Abstract
Aim:
Polysaccharide sulfate (PSS) is a new type of heparinoid synthesized with alginic acid as the basic material and then by chemical introduction of effective groups. Although PSS is successfully applied in ischemic cardio-cerebrovascular disease, its effect on cardiac function after ischemia/reperfusion (I/R) injury has previously not been investigated. The aim of the present study was to investigate whether PSS can protect the heart from I/R injury and the underlying mechanism of protection.
Methods:
Isolated rat hearts were perfused (Langendorff) and subjected to 20 min global ischemia followed by 60 min reperfusion with Kreb's Henseleit solution or PSS (0.3–100 mg/L). Myocardial contractile function was continuously recorded. Creatine kinase (CK) and lactate dehydrogenase (LDH) leakage were measured. Tumor necrosis factor-α (TNF-α) expression in cardiomyocytes was investigated. Western blot analysis for extracellular regulated kinases (ERKs), c-jun amino-terminal kinase (JNKs) and p38 mitogen-activated protein kinase (MAPK) activity was performed.
Results:
After I/R, cardiac contractility decreased, CK and LDH levels increased in the coronary effluent, and TNF-α expression increased in cardiomyocytes. PSS administration at concentrations of 1–30 mg/L improved cardiac contractility, reduced CK and LDH release and inhibited TNF-α production. Phosphorylated-p38MAPK (p-p38MAPK) and p-p54/p46-JNK increased in I/R rat hearts but diminished in PSS (1–30 mg/L) treated hearts. P-p44/p42-ERK levels were unchanged. In contrast, high concentrations of PSS (100 mg/L) had adverse effects that caused a worsening of heart function.
Conclusion:
PSS has dose-dependent cardioprotective effects on the rat heart after I/R injury. The beneficial effects may be mediated through normalization of the activity of p38 MAPK and JNK pathways as well as controlling the level of TNF-α expression.
Keywords: polysaccharide sulfate, ischemia/reperfusion, inflammation, TNF-α, MAPK
Introduction
Polysaccharide sulfate (PSS) is a new type of heparinoid, extracted from Phylum Phaeophyta. It is a linear, hydrophylic, anionic polyelectrolyte consisting primarily of β-(1,3)-linked glucose residues. PSS is synthesized with alginic acid as the basic material. By chemically introducing sulfuryl and propylene glycol residues in the hydroxyl and carboxyl group of alginic acid sodium, PSS is obtained as a diester sodium1. PSS lacks the disaccharide building blocks and 1,4-glycosidic linkages characteristic of heparin1, and it is about one-third as active as heparin as an inhibitor of blood coagulation2.
Heparin and heparin-related glycosaminoglycans are of benefit to the ischemic myocardium3, 4, 5. PSS, a new heparinoid, is known to dilute blood, lower blood viscosity, ameliorate hypercoagulation and modulate dyslipidemia6. Clinically, PSS is used to prevent and treat ischemic cardiovascular and cerebrovascular disease as well as hyperlipemia1. The results of animal experiments showed that application of PSS could protect against cerebral ischemia/reperfusion (I/R) injury2, 7. Also, PSS could protect the heart function of patients with coronary heart disease8. These findings suggest that PSS may alleviate I/R injury. However, the effect of PSS on cardiac I/R injury has never been investigated.
Mitogen-activated protein kinase (MAPK) plays an important role in the intracellular signaling pathway and is activated during ischemia or after I/R injury9, 10, 11. MAPKs include three main families: the extracellular regulated kinases (ERKs, p42/44), the c-jun amino-terminal kinase (JNKs, p54/46) and the p38 MAPK12, 13. These three families appear to have a significant role in the response and adaptation of the myocardium to stress14, 15. Therefore, we analyzed changes in the MAPK signaling pathway to investigate the molecular mechanism of the effect of PSS treatment on the rat heart during I/R.
Local inflammatory response is an important contributor to cardiac dysfunction following I/R injury16. The myocardium itself generates inflammatory cytokines, such as tumor necrosis factor-α (TNF-α), in response to acute I/R, and these locally produced inflammatory mediators cause depression of cardiac function17, 18. Hence, methods that block the inflammatory response may be protective16, 19. Heparin and heparin-related glycosaminoglycans exert a cardiac protective effect partially through anti-inflammatory activity, in addition to their anticoagulant function5, 20. Hence, in this study, we also examined the role of PSS on TNF-α production in myocardium.
The main aims of the present study were to investigate whether PSS treatment facilitated postischemic heart function recovery and to determine the optimized concentration of PSS that exerted the cardioprotective effect ex vivo. In order to explore the specific molecular mechanisms, we examined the influence of PSS on the MAPK pathway and its effect on TNF-α production in myocardium.
Materials and methods
Materials and animals
Modified Krebs–Henseleit (KH) buffer consisted of (in mmol/L) NaCl 118, KCl 4.7, CaCl2 1.5, KH2PO4 1.2, MgSO4 1.2, NaHCO3 25.2, and glucose 11.1. PSS was obtained from the Third Pharmaceutical Company (Qingdao, China, No 0509080108). Male Sprague-Dawley rats (250–300 g) were purchased from the Experiment Animal Center, Chinese Academy of Sciences in Shanghai. The procedures in our experiments were approved by the Zhejiang University Animal Care and Use Committee, and the investigation conformed to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No 85–23, revised 1996).
Isolated heart perfusion
Rats were decapitated, and their hearts were isolated. Retrograde perfusion of the hearts was performed in a nonrecirculating Langendorff apparatus with the spontaneous heart beat rate. Modified KH buffer was bubbled with 95% O2/5% CO2 at 37 °C and at pH of 7.4. A water-filled latex balloon was placed in the left ventricle via left atrium and connected to a computer coupled with a biosignal system (MedLab-U/4CS, China) through a pressure transducer. The balloon volume was adjusted to yield 4–8 mmHg of left ventricular end-diastolic pressure (LVEDP) during the equilibration period, and no further alterations in balloon volume were made. Left ventricular developed pressure (LVDP), LVEDP, maximum rate of intraventricular pressure development (dp/dtmax) and relaxation (dp/dtmin) and heart rate were recorded every 10 min during perfusion after equilibration. The coronary perfusion pressure was 100 mmHg, and the coronary flow rate was obtained by timed collection into a graduated cylinder throughout the perfusion procedure.
Experimental groups
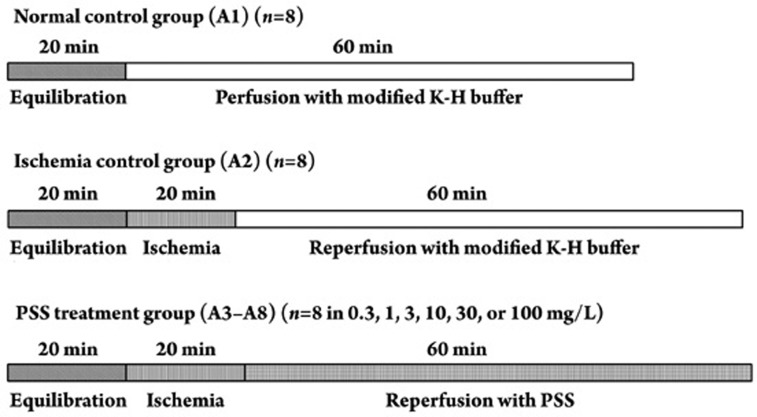
The rat hearts were randomly divided into eight groups: A1–A8. All hearts were perfused for 20 min for equilibration before the following perfusion protocol: (1) 60 min perfusion with modified KH buffer (A1); (2) 20 min global no-flow ischemia followed by 60 min reperfusion with modified KH buffer (A2), 0.3 mg/L (A3), 1 mg/L (A4), 3 mg/L (A5), 10 mg/L (A6), 30 mg/L (A7), or 100 mg/L (A8) PSS (Figure 1).
Figure 1.
Experimental protocol. All experimental groups began with a 20 min perfusion period to allow for stabilization of the isolated hearts. Then, the hearts were divided into the normal control group (A1), the ischemia control group (A2) and the PSS treatment group (A3– A8), which received different concentrations (0.3, 1, 3, 10, 30, or 100 mg/L) of PSS reperfusion for 60 min.
Determination of tissue injury
The coronary effluent during the first 30 min of reperfusion was pooled. The cumulative amounts of creatine kinase (CK) and lactate dehydrogenase (LDH) released in the coronary effluent were measured in each group (Jiancheng Co, China).
TNF-α determination
Samples from LV myocardial tissue taken for TNF-α measurements were immediately stored at -70°C at the end of perfusion until assayed. The tissue was homogenized in RIPA (150 mmol/L NaCl, 0.1% SDS, 0.5% sodium deoxycholate, 1% NP-40, 50 mmol/L Tris, pH 7.4, 20 mmol/L NaF, 2 mmol/L EGTA, 0.5% levamisole, 1 mmol/L NaVO4, 1 μg/mL leupeptin) containing 1 mmol/L PMSF. The supernatant was obtained by centrifugation (18 000×g, 15 min, 4 °C). Tumor necrosis factor-α level in the supernatant of the myocardium homogenate was determined using an ELISA kit (R&D Systems, Inc., Minneapolis, MN, USA). Final results were expressed as pg/mg protein with protein concentration measured using the BCA method (Applygen Technologies Inc, Beijing, China).
Western blot
Protein samples were electrophoresed on 12% sodium dodecylsulfate-polyacrylamide gels and transferred onto nitrocellulose membranes, which were incubated with monoclonal rabbit-anti-phosphorylated-p38MAPK (p-p38MAPK), rabbit-anti-p-p54/p46-JNK or rabbit-anti-p-p44/p42-ERK (1:1000 dilution, Cell Signaling), followed by incubation with a secondary anti-rabbit antibody. Blots were analyzed semiquantitatively using imaging software (Eastman Kodak) and normalized by comparison to glyceraldehyde phosphate dehydrogenase (GAPDH, 36 kDa).
Statistical analysis
Data are expressed as mean±SD. Data sets containing multiple groups were compared by analysis of variance using SPSS 13.0 software. Mean values between the two groups were compared by a least-significant difference test, after an F test for homogeneity of variances had been performed. If data failed to meet the requirements for equal variance, a Tamhane T2 test was used. The results were considered statistically significant at a value of P<0.05.
Results
Effects of PSS on recovery of cardiac performance in isolated I/R rat hearts
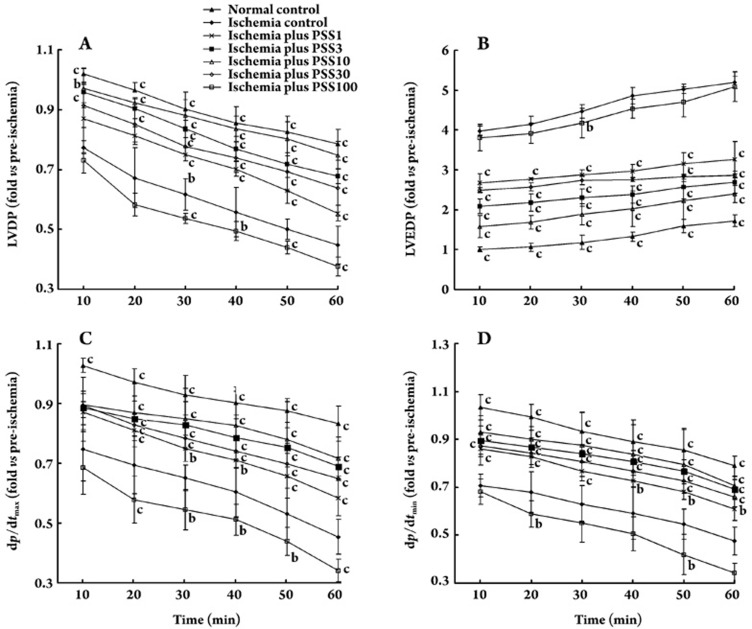
Post-ischemic recovery of cardiac function during 60 min of reperfusion was expressed as a percentage of the pre-ischemic value. As shown in Figure 2A–D, at concentrations of 1, 3, 10, and 30 mg/L, PSS accelerated the recovery of LVDP, LVEDP, dp/dtmax and dp/dtmin in isolated I/R rat hearts, but no alteration of cardiac function was observed with PSS at a concentration of 0.3 mg/L (data not shown). Moreover, after I/R, coronary flow was significantly improved at 1, 3, 10, and 30 mg/L of PSS (data not shown). Heart rate remained unchanged in the A1–A8 group before and after ischemia (data not shown). In contrast, PSS at 100 mg/L elicited a marked attenuation of contractility and heart rate in hearts with I/R.
Figure 2.
Influence of 1–100 mg/L PSS on postischemic recovery of cardiac function. The postischemic recovery of (A) left ventricular developed pressure (LVDP), (B) left ventricular end-diastolic pressure (LVEDP), and (C and D) maximum rate of intraventricular pressure development and relaxation (dp/dtmax, dp/dtmin) in the isolated hearts are shown for the 0, 1, 3, 10, 30, and 100 mg/L PSS experimental groups (n=8 in each group). Data are expressed as a percentage of the pre-ischemic value and are presented as mean±SD. bP<0.05, cP<0.01 vs ischemia control group.
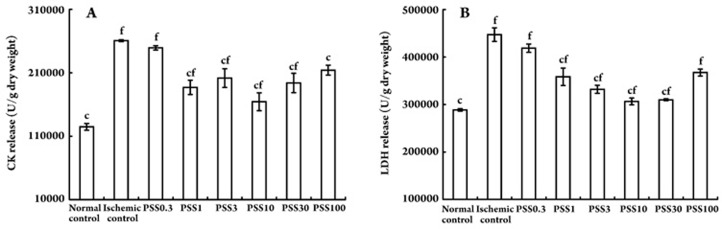
Assessment of cell membrane integrity
The cardioprotective effect of PSS was estimated by measuring CK and LDH levels in the coronary effluent. After the 20 min no-flow ischemia, the cumulative amounts of CK and LDH released in the coronary effluent during first 30 min of reperfusion averaged 124805±5238 and 288613±2569 U/g dry weight. These levels were significantly higher than those of the nonischemic rat hearts. PSS treatment (1–30 mg/L) was able to partially attenuate this effect. The amounts of released CK and LDH showed a trend consistent with mechanical activity (Figure 3).
Figure 3.
Cumulative amounts of (A) CK and (B) LDH released in coronary effluent during first 30 min of reperfusion from rat hearts subjected to 20 min ischemia with or without PSS treatment. Data are presented as mean±SD. cP<0.01 vs ischemia control group; fP<0.01 vs normal control group.
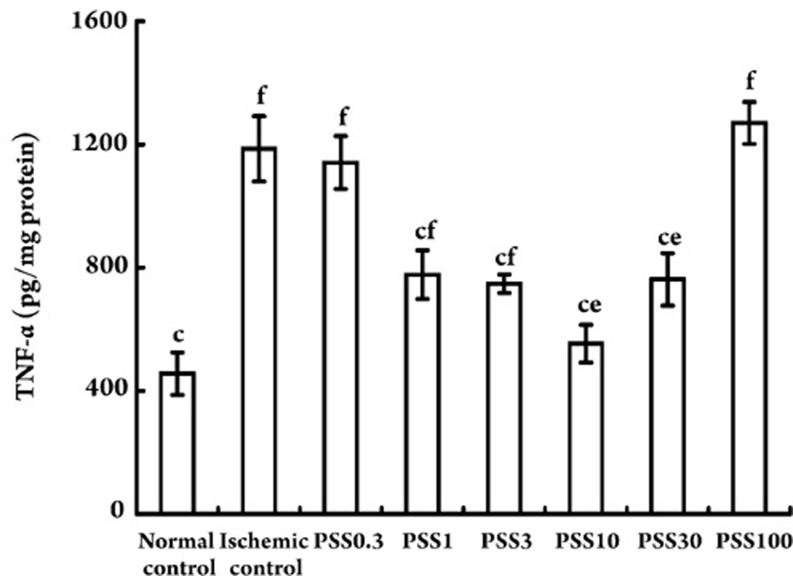
TNF-α production in the rat myocardium
Non-ischemic cardiomyocytes produced a basal level of 455.44±68.59 pg/mg protein of TNF-α. A significant amount of TNF-α (1140.83±86.16 pg/mg protein) was detected in the LV myocardium after 20 min ischemia followed by 60 min reperfusion. Treatment of ischemic rat hearts for 60 min during reperfusion with PSS at concentrations of 1, 3, 10, and 30 mg/L all caused a significant decrease in the amount of TNF-α produced. In contrast, PSS at concentrations of 0.3 and 100 mg/L did not deplete the elevated TNF-α level in I/R rat hearts (Figure 4).
Figure 4.
Concentrations of TNF-α protein level in the rat myocardium treated without or with PSS at different concentrations. Data are presented as mean±SD. cP<0.01 vs ischemia control group; eP<0.05, fP<0.01 vs normal control group.
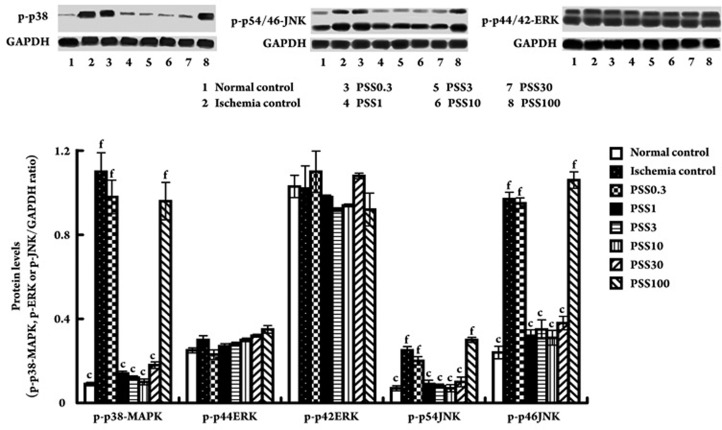
Effect of PSS on MAPK signaling pathways
I/R promoted a 12-fold activation of p38 and a 3.5-fold increase of p-p54/p46-JNK as measured by Western blot using an antibody recognizing the phosphorylated form of p38 and JNK (P<0.01 vs nonischemic hearts). p-p38 and p-p54/p46-JNK expression decreased in PSS (1–30 mg/L) treated I/R hearts compared with control I/R hearts (P<0.01). The amount of p-p44/p42-ERK was unchanged among all of the groups at all the time points measured (Figure 5).
Figure 5.
Expression of p-p38, p-p54/p46-JNK and p-p44/p42-ERK protein levels in tissue of isolated rat hearts. (A) Western blot analysis showed that p38 and p54/p46-JNK activities were suppressed in response to treatment with PSS (1–30 mg/L) while p-p44/p42-ERK expression remained unchanged. (B) p38, p54/p46-JNK and p44/p42-ERK activities were evaluated by densitometry. Levels of p-p38, p-p54/p46-JNK and p-p44/p42-ERK were normalized to GAPDH. Data are presented as mean±SD. cP<0.01 vs ischemia control group; fP<0.01 vs normal control group.
Discussion
Our study shows that the acute administration of PSS (1–30 mg/L) to I/R hearts reduced myocardial dysfunction as evidenced by the presence of significant functional improvement and diminished CK and LDH release. These data support the view that PSS possesses protective effects against myocardium I/R injury. However, a decrease in cardiac coronary flow occurred at 100 mg/L of PSS, which was associated with a prominent depression of the heart rate and a decrease in cardiac performance. This suggests that high concentrations of PSS are toxic to the heart.
Because we explored the cardioprotective effect of PSS in an isolated perfused rat heart model, the observations in this study are likely not due to the anticoagulant, blood viscosity diluting and lipid-lowering properties of PSS.
The dual phosphorylation of MAPKs on Thr/Tyr is essential for kinase activity and can be used as excellent markers of MAPK activity21. Therefore, we used MAPK phosphorylation as a readout of activation. In the present study, global cardiac ischemia caused the activation of p38 MAPK and p54/p46-JNK. After PSS (1–30 mg/L) treatment, however, we found that p38 MAPK and p54/p46-JNK activation was decreased in I/R rat hearts. The phosphorylated form of p44/p42-ERK remained unchanged in all of the groups.
In the cardiovascular system, ERKs are activated by growth factors, cytokines and so on, thereby mediating cell survival as well as cytoprotection15, 22. In contrast, JNKs and p38 MAPK are activated by cellular stresses, including oxidative stress, and they are thought to correlate with cardiomyocyte apoptosis and cardiac pathologies14. Evidence suggests that the p38 MAPK and JNK pathways have an important role in regulation of responses to cardiac I/R injury23, 24, 25. Inhibition of p38 activation results in improved myocardial function after I/R injury26. Our results suggested the possible role of JNK and p38 MAPK pathways in adaptive responses of myocardium to I/R injury. PSS administration can partially reverse the abnormal expression of members of the p38 MAPK and JNK pathways. The ERK pathway did not play a role in this pathological process with or without PSS treatment.
Cardiocytes themselves produce TNF-α in response to ischemia27, and TNF-α plays a critical role in myocardial dysfunction following acute injury28, 29, 30. In this study, we observed a significant increase in the TNF-α concentration in the isolated hearts after I/R. The application of PSS (1–30 mg/L) suppressed TNF-α protein production, which further illustrates the cardioprotective effect of PSS.
Recently, many investigators have indicated that MAPK is a key mediator in disease states characterized by inflammation31. Our results concurred with previous research that showed that acute injury resulted in changes in signal transduction through kinases such as p38 and JNK. This leads to increased expression of proinflammatory cytokines, such as TNF-α, which has been implicated in the pathogenesis of I/R related cardiac dysfunction30. Our observation of decreased p38 MAPK and p54/p46-JNK activation in I/R rat hearts after PSS treatment correlates with their decreased myocardial TNF-α production and myocardial function alterations. We therefore propose that the preserved cardiac function after PSS reperfusion may well be associated with the changes of p38 MAPK and JNK pathways and down-regulation of inflammatory activation.
In the present study, PSS treatment (1–30 mg/L) also caused an increase in coronary flow. Previous experiments showed a significant decrease in endothelial nitric oxide synthase messenger RNA expression after global cardiac ischemia. The addition of anti-TNF-α antibodies was shown to increase coronary flow and endothelial nitric oxide synthase messenger RNA expression32. This may represent an additional mechanism by which PSS can ameliorate postischemic recovery via inhibition of TNF-α production.
Therapeutic plasma concentrations of PSS in humans are 2–20 mg/L33. In our experiments, we observed cardiac arrest in the ischemic heart after reperfusion of PSS at concentrations over 30 mg/L. Moreover, concentrations below 1 mg/L may have no protective effect against I/R injury, as we did not observe any effect of PSS at 0.3 mg/L on I/R hearts. Therefore, the concentration of PSS that may exert a protective effect against I/R injury in isolated rat heart is 1–30 mg/L. Further studies are needed to explore the effective concentration in vivo.
The observation that PSS can protect the ex vivo ischemic and reperfused heart expands the spectrum of potentially favorable effects of PSS. This may have profound implications for early PSS administration in a variety of clinical conditions in which the heart is subjected to ischemia followed by reperfusion (acute coronary syndrome, coronary angioplasty, thrombolytic therapy, and cardiopulmonary bypass surgery). The beneficial effect of PSS treatment may be mediated through normalization of p38 MAPK and JNK pathway activity and inhibition of inflammatory cytokine production.
Author contribution
Ying YANG and Shen-jiang HU designed research; Ying YANG performed all the research; Liang LI and Guo-ping CHEN help to do part of the research; Ying YANG analyzed data and wrote the paper.
References
- Han ZY, Wang QA, Zeng GJ. Clinical and laboratory observations on polysaccharide sulphate (PSS) in 282 cases of ischemic cerebrovascular disease. Chin Med J (Engl) 1991;104:562–6. [PubMed] [Google Scholar]
- You Y, Xie HJ, Zhang YF, Liu ZJ, Yang QD. Effect of the P-selectin expression on cerebral blood flow in rats with cerebral ischemia-reperfusion injury. J Apoplexy Nervous Dis. 2005;22:155–7. [Google Scholar]
- Black SC, Gralinski MR, Friedrichs GS, Kilgore KS, Driscoll EM, Lucchesi BR. Cardioprotective effects of heparin or N-acetylheparin in an in vivo model of myocardial ischaemic and reperfusion injury. Cardiovasc Res. 1995;29:629–36. [PubMed] [Google Scholar]
- Gralinski MR, Driscoll EM, Friedrichs GS, DeNardis MR, Lucchesi BR. Reduction of myocardial necrosis after glycosaminoglycan administration: effects of a single intravenous administration of heparin or N-acetylheparin 2 hours before regional ischemia and reperfusion. J Cardiovasc Pharmacol Ther. 1996;1:219–28. doi: 10.1177/107424849600100305. [DOI] [PubMed] [Google Scholar]
- Park JL, Kilgore KS, Naylor KB, Booth EA, Murphy KL, Lucchesi BR. N-Acetylheparin pretreatment reduces infarct size in the rabbit. Pharmacology. 1999;58:120–31. doi: 10.1159/000028274. [DOI] [PubMed] [Google Scholar]
- Zhao MM, Li Z, Teng Z, Zhao JS, Yu XH, Watanabe Y, et al. Repeated oral treatment with polysaccharide sulfate reduces insulin resistance and dyslipidemia in diabetic dyslipidemic rat model. Yao Xue Xue Bao. 2007;42:488–91. [PubMed] [Google Scholar]
- Xie SQ, Du GJ, Ji BS, Lin HH, Xu QT, Hu XJ, et al. Effect of polysaccharide sulfate on brain environment after focal cerebral ischemia reperfusion in rat and its promotion for growth of the chick embryonic dorsal root ganglion. Chin Pharm J. 2006;41:33–6. [Google Scholar]
- Wu K, Qian WM, Wu P. Therapeutic effects of intravenous polysaccharide sulfate in treatment of coronary heart disease. Chin J Clin Pharmacol Ther. 1996;1:31–3. [Google Scholar]
- Bogoyevitch MA, Gillespie-Brown J, Ketterman AJ, Fuller SJ, Ben-Levy R, Ashworth A, et al. Stimulation of the stress-activated mitogen-activated protein kinase subfamilies in perfused heart. p38/RK mitogen-activated protein kinases and c-Jun N-terminal kinases are activated by ischemia/reperfusion. Circ Res. 1996;79:162–73. doi: 10.1161/01.res.79.2.162. [DOI] [PubMed] [Google Scholar]
- Maulik N, Yoshida T, Zu YL, Sato M, Banerjee A, Das DK. Ischemic preconditioning triggers tyrosine kinase signaling: a potential role for MAPKAP kinase 2. Am J Physiol. 1998;275:H1857–64. doi: 10.1152/ajpheart.1998.275.5.H1857. [DOI] [PubMed] [Google Scholar]
- Liao P, Wang SQ, Wang S, Zheng M, Zheng M, Zhang SJ, et al. p38 Mitogen-activated protein kinase mediates a negative inotropic effect in cardiac myocytes. Circ Res. 2002;90:190–6. doi: 10.1161/hh0202.104220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Sankula R, Tsai BM, Meldrum KK, Turrentine M, March KL, et al. P38 MAPK mediates myocardial proinflammatory cytokine production and endotoxin-induced contractile suppression. Shock. 2004;21:170–4. doi: 10.1097/01.shk.0000110623.20647.aa. [DOI] [PubMed] [Google Scholar]
- Lewis TS, Shapiro PS, Ahn NG. Signal transduction through MAP kinase cascades. Adv Cancer Res. 1998;74:49–139. doi: 10.1016/s0065-230x(08)60765-4. [DOI] [PubMed] [Google Scholar]
- Kyriakis JM, Avruch J. Sounding the alarm: protein kinase cascades activated by stress and inflammation. J Biol Chem. 1996;271:24313–6. doi: 10.1074/jbc.271.40.24313. [DOI] [PubMed] [Google Scholar]
- Wang X, Martindale JL, Liu Y, Holbrook NJ.The cellular response to oxidative stress: influences of mitogen-activated protein kinase signalling pathways on cell survival Biochem J 1998333(Pt 2): 291–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arumugam TV, Shiels IA, Woodruff TM, Granger DN, Taylor SM. The role of the complement system in ischemia-reperfusion injury. Shock. 2004;21:401–9. doi: 10.1097/00024382-200405000-00002. [DOI] [PubMed] [Google Scholar]
- Cain BS, Meldrum DR, Dinarello CA, Meng X, Joo KS, Banerjee A, et al. Tumor necrosis factor-alpha and interleukin-1beta synergistically depress human myocardial function. Crit Care Med. 1999;27:1309–18. doi: 10.1097/00003246-199907000-00018. [DOI] [PubMed] [Google Scholar]
- Maass DL, White J, Horton JW. IL-1beta and IL-6 act synergistically with TNF-alpha to alter cardiac contractile function after burn trauma. Shock. 2002;18:360–6. doi: 10.1097/00024382-200210000-00012. [DOI] [PubMed] [Google Scholar]
- Sakamoto A, Matsumura J, Mii S, Gotoh Y, Ogawa R. A prostaglandin E2 receptor subtype EP4 agonist attenuates cardiovascular depression in endotoxin shock by inhibiting inflammatory cytokines and nitric oxide production. Shock. 2004;22:76–81. doi: 10.1097/01.shk.0000129338.99410.5d. [DOI] [PubMed] [Google Scholar]
- Wright JG, Kerr JC, Valeri CR, Hobson RW., 2nd Heparin decreases ischemia-reperfusion injury in isolated canine gracilis model. Arch Surg. 1988;123:470–2. doi: 10.1001/archsurg.1988.01400280080014. [DOI] [PubMed] [Google Scholar]
- Marshall CJ. Specificity of receptor tyrosine kinase signaling: transient versus sustained extracellular signal-regulated kinase activation. Cell. 1995;80:179–85. doi: 10.1016/0092-8674(95)90401-8. [DOI] [PubMed] [Google Scholar]
- Sugden PH, Bogoyevitch MA. Intracellular signalling through protein kinases in the heart. Cardiovasc Res. 1995;30:478–92. [PubMed] [Google Scholar]
- Liao S, Porter D, Scott A, Newman G, Doetschman T, Schultz Jel J. The cardioprotective effect of the low molecular weight isoform of fibroblast growth factor-2: the role of JNK signaling. J Mol Cell. Cardiol. 2007;42:106–20. doi: 10.1016/j.yjmcc.2006.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milano G, Morel S, Bonny C, Samaja M, von Segesser LK, Nicod P, et al. A peptide inhibitor of c-Jun NH2-terminal kinase reduces myocardial ischemia-reperfusion injury and infarct size in vivo. Am J Physiol Heart Circ Physiol. 2007;292:H1828–35. doi: 10.1152/ajpheart.01117.2006. [DOI] [PubMed] [Google Scholar]
- Gao F, Yue TL, Shi DW, Christopher TA, Lopez BL, Ohlstein EH, et al. p38 MAPK inhibition reduces myocardial reperfusion injury via inhibition of endothelial adhesion molecule expression and blockade of PMN accumulation. Cardiovasc Res. 2002;53:414–22. doi: 10.1016/s0008-6363(01)00488-6. [DOI] [PubMed] [Google Scholar]
- Pantos C, Malliopoulou V, Paizis I, Moraitis P, Mourouzis I, Tzeis S, et al. Thyroid hormone and cardioprotection: study of p38 MAPK and JNKs during ischaemia and at reperfusion in isolated rat heart. Mol Cell Biochem. 2003;242:173–80. [PubMed] [Google Scholar]
- Kapadia S, Lee J, Torre-Amione G, Birdsall HH, Ma TS, Mann DL. Tumor necrosis factor-alpha gene and protein expression in adult feline myocardium after endotoxin administration. J Clin Invest. 1995;96:1042–52. doi: 10.1172/JCI118090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odeh M. Tumor necrosis factor-alpha as a myocardial depressant substance. Int J Cardiol. 1993;42:231–8. doi: 10.1016/0167-5273(93)90053-j. [DOI] [PubMed] [Google Scholar]
- Meldrum DR. Tumor necrosis factor in the heart. Am J Physiol. 1998;274:R577–95. doi: 10.1152/ajpregu.1998.274.3.R577. [DOI] [PubMed] [Google Scholar]
- Gurevitch J, Frolkis I, Yuhas Y, Paz Y, Matsa M, Mohr R, et al. Tumor necrosis factor-alpha is released from the isolated heart undergoing ischemia and reperfusion. J Am Coll Cardiol. 1996;28:247–52. doi: 10.1016/0735-1097(96)00105-2. [DOI] [PubMed] [Google Scholar]
- Stambe C, Atkins RC, Hill PA, Nikolic-Paterson DJ. Activation and cellular localization of the p38 and JNK MAPK pathways in rat crescentic glomerulonephritis. Kidney Int. 2003;64:2121–32. doi: 10.1046/j.1523-1755.2003.00324.x. [DOI] [PubMed] [Google Scholar]
- Paz Y, Frolkis I, Pevni D, Shapira I, Yuhas Y, Iaina A, et al. Effect of tumor necrosis factor-alpha on endothelial and inducible nitric oxide synthase messenger ribonucleic acid expression and nitric oxide synthesis in ischemic and nonischemic isolated rat heart. J Am Coll Cardiol. 2003;42:1299–305. doi: 10.1016/s0735-1097(03)00992-6. [DOI] [PubMed] [Google Scholar]
- Liu S, Wang CB, Guo SB, Yan YJ. The primary approach to untoward reactions and rational application of polysaccharide sulphate. Chin J Marine Drugs. 1992;11:17–9. [Google Scholar]