Abstract
OBJECTIVES:
Early preventive dental visits are essential in improving children’s oral health, especially young children at high risk for dental caries. However, there is scant information on how these children enter the dental care system. Our objectives were as follows: (1) to describe how a population-based cohort of young Medicaid-enrolled children entered dental care; and (2) to investigate the influence of caregiver characteristics on their children’s dental care–seeking patterns.
METHODS:
We relied on Medicaid claims and interview data of caregiver–child dyads who were enrolled in the Carolina Oral Health Literacy study during 2007–2008. The analytical cohort comprised 1000 children who had no dental visits before enrollment. Additional information was collected on sociodemographic characteristics, oral health status, health literacy, dental neglect, and access to care barriers. Our analyses relied on descriptive, bivariate, and multivariate methods.
RESULTS:
During the 25-month median follow-up period, 39% of the children (mean baseline age: 16 months) entered the dental care system, and 13% of their first encounters were for emergency care. Caregivers’ dental neglect emerged as a significant predictor of nonentrance. Children with reported oral health problems at baseline were more likely to enter the dental care system compared with children with better oral health, but they were also more likely to require emergency care.
CONCLUSIONS:
Caregivers have a pivotal role in children’s oral health and care. Interventions aimed at improving children’s oral health should involve community outreach to engage caregivers in a culturally appropriate manner when their children are infants or toddlers.
Keywords: caregivers, children, dental neglect, dentistry, health literacy, health services, health services use, literacy, oral health
What’s Known on This Subject:
Early establishment of a dental home is critical for addressing the “silent epidemic” of early childhood caries. Physicians and dentists have worked to improve children’s access to dental care, but little is known about caregivers’ role in this context.
What This Study Adds:
Addressing factors that affect the establishment of a child’s dental home, such as caregivers’ dental neglect and problem-driven care-seeking behaviors, is essential. Caregiver engagement seems to be pivotal for increasing use of preventive services while decreasing episodic and problem-initiated care.
Recent evidence indicates that changes in young children’s oral health during the past 2 decades in the United States have not followed marked improvements documented among other age groups.1 Dental caries remains the most common chronic disease in childhood and affects the most vulnerable.2 The most recent epidemiologic surveillance data reveal that 14% of 3- to 5-year-old US children had untreated dental decay in 2009–2010; this proportion was 25% for families living below the poverty level.3 This “silent epidemic” of childhood dental disease is characterized by marked disparities4 and confers severe multilevel effects on children, their families, communities, and the health system.5
Effective preventive strategies to address the caries epidemic for preschool-aged children are warranted. Both the American Academy of Pediatric Dentistry and the American Academy of Pediatrics have articulated the value of early preventive dental visits and the establishment of a dental home.6 Although early dental visits are an integral dimension of anticipatory guidance,7 the evidence base supporting their effectiveness in preventing dental disease is weak,8 and young children’s utilization of preventive services is low.2,9 It is estimated that ∼90% of infants and 1-year-old children had a pediatrician visit in 2000–2005, yet only 1.5% had a dental visit in the same time frame.10 A variety of “distal” factors are likely influences of young children’s receipt of preventive dental services, including health system and insurance coverage factors, physical environment, workforce availability, distribution, and cultural competency.11–14 In addition to these systemic factors, caregiver characteristics are obvious proximal influences of receiving recommended preventive dental services by young children who rely entirely on their caregivers for their oral health care.15
Nationally representative surveys have found links between caregivers’ age, health status, race, ethnicity, education, income, insurance status, and their children’s receipt of preventive dental care.9,16,17 Without proper guidance and counseling, caregivers’ dental care seeking for their children may be problem-initiated, episodic, and therefore poorly and inappropriately timed and ineffective. To make matters worse, caregivers are generally not adept at recognizing the initial signs of early childhood caries in very young children.18 This phenomenon helps explain why seeking dental care at an emergency department for nontraumatic dental conditions is not uncommon,19 illustrating a deficient preventive dental care services system.
Adding to the pivotal role of caregivers’ attitudes, beliefs, and perceptions, Kelly et al20 reported an association of “expectation of poor oral health” among low-income caregivers with nonutilization of dental care for their children. Other factors that have recently emerged as important determinants of child oral health–related behaviors and outcomes include caregivers’ health literacy,21–23 child and caregiver oral health status,24 and dental neglect.25
With this backdrop, the overarching goal of the present investigation was to expand on the knowledge base of caregiver factors that may influence children’s receipt of dental services. Using a prospective study design and in the context of a well-characterized cohort of child–caregiver dyads, we focused on sociodemographic factors, health literacy, perceived oral health status, and dental neglect. Our specific aims were as follows: (1) to describe how a population-based cohort of young Medicaid-enrolled children entered dental care; and (2) to investigate the association between caregiver characteristics and their children’s dental care–seeking patterns.
Methods
Study Description and Participants
This investigation was based on the Carolina Oral Health Literacy (COHL) cohort, a prospective study of health literacy and oral health outcomes among caregivers and children in North Carolina.26 During July 2008 to July 2009, COHL enrolled 1405 child–caregiver dyads in 7 counties in North Carolina, by using the following inclusion criteria: caregivers aged >18 years, English speaking, clients of the Supplemental Nutrition Program for Women, Infants, and Children (WIC), the primary caregivers of a healthy, Medicaid-eligible infant or child aged ≤60 months, or expecting a newborn within the ensuing 8 months. Data were collected via structured interviews at enrollment by 2 trained interviewers. Ethical approval and informed written consent were obtained, including the linkage with Medicaid claims data for the children’s lifetime up to December 2010.
Definition of the Analytical Cohort
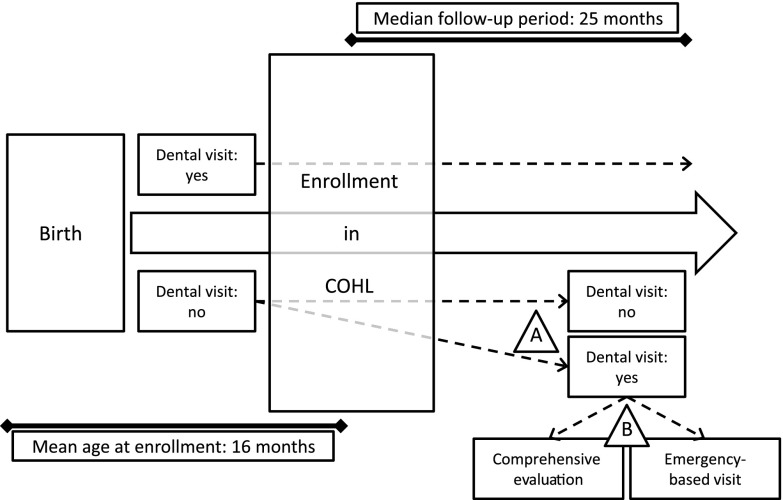
A schematic illustration of the study’s analytical cohort is presented in Fig 1. First, a subset of the entire COHL cohort of caregiver–child dyads was defined by applying the following exclusions: unborn children (n = 134 [9.5%]), 2 caregivers aged <18 years (0.1%), children with no Medicaid enrollment information (n = 60 [4.3%]), and those with <6 months of available Medicaid data during the follow-up period (n = 22 [1.6%]). Second, all available children’s Medicaid-paid (K-category) claims were reviewed to identify children who already had a dental visit before enrolling in COHL (based on any “Dxxxx” Medicaid claim codes, indicating a dental office–provided service). This step identified 187 children (13.3%) who had already entered the system and thus were excluded. In sum, a total of 405 dyads were excluded from the original cohort of 1405, resulting in an analytical sample of 1000 for the present analysis.
FIGURE 1.
Schematic representation of the COHL study’s analytical cohort of child–caregiver dyads. The current investigation included children who had not had their first dental visit at the time of COHL enrollment (n = 1000), and followed up these children prospectively to determine (A) their entry into the dental care system and (B) the type of their first dental visit.
Measures and Variables
Entry to the dental care system and mode of entry were the study’s outcomes of interest and were defined by using Medicaid-paid (K) claims filed concurrently with or after participants’ enrollment in COHL in calendar years 2008–2010. First, unique oral health–related visits were identified and characterized in the following domains: (1) hospital-based dental-related emergency visit (oral health–related diagnoses [International Classification of Diseases, Ninth Revision: 520–529] and Current Procedural Terminology procedure codes [99281-5 and RC450] filed concurrently with emergency department claims); (2) dental office–based emergency visit (D0140 or D0160); and (3) dental office–based “routine” dental visits (not falling into the previous categories and having D0150 or D0145 codes). The chronological first visit was used to categorize children’s entry into the dental care system as a comprehensive oral evaluation or emergency visit. Based on these definitions, 2 binary indicator variables were defined: dental entry (yes/no) and entry mode (comprehensive/emergency).
Covariates included caregivers’ and children’s characteristics, including sociodemographic characteristics, oral health status, health literacy, and dental neglect. Caregivers’ race was self-reported and classified as white, African American, or American Indian; age was measured in years and coded as a quartile categorical variable. Education was measured as less than high school, high school or general equivalency diploma, and some college/college or higher. Marital status was defined as single, married, or divorced/separated/other. Caregivers’ and children’s oral health status was assessed by using a National Health and Nutrition Examination Survey item: “How would you assess the condition of your/child’s teeth and gums?” Possible responses were excellent, very good, good, fair, and poor. Caregivers were asked to report on additional child oral health–related problems, including “pain,” “cavities,” “broken front teeth/teeth that need repair,” and whether they needed dental care during the preceding 12 months but could not obtain it (perceived barrier of access to care).
Because health literacy entails a wide range of skills and dimensions,27 2 literacy instruments were used: the Rapid Estimate of Adult Literacy in Dentistry (REALD)-30 and the Newest Vital Sign (NVS). The REALD-30 is a word recognition test specifically designed to address the needs of the dental environment. It includes 30 words arranged in order of increasing difficulty, which the participants are asked to pronounce, resulting in a score range of 0 (lowest) to 30 (highest literacy). The REALD-30 has been shown to have good psychometric properties28 and, in recent studies,29–32 has correlated with a wide range of oral health outcomes. In this study, a REALD-30 score <13 was used to denote low health literacy.15,32 The NVS is a comprehension and numeracy test, based on 6 questions pertaining to the interpretation of a food label.33 The instrument’s score ranges from 0 (lowest literacy) to 6 (highest literacy). Used extensively, the NVS has been found to be a valid and reliable screening tool for low health literacy.34
To measure dental neglect, we used a modified version of the Dental Neglect Scale (DNS),35,36 as described by Lee et al.29 The DNS contains 6 questions describing dental behaviors (eg, “I need dental care, but I put if off”). Participants’ agreement with these statements is assessed on a 4-point Likert scale from 1 (“definitely not”) to 4 (“definitely yes”). A DNS score ranging from 6 (least neglect) to 24 (most neglect) was computed as the sum of responses. We used a normalized DNS score to facilitate interpretation of the final models’ effect estimates.
Analytical Strategy
Descriptive statistics were used based on proportions, means, medians, and 95% confidence intervals (CIs) to present the cohort’s sociodemographic characteristics, oral health status, health literacy, and dental neglect estimates. We examined bivariate associations of these measures with entry into dental care and mode of entry by using χ2 tests for categorical variables and t tests for continuous ones. To disentangle the impact of sociodemographic factors, oral health status, health literacy, and dental neglect factors on children’s entry to the dental care system, we conducted multivariate logistic regression analyses. To account for the varying study follow-up times, we adjusted all models for children’s observed Medicaid-enrolled months. The multivariate model for “dental care entry” was constructed including a priori all caregiver’s and children’s sociodemographic characteristics (race, gender, age, and education), whereas additional variables (dental neglect, marital status, number of children, health literacy, and oral health–specific variables) were carried forward in the final model if they met a P < .2 threshold in bivariate testing and were retained if they resulted in a change in estimate of the dental neglect estimate by ≥10%. Inclusion of covariates in the multivariate model for “mode of entry” was determined in a similar fashion, using a P < .2 criterion in bivariate testing. To overcome known issues of using odds ratios (OR) for common outcomes and to facilitate interpretation, we estimated and report average marginal effects (AMEs).37,38 The AMEs correspond to changes in predicted probability of dental system entry across levels of the examined covariates. Analyses were performed by using Stata version 13.1 (StataCorp LP, College Station, TX).
Results
The analytical cohort consisted of predominantly female, single caregivers with a high school education or less who had 1 child. Most children were aged <1 year. Over the median 25-month follow-up period (range: 6–30 months), 39% of children had their first dental visit. With regard to sociodemographic characteristics, caregivers’ and children’s ages were significantly associated with the likelihood of entering the dental care system during follow-up (Table 1). Similarly, having ≥2 children compared with 1 child and being currently or formerly married were associated with an increased likelihood of system entrance.
TABLE 1.
Sociodemographic Characteristics of the Analytical Cohort of COHL Child–Caregiver Dyads (N = 1000)
| Characteristic | Totala,b | Entered the Dental Care Systema,c | Did Not Enter the Dental Care Systema,c | Pd |
|---|---|---|---|---|
| No. of subjects | 1000 (100) | 387 (39) | 613 (61) | |
| Race | .2 | |||
| White | 388 (39) | 152 (39) | 236 (61) | |
| African American | 395 (40) | 164 (42) | 231 (58) | |
| American Indian | 208 (21) | 70 (34) | 138 (66) | |
| Caregiver’s gender | .8 | |||
| Male | 38 (4) | 14 (37) | 24 (63) | |
| Female | 962 (96) | 373 (39) | 589 (61) | |
| Caregiver’s age, y (tertiles; range)e | <.001 | |||
| Q1 (18.0–21.7) | 20.0 (20.0) | 71 (29) | 170 (71) | |
| Q2 (21.7–25.0) | 23.2 (23.2) | 91 (36) | 161 (64) | |
| Q3 (25.0–30.0) | 27.2 (27.0) | 111 (44) | 140 (56) | |
| Q4 (30.0–63.9) | 36.7 (35.0) | 114 (45) | 142 (55) | |
| Child’s age, mo (at baseline interview) | <.001 | |||
| 0–11 | 512 (51) | 128 (25) | 384 (75) | |
| 12–23 | 212 (21) | 92 (43) | 120 (57) | |
| 24–35 | 162 (16) | 91 (56) | 71 (44) | |
| 36–47 | 103 (10) | 69 (67) | 34 (33) | |
| 48–59 | 11 (1) | 7 (64) | 4 (36) | |
| Education | .3 | |||
| <High school | 247 (25) | 90 (36) | 157 (64) | |
| High school/GED | 387 (39) | 144 (37) | 243 (63) | |
| Some college or higher | 366 (31) | 153 (42) | 213 (58) | |
| Marital status | .02 | |||
| Single | 660 (66) | 236 (36) | 424 (64) | |
| Married | 243 (24) | 104 (43) | 139 (57) | |
| Divorced/separated/other | 97 (10) | 47 (48) | 50 (52) | |
| No. of children | <.001 | |||
| 1 | 424 (42) | 129 (30) | 295 (70) | |
| 2 | 322 (32) | 155 (48) | 167 (52) | |
| 3 | 145 (15) | 64 (44) | 81 (56) | |
| ≥4 | 108 (11) | 39 (36) | 69 (64) |
GED, general educational development; Q, quartile.
Estimates among participants with nonmissing information in stratum.
Data are presented as n (column %).
Data are presented as n (row %).
Corresponding to χ2 tests for categorical variables and Student’s t tests for continuous variables.
Mean (median).
Table 2 presents caregivers’ and children’s oral health–related characteristics. One-third reported their oral health as fair/poor. One-quarter had low health literacy according to the REALD-30 and 17% had low health literacy according to the NVS instrument. Caregivers whose children did not enter the dental care system had poorer oral health, lower comprehension-based health literacy, and higher dental neglect; however, these differences were small in magnitude and did not meet statistical significance criteria. At baseline, small numbers of caregivers reported their children had fair or poor oral health (4%), pain (4%), or cavities (3%), but a higher proportion (11%) reported a barrier of access to dental care. With the exception of “pain,” a positive association between these oral health “problems” as well as barriers was found with subsequent entry to the dental care system.
TABLE 2.
Caregiver and Child Oral Health–Related Factors in the Analytical Cohort of COHL Child–Caregiver Dyads (N = 1000)
| Characteristic | Entire Samplea,b | Entered the Dental Care Systema,c | Did Not Enter the Dental Care Systema,c | Pd |
|---|---|---|---|---|
| No. of subjects | 1000 (100) | 387 (39) | 613 (61) | |
| Caregiver characteristics | ||||
| Caregiver oral health | .2 | |||
| Excellent/very good/good | 650 (65) | 260 (40) | 390 (60) | |
| Fair/poor | 346 (35) | 125 (36) | 221 (64) | |
| Health literacy | ||||
| Word recognitione | .7 | |||
| Adequate (REALD-30 ≥13) | 715 (75) | 283 (40) | 432 (60) | |
| Low (REALD-30 <13) | 233 (25) | 89 (38) | 144 (62) | |
| Comprehension | .1 | |||
| Low (NVS: 0–1) | 174 (17) | 60 (34) | 114 (66) | |
| Moderate (NVS: 2–3) | 416 (42) | 154 (37) | 262 (63) | |
| Higher (NVS: 4–6) | 409 (41) | 173 (42) | 236 (58) | |
| Dental neglect score (mean, 95% CI) | 11.9 (11.7 to 12.1) | 11.7 (11.3 to 12.0) | 12.0 (11.8 to 12.3) | .07 |
| Child characteristics | ||||
| Reported child oral health | .06 | |||
| Excellent/very good/good | 591 (96) | 290 (49) | 301 (51) | |
| Fair/poor | 25 (4) | 17 (68) | 8 (32) | |
| Reported child dental problems | ||||
| Pain | .2 | |||
| Yes | 27 (4) | 10 (37) | 17 (63) | |
| No | 591 (96) | 296 (50) | 295 (50) | |
| Cavities | .01 | |||
| Yes | 18 (3) | 14 (78) | 4 (22) | |
| No | 589 (97) | 286 (49) | 303 (51) | |
| Broken front tooth/teeth that need repair | .06 | |||
| Yes | 20 (3) | 14 (70) | 6 (30) | |
| No | 598 (97) | 292 (49) | 306 (51) | |
| Reported barrier of access to the dental care system | <.001 | |||
| Yes | 111 (11) | 67 (60) | 44 (40) | |
| No | 884 (89) | 318 (36) | 566 (64) |
Estimates among participants with nonmissing information in stratum.
Data are presented as n (column %).
Data are presented as n (row %).
Corresponding to χ2 tests for categorical variables and Student’s t tests for continuous variables.
Estimates excluding participants whose primary spoken language at home was not English.
Of the 387 children who had their first dental visit during the study, most entered via a comprehensive dental examination, with 52 (13%) entering with an emergency, problem-focused evaluation (Table 3). Although these results are based on small numbers, children whose caregivers reported their oral health as fair/poor were 70% more likely (24% vs 14%) to enter via an emergency visit versus children with better oral health status (Table 4). Similarly, emergency entry was more frequent among white subjects and American-Indian children (18% and 16% compared with 9% among African-American subjects). In a logistic regression model accounting for enrollment time, the OR of emergency entry for African-American children was 0.44 (95% CI: 0.22 to 0.87; P = .02) compared with white subjects. This estimate was somewhat attenuated (OR: 0.49 [95% CI: 0.24 to 1.00]; P = .05) when comprehension-based health literacy was included in the model.
TABLE 3.
Sociodemographic Correlates of Mode of Entry for Children Who Entered the Dental Care System Among the COHL Cohort of Child–Caregiver Dyads (n = 387)
| Characteristic | Mode of Entry in the Dental Care System | P | |
|---|---|---|---|
| Comprehensive Evaluation | Emergency Care | ||
| Total | 335 (87) | 52 (13) | |
| Race | |||
| White | 125 (82) | 27 (18) | .05 |
| African American | 150 (91) | 14 (9) | |
| American Indian | 59 (84) | 11 (16) | |
| Caregiver’s gender | |||
| Male | 14 (100) | 0 (0) | .1 |
| Female | 321 (86) | 52 (14) | |
| Caregiver’s age, y (tertiles; range) | .9 | ||
| Q1 (18.0–21.7) | 63 (89) | 8 (11) | |
| Q2 (21.7–25.0) | 79 (87) | 12 (13) | |
| Q3 (25.0–30.0) | 94 (85) | 17 (15) | |
| Q4 (30.0–63.9) | 99 (87) | 15 (13) | |
| Education | .8 | ||
| Did not finish high school | 80 (89) | 10 (11) | |
| High school diploma of GED | 124 (86) | 20 (14) | |
| Some college training or higher | 131 (86) | 22 (14) | |
| No. of children | .5 | ||
| 1 | 115 (89) | 14 (11) | |
| 2 | 131 (85) | 24 (15) | |
| 3 | 57 (89) | 7 (11) | |
| ≥4 | 32 (82) | 7 (18) | |
| Marital status | .9 | ||
| Single | 204 (86) | 32 (14) | |
| Married | 90 (87) | 14 (13) | |
| Divorced/separated/other | 41 (87) | 6 (13) | |
Data are presented as n (row %). GED, general equivalency diploma; Q, quartile.
TABLE 4.
Oral Health–Related Correlates of Type of Entry in the Dental Care System for Children Who Entered the Dental Care System (n = 387)
| Characteristic | Mode of Entry in the Dental Care System | P | |
|---|---|---|---|
| Comprehensive Evaluation | Emergency Care | ||
| Caregiver characteristics | |||
| Caregiver oral health | .2 | ||
| Excellent/very good/good | 221 (85) | 39 (15) | |
| Fair/poor | 112 (90) | 13 (10) | |
| Health literacy | |||
| Word recognition | .4 | ||
| Adequate (REALD-30 ≥13) | 252 (86) | 42 (14) | |
| Low (REALD-30 <13) | 83 (89) | 10 (11) | |
| Comprehension | .1 | ||
| Low (NVS: 0–1) | 54 (90) | 6 (10) | |
| Moderate (NVS: 2–3) | 138 (90) | 16 (10) | |
| Higher (NVS: 4–6) | 143 (83) | 30 (17) | |
| Dental neglect score (mean, 95% CI) | 11.7 (11.4 to 12.0) | 11.4 (10.4 to 12.4) | .6 |
| Child characteristics | |||
| Reported child oral health | .3 | ||
| Excellent/very good/good | 248 (86) | 42 (14) | |
| Fair/poor | 13 (76) | 4 (24) | |
| Reported child dental problems | |||
| Pain | .7 | ||
| Yes | 9 (90) | 1 (10) | |
| No | 251 (85) | 44 (15) | |
| Cavities | .9 | ||
| Yes | 12 (86) | 2 (14) | |
| No | 244 (85) | 42 (15) | |
| Broken front tooth/teeth that need repair | .4 | ||
| Yes | 13 (93) | 1 (7) | |
| No | 247 (85) | 45 (15) | |
| Reported barrier of access to the dental care system | .9 | ||
| Yes | 58 (87) | 9 (13) | |
| No | 275 (86) | 43 (14) | |
Data are presented as n (row %).
The final multivariate model for system entry (model 1) is presented in Table 5. Dental neglect was associated with significantly decreased predicted probability of entering the system: AME: –0.07 (95% CI: –0.11 to –0.03; P = .001) for each SD increase in DNS. Children’s age also remained strongly associated with entry. These results were virtually identical when only entry via comprehensive examination was considered (model 2). Children’s fair/poor oral health (compared with good/very good/excellent oral health) was also associated with increased likelihood of entry (AME: 0.22 [95% CI: 0.01 to 0.44]; P = .04); this estimate, however, was attenuated in analyses of comprehensive examination entry.
TABLE 5.
AMEs Estimated After Multivariate Logistic Regression Modeling of “Entering the Dental Care System” During the 25-Month Median Follow-up Period Among the Participating COHL Study Child–Caregiver Dyads (N = 1000)
| Characteristic | Model 1: Dental System Entry (Comprehensive Examination or Emergency Visit) | Model 2: Dental System Entry via Comprehensive Examination Only | ||||
|---|---|---|---|---|---|---|
| AME | 95% CI | P | AME | 95% CI | P | |
| Child oral health status | ||||||
| Excellent/very good/good | 0.00 | Ref | 0.00 | Ref | ||
| Fair/poor | 0.22 | 0.01 to 0.44 | .04 | 0.10 | −0.01 to 0.30 | .3 |
| Child’s age (years; ordinal categorical) | 0.09 | 0.05 to 0.13 | <.0005 | 0.08 | 0.04 to 0.12 | <.0005 |
| Caregiver’s age (years; quartiles) | 0.02 | −0.02 to 0.06 | .4 | 0.01 | −0.03 to 0.05 | .7 |
| Gender | ||||||
| Male | −0.09 | −0.28 to 0.10 | .3 | 0.00 | −0.20 to 0.19 | .9 |
| Female | 0.00 | Ref | 0.00 | Ref | ||
| Race | ||||||
| White | 0.00 | Ref | 0.00 | Ref | ||
| African American | 0.02 | −0.07 to 0.11 | .7 | 0.08 | −0.01 to 0.17 | .09 |
| American Indian | −0.02 | −0.12 to 0.09 | .8 | 0.01 | −0.09 to 0.12 | .8 |
| Education (ordinal categorical) | 0.01 | −0.05 to 0.06 | .8 | 0.01 | −0.05 to 0.06 | .7 |
| No. of children | ||||||
| 1 | 0.00 | Ref | 0.00 | Ref | ||
| 2 | 0.04 | −0.05 to 0.14 | .4 | −0.01 | −0.11 to 0.08 | .8 |
| 3 | −0.04 | −0.16 to 0.08 | .5 | −0.02 | −0.14 to 0.10 | .7 |
| ≥4 | −0.09 | −0.24 to 0.05 | .2 | −0.10 | −0.24 to 0.04 | .2 |
| Dental neglect (normalized DNS score)a | −0.07 | −0.11 to –0.03 | .001 | −0.05 | −0.09 to –0.01 | .01 |
| Reported barrier of access to the dental care system at enrollment interview | ||||||
| Yes | 0.10 | −0.02 to 0.21 | .1 | 0.08 | −0.03 to 0.19 | .2 |
| No | 0.00 | Ref | 0.00 | Ref | ||
| Health literacy (comprehension) | ||||||
| Low (NVS: 0–1) | 0.00 | Ref | 0.00 | Ref | ||
| Moderate (NVS: 2–3) | 0.00 | −0.12 to 0.11 | .9 | −0.02 | −0.13 to 0.10 | .8 |
| Higher (NVS: 4–6) | 0.05 | −0.07 to 0.18 | .4 | 0.01 | −0.11 to 0.13 | .9 |
Estimate corresponds to 1 SD increase in DNS score.
Discussion
This longitudinal investigation found that almost two-thirds of the young children enrolled in this population-based cohort did not enter the dental care system, whereas 13% of those who entered did so via an emergency visit. In addition to sociodemographic characteristics, caregivers’ dental neglect emerged as a significant predictor of not entering the system. Importantly, the first dental visit seemed to some degree to be problem driven; caregivers’ reports of children’s fair/poor oral health status or specific problems such as “cavities,” although infrequent, were predictive of subsequent entry to dental care. If children’s dental care services utilization is driven by perceived needs in this population, then the low amount of perceived disease at baseline could at least partially explain the low rate of entry into the system. These findings highlight suboptimal use of dental services by young children as a potential source of poor oral health outcomes and underscore the importance of caregivers’ perceptions, involvement, and engagement in their children’s oral health care.
The connection between caregivers’ and children’s oral health is well documented, but the pathways underlying this association have not been fully elucidated. Although environmental, cultural, family, and genetic factors are likely influential,11,12,39 timely and meaningful use of preventive oral health services may be critical. Mouradian et al2 found that 20% of children covered by Medicaid received preventive oral care for which they were eligible, and children from low-income and minority families were less likely to receive these services. Improving access to dental services for young children is a goal best achieved by engaging caregivers and families in a culturally, linguistically, and literacy-appropriate manner.20,40
Health literacy, although weakly associated with positive dental care–seeking patterns in this study, did not emerge as an important factor. Although more research is needed to clarify determinants such as specific skills and health literacy required for a child’s first preventive dental visit,20 it is possible that there are stronger influences, including caregivers’ perceptions and beliefs about oral health, and perceived barriers.41,42 Nevertheless, a caregiver-reported barrier of access to care was associated with subsequent increased likelihood of children’s dental care system entry; this at-first paradoxical finding is most likely a reflection of caregivers actively seeing care at the baseline interview and eventually obtaining it during the study period. The absence of an association between reported “pain” and entry is another area that warrants further investigation. In our study, this group included a very small number of children, whereas reported pain was of unknown etiology and subject to reporting and misclassification biases.
Caregivers’ dental neglect, which emerged as an important factor in this study, may entail dimensions of both neglect and avoidance of care.43 In planning of possible interventions to improve young children’s oral health, dental neglect may thus be considered as a caregiver-level risk factor. However, dental neglect may be a proxy for education, knowledge, self-efficacy, or other distal and social determinants that may or may not be modifiable. For this reason, distal, community-based interventions that use school- or family-based strategies or health promoters and circumvent “proximal” caregiver- and family-level barriers to care may be more promising compared with patient-level strategies.11
Our findings should be viewed acknowledging the study’s limitations. First, we observed a small number of emergency visits during follow-up. The sample’s characteristics, including predominantly female, low-income caregivers who were clients of WIC in 7 counties in North Carolina, limit the generalizability of our findings. In this study, we did not consider oral health screenings and preventive services delivered in medical offices as entry into the dental care system. Physicians and WIC workers in North Carolina are engaged in children’s oral health advocacy, including screenings and dental referrals; however, in this study, we did not distinguish between children who were referred and followed up on the referral versus those whose parents took the initiative to have a dental visit. We studied caregivers’ decisions and actions relative to their children’s entry into the dental care system, without an examination of whether these decisions/actions were clinically justified (ie, a scenario of an emergency visit due to teething symptoms). Finally, it was not possible to capture participants’ possible dental care– seeking behavior outside the Medicaid network, an issue of possible relevance to children whose Medicaid coverage is interrupted due to eligibility/administrative issues.44
This study’s strengths include its prospective design and the use of a nonclinical community-based cohort of caregivers and children. It also is strengthened by reliance on Medicaid claims to ascertain the incidence and type of dental visits. This approach offers a prospective insight into the influence of caregiver characteristics and may circumvent potential social desirability bias45 in caregivers’ reports.
The study’s findings illustrate a complex problem while illuminating potential targets for interventions. To facilitate early preventive dental visits for preschool-aged children enrolled in Medicaid, Askelson et al46 described the introduction of a research framework among caregivers. In a recent study, Chi et al47 highlighted the close association between well-child visits and first dental examinations among young Medicaid-eligible children, emphasizing the public health potential for using this avenue to improve children’s oral health. Emerging cost-effectiveness data provide additional support for interdisciplinary collaborations of dentistry with family medicine and pediatrics for screening and possible referral of children at high risk.48 Other promising strategies may include community-based interventions,49,50 continuing support on programs such as WIC51 and Early Head Start,52 and increased emphasis on adherence to professional recommendations for establishing a dental home by 1 year of age.
Conclusions
Caregivers’ dental neglect was significantly associated with their children not entering the dental care system over a median 25-month follow-up period, whereas entry seemed to be mostly problem driven. As the “quarterbacks” of their children’s health care, caregivers must be placed in the epicenter of efforts to promote optimal oral health behaviors, including early preventive dental visits.
Acknowledgment
The authors thank all participants of the COHL study.
Glossary
- AME
average marginal effect
- CI
confidence interval
- COHL
Carolina Oral Health Literacy
- DNS
Dental Neglect Scale
- NVS
Newest Vital Sign
- OR
odds ratio
- REALD-30
Rapid Estimate of Adult Literacy in Dentistry–30
- WIC
Supplemental Nutrition Program for Women, Infants, and Children
Footnotes
Dr Divaris performed statistical analyses and drafted the initial manuscript; Dr Lee conceptualized and designed the study, supervised the study conduct, assisted with data analysis, and critically revised the initial manuscript; Ms Baker conducted primary data collection, assisted with interpretation of results, and critically revised the initial draft of the manuscript; Dr Gizlice conducted data management and analyses, and critically revised the initial manuscript; Dr Rozier participated in the study conceptualization and design, assisted with interpretation of results, and critically revised the initial manuscript; Dr DeWalt assisted with interpretation of results and critically revised the initial manuscript; Dr Vann conceptualized and designed the study, participated in interpretation of results, and co-wrote the initial draft of the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The Carolina Oral Health Literacy (COHL) study is supported by a grant from the National Institute of Dental and Craniofacial Research (R01DE018045). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Tomar SL, Reeves AF. Changes in the oral health of US children and adolescents and dental public health infrastructure since the release of the Healthy People 2010 Objectives. Acad Pediatr. 2009;9(6):388–395 [DOI] [PubMed] [Google Scholar]
- 2.Mouradian WE, Wehr E, Crall JJ. Disparities in children’s oral health and access to dental care. JAMA. 2000;284(20):2625–2631 [DOI] [PubMed] [Google Scholar]
- 3.Dye BA, Li X, Thornton-Evans G. Oral Health Disparities as Determined by Selected Healthy People 2020 Oral Health Objectives for the United States, 2009–2010. NCHS Data Brief, No. 104. Hyattsville, MD: National Center for Health Statistics; 2012 [PubMed] [Google Scholar]
- 4.Benjamin RM. Oral health: the silent epidemic. Public Health Rep. 2010;125(2):158–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casamassimo PS, Thikkurissy S, Edelstein BL, Maiorini E. Beyond the dmft: the human and economic cost of early childhood caries. J Am Dent Assoc. 2009;140(6):650–657 [DOI] [PubMed] [Google Scholar]
- 6.American Academy on Pediatric Dentistry. American Academy of Pediatrics . Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. Pediatr Dent. 2008–2009;30(suppl 7):40–43 [PubMed] [Google Scholar]
- 7.Lee JY, Bouwens TJ, Savage MF, Vann WF, Jr. Examining the cost-effectiveness of early dental visits. Pediatr Dent. 2006;28(2):102–105, discussion 192–198 [PubMed] [Google Scholar]
- 8.Bhaskar V, McGraw KA, Divaris K. The importance of preventive dental visits from a young age: systematic review and current perspectives. Clin Cosmet Investig Dent. 2014, In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis CW, Johnston BD, Linsenmeyar KA, Williams A, Mouradian W. Preventive dental care for children in the United States: a national perspective. Pediatrics. 2007;119(3). Available at: www.pediatrics.org/cgi/content/full/119/3/e544 [DOI] [PubMed] [Google Scholar]
- 10.Section on Pediatric Dentistry and Oral Health . Preventive oral health intervention for pediatricians. Pediatrics. 2008;122(6):1387–1394 [DOI] [PubMed] [Google Scholar]
- 11.Lee JY, Divaris K. The ethical imperative of addressing oral health disparities: a unifying framework. J Dent Res. 2014;93(3):224–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher-Owens SA, Gansky SA, Platt LJ, et al. Influences on children’s oral health: a conceptual model. Pediatrics. 2007;120(3). Available at: www.pediatrics.org/cgi/content/full/120/3/e510 [DOI] [PubMed] [Google Scholar]
- 13.Edelstein BL. Dental care considerations for young children. Spec Care Dentist. 2002;22(suppl 3):11S–25S [PubMed] [Google Scholar]
- 14.Allukian M, Jr. The neglected epidemic and the surgeon general’s report: a call to action for better oral health. Am J Public Health. 2000;90(6):843–845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vann WF, Jr, Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: impact on oral health outcomes in early childhood. J Dent Res. 2010;89(12):1395–1400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewis C, Mouradian W, Slayton R, Williams A. Dental insurance and its impact on preventive dental care visits for U.S. children. J Am Dent Assoc. 2007;138(3):369–380 [DOI] [PubMed] [Google Scholar]
- 17.Yu SM, Bellamy HA, Kogan MD, Dunbar JL, Schwalberg RH, Schuster MA. Factors that influence receipt of recommended preventive pediatric health and dental care. Pediatrics. 2002;110(6). Available at: www.pediatrics.org/cgi/content/full/110/6/e73 [DOI] [PubMed] [Google Scholar]
- 18.Divaris K, Vann WF, Jr, Baker AD, Lee JY. Examining the accuracy of caregivers’ assessments of young children’s oral health status. J Am Dent Assoc. 2012;143(11):1237–1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graham DB, Webb MD, Seale NS. Pediatric emergency room visits for nontraumatic dental disease. Pediatr Dent. 2000;22(2):134–140 [PubMed] [Google Scholar]
- 20.Kelly SE, Binkley CJ, Neace WP, Gale BS. Barriers to care-seeking for children’s oral health among low-income caregivers. Am J Public Health. 2005;95(8):1345–1351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parker RM, Hernandez LM. Oral health literacy: a workshop. J Health Commun. 2012;17(10):1232–1234 [DOI] [PubMed] [Google Scholar]
- 22.Miller E, Lee JY, DeWalt DA, Vann WF, Jr. Impact of caregiver literacy on children’s oral health outcomes. Pediatrics. 2010;126(1):107–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horowitz AM, Kleinman DV. Oral health literacy: the new imperative to better oral health. Dent Clin North Am. 2008;52(2):333–344, vi [DOI] [PubMed] [Google Scholar]
- 24.Weintraub JA, Prakash P, Shain SG, Laccabue M, Gansky SA. Mothers’ caries increases odds of children’s caries. J Dent Res. 2010;89(9):954–958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muirhead V, Levine A, Nicolau B, Landry A, Bedos C. Life course experiences and lay diagnosis explain low-income parents’ child dental decisions: a qualitative study [published online ahead of print August 30, 2012]. Community Dent Oral Epidemiol. 10.1111/j.1600-0528.2012.00741.x. [DOI] [PubMed] [Google Scholar]
- 26.Lee JY, Divaris K, Baker AD, Rozier RG, Lee SY, Vann WF, Jr. Oral health literacy levels among a low-income WIC population. J Public Health Dent. 2011;71(2):152–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richman JA, Lee JY, Rozier RG, Gong DA, Pahel BT, Vann WF, Jr. Evaluation of a word recognition instrument to test health literacy in dentistry: the REALD-99. J Public Health Dent. 2007;67(2):99–104 [DOI] [PubMed] [Google Scholar]
- 28.Lee JY, Rozier RG, Lee SY, Bender D, Ruiz RE. Development of a word recognition instrument to test health literacy in dentistry: the REALD-30—a brief communication. J Public Health Dent. 2007;67(2):94–98 [DOI] [PubMed] [Google Scholar]
- 29.Lee JY, Divaris K, Baker AD, Rozier RG, Vann WF, Jr. The relationship of oral health literacy and self-efficacy with oral health status and dental neglect. Am J Public Health. 2012;102(5):923–929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Divaris K, Lee JY, Baker AD, Vann WF, Jr. Caregivers’ oral health literacy and their young children’s oral health-related quality-of-life. Acta Odontol Scand. 2012;70(5):390–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hom JM, Lee JY, Divaris K, Baker AD, Vann WF, Jr. Oral health literacy and knowledge among patients who are pregnant for the first time. J Am Dent Assoc. 2012;143(9):972–980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vann WF, Jr, Divaris K, Gizlice Z, Baker AD, Lee JY. Caregivers’ health literacy and their young children’s oral-health-related expenditures. J Dent Res. 2013;92(suppl 7):55S–62S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Osborn CY, Weiss BD, Davis TC, et al. Measuring adult literacy in health care: performance of the newest vital sign. Am J Health Behav. 2007;31(suppl 1):S36–S46 [DOI] [PubMed] [Google Scholar]
- 35.Jamieson LM, Thomson M. Dental health, dental neglect, and use of services in an adult Dunedin population sample. N Z Dent J. 2002;98(431):4–8 [PubMed] [Google Scholar]
- 36.Jamieson LM, Thomson WM. The dental neglect and dental indifference scales compared. Community Dent Oral Epidemiol. 2002;30(3):168–175 [DOI] [PubMed] [Google Scholar]
- 37.Mood C. Logistic regression: why we cannot do what we think we can do, and what we can do about it. Eur Sociol Rev. 2010;26(1):67–82 [Google Scholar]
- 38.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12(2):308–331 [Google Scholar]
- 39.Mouradian WE, Huebner CE, Ramos-Gomez F, Slavkin HC. Beyond access: the role of family and community in children’s oral health. J Dent Educ. 2007;71(5):619–631 [PubMed] [Google Scholar]
- 40.Patrick DL, Lee RS, Nucci M, Grembowski D, Jolles CZ, Milgrom P. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;6(suppl 1):S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Amin MS, Harrison RL. Understanding parents’ oral health behaviors for their young children. Qual Health Res. 2009;19(1):116–127 [DOI] [PubMed] [Google Scholar]
- 42.Isong IA, Luff D, Perrin JM, Winickoff JP, Ng MW. Parental perspectives of early childhood caries. Clin Pediatr (Phila). 2012;51(1):77–85 [DOI] [PubMed] [Google Scholar]
- 43.Thomson WM, Spencer AJ, Gaughwin A. Testing a child dental neglect scale in South Australia. Community Dent Oral Epidemiol. 1996;24(5):351–356 [DOI] [PubMed] [Google Scholar]
- 44.Federico SG, Steiner JF, Beaty B, Crane L, Kempe A. Disruptions in insurance coverage: patterns and relationship to health care access, unmet need, and utilization before enrollment in the State Children’s Health Insurance Program. Pediatrics. 2007;120(4). Available at: www.pediatrics.org/cgi/content/full/120/4/e1009 [DOI] [PubMed] [Google Scholar]
- 45.Sanzone LA, Lee JY, Divaris K, DeWalt DA, Baker AD, Vann WF, Jr. A cross sectional study examining social desirability bias in caregiver reporting of children’s oral health behaviors. BMC Oral Health. 2013;13(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Askelson NM, Chi DL, Momany E, et al. Encouraging early preventive dental visits for preschool-aged children enrolled in Medicaid: using the Extended Parallel Process Model to conduct formative research [published online ahead of print September 21, 2012] . J Public Health Dent. 10.1111/j.1752-7325.2012.00369.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chi DL, Momany ET, Jones MP, et al. Relationship between medical well baby visits and first dental examinations for young children in Medicaid. Am J Public Health. 2013;103(2):347–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Beil H, Rozier RG, Preisser JS, Stearns SC, Lee JY. Effect of early preventive dental visits on subsequent dental treatment and expenditures. Med Care. 2012;50(9):749–756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Petersen PE, Kwan S. Evaluation of community-based oral health promotion and oral disease prevention—WHO recommendations for improved evidence in public health practice. Community Dent Health. 2004;21(suppl 4):319–329 [PubMed] [Google Scholar]
- 50.Weintraub JA. Prevention of early childhood caries: a public health perspective. Community Dent Oral Epidemiol. 1998;26(suppl 1):62–66 [DOI] [PubMed] [Google Scholar]
- 51.Lee JY, Rozier RG, Norton EC, Kotch JB, Vann WF, Jr. Effects of WIC participation on children’s use of oral health services. Am J Public Health. 2004;94(5):772–777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kranz AM, Rozier RG, Zeldin LP, Preisser JS. Oral health activities of Early Head Start teachers directed toward children and parents. J Public Health Dent. 2011;71(2):161–169 [DOI] [PMC free article] [PubMed] [Google Scholar]