ABSTRACT
Purpose: The mechanisms linking cognition, balance function, and fall risk among older adults are not fully understood. An evaluation of the effect of cognition on balance tests commonly used in clinical practice to assess community-dwelling older adults could enhance the identification of at-risk individuals. The study aimed to determine (1) the association between cognition and clinical tests of balance and (2) the relationship between executive function (EF) and balance under single- and dual-task testing. Methods: Participants (24 women, mean age of 76.18 [SD 16.45] years) completed six clinical balance tests, four cognitive tests, and two measures of physical function. Results: Poor balance function was associated with poor performance on cognitive testing of EF. In addition, the association with EF was strongest under the dual-task timed up-and-go (TUG) test and the Fullerton Advanced Balance Scale. Measures of global cognition were associated only with the dual-task performance of the TUG. Postural sway measured with the Standing Balance Test, under single- or dual-task test conditions, was not associated with cognition. Conclusions: Decreased EF was associated with worse performance on functional measures of balance. The relationship between EF and balance was more pronounced with dual-task testing using a complex cognitive task combined with the TUG.
Key Words: accidental falls, aged, cognition, executive function, postural balance
RÉSUMÉ
Objectif : On ne comprend pas à fond les mécanismes qui établissent un lien entre la cognition, la fonction équilibre et le risque de chute chez les adultes âgés. L'évaluation de l'effet de la cognition sur les tests d'équilibre d'usage courant en pratique clinique pour évaluer les adultes âgés vivant dans des logements communautaires pourrait aider à repérer les personnes à risque. L'étude visait à déterminer le lien entre (1) la cognition et les tests cliniques d'équilibre et (2) la fonction d'exécution (FE) et l'équilibre au cours d'un test à tâche simple et à tâche double. Méthodes : Les participantes (24 femmes, âge moyen de 76,18 [ET 16,45] ans) se sont soumises à six tests d'équilibre clinique, quatre tests de cognition et deux mesures de fonction physique. Résultats : On a établi un lien entre une mauvaise fonction d'équilibre et un rendement médiocre au test cognitif de FE. En outre, le lien avec la FE était le plus solide dans le contexte du test chronométré à double tâche lever et marcher et du test d'équilibre avancé de Fullerton. On a établi un lien entre des mesures de la cognition globale et le rendement à l'exécution du test chronométré lever et marcher à double tâche seulement. On n'a pas établi de lien entre le balancement postural mesuré au moyen du test d'équilibre debout à tâche simple ou à tâche double et la cognition. Conclusions : On a établi un lien entre une baisse de la FE et le rendement le plus mauvais des mesures fonctionnelles de l'équilibre. Le lien entre la FE et l'équilibre était plus marqué au cours des tests à double tâche utilisant une tâche cognitive complexe combinée au test chronométré lever et marcher.
Mots clés : Fonction d'exécution, chutes accidentelles, âgé, équilibre postural, cognition
Falls among older adults are a significant public health problem and have substantial consequences for individual quality of life and independence. Each year, approximately 1.3 million community-dwelling older adults in Canada fall at least once, and half of those people will sustain multiple falls.1 Fall prevention guidelines recommend assessing balance and gait,2 but there is uncertainty as to what the best measures are for evaluating balance to determine fall risk across functional abilities.3,4 Physiotherapists play a prominent role in the assessment and prevention of falls in older adults; therefore, further evaluation of the performance capabilities of commonly used clinical measures can enhance clinicians' ability to assess and reduce risk.
An emerging area of falls research involves the role of cognition in postural control, a complex process involving the coordination of motor and sensory systems through higher-order neurological processes, executive function (EF) in particular. EF, which comprises the set of cognitive processes that use sensory information to modulate behaviour, is required for planning movements, dividing attention, and responding to changes in the environment.5–7 A recent systematic review identified EF as the cognitive domain most consistently associated with fall risk in older adults.8 An important related finding was that EF impairment can be masked by normal results on screening tests of global cognition, which evaluate multiple cognitive domains such as memory, attention, visual-spatial and executive function, and orientation to generate a single summary score.8
Observing people during a gait or balance task while they perform a secondary task (the dual-task paradigm) is an accepted way to assess the interaction between cognition and postural stability.9–11 The most prominent theory behind the dual-task paradigm is that poor multi-tasking performance is an indicator of changes in attentional capacities.12 In addition, the difficulty or novelty of a task, not just the number of simultaneous tasks, can significantly affect how well motor and cognitive information processing are performed simultaneously.13 Cognitive demands relative to a person's cognitive capacity will influence physical task performance: if the demands of executing two tasks simultaneously exceed cognitive capacity, the person's performance on either or both tasks will be degraded.5,10,13 This competition for attentional resources is believed to contribute to falls through an inability to produce an appropriate postural response.9
A relationship between gait and EF has been clearly demonstrated in the literature,5 and changes in gait under dual-task testing have been linked to falls in older adults.5,14 However, the relationship between dual-task balance testing and falls has been contradictory,15 indicating that the relationships between measures of cognitive function and balance performance under single- and dual-task testing require a more direct investigation.
The objectives of our study, therefore, were (1) to evaluate the association between cognitive function and clinical tests of balance commonly used to evaluate fall risk and (2) to determine the relationship between EF and balance performance under single- and dual-task testing. We hypothesized that (1) people with lower scores on cognitive function tests would demonstrate decreased balance and (2) those with EF impairment would demonstrate decreased balance both in absolute test scores and under dual-task testing conditions.
Methods
A convenience sample of 24 women was recruited from the community of the Sisters of St. Joseph in London, Canada. Potential participants were eligible for inclusion if they were older than 65 years, medically stable, English speaking, and able to understand simple instructions, and they were excluded if they had any neurological, musculoskeletal, or cardiorespiratory impairment that could compromise safe administration of the testing protocol. Our study was approved by the University of Western Ontario Research Ethics Board for Health Sciences Research Involving Human Subjects; all participants provided written informed consent.
Measures of balance
We evaluated six clinical tests of balance as the primary outcome measures. Usual footwear was worn for all balance tests.
Berg Balance Scale (BBS)
The BBS consists of 14 functional tasks of increasing difficulty, each scored from 0 to 4 (0=unable to perform the task; 4=task performed independently).16–19 The maximum score of 56 indicates no identifiable balance difficulties.
Timed up-and-go (TUG) test
The TUG assesses mobility and quantifies locomotor performance in older adults.20,21 In our study, participants were timed from the moment they stood up from a chair (seat height=48 cm), walked at their preferred usual pace for 3 m, turned around, walked back to the chair, and sat down. Participants were allowed to use the arms of the chair to get up and to use their mobility aid if they had one. It has been proposed that women between the ages of 65 and 85 years should be able to complete the TUG in 12 seconds or less.22
The timed up-and-go test with secondary cognitive task (TUG-cog)
Participants performed the TUG as described above while counting backwards by sevens from a number chosen randomly between 100 and 150.23
Standing Balance Test (SBT)
The SBT measures static balance in a standing position by quantifying the magnitude of postural sway.24,25 In our study, participants stood with their arms at their sides, feet comfortably apart, and eyes open for 30 seconds. A sway-metre was attached to a strap around the participant's waist with a pen on the end of a rod; postural sway movements were recorded on a sheet of millimetre graph paper. The graph paper was placed on an adjustable-height table so that the rod could be kept in a horizontal position. Maximal displacement in the frontal and sagittal planes was recorded on the graph paper, and the total sway area (cm2) was calculated by multiplying these values.
Standing Balance Test with secondary cognitive task (SBT-cog)
Participants performed the SBT as described above while counting backwards by sevens from a number randomly chosen between 100 and 150.
Fullerton Advanced Balance Scale (FAB)
The FAB is a 10-item scale that measures both static and dynamic balance.26 Each balance task is scored on a scale from 0 to 4 (0=unable to perform the task as defined; 4=task performed independently within specifications), though each task has unique wording for achieving a particular score. The maximum score of 40 indicates no identified balance difficulties.
Other measures of physical function
We measured lower-extremity strength using the 30-second chair stand test, which required participants to rise from a chair (seat height=48 cm) without using their hands as many times as possible within 30 seconds.27 The normative data for women are as follows: 11–16 repetitions for ages 65–69 years; 10–15 for ages 70–79 years; 9–14 for ages 80–84 years; 8–13 for ages 85–89 years; and 4–11 for ages 90–95 years.28
We used the 6-metre walk test (6MWT), a general measure of mobility, to determine average self-selected usual walking speed.29 Participants walked an 8 m path, using their usual mobility aid if needed, with the middle 6 m marked out to facilitate timing with a stopwatch; the 1 m at the beginning and end of the path accommodated acceleration and deceleration, ensuring that steady gait velocity was measured during the trial.
Affective and cognitive measures
Fear of falling was assessed using the Modified Falls Efficacy Scale (mFES),30 a 14-item self-report measure in which each item is rated on a scale from 0 to 10 (0=not confident at all; 10=completely confident). Responses are summed and averaged for a score out of 10. The maximum score of 10 indicates that the participant is completely confident in her balance ability.
Global cognitive status was assessed using the Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA). Both assessments have a maximum total score of 30; higher scores indicate better performance. The MMSE assesses orientation, attention, memory, and language; it has been validated as a tool with high reliability in a variety of patient populations.31 The MoCA is a valid and reliable brief screening tool used to detect mild cognitive impairment.32
Executive function was measured using the Trail Making Test (TMT). The TMT has two parts: Part A (TMT:a) requires participants to draw lines sequentially connecting 25 numbers, and Part B (TMT:b) requires them to draw lines sequentially alternating between numbers and letters (e.g., 1, A, 2, B,…). The TMT assesses visual search ability, scanning, speed of processing, mental flexibility, and executive functioning.33 Results are reported as the time in seconds required to complete the task; a longer completion time indicates greater impairment. The TMT is sensitive to a variety of neurological impairments and processes.33
Testing procedure
Each participant performed all tests during a single standardized 70-minute session. The session began with a brief subjective history given by each participant to obtain general demographic information. We recorded any self-reported falls—defined as unintentionally coming to rest on the floor or ground34—in the previous 12 months.
All participants wore a transfer belt during testing, and standby assistance was provided to ensure safety. Three testing stations were used, each with a different rater who performed the same outcome measures for all participants throughout the data collection phase. The order of testing was standardized for each participant and each station as follows: Station 1—TUG (single-task followed by dual-task condition), SBT (single-task followed by dual-task condition), and BBS; Station 2—mFES, MMSE, MoCA, and TMT Part A and B; and Station 3—FAB, 30-second chair stand, and 6MWT. All evaluators were final-year students in the Master of Physical Therapy program at the University of Western Ontario who had experience in performing all outcome measures.
Data analysis
Baseline characteristics and scores on tests of balance, cognition, and physical function were summarized using means and standard deviations or frequencies and percentages, as appropriate.
Our first objective was achieved by performing a univariate linear regression analysis between each cognitive test (the independent variable) and the balance test scores (dependent variable). A multivariable linear regression analysis, adjusted for age and history of falls, was performed between each measure of cognitive function and clinical tests of balance. Our second objective was achieved by analyzing the relationship of the TUG, TUG-cog, SBT, and SBT-cog with scores on the TMT:a and TMT:b tests. In a sensitivity analysis, two additional variables were derived: the difference in time between the TMT:a and TMT:b (TMT:b–TMT:a) and the percentage change in time between TMT:a and TMT:b ([TMT:b–TMT:a]/TMT:a).
We performed an exploratory analysis evaluating the change in test performance from the single-task to the dual-task condition, known as the dual-task cost (DTC). A DTC greater than 4 seconds has been previously established as the threshold associated with an increased fall risk in older adults.35 DTC percentage was calculated as [(single task value−dual task value)/single task value]×100%. All statistical analyses were performed using SPSS version 19.0 (SPSS, Inc., Chicago, IL) with statistical significance set at p<0.05.
Results
The convenience sample consisted of 24 women with a mean age of 76.18 (SD 16.45) years. Five participants (20.8%) reported falling in the previous 12 months; nine (37.5%) used a mobility aid. The mean number of medications was 3.25 (SD 0.76), and the mean number of comorbidities was 3.50 (SD 0.75). Results from the tests of balance, cognition, and other measures of physical performance are presented in Table 1.
Table 1.
Average Scores on Clinical Tests of Balance, Cognition, and Physical Function in a Sample of Community-Dwelling Older Women (n=24)
| Variable | Mean (SD) | Range |
|---|---|---|
| Clinical tests of balance | ||
| BBS | 47.6 (9.5) | 21–56 |
| TUG, s | 13.21 (6.80) | 8.00–34.00 |
| TUG-cog, s | 21.58 (14.17) | 8.00–63.00 |
| SBT, cm2 | 7.32 (7.83) | 1.02–36.26 |
| SBT-cog, cm2 | 6.97 (5.83) | 1.69–23.94 |
| FAB scale | 25.4 (9.4) | 4–38 |
| Clinical tests of affect and cognition | ||
| mFES | 8.9 (1.7) | 2.9–10 |
| MMSE | 28.3 (3.1) | 15–30 |
| MoCA | 24.9 (4.4) | 10–30 |
| TMT:a | 44.66 (14.48) | 27.30–80.00 |
| TMT:b | 102.97 (69.98) | 40.30–319.00 |
| Tests of physical performance | ||
| 6MWT, m/s | 1.02 (4.51) | 0.45–1.73 |
| 30 Second Chair Stand | 10.5 (4.3) | 4.0–19.0 |
BBS=Berg Balance Scale; TUG=timed up and -go test; s=seconds; TUG-cog=TUG test with cognitive dual-task of counting backwards by sevens; SBT=Standing Balance Test; SBT-cog=Standing Balance Test with cognitive dual-task of counting backwards by sevens; FAB=Fullerton Advanced Balance Scale; mFES=modified Falls Efficacy Scale; MMSE=Mini-Mental State Examination; MoCA=Montreal Cognitive Assessment; TMT:a=Trail Making Test version A; TMT:b=Trail Making Test version B; 6MWT=6-metre walk test; m/s=gait velocity in metres per second.
The adjusted linear regression demonstrated that EF was independently associated with balance function, although the method used to quantify balance function was important (Table 2). The BBS, TUG, TUG-cog, and FAB were associated with the TMT tests, but we found no association between the SBT or SBT-cog and any of the cognitive tests. The TUG-cog was independently associated with all tests of cognitive function, both global and EF-specific, and the FAB was associated with all cognitive measures except the MMSE. As time to complete the TMT:b increased, indicating poor EF, there was a worsening of balance function as indicated by the BBS, TUG, TUG-cog, and FAB. This pattern of association remained in the sensitivity analysis we performed on the difference in time between TMT:a and TMT:b, as measured by both absolute and percent change.
Table 2.
Results of Multivariable Linear Regression for the Association between Cognitive Function and Balance in Community-Dwelling Older Women (n=24)
| Clinical measures of balance, β coefficient (95% CI) |
||||||
|---|---|---|---|---|---|---|
| BBS | TUG | TUG-cog | SBT | SBT-cog | FABS | |
| MMSE | 0.75 (−0.40, 1.91) | −0.83 (−1.73, 0.07) | −2.87 (−4.47, −1.26)† | −0.52 (−1.65, 0.60) | −0.21 (−1.10, 0.67) | 0.96 (−0.13, 2.05) |
| MoCA | 0.44 (−0.04, 0.92) | −0.35 (−0.74, 0.04) | −0.93 (−1.72, −0.14)* | −0.17 (−0.66, 0.32) | −0.10 (−0.48, 0.28) | 0.47 (0.01, 0.93)* |
| TMT:a | −0.51 (−0.68, −0.34)† | 0.42 (0.29, 0.56)† | 0.85 (0.53, 1.17)† | 0.04 (−0.24, 0.32) | 0.01 (−0.21, 0.22) | −0.41 (−0.62, −0.19)† |
| TMT:b | −0.08 (−0.12, −0.04)† | 0.07 (0.04, 0.10)† | 0.16 (0.10, 0.22)† | 0.03 (0.02, 0.08) | 0.03 (−0.01, 0.07) | −0.09 (−0.12, −0.05)† |
Statistically significant at p≤0.001.
Statistically significant at p<0.05.
Note: Linear regression modelling is adjusted for age and history of falls.
BBS=Berg Balance Scale; TUG=timed up and go Test; TUG-cog=timed up and go Test with cognitive dual-task of counting backwards by sevens; SBT=Standing Balance Test; SBT-cog=Standing Balance Test with cognitive dual-task of counting backwards by sevens; FAB=Fullerton Advanced Balance Scale; MMSE=Mini-Mental State Examination; MoCA=Montreal Cognitive Assessment; TMT:a=Trail Making Test version A; TMT:b=Trail Making Test version B.
All participants took more time to complete the dual-task TUG than to complete the single-task TUG—on average, 9.61 (SD 10.51) seconds longer, or a DTC of 65.3%. Figure 1 shows the relationship between the TMT:b and both the single and dual-task TUG; as time to complete the TMT:b increased, so did the time to complete both the TUG and TUG-cog. A comparison of the dual-task to the single-task condition showed that postural sway from the SBT was increased in 13 people (64%) and decreased in 9 (37.5%). For each standing balance test, the amount of postural sway increased minimally with increasing time to complete the TMT:b, but the association was statistically insignificant (p>0.05).
Figure 1.
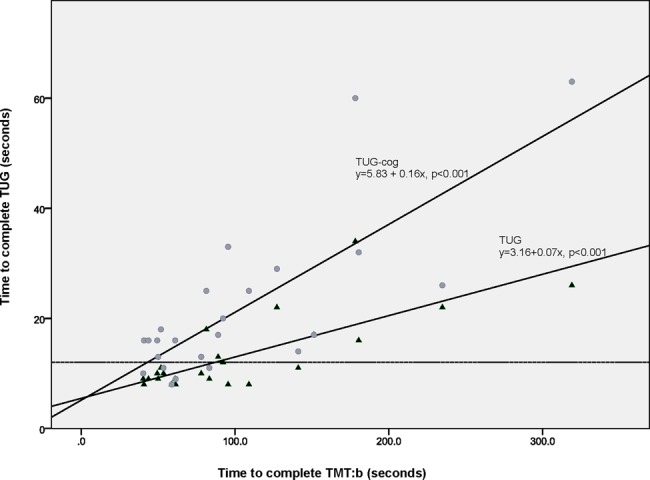
Graph of the lines of best fit from linear regression analysis for timed up and -go Test (▴) and dual-task timed up and go Test (•) scores plotted against the time to complete the Trail Making Test Part B (TMT:b) in a sample of community-dwelling older women (n=24).
Eight participants were identified as being at risk for falls (TUG≥12 s). A DTC of ≥4 seconds between the TUG and the TUG-cog identified 13 participants as being at risk. People with less than a 4 second differential had a mean increase of 18.8% in the time to complete the dual task TUG; those with greater than a 4 second differential had a mean increase of 104.6% in the time to complete the dual-task TUG.
Discussion
Our findings demonstrate that balance function is associated with EF among community-dwelling older women. Specifically, decreasing performance on EF testing was independently associated with decreasing performance on the TUG-cog and FAB. Executive dysfunction has repeatedly been associated with gait dysfunction;36–39 however, the role of EF in balance performance has not been formally evaluated in the literature.
A recent systematic review found that EF was consistently associated with increased risk of falls, while measures of global cognitive function were not useful in identifying higher risk in community-dwelling older adults without dementia.8 Our study found that two common measures of global cognitive function, the MMSE and the MoCA, were not independently associated with balance function, which is consistent with the findings of the systematic review. We have also shown that EF is related to balance function, particularly under the dual-task condition of the TUG using a secondary cognitive task. This finding is consistent with the theory that mobility problems and falls among people with cognitive impairments are, at least in part, related to their cognitive reserve.39
This study adds to our understanding of the relationship between cognition and postural stability, as it is the first study we are aware of to demonstrate that balance deficits observed in clinical tests are independently associated with executive cognitive dysfunction. An important corollary is that the term “cognitive impairment” should not be limited to a dementia diagnosis or poor results on global measures of cognition; the relationship between TMT:b and balance assessment scores suggests that the former may be a valuable tool in assessing fall risk for community-dwelling older adults.7
The SBT and SBT-cog tests were not significantly associated with any of the cognitive tests. It is possible that the task of maintaining static balance, even with the addition of a secondary cognitive challenge, did not sufficiently load the attentional system to elicit detectable differences between participants. Attention requirements are not constant and vary with the postural task, balance abilities, and age.40 As the demand for stability increases (e.g., walking vs. quiet stance), an increase in attentional resources is expected for postural control. In addition, not all cognitive tasks will interact with postural control processing in the same way, so it is possible that another type of secondary task might have yielded detectable changes. Studies have suggested that the majority of falls among community-dwelling older women result from undertaking more complex tasks such as walking, climbing stairs, carrying an object, or reaching.41,42 Therefore, static stance may not be an appropriate means of assessing fall risk for the average older adult.
Our finding that 37.5% of our sample showed reduced postural sway on the SBT-cog is in contrast to work by Bernard-Demanze and colleagues43 on dual-task effects in balance. This finding may indicate that balance function improves under dual-task testing if the secondary task leads to a heightened level of arousal, allowing the person to better attend to the two simultaneous tasks.44 Another possible explanation is that directing attention to a highly automatic process leads to a loss of efficiency in postural control mechanisms, while focusing attention on a secondary task may improve automaticity and efficiency of postural control.40 This second explanation has been demonstrated in young adults but was observed only during simple dual-task test conditions in older adults.45 It might be expected that postural control is prioritized over the cognitive task when a person has a more limited ability to attend to both tasks fully. Unfortunately, though participants were instructed to attend to both tasks equally, the dual-task cost of the cognitive task could not be evaluated. The significance of a decrease in postural sway during dual-task testing needs further evaluation to determine the relevance of this finding related to adverse outcomes such as falls.
The FAB was significantly associated with all of the cognitive measures assessed. The FAB was developed specifically to assess balance in high-functioning older adults living independently in the community and therefore contains more challenging tasks than other balance scales.26 The inclusion of advanced functional tasks may more accurately approximate the daily challenges encountered by older adults in the community that place them at risk for loss of balance.
Dual-task costs between the TUG and TUG-cog identified more participants at an elevated fall risk than the standard testing format. The dual-task test is not only fast and simple to perform but also could facilitate earlier identification of people who are at risk for falls, allowing interventions to be initiated sooner to reduce fall risk.
Our study has several limitations. Because our study was cross-sectional, we were not able to establish a causal relationship between EF impairment and balance. The association between dual-task testing of balance and future falls needs to be evaluated in a prospective cohort study. The small sample size of our study may have reduced our ability to find a statistically significant association between the cognition and balance tests, and therefore the magnitude of association is considered a conservative estimate. Another limitation of this study was that participants were all members of the same religious order and may not be representative of older community-dwelling women. These considerations will also have an effect on the generalizability of the results to older men.
Conclusions
Our study has demonstrated that balance is independently associated with cognitive function, specifically the domain of executive function (EF). Importantly, EF is a key feature to analyze when evaluating balance. This study highlights the fact that EF's contribution to postural stability can be measured through dual-task testing, which mimics the multi-tasking required in everyday situations. Further, dual-task tests may unmask subclinical impairments to identify people at risk of falls sooner than single-task tests, thus enabling earlier interventions to improve balance and decrease fall risk. Finally, our results suggest that cognition, notably EF, needs to be more thoroughly researched to determine whether adding cognitive training to standard rehabilitation strategies can improve the balance of older adults.
Key messages
What is already known on this topic
Cognition is an essential element in the maintenance of postural stability. Previous research has found that impaired executive function is consistently associated with an elevated fall risk and gait dysfunction; the association between measures of cognitive function and common clinical tests of balance used to identify fall risk has not been evaluated.
What this study adds
Executive function, measured using the Trail Making Test Part B, was independently associated with functional, but not static, balance abilities. Dual-task tests that specifically challenge the working capacity of executive function have a stronger relationship to impaired postural function. It is recommended that dual-task testing be used in assessing balance and fall risk to facilitate the earlier identification of people at risk for falls.
Physiotherapy Canada 2014; 66(2);179–186; doi:10.3138/ptc.2013-16
References
- 1.Public Health Agency of Canada. Report on seniors' falls in Canada. Ottawa: Public Works and Government Services Canada; 2005. [cited 2013 Dec 16]. Available from: http://publications.gc.ca/collections/Collection/HP25-1-2005E.pdf. [Google Scholar]
- 2.Panel on Prevention of Falls in Older Persons; American Geriatrics Society; British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–57. doi: 10.1111/j.1532-5415.2010.03234.x. http://dx.doi.org/10.1111/j.1532-5415.2010.03234.x. Medline:21226685. [DOI] [PubMed] [Google Scholar]
- 3.Muir SW, Berg K, Chesworth B, et al. Application of a fall screening algorithm stratified fall risk but missed preventive opportunities in community-dwelling older adults: a prospective study. J Geriatr Phys Ther. 2010;33(4):165–72. Medline:21717920. [PubMed] [Google Scholar]
- 4.Lamb SE, McCabe C, Becker C, et al. The optimal sequence and selection of screening test items to predict fall risk in older disabled women: the Women's Health and Aging Study. J Gerontol A Biol Sci Med Sci. 2008;63(10):1082–8. doi: 10.1093/gerona/63.10.1082. http://dx.doi.org/10.1093/gerona/63.10.1082. Medline:18948559. [DOI] [PubMed] [Google Scholar]
- 5.Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. 2008;23(3):329–42, quiz 472. doi: 10.1002/mds.21720. http://dx.doi.org/10.1002/mds.21720. Medline:18058946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing. 2006;35(Suppl 2):ii7–11. doi: 10.1093/ageing/afl077. http://dx.doi.org/10.1093/ageing/afl077. Medline:16926210. [DOI] [PubMed] [Google Scholar]
- 7.Lord SR, Sherrington C, Menz HB. Falls in older people: risk factors and strategies for prevention. Cambridge. UK: Cambridge University Press; 2007. http://dx.doi.org/10.1017/CBO9780511722233. [Google Scholar]
- 8.Muir SW, Gopaul K, Montero Odasso MM. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing. 2012;41(3):299–308. doi: 10.1093/ageing/afs012. http://dx.doi.org/10.1093/ageing/afs012. Medline:22374645. [DOI] [PubMed] [Google Scholar]
- 9.Brauer SG, Burns YR, Galley P. A prospective study of laboratory and clinical measures of postural stability to predict community-dwelling fallers. J Gerontol A Biol Sci Med Sci. 2000;55(8):M469–76. doi: 10.1093/gerona/55.8.m469. http://dx.doi.org/10.1093/gerona/55.8.M469. Medline:10952371. [DOI] [PubMed] [Google Scholar]
- 10.Woollacott M, Shumway-Cook A. Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture. 2002;16(1):1–14. doi: 10.1016/s0966-6362(01)00156-4. http://dx.doi.org/10.1016/S0966-6362(01)00156-4. Medline:12127181. [DOI] [PubMed] [Google Scholar]
- 11.Snijders AH, Verstappen CC, Munneke M, et al. Assessing the interplay between cognition and gait in the clinical setting. J Neural Transm. 2007;114(10):1315–21. doi: 10.1007/s00702-007-0781-x. http://dx.doi.org/10.1007/s00702-007-0781-x. Medline:17612789. [DOI] [PubMed] [Google Scholar]
- 12.Faulkner KA, Redfern MS, Cauley JA, et al. Health, Aging, and Body Composition Study. Multitasking: association between poorer performance and a history of recurrent falls. J Am Geriatr Soc. 2007;55(4):570–6. doi: 10.1111/j.1532-5415.2007.01147.x. http://dx.doi.org/10.1111/j.1532-5415.2007.01147.x. Medline:17397436. [DOI] [PubMed] [Google Scholar]
- 13.Dault MC, Geurts AC, Mulder TW, et al. Postural control and cognitive task performance in healthy participants while balancing on different support-surface configurations. Gait Posture. 2001;14(3):248–55. doi: 10.1016/s0966-6362(01)00130-8. http://dx.doi.org/10.1016/S0966-6362(01)00130-8. Medline:11600328. [DOI] [PubMed] [Google Scholar]
- 14.Beauchet O, Annweiler C, Dubost V, et al. Stops walking when talking: a predictor of falls in older adults? Eur J Neurol. 2009;16(7):786–95. doi: 10.1111/j.1468-1331.2009.02612.x. http://dx.doi.org/10.1111/j.1468-1331.2009.02612.x. Medline:19473368. [DOI] [PubMed] [Google Scholar]
- 15.Zijlstra A, Ufkes T, Skelton DA, et al. Do dual tasks have an added value over single tasks for balance assessment in fall prevention programs? A mini-review. Gerontology. 2008;54(1):40–9. doi: 10.1159/000117808. http://dx.doi.org/10.1159/000117808. Medline:18460873. [DOI] [PubMed] [Google Scholar]
- 16.Berg KO, Wood-Dauphinee SL, Willimas JI, et al. Measuring balance n elderly: preliminary development of an instrument. Physiother Can. 1989;41(6):304–11. http://dx.doi.org/10.3138/ptc.41.6.304. [Google Scholar]
- 17.Berg KO, Maki BE, Williams JI, et al. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992;73(11):1073–80. Medline:1444775. [PubMed] [Google Scholar]
- 18.Berg KO, Wood-Dauphinee SL, Williams JI, et al. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(Suppl 2):S7–11. Medline:1468055. [PubMed] [Google Scholar]
- 19.Muir SW, Berg K, Chesworth B, et al. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449–59. doi: 10.2522/ptj.20070251. http://dx.doi.org/10.2522/ptj.20070251. Medline:18218822. [DOI] [PubMed] [Google Scholar]
- 20.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. Medline:1991946. [DOI] [PubMed] [Google Scholar]
- 21.Scott V, Votova K, Scanlan A, et al. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing. 2007;36(2):130–9. doi: 10.1093/ageing/afl165. http://dx.doi.org/10.1093/ageing/afl165. Medline:17293604. [DOI] [PubMed] [Google Scholar]
- 22.Bischoff HA, Stähelin HB, Monsch AU, et al. Identifying a cut-off point for normal mobility: a comparison of the timed ‘up and go’ test in community-dwelling and institutionalised elderly women. Age Ageing. 2003;32(3):315–20. doi: 10.1093/ageing/32.3.315. http://dx.doi.org/10.1093/ageing/32.3.315. Medline:12720619. [DOI] [PubMed] [Google Scholar]
- 23.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903. Medline:10960937. [PubMed] [Google Scholar]
- 24.Lord SR, Castell S. Physical activity program for older persons: effect on balance, strength, neuromuscular control, and reaction time. Arch Phys Med Rehabil. 1994;75(6):648–52. doi: 10.1016/0003-9993(94)90187-2. http://dx.doi.org/10.1016/0003-9993(94)90187-2. Medline:8002763. [DOI] [PubMed] [Google Scholar]
- 25.Lord SR, Menz HB, Tiedemann A. A physiological profile approach to falls risk assessment and prevention. Phys Ther. 2003;83(3):237–52. Medline:12620088. [PubMed] [Google Scholar]
- 26.Rose DJ, Lucchese N, Wiersma LD. Development of a multidimensional balance scale for use with functionally independent older adults. Arch Phys Med Rehabil. 2006;87(11):1478–85. doi: 10.1016/j.apmr.2006.07.263. http://dx.doi.org/10.1016/j.apmr.2006.07.263. Medline:17084123. [DOI] [PubMed] [Google Scholar]
- 27.Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–9. doi: 10.1080/02701367.1999.10608028. http://dx.doi.org/10.1080/02701367.1999.10608028. Medline:10380242. [DOI] [PubMed] [Google Scholar]
- 28.Jones CJ, Rikli RE. Measuring functional fitness of older adults. J Active Aging. 2002 Mar-Apr;:24–30. [Google Scholar]
- 29.Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13(10):881–9. doi: 10.1007/s12603-009-0246-z. http://dx.doi.org/10.1007/s12603-009-0246-z. Medline:19924348. [DOI] [PubMed] [Google Scholar]
- 30.Hill KD, Schwarz JA, Kalogeropoulos AJ, et al. Fear of falling revisited. Arch Phys Med Rehabil. 1996;77(10):1025–9. doi: 10.1016/s0003-9993(96)90063-5. http://dx.doi.org/10.1016/S0003-9993(96)90063-5. Medline:8857881. [DOI] [PubMed] [Google Scholar]
- 31.Molloy DW, Alemayehu E, Roberts R. Reliability of a standardized mini-mental state examination compared with the traditional mini-mental state examination. Am J Psychiatry. 1991;148(1):102–5. doi: 10.1176/ajp.148.1.102. Medline:1984692. [DOI] [PubMed] [Google Scholar]
- 32.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9. doi: 10.1111/j.1532-5415.2005.53221.x. http://dx.doi.org/10.1111/j.1532-5415.2005.53221.x. Medline:15817019. [DOI] [PubMed] [Google Scholar]
- 33.Tombaugh TN. Trail Making Test A and B: normative data stratified by age and education. Arch Clin Neuropsychol. 2004;19(2):203–14. doi: 10.1016/S0887-6177(03)00039-8. http://dx.doi.org/10.1016/S0887-6177(03)00039-8. Medline:15010086. [DOI] [PubMed] [Google Scholar]
- 34.Speechley M, Belfry S, Borrie MJ, et al. Risk factors for falling among community-dwelling veterans and their caregivers. Can J Aging. 2005;24(3):261–74. doi: 10.1353/cja.2005.0083. http://dx.doi.org/10.1353/cja.2005.0083. Medline:16421850. [DOI] [PubMed] [Google Scholar]
- 35.Lundin-Olsson L, Nyberg L, Gustafson Y. Attention, frailty, and falls: the effect of a manual task on basic mobility. J Am Geriatr Soc. 1998;46(6):758–61. doi: 10.1111/j.1532-5415.1998.tb03813.x. Medline:9625194. [DOI] [PubMed] [Google Scholar]
- 36.Muir SW, Speechly M, Wells J, et al. Gait assessment in mild cognitive impairment and Alzheimer's disease: the effect of dual-task challenges across the cognitive spectrum. Gait Posture. 2012;35(1):96–100. doi: 10.1016/j.gaitpost.2011.08.014. http://dx.doi.org/10.1016/j.gaitpost.2011.08.014. Medline:21940172. [DOI] [PubMed] [Google Scholar]
- 37.Montero-Odasso M, Muir SW, Speechley M. Dual-task complexity affects gait in people with mild cognitive impairment: the interplay between gait variability, dual tasking, and risk of falls. Arch Phys Med Rehabil. 2012;93(2):293–9. doi: 10.1016/j.apmr.2011.08.026. http://dx.doi.org/10.1016/j.apmr.2011.08.026. Medline:22289240. [DOI] [PubMed] [Google Scholar]
- 38.Montero-Odasso M, Verghese J, Beauchet O, et al. Gait and cognition: a complementary approach to understanding brain function and the risk of falling. J Am Geriatr Soc. 2012;60(11):2127–36. doi: 10.1111/j.1532-5415.2012.04209.x. Medline:23110433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beauchet O, Annweiler C, Montero-Odasso M, et al. Gait control: a specific subdomain of executive function? J Neuroeng Rehabil. 2012;9(1):12. doi: 10.1186/1743-0003-9-12. http://dx.doi.org/10.1186/1743-0003-9-12. Medline:22321772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shumway-Cook A, Woollacott M. Motor control: translating research into clinical practice. 4th ed. Philadelphia: Wolters Kluwer; 2012. [Google Scholar]
- 41.Herman T, Mirelman A, Giladi N, et al. Executive control deficits as a prodrome to falls in healthy older adults: a prospective study linking thinking, walking, and falling. J Gerontol A Biol Sci Med Sci. 2010;65(10):1086–92. doi: 10.1093/gerona/glq077. http://dx.doi.org/10.1093/gerona/glq077. Medline:20484336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nachreiner NM, Findorff MJ, Wyman JF, et al. Circumstances and consequences of falls in community-dwelling older women. J Womens Health (Larchmt) 2007;16(10):1437–46. doi: 10.1089/jwh.2006.0245. http://dx.doi.org/10.1089/jwh.2006.0245. Medline:18062759. [DOI] [PubMed] [Google Scholar]
- 43.Bernard-Demanze L, Dumitrescu M, Jimeno P, et al. Age-related changes in posture control are differentially affected by postural and cognitive task complexity. Curr Aging Sci. 2009;2(2):135–49. http://dx.doi.org/10.2174/1874609810902020135. Medline:20021408. [PubMed] [Google Scholar]
- 44.Andersson G, Hagman J, Talianzadeh R, et al. Effect of cognitive load on postural control. Brain Res Bull. 2002;58(1):135–9. doi: 10.1016/s0361-9230(02)00770-0. http://dx.doi.org/10.1016/S0361-9230(02)00770-0. Medline:12121823. [DOI] [PubMed] [Google Scholar]
- 45.Huxhold O, Li S-C, Schmiedek F, et al. Dual-tasking postural control: aging and the effects of cognitive demand in conjunction with focus of attention. Brain Res Bull. 2006;69(3):294–305. doi: 10.1016/j.brainresbull.2006.01.002. http://dx.doi.org/10.1016/j.brainresbull.2006.01.002. Medline:16564425. [DOI] [PubMed] [Google Scholar]


