Abstract
Background and Purpose
The last known normal (LKN) time is a critical determinant of IV tPA eligibility; however, the accuracy of EMS-reported LKN times is unknown. We determined the congruence between EMS-reported and neurologist-determined LKN times and identified predictors of incongruent LKN times.
Methods
We prospectively collected EMS-reported LKN times for patients brought into the ED with suspected acute stroke and calculated the absolute difference between the EMS-reported and neurologist-determined LKN times (|ΔLKN|). We determined the rate of inappropriate IV tPA use if EMS-reported times had been used in place of neurologist-determined times. Univariate and multivariable linear regression assessed for any predictors of prolonged |ΔLKN|.
Results
Of 251 patients, mean and median |ΔLKN| were 28 and 0 minutes, respectively. |ΔLKN| was <15 min in 91% of the entire cohort and was <15 min in 80% of patients with a diagnosis of stroke (n=86). Of patients who received IV tPA, none would have been incorrectly excluded from IV tPA if the EMS LKN time had been used. Conversely, of patients who did not receive IV tPA, 6% would have been incorrectly included for IV tPA consideration had the EMS time been used. In patients with wake-up stroke symptoms, EMS underestimated LKN times: mean EMS LKN time - neurologist LKN time = −208 minutes. The presence of wake-up stroke symptoms (p<0.0001) and older age (p=0.019) were independent predictors of prolonged |ΔLKN|.
Conclusions
EMS-reported LKN times were largely congruent with neurologist-determined times. Focused EMS training regarding wake-up stroke symptoms may further improve accuracy.
Keywords: Last Known Normal Time, Emergency Medical Services, Acute Stroke, Wake-Up Stroke
Background and Purpose
The correct identification of a patient’s “last known normal” (LKN) time is critical for determining a patient’s eligibility for time-dependent acute ischemic stroke treatments such as intravenous (IV) tPA.1 The American Heart Association recently provided guidelines for the “Early Management of Patients with Acute Ischemic Stroke” which included specific recommendations on “Prehospital Evaluation”, suggesting that Emergency Medical Services (EMS) responders should determine “time of symptom onset or last known normal, and obtain family contact information, preferably a cell phone”.2 The National Association of EMS Physicians additionally recommends that EMS “personnel should be skilled in the performance of prehospital stroke screening and in determining the timing, onset, and nature of symptoms.3, 4 Routinely, the LKN time is independently gathered by both EMS at the scene as well as by physicians after a patient’s arrival to the emergency department (ED). When the patient can give a history or when witnesses are immediately available, verification of LKN time is easily performed; however, not infrequently, physicians have difficulty with verification in patients with aphasia and when witnesses are not immediately available. At our institution EMS does not routinely transport the family or witnesses of acute stroke patients, so the initial stroke evaluation frequently occurs prior to the arrival of collateral sources. In these cases, decisions regarding IV tPA administration are delayed leading to prolongation of door-to-needle times (DNT).
Ideally, EMS-reported LKN times could be relied upon by physicians, allowing for expedited therapeutic decision making. While studies have assessed the accuracy of EMS in diagnosing acute stroke in the field,5, 6 the accuracy of EMS in gathering specific stroke-related information (such as LKN time) has not been well studied. In non-selected adult and pediatric populations, several studies have evaluated accuracy of EMS-reported data. One study evaluated the accuracy of EMS-collected demographic information including name, date of birth, and social security number for all-comers to a single emergency department. 7 The overall accuracy in data collected was 74%; varying from 33% for social security number to 83% for patient name. The accuracy of pediatric weight estimates by EMS was evaluated in children needing prehospital medication administration en-route, demonstrating 82% accuracy for EMS weight estimates (within 20% of actual weights).8 In addition to inaccurate or neglected data collection in the field, information may be lost when EMS communicates patient data to the ED hospital personnel. A study of trauma patients found that only 73% of key information (including vital signs and Glasgow coma scale) verbally transmitted by EMS was received and documented accurately by ED hospital staff.9
In 2010, we performed a detailed review of our hospital’s acute stroke protocol to identify which factors contribute to prolonged DNT or prevent patients from being treated with IV tPA due to falling outside of the IV tPA window.10 Of several factors, contacting witnesses (in person or by phone) to confirm the EMS-reported LKN time was identified as a potential source of delay. In this study, we compared the congruence of EMS-reported and neurologist-determined LKN times, assessing which variables may predict incongruence so as to direct future EMS education.
Methods
Data Collection
Patient data were prospectively collected from a large, urban, tertiary care hospital and comprehensive stroke center in St. Louis, Missouri. The LKN times provided by EMS were prospectively recorded from August 2010 to August 2012 by stroke research coordinators who attend acute stroke pager activations in the ED during weekday daytime hours. Data were not collected when the stroke research coordinators were unable to attend acute stroke activations due to being out of the hospital after hours or if other research responsibilities prevented them from going to the ED. The acute stroke pager is activated by the nurses in the ED Communication Center taking calls from EMS or by the triage nurse who is assessing walk-in patients (the current cohort did not include any walk-in patients, only EMS-transported patients). An extensive list of symptoms (i.e., “weakness” or “vision changes”) may lead to activation in order to include all potential patients who may be candidates for acute stroke therapies. Clinical data were prospectively collected as part of the Cognitive Rehabilitation Research Group (CRRG) Stroke Registry developed at Washington University in 1998. This registry includes the following clinical information: demographics; past medical history; ED diagnosis (as determined by the neurologist covering the ED which includes ischemic stroke, transient ischemic attack (TIA), intracerebral hemorrhage (ICH), or other non-stroke diagnosis); itemized National Institutes of Health Stroke Scale (NIHSS) obtained on ED arrival; and several metrics including the LKN time as determined by the neurology resident evaluating the patient, patient arrival time in the ED, neurologist-evaluation time, and DNT for IV tPA-treated patients. In addition, the variable of “wake-up” stroke symptoms was retrospectively obtained by physician review (DRC) of the neurology consultation note in the ED medical record without knowledge of the individual EMS-reported LKN times collected by the stroke coordinators.
EMS Training
The majority of EMS agencies in the Greater St. Louis catchment area of this urban, tertiary care hospital require a minimum of annual training in the rapid response of suspected stroke patients and are trained to utilize the Los Angeles Pre-Hospital Stroke Scale for stroke screening. EMS personnel are trained to prenotify the ED of any suspected stroke in transit. A minority of patients within this cohort were transported from rural EMS agencies which have more variable EMS training and protocols for suspected stroke patients. In the two years prior to collecting EMS LKN times (from 5/2008 to 5/2010), several EMS agencies in the St. Louis area were targeted for additional stroke-specific training as part of the NIH-funded Specialized Programs of Translational Research in Acute Stroke (SPOTRIAS) network. During this time, biannual training sessions were conducted at EMS and fire departments in the Greater St. Louis region. These continuing education courses were conducted by an ED physician (DKT) to improve EMS stroke symptom identification and train EMS in acute evaluation and prehospital notification for suspected acute stroke patients. Specific training was performed on how to determine time of symptom onset and who may have witnessed the onset; however, no specific training was provided with respect to wake-up stroke symptoms.
Physician Training
The acute tPA evaluation is performed by neurology residents in conjunction with ED residents. 10, 11 Supervision is provided by ED attendings (who are physically present) and stroke attendings (who are always available by phone if not physically present). All neurology residents are required to attend acute stroke training and obtain NIHSS certification prior to beginning their neurology training. The annual training includes: (1) National Institute of Health Stroke Scale (NIHSS) training; (2) review of NINDS and ECASS-3 tPA study protocols 12,13; (3) review of data on outcome as a function of early treatment14; and (4) several case studies of patients treated with tPA. This training emphasizes independent determination of the LKN time from the most reliable source (patient first, followed by a witness if the patient demonstrates altered mental status or aphasia), rather than using the EMS-reported LKN time or any other second-hand source. In addition, a quality-control committee comprised of a stroke attending, ED attendings, neurology chief resident, ED clinical nurse manager, and ED clinical pharmacist meet monthly to review all IV tPA cases, providing feedback to treating resident physicians and ED staff.
Statistical Analysis
For patients brought into the ED by EMS with suspected stroke, the absolute difference between EMS-reported LKN time and neurologist-determined LKN time (|ΔLKN|) was calculated for each patient. Numbers of patients with |ΔLKN| < 15 min were calculated (an error window of 15 minutes was chosen as a short time window which would be unlikely to adversely affect tPA-related or other clinical-decision making). IV tPA error rates (defined as inappropriate use of IV tPA if the EMS-reported LKN times had been used in place of the neurologist-determined times) were calculated to determine if using the EMS-reported LKN time would have incorrectly placed a patient either within or outside of the 4.5 hour time window for IV tPA, irrespective of other clinical inclusion/exclusion criteria. To assess for predictors of prolonged |ΔLKN|, univariate regression analysis was performed between |ΔLKN| and several variables including: age, gender, race, total baseline NIHSS, NIHSS item1a (level of consciousness) and item 9 (best language), onset-to-ED arrival time (when prolonged may indicate lack of a witness and difficulty in determining an accurate LKN time), the presence of wake-up stroke symptoms, and if the patient was brought by an EMS agency that had stroke-specific training. A linear multivariable regression model was then created to fit |ΔLKN| using a forward stepwise procedure to select candidate predictors, with a p≤0.20 required for entry and p≤0.05 required to be retained. For each variable, β=Regression Coefficient and (SE)=standard error. A chi-square test was used to compare the frequency of patients with |ΔLKN| >15 minutes between wake-up and non-wake up stroke symptom patients. Statistical analysis was performed using SPSS v. 19.
Results
Patient characteristics
EMS-reported LKN times were prospectively collected for 251 acute stroke pager activations. Baseline characteristics are shown in Table 1. Of the 251 patients, 34% carried an ED diagnosis of ischemic stroke (N=86) and 37% of this latter group was treated with IV tPA (N=32). The St. Louis EMS agencies with additional stroke-specific training over a two year period prior to this data collection transported 61% of patients within the cohort (N=153).
Table 1.
Baseline Characteristics of All Acute Stroke Alerts with Neurologist and EMS-reported LKN times
| Baseline Characteristics | N = 251 |
|---|---|
| Mean Age in Years ± SD | 65 ± 18 |
| Female Gender, n (%) | 143 (57%) |
| African American Race, n (%) | 141 (56%) |
| ED NIHSS on arrival for entire cohort, median [IQR] | 4.5 [1,9] |
| ED NIHSS on arrival for patients with stroke diagnosis, median [IQR] | 8 [5,14] |
| Final ED Diagnosis determined by Evaluating Neurologist | |
| Ischemic Stroke, n (%) | 86 (34%) |
| Hemorrhagic Stroke, n (%) | 16 (6%) |
| TIA, n (%) | 27 (11%) |
| Other/Unknown Diagnosis, n (%) | 120 (48%) |
| Patients with Final ED Diagnosis of Ischemic stroke who received IV tPA, n (%) | 32 (37%) |
| Patients brought in by EMS agency that had additional stroke-specific training vs. other EMS agency, n (%) | 153 (61%) |
Comparison of EMS-Reported and Neurologist-Determined LKN Times and IV tPA Error Rates if EMS-reported Times had been Used in Clinical Decision-Making
For all 251 acute stroke pager activations, mean and median |ΔLKN| times were 28 minutes and 0 minutes, respectively. EMS-reported and neurologist-determined LKN times agreed within 15 minutes 91% of the time. For the subgroup of patients with a final ED diagnosis of stroke (N=86), |ΔLKN| was < 15 minutes 80% of the time. Of patients with an ED diagnosis of stroke and who received IV tPA, none (0%) would have been incorrectly excluded from IV tPA if EMS-reported LKN times had been used in place of physician LKN times. Of stroke patients who did not receive IV tPA, 3 (6%) would have been incorrectly included for IV tPA administration if the EMS-reported LKN times had been used for clinical decision-making (Table 2).
Table 2.
Differences between EMS-reported and neurologist-determined LKN Times and IV tPA error rates
| All Acute Stroke Pager Activations n = 251 |
Patients with ED Diagnosis of Stroke n = 86 |
IV tPA – Treated Stroke Patients n = 32 |
Non IV tPA-Treated Stroke Patients n = 54 |
|
|---|---|---|---|---|
| |ΔLKN|*, mean ± SD | 28 ± 109 | 36 ± 132 | 12 ± 29 | 57 ± 165 |
| |ΔLKN|, median [IQR] | 0 [0,0] | 0 [0,0] | 0 [0,0] | 0 [0,0] |
| |ΔLKN| < 15 min, n (%) | 229 (91%) | 69 (80%) | 27 (84%) | 42 (78%) |
| Incorrectly included for IV tPA administration if EMS-reported LKN times were used, n (%) | N/A | 3 (6%) | ||
| Incorrectly excluded for IV tPA administration if EMS-reported LKN times were used, n (%) | 0 (0%) | N/A |
|ΔLKN| = absolute difference in EMS-reported and neurologist-determined last known normal times
SD = Standard Deviation; [IQR] = [25th percentile, 75th percentile]
Predictors of LKN Incongruence between EMS and Neurologists
Regression analysis identified only three potential predictors of prolonged |ΔLKN| on univariate analysis: older age (p=0.17), onset-to-ED-arrival time (p<0.001), and presence of wake-up stroke symptoms (p<0.0001). Older age and wake-up stroke symptoms were found to be independent predictors of |ΔLKN| in multivariable analysis: (1) age [β(SE) = 0.778 (0.330), p=0.016] and (2) wake-up stroke symptoms [β (SE) = 226.5 (35.7), p<0.0001] (Table 3). Other variables such as NIHSS items 1a (altered consciousness) or item 9 (aphasia) or being transported by EMS agencies that had received specific stroke training were not associated with incongruence of LKN times.
Table 3.
Predictors of prolonged |ΔLKN| between EMS-reported and neurologist-determined LKN times
| Univariate Predictors of prolonged |ΔLKN| | Multivariable Predictors of prolonged |ΔLKN| | |
|---|---|---|
| Age | p=0.17 | β (SE) = 0.778 (0.330), p=0.016 |
| Female gender | p=0.57 | Not included |
| African American | p=0.35 | Not included |
| Admission NIHSS | p=0.90 | Not included |
| Item 1A on NIHSS: Altered LOC | p=0.39 | Not included |
| Item 9 on NIHSS: Aphasia | p=0.71 | Not included |
| Onset-to-Arrival Time | p<0.001 | p=0.92 |
| Wake-Up Stroke Symptoms, n (%) | p<0.0001 | β (SE) = 226.5 (35.7), p<0.0001 |
| Brought in by EMS agency that had Stroke-Specific Training | p=0.54 | Not included |
|ΔLKN| = absolute difference in EMS-reported and neurologist-determined last known normal times
β (SE) = Regression Coefficient (Standard Error)
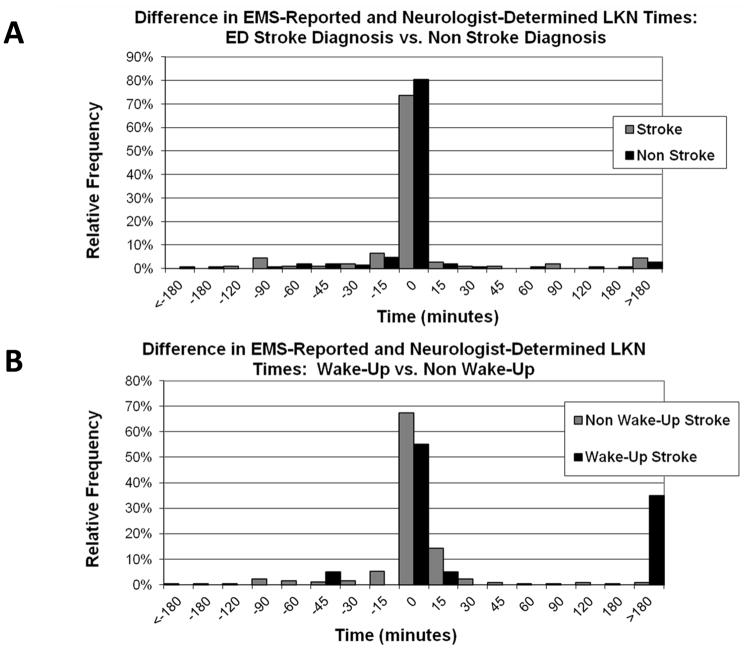
Further characterization of patients with wake-up stroke symptoms revealed that EMS was significantly underestimating the LKN time in wake-up stroke patients by equating the wake-up time with the time the patient was last known to be normal. The mean non-absolute difference in LKN times (EMS-reported – neurologist-determined) for patients with wake-up stroke symptoms was −207 minutes. Wake-up stroke patients had less congruence in LKN times between EMS and neurologists compared to non-wake up stroke patients: |ΔLKN| time < 15 minutes in only 47% of wake-up compared to 85% of non-wake up stroke patients; (p < 0.001). Moreover, of the patients who would have been incorrectly included for tPA administration if EMS-reported times had been used, all were wake-up stroke patients. Histograms of patients distributed across ΔLKN time (−180 minutes to 180 minutes) were plotted for stroke vs. non-stroke patients (Figure, A) and for wake-up vs. non-wake up patients (Figure, B). While the distributions for stroke vs. non-stroke patients are similar, distributions for wake-up vs. non-wake-up patients differ, indicating greater inaccuracy for EMS when determining LKN for wake-up stroke patients.
Figure.
Frequency histograms for the differences in EMS-reported and neurologist-determined LKN times (ΔLKN) for: (A) patients with an ED diagnosis of Stroke (gray) compared to Non-Stroke (black) and (B) patients without wake-up stroke symptoms (gray) and with wake-up stroke symptoms (black).
Discussion
Our study suggests that well-trained EMS providers frequently obtain LKN times similar to those determined by the neurology team in patients with suspected acute stroke. Given that EMS may have direct contact with witnesses, it would be useful if EMS-reported times could be relied upon in instances when these individuals cannot be efficiently reached by physicians once the patient arrives in the ED. This study evaluated several variables that may impact accurate determination of LKN times. Of the baseline demographic factors, older age was found to be a predictor of LKN incongruence. Advanced age is associated with living alone and social isolation;15 accordingly, older patients may be less likely to have a witness on scene to convey a LKN time to EMS. The variable that most significantly impacted LKN congruence between EMS and neurologists was the presence of wake-up stroke symptoms. EMS underestimated the LKN time by reporting the awakening time as the LKN time rather than the time the patient was known to be normal the day prior. Given this finding, continued education on obtaining LKN times with particular inquiry into the presence of symptoms on awakening may improve the accuracy of EMS-reported LKN times. An additional variable that was associated with LKN accuracy on univariate analysis (but not an independent predictor on multivariable analysis) was onset-to-ED-arrival time. When a patient presents late to the ED, this may indicate that no witness was present at the time of stroke onset and therefore may make it more difficult to determine an accurate LKN time both by neurologists and EMS. Variables assessing stroke severity (total NIHSS) and specific markers of altered consciousness or aphasia (itemized NIHSS) were not identified as predictors of LKN inaccuracy. This may suggest that EMS personnel are correctly assessing patients with respect to the presence of altered mental status or aphasia and are appropriately seeking out a witness to provide this time. We found that the EMS LKN times from agencies that had received additional stroke-specific training were not more accurate than EMS LKN times from untrained sites. This is likely due to the training having been performed two years prior to our study, during which personnel turnover and loss of the learned material may have occurred. Moreover, while the additional stroke-specific training did include training on obtaining onset time, there was not specific training on investigating wake-up stroke symptoms.
It is well known that prehospital notification by EMS decreases several hospital-based patient metrics including arrival to patient evaluation, CT completion, and IV tPA treatment times, likely by increasing team preparedness prior to patient arrival. 16–19 Accordingly, current guidelines for acute stroke management recommend initiation of stroke management in the field and prehospital communication with receiving hospitals to optimize mobilization of stroke resources.2–4 Given that the ultimate goal of such guidelines is to minimize the time from stroke onset to tPA administration, the most efficient and accurate way to determine tPA eligibility would ideally involve direct communication between EMS personnel at the scene and the treating ED or neurology physicians. However, at present, mechanisms to support this direct line of communication are not commonly available outside of research settings. Until such systems are in place, EMS will frequently be the only contact with collateral sources within the time frame necessary for determining a patient’s eligibility for tPA. If future studies demonstrate high congruence between EMS-reported and physician-determined LKN times, then EMS-reported LKN times could be utilized more frequently to avoid prolonged DNT and excluding patients from treatment who should have been included.
Beyond a small sample size, the study has additional methodological limitations. Patient information was collected as a convenience sample by stroke research coordinators during daytime hours on weekdays and thus does not include data on any patients who presented overnight or on weekends; thus, our results may not be valid during off-hours, if witnesses are more difficult to contact during off-hours. While the current data are likely generalizable to other large, urban, tertiary care hospitals, at least two factors limit the generalizability of our results to other institutions and regions: (1) the majority of patients in our cohort were transported by EMS agencies that have undergone additional stroke-specific education two years prior to our data collection and (2) a minority of patients were brought into our institution from rural EMS agencies outside of the greater St. Louis region which likely have more variable stroke screening and training protocols. Thus, it would be important to assess the overall accuracy of determining LKN times within other cohorts. Finally, the neurologist-determined LKN time was considered the gold-standard which may not always be correct. Given the systematic physician training on determining LKN times at our institution, however, we believe that error in the neurologist-determined times was minimized.
Conclusions
LKN times obtained by EMS personnel were similar to neurologist-determined times; however these findings need to be confirmed in larger cohorts across different regions. Future EMS training with regard to inquiring about wake-up stroke symptoms may improve the accuracy of EMS-reported LKN times.
Acknowledgments
We would like to acknowledge the efforts of the Washington University neurology and ED residents, Stroke Research Coordinators, and the St. Louis metropolitan area EMS providers.
Funding: This study was supported by NIH K23NS069807 to AF and NIH 5P50NS055977 to DKT, JML, and PP.
Footnotes
Disclosures: None
References
- 1.Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from tpa therapy? An analysis of patient eligibility. Neurology. 2001;56:1015–1020. doi: 10.1212/wnl.56.8.1015. [DOI] [PubMed] [Google Scholar]
- 2.Jauch EC, Saver JL, Adams HP, Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 3.Naemsp. Naemsp position statement. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2007;11:312. [Google Scholar]
- 4.Crocco TJ, Grotta JC, Jauch EC, Kasner SE, Kothari RU, Larmon BR, et al. Ems management of acute stroke--prehospital triage (resource document to naemsp position statement) Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2007;11:313–317. doi: 10.1080/10903120701347844. [DOI] [PubMed] [Google Scholar]
- 5.Ramanujam P, Guluma KZ, Castillo EM, Chacon M, Jensen MB, Patel E, et al. Accuracy of stroke recognition by emergency medical dispatchers and paramedics--san diego experience. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2008;12:307–313. doi: 10.1080/10903120802099526. [DOI] [PubMed] [Google Scholar]
- 6.Kothari R, Barsan W, Brott T, Broderick J, Ashbrock S. Frequency and accuracy of prehospital diagnosis of acute stroke. Stroke. 1995;26:937–941. doi: 10.1161/01.str.26.6.937. [DOI] [PubMed] [Google Scholar]
- 7.Brice JH, Friend KD, Delbridge TR. Accuracy of ems-recorded patient demographic data. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2008;12:187–191. doi: 10.1080/10903120801907687. [DOI] [PubMed] [Google Scholar]
- 8.Lim CA, Kaufman BJ, O’Connor J, Jr, Cunningham SJ. Accuracy of weight estimates in pediatric patients by prehospital emergency medical services personnel. Am J Emerg Med. 2013;31:1108–1112. doi: 10.1016/j.ajem.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 9.Carter AJ, Davis KA, Evans LV, Cone DC. Information loss in emergency medical services handover of trauma patients. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2009;13:280–285. doi: 10.1080/10903120802706260. [DOI] [PubMed] [Google Scholar]
- 10.Ford AL, Williams JA, Spencer M, McCammon C, Khoury N, Sampson TR, et al. Reducing door-to-needle times using toyota’s lean manufacturing principles and value stream analysis. Stroke. 2012;43:3395–3398. doi: 10.1161/STROKEAHA.112.670687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ford AL, Connor LT, Tan DK, Williams JA, Lee JM, Nassief AM. Resident-based acute stroke protocol is expeditious and safe. Stroke. 2009;40:1512–1514. doi: 10.1161/STROKEAHA.108.527770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tissue plasminogen activator for acute ischemic stroke. The national institute of neurological disorders and stroke rt-pa stroke study group. N Engl J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 13.Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 14.Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: Pooled analysis of atlantis, ecass, and ninds rt-pa stroke trials. Lancet. 2004;363:768–774. doi: 10.1016/S0140-6736(04)15692-4. [DOI] [PubMed] [Google Scholar]
- 15.Nicholson NR. A review of social isolation: An important but underassessed condition in older adults. J Prim Prev. 2012;33:137–152. doi: 10.1007/s10935-012-0271-2. [DOI] [PubMed] [Google Scholar]
- 16.Abdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LH. Advance hospital notification by ems in acute stroke is associated with shorter door-to-computed tomography time and increased likelihood of administration of tissue-plasminogen activator. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2008;12:426–431. doi: 10.1080/10903120802290828. [DOI] [PubMed] [Google Scholar]
- 17.Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2012;5:514–522. doi: 10.1161/CIRCOUTCOMES.112.965210. [DOI] [PubMed] [Google Scholar]
- 18.McKinney JS, Mylavarapu K, Lane J, Roberts V, Ohman-Strickland P, Merlin MA. Hospital prenotification of stroke patients by emergency medical services improves stroke time targets. J Stroke Cerebrovasc Dis. 2013;22:113–118. doi: 10.1016/j.jstrokecerebrovasdis.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 19.Prabhakaran S, O’Neill K, Stein-Spencer L, Walter J, Alberts MJ. Prehospital triage to primary stroke centers and rate of stroke thrombolysis. JAMA neurology. 2013;70:1126–1132. doi: 10.1001/jamaneurol.2013.293. [DOI] [PubMed] [Google Scholar]