Abstract
A 23-year-old male was admitted with chest pain. The electrocardiogram showed ST elevation in leads DI, aVL, V2-V6. Troponin T was 1.1ng/mL. Left ventricular systolic function was globally reduced (ejection fraction 45%). The patient was treated with thrombolytic. Twenty-four hours after admission pruriginous vesicles with a clear content and surrounded by a pink halo appeared on his face, head and torso, suggesting varicella-zoster infection. This case illustrates the difficulties of diagnosis in acute myocarditis.
Keywords: varicella-zoster, myocardial infarction, myocarditis
Introduction
Infection with varicella-zoster virus is in most cases a self-limiting disease with rare but possibly severe cardiac complications.
We report the case of a patient with clinical findings of myocarditis mimicking myocardial infarction and infection by varicella-zoster virus.
Case report
The patient was a 23-year-old male, who arrived at the emergency unit complaining of constrictive precordial pain that irradiated to both shoulders and was accompanied by sweating and weakness for 2 hours. The patient reported a previous episode of chest pain, 12 hours ago, that lasted 20 minutes. The patient had no history of personal of family cardiovascular disease. He was non-smoker and he did not use illicit drugs or excessive alcohol.
On physical examination the patient was obese, slightly pale and sweating. The blood pressure was 110/80mmHg in both upper limbs, his heart rate was 110bpm; the lungs showed no rales, and the peripheral pulses were palpable. There was no pericardial rub.
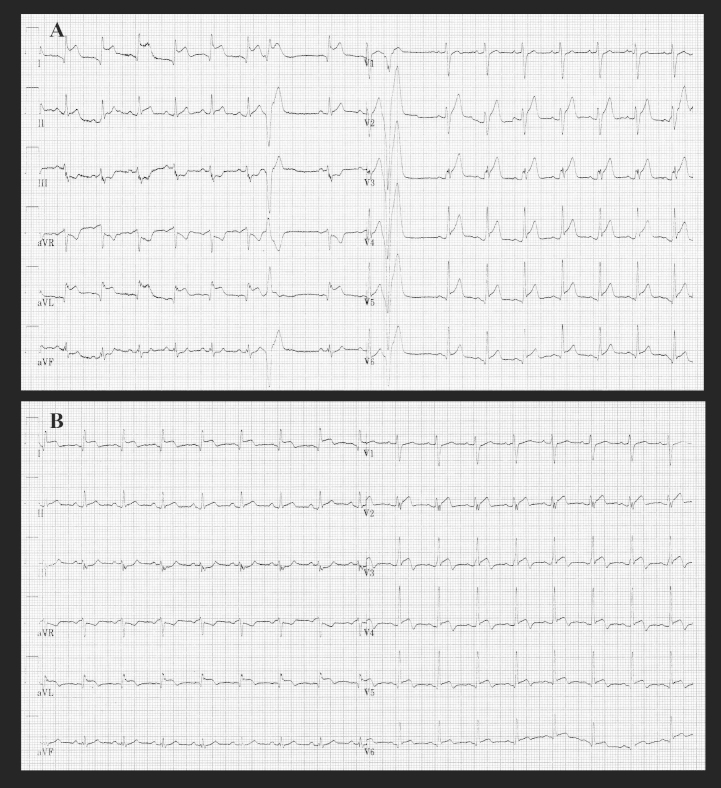
The admission electrocardiogram (Fig.1a) showed sinus tachycardia, with early premature ventricular beats, q waves in DI, aVL, V5-V6 leads, ST segment elevation in DI, aVL, V2-V6 (extending to V9) engulfing the T wave, with reciprocal ST changes in DIII and aVF leads.
Fig.1.
a-Electrocardiogram at admission; b- Electrocardiogram at 24 hours after admissionn
Fig. 1.
The emergency room troponin T test was positive (TnT=1.1ng/mL, reference range 0-0.1ng/mL). The echocardiogram revealed normal left ventricular size, a left ventricular ejection fraction of 45%, with regional wall motion abnormalities, including apical akinesia, lateral wall and septal dyskinesia, suggestive for a left anterior descending artery involvement. No intracardiac thrombi were observed, and the pericardium was normal.
These findings supported a working diagnosis of ST segment elevation acute coronary syndrome.
The patient received intravenous Nitroglycerin, Aspirin-150 mg, Clopidogrel-300mg, Enoxaparin-0.1mg/kg, Metoprolol-10mg i.v. Due to persistence of pain and of ECG changes more than 30 minutes, and having no possibility of primary percutaneous coronary intervention, it was decided to administer a thrombolytic drug (Reteplase 10 U i.v. repeated once at 30 minutes). Evolution was favorable, with remission of pain, but without significant electrocardiographic signs of reperfusion (Fig.1b).
Twenty-four hours after admission pruriginous vesicles with a clear content and surrounded by a pink halo appeared on the patient’s face, head and torso.
The clinical diagnosis of varicella-zoster infection was then established and the patient was started on Acyclovir 1600mg/day.
The usual laboratory analyses were normal as were protein S, protein C, antithrombin III, cryoglobulins, immunoelectrophoresis; high-sensitivity C-reactive protein was 4.88mg/L.
The patient gradually improved and was discharged seven days after admission.
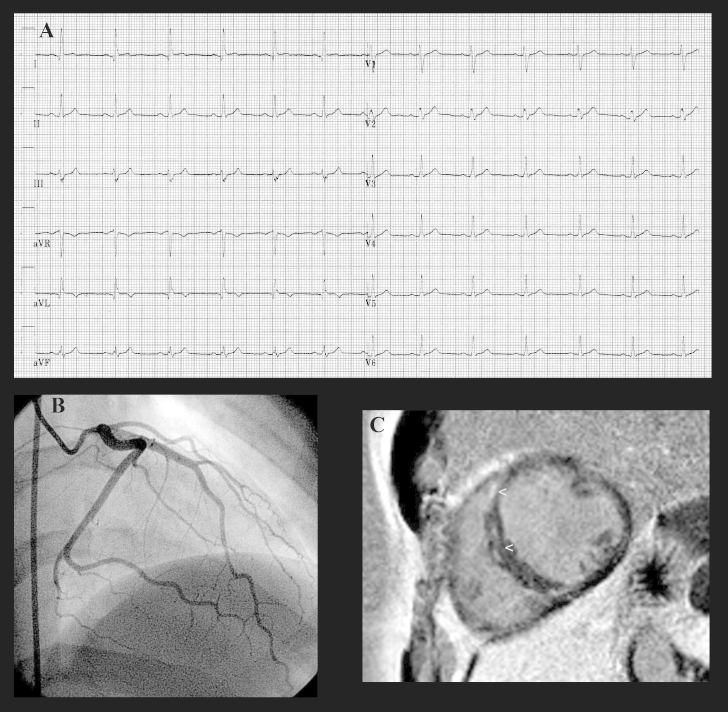
Two months after discharge the patient was reassessed. The ECG showed q waves and negative T waves in DI and aVL leads (Fig. 2a).
Fig.2.
a- Electrocardiogram at 2-months follow-up; b- Coronary angiography at 2-months follow-up - normal left coronary artery; c- Magnetic resonance imaging at 2-months follow-up - dynamic postcontrast T1 sequence with moderate focal capture in the septal myocardium (arrows)
Coronary angiography revealed a normal left coronary artery (Fig.2b) and a hypoplasic right coronary artery.
The echocardiographic assessment showed that the regional wall motion abnormality was significantly improved.
Magnetic resonance imaging showed mid-myocardial to epicardial patchy areas of enhancement (Fig.2c).
Discussion
We report a case of varicella-zoster myocarditis that presented as an acute myocardial infarction and was managed accordingly. At admission the patient had no signs or symptoms of a recent or present viral infection. Despite the patient having a low risk score for coronary heart disease, in the presence of persistent chest pain, with localized ST segment elevation and segmental left ventricular systolic dysfunction, with elevated myocardial enzymes, and in the absence of elements supporting another diagnosis, the possibility of an acute coronary syndrome could not be dismissed. Coronary spasm was excluded due to the persistence of ST segment elevation even after administration of intravenous Nitroglycerin, and due to the absence of possible causes such as illicit drug abuse.
The particularity of our case consists of late appearance of rash and clinical features of varicella infection and hence virtually impossible early diagnosis of viral myocarditis. There was also an atypical electrocardiographic pattern suggestive of necrosis not limited to the apex or possibly diffuse repolarization changes as often happen in myocarditis.
The fact that the patient has q waves suggestive of necrosis two months after discharge without recurrence of infection during this period, and the persistent reduction of LV ejection fraction with normal coronary angiography and minimal infiltrates in the interventricular septum at magnetic resonance imaging is also noteworthy.
Myocarditis is a heterogeneous disease with a wide spectrum of clinical manifestations, and can present as an acute myocardial infarction [1,2].
Cardiac involvement in varicella infection is rare. Myocarditis has long been associated with varicella infection. The pathological mechanism includes the direct cytopathic effect and the involvement of secondary auto-immune effects leading to myocardial cellular destruction and consecutive ventricular dysfunction. Clinical manifestation of myocarditis may vary from an asymptomatic state secondary to focal infection to severe heart failure. In some cases, clinical manifestations, electrocardiographic and laboratory findings simulate myocardial infarction. Complications of viral myocarditis include arrhythmias and progression to dilated cardiomyopathy and heart failure [3-5].
Pericarditis and secondary pericardial effusion may result in cardiac tamponade or chronic pericardial constriction [6].
The clinical presentation of myocarditis can be misleading. In our patient, due to the absence of symptoms and signs of a viral infection, an acute coronary syndrome could not be excluded. Varicella zoster infections are common in children and young adults and most recover without complication. Clinicians should be aware of possible cardiac complications.
References
- 1.Franken RA, Franken M. Pseudo-Myocardial Infarction During an Episode of Herpes Zoster. Arq Bras Cardiol. 2000;75(6):523–530. doi: 10.1590/s0066-782x2000001200006. [DOI] [PubMed] [Google Scholar]
- 2.De A, Myridakis D, Kerrigan M, Kiblawi F. Varicella myopericarditis mimicking myocardial infarction in a 17-year-old boy. Tex Heart Inst. J. 2011;38(3):288–290. [PMC free article] [PubMed] [Google Scholar]
- 3.Abrams D, Derrick G, Penny DJ, Shinebourne EA, Redington AN. Cardiac complications in children following infection with varicella zoster virus. Cardiol Young. 2001;11(6):647–652. doi: 10.1017/s1047951101001019. [DOI] [PubMed] [Google Scholar]
- 4.Chen EF, Paterick TE. 20-Year-Old Man With Chest Pain and Malaise. Mayo Clin Proc. 2007;82(9):1124–1127. doi: 10.4065/82.9.1124. [DOI] [PubMed] [Google Scholar]
- 5.Mallet E, Maitre M, Delalande-Dutilleul L, Marguet C, Mouterde O. Evaluation of varicella complications through a retrospective hospital survey in a paediatric center over 16 years in France. Arch Pediatr. 2004;11(9):1145–1151. doi: 10.1016/j.arcped.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Shefler A, Archer N, Walia R. Cardiac tamponade after varicella infection. Eur J Pediatr. 1998;157(7):564–566. doi: 10.1007/s004310050879. [DOI] [PubMed] [Google Scholar]