Abstract
Objective
Injection of botulinum toxin into the anal sphincter is a novel and safe new treatment of chronic idiopathic constipation and anal fissure in children. The purpose of this study was to determine the utility of intra sphincteric injection of botox in the treatment of children with refractory constipation.
Methods
All children who suffered from chronic constipation for more than three months, and who had not responded to medical treatment, were referred to pediatrics surgical clinic for surgical intervention by pediatric gastroenterologist. The patients were randomly divided into cases and control group. The control group received no injection and was only treated with stool softeners. The case group received this therapy in addition to injection. After the botox injection, patients were asked about the presence of the signs of constipation including painful defecation, vomiting, stool consistence, soiling and defecation interval.
Findings
Defecation of painful stool existed in 88% of patients before botox injection and it was reduced to 15% after botox injection. In the control group, 90% of patients had painful defecation, which reduced to 86% after medical treatment (P=0.0001). Stool was hard in 80% of patients before was reduced to 28% after botox injection. In the control group, it existed in 81% of children and reduced to 78% after medical treatment (P=0.0001). Soiling existed in 62% of patients before and was reduced to 8% after botox injection, but in the control group it reduced from 62% to 42.5% after medical treatment (P=0.0001). In the control group, 98% of the patients had defecation intervals more than 3 days and it was the same after medical treatment. In case group, this index before botox injection was 9.1 days, and after botox injection was reduced to 2.6 days (P=0.0001).
Conclusion
Our study results showed that injection of botulinum toxin into anal sphincter is an effective and safe new treatment of chronic idiopathic constipation in children.
Keywords: Botulinum Toxin, Botox, Constipation, Defecation, Children
Introduction
Constipation as a common disorder in children accounts for more than 3% of visits to a pediatrician and 10 to 25% of visits to pediatric gastroenterologist[1]. Constipation is classified as functional and organic[1]. Functional constipation accounts for 95% of children with chronic constipation while only 5% have an organic cause for their symptoms[2]. Chronic functional constipation (CFC) is defined as a delay in defecation with less than three times per week existing for more than two weeks and being associated with stool withholding behavior. It is also associated with painful defecation, without underlying anatomic or medical etiologies. Thus, CFC is also called idiopathic. Treatment includes primary stool evacuation, toilet training, high fiber diet and laxative administration[1]. Children usually are treated with a combination of toilet training, running a bowel diary, and oral laxatives. In many patients, this does not provide effective improvement, so newer treatment is required[3].
The early difficulty with defecation that causes pain, fear, and refusal to use toilet, often progresses to the formation of vicious cycles of increasing fecal retention and the rectum increases in capacity, then the experience of passing large, hard stools is repeated. There is increasing distress as overflow fecal incontinence compounds the problem for the older child[4].
Surgical treatment has been used in children’s refractory constipation treatment. However, surgical methods are often regarded to be traumatic. Topical muscle relaxants have been used in recent decades. The evolution began with nitrates, which were helpful in adult chronic fissure. Botulinum toxin A, a widely applicable acetyl-cholinesterase inhibitor that causes clinically reversible muscle paralysis, is now a popular drug for treating many conditions associated with smooth or skeletal muscle dysfunction[5].
Transcutaneous needle-free injection of botulinum toxin into the anal sphincter is a novel and safe new treatment of chronic idiopathic constipation and anal fissure in children[6].
The purpose of this study was to determine the utility of intra sphincteric injection of botox in the treatment of children with refractory constipation referred to our center.
Subjects and Methods
This was a prospective case control study which was done in Children’s Medical Center in Tehran University of Sciences.
All children who suffered from chronic constipation for more than three months, and who had not responded to medical treatment, were referred to pediatric surgical clinic for interventions by pediatric gastroenterologist. Perineal examination in the first step provided that they did not have macroscopic anatomical abnormalities. In case of accompanying diseases or abnormal anus and perineum, and children with transition zone in barium enema were excluded from the study. Also, manometry and rectal biopsy was performed in all children. Those with ganglion cells in their rectal biopsy and who had high threshold recto anal inhibitory reflex (RAIR) or absent RAIR in manometry, entered the study.
The patients were randomly divided into cases and control group. The control group received no injection and were treated exclusively with stool softeners. The case group received botulinum toxin injection in addition to this therapy. botox injection was carried out under general anesthesia in three regions of the anal sphincter in lithotomy position. The botulinum toxin Dysport was injected in sphincter in 3, 6 and 9 o’clock. It was not injected in 12 o’clock to avoid the possibility of urinary incontinence. Total Dysport dosis was 160 units, half of it (i.e. 80 units) was injected in 6 o’clock and one-fourth (i.e. 40 U) in 3 o’clock and one-fourth in 9 o’clock, Injection was done simultaneously in both internal and external anal sphincters.
In the first month after injection, all patients were evaluated once a week and were investigated regarding the improvement or recurrence of symptoms and followed up monthly in the first six months. The response to botox injection six months after injection was compared with the control group.
For evaluation of the patients’ condition after the botox injection, patients were asked questions about the presence of the signs of constipation including painful defecation, vomiting, stool’s consistency, soiling and defecation intervals.
The sample size based on statistical calculations is 88 patients (44 cases and 44 controls). Continuous variables are expressed in the form of mean and standard deviation. For comparing proportions, chi 2 test and for comparing quantitative variables, t-test was used.
Findings
Defecation of painful stool existed in 88% of patients before botox injection and it was reduced to 15% after botox injection. In the control group,90% of patients had painful defecation, which reduced to 86% after medical treatment and the difference was statistically significant (P=0.0001).
Stool condensation existed in 80% of patients before botox injection, and it was reduced to 28% after botox injection. In the control group, it existed in 81% of children and reduced to 78% after medical treatment and the difference was statistically significant (P=0.0001).
Soiling existed in 62% of patients before botox injection and was reduced to 8% after botox injection. In the control group it reduced from 62% to 42.5% after medical treatment and the difference was statistically significant (P=0.0001).
Defection interval more than 3 days existed in 100% of patients before botox injection and it was reduced to 15% after botox which was also statistically significant (P=0.0001). In the control group, 98% of the patients had defection intervals more than 3 days and it was the same after medical treatment. In average, defecation interval before botox injection was 9.1 days, and after botox injection was reduced to 2.6 days, which is statistically significant. (P=0.0001). In botox injection group there were 22 boys and 18 girls, the difference was not statistically significant. In Table 1, the symptoms of chronic constipation before and after the botox injection are expressed as percentages. In Table 2, the percentage of decrease in signs has been brought based on the sex of patients in which there was no significant differece between girls and boys, therefore, the effect of botox injection did not have any relation with the sex of patient with chronic idiopathic constipation.
Table 1.
Symptoms of chronic constipation before and after botox injection
| Symptoms | Before botox injection | After botox injection | P. value |
|---|---|---|---|
| painful defecation | 87.5% | 15% | 0.0001 |
| Stool condensation | 80% | 27.5% | 0.0001 |
| Soiling | 62.5% | 7.5% | 0.0001 |
| Defecation interval more than 3 days | 100% | 15% | 0.0001 |
Table 2.
Percentages of decrease in signs and symptoms of chronic constipation before and after botulinum toxin injection based on the sex of patients
| Parameter | Gender | Before injection | After injection | P. value | P. value male/female |
|---|---|---|---|---|---|
| Painful defecation | Female | 89% | 0.06% | 0.0001 | 0.1 |
| Male | 86% | 23% | 0.0001 | ||
| Stool condensation | Female | 89% | 22% | 0.0001 | 0.4 |
| Male | 73% | 32% | 0.0001 | ||
| Soiling | Female | 56% | 0% | 0.0001 | 0.1 |
| Male | 68% | 14% | 0.0001 | ||
| Defecation interval more than | Female | 100% | 5.6% | 0.0001 | 0.1 |
| Male | 100% | 23% | 0.0001 |
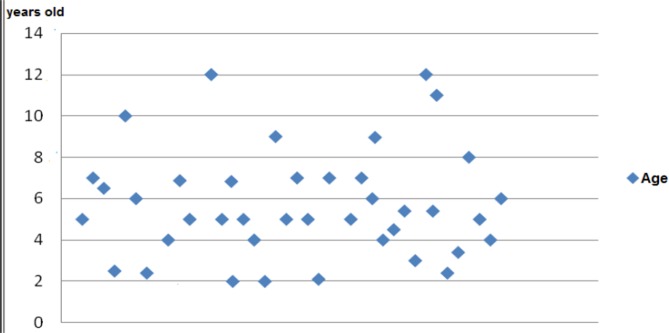
In this study, the minimum age of the patients was 2 years and the maximum 12 years, the most frequent age group was 5 years. Diagram 1 shows the frequency of age group’s distribution in botox injection group. In Table 3 the decrease of signs is compared between two groups of above and below 5 year olds, in which a significant difference is not evident. Therefore, the effect of botox injection has no relationship with the age of patients with chronic idiopathic constipation. In Table 3, the decrease of signs has been compared between the two groups of above and below 5 year olds, in which a significant difference was also not observed. Therefore, the effect of botox injection has no relationship with the age of patients with chronic idiopathic constipation.
Diagram 1.
The age distribution in children with refractory chronic constipation who received botulinum toxin injection
Table 3.
Signs and symptoms of chronic constipation in two above and below 5 year olds, before and after botulinum toxin injection
| Symptom | Age | Before injection | After injection | P. value | Ratio |
|---|---|---|---|---|---|
| Pain full defecation | 5y> | 88% | 18% | 0.0001 | 0.6 |
| 5y ≤ | 87% | 13% | 0.0001 | ||
| Stool Condensation | 5y> | 71% | 29% | 0.01 | 0.8 |
| 5y ≤ | 87% | 26% | 0.0001 | ||
| Soiling | 5y> | 41% | 12% | 0.02 | 0.3 |
| 5y ≤ | 78% | 0.04% | 0.0001 | ||
| Defecation interval more than 3 days | 5y> | 100% | 18% | 0.0001 | 0.6 |
| 5y ≤ | 100% | 13% | 0.0001 |
Discussion
Constipation is a common problem in children. The incidence of constipation is reported from 0.3% to 8% in childhood[2, 10, 12]. When constipation becomes chronic and refractory, it produces much distress and problems for the child and family[2]. The exact cause of chronic constipation is not identified in most children, therefore it is diagnosed as functional or idiopathic[3].
Anorectal manometry has shown some abnormalities in these patients including higher threshold to rectal distention or abnormal rectal sensation[3]. Another cause of chronic and refractory constipation is internal anal sphincter achalasia. Internal anal sphincter achalasia (IASA) is a chronic constipation that is clinically very similar to Hirschsprung’s disease. In patients with IASA, ganglion cells are seen in rectal biopsy and in manometric evaluation rectoanal inhibitory reflex is absent[7, 8]. Anal achalasia can cause obstruction or constipation in children who have undergone pull through procedure for treatment of HD[7, 9]. Anal achalasia can be seen and cause constipation in otherwise healthy children[10].
Anal dilatation might have a role in management of chronic refractory idiopathic constipation in children in preschool age[11]. The traditional treatment of IASA is myectomy or myotomy[7]. Another treatment of IASA is forceful dilatation of anal sphincter[12].
An alternative approach to treatment of IASA in patients without HD is toxin botulinum injection in anal sphincter[7, 10]. Toxin botulinum interferes with acetylcholine release at the neuromuscular junction in anal sphincter after injection[7]. By this mechanism, it produces a chemical denervation of sphincter[13]. Therefore intra sphincteric botulinum toxin injection by inhibition of neural stimulation to sphincter can induce a chemical myectomy and it may be useful in treatment of IASA[7, 10, 14] and chronic idiopathic constipation[7].
In one study, toxin botulinum injection in internal anal sphincter had definite effect in improvement of patients who had obstruction or constipation after pull through for treatment of Hirschsprung’s disease. In these patients, residual aganglionosis and anastomotic stricture were ruled out by rectal biopsy and barium enema and physical examination[4].
In another study injection of botulinum toxin had a transient effect in treatment of most children with anismus and in some patients it showed a long term effect[5]. In this study painful defecation existed in 88% of patients before toxin botulinum injection and it was reduced to 15% after toxin botulinum injection and the difference was statistically significant (P=0.0001).
Moreover, Stool condensation existed in 80% of these patients before toxin botulinum injection, it was reduced to 28% after toxin botulinum injection, the difference is statistically significant (P=0.0001). Soiling existed in 62% of patients before botox injection and was reduced to 8% after botox injection. In the control group it reduced from 62% to 42.5% after medical treatment and the difference was statistically significant (P=0.0001). Defection interval more than 3 days existed in 100% of patients before botox injection and it was reduced to 15% after botox which is also statistically significant (P=0.0001). In the control group, 98% had defection intervals more than 3 days and it remained the same after medical treatment. In average defecation interval before botox injection was 9.1 days and after botox injection was reduced to 2.6 days which is also statistically significant (P=0.0001).
Conclusion
Injectio of botulinum toxin into the anal sphincter is an effective and safe new treatment of chronic idiopathic constipation in children.
Acknowledgment
We hereby thank Dr. Najafi, the head of gastroenterology division of Children’s Medical Center. This study was approved by Vice-chancellor for Research of School of Medicine as a dissertation and approved by ethical committee of Tehran University of Medical Sciences.
Conflict of Interest
None
References
- 1.Karami H, Khademloo M, Niari P. Polyethylene glycol versus paraffin for the treatment of childhood functional constipation. Iran J Pediatr. 2009;19(3):255–61. [Google Scholar]
- 2.Monajemzadeh M, Kalantari M, Yaghmai B. Hirschsprung’s disease: a clinical and pathologic study in iranian constipated children. Iran J Pediatr. 2011;21(3):362–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Khodadad A, Sabbaghian M. Role of synbiotics in the treatment of childhood constipation: a double-blind randomized placebo controlled trial. Iran J Pediatr. 2010;20(4):387–92. [PMC free article] [PubMed] [Google Scholar]
- 4.Management of childhood constipation. Postgrad Med J. 2003;79(937):616–21. doi: 10.1136/pmj.79.937.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chao NSY, Wong BPY, Leung MWY, et al. Botulinum toxin in the treatment of refractory constipation associated with anal sphincter hypertonicity: A pilot prospective study in Chinese children. Surgical Practice. 2011;15(1):7–11. [Google Scholar]
- 6.Keshtgar AS, Ward HC, Clayden GS. Transcutaneous needle-free injection of botulinum toxin: a novel treatment of childhood constipation and anal fissure. J Pediatr Surg. 2009;44(9):1791–8. doi: 10.1016/j.jpedsurg.2009.02.056. [DOI] [PubMed] [Google Scholar]
- 7.Irani K, Rodrigues L, Doody DP, et al. Botulinum toxin for the treatment of chronic constipation in children with anal sphincter dysfunction. Pediatr Surg Int. 2008;24(7):779–83. doi: 10.1007/s00383-008-2171-3. [DOI] [PubMed] [Google Scholar]
- 8.De Caluwe D, Yoneda A, Aki U, et al. Internal anal sphincter achalasia: outcome after internal sphincter myectomy. J Pediatr Surg. 2001;36(5):736–8. doi: 10.1053/jpsu.2001.22949. [DOI] [PubMed] [Google Scholar]
- 9.Minkes RK, Langer JC. A prospective study of botulinum toxin for internal anal sphincter hypertonicity in children with Hirschsprung’s disease. J Peddiatr Surg. 2000;35(12):1733–6. doi: 10.1053/jpsu.2000.19234. [DOI] [PubMed] [Google Scholar]
- 10.Ciamarra P, Nurko S, Barksdale E, et al. Internal anal sphincter achalasia in children: clinical characteristics and treatment with clostridium botulinum toxin. J Peddiatr Gastroenterol Nutr. 2003;37(3):315–9. doi: 10.1097/00005176-200309000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Keshtgar AS, Ward HC, Clayden GS, et al. Role of anal dilatation in treatment in idiopathic constipation in children: long term follow up of a double-blind randomized controlled study. Pediatr Surg Int. 2005;21(2):100–5. doi: 10.1007/s00383-004-1336-y. [DOI] [PubMed] [Google Scholar]
- 12.Freeman NV. Intractable constipation in children treated by forceful anal stretch or anorectal myectomy: preliminary communication. J R Soc Med. 1984;77(Suppl 3):6–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Pasricha PJ, Ravich WJ, Hendrix TR, et al. Intrasphicteric botulinum toxin for the treatment of achalasia. N Engl J Med. 1995;332(12):774–8. doi: 10.1056/NEJM199503233321203. [DOI] [PubMed] [Google Scholar]
- 14.Messineo A, CodrIch D, Monai M, et al. The treatment of internal anal sphincter achalasia with botulinum toxin. Pediatr Surg Int. 2001;17(7):521–3. doi: 10.1007/s003830100583. [DOI] [PubMed] [Google Scholar]