Abstract
Objective
To examine and describe regional variation in outcomes for persons with stroke receiving inpatient medical rehabilitation.
Design
Retrospective cohort design.
Setting
Inpatient rehabilitation units and facilities contributing to the Uniform Data System for Medical Rehabilitation (UDSMR) from the United States.
Participants
143,036 patients with stroke discharged from inpatient rehabilitation during 2006 and 2007.
Interventions
Not applicable.
Main Outcome Measures
Community discharge, length of stay, discharge functional status ratings (motor, cognitive), across ten geographic service regions defined by the Centers for Medicare and Medicaid Services (CMS).
Results
Approximately 71% of the sample was discharged to the community. After adjusting for covariates, the percentage discharged to the community varied from 79.1% in the southwest (CMS 9) to 59.4% in the northeast (CMS 2). Adjusted length of stay varied by 2.1 days with CMS 1 having the longest length of stay at 18.3 days and CMS 5 and 9 being the shortest at 16.2 days.
Conclusion
Rehabilitation outcomes for persons with stroke varied across CMS regions. Substantial variation in discharge destination and length of stay remained after adjusting for demographic and clinical characteristics.
Keywords: Rehabilitation, Quality of healthcare, Health services
Persons with stroke represent the largest impairment group of Medicare beneficiaries receiving inpatient medical rehabilitation services in the U.S.1 These services are provided in different settings governed by a variety of rules and regulations. The settings operate using diverse admission policies, staffing ratios and service delivery patterns. For example, inpatient rehabilitation facilities (IRFs) have a Centers for Medicare and Medicaid Services (CMS) compliance requirement that identifies 13 conditions as eligible for services within an IRF.1 Stroke has consistently been the most common Medicare rehabilitation impairment group receiving services in IRFs over the past five years and represents between 16% and 21% of all IRF Medicare cases.1
There is variation nationally in the availability of inpatient rehabilitation facilities. The four states with the highest number of IRFs are Texas, California, Pennsylvania, and New York.1 Each have between 70 and 90 facilities, while Wyoming, West Virginia, Vermont and Delaware each have less than 5.2 State level differences in the number of IRF beds per Medicare beneficiary are different than the geographic distribution of IRF settings by state.2 The impact of these geographic differences on rehabilitation outcomes is largely unknown.
Regional variation has been reported in healthcare for more than 20 years.3–5 The majority of regional variation studies examine acute care services. Researchers have found variation across diagnostic groups from cardiac to cancer.6–9 The presence and reasons for regional variation in the use of health services nationally have been debated in healthcare reform discussions.10–13 Not only does regional variation exist in service use, but it has also been noted in healthcare spending.14–17
A common concern is that higher service use and costs do not translate into better quality or higher satisfaction with care.11 There is currently a heightened emphasis on reducing regional variation as part of health care reform. This discussion is described as a “win-win,” where focused strategies can lead to cost savings while improving quality of care. Regional variation is an important issue for providers, payers and policy makers as they attempt to improve efficiency and maximize the quality of healthcare delivery systems.18
A few studies have examined regional differences in post-acute rehabilitation services and outcomes.19,20–26 Researchers studying the use of post-acute-care following stroke and other common diagnoses found significant regional variation, which they attributed, in part, to practice styles, facility availability and regulations.22 A study of disparities in post-acute care including Arizona, Florida, New Jersey, and Wisconsin, by Freburger and colleagues26 found significant regional differences in IRF and skilled nursing facility (SNF) use after adjusting for individual, facility, and state differences. Other studies examining SNF rehabilitation following hip replacement found significant regional differences in the amount of treatment provided.27–29 Regional differences in physical and occupational therapy services in stroke rehabilitation have also been reported.23;30
Understanding how geographic variability is associated with outcomes will help rehabilitation professionals and administrators implement practice guidelines and quality improvement programs designed to improve care in areas with poor outcomes.31 An important step in this process is to describe region specific outcomes of rehabilitative care at the national level.
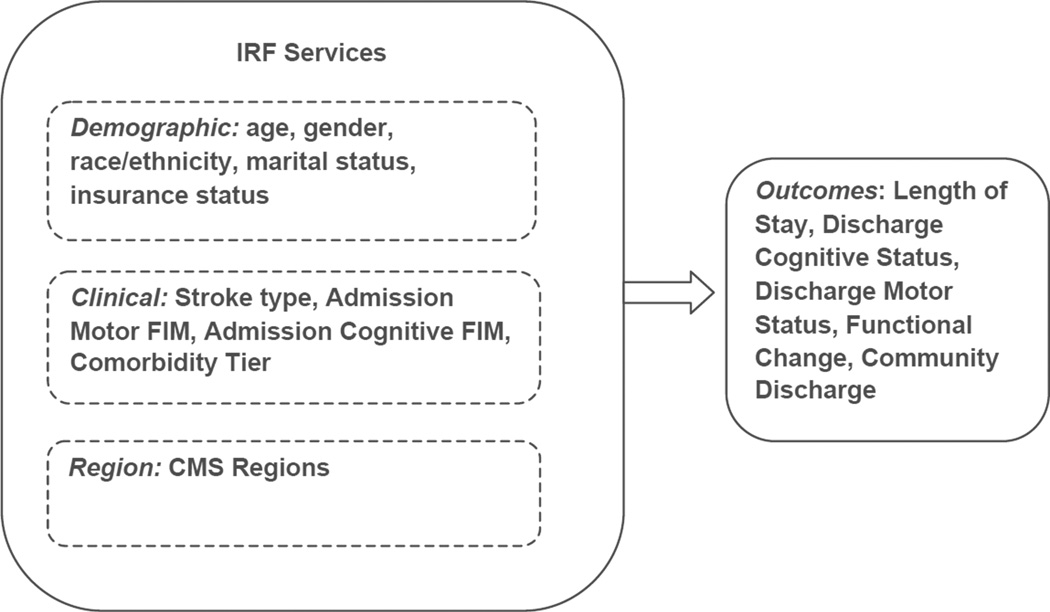
The purpose of this study was to examine regional differences in stroke rehabilitation outcomes in a large national sample including: a) length of stay (LOS), b) functional status (discharge motor and cognitive status, overall functional change), and c) the percentage of patients discharged to the community. Conceptually, variation in health service use and rehabilitation is linked to geography as well as demographic, clinical, and other factors that influence care decisions and resource utilization.26;32–34 Our study was guided by Kane and Radosevich’s35 conceptual model for health outcomes research. We categorized variables that influence rehabilitation outcomes into demographic, clinical, and regional factors (Figure 1).
Figure 1.
Conceptual model for variation in stroke rehabilitation dependent on three components: Demographic factors, clinical factors, and geographic region.
Our main focus was to provide basic descriptive information regarding regional variation in outcomes for persons receiving inpatient rehabilitation following a stroke. Based on the conceptual model, our previous research and clinical experience, and the existing literature, we hypothesized that differences in outcomes would be present across regions after adjusting for demographic and clinical factors.
METHODS
Data Source
We used a retrospective cohort design to examine inpatient rehabilitation records across ten geographic regions. Data were obtained from the Uniform Data System for Medical Rehabilitation (UDSMR). The UDSMR database is the largest non-governmental data repository for inpatient medical rehabilitation information in the U.S.36 The UDSMR database includes patient records from 1987 for 850 to 900 rehabilitation hospitals or facilities across the nation. For this study, we used patient demographics, clinical information, and rehabilitation outcomes from 2006 and 2007 contained in the UDSMR database.
Study Sample
The sample included individuals with stroke based on ICD-9 codes (430 to 433.9, 436 & 439). The eligible sample included adults between the age of 18 and 100 years living at home prior to their acute stroke and were discharged from an IRF in 2006 or 2007 (N = 167,450 patient records). A patient record was excluded if it was not an IRF admission for initial rehabilitation (n = 9,700). Records were also excluded if they reflected an atypical course of rehabilitation. For example, greater than 30 days from acute event to IRF admission (n = 11,577), an IRF stay under 3 days (n = 2,997), or greater than 3 standard deviations of the logarithm for length of stay (n = 1,523). Records with missing data for key variables, e.g., age, discharge setting, were excluded (n=1,859). We included patients with program interruptions (n=1,340). These records represented 1% of the sample and in our sensitivity analysis did not influence the results. Given that program interruptions represent patient stays that were distributed across regions we chose to leave these records in our analysis. The final sample included 143,036 patients, which represents approximately 85% of the eligible patient records.
Study Variables
Based on our experience with stroke outcomes studies using large national datasets,37–40 we examined three common stroke rehabilitation outcomes. Consistent with our conceptual model, we entered demographic characteristics, clinical factors, and geographic region as covariates.
Community discharge
Discharge settings in the UDSMR database are grouped into categories. Community includes home, board-and-care settings, transitional living and assisted living. Long-term care includes nursing home, skilled nursing facilities, chronic hospitals and other alternate care settings. Acute care includes discharges to units in the same facility as well as other acute facilities. Rehabilitation includes settings in other facilities or sub-acute settings within the same IRF. In this study, we dichotomized discharge settings into those returning to community and those needing institutional levels of care.
Length of stay
Rehabilitation length of stay was calculated as the total number of days spent in the inpatient medical rehabilitation unit or hospital.
Functional status
Motor and cognitive function at discharge and overall functional gain were assessed with the FIM instrument (FIM™). In 2002, the items from the FIM instrument were incorporated into the Inpatient Rehabilitation Facilities-Patient Assessment Instrument (IRF-PAI).41 The FIM instrument is a standardized measure of disability and burden of care that is used in inpatient rehabilitation facilities across all geographic regions.42
The FIM instrument is administered within 3 days of admission and 3 days of discharge and includes 18 items that cover 6 functional subscales: self-care, sphincter control, transfers, locomotion, communication, and social cognition. The first four subscales denote the motor domain and the latter two denote the cognitive domain. All items are measured on a seven point scale from 1 (total assistance) to 7 (complete independence). Motor domain ratings range from 13 to 91 with cognition ratings ranging from 5–35. Overall FIM ratings range from 18 to 126. Functional change was defined as the difference between admission and discharge FIM ratings.37;43;44 The reliability and validity of the FIM instrument have been studied extensively in patients with stroke and other impairments.45
Demographic Factors
Demographic variables known to influence rehabilitation outcomes46;47 were used as covariates. These factors included age, gender, race/ethnicity, marital status, and insurance status. Race/ethnicity was coded as non-Hispanic white, Black, Hispanic and other. Marital status was dichotomized as married verses unmarried/single. Insurance status was classified as Medicare, Medicare managed care, Medicaid, managed care, commercial insurance, and other.
Clinical Factors
Clinical factors include stroke type, comorbidities, and admission functional status. Stroke types included ischemic, hemorrhagic, and other. We used the CMS tier system to classify comorbidity level. CMS tiers reflect specific comorbidities that influence rehabilitation service use.42;48 Studies of inpatient rehabilitation including stroke have shown that tier levels influence outcomes of care.49;50 We considered the sum of each patient’s commobid conditions included in the IRF-PAI to reflect medical severity. This approach has a potential ceiling effect because IRF-PAI limits the number or comorbid diagnoses to ten. We considered the Elixhauser and Charleson indices, but were not able to use these methods because we did not have access to acute-care records and could not develop an accurate score based on a “look-back” period.
Geographic Region
The geographic region variable was the Centers for Medicare and Medicaid Services (CMS) regions. CMS has 10 offices monitoring healthcare at the regional, state and local level.51 Consistent with CMS regions UDSMR patient records were categorized into the following regions by state: CMS 1 = CT, MA, ME, NH, RI, VT; CMS 2 = NJ, NY; CMS 3 = DC, DE, MD, PA, VA, WV; CMS 4 = AL, FL, GA, KY, MS, NC, SC, TN; CMS 5 = IL, IN, MI, MN, OH, WI; CMS 6 = AR, LA, NM, OK, TX; CMS 7 = IA, KS, MO, NE; CMS 8 = CO, MT, ND, SD, UT, WY; CMS 9 = AZ, CA, HI, NV; and CMS 10 = AK, ID, OR, WA. We dummy coded CMS region for inclusion in our models.
Data Analysis
Demographic and clinical characteristics, along with outcomes, were stratified by CMS region and examined descriptively using measures of central tendency and proportions. Linear regression was used with continuous outcome measures to determine region specific LOS and discharge FIM ratings (motor, cognitive, change). Logistic regression was used for community discharge by region. Reference categories for nominal covariates were identified based on unadjusted descriptive percentages: the most frequent category was selected for all variables. For the region variable, CMS 10 was used as the reference category because that region had the lowest unadjusted LOS with the highest community discharge percentage and highest mean admitting functional status ratings across all regions (see Table 2).
Table 2.
Sample clinical characteristics and outcomes by CMS region (unadjusted)
| Variables | CMS 1 | CMS 2 | CMS 3 | CMS 4 | CMS 5 | CMS 6 | CMS 7 | CMS 8 | CMS 9 | CMS 10 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stroke Type | |||||||||||
| Ischemic % | 81.5 | 75.0 | 74.6 | 79.2 | 77.0 | 77.3 | 77.3 | 73.3 | 71.8 | 80.3 | 76.7 |
| Hemorrhagic | 15.7 | 14.6 | 13.7 | 12.5 | 13.8 | 11.2 | 15.5 | 20.3 | 17.8 | 15.2 | 14.0 |
| Other | 2.8 | 10.4 | 11.7 | 8.3 | 9.2 | 11.5 | 7.2 | 6.4 | 10.4 | 4.5 | 9.3 |
| Tier Level | |||||||||||
| Comorbidity | |||||||||||
| None % | 75.8 | 82.3 | 76.9 | 76.9 | 79.0 | 78.2 | 79.4 | 78.6 | 78.4 | 83.3 | 78.4 |
| Low | 18.4 | 13.9 | 18.6 | 19.4 | 18.0 | 18.2 | 16.9 | 18.9 | 17.6 | 14.7 | 17.9 |
| Medium | 3.5 | 1.7 | 2.2 | 1.6 | 1.3 | 1.4 | 1.8 | 1.2 | 2.1 | 0.9 | 1.7 |
| High | 2.3 | 2.0 | 2.2 | 2.1 | 1.8 | 2.2 | 1.9 | 1.3 | 1.9 | 1.0 | 2.0 |
| FIM Admission | |||||||||||
| Cognitive | 19.0(7.9) | 21.9(8.2) | 20.5(7.8) | 19.2(7.8) | 21.2(7.6) | 19.4(7.8) | 20.1(7.6) | 19.9(7.7) | 19.2(7.5) | 22.2(7.0) | 20.1(7.8) |
| Motor | 32.4(13.9) | 33.7(13.3) | 34.8(13.1) | 32.0(12.5) | 36.4(13.1) | 33.0(13.0) | 35.8(13.3) | 36.8(14.4) | 32.8(12.4) | 39.6(12.7) | 34.1(13.1) |
| Total | 52.9(20.0) | 57.3(19.5) | 57.1(19.1) | 53.1(18.5) | 59.6(18.7) | 54.8(19.4) | 58.1(19.1) | 59.2(20.3) | 54.2(18.3) | 64.5(17.7) | 56.2(19.1) |
| FIM Discharge | 29.0(16.8) | 23.8(14.9) | 24.7(14.3) | 24.8(14.4) | 24.3(14.2) | 25.4(15.2) | 25.1(14.9) | 26.5(16.6) | 26.1(14.8) | 24.6(13.8) | 25.1(14.8) |
| Cognitive | 24.7(7.2) | 25.5(7.5) | 24.6(7.2) | 23.6(7.4) | 25.2(7.0) | 23.8(7.4) | 24.4(6.9) | 24.5(7.2) | 23.8(7.3) | 26.1(6.4) | 24.4(7.3) |
| Motor | 54.2(18.9) | 52.4(18.4) | 53.8(17.0) | 50.8(16.9) | 54.9(16.4) | 52.2(17.0) | 54.8(16.9) | 56.9(17.6) | 52.4(16.3) | 58.9(15.7) | 53.2(17.1) |
| Total | 81.9(25.3) | 81.2(24.8) | 81.8(23.3) | 78.0(23.3) | 83.9(22.3) | 80.2(23.6) | 83.2(22.8) | 85.7(23.8) | 80.3(22.5) | 89.6(20.9) | 81.3(23.4) |
| FIM Change | 29(16.8) | 23.9(15) | 24.8(14.4) | 24.9(14.5) | 24.3(14.2) | 25.5(15.3) | 25.1(14.9) | 26.5(16.7) | 26.1(14.9) | 24.7(13.8) | 25.1(14.8) |
| Length of Stay | 18.9(11.2) | 17.3(9.4) | 16.3(9.9) | 17.1(8.7) | 15.2(8.5) | 16.6(8.9) | 16.3(9.2) | 16.6(10.7) | 16.7(8.9) | 14.5(8.2) | 16.5(9.2) |
| Community Discharge % | 62.0 | 63.3 | 70.5 | 73.2 | 70.6 | 72.4 | 68.6 | 72.0 | 78.1 | 81.9 | 71.4 |
Continuous variables presented as mean (standard deviation), categorical variables as percent (%).
We used an ordinary least squares method to adjust for demographic, clinical factors at admission to calculate region specific outcomes. Standard regression diagnostics (goodness-of-fit, multicollinarity, homoscedasticity, outliers) were computed for each of the models examining a primary outcome.52 Finally, we constructed maps showing regional outcomes for the typical stroke patient using ArcGIS 10 Software.53 All other analyses were conducted using SPSS ver. 19.
RESULTS
The sample was 51.6% female with a mean age of 70.6 (± 13.6) years. Fifty percent of the sample was married. The sample was 71.9% non-Hispanic white. The portion of non-Hispanic white varied from 59.1% in CMS region 2 to 88.5% in CMS region 8. The most common stroke type was an ischemic event (76.7%) which varied across CMS regions from 71.8% for region 9 to 81.5% for region 1. CMS region 4 (southeast) had the highest number of patients with stroke (n = 28,522) representing 21% of the sample (see Table 1). Overall, 17.9% of the sample was classified with low-level tier comorbidity with 1.7% moderate and 2.0% high tier. Mean admission FIM ratings ranged from 52.9 in CMS region 1 to 64.5 in CMS 10. The pattern across the regions was similar for both cognitive and motor domains at admission. The two largest primary insurance carriers were Medicare at 62% and private commercial insurance at 16%. Insurance status varied across CMS regions with the Medicare percentages ranging from CMS 6 = 67.5% to CMS 2 = 54.9%.
Table 1.
Sample demographic characteristics by CMS region (unadjusted)
| Variables | CMS 1 | CMS 2 | CMS 3 | CMS 4 | CMS 5 | CMS 6 | CMS 7 | CMS 8 | CMS 9 | CMS 10 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Patients | 6159 | 13357 | 18846 | 28522 | 21918 | 22618 | 8501 | 4004 | 13717 | 4394 | 143036 |
| Age (mean, sd) | 72.1(13.4) | 70.7(13.7) | 71.3(13.3) | 69.9(13.5) | 70.8(13.5) | 70.9(13.1) | 70.3(13.8) | 70.6(14.0) | 69.6(14.1) | 70.1(13.6) | 70.6(13.5) |
| Female % | 50.9 | 52.0 | 52.5 | 52.1 | 51.5 | 53.2 | 50.3 | 50.5 | 49.2 | 47.5 | 51.6 |
| Race/Ethnicity % | |||||||||||
| White | 83.8 | 59.1 | 80.9 | 68.6 | 79.5 | 63.6 | 83.3 | 88.5 | 60.1 | 80.5 | 71.9 |
| Black | 6.7 | 21.4 | 14.5 | 20.6 | 15.8 | 18.1 | 10.8 | 2.2 | 8.1 | 2.7 | 15.3 |
| Hispanic | 2.8 | 10.4 | 0.8 | 3.2 | 1.8 | 12.3 | 0.9 | 4.6 | 13.0 | 2.6 | 5.6 |
| Other | 6.7 | 9.1 | 3.7 | 7.5 | 2.9 | 6.1 | 5.0 | 4.6 | 18.8 | 14.3 | 7.3 |
| Unmarried % | 50.7 | 55.0 | 51.3 | 50.4 | 50.7 | 49.1 | 49.0 | 44.3 | 46.9 | 44.1 | 50.0 |
| Primary Insur. % | |||||||||||
| Medicare | 64.2 | 54.9 | 57.9 | 64.5 | 64.1 | 67.5 | 64.3 | 66.0 | 54.0 | 56.1 | 61.9 |
| Medicaid | 4.1 | 4.9 | 2.8 | 3.4 | 3.7 | 2.6 | 4.7 | 2.5 | 8.4 | 523 | 4.0 |
| Medicare managed | 4.3 | 11.6 | 9.9 | 5.0 | 6.6 | 5.0 | 5.0 | 3.2 | 7.5 | 11.2 | 6.9 |
| Commercial | 15.3 | 14.0 | 15.7 | 16.4 | 15.5 | 15.9 | 16.0 | 17.3 | 16.3 | 16.4 | 15.8 |
| Managed Care | 8.0 | 6.7 | 7.7 | 3.7 | 4.5 | 2.4 | 4.4 | 3.5 | 8.3 | 5.4 | 5.1 |
| Other | 4.3 | 7.9 | 6.1 | 7.0 | 5.6 | 6.6 | 5.6 | 7.3 | 5.5 | 5.8 | 6.3 |
Continuous variables presented as mean (standard deviation), categorical variables as percent (%).
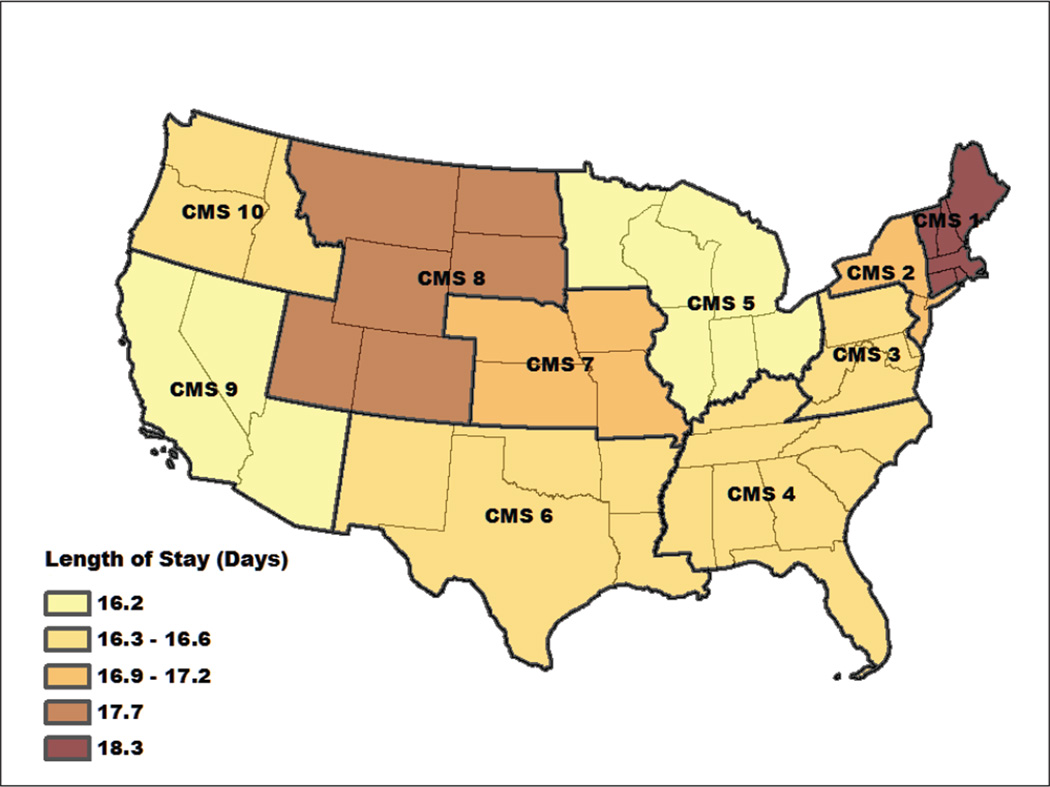
The unadjusted mean LOS varied across regions from 14.5 days (CMS 10) to 18.9 days (CMS 1) (Table 2). The regression analyses for the continuous outcome measures indicated that LOS for region CMS 5 was significantly lower than CMS 10 (16.6 days) which was at the national median (CMS 5:b=−0.37, CI −0.62, −0.12), while CMS 8 (b=1.15 CI 0.82, 1.48) and CMS 1 (b=1.70, CI 1.40, 2.00) were significantly above. Overall, adjusted LOS varied by 2.1 days across the 10 CMS regions (see Figure 2 and Table 3). Compared to persons who were non-Hispanic white, persons who were Hispanic had shorter LOS (b=−1.03; CI −1.21, −0.85). For clinical characteristics, higher admission motor ratings were associated with shorter LOS (b=−.39; CI −0.4, −0.39). Compared to non-tier comorbidities, both medium tier (b=2.36; CI 2.05, 2.67) and high tier (b=0.99; CI 0.70, 1.29) groups had longer LOS.
Figure 2.
Regional differences in LOS after adjusting for demographic and clinical factors across CMS regions. National median was 16.6 days (CMS 10). Lighter areas reflect shorter LOS. LOS varied by two days across the CMS regions.
Table 3.
Regression coefficients and confidence intervals across stroke outcomes
| Length of Stay | Discharge Motor | Functional Gain | Community Discharge | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | 95 % | CI | b | 95 % | CI | b | 95 % | CI | OR | 95 % | CI | |
| Age | −0.07 | −0.07 | −0.06 | −0.14 | −0.15 | −0.14 | −0.20 | −0.20 | −0.19 | 0.98 | 0.98 | 0.98 |
| Male | 0.34 | 0.26 | 0.43 | 0.01 | −0.11 | 0.13 | 0.00 | −0.15 | 0.16 | 0.86 | 0.84 | 0.88 |
| Married | −0.42 | −0.51 | −0.34 | −0.23 | −0.35 | −0.10 | −0.21 | −0.37 | −0.05 | 1.70 | 1.65 | 1.75 |
| Race/Ethnicity (White) | ||||||||||||
| Black | −0.68 | −0.80 | −0.56 | −1.42 | −1.59 | −1.25 | −2.06 | −2.28 | −1.84 | 1.20 | 1.16 | 1.25 |
| Hispanic | −1.03 | −1.21 | −0.85 | −1.34 | −1.60 | −1.08 | −1.83 | −2.17 | −1.49 | 1.41 | 1.33 | 1.50 |
| Other | −0.20 | −0.36 | −0.04 | 0.05 | −0.18 | 0.28 | −0.20 | −0.50 | 0.10 | 1.27 | 1.20 | 1.34 |
| Stroke Type (Ischemic) | ||||||||||||
| Hemorrhagic | 0.02 | −0.10 | 0.14 | 1.02 | 0.84 | 1.19 | 1.19 | 0.97 | 1.42 | 0.97 | 0.93 | 1.01 |
| Other | −0.77 | −0.91 | −0.63 | −0.87 | −1.07 | −0.67 | −1.19 | −1.45 | −0.93 | 1.06 | 1.01 | 1.11 |
| Insurance (Medicare) | ||||||||||||
| Medicaid | 0.71 | 0.48 | 0.93 | 0.16 | −0.16 | 0.48 | 0.00 | −0.42 | 0.42 | 1.21 | 1.12 | 1.30 |
| Medicare managed | 0.08 | −0.08 | 0.25 | −0.41 | −0.64 | −0.17 | −0.55 | −0.85 | −0.24 | 1.08 | 1.03 | 1.14 |
| Commercial | 0.86 | 0.73 | 0.99 | 1.04 | 0.84 | 1.23 | 1.47 | 1.22 | 1.72 | 1.45 | 1.38 | 1.51 |
| Managed Care | 1.10 | 0.91 | 1.29 | 1.30 | 1.01 | 1.58 | 1.65 | 1.29 | 2.02 | 1.40 | 1.31 | 1.50 |
| Other | 0.45 | 0.26 | 0.64 | 0.27 | 0.00 | 0.54 | 0.42 | 0.06 | 0.77 | 1.40 | 1.31 | 1.50 |
| Admission FIM | ||||||||||||
| Motor | −0.39 | −0.40 | −0.39 | 0.88 | 0.88 | 0.89 | −0.09 | −0.09 | −0.08 | 1.08 | 1.08 | 1.08 |
| Cognitive | 0.04 | 0.04 | 0.05 | 0.20 | 0.19 | 0.21 | −0.05 | −0.06 | −0.04 | 1.03 | 1.03 | 1.03 |
| Comorbidity (non-Tier) | ||||||||||||
| Tier low | −0.20 | −0.31 | −0.09 | −1.31 | −1.46 | −1.16 | −1.49 | −1.69 | −1.29 | 0.82 | 0.80 | 0.85 |
| Tier medium | 2.36 | 2.05 | 2.67 | −2.46 | −2.90 | −2.01 | −2.79 | −3.37 | −2.21 | 0.77 | 0.70 | 0.84 |
| Tier high | 0.99 | 0.70 | 1.28 | −2.89 | −3.31 | −2.47 | −3.38 | −3.92 | −2.84 | 0.61 | 0.56 | 0.66 |
| Region (CMS 10) | ||||||||||||
| CMS 1 | 1.70 | 1.40 | 2.00 | 2.76 | 2.32 | 3.19 | 4.13 | 3.57 | 4.70 | 0.62 | 0.56 | 0.69 |
| CMS 2 | 0.67 | 0.41 | 0.94 | −0.69 | −1.08 | −0.31 | −0.56 | −1.06 | −0.07 | 0.50 | 0.45 | 0.55 |
| CMS 3 | 0.08 | −0.18 | 0.33 | −0.05 | −0.41 | 0.32 | 0.22 | −0.26 | 0.70 | 0.76 | 0.69 | 0.83 |
| CMS 4 | −0.21 | −0.45 | 0.04 | −0.35 | −0.71 | 0.01 | −0.07 | −0.54 | 0.39 | 1.07 | 0.98 | 1.18 |
| CMS 5 | −0.37 | −0.62 | −0.12 | −0.48 | −0.84 | −0.12 | −0.11 | −0.58 | 0.36 | 0.65 | 0.60 | 0.72 |
| CMS 6 | −0.14 | −0.39 | 0.11 | 0.49 | 0.12 | 0.85 | 0.96 | 0.49 | 1.44 | 0.96 | 0.88 | 1.05 |
| CMS 7 | 0.39 | 0.11 | 0.67 | −0.08 | −0.49 | 0.33 | 0.26 | −0.27 | 0.79 | 0.62 | 0.56 | 0.69 |
| CMS 8 | 1.15 | 0.82 | 1.48 | 1.09 | 0.61 | 1.57 | 1.60 | 0.98 | 2.22 | 0.74 | 0.66 | 0.83 |
| CMS 9 | −0.32 | −0.58 | −0.06 | 0.43 | 0.05 | 0.81 | 0.99 | 0.50 | 1.49 | 1.29 | 1.18 | 1.43 |
Reference category for logistic regression in ().
b = regression coefficient
OR = odds ratio
CI = confidence interval
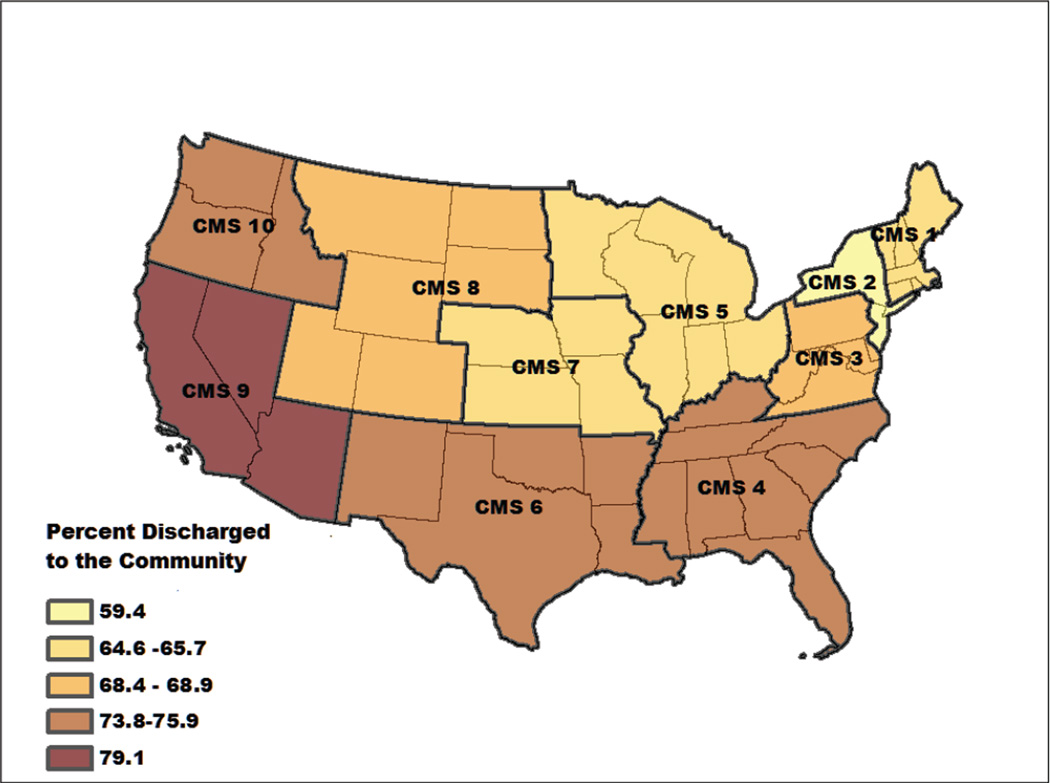
The unadjusted community discharge percentages ranged from 62.0% to 81.9% regionally. For persons who were institutionalized, the largest percentage (44.1%, n=18,351) were in long-term-care settings. After entering covariates the average community discharge percentage across all CMS regions was 69.0% percent. The adjusted percentage of individuals discharged to the community varied from 79.1% in the southwest (CMS 9) to 59.4% in the northeast (CMS 2). Figure 3 shows a map of the adjusted differences in community discharge across CMS regions.
Figure 3.
Percentage of individuals discharged to the community following stroke rehabilitation after adjusting for demographic and clinical factors. Community discharge varied by 20% across the CMS regions.
The logistic regression analysis indicated that married patients were more likely to return to community (OR=1.70; CI 1.65, 1.75). Compared to non-Hispanic white patients, other race/ethnic groups had greater odds of community discharge. The OR for African Americans was 1.20 (CI 1.16, 1.25), and 1.41 (CI 1.33, 1.50) for Hispanics. Higher FIM instrument motor and cognitive ratings at admission significantly increased the likelihood of community discharge (motor OR=1.08; CI 1.08, 1.08; cognitive OR=1.03; CI 1.02, 1.03), while patients with comorbid conditions were less likely to return to the community (see Table 3).
Unadjusted mean total FIM discharge ratings ranged from 78.0 (CMS 4) to 89.6 (CMS 10) across regions. After controlling for covariates, the mean FIM change was 26 points with a 4.7 point difference across regions. The majority of this difference was due to changes in motor ratings which varied by 3.5 points across regions. In the adjusted analyses, persons in the Black and Hispanic race/ethnic groups demonstrated significantly less change in function compared to non-Hispanic whites. Likewise, persons in a tier comorbidity category had significantly less change in FIM ratings than patients without a tier comorbidity. Table 3 shows the regression coefficients for discharge motor and overall change in FIM instrument ratings.
DISCUSSION
The purpose of our study was to explore regional variation in post-acute medical rehabilitation outcomes. The findings suggest there are regional differences, most notably in community discharge rates and LOS. Regional variation in rehabilitation outcomes remained after controlling for the extensive variability in observed patient characteristics and clinical factors across regions.
Discharge to the community has been identified as an important outcome and quality indicator for inpatient rehabilitation.54 The finding of a 20% difference in community discharge rates across CMS regions suggests that complex environmental and social factors along with patient demographics and clinical factors contribute to discharge outcomes for patients receiving stroke rehabilitation in ways we currently do not understand. The region with the highest percent of community discharge after adjusting for basic patient and clinical variables was the southwest (CMS 9 = 79.1%) while the lowest region was the northeast (CMS 2 = 59.4%). These two regions represent diverse geographic areas with different types and availability of resources to assist individuals attempting to reintegrate into the community following a stroke. There were obvious differences in demographic and clinical factors across regions; e.g. CMS region 2 included fewer Medicare patients and demonstrated greater racial/ethnic diversity. Both of these factors can influence discharge decisions with persons from underrepresented groups discharged home at higher rates.55 Recent research has also suggested that Medicaid beneficiaries from underrepresented groups are less likely to receive institutional care than non-Hispanic whites.26 Differences among racial/ethnic groups and health insurance status highlight the need to adjust for demographic and clinical factors in our analyses. These are complex issues involving many potential confounds. Howard et al. examined these complex relationships in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. REGARDS is a prospective population-based observational study of 30,239 adults > 45 years of age.56 We are also exploring regional variation using a small-area analysis approach based on hospital referral regions (HRR) rather than the large-area analysis involving CMS regions reported in this study. We believe HRRs will provide a more sensitive approach to examine the influential factors identified in the current study.
We considered whether the difference in community discharge might be attributable to access or volume, but discarded these hypotheses since the two regions with the largest disparity in community discharge had comparable numbers of facilities capable of treating an equivalent volume of patients. With respect to facility networks and referral patterns, we were unable to examine availability of alternate post-acute care venues, which has been shown to influence admission to inpatient rehabilitation.57 Information regarding alternative post-acute care facilities was not available in our dataset and this is an important area for future research.
When examining LOS, regional differences have important resource and cost implications. The median LOS across the ten regions was 16.6 days (CMS 3 and 10). Based on the regression analyses the two regions with the shortest length of stay (CMS 5 and 9) are approximately half a day shorter than the median. After adjusting for relevant covariates there is a 2.1 day difference between the regions with the lowest and highest mean LOS. In fiscal year 2006, the mean cost per patient day for inpatient medical rehabilitation for stroke ranged from $900 to $1,100 depending on severity and estimated service use.58 In 2010 the mean per-day cost for inpatient medical rehabilitation across all impairment groups was $1,304.1
Our results indicate that functional status and change in function as measured by the FIM instrument are relatively stable across regions. All CMS regions demonstrated functional change of approximately 25 points from admission to discharge reflecting improvement in functional independence during rehabilitation for persons with stroke.59 Across regions, the mean difference in functional change was less than five points suggesting that change did not vary substantially. The stability of functional assessment data is consistent with prior research showing acceptable reliability for the FIM instrument across IRF impairment groups and treatment settings.45
The goal of identifying differences in rehabilitation outcomes across geographic regions is to ultimately develop programs, and identify administrative processes or structural changes that can be implemented to improve individual patient independence. In the Donabedian60 framework of Structure - Process – Outcomes; process measures are often preferred because they are closer to outcomes, and may lead more directly to interventions to enhance outcomes.34;61 In general, rehabilitation outcome researchers are limited by a lack of accepted process measures.61 This is true for our investigation as well.
Minimizing regional variation by improving care in lower performing regions has been demonstrated to lead to higher quality and patient satisfaction in acute care settings.11 It is logical that similar improvements might be seen in post-acute care venues including inpatient rehabilitation. Our study is an initial step to better understanding how process, structure, and outcomes vary geographically for inpatient medical rehabilitation services. This is a complex issue that cannot be resolved by a single investigation. We have started the exploration of post-acute geographic variation in rehabilitation outcomes at a macro level by focusing on CMS regions. We realize this is a crude approach but it provides important information in identifying areas and directions for future research. For example, we are currently examining discharge setting and length of stay information in the CMS MedPAR (medical provider annual review) and the IRF-PAI files using hospital referral regions.
Study Limitations
In addition to the limitations associated with the CMS regions and the lack of process measures in the UDSMR dataset, our study has some other weaknesses. The UDSMR data provides excellent information regarding the person’s inpatient rehabilitation experience. It does not, however, include information about services received prior to rehabilitation admission or treatment provided in the acute care setting. We also did not have detailed facility level information, such as number of beds, type of staff, or hours and intensity of services provided to patients. As with all large administrative datasets involving secondary data analysis, there are potential issues with coding accuracy and data integrity. Facilities that submit information to the UDSMR are required to complete a credentialing process. Previous research has demonstrated excellent reliability for the collection of the functional status information included in the UDSMR data files.45
Discharge to community is an area where we found substantial variation across CMS regions. We believe discharge destination and transition to the community are important topics for future research. Previous studies have demonstrated the central role of clinical, social, environmental and functional performance factors in successful home and community reintegration.57;62–64 Proximity and availability of rehabilitative facilities is an obvious factor potentially influencing discharge destination that we were not able to examine at the level of the CMS regions20 and this is another important topic for future research.
Conclusions
Understanding regional variation related to community discharge is an essential step in developing strategies for care transition. Future research to define and establish these strategies will be important for medical rehabilitation and other post-acute care settings as components of the Affordable Care Act, including accountable care organizations, medical homes, and bundled payments are implemented as part of health care reform. Rehabilitation investigators should be active contributors to this process.
Acknowledgement
Supported by the National Institute of Child Health and Human Development, NIH (K01-HD068513– Reistetter) and (R24 HD065702 - Ottenbacher, Graham, Karmarkar) and by the Institute for Translational Sciences at UTMB with support in part by an NIH Clinical and Translational Science Award (UL1RR029876) The funding organizations had no role in the design and conduct of the study; collection, management, analysis, interpretation, and preparation of the manuscript. Dr. Reistetter had full access to the data and takes responsibility for the integrity and the accuracy of the data analysis.
Abbreviations
- CMS
Centers for Medicare and Medicaid Services
- FIM
Functional Independence Measure
- IRF
Inpatient Rehabilitation Facility
- IRF-PAI
Inpatient Rehabilitation Facility-Patient Assessment Instrument
- ICD-9
International Classification of Diagnoses
- LOS
Length of Stay
- SNF
Skilled Nursing Facilities
- UDSMR
Uniform Data System for Medical Rehabilitation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented, in part, to the American Occupational Therapy Association, Orlando Florida April 2010, and to the American Congress of Rehabilitation Medicine, Quebec Canada October 2010.
Reference List
- 1.MedPAC. Report to the Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission; 2012. [Google Scholar]
- 2.RTI International. Walham, MA: 2008. [Accessed September 22,2011]. Examining Relationships in an Integrated Hospital System: Final Report. http://aspe.hhs.gov/health/reports/08/examine/report.html. [Google Scholar]
- 3.Ashton CM, Petersen NJ, Souchek J, et al. Geographic variations in utilization rates in Veterans Affairs hospitals and clinics. N Engl J Med. 1999;340:32–39. doi: 10.1056/NEJM199901073400106. [DOI] [PubMed] [Google Scholar]
- 4.Birkmeyer JD, Sharp SM, Finlayson SR, Fisher ES, Wennberg JE. Variation profiles of common surgical procedures. Surgery. 1998;124:917–923. [PubMed] [Google Scholar]
- 5.Wennberg DE, Lucas FL, Birkmeyer JD, Bredenberg CE, Fisher ES. Variation in carotid endarterectomy mortality in the Medicare population: trial hospitals, volume, and patient characteristics. JAMA. 1998;279:1278–1281. doi: 10.1001/jama.279.16.1278. [DOI] [PubMed] [Google Scholar]
- 6.Fisher E, Bell JE, Tomak I, Esty A, Goodman D. Trends in Regional Variation in Hip Knee and Sholder Replacement: A Dartmouth Atlas Surgery Report. [Accessed May 21, 2010]; 4-15-2010. http://www.dartmouthatlas.org/downloads/reports/Joint Replacement0410.pdf. [PubMed] [Google Scholar]
- 7.Domanski M, Antman EM, McKinlay S, et al. Geographic variability in patient characteristics, treatment and outcome in an International Trial of Magnesium in acute myocardial infarction. Controlled Clinical Trials. 2004;25:553–562. doi: 10.1016/j.cct.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Krupski TL, Kwan L, Afifi AA, Litwin MS. Geographic and socioeconomic variation in the treatment of prostate cancer. Journal of Clinical Oncology. 2005;23:7881–7888. doi: 10.1200/JCO.2005.08.755. [DOI] [PubMed] [Google Scholar]
- 9.Sporer SM, Weinstein JN, Koval KJ. The geographic incidence and treatment variation of common fractures of elderly patients. Journal of the American Academy of Orthopaedic Surgeons. 2006;14:246–255. doi: 10.5435/00124635-200604000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Berkowitz SA, Gerstenblith G, Herbert R, Anderson G. Improving regional variation using quality of care measures. Risk Management & Healthcare Policy. 2009;2:91–96. doi: 10.2147/RMHP.S6583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenthal T. Geographic variation in health care. Annual Review of Medicine. 2012;63:493–509. doi: 10.1146/annurev-med-050710-134438. [Review]. [DOI] [PubMed] [Google Scholar]
- 12.Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. Health Affairs Suppl Web Exclusives:W96–114, 2002. 2002 Jul-Dec;:W96–W114. doi: 10.1377/hlthaff.w2.96. [DOI] [PubMed] [Google Scholar]
- 13.Wennberg JE, Peters PG., Jr Unwarranted variations in the quality of health care: can the law help medicine provide a remedy/remedies? Specialty Law Digest Health Care Law (305):9–25, 2004. 2004 Sep;:9–25. [PubMed] [Google Scholar]
- 14.Cooper RA. States with more health care spending have better-quality health care: lessons about Medicare. Health Affairs. 2009;28:w103–w115. doi: 10.1377/hlthaff.28.1.w103. [DOI] [PubMed] [Google Scholar]
- 15.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Int Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [Summary for patients in Ann Intern Med. 2003 Feb 18; 138(4):I36; PMID: 12585853]. [DOI] [PubMed] [Google Scholar]
- 16.Fisher ES, Bynum JP, Skinner JS. Slowing the growth of health care costs--lessons from regional variation. N Engl J Med. 2009;360:849–852. doi: 10.1056/NEJMp0809794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Y, Baik SH, Fendrick AM, Baicker K. Comparing local and regional variation in health care spending. N Engl J Med. 2012;367:1724–1731. doi: 10.1056/NEJMsa1203980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wennberg DE, Wennberg JE. Addressing variations: is there hope for the future? Health Affairs Suppl Web Exclusives:W3-614-7, 2003. 2003 Jul-Dec;:W3–W7. doi: 10.1377/hlthaff.w3.614. [DOI] [PubMed] [Google Scholar]
- 19.Tian W, DeJong G, Brown M, Hsieh CH, Zamfirov ZP, Horn SD. Looking upstream: factors shaping the demand for postacute joint replacement rehabilitation. Arch Phys Med Rehabil. 2009;90:1260–1268. doi: 10.1016/j.apmr.2008.10.035. [DOI] [PubMed] [Google Scholar]
- 20.Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medicare Spending and Outcomes After Postacute Care for Stroke and Hip Fracture. Medical Care. 2010;48:776–784. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ilett PA, Brock KA, Graven CJ, Cotton SM. Selecting patients for rehabilitation after acute stroke: are there variations in practice? Arch Phys Med Rehabil. 2010;91:788–793. doi: 10.1016/j.apmr.2009.11.028. [DOI] [PubMed] [Google Scholar]
- 22.Kane RL, Lin WC, Blewett LA. Geographic variation in the use of post-acute care. Health Services Research. 2002;37:667–682. doi: 10.1111/1475-6773.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DeJong G. Physical Therapy Activities in Stroke, Knee Arthroplasty, and Traumatic Brain Injury Rehabilitation: Their Variation, Similarities, and Association With Functional Outcomes. 2011 doi: 10.2522/ptj.20100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.FitzGerald JD, Boscardin WJ, Ettner SL. Changes in regional variation of Medicare home health care utilization and service mix for patients undergoing major orthopedic procedures in response to changes in reimbursement policy. Health Services Research. 2009;44:1232–1252. doi: 10.1111/j.1475-6773.2009.00983.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freburger JK, Holmes GM, Ku LJE, Cutchin MP, Heatwole-Shank K, Edwards LJ. Disparities in Post-Acute Rehabilitation Care for Joint Replacement. Arthritis Care & Research. 2011;63:1020–1030. doi: 10.1002/acr.20477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freburger JK, Holmes GM, Ku LJ, Cutchin MP, Heatwole-Shank K, Edwards LJ. Disparities in Postacute Rehabilitation Care for Stroke: An Analysis of the State Inpatient Databases. Arch Phys Med Rehabil. 2011;92:1220–1229. doi: 10.1016/j.apmr.2011.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeJong G, Hsieh CH, Gassaway J, et al. Characterizing rehabilitation services for patients with knee and hip replacement in skilled nursing facilities and inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2009;90:1269–1283. doi: 10.1016/j.apmr.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 28.DeJong G, Tian W, Smout RJ, et al. Long-term outcomes of joint replacement rehabilitation patients discharged from skilled nursing and inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2009;90:1306–1316. doi: 10.1016/j.apmr.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 29.DeJong G, Horn SD, Smout RJ, Tian W, Putman K, Gassaway J. Joint replacement rehabilitation outcomes on discharge from skilled nursing facilities and inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2009;90:1284–1296. doi: 10.1016/j.apmr.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 30.Latham NK, Jette DU, Coster W, et al. Occupational therapy activities and intervention techniques for clients with stroke in six rehabilitation hospitals. Am J Occup Ther. 2006;60:369–378. doi: 10.5014/ajot.60.4.369. [DOI] [PubMed] [Google Scholar]
- 31.Dowla N, Chan L. Improving Quality in Stroke Rehabilitation. Top Stroke Rehabil. 2010;17:230–238. doi: 10.1310/tsr1704-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anderson JG. Demographic factors affecting health services utilization: a causal model. Medical Care. 1973;11:104–120. doi: 10.1097/00005650-197303000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Foster M, Tilse C. Referral to rehabilitation following traumatic brain injury: a model for understanding inequities in access. Social Science & Medicine. 2003;56:2201–2210. doi: 10.1016/s0277-9536(02)00236-8. [Review] [55 refs]. [DOI] [PubMed] [Google Scholar]
- 34.Strasser D. Unraveling the Conundrum of Quality. Top Stroke Rehabil. 2010;17:225–229. doi: 10.1310/tsr1704-225. [DOI] [PubMed] [Google Scholar]
- 35.Kane RL, Radosevich DM. Conducting Health Outcomes Research. Sudbury MA: Jones and Bartlett Learning; 2013. Models and Causal Thinking; pp. 25–38. [Google Scholar]
- 36.UDSMR. Uniform Data System for Medical Rehabilitation. [Accessed April 24, 2007];2007 http://udsmr org [serial online] [Google Scholar]
- 37.Granger CV, Markello SJ, Graham JE, Deutsch A, Ottenbacher KJ. The Uniform Data System for Medical Rehabilitation Report of Patients with Stroke Discharged from Comprehensive Medical Programs in 2000–2007. Am J Phys Med Rehabil. 2009;88:961–972. doi: 10.1097/PHM.0b013e3181c1ec38. [DOI] [PubMed] [Google Scholar]
- 38.Ottenbacher KJ, Smith PM, Illig SB, Fiedler RC, Gonzales V, Granger CV. Characteristics of persons rehospitalized after stroke rehabilitation. Arch Phys Med Rehabil. 2001;82:1367–1374. doi: 10.1053/apmr.2001.26088. [DOI] [PubMed] [Google Scholar]
- 39.Ottenbacher KJ, Smith PM, Illig SB, Linn RT, Ostir GV, Granger CV. Trends in length of stay, living setting, functional outcome, and mortality following medical rehabilitation. JAMA. 2004;292:1687–1695. doi: 10.1001/jama.292.14.1687. [DOI] [PubMed] [Google Scholar]
- 40.Reistetter TA, Graham JE, Deutsch A, Granger CV, Markello S, Ottenbacher KJ. Utility of functional status for classifying community versus institutional discharges after inpatient rehabilitation for stroke. Arch Phys Med Rehabil. 2010;91:345–350. doi: 10.1016/j.apmr.2009.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.UB Foundation Activities. The Inpatient Rehabilitation Facility - Patient Assessment Instrument (IRF-PAI) Training Manual. 2004 http://www cms hhs gov/InpatientRehabFacPPS/downloads/irfpaimanual040104 pdf [serial online] Available from: Centers for Medicare and Medicaid Services.
- 42.US Department of Education. Federal Register. No 151. Vol 72. Washington DC: 2007. [Google Scholar]
- 43.Carod-Artal FJ, Medeiros MS, Horan TA, Braga LW. Predictive factors of functional gain in long-term stroke survivors admitted to a rehabilitation programme. Brain Injury. 2005;19:667–673. doi: 10.1080/02699050400013626. [DOI] [PubMed] [Google Scholar]
- 44.Foley N, McClure JA, Meyer M, Salter K, Bureau Y, Teasell R. Inpatient rehabilitation following stroke: amount of therapy received and associations with functional recovery. Disabil Rehabil. 2012;34:2132–2138. doi: 10.3109/09638288.2012.676145. [DOI] [PubMed] [Google Scholar]
- 45.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77:1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 46.Turhan N, Atalay A, Muderrisoglu H. Predictors of functional outcome in first-ever ischemic stroke: a special interest to ischemic subtypes, comorbidity and age. Neurorehabilitation. 2009;24:321–326. doi: 10.3233/NRE-2009-0485. [DOI] [PubMed] [Google Scholar]
- 47.Atalay A, Turhan N. Determinants of length of stay in stroke patients: a geriatric rehabilitation unit experience. International Journal of Rehabilitation Research. 2009;32:48–52. doi: 10.1097/MRR.0b013e32830d3689. [DOI] [PubMed] [Google Scholar]
- 48.Carter GM, Totten ME. Preliminary analysis for refinement of the tier comorbidities in the inpatient rehabilitation facility prospective payment system. Santa Monica, CA: Rand Corporation; 2005. [Google Scholar]
- 49.Graham JE, Ripsin CM, Deutsch A, et al. Relationship between diabetes codes that affect Medicare reimbursement (tier comorbidities) and outcomes in stroke rehabilitation. Arch Phys Med Rehabil. 2009 doi: 10.1016/j.apmr.2009.01.014. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reistetter TA, Graham JE, Deutsch A, Markello SJ, Granger CV, Ottenbacher KJ. Diabetes Comorbidity and Age Influence Rehabilitation Outcomes After Hip Fracture. Diabetes Care. 2011;34:1375–1377. doi: 10.2337/dc10-2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Center for Medicare and Medicaid Services. Center for Medicare and Medicaid Services: Regional Offices. [Accessed February 4];2009 http://www cms hhs gov/InpatientRehabFacPPS/downloads/irfpaimanual040104 pdf [serial online] 10 A.D.
- 52.Hosmer D, Lemeshow S. Applied Logistic Regression. 2nd ed. New York: John Wiley & Sons; 2000. [Google Scholar]
- 53.ESRI. ArcGIS Desktop: Release 10. Redlands, CA: Environmental Systems Research Institute; 2011. [Google Scholar]
- 54.Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Washington, DC: 2011. [Google Scholar]
- 55.Bhandari VK, Kushel M, Price L, Schillinger D. Racial disparities in outcomes of inpatient stroke rehabilitation. Arch Phys Med Rehabil. 2005;86:2081–2086. doi: 10.1016/j.apmr.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 56.Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 57.Buntin MB. Access to postacute rehabilitation. Arch Phys Med Rehabil. 2007;88:1488–1493. doi: 10.1016/j.apmr.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 58.Department of Health and Human Services. Inpatient Rehabilitation Facility Prospective Payment System for FY 2006 Final Rule. Washington DC: 2005. Federal Register: Medicare Program. [PubMed] [Google Scholar]
- 59.Beninato M, Gill-Body KM, Salles S, Stark PC, Black-Schaffer RM, Stein J. Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Arch Phys Med Rehabil. 2006;87:32–39. doi: 10.1016/j.apmr.2005.08.130. [DOI] [PubMed] [Google Scholar]
- 60.Donabedian A. Evaluating the quality of medical care. Milbank Quarterly. 2005;83:691–729. doi: 10.1111/j.1468-0009.2005.00397.x. 1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hoenig H, Lee J, Stineman M. Conceptual Overview of Frameworks for Measuring Quality in Rehabilitation. Top Stroke Rehabil. 2010;17:239–251. doi: 10.1310/tsr1704-239. [DOI] [PubMed] [Google Scholar]
- 62.Deutsch A, Granger CV, Heinemann AW, et al. Poststroke rehabilitation: outcomes and reimbursement of inpatient rehabilitation facilities and subacute rehabilitation programs. Stroke. 2006;37:1477–1482. doi: 10.1161/01.STR.0000221172.99375.5a. [DOI] [PubMed] [Google Scholar]
- 63.Mutai H, Furukawa T, Araki K, Misawa K, Hanihara T. Factors associated with functional recovery and home discharge in stroke patients admitted to a convalescent rehabilitation ward. Geriatrics & gerontology international. 2012;12:215–222. doi: 10.1111/j.1447-0594.2011.00747.x. [DOI] [PubMed] [Google Scholar]
- 64.Denti L, Agosti M, Franceschini M. Outcome predictors of rehabilitation for first stroke in the elderly. European journal of physical & rehabilitation medicine. 2008;44:3–11. [PubMed] [Google Scholar]