Abstract
Objective
Develop the WVCR–Linked dataset by combining the West Virginia Cancer Registry (WVCR) with Medicare, Medicaid, and other data sources. Determine health care utilization, costs, and overall burden of four major cancers among the elderly in a rural and medically underserved state population, and to compare them with national estimates.
Method
We extracted personal identifiers from the West Virginia Cancer Registry (WVCR) data file for individuals ≥ 65 years of age with an incident diagnosis of any cancer between January 1, 2002 and December 31, 2007. We linked the extracted data with Medicare and Medicaid administrative data using deterministic record linkage procedures. We updated missing vital status information by linking the National Death Index (NDI) data file. The updated WVCR–Linked dataset was enriched by links to the U.S. decennial census (2000) file and the Area Resource File.
Results
We identified 42,333 individuals, of which 41,574 (98.2%) and 6,031 (14.3%) individuals were matched with Medicare and Medicaid administrative data files, respectively. The NDI data added or updated vital status information for 3,295 (7.8%) individuals in the WVCR–Linked dataset.
Conclusion:
The WVCR–Linked dataset is a comprehensive dataset offering many opportunities to understand factors related to cancer treatment patterns, costs, and outcomes in a rural and medically underserved elderly Appalachian population. Following our example, non-participant states in the Surveillance, Epidemiology and End Results (SEER) program can build a powerful dataset to identify and target cancer disparities, and to improve cancer-related outcomes for their elderly and dual-eligible citizens.
Keywords: Cancer, Medicare, Medicaid, Appalachian, Data Linkage
Introduction
In the United States, the elderly carry a disproportionate burden of cancer. According to the data from the Surveillance, Epidemiology, and End Results (SEER) program, during the period 2004–2008 the median age at cancer diagnosis of all sites was 66 years (Howlader et al., 2011). During the same period, 53.9% of all incident cases of cancer and 69.5% of cancer deaths occurred in patients 65 years of age or older (Howlader et al., 2011). This pattern is expected to persist as the estimated number of elderly in the U.S. doubles to nearly 70 million by 2030. A significant reduction in cancer incidence and mortality can be achieved if the elderly have access to proven prevention and screening interventions, and if elderly cancer patients receive timely and medically effective therapies. Unfortunately, many rural areas of the U.S. are economically underdeveloped and medically underserved (Behringer, 1994; Newell-Withrow, 1997), and the elderly in these regions carry a higher burden of cancer compared to their urban counterparts (Monroe, Ricketts, & Savitz, 1992).
Rural areas in the U.S. are known to report a higher prevalence of cancer and a higher crude all-cause mortality rate (Ricketts, 1999; Miller, Stokes, & Clifford, 1987). While adjusting the data for age, race, and sex distributions effectively eliminates any rural disadvantage with regard to cancer incidence and mortality (Monroe et al., 1992), notable exceptions exist among select rural subpopulations. One such area is the Appalachian region, a population representing 8.1% of the total U.S. population (CDC, 2002; ARC, 2011). Forty-two percent of the Appalachian population live in rural areas, compared to 20% of the national population (ARC, 2011). The death rate in rural Appalachia for all cancers is higher than all of Appalachia, and it is significantly higher than the national cancer death rate (CDC, 2002). These observed cancer disparities can be attributed to limited access to quality medical care facilities, less access to or utilization of early cancer detection programs, increased prevalence of behavioral risk factors like tobacco use and sedentary life style, and socioeconomic factors, such as low income and education (CDC, 2009; Casey, Thiede, & Klingner, 2001; Casto et al., 2009; Hall, Uhler, Coughlin, & Miller, 2002; Silverstein, Nietert, Ye, & Lackland, 2002; Wingo et al., 2005; Wright, Champagne, Dever, & Clark, 1985). In addition to being medically underserved, this rural population also experiences variations in the quality, availability, and accessibility of services when compared to their urban counterparts (Amey, Miller, & Albrecht, 1997). Population based cancer research aimed at identifying such variation in cancer care and improving cancer outcomes in the rural and medically underserved elderly population is much needed. Unfortunately, such research has been challenging due to limitations in available data sources.
State cancer registries have long served as the sole data source for regional cancer incidence and mortality statistics. While they provide detailed information on cancer diagnosis, tumor stage, and initial treatment, they do not track patients longitudinally. This lack of health service usage information over a patient's lifetime limits the value of cancer registry data for health service research. A strategy to overcome this limitation is to link cancer registry data with other sources that provide information on health service usage. This strategy was employed in creating the SEER–Medicare linked dataset, the most widely used data source to study cancer disparities among the elderly in the U.S. (Warren, Klabunde, Schrag, Bach, & Riley, 2002). While SEER data provide detailed clinical information on cancer and initial treatment, the linked Medicare claims data also provide longitudinal information on health services use after diagnosis. In the past 15 years, the SEER–Medicare linked dataset has served as the basis for cancer related health services research, documenting patterns of cancer care and outcomes, and disparities thereof, in subgroups of the elderly population. However, the linked dataset represents only 18 cancer registries from only 15 states, and reflects a population that is more likely to be residing in urban settings (Warren et al., 2002). The data also lacks Medicaid enrollment and usage information for individuals dually eligible for both Medicare and Medicaid, who are known to embody the characteristics associated with health care disparities. Given these limitations, the SEER–Medicare linked dataset does not fully describe the burden of cancer among the elderly in states that are predominantly rural and medically underserved.
Efforts to study cancer disparities in non-SEER states have been undertaken through the linkage of individual state-level cancer registry data with various administrative datasets:
Medicare data (Bradley, et al., 2007; Fleming, Rastogi, Dmitrienko, & Johnson, 1999; Koroukian, 2008; Setoguchi et al., 2007),
Medicaid data (Boscoe, Schrag, Chen, Roohan, & Schymura, 2011; Bradley, Gardiner, Given, & Roberts, 2005; Bradley et al., 2007; Chan, Gomez, O'Malley, Perkins, & Clarke, 2006; Chien, Adams, & Yang, 2011; Koroukian 2003; Koroukian 2008; Perkins et al., 2001; Pollitt, Clarke, Shema, & Swetter, 2008; Ramsey et al., 2008; Schrag, Virnig, & Warren, 2009; Snyder & Foley, 2010),
hospital discharge data (VanEenwyk, Campo, & Ossiander, 2002), and
primary medical record data (Enestvedt et al., 2008).
Selective linkage of state-level cancer registry data with both Medicare and Medicaid data have been accomplished by researchers in North Carolina, New York, and California; however, these linkages were limited by the population under study (Kamal et al., 2012; Camacho et al., 2009; Sanoff et al., 2012). Linkage of entire state-level cancer registry data with both Medicare and Medicaid data is currently available only in two states: Michigan and Ohio (Bradley et al., 2007; Koroukian, 2008). Researchers in the State of Georgia are currently in the process of creating a similarly linked dataset of their cancer registry with Medicare and Medicaid research files (Lipscomb & Gillespie, 2011). The Michigan cancer registry linked dataset was developed to study cancer related disparities, especially by dual Medicare–Medicaid eligibility status (Bradley et al., 2007). The Ohio cancer registry linked dataset was developed to study geriatric cancer care (Koroukian, 2008). The linked West Virginia Cancer Registry Medicare–Medicaid (WVCR– Linked) dataset, described below in detail, is similar to the Michigan and Ohio linked datasets, and addresses the need for a data source to carry out cancer related health services research in the rural and medically underserved elderly population.
West Virginia is the only state situated entirely within the Appalachian region and is the third most rural state in the nation. Fifty of the 55 counties in the state are designated as medically underserved areas, and all or part of 40 counties in the state are classified as health professional shortage areas (WVHCA, 2010). The age-adjusted all site cancer incidence rate among the elderly is higher in the state in comparison to the rest of the country, with incidence rates being particularly high for invasive colorectal and lung cancers (WVDHHR, 2009). Exhibit 1 compares the age adjusted incidence and mortality rates for the 4 common cancers among those aged 65 years and older in West Virginia and the U.S. As the state is representative of Appalachia and similar to many other rural and medically underserved states, it serves as an excellent laboratory for studying and addressing cancer disparities in a rural and medically underserved elderly population. The purpose of this paper is to describe in detail the data linkage process and the resulting analytic WVCR–Linked dataset, to report linkage results, and to discuss the potential uses and limitations of the WVCR–Linked dataset, for health services and epidemiologic research, in a rural and medically underserved elderly U.S. population.
Exhibit 1. Age-adjusted cancer incidence and mortality rates among individuals aged 65 years and older in West Virginia (WV) and in the United States (US), 2002–2006.
| Site of Cancer | Lung & Bronchus | Prostate | Colorectal | Breast | All Sites | |
|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
| Total # of New Cases2 | WV | 10,661 | 7,637 | 6,991 | 5,085 | 50,154 |
| Incidence Rate1,2 | WV | 481.5 | 836.4 | 316.1 | 229.6 | 2265.7 |
| US | 378.5 | 869.2 | 279.4 | 243.2 | 2184.6 | |
| Total # of Deaths3 | WV | 8,645 | 1,555 | 2,910 | 1,442 | 26,279 |
| Mortality Rate1,3 | WV | 390.6 | 193.3 | 131.7 | 65.2 | 1188.1 |
| US | 310.8 | 202.7 | 113.9 | 66.8 | 1077.7 | |
Age-adjusted rates per 100,000 (2000 US Std. Population).
United States Cancer Statistics: 1999–2006 Incidence, WONDER On-line Database. United States Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2010. Accessed at http://wonder.cdc.gov/cancer-v2006.html on Aug 19, 2011.
United States Cancer Statistics: 1999–2006 Mortality, WONDER On-line Database. United States Department of Health and Human Services, Centers for Disease Control and Prevention; 2010. Accessed at http://wonder.cdc.gov/CancerMort-v2006.html on Aug 19, 2011.
Methods
Overview
The WVCR–Linked dataset was developed by linking the West Virginia Cancer Registry data file with the Medicare and Medicaid enrollment and claims data files, the National Death Index (NDI) data file, the U.S. decennial census (2000) data files, and the Area Resource File (ARF) data file (Exhibit 2). The current version contains data on all individuals aged 65 years or older, and diagnosed with any cancer in West Virginia during the years 2002–2007. This project was approved by the West Virginia University—Institutional Review Board, the West Virginia Department of Health and Human Resources (WVDHHR), the West Virginia Bureau for Medical Services (WVBMS), and by the Centers for Medicare & Medicaid Services (CMS).
Exhibit 2.
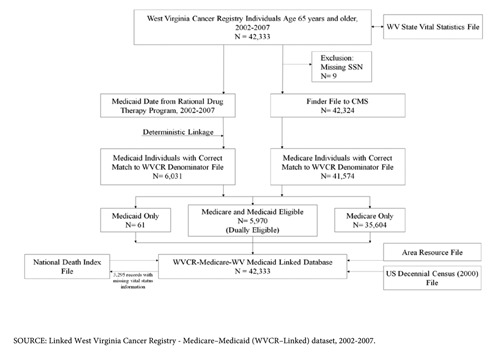
Flowchart showing processes involved in linking the West Virginia cancer registry data file with the Medicare and West Virginia Medicaid administrative data files.
Data Sources
West Virginia Cancer Registry Dataset
Established by the WVDHHR in 1991, the WVCR is a statewide population-based cancer registry that tracks cancer incidence and mortality in the State of West Virginia (WVDHHR, 2009). The registry is funded by both state and federal funding, with the latter administered through a cooperative agreement with the Centers for Disease Control and Prevention's (CDC), National Program of Cancer Registries (NPCR). The registry collects and maintains information on patient identifiers, including first name, last name, social security number (SSN), date of birth, gender, race, county, address of residence, and ZIP Code as well as cancer-specific data, including date of diagnosis, type of cancer diagnosis, tumor stage, tumor grade, and type of initial cancer treatment. Information on vital status, date of death, and cause of death is regularly updated in the registry using in-state death records from the West Virginia Vital Registration Office. The registry lacks information on deaths that occurred out of state, and any cancer treatment that was received following the initial treatment plan. The registry data are complete and have consistently met the data quality standards of the NPCR. Based on timeliness, completeness, and data quality, the registry has been certified by the North American Association of Central Cancer Registries (NAACCR) at the highest (gold) level for diagnosis years 1999 through 2007 (WVCR, 2011). A data file containing information on all reportable tumors diagnosed between 2002 and 2007, among individuals aged 65 years and older in West Virginia, was extracted from the registry and used for linkage purposes in this study.
Medicare Administrative Dataset
Administered by CMS, Medicare is the federally funded program that provides health insurance for more than 47-million people, including nearly all persons age 65 years and older. In West Virginia, it insures 21% of the total population of which 75.4% are elderly (KSHF, 2010). Medicare administrative data files pertaining to services provided to all West Virginia beneficiaries during the years 2002–2007 were purchased from CMS. These files include a Medicare denominator file and separate claims files for inpatient, outpatient, physician and supplier, skilled nursing facility, durable medical equipment, home health agency, and hospice related services provided to beneficiaries enrolled in fee-for-service (FFS) plans. The Medicare denominator file provides information on each beneficiary's age, race, sex, Medicare enrollment history, and their participation in managed care programs. The claims files contain patient demographic data, diagnosis and procedure codes, dates of services, charges, amount paid, provider identification number, and beneficiary county codes. A unique, encrypted, beneficiary identification number (BeneID) can be used to retrieve individual specific enrollment history and claims data across the different files. Claim files were not available for services provided to the approximately 22% of Medicare beneficiaries who were enrolled in managed care plans (KSHF, 2010).
Medicaid Administrative Dataset
Medicaid is the jointly funded federal–state health insurance program for individuals and families with low-income and resources in the U.S. In West Virginia, the Medicaid program insures approximately 22% of the population of which 10% are elderly, and most of whom are dually enrolled in Medicare and Medicaid (KSHF, 2009). For Medicare beneficiaries who are eligible for full Medicaid coverage, the Medicaid program supplements Medicare coverage by providing services and supplies that are available under the state's Medicaid program. Medicaid administrative data files pertaining to services provided to all West Virginia beneficiaries irrespective of their age or eligibility type during the years 2002–2007 were obtained from WVBMS. These files include a Medicaid eligibility file and separate claims files for inpatient, outpatient hospital and non-institutional care, provider, and pharmacy services provided to beneficiaries enrolled in the FFS plan. The Medicaid eligibility file contains beneficiary demographic information, SSN, date of birth, and information on month-by-month Medicaid eligibility in FFS and managed care programs. Medicaid claims data files contain itemized claims for services provided to beneficiaries based on diagnostic and procedure codes. Unique encrypted Medicaid identifiers can be used to retrieve individual specific eligibility and claims data across the different files. As with Medicare administrative files, encounter level claims data were not available for services provided to the approximately 46% of overall West Virginia Medicaid beneficiaries who were enrolled in managed care plans (KSHF, 2009).
National Death Index File
Maintained by the National Center for Health Statistics (NCHS), the National Death Index (NDI) is a central computerized index of death record information collected from state vital statistic offices across the U.S. Specifically, it contains date of death and cause of death information as reported on death certificates. An NDI file containing missing vital status information for select individuals who migrated out of state, following an incident diagnosis of cancer in West Virginia, was purchased and used to update the WVCR–Linked dataset.
U.S. 2000 Decennial Census File
Census data files from the 2000 decennial census containing census tract level indicators of socioeconomic status, like income and education, were obtained from the U.S. Census Bureau (2000).
Area Resource File
The Area Resource File is a national county-level health resource information dataset purchased from the U.S. Department of Health and Human Services, Health Resources and Services Administration (2011). The dataset contains more than 6,000 variables for each of the nation's counties and includes information on health facilities, health professions, resource scarcity, health status, economic activity, health training programs, and socioeconomic and environmental characteristics (Department of Health and Human Services, 2011).
Record Linkage
The WVCR data file served as the ‘case source file’ for all data linkages; records from the WVCR data file were linked individually by patient identifiers with records in other data files. All data linkages were performed at the WVCR office in Charleston, West Virginia, and involved the steps as depicted in Exhibit 2. In linking the data files our priority was to ensure that we captured all possible cancer cases that were insured by Medicare and Medicaid.
A deterministic record linkage method was chosen instead of the probabilistic record linkage method, as researchers have consistently found matching results to be insensitive to this choice, as long as both are equally well conceived and thorough (Bradley et al., 2007; Gomatam, Carter, Ariet, & Mitchell, 2002). The use of the probabilistic linkage approach would have resulted in similar match rates given the high quality of the WVCR data file.
WVCR–Medicare Linkage
To extract Medicare data, we sent a finder file containing the SSN, gender, and date of birth for individuals listed in the WVCR data file to Buccaneer Computer Systems & Service, Inc. (BCSSI), a CMS data contractor. BCSSI used the identifiers from the finder file in a deterministic algorithm to link records with the Medicare enrollment data file. Individuals without a SSN were excluded from the linking process. BCSSI extracted administrative records for the period 2002–2007 for all West Virginia beneficiaries linked using the finder file. The linked Medicare enrollment and administrative data and a ‘SSN to BeneID crosswalk’ file were sent to WVCR. We used the crosswalk file to link the WVCR data file with the Medicare files.
WVCR–Medicaid Linkage
In this step, we linked Medicaid administrative data files with a WVCR data file using a deterministic record linkage method developed by Potosky, Riley, Lubitz, Mentnech, & Kessler, (1993) to link the SEER–Medicare data and employed in studies similar to this one (Koroukian, Cooper, & Rimm, 2003; Koroukian, 2008). Based on this algorithm, records were considered as matched if the following variables from the two data files agreed: 1) SSN, first name, last name; 2) SSN, last name, month of birth, and gender; or 3) SSN, first name, month of birth, and gender. Instead of using the full first and last name, the first six letters were used after eliminating hyphens and apostrophes during matching. The first author reviewed questionable matches.
WVCR–NDI Linkage
We compared a list of individuals extracted from the WVCR data file with missing vital status, date of death, and\or cause of death information as of December 31, 2007 (study cut-off date) with more current vital status and date of death information from the linked Medicare denominator data files. We sent a finder file to NCHS containing SSN, name, date of birth, and sex, excluding individuals identified as alive in the linked Medicare enrollment data files. NCHS returned an NDI data file containing records for matched individuals that we used to update missing vital status information in the WVCR–Linked dataset.
Updating missing vital status data in the WVCR–Linked dataset using the NDI data file is an important step in the data creation process, making the dataset useful for meaningful survival analyses.
WVCR–Census File–ARF Linkage
We geocoded the census tract ID for individuals in the WVCR–Linked dataset using their residence address at the time of diagnosis. The decennial census (2000) provided data on income and educational attainment at the census tract level and these were linked by census tract ID to individual records in the WVCR–Linked dataset. The Area Resource File was linked with the WVCR–Linked dataset using an individual's county code at the time of diagnosis.
All direct patient identifiers including SSN, name, city of residence, and street address at the time of diagnosis, were removed from the WVCR–Linked dataset, resulting in a de-identified analytic dataset that was released to investigators.
Linkage Analysis
The quality of match between the WVCR data file and Medicare\Medicaid administrative data files was evaluated along with the significance of updates from the NDI. The study variables included cancer site\stage, date of diagnosis, vital status, date of death, and individual demographics. We stratified patients by year of diagnosis. We categorized cancer stage as in-situ, local, regional, distant, and unstaged using SEER Summary Stage 2000. Age at diagnosis was categorized as less than 65 years, 65–69 years, 70–74 years, 75–79 years, 80–84 years, and 85 years and older. Given that the state is predominately White, race was classified as White, Black, and Other. We performed Chi-square and Fisher's Exact tests to compare demographics and cancer stage between Medicare and non-Medicare groups, and between Medicaid and non-Medicaid groups.
We summed months of enrollment in Medicare and/or Medicaid among enrolled individuals in the WVCR–Linked dataset, and reported person-months of Medicare and/or Medicaid enrollments by enrollment type and by major cancer types. We evaluated the timing of Medicare/Medicaid enrollment with respect to incident cancer diagnosis month by comparing the proportion of individuals who were enrolled in Medicare/Medicaid at least three months prior to the cancer diagnosis month (Pre-Diagnosis group) with those enrolled in Medicare/Medicaid during the three months prior to the cancer diagnosis month, during the cancer diagnosis month, or after the cancer diagnosis month (Peri/Post-Diagnosis group). Continuity of Medicare and/or Medicaid enrollment was determined by following each individual's enrollment history from their incident cancer diagnosis date through their date of death or study cut-off date (December 31, 2007). We performed a stratified analysis by major cancer types to determine proportions related to timing/continuity of enrollment. SAS version 9.1 (Cary, NC) was used in all data file links and analyses.
Results
The process described in this paper, from initial data request application to the creation of the de-identified analytic WVCR–Linked dataset, required about 18 months (Exhibit 2). A total of 42,333 individuals, aged 65 years or older when diagnosed with cancer, were identified from the WVCR data file with 44,887 cancer records during the period 2002–2007. Only 9 individuals had a missing SSN and could not be linked with Medicare and Medicaid administrative data files.
Using the SSN to BeneID crosswalk, we were able to match correctly a maximum of 41,574 (98.2%) individuals from the WVCR with the Medicare data files using the SSN alone. Matches with SSN and gender (97%) or SSN and date of birth (93%) resulted in lower rates. For Medicaid, we matched a maximum of 6,031 (14.3%) individuals from the WVCR data file with Medicaid records. We matched 5,790 (12.9%) individuals based on SSN, first name, and last name; 5,860 (13.1%) based on SSN, last name, month of birth, and gender; and, 5,747 (12.8%) based on SSN, first name, month of birth, and sex.
We identified 5,970 (14.1%) individuals from the WVCR data file who were dually eligible for both Medicaid and Medicare (Exhibit 2). While the match rate with Medicaid administrative data files ranged from 13.7% to 14.6% across study years, the match rate varied considerably by cancer site, with lower match rates observed in prostate cancer patients than in breast, colorectal, or lung cancer patients (Exhibit 3).
Exhibit 3. Summary of matching results between the West Virginia cancer registry data file and the Medicare and Medicaid administrative data files for individuals aged 65 years and older at cancer diagnosis, 2002–2007.
| Year of Diagnosis | Cases Reported | Unique Individuals | Unique Individuals Matched with Medicare Files | Unique Individuals Matched with Medicaid Files | Unique Individuals Deceased by December 31, 2007 | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||
| N | N | N | % | N | % | N | % | |
|
|
|
|
|
|
|
|
|
|
| 2002 | 7,652 | 7,450 | 7,296 | 97.9 | 1,087 | 14.6 | 4,543 | 61.0 |
| 2003 | 7,314 | 7,141 | 6,992 | 97.9 | 1,022 | 14.3 | 4,207 | 58.9 |
| 2004 | 7,389 | 7,218 | 7,076 | 98.0 | 1,002 | 13.9 | 3,859 | 53.5 |
| 2005 | 7,409 | 7,236 | 7,117 | 98.4 | 1,051 | 14.5 | 3,491 | 48.2 |
| 2006 | 7,533 | 7,356 | 7,259 | 98.7 | 1,007 | 13.7 | 2,889 | 39.3 |
| 2007 | 7,590 | 7,360 | 7,247 | 98.5 | 1,041 | 14.1 | 1,666 | 22.6 |
| 2002–207 | 44,887 | 42,333 | 41,574 | 98.2 | 6,031 | 14.3 | 20,066 | 47.4 |
SOURCE: Linked West Virginia Cancer Registry - Medicare–Medicaid (WVCR–Linked) dataset, 2002-2007.
Exhibit 3 also summarizes the match rate and number of individuals matched according to the year of initial cancer diagnosis at age 65 or older. The denominators for the match rates consisted of individuals reported by the WVCR data file as diagnosed with cancer at age 65 or older in that year. During any given year, the linkage process matched 97.9% to 98.7% of all individuals found in the WVCR data file. The number of cases exceeds the total number of individuals in Exhibit 3, because individuals with multiple primary cancers are counted more than once.
A total of 3,295 (7.8%) individuals had missing vital status, date of death, and/or cause of death information in the WVCR–Linked dataset. Exhibit 3 shows the proportion of decedents by year of diagnosis in the WVCR–Linked dataset after the NDI update. Overall, 47.4% (20,066) of individuals with diagnoses of cancer at age 65 years and older died during the years 2002– 2007. The proportion of patients deceased by the end of 2007 was 19.7%, 43.3%, 76.9%, and 18.7% in each of breast, colorectal, lung, and prostate cancer diagnosed patients, respectively.
Exhibit 4 compares demographics and cancer stage data between cases that were and were not successfully matched with Medicare and Medicaid administrative data files. The results indicate that individuals who are elderly, women, non-White, and diagnosed with regional\distant cancer stage are disproportionately represented among those who were not matched with the Medicare files (p ≤ 0.05). These differences are similar to that reported in the SEER–Medicare files (Potosky et al., 1993). The proportion of cancer cases enrolled in Medicaid also displays substantial differences by gender, race, age, and cancer stage. Elderly White women with regional\distant stage diagnosis are more likely to be enrolled in Medicaid compared to their counterparts (p ≤ 0.05).
Exhibit 4. Comparison of cancer cases from the West Virginia cancer registry data file, by matching status with the Medicare and Medicaid administrative data files, 2002–2007.
| Characteristics | Medicare | Medicaid | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Cases Matched | Cases Not Matched | Cases Matched | Cases Not Matched | |||||
|
|
|
|
|
|||||
| N | % | N | % | N | % | N | % | |
|
|
|
|
|
|
|
|
|
|
| Sex1 | ||||||||
| Male | 23,707 | 53.8 | 326 | 41.4 | 2,525 | 39.7 | 21,508 | 55.8 |
| Female | 20,393 | 46.2 | 461 | 58.6 | 3,832 | 60.3 | 17,022 | 44.2 |
| Age2 | ||||||||
| < 65 | 3 | 0 | 0 | 0 | 0 | 0 | 3 | 0 |
| 65-69 | 10,552 | 23.9 | 179 | 22.7 | 1,665 | 26.2 | 9,066 | 23.5 |
| 70-74 | 10,713 | 24.3 | 150 | 19.1 | 1,512 | 23.8 | 9,351 | 24.3 |
| 75-79 | 10,453 | 23.7 | 176 | 22.4 | 1,282 | 20.2 | 9,347 | 24.3 |
| 80-84 | 7,345 | 16.7 | 143 | 18.2 | 1,027 | 16.2 | 6,461 | 16.8 |
| 85+ | 5,034 | 11.4 | 139 | 17.7 | 871 | 13.7 | 4,302 | 11.2 |
| Race3,2 | ||||||||
| White | 43,030 | 97.6 | 742 | 94.3 | 6,106 | 96.1 | 37,666 | 97.8 |
| Black | 929 | 2.1 | 25 | 3.2 | 231 | 3.6 | 723 | 1.9 |
| Other | 136 | 0.3 | 20 | 2.5 | 19 | 0.3 | 137 | 0.4 |
| SEER Summary Stage (2000)4,2 | ||||||||
| In situ | 2,717 | 6.2 | 41 | 5.2 | 302 | 4.8 | 2,456 | 6.4 |
| Local | 17,757 | 40.3 | 273 | 34.7 | 2,288 | 36 | 15,742 | 40.9 |
| Regional | 7,453 | 16.9 | 115 | 14.6 | 1,154 | 18.2 | 6,414 | 16.6 |
| Distant | 9,970 | 22.6 | 198 | 25.2 | 1,445 | 22.7 | 8,723 | 22.6 |
| Unstaged | 5.748 | 13 | 143 | 18.2 | 1,094 | 17.2 | 4,797 | 12.5 |
| Not Applicable | 448 | 1 | 17 | 2.2 | 74 | 1.2 | 391 | 1 |
|
| ||||||||
| Total number of Cases5 | 44,100 | 100 | 787 | 100 | 6,357 | 100 | 38,530 | 100 |
Fisher Exact test, p ≤ 0.05 for both Medicare and Medicaid groups.
Chi-square test, p ≤ 0.05 for both Medicare and Medicaid groups.
5 cases have missing information.
7 cases have missing information.
Includes persons age 65 or older with cancer diagnosis reported by WVCR.
SOURCE: Linked West Virginia Cancer Registry - Medicare–Medicaid (WVCR–Linked) dataset, 2002-2007.
Exhibit 5 shows the timing of Medicare/Medicaid enrollment among matched individuals by cancer type. The proportion of Medicare matched individuals in the pre-diagnosis group was 0.95 for all cancer sites combined and was almost the same for the four major cancer sites. However, among Medicaid matched individuals, the proportion of those in the pre-diagnosis group was less than 0.71 for all cancer sites combined. This proportion also varied for the four major cancer sites.
Exhibit 5.
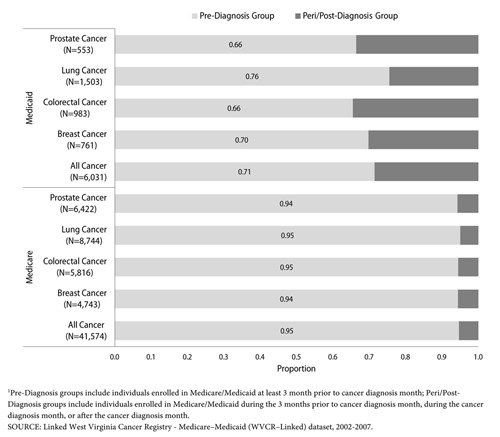
Proportion of population enrolled in Medicaid/Medicare prior to incident cancer diagnosis¹, among individuals aged 65 years and older at the time of diagnosis, in West Virginia, 2002–2007.
The proportion of Medicare-matched continuously enrolled individuals was 0.78 for all cancers, and ranged from 0.73–0.82 among the 4 major cancer sites. However the proportion of Medicaid-matched continuously enrolled individuals was only 0.58 for all cancers, and ranged from 0.43–0.64 among the 4 major cancer sites. Among dual eligible individuals, the proportion was 0.54 for all cancers, and ranged from 0.41–0.60 among the four major cancer sites.
Distribution of cancer cases in the WVCR–Linked dataset by stage at diagnosis makes it evident that for relatively common cancers such as breast, colorectal, lung, and prostate, there are sufficient numbers of cases by stage for a variety of studies (Exhibit 6). Exhibit 6 also shows the total person-months of Medicare and/or Medicaid enrollment spanning 2002–2007 for each cancer site. This information provides an estimate of available sample sizes for studies that require health care utilization information following a cancer diagnosis month.
Exhibit 6. Frequency of incident cancer cases by stage at diagnosis, and availability of person-months of Medicare/Medicaid enrollment information among individuals aged 65 years and older in West Virginia, by cancer site, 2002–2007.
| Cancer Site | Stage at Diagnosis | Person-months1 | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| All Stages | In Situ | Local | Regional | Distant | Unstaged | Medicare | Medicaid | Dual Eligible | |
|
|
|
|
|
|
|
|
|
|
|
| All Sites2 | 44,880 | 2,758 | 18,030 | 7,568 | 10,168 | 5,891 | 2,385,940 | 193,512 | 176,932 |
| Colorectal | 6,155 | 351 | 2,550 | 1,825 | 872 | 557 | 336,362 | 30,139 | 28,174 |
| Lung and Bronchus | 9,019 | 14 | 1,837 | 1,956 | 3,855 | 1,357 | 395,351 | 43,556 | 38,734 |
| Breast | 4,979 | 735 | 2,714 | 1,045 | 252 | 233 | 307,203 | 27,734 | 25,978 |
| Prostate | 6,510 | 7 | 5,231 | 273 | 273 | 726 | 403,341 | 15,596 | 14,656 |
| Bladder | 2,506 | 991 | 1,120 | 168 | 90 | 137 | 146,713 | 9,698 | 8,952 |
| Head and Neck | 1,537 | 34 | 739 | 422 | 197 | 145 | 83,782 | 8,216 | 7,417 |
| Upper GI Tract | 1,356 | 19 | 393 | 372 | 318 | 254 | 60,235 | 5,256 | 4,840 |
| Lymphoma | 1,224 | 0 | 240 | 209 | 618 | 157 | 65,798 | 4,380 | 4,141 |
| Cervical | 138 | 1 | 50 | 50 | 21 | 16 | 6,426 | 1,656 | 1,425 |
| Uterine | 940 | 7 | 579 | 193 | 51 | 110 | 53,837 | 5,586 | 4,806 |
| Ovarian | 525 | 0 | 54 | 79 | 297 | 95 | 23,930 | 2,988 | 2,563 |
| Testicular | 17 | 0 | 8 | 2 | 7 | 0 | 863 | 54 | 53 |
| Kidney and Ureter | 1,324 | 61 | 733 | 202 | 187 | 141 | 73,866 | 5,090 | 4,531 |
| Pancreatic and Biliary | 1,714 | 10 | 255 | 384 | 582 | 483 | 68,736 | 6,718 | 5,905 |
| Skin | 1,907 | 512 | 979 | 190 | 82 | 144 | 113,885 | 6,918 | 6,444 |
| Brain and CNS3 | 1,003 | 0 | 279 | 73 | 13 | 231 | 50,100 | 4,088 | 3,822 |
NOTES. Frequency distribution of all cancer types by stage is given here for informational purposes only; actual data usage for research purposes is currently approved by data providers for only breast, colorectal, lung, and prostate cancer; use of other cancer data for research purposes will require prior approval from all data providers.
Person-months of enrollment in Medicare and/or Medicaid from 2002–2007.
465 cases had stage categorized as ‘Not applicable,’ 7 had missing stage information.
407 cases had stage categorized as Not applicable.
SOURCE: Linked West Virginia Cancer Registry - Medicare–Medicaid (WVCR–Linked) dataset, 2002-2007.
Discussion
Health services and outcomes research studies covering the entire continuum of cancer care can be conducted for a rural and medically underserved elderly population using the comprehensive WVCR–Linked dataset. This includes studies related to economics of cancer care (Luo, Bradley, Dahman, & Gardiner, 2010), health care systems' delivery (Clement, Bradley, & Lin, 2009), cancer risk factors and prevention (Bradley, Given, & Roberts, 2002; Snyder et al., 2011), quality of cancer treatment (Hadley et al., 2010), and palliative/ end-of-life care (Legler, Bradley, & Carlson, 2011). For the first time, this dataset makes it possible to conduct studies of different aspects of cancer care in this population, as the linked SEER–Medicare dataset made possible the studies of other populations. The dataset provides an avenue to study the accuracy and completeness of initial treatment information as recorded in the cancer registry. It can also be used to study disparities in the delivery of cancer care, which might help in better understanding the variations in patterns of care and outcomes in the state. Policy makers can use the WVCR– Linked dataset to identify and promote interventions at the state level, which have been shown to be effective in reducing cancer disparities (Bell & Standish, 2005).
Combining administrative databases with clinical data collected by a cancer registry overcomes several of the pitfalls of using either data source alone for health services research. Linking cancer registry data files with Medicare and Medicaid administrative data files is a powerful strategy for evaluating cancer care among the elderly, and can provide a comprehensive longitudinal data source. This study describes the use of this strategy in creating the WVCR–Linked dataset to enable future research that may improve our understanding of the patterns of costs, utilization, and medical outcomes of cancer prevention and treatment services among elderly in a rural and medically underserved state population.
The WVCR–Linked dataset is similar in structure to the SEER–Medicare dataset except for the addition of Medicaid data files. The quality and completeness of the WVCR–Linked dataset is evident from the high match rates obtained while linking the WVCR data file with Medicare and Medicaid data files. The overall WVCR–Medicare match rate of 98.2% is higher than the SEER–Medicare match rate of 93% (Potosky et al., 1993).
Possible explanations for why 759 individuals from the WVCR data file were not matched with Medicare administrative data files include: (1) individuals might not be enrolled in Medicare, as approximately 2% of all elderly are not enrolled in Medicare (Potosky et al., 1993); (2) individuals might be out of state residents diagnosed with cancer in West Virginia; (3) incorrectly recorded SSN, sex, or date of birth information in the WVCR data file; and/or (4) incorrect matches between the individuals' SSN from the WVCR data file and that from the CMS administrative data files.
The use of a cost-effective deterministic linkage approach to link Medicaid administrative data files with WVCR data file resulted in a match rate (14.3%) that is comparable to that found in prior studies (Bradley et al., 2007; Koroukian, 2008). As NCHS data extraction charges are based on the number of records submitted and the number of years searched, identifying the subset of individuals with missing vital status information using both the WVCR data file and the Medicare denominator file, and limiting the search for their vital status between the years 2002–2007, was a cost-effective strategy.
Overall, the WVCR–Linked dataset lacked Medicare\Medicaid information for only nine individuals who were left out of the linkage process due to missing SSNs. When comparing matched versus unmatched cases, unmatched cases represented patients who were older, women, or of non-White race. Unmatched cases were more frequently diagnosed at distant\regional stages or not staged at all. Among Medicaid patients, the lower match rate among prostate cancer patients is similar to that found in the Ohio study and was expected, given that the Medicaid program serves primarily women, and older women are more likely than older men to have the income threshold necessary to qualify for Medicaid benefits (Koroukian, 2008).
Timing of enrollment among Medicare/Medicaid matched individuals highlights the fact that while most individuals are enrolled in Medicare prior to cancer diagnosis, the proportion of individuals enrolled in Medicaid prior to their cancer diagnosis was lower. This may be attributed to Medicare enrollees becoming Medicaid eligible due to increasing cancer treatment-related financial hardship. Given the varying burden of cancer by cancer type, significant variation in the proportion of individuals who enrolled in Medicaid peri/post cancer diagnosis was seen among the four major cancer types. With the majority of Medicare and/or Medicaid matched individuals continuously enrolled, the WVCR–Linked dataset can be used for a complete evaluation of health service utilization following incident cancer diagnosis till death or till the study cut-off period (December 31, 2007).
The WVCR–Linked dataset has several limitations with regard to cancer disparities research. The dataset is specific to West Virginia and the ability to generalize the findings from studies using it may be limited. However, the demographic profile of the population in West Virginia is very similar to that of neighboring states in Appalachia (ARC, 2011). Given the lack of data sources for comprehensive cancer related health services research from this region, the WVCR–Linked dataset makes it possible for the first time to compare outcomes between these rural states and other states/regions that are represented in the SEER–Medicare dataset. The WVCR–Linked dataset is restricted to the elderly population, and this limits the ability to study cancer disparities in the younger population aged less than 65 years. This also limits studies comparing cancer outcomes between the young and the elderly. As the population in West Virginia is predominantly White, the WVCR–Linked dataset doesn't provide sufficient cases for identifying racial disparities in cancer outcomes. This is a limitation shared my many national data sources and is not specific to the WVCR–Linked dataset (Arispe, Holmes, & Moy, 2005; Bradley et al., 2007). Medicare and Medicaid are the only insurance groups represented in the WVCR–Linked dataset. Information for services provided by other insurance carriers and through VA hospitals are not captured in the WVCR–Linked dataset and hence cannot be ascertained. However, Medicare and Medicaid are the largest and most comprehensive insurance providers to the elderly in rural areas. The WVCR–Linked dataset also lacks Medicare and Medicaid managed care claims data. Incomplete or inaccurately coded bills in claims files (Iezzoni, 1990; Potosky et al., 1993) also pose potential problems in data analysis. Finally, the files do not contain individual level socioeconomic information such as educational attainment, marital status, or family income. However aggregate measures of socioeconomic status at the census tract level are available through 2000 decennial census data in the WVCR–Linked dataset.
Linking data from the WVCR, the Medicare program, and the West Virginia state Medicaid program has been a complex technical task. We relied heavily on collaboration and investment from researchers and state administrators, especially those administering the WVCR and the Medicaid program. Such collaborative arrangements are required to create a data infrastructure necessary to address many of the health care questions regarding cancer disparities and quality of care in the elderly. The data linkage process provided important lessons on how to efficiently link cancer registry data files with Medicare and Medicaid data files.
Researchers from non-SEER states considering a similar project in their state can gain from our experience in creating the WVCR–Linked dataset. In our view, success depends upon a number of factors, including degree of completeness of SSNs in the state cancer registry data and the extent of managed care penetration in both Medicare and Medicaid within the state. Researchers interested in identifying the usefulness of a similar linked dataset, could start by identifying the quality of state cancer registry data and the level of managed care penetration in both Medicare and Medicaid populations. Successful and timely completion of such a project depends on the vision shared by participating organizations and their collaborative structure in the state.
In conclusion, successful linkage of the WVCR data file with administrative and claims files from important sources represents a significant step in research efforts to reduce cancer disparities in the rural and medically underserved elderly population. This project capitalized on existing data sources and fits well with the national research agenda (NCI, 2001). Research using this unique resource should advance the understanding of factors related to treatment patterns, costs, and outcomes in this population. The information gained from the analysis of this dataset can be used to guide policies that ensure the rural elderly receive timely and appropriate cancer care.
Acknowledgment
We would like to acknowledge Myra Fernatt, Dr. Alana Hudson, and Dr. Loretta Haddy from West Virginia Cancer Registry; Commissioner Nancy Atkins, and Nora Antlake from West Virginia Bureau of Medical Services; and Steve Small and Sirish Shrestha from West Virginia University, School of Pharmacy, Rational Drug Therapy Program, for their administrative and material support.
Footnotes
Disclaimer: We would like to acknowledge that this project was supported by grant number 1R24HS018622-01 (PI: S. Madhavan) from the Agency of Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
References
- Amey CH, Miller MK, Albrecht SL. The role of race and residence in determining stage at diagnosis of breast cancer. The Journal of Rural Health. 1997 Spring;13(2):99–108. doi: 10.1111/j.1748-0361.1997.tb00939.x. [DOI] [PubMed] [Google Scholar]
- ARC (Appalachian Regional Commission) The Appalachian region. 2011 Retrieved from http://www.arc.gov/index.do?nodeId=2.
- Arispe IE, Holmes JS, Moy E. Measurement challenges in developing the national healthcare quality report and the national healthcare disparities report. Medical Care. 2005 Mar;43(3, Suppl):I17–I23. doi: 10.1097/00005650-200503001-00004. [DOI] [PubMed] [Google Scholar]
- Behringer B. Health care services in Appalachia. In: Couto RA, Simpson NK, Harris G, editors. Sowing Seeds in the Mountains, Community-based Coalitions for Cancer Prevention and Control. Bethesda, MD: NIH, National Cancer Institute; 1994. pp. 62–80. NIH Publication No. 94-3779. [Google Scholar]
- Bell J, Standish M. Communities and health policy: a pathway for change. Health Affairs (Project Hope) 2005 Mar-Apr;24(2):339–342. doi: 10.1377/hlthaff.24.2.339. [DOI] [PubMed] [Google Scholar]
- Boscoe FP, Schrag D, Chen K, Roohan PJ, Schymura MJ. Building capacity to assess cancer care in the Medicaid population in New York State. Health Services Research. 2011 Jun;46(3):805–820. doi: 10.1111/j.1475-6773.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley CJ, Given CW, Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. Journal of the National Cancer Institute. 2002 Apr;94(7):490–496. doi: 10.1093/jnci/94.7.490. [DOI] [PubMed] [Google Scholar]
- Bradley CJ, Gardiner J, Given CW, Roberts C. Cancer, Medicaidenrollment, and survival disparities. Cancer. 2005 Apr;103(8):1712–1718. doi: 10.1002/cncr.20954. [DOI] [PubMed] [Google Scholar]
- Bradley CJ, Given CW, Luo Z, Roberts C, Copeland G, Virnig BA. Medicaid, Medicare, and the Michigan Tumor Registry: a linkage strategy. Medical Decision Making. 2007 Jul-Aug;27(4):352–363. doi: 10.1177/0272989X07302129. [DOI] [PubMed] [Google Scholar]
- Camacho FT, Wu J, Wei W, Kimmick G, Anderson RT, Balkrishnan R. Cost impact of oral capecitabine compared to intravenous taxane-based chemotherapy in first-line metastatic breast cancer. Journal of Medical Economics. 2009 Sep;12(3):238–245. doi: 10.3111/13696990903269673. [DOI] [PubMed] [Google Scholar]
- Casey MM, Thiede CK, Klingner JM. Are rural residents less likely to obtain recommended preventive healthcare services? American Journal of Preventive Medicine. 2001 Oct;21(3):182–188. doi: 10.1016/S0749-3797(01)00349-X. [DOI] [PubMed] [Google Scholar]
- Casto BC, Sharma S, Fisher JL, Knobloch TJ, Agrawal A, Weghorst CM. Oral cancer in Appalachia. Journal of Health Care for the Poor and Underserved. 2009 Feb;20(1):274–285. doi: 10.1353/hpu.0.0097. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Cancer death rates—Appalachia,1994-1998. Morbidity and Mortality Weekly Report. 2002 Jun;51(24):527–529. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) State-specific prevalence and trends in adult cigarette smoking--United States,1998–2007. Morbidity and Mortality Weekly Report. 2009 Mar;58(9):221–226. [PubMed] [Google Scholar]
- Chan JK, Gomez SL, O'Malley CD, Perkins CI, Clarke CA. Validity of cancer registry medicaid status against enrollment files: implications for population-based studies of cancer outcomes. Medical Care. 2006 Oct;44(10):952–955. doi: 10.1097/01.mlr.0000220830.46929.43. [DOI] [PubMed] [Google Scholar]
- Chien LN, Adams EK, Yang Z. Medicaid enrollment at early stage of disease: the Breast and Cervical Cancer Prevention and Treatment Act in Georgia. Inquiry. 2011 Fall;48(3):197–208. doi: 10.5034/inquiryjrnl_48.03.02. [DOI] [PubMed] [Google Scholar]
- Clement JP, Bradley CJ, Lin C. Organizational characteristics and cancer care for nursing home residents. Health Services Research. 2009 Dec;44(6):1983–2003. doi: 10.1111/j.1475-6773.2009.01024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enestvedt CK, Mayo SC, Diggs BS, Mori M, Austin DA, Shipley DK, Billingsley KG. Diagnostic laparoscopy for patients with potentially resectable pancreatic adenocarcinoma: is it cost-effective in the current era? Journal of Gastrointestinal Surgery. 2008 Jul;12(7):1177–1184. doi: 10.1007/s11605-008-0514-y. [DOI] [PubMed] [Google Scholar]
- Fleming ST, Rastogi A, Dmitrienko A, Johnson KD. A comprehensive prognostic index to predict survival based on multiple comorbidities: a focus on breast cancer. Medical Care. 1999 Jun;37(6):601–614. doi: 10.1097/00005650-199906000-00009. [DOI] [PubMed] [Google Scholar]
- Gomatam S, Carter R, Ariet M, Mitchell G. An empirical comparison of record linkage procedures. Statistics in Medicine. 2002 May;21(10):1485–1496. doi: 10.1002/sim.1147. [DOI] [PubMed] [Google Scholar]
- Hadley J, Yabroff KR, Barrett MJ, Penson DF, Saigal CS, Potosky AL. Comparative effectiveness of prostate cancer treatments: evaluating statistical adjustments for confounding in observational data. Journal of the National Cancer Institute. 2010 Dec;102(23):1780–1793. doi: 10.1093/jnci/djq393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall HI, Uhler RJ, Coughlin SS, Miller DS. Breast and cervical cancer screening among Appalachian women. Cancer Epidemiology, Biomarkers & Prevention. 2002 Jan;11(1):137–142. [PubMed] [Google Scholar]
- Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, et al.Edwards BK, editors. SEER Cancer Statistics Review,1975–2008. Retrieved from http://seer.cancer.gov/csr/1975_2008/ (based on November 2010 SEER data submission, posted to the SEER web site, 2011)
- Iezzoni LI. Using administrative diagnostic data to assess the quality of hospital care. Pitfalls and potential of ICD-9-CM. International Journal of Technology Assessment in Health Care. 1990;6(2):272–281. doi: 10.1017/S0266462300000799. [DOI] [PubMed] [Google Scholar]
- Kaiser State Health Facts (KSHF) West Virginia Medicaid & CHIP Enrollment. [Accessed on September 17, 2011];2009 Retrieved from http://www.statehealthfacts.org/profileind.jsp?cat=4&rgn=50.
- Kaiser State Health Facts (KSHF) West Virginia Medicare Enrollment. [Accessed September 17, 2011];2010 Retrieved from http://www.statehealthfacts.org/profileind.jsp?cat=6&rgn=50&cmprgn=1.
- Kamal AH, Camacho F, Anderson R, Wei W, Balakrishnan R, Kimmick G. Similar survival with single-agent capecitabine or taxane in first-line therapy for metastatic breast cancer. Breast Cancer Research and Treatment. 2012 Mar; doi: 10.1007/s10549-012-2037-1. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Koroukian SM. Assessing the effectiveness of Medicaid in breast and cervical cancer prevention. Journal of Public Health Management and Practice. 2003 Jul-Aug;9(4):306–314. doi: 10.1097/00124784-200307000-00009. [DOI] [PubMed] [Google Scholar]
- Koroukian SM. Linking the Ohio Cancer Incidence Surveillance System with Medicare, Medicaid, and Clinical Data from Home Health Care and Long Term Care Assessment Instruments: Paving the Way for New Research Endeavors in Geriatric Oncology. Journal of Registry Management. 2008 Winter;35(4):156–165. [PMC free article] [PubMed] [Google Scholar]
- Koroukian SM, Cooper GS, Rimm AA. Ability of Medicaid claims data to identify incident cases of breast cancer in the Ohio Medicaid population. Health Services Research. 2003 Jun;38(3):947–960. doi: 10.1111/1475-6773.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legler A, Bradley EH, Carlson MD. The effect of comorbidity burden on health care utilization for patients with cancer using hospice. Journal of Palliative Medicine. 2011 Jun;14(6):751–756. doi: 10.1089/jpm.2010.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipscomb J, Gillespie TW. State-level cancer quality assessment and research: building and sustaining the data infrastructure. Cancer Journal (Sudbury, Mass.) 2011 Jul-Aug;17(4):246–256. doi: 10.1097/PPO.0b013e3182296422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Z, Bradley CJ, Dahman BA, Gardiner JC. Colon cancer treatment costs for Medicare and dually eligible beneficiaries. Health Care Financing Review. 2010 Fall;31(1):35–50. [PMC free article] [PubMed] [Google Scholar]
- Miller MK, Stokes CS, Clifford WB. A comparison of the rural-urban mortality differential for deaths from all causes, cardiovascular disease and cancer. The Journal of Rural Health. 1987 Jul;3(2):23–34. doi: 10.1111/j.1748-0361.1987.tb00165.x. [DOI] [PubMed] [Google Scholar]
- Appalachian Regional Commission, A. C. Ricketts TC, Savitz LA. Cancer in rural versus urban populations: a review. The Journal of Rural Health. 1992 Summer;8(3):212–220. doi: 10.1111/j.1748-0361.1992.tb00354.x. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute (NCI) The Nation's Investment in Cancer Research. Bethesda, MD: National Institutes of Health; 2001. Pub. 02-4373. [Google Scholar]
- Newell-Withrow C. A glance at Appalachia. Journal of Cultural Diversity. 1997 Winter;4(4):129–131. [PubMed] [Google Scholar]
- Perkins CI, Wright WE, Allen M, Samuels SJ, Romano PS. Breast cancer stage at diagnosis in relation to duration of medicaid enrollment. Medical Care. 2001 Nov;39(11):1224–1233. doi: 10.1097/00005650-200111000-00009. [DOI] [PubMed] [Google Scholar]
- Pollitt RA, Clarke CA, Shema SJ, Swetter SM. California Medicaid enrollment and melanoma stage at diagnosis: a population-based study. American Journal of Preventive Medicine. 2008 Jul;35(1):7–13. doi: 10.1016/j.amepre.2008.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potosky AL, Riley GF, Lubitz JD, Mentnech RM, Kessler LG. Potential for cancer related health services research using a linked Medicare-tumor registry database. Medical Care. 1993 Aug;31(8):732–748. doi: 10.1097/00005650-199308000-00006. [DOI] [PubMed] [Google Scholar]
- Ramsey SD, Zeliadt SB, Richardson LC, Pollack L, Linden H, Blough DK, Anderson N. Disenrollment from Medicaid after recent cancer diagnosis. Medical Care. 2008 Jan;46(1):49–57. doi: 10.1097/MLR.0b013e318158ec7f. [DOI] [PubMed] [Google Scholar]
- Ricketts TC, editor. Rural health in the United States. New York, NY: Oxford University Press; 1999. [Google Scholar]
- Sanoff HK, Carpenter WR, Freburger J, Li L, Chen K, Zullig LL, et al. Schrag D. Comparison of adverse events during 5-fluorouracil versus 5-fluorouracil/oxaliplatin adjuvant chemotherapy for stage III colon cancer: A Population-based analysis. Cancer. 2012 Jan; doi: 10.1002/cncr.27422. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrag D, Virnig BA, Warren JL. Linking tumor registry and Medicaid claims to evaluate cancer care delivery. Health Care Financing Review. 2009 Summer;30(4):61–73. [PMC free article] [PubMed] [Google Scholar]
- Setoguchi S, Solomon DH, Glynn RJ, Cook EF, Levin R, Schneeweiss S. Agreement of diagnosis and its date for hematologic malignancies and solid tumors between medicare claims and cancer registry data. Cancer Causes & Control. 2007 Jun;18(5):561–569. doi: 10.1007/s10552-007-0131-1. [DOI] [PubMed] [Google Scholar]
- Silverstein MD, Nietert PJ, Ye X, Lackland DT. Access to care and stage at diagnosis for patients with lung cancer and esophageal cancer: analysis of the Savannah River Region Information System cancer registry data. Southern Medical Journal. 2002 Aug;95(8):900–908. [PubMed] [Google Scholar]
- Snyder JW, Foley KL. Disparities in colorectal cancer stage of diagnosis among Medicaid-insured residents of North Carolina. North Carolina Medical Journal. 2010 May-Jun;71(3):206–212. [PubMed] [Google Scholar]
- Snyder CF, Frick KD, Herbert RJ, Blackford AL, Neville BA, Carducci MA, Earle CC. Preventive care in prostate cancer patients: following diagnosis and for five-year survivors. Journal of Cancer Survivorship: Research and Practice. 2011 Sep;5(3):283–291. doi: 10.1007/s11764-011-0181-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. Census of Population and Housing, Population and Housing Unit Counts PHC-3. [Accessed September 3, 2011];2000 Retrieved from http://www.census.gov/compendia/statab/2011/tables/11s0029.pdf.
- U.S. Department of Health and Human Services, Health Resources and Services Administration. Area Resource File – Overview. [Accessed September 3, 2011];2011 Retrieved from http://arf.hrsa.gov/overview.htm.
- VanEenwyk J, Campo JS, Ossiander EM. Socioeconomic and demographic disparities in treatment for carcinomas of the colon and rectum. Cancer. 2002 Jul;95(1):39–46. doi: 10.1002/cncr.10645. [DOI] [PubMed] [Google Scholar]
- Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER–Medicare data: content, research applications, and generalizability to the United States elderly population. Medical Care. 2002 Aug;40(8, Suppl):IV-3–IV-18. doi: 10.1097/01.MLR.0000020942.47004.03. [DOI] [PubMed] [Google Scholar]
- West Virginia Cancer Registry (WVCR) About the West Virginia Cancer Registry. [Accessed September 17, 2011];2011 Retrieved from http://www.dhhr.wv.gov/oeps/cancer/Pages/AboutWVCR.aspx.
- West Virginia Department of Health and Human Resources(WVDHHR) Cancer Incidence in West Virginia. [Accessed September 17, 2011];2009 Retrieved from http://www.dhhr.wv.gov/oeps/cancer/Documents/Cancer_Incidence_in_WV_pdf.
- West Virginia Health Care Authority (WVHCA) West Virginia State Health Plan. [Accessed September 17, 2011];2010 Retrieved from http://www.hcawv.org/PolicyPlan/shpBmat/shpProPiper.pdf.
- Wingo PA, Howe HL, Thun MJ, Ballard-Barbash R, Ward E, Brown ML, et al. Edwards BK. A national framework for cancer surveillance in the United States. Cancer Causes & Control. 2005 Mar;16(2):151–170. doi: 10.1007/s10552-004-3487-5. [DOI] [PubMed] [Google Scholar]
- Wright JS, Champagne F, Dever GE, Clark FC. A comparative analysis of rural and urban mortality in Georgia, 1979. America n Journal of Preventive Medicine. 1985 Jan-Feb;1(1):22–29. [PubMed] [Google Scholar]


