 percentage points (when accounting for non-response) vs. 9 percentage points (when non-response was not accounted for). Results were robust to the choice of difference child growth references (i.e,, CDC vs. International Obesity Task Force).
Discussion
Adolescent obesity surveillance and prevention efforts must take into account selective non-response for self-reported height and weight, particularly for younger teens. Results should be replicated in a nationally-representative sample.
Keywords: Adolescent, Obesity, Self Report
INTRODUCTION
There is growing concern about the rising prevalence of child and adolescent obesity (Adair, 2008; Hedley et al., 2004; Ogden, Flegal, Carroll, & Johnson, 2002). Obesity is associated with increased risk of chronic disease, and with excess disability, morbidity, and mortality. Among children and adolescents, increasing obesity has been linked to rising rates of Type 2 diabetes and other conditions associated with the metabolic syndrome (Dietz, 1998; Fagot-Campagna, 2000). Obese children tend to remain obese into adulthood (Serdula et al., 1993); therefore, the increasing prevalence of childhood and adolescent obesity is likely to drive adult prevalence, and its associated financial and health burden, for decades to come.
Accurate measurement of childhood and adolescent obesity prevalence is an important component of surveillance and prevention efforts. While some population surveys such as the National Health and Nutrition Survey (NHANES) collect anthropometric measures in the field, others such as the National Health Interview Survey (NHIS) and the Youth Risk Behavior Survey (YRBS) rely on self-reported height and weight. As attention to obesity grows, more surveillance and survey programs are likely to include self-reported height and weight.
An extensive literature has documented consistent biases in adult self-reports (Gorber, Tremblay, Moher, & Gorber, 2007; Lee, 2005; Nyholm et al., 2007; Spencer, Appleby, Davey, & Key, 2007): respondents typically overestimate height and underestimate weight, thereby underestimating BMI and obesity prevalence. The direction and extent of bias in self-reports vary by age, gender, and body size. A much smaller number of adolescent validity studies are less conclusive (Brener, McManus, Galuska, Lowry, & Wechsler, 2003; Fortenberry, 1992; Sherry, Jefferds, & Grummer-Strawn, 2007; Strauss, 1999), but suggest that adolescent self-reports also bias obesity prevalence downward, due to consistent underestimation of weight and, for some groups, overestimation of height. As with adults, error in adolescents’ self-reports is associated with sociodemographic and anthropometric characteristics.
Few studies have systematically examined another important source of bias when using self-reports to calculate adolescent BMI: the non-random failure to report height and weight in a survey setting. Failure to report may occur for many reasons. Adolescents, particularly at younger ages, may not know their current height and weight due to recent growth spurts. Limited healthcare access may yield fewer opportunities to be weighed or measured in a clinical setting. Parents, particularly those with lower levels of education, may be less concerned with monitoring children's height and weight. Adolescents who are uncomfortable with their body size may be reluctant to reveal height or weight. If the correlates of failure to report anthropometry also predict higher body mass, then obesity prevalence calculated from adolescent self-reports will suffer additional downward bias, further compromising its validity.
The objective of this study was to assess the degree to which self-reports of height and weight result in underestimation of adolescent obesity among different adolescent subgroups, with a novel focus on the impact of failure to report height and weight.
METHODS
Study design and analytic sample
This study uses the Los Angeles Family and Neighborhood Survey (L.A.FANS), a longitudinal study of approximately 3,000 households in Los Angeles County. The first wave of L.A.FANS was conducted in 2000-2001 in a stratified probability sample of 65 neighborhoods (census tracts) in Los Angeles County with oversamples in high-poverty census tracts (Sastry, Ghosh-Dastidar, Adams, & Pebley, 2006). In each sampled household, a randomly selected child or teen was interviewed, as well as a randomly selected sibling of the focal child. L.A.FANS-2, used in this analysis, was collected between August 2006 and December 2008. All eligible L.A.FANS-1 households still living within Los Angeles County were re-contacted and re-interviewed, and a sample of new residents in the original 65 census tracts was added. Of the 2466 eligible child respondents from L.A.FANS-1, 1573 (64%) were re-interviewed for L.A.FANS-2, with an additional 314 new entrants (Peterson et al., 2011).
Adolescents ages 12 and older were interviewed directly via audio computer-assisted self-interview (audio CASI) and were asked to report their height and weight. They were later measured and weighed by trained interviewers using standard procedures. Detailed sociodemographic data were also collected for all adolescent respondents. L.A.FANS was reviewed and approved by the Institutional Review Boards of the University of California, Los Angeles, RAND, and RTI International. Adolescent respondents provided informed consent.
For the present study, we focus on the 626 non-Hispanic white, non-Hispanic black and Hispanic respondents ages 12-17 in the L.A.FANS-2 sample. We excluded 13 cases due to pregnancy or illness affecting height and weight (5) or to missing anthropometric or sociodemographic measures (8). For the remaining analytic sample of 613 respondents, analyses were conducted using the largest sample size possible. For height analyses, 573 respondents had measured height (of whom 494 also had self-reported height and 831 did not) and 36 had self-reported but not measured height. Of the same 613 respondents, 573 had measured weight (of whom 513 also had self-reported weight and 60 did not), and 40 had self-reported but not measured weight.
Study variables
Outcome variables were constructed from measured and self-reported height and weight. Adolescents who refused to provide a self-report, or replied “don’t know” to the prompt for height or weight, were coded as failing to report. These two responses were combined because adolescents may choose “don’t know” when they are in fact refusing and conversely may refuse to report when they do not know their height and weight. Exploratory analysis indicated no differences in the predictors of “don’t know” vs. refused responses.
Dichotomous variables were created to indicate whether the adolescent overestimated or underestimated height and weight by more than 3%. Analyses using larger and smaller cutoffs yielded similar results. Error in self-reports was calculated as the absolute value of self-reported minus measured value. Body mass index (BMI in units of kg/m2) was calculated from measured height and weight (“measured BMI”) and also from self-reported height and weight (“self-reported BMI”). Obesity was defined using the CDC pediatric cutoff of the 95th percentile of sex-specific BMI-for-age from the 2000 NCHS growth reference charts.. (Ogden, Kuczmarski, et al., 2002) Age- and sex-standardized height-for-age and BMI-for-age z-scores were also calculated using the 2000 NCHS growth references charts (Kuczmarski, Ogden, & Guo, 2002). Z-scores were used to control for child height and BMI in models predicting error in self-reports and failure to report. Height-for-age and BMI-for-age were dichotomized in the final stage of the analysis, with tall-for-age respondents defined as above the median height-for-age, and high BMI-for-age respondents defined as above the median BMI-for-age.
Sociodemographic controls included gender, age, race/ethnicity, insurance status, and mother's education. Race/ethnicity was categorized as non-Hispanic white (hereafter, white), Hispanic, or non-Hispanic black (hereafter, black). Asian and other race/ethnic groups were not included in the analysis due to small sample sizes. Insurance status was based on the respondent's primary caregiver's report of whether the child was covered by health insurance in the month preceding the interview. Mother's educational status was dichotomized as less than the completion of high school vs. completion of high school or additional education.
Statistical analyses
Multiple logistic and linear regression models were used to examine the correlates of bias in self-reported height and weight. The first set of analyses examined which adolescents failed to report height and weight, using all adolescents in the sample with measured height and weight. The second set of analyses estimated the predictors of underestimation and overestimation of height and weight (by at least 3%). In the third set of models, OLS regression was used to estimate the magnitude of the error in self-reported height and weight. The second and third sets of models included only those respondents with both measured and self-reported height and weight, and thus have smaller sample sizes than the first set. All models included the following sociodemographic predictors: age, gender, race/ethnicity, insurance status of the child, and mother's education. Height-for-age z-score was included as a predictor in height models; weight models included BMI-for-age z-score.
The last analysis compared four estimates of obesity prevalence, based on (1) self-reported BMI; (2) measured BMI for respondents with self-reported BMI; (3) measured BMI for respondents without self-reported BMI; and (4) measured BMI for all measured respondents (the pooled sample of groups (2) and (3)). The validity or sensitivity of self-reported BMI is obtained by comparing (1) vs. (2) using McNemar's test for paired proportions. Differences in obesity prevalence between those who did and did not provide self-reports are revealed in a comparison of (2) vs. (3) using a two-sample test of proportions. The magnitude of the bias from these 2 sources combined is captured in the comparison of (4) vs. (1) using a maximum likelihood test of differences for overlapping samples. All statistical analyses were conducted using Stata 12.0 (Stata Corporation, College Station, Texas).
RESULTS
Descriptive statistics for the analytic sample are presented in Table 1, separately for younger and older adolescents. While average measured BMI was slightly lower for younger vs. older adolescents (23.6 vs. 24.7 kg/m2), obesity prevalence was higher among the younger group (33% vs 26%) according to the CDC obesity definition. Failure to report height and weight was more common among younger adolescents, with 23% failing to report height and 16% failing to report weight. In contrast, only 9% and 6% of older adolescents failed to report height and weight, respectively. Young respondents were also more likely to both overestimate and underestimate height and weight, compared to older teens, and to have larger errors in their reports.
Table 1.
Sociodemographic, Anthropometric, and Data Completion Characteristics, Los Angeles County Adolescents, 2006-08.
| Age 12-13 Mean or proportion (SD) | Age 14-17 Mean or proportion (SD) | |
|---|---|---|
| Male | 0.54 | 0.50 |
| Age in years | 12.5 (0.5) | 15.5 (1.0) |
| Mothers education < high school | 0.46 | 0.42 |
| Child had health insurance last month | 0.81 | 0.82 |
| Race/ethnicity | ||
| Non-Hispanic White | 0.14 | 0.18 |
| Hispanic | 0.80 | 0.74 |
| Black | 0.06 | 0.08 |
| Measured BMI (kg/m2) | 23.6 (6.3) | 24.7 (6.1) |
| Weight status based on measured BMI | ||
| Obese | 0.33 | 0.26 |
| Overweight | 0.19 | 0.17 |
| Normal/underweight | 0.48 | 0.57 |
| Self-report of body measurements | ||
| Fail to report height | 0.22 | 0.09 |
| Fail to report weight | 0.16 | 0.06 |
| Self-reported BMI (kg/m2) | 21.8 (5.3) | 23.9 (5.3) |
| Weight status based on self-reported BMI | ||
| Obese | 0.22 | 0.19 |
| Overweight | 0.19 | 0.19 |
| Normal/underweight | 0.59 | 0.63 |
| Error in self-reported height | ||
| Underestimate by > 3% | 0.13 | 0.07 |
| Overestimate by > 3% | 0.15 | 0.10 |
| Absolute value of error (cm.) | 4.7 (7.3) | 3.3 (3.7) |
| Error in self-reported weight | ||
| Underestimate by > 3% | 0.52 | 0.34 |
| Overestimate by > 3% | 0.14 | 0.17 |
| Absolute value of error (kg.) | 4.2 (6.6) | 3.5 (4.7) |
| Completeness of anthropometric measures | ||
| Has measured and self-reported height and weight | 0.68 | 0.82 |
| Has measured but not reported height and weight | 0.28 | 0.11 |
| Has self-reported but not measured height and weight | 0.05 | 0.07 |
| Maximum (N)a | 216 | 397 |
Maximum (N) represents maximum number of respondents in each age group. Some respondents do not report height and/or weight, or are missing measured values of height and/or weight. See text for details.
Odds ratios for models predicting non-response are presented in Column 1 of Table 2. For both height (top panel) and weight (bottom panel), a one-year increase in age significantly reduced the odds of failing to report by one-third (OR=0.67, 95% CI 0.57,0.79 for height; OR = 0.67, 95% CI: 0.56, 0.80 for weight). Hispanic and black adolescents had significantly higher odds of failing to report height, but not weight, than whites (OR=5.96, 95% CI 1.37,25.87 for Hispanics; OR = 7.91, 95% CI: 1.43, 43.73 for blacks). Adolescents whose mothers did not complete high school had almost double the odds (OR=1.86, 95% CI 1.09, 3.17) of failing to report height compared to teens with more educated mothers.
Table 2.
Failure to Report and Errors in Self-Reported Height and Weight, Los Angeles County Adolescents (2006−8).
| (1) | (2) | (3) | (4) | |||||
|---|---|---|---|---|---|---|---|---|
| Odds ratios and confidence intervals from logistic models | Coefficients and confidence intervals from OLS model | |||||||
| Fail to report | Overestimate by >3% | Underestimate by >3% | Absolute value of error (measured-self report) | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | P | 95% CI | |
| Height in cm.a | ||||||||
| Height-for-age z-score | 0.89 | 0.70, 1.14 | 0.71 | 0.53, 0.93* | 1.04 | 0.77, 1.42 | −.19 | −.63, 0.24 |
| Age (in Years >12) | 0.67 | 0.57, 0.79** | 0.78 | 0.65, 0.95* | 0.79 | 0.64, 0.97* | −.47 | −.77, −.18** |
| Male | 0.96 | 0.59, 1.58 | 1.04 | 0.58, 1.86 | 1.88 | 0.96, 3.66 | 0.48 | −.44, 1.40 |
| Hispanic ethnicity | 5.96 | 1.37, 25.87* | 4.97 | 1.45, 17.00* | 3.70 | 1.06, 12.97* | 1.84 | 0.54, 3.15** |
| Black | 7.91 | 1.43, 43.73* | 2.15 | 0.34, 13.68 | 4.42 | 0.92, 21.26 | 1.17 | −.88, 3.21 |
| Not insured | 1.33 | 0.75, 2.36 | 0.94 | 0.46, 1.94 | 0.85 | 0.36, 2.02 | −.16 | −1.37, 1.05 |
| Mother's education < High school | 1.86 | 1.09, 3.17* | 0.80 | 0.44, 1.44 | 0.88 | 0.45, 1.75 | 0.17 | −.85, 1.20 |
| Constant | 3.26 | 1.86, 4.66** | ||||||
| Nb | 577 | 494 | 494 | 494 | ||||
| Weight in kg.a | ||||||||
| BMI-for-age z-score | 1.10 | 0.84, 1.45 | 0.43 | 0.33, 0.55** | 1.97 | 1.60, 2.42** | 1.47 | 1.04, 1.89** |
| Age (in Years >12) | 0.67 | 0.56, 0.80** | 1.06 | 0.90, 1.23 | 0.80 | 0.71, 0.89** | −.24 | −.51, 0.03 |
| Male | 0.86 | 0.49, 1.51 | 1.84 | 1.09, 3.09* | 0.72 | 0.49, 1.07 | 0.29 | −.62, 1.20 |
| Hispanic ethnicity | 1.89 | 0.61, 5.87 | 1.30 | 0.64, 2.67 | 1.14 | 0.63, 2.04 | −.25 | −1.58, 1.08 |
| Black | 3.73 | 0.91, 15.32 | 2.41 | 0.87, 6.70 | 1.26 | 0.50, 3.14 | 1.27 | −.83, 3.37 |
| Not insured | 1.34 | 0.69, 2.61 | 1.01 | 0.49, 2.12 | 0.94 | 0.57, 1.54 | 0.29 | −0.90, 1.48 |
| Mother's education < High school | 1.58 | 0.85, 2.95 | 0.74 | 0.41, 1.33 | 1.11 | 0.72, 1.70 | 0.57 | −0.44, 1.57 |
| Constant | 2.77 | 1.41, 4.14** | ||||||
| Nb | 573 | 513 | 513 | 513 | ||||
p < .05
p < .01.
Reference groups for dichotomous variables: Male (female); Hispanic, black (white); Not insured (insured); Mother's education < high school (mother's education high school or above).
See text for sample size explanations.
Systematic errors in self-reports were also found. Misreporting of weight was very sensitive to BMI: adolescents reduced their odds of overestimating weight by more than half (OR=0.43, 95% CI 0.33,0.55) and doubled their odds of underestimating weight (OR=1.97, 95% CI 1.60, 2.42) for each standard deviation increase in the BMI-for-age score. Increasing age was associated with lower odds of overestimating and underestimating height (Columns 2 and 3, top panel, OR=0.78, 95% CI 0.65,0.99 for overestimation; OR = 0.79, 95% CI: 0.64, 0.97 for underestimation). Older age was also associated with lower odds of underestimation of weight (Column 3, bottom panel, OR=0.80, 95% CI 0.71, 0.89). A notable result was the large and significant odds ratios for overestimation and underestimation of height by Hispanics (OR=4.97, 95% CI 1.45, 17.00 for overestimation; OR = 3.70, 95% CI: 1.06, 12.97 for underestimation)
Column 4 reports results from the OLS models predicting the absolute value of error in self reports. The constant term represents the error for 12-year-old white girls with insurance, mothers with high school or higher education, and height-for-age or BMI-for-age z-scores of 0. This reference group misestimated height by about 3.3 centimeters and weight by about 2.8 kilograms. Size of error did not change with increased height-for-age, but increased with larger BMI-for-age (β = 1.47, 95% CI 1.04, 1.89). Each additional year of age significantly improved the precision of self-reported height, by an average of almost a half centimeter (β = -0.47, 95% CI -0.77, -0.18). Consistent with their higher odds of both underestimating and overestimating height, Hispanics had a significantly larger height error (β = 1.84, 95% CI 0.54, 3.15) compared to whites.
Taken together, the models in Table 2 indicate several important sources of systematic bias in obesity estimates based on self-reports. In general, younger adolescents failed to report height or weight more frequently than their counterparts, and would therefore be disproportionately excluded from estimates based on self-reports. Young teens also had more frequent and larger errors in self-reported height, and more frequent underestimation of weight, reducing the precision of self-reported BMI in this group. Hispanic adolescents had higher odds of failing to report height and, when they did report height, to report with more error.
The tendency for shorter (for age) teens to overestimate height and heavier (for age) teens to underestimate weight will bias downward estimates of obesity prevalence calculated from self-reported height and weight. The magnitude of this bias is demonstrated in Table 3 with four estimates of obesity prevalence for all adolescents and then for each subgroup of interest. The proportion of the 471 adolescents with both measured and self-reported height and weight who were classified as obese based on self-reports was 0.20 (column 1, 95% CI 0.16, 0.24). The estimated prevalence for the same 469 respondents based on measured height and weight was 0.28, 8 percentage points (40%) higher and a significant difference (column 2, 95% CI 0.23, 0.32). Among the 102 adolescents who did not report height and weight, however, obesity prevalence based on measured BMI was even higher at .32 (column 3, 95% CI 0.23, 0.423). For all 573 adolescents with measured height and weight, the prevalence was .29 (column 4, 95% CI 0.25, 0.33). These estimates suggest that self-reported obesity was underestimated by 9 percentage points (column 4 – column 1), rather than by the 8 percentage points that would be calculated in a validity study based on respondents with both measured and self-reported anthropometry (column 2 – column 1).
Table 3.
Obesity Prevalence Based on Self-reported and Measured Height and Weight, Los Angeles County Adolescents (2006-8).
| NOTE: UNWEIGHTED RESULTS, CDC OBESITY CUTOFFS. PROBLEM: RESULTS ARE NOT WEIGHTED, BUT I BELIEVE THIS IS A BETTER APPROACH AS THE TESTS OF SIGNIFANT DIFFERENCES ARE MORE ACCURATE, WHICH IS THE CRUX OF THE PAPER MORE THAN THE ABSOLUTE PREVALENCE NUMBERS. | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |||||||||
| Based on self-reported height and weighta | Based on measured height and weight | |||||||||||
| Respondent has self-reported height and weight | Respondent does not have self-reported height and weight | All measured respondents | ||||||||||
| Prop. obese | 95% Confidence Interval | (N) | Prop. obese | 95% Confidence Interval | (N) | Prop. obese | 95% Confidence Interval | (N) | Prop. obese | 95% Confidence Interval | (N) | |
| All respondents | 0.20 | 0.16, 0.23 | (471) | 0.28* | 0.24, 0.32 | (471) | 0.32 | 0.23, 0.42 | (102) | 0.29* | 0.25, 0.33 | (573) |
| Ages 12-13 | 0.21 | 0.15, 0.29 | (145) | 0.30* | 0.23, 0.39 | (145) | 0.40 | 0.28, 0.53 | (60) | 0.33* | 0.27, 0.40 | (205) |
| Ages 14-17 | 0.19 | 0.15, 0.23 | (326) | 0.27* | 0.22, 0.32 | (326) | 0.21 | 0.10, 0.37 | (42) | 0.26* | 0.22, 0.31 | (368) |
| Short-for-age | 0.15 | 0.10, 0.20 | (238) | 0.24* | 0.18, 0.29 | (238) | 0.17 | 0.08, 0.31 | (46) | 0.23* | 0.18, 0.28 | (284) |
| Tall-for-age | 0.24 | 0.19, 0.31 | (233) | 0.33* | 0.27, 0.39 | (233) | 0.45 | 0.31, 0.59 | (56) | 0.35* | 0.30, 0.41 | (289) |
| High BMI-for-ageb | 0.40 | 0.33, 0.46 | (231) | 0.57* | 0.50, 0.64 | (231) | 0.57 | 0.43, 0.70 | (58) | 0.57* | 0.51, 0.63 | (289) |
| Girls | 0.12 | 0.08, 0.17 | (225) | 0.20* | 0.15, 0.26 | (225) | 0.27 | 0.16, 0.42 | (51) | 0.21* | 0.17, 0.27 | (276) |
| Boys | 0.26 | 0.21, 0.32 | (246) | 0.35* | 0.29, 0.42 | (246) | 0.37 | 0.24, 0.52 | (51) | 0.36* | 0.30, 0.42 | (299) |
| White | 0.07 | 0.03, 0.15 | ( 87) | 0.11 | 0.06, 0.20 | ( 87) | 0.25 | 0.00, 0.81 | ( 4) | 0.12 | 0.06, 0.21 | ( 91) |
| Hispanic | 0.23 | 0.18, 0.27 | (354) | 0.32* | 0.27, 0.37 | (354) | 0.34 | 0.24, 0.45 | (91) | 0.33* | 0.28, 0.39 | (445) |
| Black | 0.20 | 0.08, 0.39 | ( 30) | 0.27 | 0.12, 0.46 | ( 30) | 0.14 | 0.00, 0.58 | ( 7) | 0.24 | 0.12, 0.41 | ( 37) |
| Not insured last month | 0.33 | 0.23, 0.44 | ( 82) | 0.44* | 0.33, 0.55 | ( 82) | 0.48 | 0.28, 0.69 | (25) | 0.45* | 0.36, 0.56 | (107) |
| Insured last month | 0.17 | 0.13, 0.21 | (389) | 0.25* | 0.20, 0.29 | (389) | 0.27 | 0.18, 0.39 | (77) | 0.25* | 0.21, 0.29 | (466) |
| Mother's education | ||||||||||||
| < high school | 0.24 | 0.18, 0.30 | (197) | 0.37* | 0.30, 0.44 | (197) | 0.29 | 0.18, 0.42 | (59) | 0.35* | 0.29, 0.41 | (256) |
| High school /college | 0.16 | 0.12, 0.21 | (274) | 0.22* | 0.17, 0.27 | (274) | 0.37† | 0.23, 0.53 | (43) | 0.24* | 0.19, 0.29 | (317) |
Significantly different from self-reported obesity (Column 1) for same respondent group (same row) at p < .05 using a McNemar's test ((2) vs. (1)) or maximum likelihood estimation for overlapping samples ((4) vs. (1)).
Significantly different from obesity prevalence based on measured height and weight for respondents with self-reported height and weight (Column 2) for same respondent group (same row) at p < .05, using chi-squared test ((3) vs. (2)).
Includes only those respondents who also have measured height and weight.
Obesity prevalence estimates for all low BMI-for-age respondents are zero and are not shown
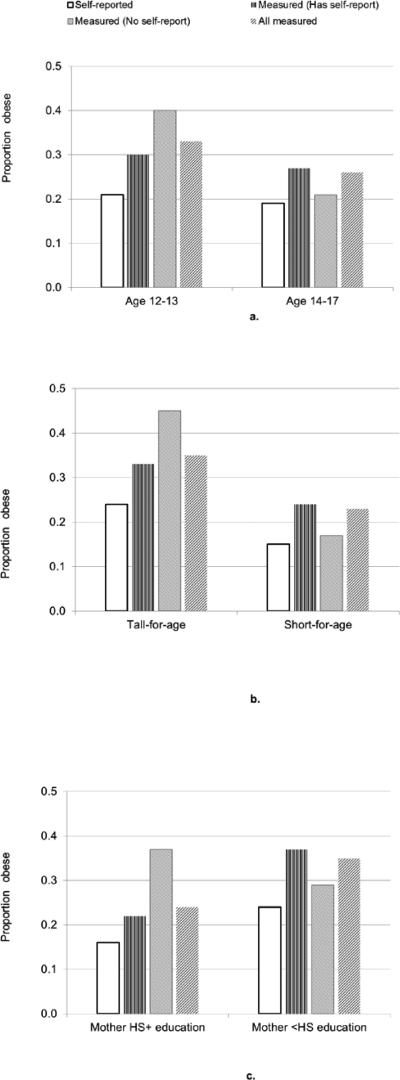
The remainder of Table 3 points to the specific subgroups that are driving these gaps in estimated prevalence. Results are striking for younger vs. older adolescents: Among the younger group, measured obesity prevalence for those who did not report height and weight (0.40, 95% CI 0.28, 0.53) was 33% higher than the measured prevalence for those who did (0.30, 95% CI 0.23, 0.39) and almost twice the self-reported prevalence (0.21, 95% CI 0.15, 0.29). In contrast, obesity prevalence for older teens who did not report height and weight was lower (0.21, 95% CI 0.10, 0.37) than the prevalence among older teens who did report height and weight (0.27, 95% CI 0.22, 0.32). This difference is shown clearly in Figure 1a.
Figure 1.
Obesity Prevalence Estimates Based on Self-reported and Measured Height and Weight by Subgroup, Adolescents Ages 12-17, Los Angeles County, 2006-08. HS+ = high school or higher. <HS = less than high school.
Among adolescents in the top half of the height-for-age distribution in the sample, self-reported obesity prevalence was 0.24 (95% CI 0.19, 0.31), while the measured prevalence for those with and without self-reports was 0.33 (95% CI 0.27, 0.39) and 0.45 (0.31, 0.59) respectively. These prevalence estimates are presented in Figure 1b, with the short-for-age respondents shown for comparison. Finally, among adolescents whose mothers had at least a high school education, the obesity prevalence estimate for those without self-reports (0.37, 95% CI 0.23, 0.53) was significantly higher than for their counterparts who reported height and weight (0.22, 95% CI 0.17, 0.27) (shown in Figure 1c, with the comparison group of respondents whose mothers had less than high school education). This difference leads to a marginal underestimation of self-reported obesity of 2 percentage points when non-response is taken into account (column 4 vs. column 2).
DISCUSSION
Adolescent self-reported height and weight underestimates obesity prevalence by even larger amounts than existing validity studies indicate. This underestimation is due both to failure to report height and weight and to misreported values of these measures. In this study, adolescents with higher BMI were less likely to report height and/or weight. Younger adolescents (age 12-13), in particular, were both less likely than older adolescents to report height and weight and less likely to correctly estimate height and weight when they did report these measures. Comparisons in Table 3 indicate that self-reported height and weight underestimated adolescent obesity by as much as 31% overall, and by 36% for young adolescents.
These results have important implications for the interpretation of published obesity prevalence estimates based on self-reports and their use in designing obesity prevention policies and programs. With few exceptions (Elgar, Roberts, Tudor-Smith, & Moore, 2005; Himes, Hannan, Wall, & Neumark-Sztainer, 2005; Jansen, Van de Looij-Jansen, Ferreira, De Wilde, & Brug, 2006), most existing studies offer no discussion of potential bias caused by missing self-reports. None that we are aware of quantify the magnitude or direction of this non-response bias in obesity prevalence. Our results suggest that obesity prevalence based on self-reports is underestimated by at least one percentage point due solely to non-response and that this underestimation may be as high as three percentage points for younger adolescents.
Previous validity studies have found distinct patterns of errors in self-reports for Mexican-American adults (Gillum & Sempos, 2005) (compared to whites) and for Mexican-American adolescents (Davis & Gergen, 1994). In this study, Hispanic adolescents were more likely than whites to fail to report height, and to report height with error, even when controlling for anthropometry and socioeconomic status. However, non-response appears to be less selective on obesity for Hispanic teens, leading to a smaller gap in obesity prevalence between those who did and did not report height and weight for Hispanic compared with white respondents.
Further complicating child obesity prevalence studies is the existence of multiple child growth references and obesity definitions (Flegal & Ogden, 2011), including the CDC growth references used in the present study (Kuczmarski et al., 2002), the International Obesity Task Force references (Cole, Bellizzi, Flegal, & Dietz, 2000), and the WHO Child Growth Standards (WHO Multicentre Growth Reference Study Group, 2006). Generally, the CDC references tend to produce higher obesity prevalence estimates compared to the IOTF references (Edwards, Evans, & Brown, 2008; Shields & Tremblay, 2010; Twells & Newhook, 2011; Vidal, Carlin, Driul, Tomat, & Tenore, 2006). To evaluate whether our results were robust to the choice of growth reference, we replicated all analyses using the IOTF references. Consistent with prior studies, obesity prevalence was lower when IOTF references were used: for younger teens, measured obesity prevalence was 27% (vs. 33% using the CDC references) while self-reported obesity prevalence was only 13% (compared to 23%). For older teens, the prevalence estimates based on the IOTF cutoffs were 22% (measured) and 17% (self-report) vs. 26% and 19% in the present study. The models of failure to report height and weight and errors in self-reported height and weight (shown in Table 2) do not incorporate IOTF or CDC definitions of obesity and were therefore not affected by choice of growth reference. While the prevalence comparisons shown in Table 3 were lower using the IOTF references, the differences across the subgroups were comparable to the CDC-based analyses. The additional underestimation of self-reported vs. measured obesity due to failure to report increased from 3 to 4 percentage points for younger teens in the IOTF analysis, and the difference between younger teens with and without self-reported height and weight was statistically significant. Generally, our key findings were robust to different growth references, with the notably lower prevalence estimates for the IOTF references.
The study has several important limitations. L.A.FANS is not a nationally-representative sample, so results should be replicated with data from other regions and particularly for Asian adolescents not represented here. The L.A.FANS sampling scheme also oversampled poor neighborhoods, so results should be interpreted accordingly. Small sample sizes in several cells, particularly black and white respondents with no self-reported height or weight may limit the robustness of our results and their generalizability. The analysis should also be replicated using other survey methods to determine whether audio-CASI affected the frequency of non-response and the accuracy of responses. In other adolescent studies, audio-CASI has increased responses to questions about sensitive topics (Turner et al., 1998).
What options do researchers have for minimizing the impact of this observed “double bias”? One obvious strategy is to measure participants rather than rely on self-reports, but measurement is expensive and only possible in face-to-face interviews. A second option is to develop improved interview formats, technologies, and prompts that reduce “don’t know” responses and refusals. Such improvements should be informed by a nuanced understanding of the determinants of non-response. However, if non-response and inaccurate answers reflect a genuine lack of knowledge among adolescents about height and weight, improved survey methods will not increase the accuracy of obesity prevalence estimates.
Alternatively, interviewers might ask parents rather than adolescents about their children's height and weight. However, previous research suggests that parents may misreport (and perhaps misperceive) children's body size. Generally, parents underreport overweight children (Goodman, Hinden, & Khandelwal, 2000; Maynard, Galuska, Blanck, & Serdula, 2003) and do not report concerns about weight status or poor health for obese or overweight children (Wake, Salmon, Waters, Wright, & Hesketh, 2002). Other studies have shown that parents overestimate the weight of young children (Akinbami & Ogden, 2009) and that mothers are more likely to classify overweight daughters than overweight sons as obese (Maynard et al., 2003).
Some researchers have proposed correction factors derived from validity studies to account for errors in self-reported BMI (Jansen et al., 2006); or lowering the obesity threshold when using self-reported height and weight (Dauphinot et al., 2009). We are skeptical that correction factors can be identified for adolescents that are reliable over time and across populations. Results presented here indicate that patterns of non-response and error vary considerably by age, body size, and sociodemographic factors. As suggested above, non-response and error may also be affected by survey methods. Moreover, patterns of non-response and inaccurate reporting may change over time as programs to increase adolescent and parental awareness of obesity become more common (Nihiser et al., 2007).
Reversing the rise of obesity in child and adolescent populations will require accurate surveillance for monitoring, prevention, and evaluation. Health surveys that include self-reported height and weight for adolescents must endeavor to avoid selective non-response. At the very least, we recommend that published studies of adolescent obesity prevalence calculated from self-reports be explicit about non-response and its implications for the direction and magnitude of bias in estimates. Our results suggest that ignoring non-response magnifies the problem of underestimating obesity prevalence, particularly for younger adolescents. We should not permit biased prevalence estimates to undermine obesity prevention efforts.
Contributor Information
Alison M. Buttenheim, University of Pennsylvania.
Noreen Gol, Princeton University.
Anne R. Pebley, University of California, Los Angeles.
REFERENCES
- Adair LS. Child and adolescent obesity: epidemiology and developmental perspectives. Physiology & Behavior. 2008;94:8–16. doi: 10.1016/j.physbeh.2007.11.016. [DOI] [PubMed] [Google Scholar]
- Akinbami LJ, Ogden CL. Childhood Overweight Prevalence in the United States: The Impact of Parent-reported Height and Weight. Obesity Research. 2009;17:1574–1580. doi: 10.1038/oby.2009.1. [DOI] [PubMed] [Google Scholar]
- Brener ND, McManus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. Journal of Adolescent Health. 2003;32:281–287. doi: 10.1016/s1054-139x(02)00708-5. [DOI] [PubMed] [Google Scholar]
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. British Medical Journal. 2000;320:1240. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauphinot V, Wolff H, Naudin F, Gueguen R, Sermet C, Gaspoz JM, Kossovsky MP. New obesity body mass index threshold for self-reported data. Journal of Epidemiology & Community Health. 2009;63:863–864. doi: 10.1136/jech.2008.077800. [DOI] [PubMed] [Google Scholar]
- Davis H, Gergen PJ. The weights and heights of Mexican-American adolescents: the accuracy of self-reports. American Journal of Public Health. 1994;84:459–462. doi: 10.2105/ajph.84.3.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–525. [PubMed] [Google Scholar]
- Edwards J, Evans J, Brown AD. Using routine growth data to determine overweight and obesity prevalence estimates in preschool children in the Capital Health Region of Alberta. Canadian Journal of Public Health. 2008;99 doi: 10.1007/BF03405451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar F, Roberts C, Tudor-Smith C, Moore L. Validity of self-reported height and weight and predictors of bias in adolescents. Journal of Adolescent Health. 2005;37:371–375. doi: 10.1016/j.jadohealth.2004.07.014. [DOI] [PubMed] [Google Scholar]
- Fagot-Campagna A. Emergence of type 2 diabetes mellitus in children: epidemiological evidence. Journal of Pediatric Endocrinology & Metabolism. 2000;13:1395–1402. doi: 10.1515/jpem-2000-s613. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Ogden CL. Childhood Obesity: Are We All Speaking the Same Language? Advances in Nutrition: An International Review Journal. 2011;2:159S–166S. doi: 10.3945/an.111.000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortenberry JD. Reliability of adolescents' reports of height and weight. Journal of Adolescent Health. 1992;13:114–117. doi: 10.1016/1054-139x(92)90076-n. [DOI] [PubMed] [Google Scholar]
- Gillum RF, Sempos CT. Ethnic variation in validity of classification of overweight and obesity using self-reported weight and height in American women and men: the Third National Health and Nutrition Examination Survey. Nutrition Journal. 2005;4:e27. doi: 10.1186/1475-2891-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106:52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- Gorber SC, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obesity Reviews. 2007;8:307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of Overweight and Obesity Among US Children, Adolescents, and Adults, 1999-2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Himes JH, Hannan P, Wall M, Neumark-Sztainer D. Factors Associated with Errors in Self-reports of Stature, Weight, and Body Mass Index in Minnesota Adolescents. Annals of Epidemiology. 2005;15:272–278. doi: 10.1016/j.annepidem.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Jansen W, Van de Looij-Jansen P, Ferreira I, De Wilde E, Brug J. Differences in measured and self-reported height and weight in Dutch adolescents. Annals of Nutrition and Metabolism. 2006;50:339–346. doi: 10.1159/000094297. [DOI] [PubMed] [Google Scholar]
- Kuczmarski R, Ogden CL, Guo S. 2000 CDC Growth Charts for the United States: Methods and Development. National Center for Health Statistics; Hyattsville, MD: 2002. [PubMed] [Google Scholar]
- Lee SK. Validity of self-reported weight and height: comparison between immigrant and non-immigrant Mexican Americans in NHANES III. Journal of Immigrant Health. 2005;7:127–131. doi: 10.1007/s10903-005-2646-4. [DOI] [PubMed] [Google Scholar]
- Maynard LM, Galuska DA, Blanck HM, Serdula MK. Maternal perceptions of weight status of children. Pediatrics. 2003;111:1226–1231. [PubMed] [Google Scholar]
- Nihiser A, Lee S, Wechsler H, McKenna M, Odom E, Reinold C, Grummer-Strawn L. Body mass index measurement in schools. Journal of School Health. 2007;77:651–671. doi: 10.1111/j.1746-1561.2007.00249.x. [DOI] [PubMed] [Google Scholar]
- Nyholm M, Gullberg B, Merlo J, Lundqvist-Persson C, Råstam L, Lindblad U. The Validity of Obesity Based on Self-reported Weight and Height: Implications for Population Studies. Obesity Research. 2007;15:197–208. doi: 10.1038/oby.2007.536. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA. 2002;288:1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, Johnson CL. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109:45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- Peterson C, Pebley A, Sastry N, Yuhas K, Ghosh-Dastidar B, Haas A, Bitler M. The Los Angeles Family and Neighborhood Survey, Wave 2: User's Guide and Codebook. 2011 RAND Working Paper WR-240/20-LAFANS. [Google Scholar]
- Sastry N, Ghosh-Dastidar B, Adams J, Pebley A. The design of a multilevel survey of children, families, and communities: The Los Angeles Family and Neighborhood Survey. Soc Sci Res. 2006;35:1000–1024. [Google Scholar]
- Serdula M, Ivery D, Coates R, Freedman D, Williamson D, Byers T. Do obese children become obese adults? A review of the literature. Preventive Medicine. 1993;22:167–177. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- Sherry B, Jefferds M, Grummer-Strawn L. Accuracy of adolescent self-report of height and weight in assessing overweight status: a literature review. Archives of Pediatrics & Adolescent Medicine. 2007;161:1154. doi: 10.1001/archpedi.161.12.1154. [DOI] [PubMed] [Google Scholar]
- Shields M, Tremblay MS. Canadian childhood obesity estimates based on WHO, IOTF and CDC cut-points. International Journal of Pediatric Obesity. 2010;5:265–273. doi: 10.3109/17477160903268282. [DOI] [PubMed] [Google Scholar]
- Spencer E, Appleby P, Davey G, Key T. Validity of self-reported height and weight in 4808 EPIC–Oxford participants. Public Health Nutrition. 2007;5:561–565. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]
- Strauss RS. Comparison of measured and self-reported weight and height in a cross-sectional sample of young adolescents. International Journal of Obesity and Related Metabolic Disorders. 1999;23:904–908. doi: 10.1038/sj.ijo.0800971. [DOI] [PubMed] [Google Scholar]
- Turner C, Ku L, Rogers S, Lindberg L, Pleck J, Sonenstein F. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:847–848. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- Twells LK, Newhook LA. Obesity prevalence estimates in a Canadian regional population of preschool children using variant growth references. BMC Pediatrics. 2011;11:21. doi: 10.1186/1471-2431-11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidal E, Carlin E, Driul D, Tomat M, Tenore A. A comparison study of the prevalence of overweight and obese Italian preschool children using different reference standards. European journal of pediatrics. 2006;165:696–700. doi: 10.1007/s00431-006-0152-x. [DOI] [PubMed] [Google Scholar]
- Wake M, Salmon L, Waters E, Wright M, Hesketh K. Parent-reported health status of overweight and obese Australian primary school children: a cross-sectional population survey. International Journal of Obesity. 2002;26:717–724. doi: 10.1038/sj.ijo.0801974. [DOI] [PubMed] [Google Scholar]
- WHO Multicentre Growth Reference Study Group WHO Child Growth Standards based on length/height, weight, and age. Acta Paediatrica. 2006;95:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]