Abstract
This study assessed the patterns of nonhospice health care utilization among 207 deceased cancer patients and focused on outcomes after cancer treatment was stopped. A total of 117 (57%) were enrolled in hospice. The mean cumulative number of emergency department visits, hospitalizations, or other noncancer clinic visits (standard deviation) among those enrolled and not enrolled in hospice was 1.8 (± 1.8) and 3.11 (± 3.0), respectively (P < .0001). Among hospice enrollees, the mean cumulative visits (standard deviation) was 1.29 (± 1.7) and 0.5 (± 1.0) before and after enrollment, respectively (P < .0001). For patients who eventually enrolled, the rates of nonhospice health care visits (visits per week) yielded a trend to suggest a decline (P = .054). Hospice was associated with a drop in nonhospice-related health care utilization, thus suggesting it provides timely medical interventions and favorable continuity of care.
Keywords: hospice, end of life, cancer, health care utilization
Hospice has become the paradigm for high-quality end-of-life care.1 A robust literature describes how patients with cancer and noncancer patients who enroll in hospice consume less health care resources and, not surprisingly, generate less health care expenditure.2,3 In fact, a recent study from Carlson et al demonstrated that disenrollment from hospice is associated with greater use of health care resources and a rise in health care expenditures in patients with cancer.4 To our knowledge, however, previous studies have not yet evaluated the converse situation, namely, whether enrollment in hospice is associated with a decline in emergency department visits, hospitalizations, and other outpatient medical visits in patients with cancer, after they stop cancer treatment. Such information might provide further insight into the role of hospice at the end of life.
This last issue is an important one. Nationally, over 60% of the patients with cancer are never enrolled in hospice.5 These patients must resort to a variety of other venues for health care. These patients seem especially vulnerable, acquiring such care, in part, by means of visits to the emergency department and admissions to the hospital. The former often leads to a lack of continuity of care and inconvenience, as patients typically see a different health care provider during each emergency department visit and their waiting times can be long.6 Knowing whether hospice truly circumvents these other, less favorable options after patients stop cancer treatment and appears to provide greater continuity of care and more expeditious health care would be of value.
In this context, the current study had a singular purpose. Its primary goal was to examine patterns of health care utilization and specifically to examine whether enrollment of end-of-life patients with cancer in hospice was associated with a decrease in other, less optimal health care utilization.
Patients and Methods
Overview
This single-institution study relied on a retrospective review of medical records. Patients who had died between January 2005 and September 2011 were the focus of this report. The Mayo Clinic Tumor Registry provided a list of deceased cancer patients who met this criterion as well as the eligibility criteria described subsequently. Information on death was gathered from the Social Security Death Index as well as from supplemental sources on vital status, such as the Mayo Clinic medical record. The Mayo Clinic Institutional Review Board deemed this study exempt.
Eligibility
This study was restricted to decedents ≥18 years of age. Only patients who were residing within Olmsted County, Minnesota, at time of cancer diagnosis and who had received chemotherapy at the Mayo Clinic were included. The rationale for these last 2 criteria rested on the fact that subsequent hospitalization and hospice enrollment would be more accurately documented in the Mayo Clinic medical record under such circumstances.
Medical Record Review
All medical records were reviewed in depth by one author (E.K.S.), and the study data were extracted by hand. Another author (A.J.) re-reviewed select medical records to check the accuracy of data abstraction. The following information was extracted from each record: patient gender; race; marital status at death; dates of birth, cancer diagnosis, and death; types of cancer treatment administered (surgery, radiation, transplantation, chemotherapy); date of last cancer chemotherapy; date of last oncology clinic note and whether that note recommended stopping cancer treatment (yes, no, unable to determine); whether the patient was enrolled in hospice and, if so, the date of enrollment; and number of emergency department visits, hospitalizations, and noncancer health care provider clinical visits since enrollment in hospice. The latter types of health care visits were recorded because they were considered to be the most frequent and the most encompassing of the major of medical visits that a patient with cancer would utilize at the end of life. In the event a patient was evaluated in the emergency department and then hospitalized, the emergency department visit was not counted in a conservative effort to avoid redundancy.
Statistical Analyses
The primary intention of this study was to provide descriptive data. However, limited statistical analyses were performed using SPSS version 20 (IBM Corporation, Chicago, Illinois). Descriptive data are presented as frequencies, percentages, medians, and means (± standard deviation). An independent sample t test was performed to compare the mean cumulative number of visits between those enrolled in hospice and those not enrolled after stopping cancer treatment. A paired sample t test was performed to compare the mean number of visits prior to and following hospice enrollment. Visit rates were also compared before (number of visits/weeks between last chemotherapy and hospice enrollment) and after hospice enrollment (number of visits/weeks between hospice enrollment and death) for those patients who had enrolled in hospice by means of a related samples Wilcoxon signed-rank test. A P value <.05 was deemed statistically significant.
Results
Demographics
A total of 207 deceased cancer patients were identified in the Tumor Registry as meeting the eligibility criteria described previously. The median age at death was 69 years (range 21–94 years). Additional patient characteristics are shown in Table 1.
Table 1.
Characteristics of Patients Who Died of Cancer.
| Characteristicsa | Hospice Enrollment
|
|
|---|---|---|
| Yes (n = 117) N (%)b | Noc (n = 90) N (%)b | |
| Sex | ||
| Male | 61 (52) | 46 (51) |
| Female | 56 (48) | 44 (49) |
| Marital status | ||
| Married | 86 (74) | 58 (64) |
| Widowed | 15 (13) | 9 (10) |
| Single (never married) | 6 (5) | 14 (16) |
| Divorced | 10 (8) | 9 (10) |
| Race/ethnicity | ||
| White | 101 (92) | 77 (85) |
| Asian/Pacific Islander | 3 (3) | 8 (9) |
| Hispanic | 3 (3) | 3 (3) |
| Black | 3 (3) | 1 (1) |
| Unknown | 0 (0) | 1 (1) |
| Cancer type | ||
| Thoracic | 36 (31) | 21 (23) |
| Gastrointestinal | 37 (32) | 13 (14) |
| Hematologic | 11 (9) | 35 (39) |
| Genitourinary | 12 (10) | 6 (7) |
| Breast/gynecologic | 10 (8) | 7 (8) |
| Brain | 8 (7) | 3 (3) |
| Other | 3 (3) | 5 (6) |
| Cancer treatmentd | ||
| Chemotherapy | 116 (99) | 88 (98) |
| Radiation | 66 (56) | 35 (39) |
| Surgery | 37 (32) | 15 (17) |
| Transplant | 7 (6) | 11 (12) |
At the time of patient death unless otherwise specified.
Percentages sometimes do not sum to 100 because of rounding.
Hospice enrollment could not be determined for 1 individual; but for descriptive purposes, this decedent is included here.
Under cancer treatment, the percentages do not sum to 100 as categories are not mutually exclusive; 63% of the patients received more than 1 treatment modality, most commonly chemotherapy plus radiation.
Among 147 (72%) of the 204 patients who received chemotherapy, the last cancer-related outpatient note recommended that cancer treatment be stopped because of lack of further viable treatment options. In all other patients, this recommendation was not made (22%) or it could not be determined from the note with certainty (6%). Seventeen (8%) patients received chemotherapy within 2 weeks of death.
Hospice and Related Outcomes
A total of 117 (57%) deceased cancer patients were enrolled in hospice. Analyses of demographics between those enrolled and not enrolled revealed no clinically and statistically significant findings, except for the fact that a greater proportion of patients who had previous radiation and/or surgery had enrolled in hospice (data not shown). With regard to timing, only 6% of the patients entered hospice at 2 weeks or less after the last chemotherapy. The median time between the last chemotherapy and enrollment into hospice was 7 weeks (range 0–111 weeks). The median time on hospice was 2 weeks (range 0–23 weeks).
The mean cumulative number of emergency department visits, hospitalizations, or other, noncancer clinic visits among patients enrolled and not enrolled in hospice was 1.8 (± 1.8) and 3.11 (± 3.0), respectively (P < .0001). Among patients who enrolled in hospice, the mean cumulative number of visits was 1.29 (± 1.7) prior to hospice enrollment and 0.5 (± 1.0) after enrollment (P < .0001). For patients who eventually enrolled in hospice, the rates of nonhospice health care visits, expressed as visits per week, yielded a trend to suggest a drop in nonhospice health care utilization, with a median event rate of 0.05 before hospice (range 0–7) and a median event rate after hospice of 0.00 (range 0–3; P = .054).
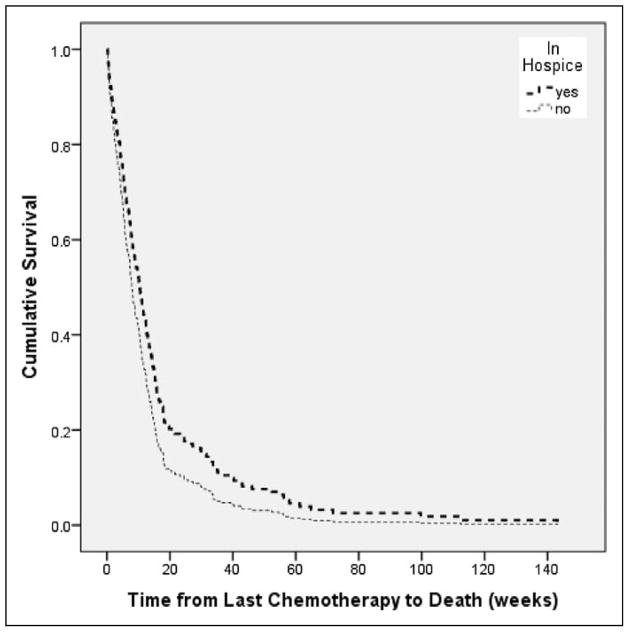
The median survival from last cancer treatment to death among patients enrolled in hospice was 12 weeks (range 0.29–112 weeks); in patients never enrolled, the median interval was 5 weeks (range 0.28–143 weeks; Figure 1).
Figure 1.
The median survival from last cancer treatment to death among patients enrolled in hospice was 12 weeks (range 0.29–112 weeks), as shown in the top curve; in patients never enrolled, this interval was 5 weeks (range 0.28–143 weeks), as shown in the bottom curve.
Discussion
This study sought to understand the patterns of nonhospice medical care among patients who had stopped cancer treatment both before and after enrollment in hospice. This study provides an important observation: enrollment in hospice is associated with a drop in nonhospice health care utilization. Although previous studies have shown that large groups of patients in hospice generate a lower degree of health care utilization and less cost and although a previous study shows an increase in health care utilization after hospice disenrollment, to our knowledge, our study is the first to suggest a temporal drop in health care utilization after enrollment in hospice.1–4 This observation is important because it suggests to patients and their families that hospice provides a reliable, end-of-life health care resource with timely medical interventions and favorable continuity of care. Some might argue that, by definition, hospice reduces health care utilization, but, to our knowledge, no prior studies apart from this one have actually shown that this reduction is actually occurring.
The current study has limitations, most notably the fact that its descriptive, retrospective design precludes any understanding of the bias that might be occurring between patients who chose hospice services and those who did not. Certainly, patients who chose hospice may be fundamentally different from those who did not, and the design of this study is such that those differences are unable to be discerned in a meaningful manner. Future prospective studies might be of value in understanding such differences.
Furthermore, the fact that hospice patients in our study appeared to survive longer than others is an important observation that merits further discussion. Importantly, our study design restricted our assessments only to deceased cancer patients, an approach that makes it impossible to provide a general statement that survival among patients who enroll in hospice is longer than it is in those who do not. Thus, although we observed longer survival among hospice enrollees, we cannot conclude from this study that hospice itself is associated with longer survival. Instead, we must continue to rely on a growing body of literature, which suggests hospice and palliative care are associated with a survival advantage.7–10 Again, a prospectively conducted study might be of value in understanding whether such survival differences truly exist and whether they would persist within a multivariate analysis.
In summary, this study observed that enrollment in hospice is associated with a drop in nonhospice health care utilization. Current practices suggest that incurable cancer patients are not always receiving hospice services even after the realization that no further cancer treatment is available. The findings from the current study provide further information that can be used to educate patients, family members, and perhaps even health care providers on yet another potential benefit of hospice.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by K24CAB1099.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Reprints and permission: sagepub.com/journalsPermissions.nav
References
- 1.Meier DE. Increased access to palliative care and hospice services: opportunities to improve value in health care. Milbank Q. 2011;89(3):343–380. doi: 10.1111/j.1468-0009.2011.00632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor DH. The effect of hospice on Medicare and informal care costs: the US Experience. J Pain Symptom Manage. 2009;38(1):110–114. doi: 10.1016/j.jpainsymman.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Pyenson B, Connor S, Fitch K, Kinzbrunner B. Medicare cost in matched hospice and non-hospice cohorts. J Pain Symptom Manage. 2004;28(3):200–210. doi: 10.1016/j.jpainsymman.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Carlson MD, Herrin J, Du Q, et al. Impact of hospice disenrollment on health care use and medicare expenditure for patients with cancer. J Clin Oncol. 2010;28(28):4371–4375. doi: 10.1200/JCO.2009.26.1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCarthy EP, Burns RB, Davis RB, Phillips RS. Barriers to hospice care among older patients dying with lung and colorectal cancer. J Clin Oncol. 2003;21(4):728–735. doi: 10.1200/JCO.2003.06.142. [DOI] [PubMed] [Google Scholar]
- 6.Cree M, Bell NR, Johnson D, Carriere KC. Increased continuity of care associated with decreased hospital care and emergency department visits for patients with asthma. Dis Manag. 2006;9(1):63–71. doi: 10.1089/dis.2006.9.63. [DOI] [PubMed] [Google Scholar]
- 7.Connor SR, Pyenson B, Fitch K, Spence C, Iwasaki K. Comparing hospice and non-hospice patient survival among patients who die within a three-year window. J Pain Symptom Manage. 2007;33(3):238–246. doi: 10.1016/j.jpainsymman.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Temel JS, Greer JA, Muzikansy A, et al. Early palliative care for patients with metastatic non-small cell lung cancer. N Engl J Med. 2010;363(8):733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 9.Skinner J. Is more care better care? The New York Times. 2009 Jun 13; [Google Scholar]
- 10.Saito AM, Landrum MB, Neville BA, Ayanian JZ, Earle CC. The effect of survival of continuing chemotherapy to near death. BMC Palliat Care. 2011;10:14. doi: 10.1186/1472-684X-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]