Abstract
Objective
To examine care system choices for Veterans dually-eligible for VA and Medicare FFS following changes in VA eligibility policy, which expanded availability of VA health care services.
Data Sources
VA and Medicare FFS enrollment and outpatient utilization databases in 1999 and 2004. Study Design: Multinomial logistic regression was used to examine odds of VA-only and Medicare-only utilization, relative to dual utilization, in 1999 and 2004. Observational cohort comprising a 5% random sample of dually-eligible Veterans: 73,721 in 1999 and 125,042 in 2004.
Principal Findings
From 1999 to 2004, persons with the highest HCC risk scores had decreasing odds of exclusive VA reliance (OR=0.26 in 1999 and 0.17 in 2004, p<0.05), but had increasing odds of exclusive Medicare reliance (OR=0.43 in 1999 and 0.56 in 2004, p<0.05).Persons in high VA priority groups had decreasing odds of exclusive VA reliance, as well as decreasing odds of exclusive Medicare reliance, indicating increasing odds of dual use. Newly eligible Veterans with the highest HCC risk scores had higher odds of dual system use, while newly eligible Black Veterans had lower odds of dual system use.
Conclusions
Veterans newly eligible for VA healthcare services, particularly those with the highest risk scores, had higher odds of dual system use compared to earlier eligibles. Providers should ensure coordination of care for Veterans who may be receiving care from multiple sources. Provisions of the Patient Protection and Affordable Care Act may help to ensure care coordination for persons receiving care from multiple systems.
Keywords: Veterans, Department of Veterans Affairs (VA), Medicare, Centers for Medicare & Medicaid Services (CMS), dual utilization, enrollment, eligibility
In 1996, the Veterans' Health Care Eligibility Reform Act (the Act) opened up eligibility for Veterans Affairs (VA) health care services to a larger population of Veterans than was previously served. Prior to the Act, Veterans were generally only eligible for VA health care services on the basis of a service-connected disability (H.R. 3118, 1996). Veterans who would have, in the absence of the Act, only been eligible for Medicare now found themselves eligible for health care services through both Medicare and the VA. Thus, some newly-eligible Veterans chose to receive care exclusively through the Medicare system, while some chose to use care exclusively in the VA system and others used care under both systems. The purpose of this paper is to examine how the population receiving care in the VA changed from 1999 to 2004, and how Veterans who found themselves newly eligible for VA and Medicare chose to receive care.
The Veterans Health Care Eligibility Reform Act and other VA Policy Changes
Following the implementation of the Act, any Veteran could apply for VA health care services. Veterans were assigned to priority groups to determine eligibility and cost-sharing. During the initial implementation of the Act, Veterans were classified into seven priority groups for enrollment eligibility. Assignment to the priority groups is based on level of service-connected disability and income (see Exhibit 1 for detailed criteria). The higher VA priority groups pay no co-payments, while the lower priority groups incur small co-payments. At the beginning of FY 2003 (October 1, 2002), eligibility was further expanded by the addition of higher-income Veterans who were classified into a new priority group 8. However, by January 2003, VA stopped enrolling new Veterans in group 8 (though enrollment was reinstated in June 2009). The expanded VA eligibility allowed many Veterans who had previously been eligible only for Medicare to become eligible for health care services under both VA and Medicare. Furthermore, the Act expanded VA health care services to include a greater emphasis on primary care, mental health care and women's health than had previously been offered through the VA.
Exhibit 1. Veterans Administration enrollment category by high (1–6) and low (7–8) priority groups (Jan. 2010).
| 1 |
|
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
| 6 |
|
| 7 |
|
| 8 |
|
At the end of this enhanced enrollment priority group placement time period, Veterans will be assigned to the highest Priority Group for which they qualify based on their unique eligibility status at that time.
Due to income relaxation rules implemented on June 15, 2009 Veterans with household income above the VA national Threshold or the GMT income threshold for their resident location by 10 percent or less, who agree to pay copays, are eligible for enrollment in Priority Group 8. The GMT thresholds can be located on the VA Web site.
Mechanisms Influencing Choice of Health Care System
Conflicting mechanisms can influence the choice to receive care under the VA or under Medicare. Cost-sharing is higher under Medicare fee-for-service (FFS) than under the VA. During the study time period, Medicare FFS required cost-sharing of 20% of charges for most outpatient services, and 50% of charges for mental health and substance abuse treatment (CMS, 2011a), though cost-sharing rates varied based on the type of service. Under the VA system, the level of co-payments can vary by year, priority group, and the type of medical service; many Veterans pay no co-payments and, among those who do, co-payments for outpatient care (including mental health care) have been set at $15 for primary care and $50 for specialty care since 2001 (VA, 2001, 2012). Thus, many patients pay no co-payments under the VA system, and those who do generally incur far less cost-sharing than under Medicare FFS. Beyond cost-sharing, other factors such as convenience and perceived quality may influence the choice of health care system. Distance from a VA facility relative to a Medicare facility might affect a person's choice (Hynes et al., 2007; Petersen et al., 2010). Additionally, the VA may be perceived as providing inferior quality of care compared to community providers, despite the advancements made by the VA in the past twenty years (Longman, 2010). Furthermore, persons who had an established relationship with a Medicare health care provider prior to VA enrollment may want to maintain that relationship.
Previous Research on Persons with Dual VA and Medicare Eligibility
A number of studies have examined health care utilization among dually-eligible Veterans. Hynes and colleagues (2007) provided one of the first analyses of utilization among dually-eligible Veterans in 1999, and found that Veterans who are Black, who lived closer to a VA facility, or who were assigned to a higher VA priority group, had greater probability of reliance on VA exclusively, while Veterans with greater medical risk were more likely to use services under both the VA and Medicare. The findings regarding distance from a VA facility and VA priority group have been confirmed by others (Petersen et al., 2010; Berke et al., 2009; Maciejewski et al.; 2009, Zhu et al.; 2010). Petersen and colleagues (2010) examined inpatient, outpatient, and overall utilization among dually-eligible Veterans in 2003 and 2004 and found that, while most health conditions were associated with lower reliance on the VA health care system, mental health and substance abuse disorders were associated with higher reliance on the VA system. Liu and colleagues (2010) examined outpatient utilization among dually-eligible Veterans from 2000–2004 and found that, while many VA patients received care under the Medicare system for primary care (30%) and specialty care (60%), very few received mental health care under Medicare (3–4%). Liu and colleagues also found that patients receiving care in VA community-based outpatient clinics (CBOCs) had higher rates of care from Medicare, raising the question of whether the establishment of CBOCs has improved access to care or simply led to fragmented care among that population. Furthermore, Liu and colleagues (2011) found that the population relying exclusively on the VA for primary and specialty outpatient services declined from 2000–2004. Other studies have examined utilization among dually-eligible Veterans with kidney disease (Fischer et al., 2010), dementia (Zhu et al., 2009, 2010), and propensity to enroll in a Medicare managed care plan (Maciejewski et al., 2009).
In this study, we examine how the population of Veterans receiving outpatient care in the VA health care system and the health care usage patterns have changed from 1999 to 2004. Throughout the study time period, VA policies have resulted in expanded eligibility, particularly for Veterans without service-connected disabilities. These policies can influence the type of population served at any given time. As clinicians and policymakers seek to understand the utilization choices of this population, understanding trends in service utilization can help to identify areas of unmet health care need, or alternatively, areas in which there are duplications of services.
Methods
Data
We used a retrospective, cross-sectional study design, identifying Veterans who were eligible to use VA and Medicare healthcare in calendar year 2004. We identified VA utilization by searching all VA workload data files containing records of outpatient care provided at a VA facility or paid for by the VA on a fee-basis for calendar year 2004 (Hynes et al., 2007). Medicare use was determined by searching CMS fee-for-service (FFS) Outpatient, Home Health Agency, and Carrier (Physician/Supplier) Standard Analytic Files (SAFs) (ResDAC, 2011). Geographic data on urban/rural nature and poverty level of the patient's ZIP Code was derived from 2000 Census data, and information on supply of hospital beds in the community was obtained by the Area Resource File (ARF) (HRSA, 2011).
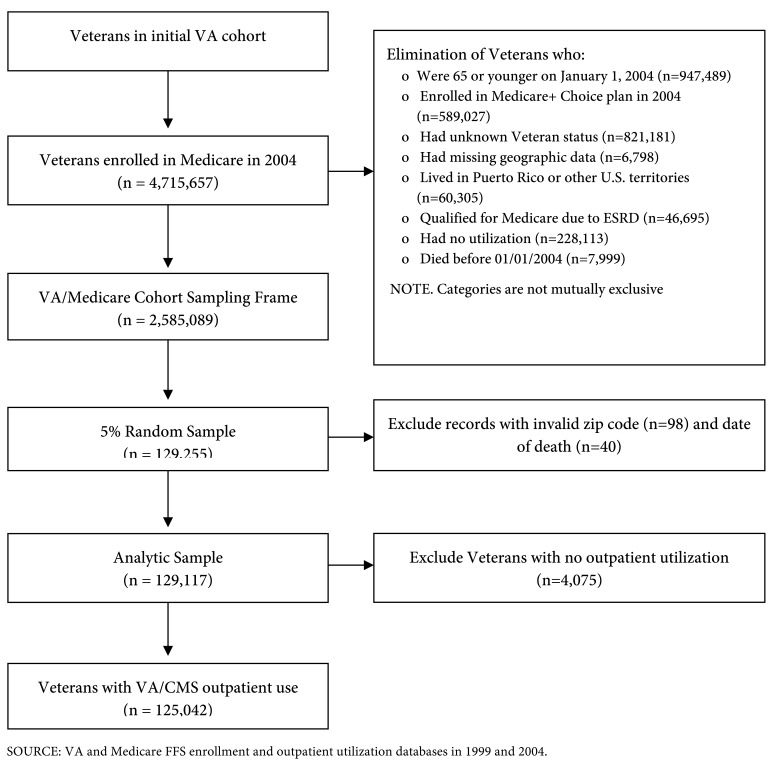
Our sampling frame comprised 12,984,025 veterans who had used VA healthcare services between calendar years 1997 and 2004, were eligible to use VA healthcare, because they enrolled with the VHA, or received compensation or pension benefits from the VA. We combined data from our sampling frame with Medicare enrollment data using conservative matching criteria to ensure valid data linkages (Fleming et al., 1992). Details of the dataset creation have been described elsewhere (Hynes et al., 2007). We identified a cohort of 4,715,657 Veterans eligible for VA healthcare and enrolled in Medicare during 2004 (Exhibit 2). We excluded individuals under age 65, with unknown Veteran priority status, with End Stage Renal Disease, enrolled in a Medicare Advantage plan, with missing or invalid ZIP Codes, or those who lived in Puerto Rico or other U.S. territories. In addition, we excluded 228,113 Veterans with no healthcare use in either VA or Medicare in 2004, since no information was available on other sources of health insurance, nor, therefore, whether there was any healthcare use outside of VA or Medicare. Our final cohort comprised 2,585,089 million Veterans. We selected a five percent random sample of those with outpatient utilization in either the VA or Medicare systems. Exclusion criteria are listed in Exhibit 2; the final analytic cohort is 125,042 for 2004. We also drew a five percent sample from a 1999 cohort previously identified by Hynes et al. (2007), for a cohort size of 73,721 for 1999. This study was approved by the Edward Hines Jr. VA Hospital Institutional Review Board.
Exhibit 2.
Cohort development for 2004 VA/CMS five percent analytic sample
Analysis
Multinomial logistic regression was used to examine the characteristics predicting three categories of service utilization: VA-only, Medicare Fee-for-Service (FFS)-only or dual use (VA and Medicare FFS). The model can be illustrated using the expression:
where i=individual and j=outcome (VA-only, Medicare-only or dual use).
The multinomial logistic regression model generates odds ratios comparing the odds of VA only utilization to dual use, and Medicare FFS-only compared to dual use. “Seemingly unrelated regression” (SUR) (where several individual regression models are combined into a single model) is used to enable us to compare coefficients between models for 1999 and 2004 using the dummy-variable variant of the Chow Test (Gujarati, 1995; Kennedy, 1998; Gould, 2011). The SUR models are clustered by individual, as about two percent (n=2511) of individuals were identified in both of the 5 percent random samples of dually-eligible Veterans in 1999 and 2004.
The multinomial logistic models are generally required to uphold the assumption of Independence of Irrelevant Alternatives (IIA), although in some cases, it has been argued that the IIA assumption is not strictly necessary (Grilli & Rampichini, 2007; Zhu et al., 2010). Two common tests for IIA include the Hausman test and Small-Hsiao test. Each of the models passed at least the Small-Hsiao test, and most passed both tests. The results of the IIA test are reported in each multinomial logistic regression table. All analyses were conducted using Stata version 12 (Stata, 2011).
Variables Used in the Analysis
A number of patient characteristics are examined which are believed to influence the demand for health care service use. These include patient demographic characteristics, measures of health status, and access to health care services in the community. Patient characteristics included age, gender, race, vital status (alive as of 12/31 of the file year), priority level within the VA, and a Hierarchical Condition Category (HCC) risk score. Age, gender, race, Medicaid enrollment, and vital status were obtained from the Medicare Vital Status file (Arday et al., 2000; Boehmer et al., 2002). Age was analyzed in three categories: 66 to 74 years, 75 to 84 years, and 85 years or older. Race was defined as a dichotomous variable indicating Black or non-Black race, as Medicare data do not differentiate between race and ethnicity, and this is the categorization with the lowest rate of misclassification (Waldo, 2004).
VA priority level and HCC risk scores are included to provide a measure of patient health status. VA Priority level was defined as a dichotomous variable where “high priority” Veterans included VA Priority Groups 1–6, while the “low priority” designation included VA Priority Groups 7 and 8. To account for patient health status, we computed risk scores based on all VA and Medicare healthcare claims data using the Hierarchical Condition Category (HCC) method (Hynes et al., 2007; Pope et al., 2004). The HCC method has been used to risk-adjust payments to Medicare + Choice plans since 2004 (Hynes et al., 2007). We divided the sample into quartiles based on HCC values.
A number of measures of access to health care in the community are included to account for availability of VA health care services, as well as competing Medicare-covered community-based services. Geographic access measures included distance to the nearest VA inpatient hospital, the urban/rural nature and poverty level of the patient's ZIP Code, and the supply of short-term community hospital beds in the county of residence. Distance to the nearest VA hospital was measured in miles as straight-line distance between the location of healthcare facility and the center of the ZIP Code of the patient's residence, and was obtained from the VA Planning Systems Support Group (VA, 2005). The urban/rural nature of the ZIP Code is based on 2000 census data from the VA Planning Systems Support Group (VA, 2005). Poverty level was derived from the 2000 census as a dichotomous measure indicating whether at least 20% of households in the ZIP Code were below the poverty level; i.e., high poverty (VA, 2005). The level of the healthcare resources in the individual's county of residence was measured using the number of short-term general hospital beds as a proxy for all healthcare resources. Counties were divided into four equally sized groups: Low (0–137 beds), Medium-Low (138–517 beds), Medium-High (518–1656 beds), and High (1657–24791 beds) (HRSA, 2011).
Finally, in the 2004 models, we included an indicator of whether the individual was newly eligible for VA between 2000 and 2004. This indicator is distinct from whether the individual was observed in both 5% samples, as one could be eligible for VA in 1999, but not picked up in the 5% sample. Including this variable allows us to examine the population newly eligible for VA health care services.
Findings
Exhibit 3 describes the characteristics of the analytic sample. The sample is predominantly male (98 percent in 1999) and non-Black (92 percent in 1999). The percentage of the sample who were dual users of VA and Medicare increased over the time period of the study (46 percent in 1999 and 56 percent in 2004, p<0.01). Likewise, the percentage of the sample relying exclusively on VA care declined during this time period, from 19 percent in 1999 to 14 percent in 2004 (p<0.01), and the population relying exclusively on Medicare decreased from 35 percent in 1999 to 30 percent in 2004 (p<0.01). The proportion of the sample classified into a low priority VA eligibility group increased from 1999 to 2004 (21 percent in 1999 versus 41 percent in 2004, p<0.01). In addition, the proportion of the population living in a low poverty ZIP Code increased, from 86 percent in 1999 to 89 percent in 2004 (p<0.01). The proportion of the sample living 40 or more miles from the nearest VA facility increased slightly from 41% in 1999 to 43% in 2004, p<0.01).
Exhibit 3. Sample Characteristics of VA and Medicare outpatient users, 1999 and 2004: Percent (Std.Dev.).
| Full 5% Sample | VA-Only Users | |||
|---|---|---|---|---|
| 1999 | 2004 | 1999 | 2004 | |
|
|
|
|||
| Total N | 73,721 | 125,042 | 13,736 | 17,922 |
| (100) | (100) | (18.6) | (14.3) | |
| VA Only Use | 18.6 | 14.3† | 100.0 | 100.0 |
| (38.9) | (35.0) | |||
| VA & Medicare Use | 46.1 | 56.1† | -- | -- |
| (49.8) | (49.2) | |||
| Medicare Only Use | 35.2 | 29.6† | -- | -- |
| (47.8) | (45.6) | |||
| Age as of (12/31/2003) | ||||
| 66–74 | 53.6 | 45.8† | 64.0 | 59.7† |
| (49.9) | (49.8) | (48.0) | (49.0) | |
| 75–84 | 42.6 | 47.0† | 33.4 | 35.9† |
| (49.4) | (49.9) | (47.2) | (48.0) | |
| 85+ | 3.8 | 7.3† | 2.6 | 4.4† |
| (19.2) | (25.9) | (16.0) | (20.6) | |
| Race | ||||
| Non-Black | 91.6 | 93.2† | 82.5 | 84.3† |
| (27.7) | (25.1) | (38.0) | (36.3) | |
| Black | 8.4 | 6.8† | 17.5 | 15.7† |
| (27.7) | (25.1) | (38.0) | (36.3) | |
| Gender | ||||
| Female | 2.0 | 2.0 | 2.1 | 1.9 |
| (13.9) | (14.1) | (14.3) | (13.6) | |
| Male | 98.0 | 98.0 | 97.9 | 98.1 |
| (13.9) | (14.1) | (14.3) | (13.6) | |
| VA priority level | ||||
| Low | 21.0 | 40.7† | 8.4 | 17.7† |
| (40.8) | (49.1) | (27.7) | (38.1) | |
| High | 79.0 | 59.3† | 91.6 | 82.3† |
| (40.8) | (49.1) | (27.7) | (38.1) | |
| HCC risk score | ||||
| Low | 25.0 | 25.1 | 32.6 | 38.4† |
| (43.3) | (43.3) | (46.9) | (48.6) | |
| Medium-Low | 25.0 | 25.0 | 29.0 | 29.4 |
| (43.3) | (43.3) | (45.4) | (45.6) | |
| Medium-High | 25.0 | 25.0 | 23.1 | 20.9† |
| (43.3) | (43.3) | (42.1) | (40.6) | |
| High | 25.0 | 25.0 | 15.4 | 11.4† |
| (43.3) | (43.3) | (36.1) | (31.7) | |
| Type of ZIP Code | ||||
| Rural | 20.9 | 20.1† | 20.7 | 20.8 |
| (40.6) | (40.1) | (40.5) | (40.6) | |
| Urban | 79.1 | 79.9† | 79.3 | 79.2 |
| (40.6) | (40.1) | (40.5) | (40.6) | |
| Poverty level of ZIP Code | ||||
| Low | 85.9 | 88.6† | 78.8 | 82.2† |
| (34.8) | (31.8) | (40.9) | (38.3) | |
| High | 14.1 | 11.4† | 21.2 | 17.8† |
| (34.8) | (31.8) | (40.9) | (38.3) | |
| Medicaid enrollment | 7.6 | 7.9† | 4.8 | 7.0† |
| (26.5) | (27.0) | (21.4) | (25.6) | |
| Distance to VA | ||||
| < 5 miles | 12.8 | 10.1† | 21.9 | 17.7† |
| (33.4) | (30.1) | (41.4) | (38.1) | |
| 5–9.9 miles | 11.9 | 10.8† | 15.1 | 15.1 |
| (32.4) | (31.1) | (35.8) | (35.9) | |
| 10–19.9 miles | 14.6 | 15.5† | 15.4 | 16.3† |
| (35.3) | (36.2) | (36.1) | (36.9) | |
| 20–39.9 miles | 19.7 | 20.7† | 17.0 | 19.2† |
| (39.8) | (40.5) | (37.6) | (39.4) | |
| 40+ miles | 40.9 | 42.8† | 30.5 | 31.7† |
| (49.2) | (49.5) | (46.0) | (46.5) | |
Differences in means between the years are statistically significant at p <0.05
SOURCE:VA and Medicare FFS enrollment and outpatient utilization databases in 1999 and 2004.
Exhibit 4 describes the VA priority group distribution in 2004 of new VA eligibles (those who were eligible from 2000 to 2004) and those who were eligible in 1999. Veterans who were eligible in 1999 were more likely to be in high VA priority groups, particularly groups 1–5, while new VA eligibles were more likely to be in the lower priority groups 7–8. Two sample t-tests indicated that the comparisons of the two cohorts within each priority group are statistically significantly different (p<0.01).
Exhibit 4. Priority Groups in 2004 of Persons Eligible for VA in 1999 and Between 2000 and 2004 Percent (St.Dev).
| Percent Enrolled | ||
|---|---|---|
| Eligible in 1999 | Eligible between 2000 and 2004 | |
|
|
||
| Priority Group 1 | 13.1 | 1.7 |
| (33.7) | (12.8) | |
| Priority Group 2 | 7.3 | 1.2 |
| (26.1) | (11.0) | |
| Priority Group 3 | 14.2 | 4.1 |
| (34.9) | (19.8) | |
| Priority Group 4 | 4.9 | 2.4 |
| (21.5) | (15.4) | |
| Priority Group 5 | 33.1 | 31.7 |
| (47.1) | (46.5) | |
| Priority Group 6 | 0.8 | 0.6 |
| (8.8) | (7.8) | |
| Priority Group 7 | 1.9 | 6.1 |
| (13.6) | (23.9) | |
| Priority Group 8 | 24.8 | 52.2 |
| (43.2) | (50.0) | |
|
| ||
| Total Percent | 100 | 100 |
| Total N | 69,669 | 55,373 |
NOTE. Two-sample t-tests indicate percents across cohorts in each priority group are statistically significantly different from one another, p<0.01.
SOURCE: VA and Medicare FFS enrollment and outpatient utilization databases in 1999 and 2004.
Exhibit 5 describes the characteristics predicting outpatient service utilization under each system. The first two columns examine probability of exclusive VA use compared to dual use. Compared to those ages 65–74, older persons had lower odds of exclusive VA use (OR=0.67 [95% CI: 0.64, 0.70] for persons age 75–84 and OR=0.70 [0.61, 0.79] for persons age 85 and older in 1999). Blacks had higher odds of VA only use (OR=2.17[2.02, 2.34]. Persons with high HCC risk scores have lower odds of VA only use, (OR=0.26[0.25, 0.28] for the highest risk quartile in 1999). Persons living in urban ZIP Codes have lower odds of VA only use (OR=0.79[0.75, 0.84] in 1999). Persons in high poverty ZIP Codes have higher odds of VA only use (OR=1.28[1.21, 1.36], as do persons classified by the VA as high priority 3.53[3.23, 3.78].Those who were enrolled in Medicaid had lower odds of exclusive VA reliance (OR=0.63 [0.57, 0.70] in 1999). Persons living furthest from the VA (40+ miles) have the lowest odds of exclusive VA reliance (OR=0.32 [0.29, 0.34].
Exhibit 5. Characteristics Predicting Single System or Dual VA/Medicare Outpatient Service Use in 1999 and 2004: OR,[95%CI].
| VA Only Vs. Dual Use | Medicare Only Vs. Dual use | |||
|---|---|---|---|---|
| 19991 (n=73,721) | 20041 (n=125,042) | 19992 (n=73,721) | 20041 (n=125,042) | |
|
|
|
|||
| Age as of 12/31/03 | ||||
| 66–74 | REF | REF | REF | REF |
| 75–84 | 0.67 | 0.62† | 1.29 | 1.10† |
| [0.64, 0.70] | [0.60, 0.65] | [1.24, 1.33] | [1.07, 1.13] | |
| 85+ | 0.70 | 0.59† | 2.18 | 1.60† |
| [0.61, 0.79] | [0.54, 0.64] | [2.01, 2.38] | [1.52, 1.69] | |
| Race | ||||
| Non-Black | REF | REF | REF | REF |
| Black | 2.17 | 2.24 | 0.71 | 1.07† |
| [2.02, 2.34] | [2.10, 2.38] | [0.66, 0.76] | [1.01, 1.14] | |
| Gender | ||||
| Female | REF | REF | REF | REF |
| Male | 0.87 | 1.10† | 1.13 | 0.88† |
| [0.74, 1.01] | [0.97, 1.25] | [1.00, 1.28] | [0.81, 0.96] | |
| VA priority level | ||||
| Low | REF | REF | REF | REF |
| High | 3.53 | 2.96† | 0.79 | 0.64† |
| [3.23, 3.78] | [2.83, 3.10] | [0.76, 0.83] | [0.62, 0.65] | |
| HCC risk score | ||||
| Low | REF | REF | REF | REF |
| Medium-Low | 0.72 | 0.64† | 0.66 | 0.72† |
| [0.68, 0.76] | [0.61, 0.67] | [0.63, 0.69] | [0.69, 0.75] | |
| Medium-High | 0.49 | 0.38† | 0.54 | 0.61† |
| [0.47, 0.52] | [0.36, 0.40] | [0.51, 0.56] | [0.58, 0.63] | |
| High | 0.26 | 0.17† | 0.43 | 0.56† |
| [0.25, 0.28] | [0.16, 0.18] | [0.41, 0.46] | [0.54, 0.58] | |
| Type of ZIP Code | ||||
| Rural | REF | REF | REF | REF |
| Urban | 0.79 | 0.77 | 1.13 | 1.05† |
| [0.75, 0.84] | [0.73, 0.81] | [1.08, 1.18] | [1.01, 1.09] | |
| ZIP Code Poverty Level | ||||
| Low | REF | REF | REF | REF |
| High | 1.28 | 1.32 | 0.85 | 0.95† |
| [1.21, 1.36] | [1.25, 1.39] | [0.81, 0.90] | [0.91, 0.99] | |
| Medicaid enrollment | 0.63 | 0.96† | 2.00 | 2.30† |
| [0.57, 0.70] | [0.89, 1.03] | [1.88 2.13] | [2.19, 2.41] | |
| Distance to Nearest VA | ||||
| < 5 miles | REF | REF | REF | REF |
| 5–9.9 miles | 0.79 | 0.86 | 1.23 | 1.15 |
| [0.73, 0.85] | [0.80, 0.92] | [1.15, 1.32] | [1.08, 1.22] | |
| 10–19.9 miles | 0.68 | 0.67 | 1.34 | 1.18† |
| [0.63, 0.73] | [0.63, 0.72] | [1.25, 1.44] | [1.12, 1.25] | |
| 20–39.9 miles | 0.47 | 0.51 | 1.28 | 1.07† |
| [0.43, 0.51] | [0.48, 0.55] | [1.20, 1.38] | [1.01. 1.13] | |
| 40+ miles | 0.32 | 0.33 | 1.29 | 1.01† |
| [0.29, 0.34] | [0.31, 0.36] | [1.21, 1.38] | [0.96, 1.07] | |
| Newly eligible 2000–2004 | NA | 0.43 | NA | 0.94 |
| [0.41, 0.45] | [0.91, 0.96] | |||
Differences in ORs between the model years are statistically significant at p <0.05.
Model passed Hausman and Small-Hsiao IIA Tests.
Model passed Small-Hsiao IIA Test only.
All models adjust for VA Integrated Service Network region of residence, days of enrollment, patient vital status, and supply of short-term community hospital beds in the Veteran's county of residence.
SOURCE: VA and Medicare FFS enrollment and outpatient utilization databases in 1999 and 2004.
The third and fourth columns of Exhibit 5 examine the probability of exclusive Medicare use, compared to dual use. Persons with high HCC risk scores have lower odds of Medicare only use, indicating that persons with high HCC risk scores have greater odds of dual use than of exclusive VA or Medicare use. Persons living in urban areas have higher odds of exclusive Medicare reliance (OR=1.13 [1.08, 1.18] in 1999), as do persons living furthest from a VA facility, 40+ miles, (OR=1.29 [1.21, 1.38] in 1999), while persons living in high poverty ZIP Codes have lower odds of exclusive Medicare reliance (OR=0.85[0.81, 0.90], as do persons assigned to a high VA priority group (OR=0.79[0.76, 0.83]).
As Exhibit 5 also reports the results of the dummy-variable variant Chow Test comparing coefficients from 1999 and 2004, it allows us to examine how utilization patterns have changed over time. From 1999 to 2004, persons over age 85 had lower odds of exclusive VA use, compared to persons age 65–74 (OR=0.70 [0.61, 0.79] in 1999 versus OR=0.59 [0.54, 0.64] in 2004, p<0.05]. Persons with the highest HCC risk scores had decreasing odds of exclusive VA reliance (OR=0.26[0.25, 0.28] in 1999 and 0.17 [0.16, 0.18] in 2004, p<0.05), but had increasing odds of exclusive Medicare reliance (OR=0.43[0.41, 0.46] in 1999 and 0.56[0.54, 0.58] in 2004, p<0.05). Those in the highest VA priority groups had decreasing odds of exclusive VA reliance (OR=3.53[3.23, 3.78] in 1999 and 2.96[2.83, 3.10] in 2004, p<0.05), as well as decreasing odds of exclusive Medicare reliance (OR=0.79[0.76, 0.83] in 1999 and 0.64 [0.62, 0.65] in 2004, p<0.05). Persons living further from VA facilities (i.e., 40+ miles) had lower odds of exclusive Medicare reliance in 2004 than in 1999 (OR=1.29 [1.21, 1.38] and 1.01 [0.96, 1.07] in 2004, p<0.05). New VA eligibles, persons who were eligible between 2000 and 2004, had lower odds of exclusive VA reliance (OR=0.43 [0.41, 0.45]) and lower odds of exclusive Medicare reliance (OR=0.94[0.91, 0.96]), thus indicating that new VA eligibles had greater odds of seeking care in both systems.
Exhibit 6 compares service utilization patterns in 2004 between new VA eligibles (between 2000 and 2004) and those eligible in 1999. Among Blacks, new eligibles had higher odds of exclusive VA use (OR=2.69 versus 2.09 p<0.05) and of exclusive Medicare use (OR=1.43 versus OR 0.91, p<0.05) than prior eligibles, indicating that, among Blacks, new eligibles had lower odds of dual service use than prior eligibles. Among persons with a high VA priority level, new eligibles had higher odds of exclusive Medicare use (OR=0.80 versus 0.50, p<0.05) than prior eligibles. Likewise, among persons with the highest HCC scores, new eligibles had lower odds of exclusive VA use (OR=0.10 versus 0.20 p<0.05) and higher odds of exclusive Medicare use (OR=0.65 versus 0.48, p<0.05) than prior eligibles. However, the fact that odds ratios are less than one for both exclusive Medicare and VA use indicates a higher rate of dual service utilization among this population. Among those enrolled in Medicaid, new eligibles had higher odds of exclusive VA use (OR=1.31 versus 0.89 p<0.05) and similar odds of exclusive Medicare use. Additionally, newly eligible persons age 75–84 had lower odds of exclusive VA use (OR=0.55 versus 0.65, p<0.05), while those living in an urban ZIP Code had lower odds of exclusive Medicare use (OR=1.01 versus 1.09, p<0.05). Newly eligible persons living 40 or more miles from the nearest VA facility had higher odds of exclusive VA use (OR=0.39 versus 0.32, p<0.05) and lower odds of exclusive Medicare use (OR=0.93 versus 1.09, p<0.05).
Exhibit 6. Characteristics Predicting Single System or Dual VA/Medicare Outpatient Service Use in 2004 Among Persons Eligible for VA 1999 and Newly Eligible in 2000–2004: OR, [95%CI].
| VA Only Vs. Dual Use | Medicare Only Vs. Dual Use | |||
|---|---|---|---|---|
| Eligible in 19991 (n=69,669) |
Newly Eligible 2000–20041 (n=55,373) |
Eligible in 19991 (n=69,669) |
Newly Eligible 2000–20042 (n=55,373) |
|
|
|
|
|||
| Age as of 12/31/03 | ||||
| 66–74 | Ref | Ref | Ref | Ref |
| 75–84 | 0.65† | 0.55 | 1.08 | 1.12 |
| [0.62, 0.68] | [0.51, 0.59] | [1.04, 1.12] | [1.08, 1.17] | |
| 85+ | 0.58 | 0.58 | 1.56 | 1.69 |
| [0.53, 0.64] | [0.47, 0.70] | [1.45, 1.66] | [1.56, 1.83] | |
| Race | ||||
| Non-Black | Ref | Ref | Ref | Ref |
| Black | 2.09† | 2.69 | 0.91† | 1.43 |
| [1.95, 2.25] | [2.34, 3.09] | [0.85, 0.99] | [1.29, 1.59] | |
| Gender | ||||
| Female | Ref | Ref | Ref | Ref |
| Male | 1.12 | 1.01 | 0.92 | 0.85 |
| [0.97, 1.30] | [0.78, 1.31] | [0.81, 1.03] | [0.74, 0.98] | |
| VA priority level | ||||
| Low | Ref | Ref | Ref | Ref |
| High | 3.05 | 2.75 | 0.50† | 0.80 |
| [2.87, 3.24] | [2.56, 2.95] | [0.48, 0.52] | [0.76, 0.83] | |
| HCC risk score | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium-Low | 0.72† | 0.50 | 0.65† | 0.78 |
| [0.68, 0.76] | [0.46, 0.54] | [0.62, 0.69] | [0.74, 0.82] | |
| Medium-High | 0.44† | 0.24 | 0.55† | 0.65 |
| [0.42, 0.47] | [0.22, 0.27] | [0.52, 0.58] | [0.62, 0.69] | |
| High | 0.20† | 0.10 | 0.48† | 0.65 |
| [0.18, 0.21] | [0.08, 0.11] | [0.46, 0.51] | [0.61, 0.68] | |
| Type of ZIP Code | ||||
| Rural | Ref | Ref | Ref | Ref |
| Urban | 0.77 | 0.79 | 1.09† | 1.01 |
| [0.72, 0.82] | [0.72, 0.87] | [1.04, 1.15] | [0.96, 1.06] | |
| ZIP Code Poverty Lvl. | ||||
| Low | Ref | Ref | Ref | Ref |
| High | 1.33 | 1.25 | 0.92 | 1.00 |
| [1.25, 1.42] | [1.12, 1.40] | [0.86, 0.97] | [0.93, 1.07] | |
| Medicaid Enrollment | 0.89† | 1.31 | 2.41 | 2.27 |
| [0.82, 0.96] | [1.10, 1.54] | [2.28, 2.56] | [2.08, 2.47] | |
| Dist. to Nearest VA | ||||
| < 5 miles | Ref | Ref | Ref | Ref |
| 5–9.9 miles | 0.87 | 0.84 | 1.20 | 1.08 |
| [0.81, 0.95] | [0.73, 0.96] | [1.11, 1.30] | [0.99, 1.18] | |
| 10–19.9 miles | 0.68 | 0.69 | 1.28† | 1.09 |
| [0.62, 0.73] | [0.61, 0.79] | [1.18, 1.37] | [1.00. 1.18] | |
| 20–39.9 miles | 0.50 | 0.57 | 1.14† | 0.99 |
| [0.46, 0.54] | [0.50, 0.65] | [1.05, 1.22] | [0.91, 1.08] | |
| 40+ miles | 0.32† | 0.39 | 1.09† | 0.93 |
| [0.30, 0.35] | [0.34, 0.44] | [1.01, 1.17] | [0.85, 1.01] | |
Differences in ORs between the model years are statistically significant at p <0.05.
Model passed Hausman and Small-Hsiao Tests for IIA.
Model passed Small-Hsiao IIA Test only.
Model passed Hausman IIA Test only.
All models adjust for VA Integrated Service Network region of residence, days of enrollment, patient vital status, and supply of short-term community hospital beds in the Veteran's county of residence.
SOURCE: VA and Medicare FFS enrollment and outpatient utilization databases in 1999 and 2004.
Discussion
The expansion of VA eligibility increased the services available to many Veterans who would have otherwise been receiving care exclusively in the Medicare system, but also may have made coordination of care more difficult as the expansion enabled them to receive care in both systems. Veterans newly eligible for VA healthcare had lower odds than previous eligibles of relying exclusively on either the VA or Medicare systems, indicating that new eligibles were more likely to be using both systems of care. Furthermore, Veterans with the highest HCC risk scores had lower odds of either exclusive VA or Medicare use, though new eligibles had slightly higher odds of exclusive Medicare use than prior eligibles. However, newly-eligible Black Veterans had lower odds of dual system use. Interestingly, newly eligible Veterans living 40 or more miles from the nearest VA facility had higher odds of exclusive VA reliance than prior eligibles. This may indicate that newly eligible persons who chose to receive some care in VA despite living further from a VA facility may have found it advantageous to use VA for all of their health care. Although it is not possible in this data to link particular changes in VA eligibility policies with changes in eligibility, the results show the changes in the service utilization among those newly eligible to the VA.
Our results are consistent with earlier analyses of utilization for dual-eligibles in 1999. In both 1999 and 2004, we found that persons assigned to high VA priority groups had higher odds of exclusive VA use, and persons with higher medical risk had lower odds of exclusive VA use (Hynes et al., 2007). Consistent with prior research, we found evidence that VA enrollees are increasingly seeking care in the Medicare system (Petersen et al., 2010; Liu et al., 2010, 2011). This study documents the changes in the dually-eligible population over time during the time period of the VA eligibility expansions (1999–2004), and demonstrates the need for providers and policymakers to recognize the changes in the population served in the VA health care system. VA eligibles are increasingly likely to be receiving services from multiple providers in the community. This trend could be beneficial to elderly Veterans if it allows the Veteran to select preferred providers or provides access to services not available under the VA system. However, as was noted above, Medicare FFS generally requires much higher cost-sharing than does the VA. The fact that elderly Veterans are willing to incur the higher cost-sharing under Medicare may indicate substantial unmet needs through the VA health care system.
Several limitations should be noted. The sample only includes Veterans who received outpatient treatment and may not be applicable to those who only received inpatient treatment or other treatment types, such as residential or domiciliary care. It should be noted that no information was available on eligibility for coverage under private insurance; the analyses in this paper understate health care utilization of Veterans with access to care under these payers. Furthermore, this sample excludes those who were enrolled in a Medicare managed care plan, because data limitations prevented the calculation of their utilization or risk scores. Most importantly, the data do not permit examination of utilization following specific eligibility policy changes, as most policy changes take time to have an effect. Despite these limitations, the ability to link VA and Medicare data provides a much fuller picture of health care utilization than simply examining either VA or Medicare utilization separately, and illustrates how the population relying on VA care exclusively has changed during this climate of expanded VA eligibility.
Conclusion
The population utilizing VA health care has been changing over time. Changes in the eligibility policy of healthcare systems can shape the characteristics of persons receiving care in VA and Medicare. During the time period from 1999–2004, VA eligibility policy resulted in expanded eligibility for Veterans. During this time period, the population relying exclusively on the VA for health care changed; sicker Veterans and newly-eligible Veterans had lower odds of exclusively relying on the VA for service and higher odds of seeking at least some care in the community under the Medicare FFS system.
Further research should examine whether the shift towards greater use of Medicare services is indicative of unmet needs in the VA population. For example, examining whether elderly Veterans use VA care exclusively for a time and then switch to Medicare exclusively, could indicate whether unmet needs exist in the VA system. Likewise, if similar services are utilized in each system close together in time, it could indicate concerns with quality of care and the seeking of second opinions. However, if similar types of care are utilized further apart in time, it may indicate duplication of services and lack of coordination of care across systems. Ultimately, the best way to learn of the experiences of elderly Veterans is to conduct surveys and interviews to learn why they choose to use services in one system versus the other. In addition, it would be interesting to consider the ways in which policy changes influence incentives to use one system or the other. For instance, in June 2009, the VA re-opened enrollment in priority group 8 for the highest-income Veterans (VA, 2001). These individuals are likely to have had established relationships with providers prior to VA enrollment. Meanwhile, in 2006, Medicare began offering coverage for prescription drugs through Part D (CMS, 2011b). With the advent of the Patient Protection and Affordable Care Act (PPACA), new changes will be implemented into Medicare, such as the introduction of Accountable Care Organizations (ACOs) (Lieberman, 2011), which may alter the incentives for relying on VA and Medicare.
While expanded VA eligibility resulted in greater options for receipt of medical care services, greater fragmentation of care may be an unintended consequence. Some provisions of the PPACA may help to address this fragmentation by fostering improved communication across health care systems, through use of the electronic medical record, and by promoting the use of patient centered medical homes for Medicaid-eligible persons with serious chronic illnesses (Mechanic, 2012). The PPACA could therefore help to ensure improved quality of care along with expanded access to care for Veterans.
Acknowledgments
The authors wish to thank Kevin Stroupe, PhD, for providing valuable advice in the development of this article.
Footnotes
Disclaimer: This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development Service, VA Information Resource Center (SDR 98-004), VA/CMS Data for Research Project (SDR 02-237). Dr. Hynes was supported by a VA Research Career Scientist Award (RCS 98-352). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- Arday SL, Arday DR, Monroe S, Zhang J. HCFA's racial and ethnic data: current accuracy and recent improvements. Health Care Financing Review. 2000;21:107–116. [PMC free article] [PubMed] [Google Scholar]
- Berke EM, West AN, Wallace AE, Weeks WB. Practical and Policy Implications of Using Different Rural–Urban Classification Systems: A Case Study of Inpatient Service Utilization Among Veterans Administration Users. The Journal of Rural Health. 2009;25(3):259–266. doi: 10.1111/j.1748-0361.2009.00228.x. [DOI] [PubMed] [Google Scholar]
- Boehmer U, Kressin NR, Berlowitz DR, Christiansen CL, Kazis LE, Jones JA. Self-reported vs administrative race/ethnicity data and study results. American Journal of Public Health. 2002;92:1471–1472. doi: 10.2105/AJPH.92.9.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS) Your Medicare Coverage. 2011a Retrieved from http://www.medicare.gov/Coverage/Home.asp.
- Centers for Medicare and Medicaid Services (CMS) What is Part D (Medicare Prescription Drug Coverage?) 2011b Retrieved from http://www.medicare.gov/navigation/medicare-basics/medicare-benefits/part-d.aspx.
- Fischer MJ, Stroupe KT, Kaufman JS, O'hare AM, Browning MM, Huo Z, Hynes DM. Predialysis Nephrology Care Among Older Veterans Using Department of Veterans Affairs or Medicare-Covered Services. The American Journal of Managed Care. 2010;16(2):e57–e66. [PubMed] [Google Scholar]
- Fleming C, Fisher ES, Chang CH, Bubolz TA, Malenka DJ. Studying outcomes and hospital utilization in the elderly: The advantages of a merged data base for Medicare and Veterans Affairs hospitals. Medical Care. 1992;30:377–391. doi: 10.1097/00005650-199205000-00001. [DOI] [PubMed] [Google Scholar]
- Gould W. Can You Explain Chow Tests. 2011 Jun; Retrieved from http://www.stata.com/support/faqs/stat/chow3.html.
- Grilli L, Rampichini C. A multilevel multinomial logit model for the analysis of graduates' skills. Statistical Methods & Applications. 2007;16:381–393. doi: 10.1007/s10260-006-0039-z. [DOI] [Google Scholar]
- Gujarati D. Basic Econometrics. Third Edition. New York, NY: McGraw-Hill; 1995. [Google Scholar]
- Health Resources and Services Administration (HRSA) Area Resource File. 2011 Retrieved from http://arf.hrsa.gov/
- H.R. 3118. Bill Summary and Status, 104th Congress 1995–1996, Veterans' Health Care Eligibility and Reform Act of 1996. 1996 Retrieved from http://thomas.loc.gov/cgi-bin/bdquery/z?d104:H.R.3118:.
- Hynes DM, Koelling K, Stroupe K, Arnold N, Mallin K, Sohn MW, et al. Kok L. Veterans' access to and use of Medicare and Veterans Affairs health care. Medical Care. 2007;45:214–223. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
- Kennedy P. A Guide to Econometrics. Fourth Edition. Cambridge, MA: The MIT Press; 1998. [Google Scholar]
- Lieberman S. Pioneer ACOs: The Right Direction, but Where's the Goal? 2011 May; Retrieved from http://healthaffairs.org/blog/2011/05/25/pioneer-acos-the-right-direction-but-whats-the-goal/
- Liu CF, Manning WM, Burgess JF, Hebert PL, Bryson CL, Fortney JC, et al. Maciejewski ML. Reliance on Veterans Affairs Outpatient Care by Medicare-Eligible Veterans. Medical Care. 2011;49(10):911–917. doi: 10.1097/MLR.0b013e31822396c5. [DOI] [PubMed] [Google Scholar]
- Liu CF, Chapko M, Bryson CL, Burgess JF, Fortney JC, Perkins M, et al. Maciejewski ML. Use of outpatient care in Veterans Health Administration and Medicare among Veterans receiving primary care in community-based and hospital outpatient clinics. Health Services Research. 2010;45(5 Pt. 1):1268–1286. doi: 10.1111/j.1475-6773.2010.01123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longman P. Best Care Anywhere: Why VA Healthcare is Better than Yours. 2nd Edition. Berrett-Koelher Publishers; 2010. [Google Scholar]
- Maciejewski ML, Birken S, Perkins M, Burgess JF, Sharp N, Liu C. Medicare Managed Care Enrollment by Disability-Eligible and Age-Eligible Veterans. Medical Care. 2009;47(11):1180–1185. doi: 10.1097/MLR.0b013e3181b58e17. [DOI] [PubMed] [Google Scholar]
- Mechanic D. Seizing Opportunities under the Affordable Care Act for Transforming the Mental and Behavioral Health System. Health Affairs. 2012;31(2):376–382. doi: 10.1377/hlthaff.2011.0623. [DOI] [PubMed] [Google Scholar]
- Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship Between Clinical Conditions and Use of Veterans Affairs Health Care Among Medicare-Enrolled Veterans. Health Services Research. 2010;45(3):762–791. doi: 10.1111/j.1475-6773.2010.01107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope GC, Kautter J, Ellis RP, Ash AS, Ayanian JZ, Lezzoni LI, et al. Robst J. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financing Review. 2004;25:119–141. [PMC free article] [PubMed] [Google Scholar]
- Research Data Assistance Center (ResDAC) 2011 Available CMS Data.Retrieved from http://www.resdac.org/Available_CMS_Data.asp.
- Stata. Data Analysis and Statistical Software (Release 8) [Computer software] Retrieved from http://www.stata.com/stata8/
- VA (Department of Veterans Affairs) Copayments for Inpatient Hospital Care and Outpatient Medical Care, Final Rule. Federal Register. 2001 Dec 6;66:63446–63449. [PubMed] [Google Scholar]
- VA (Department of Veterans Affairs) Veterans Health Administration, Office of the Under Secretary for Health for Policy and Planning System Support Group. FY2003 Geographic Access to Veterans Health Administration Services. 2005 Retrieved from http://vaww.pssg.med.va.gov/PSSG/pssg_vast_data.htm/
- VA (Department of Veterans Affairs) Health Care Eligibility and Enrollment. 2012 Retrieved from http://www.va.gov/healthbenefits/cost/copays.asp.
- Waldo DR. Accuracy and Bias of Race/Ethnicity Codes in the Medicare Enrollment Database. Health Care Financing Review. 2004;26(2):61–72. [PMC free article] [PubMed] [Google Scholar]
- Zhu CW, Penrod JD, Ross JS, Dellenbaugh C, Sano M. Use of Medicare and Department of Veterans Affairs Health Care by Veterans with Dementia: A Longitudinal Analysis. Journal of the American Geriatrics Society. 2009;57:1908–1914. doi: 10.1111/j.1532-5415.2009.02405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu CW, Livote EE, Ross JS, Penrod JD. A Random Effects Multinomial Logit Analysis of Using Medicare and VA Healthcare Among Veterans with Dementia. Home Health Care Services Quarterly. 2010;29:91–104. doi: 10.1080/01621424.2010.493771. [DOI] [PMC free article] [PubMed] [Google Scholar]