Abstract
BACKGROUND AND OBJECTIVES:
In 2010, the Bioethics Committee of the American Academy of Pediatrics issued recommendations that pediatric hematopoietic stem cell donors should have an independent advocate. Formulating appropriate guidelines is hindered by the lack of prospective empirical evidence from families about the experience of siblings during typing and donation. Our aim was to provide these data.
METHODS:
Families with a child scheduled to undergo hematopoietic stem cell transplant were recruited. All family members, including children aged 9 to 22 years, were eligible. Qualitative interviews were conducted within 3 time periods: pretransplant, 6 to 8, and 9 to 11 months posttransplant. Quantitative scales assessing decision satisfaction and regret were administered at time 2.
RESULTS:
Thirty-three families were interviewed. Of the 119 family members, 76% perceived there was no choice in the decision to HLA-type siblings; 77% perceived no choice in sibling donation; 86% had no concerns about typing other than needle sticks; and 64% had no concerns about donation. Common concerns raised were dislike of needle sticks (19%), stress before typing results (14%), and fear of donation (15%). Posttransplantation, 33% of donors wished they had been given more information; 56% of donors stated they benefited from donation. Only 1 donor expressed regret posttransplant.
CONCLUSIONS:
Most family members did not view sibling typing and donation as a choice, were positive about the experience, and did not express regrets. We recommend education for all siblings before typing, comprehensive education for the donor by a health care provider pretransplant, and systematic donor follow-up after transplantation.
Keywords: hematopoietic stem cell transplant, sibling donors, ethics, guidelines, donor advocates
What’s Known on This Subject:
The American Academy of Pediatrics has recommended that sibling donors should have an independent advocate. Defining the need for and role of this advocate is hampered by a lack of empirical data.
What This Study Adds:
This study provides prospective family data regarding siblings’ experiences during HLA typing and donation pre- and posttransplantation. Most family members, including the siblings, perceive no choice in typing or donation, yet have few concerns and report positive aspects to participating.
In 2010, the Bioethics Committee of the American Academy of Pediatrics (AAP) recommended that each pediatric hematopoietic stem cell (HSC) donor have an independent advocate appointed before HLA typing who has the power, in consultation with health care professionals and ethics committees, to deny or delay the typing.1 Objections to this include the following: (1) requiring an independent advocate shows disrespect for parental rights; (2) there is no documented need; (3) independence and appointment before HLA typing are impractical; and (4) denying or delaying typing poses a threat to the stem cell recipient.2–4 The lead author (L.F.R.) replied that these objections mischaracterize the role of the advocate, who should be considered an “ally” of the donor and family.5,6
One barrier to determining appropriate stringency for a donor protection policy is the relative lack of empirical data regarding the experience of families and specifically siblings who are typed and/or serve as donors.7,8 Most studies have relied on cross-sectional, retrospective interviews years after donation,9–12 with few exceptions.13–15 Across these studies, both positive and negative psychosocial consequences of typing and donation are reported, including sibling donors’ lack of choice, lack of appropriate information, and need for greater support.7–13
The purpose of this study was to prospectively document (pretransplant through 9 to 11 months posttransplant) all family members’ views regarding choice, concerns/regrets, and benefit of sibling HLA typing and HSC donation.
Methods
Families with a child scheduled to undergo HSC transplantation (HSCT) at 1 of 4 geographically diverse sites (Atlanta, Georgia; Philadelphia, Pennsylvania; Kansas City, Missouri; Calgary, Canada) were eligible for participation. All family members identified by the parents, including step-parents, grandparents, and any children, including half-siblings and cousins aged 9 to 22 years, were eligible. Two institutions had donor programs; at one an independent pediatrician provided donor medical clearance and at the other, members of the transplant department, including a clinical psychologist, a social worker, and a physician, met with the donor. Interviews were conducted between 2007 and 2010 before the AAP recommendations were issued. The study was approved by research review boards at each site.
Mixed methods were used. After securing consent and assent, interviews were conducted with all available family members at 3 time points, pretransplant (T1), and 6 to 8 months (T2) and 9 to 11 months (T3) posttransplant, at their home or a private place of their choosing. We report here on a secondary analysis of the interviews with a specific focus on responses regarding child choice, concern/regret and benefit of HLA typing, and HSC donation. Two quantitative scales focusing on the donor decision were completed at T2, the Satisfaction with Decision Scale,16 completed by caregivers, and the Decision Regret Scale,17 completed by all family members. The Satisfaction with Decision Scale is a 6-item self-report scale with a 5-point Likert scale response format; lower summed scores indicate greater satisfaction. The Decision Regret Scale is a 5-item self-report scale also with a 5-point Likert scale; lower summed scores indicate less regret.
Data Analysis
All interviews were audio-recorded, transcribed verbatim, redacted for errors, and content coded inductively by investigators at each site and reviewed independently (by RP and PH) for consistency in the application of codes. For this secondary analysis, 2 investigators (RP, KH) reviewed each coded interview to extract data about child choice for typing and donation (T1) and perceived benefits and concerns of typing (T1) and donation (T1, T2, T3). All data were tallied by family role. The median and interquartile range are reported by family member role for the scores on the Decision Regret and Decision Satisfaction Scales.
Results
Participants
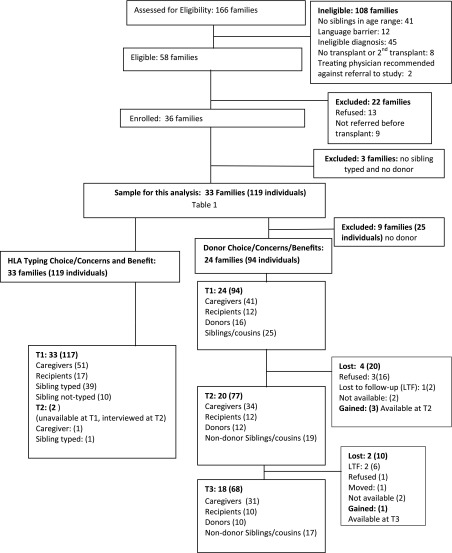
Forty-nine eligible families were offered the study; 13 (27%) refused, and 119 members of 33 families comprised the sample for this analysis. Patients in enrolled families were younger than those in families that refused (mean age 11.0 vs 13.9, P = .016). No other significant differences were found. Figure 1 presents a CONSORT diagram for the overall study. Table 1 describes the demographics.
FIGURE 1.
Explanation of sample for analysis. LTF, lost to follow-up. aIndividuals noted in parentheses.
TABLE 1.
Demographics for the 33 Families Who Had a Sibling Tested
| Demographics | Caregivers | Recipients | Donors | Siblings/Half-siblings/Cousins | Total |
|---|---|---|---|---|---|
| Total | 52 | 17 | 16 | 34 | 119 |
| Gender | |||||
| Male | 25 | 9 | 10 | 17 | 60 |
| Female | 27 | 8 | 6 | 17 | 59 |
| Race/ethnicity | |||||
| White | 31 | 9 | 10 | 10 | 60 |
| African American | 16 | 6 | 5 | 19 | 46 |
| Hispanic | 3 | 1 | 1 | 2 | 7 |
| White/Hispanic | 0 | 1 | 0 | 3 | 4 |
| Asian | 2 | 0 | 0 | 0 | 2 |
| Age range/mean | |||||
| Age range | 29–64 | 10–18 | 9–18 | 9–22 | 11–15 |
| Mean | 40.3 | 14.5 | 13.4 | 14.6 | 13 |
| Caregivers’ education | |||||
| ≥College degree | 21 | ||||
| <College degree | 28 | ||||
| Missing | 3 | ||||
| Family income | |||||
| ≥$60 000 | 13 | ||||
| <$60 000 | 15 | ||||
| Missing/refusal | 3/1 | ||||
| Families by site | Malignant | Nonmalignant | |||
| Emory | 14 | 4 | |||
| CHOP | 7 | 0 | |||
| Alberta | 4 | 1 | |||
| Kansas City | 2 | 1 | |||
CHOP, Children’s Hospital of Philadelphia.
HLA Typing
Concerns
At T1, most individuals (102 [86%]) across 3 (100%) families expressed no concerns about having siblings typed other than dislike of needle sticks. Twenty-three (19%) individuals (11 [21%] caregivers, 10 [25%] typed siblings, 1 [10%] not-typed sibling and 1 [6%] recipient) across 12 (36%) families reported that they or another child disliked needle sticks. Seventeen (14%) individuals (6 [12%] caregivers, 10 [25%] typed siblings, 1 [10%] not-typed sibling) across 11 (33%) families stated that the waiting period between typing and the return of results was stressful, with 1 typed sibling having nightmares. Of these, 8 (7%) individuals (2 [4%] caregivers, 5 [13%] typed siblings, and 1 [10%] not-typed sibling) from 6 (18%) families reported that they or another child were worried that they might be a match and hoped it would be someone else.
Two additional children expressed notable concerns. One donor sibling found the whole typing process stressful. This 12-year-old stated he was not informed before typing that he would have his blood drawn nor why. A 17-year-old was opposed to her brother being typed because of his cognitive deficits for fear that, if he were the donor, he would blame himself if his brother died.
Benefits
Thirty-eight (32%) individuals across 19 (58%) families mentioned some benefit received from typing, including a role in helping the ill child get better (23 [19%] individuals across 14 [42%] families) and/or the hope that he or she could be a donor (16 [13%] individuals across 7 [21%] families). One half-sibling convinced the health care team to type her because she thought it unfair that only full siblings had a chance to help.
Choice
Pretransplant, 68 (76%) individuals across 29 (88%) families reported that siblings had no choice in whether to be HLA typed (Table 2). Sibling choice was not discussed for the remaining 4 families (30 individuals). The perception of no sibling choice was universal among members of 17 (59%) of 29 families. There were no families in which all of the interviewed members stated that siblings had a choice. In 3 (10%) families, at least 1 caregiver stated that siblings had a choice, but at least 1 sibling stated he or she did not. All siblings were willing to be HLA typed. As one 14-year-old donor said, “We just walked into the hospital one day and mom said, ‘well, [recipient’s name] needs a bone marrow transplant, so, we’re all gonna get tested’……. if we really didn’t want to, I’m sure she wouldn’t have made us, but, there was not any part of me that didn’t want to do it.”
TABLE 2.
Did the Sibling Have a Choice About Whether to Be HLA Typed?
| Role in Family, n = Asked Whether Sibling Had a Choice About Typing | No, n (% Asked) | Yes, n (% Asked) | Do Not Know, n (% Asked) |
|---|---|---|---|
| Caregiver: n = 40/52 (77%) | 31 (78) | 6 (15) | 3 (8) |
| Recipient: n = 7/17 (76%) | 6 (86) | 0 | 1 (14) |
| Sibling typed: n = 33/40 (83%) | 24 (73) | 8 (24) | 1 (3) |
| Sibling not-typed: n = 9/10(90%) | 6 (67) | 1 (11) | 2 (22) |
| Total: n = 89/119 (75%) | 68 (76) | 14 (16) | 7 (7) |
Donation
Concerns
Pretransplant, 22 (23%) individuals across 14 (58%) families expressed concerns for the donor. Fourteen (15%) individuals (4 [10%] caregivers, 2 [13%] donors, 5 [20%] nondonor siblings/cousins, and 3 [25%] recipients) across 7 (29%) families stated that the donor was frightened before donation. Three (19%) donors worried that the transplant would not be effective and their cells would be rejected; none seemed to see this as being their fault. In 2 of these cases, the recipient did well. The third recipient relapsed, but her 15-year-old donor did not express feelings of guilt or regret at T2 or T3. Five (5%) individuals (3 [7%] mothers, 1 [6%] donor, and 1 [4%] half-sibling) across 4 (17%) families reported other concerns. The concern of the sibling for her cognitively delayed brother also encompassed donation. Three mothers were concerned about risks to the donor, such as pain. The donor described previously who was not informed before typing was also not informed about the number of needle sticks or the side effects of granulocyte colony-stimulating factor, which were significant for him. Mostly, he felt unappreciated: “[The recipient] is just the main attraction. I wasn’t really noticed unless I was doing something that was like towards the transplant, like getting a needle injection or a blood-taking needle.” Both of his parents were concerned by his level of pain and the mother wondered if they should have searched for an unrelated donor.
Posttransplant, 12 (16%) individuals across 9 (45%) families expressed concerns for the donor. Six (8%) individuals (4 [33%] donors, 2 [11%] nondonor siblings) from 5 (25%) families reported that the procedure was somewhat painful, but they were not upset or regretful. Five (6%) individuals (4 [33%] donors and 1 [3%] mother) wished they had been better informed before donation about certain aspects of the process, such as side effects of medications and details of hospital procedure. One of the donors was wistful that the family had not planned something special for him. Three (4%) individuals (2 [6%] parents and 1 [8%] donor) from 1 (5%) family expressed a serious concern posttransplant. A 9-year-old donor was the only donor who reported that she regretted the donation. The donation was painful and “I was upset because I was wondering where mommy was, she did not come home because of the transplant.” She also reported that she believed her mother was the better match.
In all, 60 (64%) individuals from 9 (38%) families expressed no concern pre- or posttransplant. Of note, 2 patients died and their families refused the second interview, so we could not gauge regret in these families.
Benefits
Thirty-eight (40%) individuals across 21 (88%) families reported that the donor benefited from the donation. The benefit was variously expressed as feeling good about having a part in trying to save the ill child’s life; helping the ill child feel better; creating a new closeness with the ill child; helping the family return to normal; making others proud; and becoming a better person. One 14-year-old donor stated, “I just wanted to be a part of him getting through this big important disease.” Another 10-year-old donor explained, “It makes me feel better to do that for my sister…. then the whole family could be together and its fun, well, not fun, but, you are the one that’s doing it, bringing the family back together. It’s a good feeling inside.”
Choice
Seventy-seven (80%) individuals from 24 (100%) families were asked if there was a choice about donation. Of these, 59 (77%) individuals from 23 (96%) families perceived that there was no choice regarding donation for the matched sibling (Table 3). The perception of no sibling choice about donation was universal across 14 (58%) families. In the only 2 families (8%) headed by grandparents, all interviewed members stated that siblings had a choice. In another 2 (8%) families, 1 or both parents reported that there was a choice about donation, but the donor reported that there was no choice. One donor stated, “It was just something that had to be done.” The other was ambivalent about whether he had a choice. He first stated that his mother had offered him a choice, “But, I decided just to do it for my sister.” Later in the interview he commented, “They want me to have free choice, but, I still sort of feel like I was made to do this.” This is the same 12-year-old donor who reported that the whole process was stressful.
TABLE 3.
Did the Sibling Donor Have a Choice About Whether to Donate?
| Role in Family, n = Asked Whether Donor Had a Choice About Donation | No, n (% Asked) | Yes, n (% Asked) | Do Not Know, n (% Asked) |
|---|---|---|---|
| Parent: n = 37/39a (95%) | 32 (80) | 5 (13) | 0 |
| Grandparent: n = 3/3(100%) | 0 | 3 (100) | 0 |
| Recipient: n = 7/12 (58%) | 5 (71) | 2 (29) | 0 |
| Donor: n = 12/16 (75%) | 11 (92) | 1 (8) | 0 |
| Non-donor sibling: n = 10/15a (67%) | 8 (80) | 2 (20) | 0 |
| Half-sibling: n = 5/6 (83%) | 3 (60) | 1 (20) | 1 (20) |
| Cousin: n = 3/5 (60%) | 0 | 0 | 3 (100) |
| Total: 77/96a (80%) | 59 (77) | 14 (18) | 4 (5) |
One parent and 1 nondonor sibling were asked at T2 because they were unavailable at T1.
Only 1 family reported any donor hesitation. A father explained that his 20-year-old son hesitated because he feared donation would impact his career, but agreed when he learned the time commitment was minimal.
Quantitative Scales
Median scores on the Decision Regret scale were low across all family members, indicating no to low regret about the donor decision. Similarly, low median scores on the Decision Satisfaction scale indicate moderately high to high caregiver satisfaction with the donor decision (Table 4).
TABLE 4.
Regret and Satisfaction With the Decision to Use a Sibling as the Donor
| Role | Decision Regreta | Decision Satisfactionb | ||||
|---|---|---|---|---|---|---|
| n | Median | IQR | n | Median | IQR | |
| Parent | 30 | 1.0 | 1.0–1.2 | 30 | 1.0 | 1.0–1.2 |
| Recipient | 11 | 1.0 | 1.0–1.8 | —c | —c | —c |
| Donor | 12 | 1.1 | 1.0–1.7 | —c | —c | —c |
| Sibling and cousin | 17 | 1.1 | 1.0–1.7 | —c | —c | —c |
| Grandparent | 3 | 2.0 | 3 | 2.0 | ||
IQR, interquartile range (25th–27th percentile) reported for n > 5.
1, no regret; 5 high regret.
1, high satisfaction; 5, low satisfaction.
Scale not administered.
Discussion
Most of the 119 family members within 33 families reported no concerns with HLA typing or HSC donation (86%, 64%, respectively) in this year-long, prospective study. The reported HLA typing concerns (fear of needle sticks, stress, worry and nightmares about donation) might have been alleviated if transplant centers routinely explained the process of typing and donation to all typed children. Such education could be performed by an “advocate” or other health care professional. This educational role, however, is distinct from a potential advocate role of screening children pre-HLA typing to determine if they are appropriate candidates for typing. Screening before typing is needed only when it is questionable whether the child, even if a match, should be the donor.18,19 This is likely to be a rare circumstance. A careful analysis of the 2 concerned donors in our study did not lead us to believe that these children should not have been donors. Rather, these children likely would have benefited from support and counseling throughout the transplant period. We cannot be certain that all cases in which a child should not be a donor will be easily identifiable before typing. We recommend, therefore, that the transplant team be alert to family circumstances, such as abuse or no relationship with the recipient, which may require further dialogue before systematically typing all siblings. However, instituting a formal screening process before HLA typing for the rare exception seems unnecessary.
The most frequent concerns about donation were fearfulness before donation (23%), pain during donation (8%), and desire for more information (6%) after donation. These data suggest that donors (and other family members) may need better access to more complete and frank information about donation and hospital procedures. We did identify an area of need: systematic posttransplant donor follow-up and education. A number of concerns were mentioned posttransplant that could be addressed through psychosocial support.11
Should the professionals performing the medical clearance and providing support and education to children be independent of the patient’s transplant team? Our data do not answer this question. One of the 2 concerned donors was screened by an independent pediatrician and the other had a psychosocial assessment, although not necessarily independent, before donation. Most of the donors in our study had no independent medical or psychosocial screening and no concerns.
Most family members stated that siblings had no choice about typing or donation (76%, 77%, respectively); only 1 donor reported he had a choice, confirming previous findings that no choice is involved in sibling donation.10,11 But our data also document that the lack of choice was not a concern for either parents or children. Lack of choice, whether a concern or not, may imply the need for an advocate to help the family understand the medical options, but this information may be most effective coming from the treating physician.20 From the donor perspective, “no choice” becomes concerning in the case of “forced no choice.”11 One 9-year-old donor did regret donation, but her expressed concerns were absence of her mother and believing that she was not the best HLA match, not lack of choice. She was asked and did assent to donation. Support and education of this donor may have helped, but expressions of lack of choice did not seem to indicate the need for an advocate to explain that there was a choice.
One of the more contentious AAP recommendations is that the advocate have the power to prevent donation. As noted previously, we found no evidence that the 2 concerned donors should not have donated. For these 33 families, this power was not needed.
An important theme in our findings was benefit to the donor in the form of having a role to play and being included in the family fight against the ill child’s disease. Even being able to be HLA-typed made some children feel that they had a role. Our findings from both the interviews and quantitative scales can be used by clinicians to advise families before transplantation that the great majority of siblings and parents did not regret typing and donation and even found it beneficial.
Several limitations should be noted: the infrequent expression of concern could result from it being unacceptable in the child’s eyes to voice a concern during this difficult time. However, our use of both private interview and quantitative methods and our repeated contact with the family members over a year lessens the likelihood of family members not disclosing their concerns to us. In addition, 13 (27%) of 49 families approached declined participation. Although our findings do not represent all transplant families with a child undergoing HSCT, the similarity of our findings across 4 geographically distinct settings helps to support their validity. Finally, because our study preceded the AAP recommendations, we cannot provide data on whether an independent advocate with veto power is necessary before typing, although these 33 families did not appear to need one. The most important lack was education and psychosocial support.
Conclusions
Our longitudinal study of 119 family members of pediatric HSCT patients showed that most were positive about the opportunity to donate and did not express concerns. Our study identified several needed improvements to the typing and donation process: education for all siblings before typing, enhanced education of the donor and family members, and psychosocial follow-up with the donor posttransplant to assess and ameliorate concerns. An advocate or other mechanism could accomplish these tasks.
Glossary
- AAP
American Academy of Pediatrics
- HSC
hematopoietic stem cell
- HSCT
hematopoietic stem cell transplantation
- T1
T2, T3, time 1, time 2, time 3
Footnotes
Dr Pentz conceptualized and designed the study, acquired the data, analyzed the data, and drafted the initial manuscript and revised it; Dr Alderfer, Ms Pelletier, and Ms Stegenga conceptualized and designed the study, acquired the data, and reviewed and revised the manuscript; Dr Haight designed the study, acquired and interpreted data, and reviewed and revised the manuscript; Mr Hendershot analyzed and interpreted the data, and reviewed and revised the manuscript; Ms Dixon designed the study, acquired data, coordinated the data collection at 4 sites, analyzed the data, and reviewed and revised the manuscript; Dr Fairclough conceptualized and designed the study, analyzed the data, and reviewed and revised the manuscript; Dr Hinds conceptualized and designed the study and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: All phases of this study were supported by National Institutes of Health grant, 1R21CA131875–01A1. Ms Stegenga’s contribution was supported by an Oncology Nursing Society Research Foundation Fellowship. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found on page e1356, online at www.pediatrics.org/cgi/doi/10.1542/peds.2014-0375.
References
- 1.American Academy of Pediatrics. Committee on Bioethics . Children as hematopoietic stem cell donors. Pediatrics. 2010;125(2):392–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Revera GH, Frangoul H. A parent’s point of view on the American Academy of Pediatrics policy statement: children as hematopoietic stem cell donors. Pediatr Blood Cancer. 2011;56(4):515–516 [DOI] [PubMed] [Google Scholar]
- 3.Joffe S, Kodish E. Protecting the rights and interests of pediatric stem cell donors. Pediatr Blood Cancer. 2011;56(4):517–519 [DOI] [PubMed] [Google Scholar]
- 4.Wells RJ. The American Academy of Pediatrics policy statement—children as hematopoietic stem cell donors. Pediatr Blood Cancer. 2011;57(6):1086–1087, author reply 1088–1089 [DOI] [PubMed] [Google Scholar]
- 5.Ross LF, Antommaria AHM. In further defense of the American Academy of Pediatrics Committee on Bioethics “Children as Hematopoietic Stem Cell Donors” Statement. Pediatr Blood Cancer. 2011;57(6):1088–1089 [Google Scholar]
- 6.Ross LF. In defense of the American Academy of Pediatrics policy statement—children as hematopoietic stem cell donors. Pediatr Blood Cancer. 2011;56(4):520–523 [DOI] [PubMed] [Google Scholar]
- 7.Wiener LS, Steffen-Smith E, Fry T, Wayne AS. Hematopoietic stem cell donation in children: a review of the sibling donor experience. J Psychosoc Oncol. 2007;25(1):45–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Packman W, Weber S, Wallace J, Bugescu N. Psychological effects of hematopoietic SCT on pediatric patients, siblings and parents: a review. Bone Marrow Transplant. 2010;45(7):1134–1146 [DOI] [PubMed] [Google Scholar]
- 9.Packman W, Crittenden M, Fischer JBR, Schaeffer E, Bongar B, Cowan MJ. Siblings' perceptions of the bone marrow transplantation process. J Psychosoc Oncol. 1997;15(3/4):81–105 [Google Scholar]
- 10.Packman W, Gong K, VanZutphen K, Shaffer T, Crittenden M. Psychosocial adjustment of adolescent siblings of hematopoietic stem cell transplant patients. J Pediatr Oncol Nurs. 2004;21(4):233–248 [DOI] [PubMed] [Google Scholar]
- 11.MacLeod KD, Whitsett SF, Mash EJ, Pelletier W. Pediatric sibling donors of successful and unsuccessful hematopoietic stem cell transplants (HSCT): a qualitative study of their psychosocial experience. J Pediatr Psychol. 2003;28(4):223–230 [DOI] [PubMed] [Google Scholar]
- 12.Wilkins KL, Woodgate RL. An interruption in family life: siblings’ lived experience as they transition through the pediatric bone marrow transplant trajectory. Oncol Nurs Forum. 2007;34(2):E28–E35 [DOI] [PubMed] [Google Scholar]
- 13.Shama WI. The experience and preparation of pediatric sibling bone marrow donors. Soc Work Health Care. 1998;27(1):89–99 [DOI] [PubMed] [Google Scholar]
- 14.Heiney SP, Bryant LH, Godder K, Michaels J. Preparing children to be bone marrow donors. Oncol Nurs Forum. 2002;29(10):1485–1489 [DOI] [PubMed] [Google Scholar]
- 15.Pot-Mees CC, Zeitlin H. Psychosocial consequences of bone marrow transplantation in children: a preliminary communication. J Psychosoc Oncol. 1987;5(2):73–81 [Google Scholar]
- 16.Holmes-Rovner M, Kroll J, Schmitt N, et al. Patient satisfaction with health care decisions: the satisfaction with decision scale. Med Decis Making. 1996;16(1):58–64 [DOI] [PubMed] [Google Scholar]
- 17.Brehaut JC, O’Connor AM, Wood TJ, et al. Validation of a decision regret scale. Med Decis Making. 2003;23(4):281–292 [DOI] [PubMed] [Google Scholar]
- 18.Opel DJ, Diekema DS. The case of A.R.: the ethics of sibling donor bone marrow transplantation revisited. J Clin Ethics. 2006;17(3):207–219 [PubMed] [Google Scholar]
- 19.Pentz RD, Chan KW, Neumann JL, Champlin RE, Korbling M. Designing an ethical policy for bone marrow donation by minors and others lacking capacity. Camb Q Healthc Ethics. 2004;13(2):149–155 [DOI] [PubMed] [Google Scholar]
- 20.Pentz RD, Pelletier W, Alderfer MA, Stegenga K, Fairclough DL, Hinds PS. Shared decision-making in pediatric allogeneic blood and marrow transplantation: what if there is no decision to make? Oncologist. 2012;17(6):881–885 [DOI] [PMC free article] [PubMed] [Google Scholar]