On the eve of the 40th anniversary of launching of the Expanded Programme on Immunization (EPI) in 1974, during the twenty-seventh World Health Assembly (WHA), fundamental questions about the level of financing needed to sustain achievements and scale up the EPI in low- and lower-middle income countries continue to permeate the discourse on the economics of immunization. The answer to this question is all the more important in light of the fact that at the sixty-fifth WHA in 2012, ministers of health embraced the Global Vaccine Action Plan (GVAP) – a 10-year global strategic plan for immunization.1 But how much – and in what areas – are the investments needed for this decade?
Today, improved transparency in pricing information allows for relatively accurate vaccine cost estimates.2 Unfortunately, trends in the health system costs of delivering vaccination beyond the cost of the vaccines themselves continue to be poorly understood. During the EPI’s first three decades of existence, they were fairly homogenous. The six basic antigens1 included in the EPI were inexpensive and health system inputs, such as the human resources for vaccination and the vaccine supply chain and logistics infrastructure, accounted for the largest share of total costs in country programmes.3 It was common knowledge that EPI vaccines represented 20% of overall investment in national immunization programmes in low- and lower-middle income countries.4
With the turn of the millennium came a paradigm shift away from this earlier established trend as countries began introducing new vaccines, such as the pentavalent vaccine, a five–in-one combination of the antigens against diphtheria, tetanus and pertussis with those against hepatitis B (HepB) and Haemophilus influenzae type b (Hib).2 During the period from 2000 to 2010, countries rapidly scaled up the use of pentavalent vaccine and, as a result, the total cost of country immunization programmes doubled or tripled.5 Recurrent investments in vaccines suddenly comprised the bulk of immunization programme costs: an average of more than 50% of total investments, and in many cases, well over this average.6 Part of the reason for this rise in the component of the total costs comprised by vaccines was that the incremental health system (i.e. non-vaccine) costs of introducing the pentavalent vaccine were marginal, since this product, despite adding two new antigens – HepB and Hib – to EPI schedules, required no more injections than the previously administered trivalent diphtheria–pertussis–tetanus (DPT) vaccine. In addition, pentavalent vaccines required little additional storage space in the vaccine cold chain.7
Looking ahead, the current decade will see the accelerated introduction into national EPI programmes of additional new, expensive, but highly effective vaccines, such as pneumococcal conjugate vaccine and the vaccines against rotavirus and human papilloma virus (HPV).3 These products are bulkier than the pentavalent vaccine and will require more cold chain storage space and more injections. The health system costs associated with delivering these newer vaccines are likely to outweigh the costs of the vaccines themselves – which reverses the trend in relative importance of vaccine to non-vaccine costs once again.
Investment in this decade
To gain insights into the investments needed to cover non-vaccine health system costs over the decade from 2011 to 2020, a needs-based costing exercise was undertaken by the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) as part of the work done by a multi-partner group of experts. The group calculated the overall investment for vaccination that will be required in 94 low- and lower-middle income countries over the period from 2011 to 2020, and the investment relative to 2010, the year used as the baseline.8
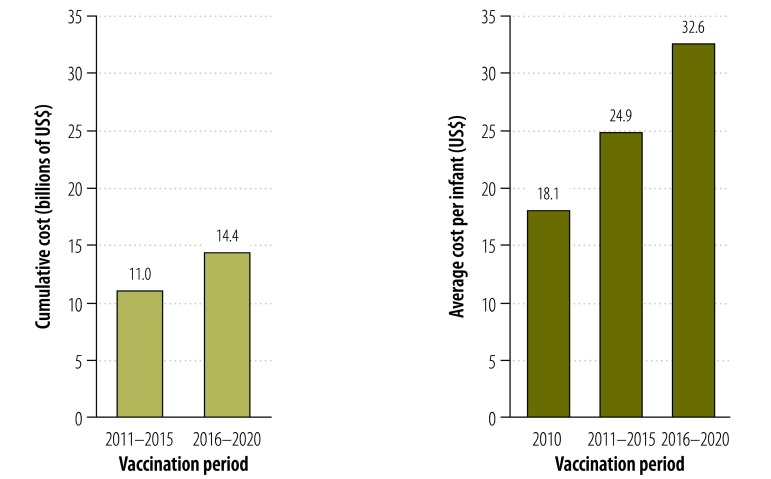
The estimated non-vaccine costs to the health system of delivering routine vaccination will require an investment of 25.4 billion United States dollars (US$) during this decade (Fig. 1). The average health system cost per child (as measured by the number of infants in the birth cohort) will rise from US$ 18.1 at baseline (2010) to US$ 24.9 during the period from 2011 to 2015 and to US$ 32.6 from 2016 to 2020. This almost amounts to a doubling of total health system costs over the current decade and to a tripling of such costs relative to the previous decade.
Fig. 1.
Delivery (i.e. non-vaccine) health system costs of routine vaccination, absolute values and average cost per child, 2010–2020
US$, United States dollars.
In reviewing the annual trend over the decade from 2011 to 2020, the annual peak of US$ 3.0 billion observed midway suggests both a doubling of needs from the 2010 baseline estimate, and that capital investments in infrastructure should be front-loaded in the earlier years of the decade to ensure that countries are ready to introduce new vaccines as planned and to expand access to quality vaccination services. Such a profile is consistent with the expected performance targets and peaks in demand for pneumococcal, rotavirus and HPV vaccines,8 as well as with estimates from the global investment framework for women and children’s health.9
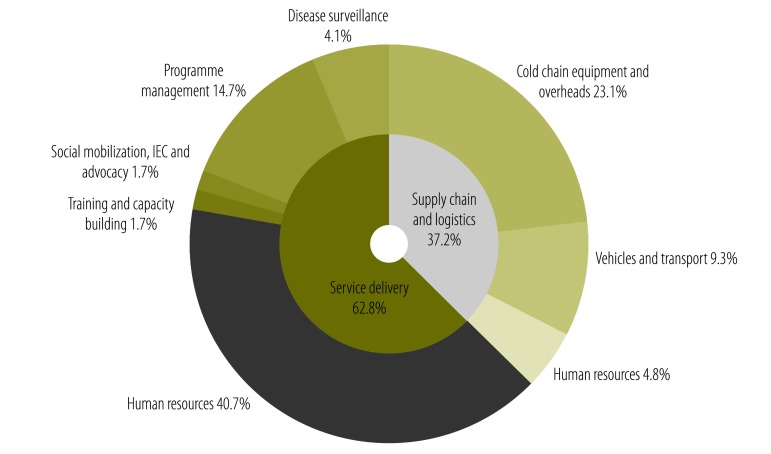
A detailed review of the composition of costs reveals that investments in the components that are needed for service delivery represent 63% of total investments (Fig. 2). The remaining 37% is comprised of measures to ensure the uninterrupted availability of vaccines and supplies at the service delivery levels throughout vaccination supply chains. A deeper look into these cost categories underscores the importance of investing in human resources – for service delivery and supply chains – and in cold chain infrastructure, particularly at the subnational and last-mile levels. Together, these two cost categories represent nearly 70% of the overall US$ 25.4 billion required during this decade.
Fig. 2.
Breakdown of the delivery (i.e. non-vaccine) health systems costs of routine vaccination
IEC, Information, education and communication.
Human resources and supply chain strengthening
Like any public health programme, routine vaccination services critically depend on the skills and commitment of a strong, sufficient health workforce. Existing evidence points to a global shortage of health workers worldwide, and particularly in low- and lower-middle income countries.10 This shortage undermines the EPI because the need for human resource sharing in the health system is such that the same health worker is often expended across multiple programmes, including vaccination services.11 It is no surprise that substantial increases in full-time equivalent staff for vaccination represents the better part of projected non-vaccine health system investments.
Although the success of the EPI over the past 40 years can be attributed in large measure to the reach of vaccination supply chains, recent findings have cast light on the critical weaknesses of the supply chain in most countries.12 Much of the infrastructure was developed 30 years ago and has not kept pace with today’s needs and immunization priorities. During the past decade, little attention and funding have been devoted to the upkeep of in-country vaccination supply chains, despite enduring challenges in vaccine storage, distribution, handling and stock control.13 Coupled with the growing complexities of this decades’ EPI as newer vaccines and delivery strategies, as outlined in the GVAP, are deployed, vaccination supply chains are under intense pressure to adapt, innovate and scale up. Recent studies suggest that, if countries continue with “business as usual”, vaccination supply chains will thwart the attainment of this decade’s immunization goals.14 The urgent need to address this bottleneck explains why this cost component represents the second largest non-vaccine cost driver.
Policy and practice implications
As the world celebrates the 40th anniversary of the launching of the EPI, many of the poorest countries are embarking on an ambitious strategy, in alignment with the GVAP. The purpose of the strategy is to sustain the achievements of past decades in the area of immunization and further expanding them by adopting new vaccines, reducing coverage gaps in routine vaccination by addressing inequities in access, and protecting people against vaccine-preventable diseases beyond childhood.15 But in addition to investing in vaccines, it is critical to renew investments in strengthening the ability of health systems to deliver vaccines and vaccination services and in ensuring that systems are sufficiently resilient. The findings from this WHO and UNICEF analysis clearly highlight the need for substantial front-loaded investment beyond the vaccines themselves if the goals established for this decade are to be met. Contrary to the trends observed in the last decade, when the EPI was expanded to include the pentavalent vaccine, in the current decade non-vaccine costs will make up a greater proportion of the needed investment. This conflicts with the widely accepted view that vaccines, and particularly new ones, represent the lion’s share of routine vaccination costs in the poorest countries. System investments for vaccination delivery will supersede investments in the vaccines themselves, despite the higher cost of many new vaccine products.
From a policy and practice perspective, these findings highlight the imperative this decade to strengthen human resources and the immunization supply chain at all levels of the health system – this is the backbone of routine immunization programmes in low- and lower-middle income countries. The key challenge will be mobilizing the resources to finance non-vaccine immunization components in each country. Doing so is no small feat. Securing funds to cover non-vaccine costs has always been more difficult than getting national or international funding to pay for the vaccines. According to projections of future financial flows for vaccination in 2011 to 2020, 65% of the need for routine vaccination will not be met.8 Strategies to fill the expected funding gaps are all the more pressing because of the impact that front-loading investments in earlier years would exert on countries’ readiness to introduce new vaccines and because achieving certain infrastructural improvements can take several years. The EPI’s continued success and the health and economic benefits that immunization will confer during the decade from 2011 to 2020 will hinge on sufficient financing of the non-vaccine components of routine vaccination services. Failing to mobilize adequate resources to finance these critical programme components will seriously compromise the ability of low- and lower-middle income countries to meet the targets of this decade’s Global Vaccine Action Plan.
Competing interests:
None declared.
References
- 1.World Health Organization [Internet]. World Health Assembly endorsed the Global Vaccine Action Plan and World Immunization Week (WHO press release). 2012 May 25. Geneva: WHO; 2014. Available from: http://www.who.int/immunization/newsroom/global_vaccine_action_plan/en/ [accessed 20 January 2014].
- 2.United Nations Children’s Fund [Internet]. Supplies and logistics: vaccine price data New York: UNICEF; 2014. Available from: http://www.unicef.org/supply [accessed 20 January 2014].
- 3.Khaleghian P. Immunization financing and sustainability: a review of the literature (Special Initiatives Report No. 40). Bethesda: Partnerships for Health Reform Project, Abt Associates Inc.; 2001.
- 4.State of the world's vaccines and immunization 2nd ed. Geneva: World Health Organization; 2002. Available from: http://www.who.int/immunization/sowvi/en/ [accessed 3 February 2014]. [Google Scholar]
- 5.Lydon P, Levine R, Makinen M, Brenzel L, Mitchell V, Milstien JB, et al. Introducing new vaccines in the poorest countries: what did we learn from the GAVI experience with financial sustainability? Vaccine. 2008;26:6706–16. doi: 10.1016/j.vaccine.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Kamara L, Lydon P, Bilous J, Vandelaer J, Eggers R, Gacic-Dobo M, et al. Global Immunization vision and strategy (GIVS): a mid-term analysis of progress in 50 countries. Health Policy Plan. 2012;27:1–9. doi: 10.1093/heapol/czs020. [DOI] [PubMed] [Google Scholar]
- 7.Griffiths UK, Korczak VS, Ayalew D, Yigzaw A. Incremental system costs of introducing combined DTwP-hepatitis B-Hib vaccine into national immunization services in Ethiopia. Vaccine. 2009;27:1426–32. doi: 10.1016/j.vaccine.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 8.Gandhi G, Lydon P, Cornejo S, Brenzel L, Wrobel S, Chang H. Projections of the costs, financing and possible funding gaps across low and lower middle income country immunization programmes over the decade, 2011-2020. Vaccine. 2013;31S:B137–48. doi: 10.1016/j.vaccine.2013.01.036. [DOI] [PubMed] [Google Scholar]
- 9.Stenberg K, Axelson H, Sheehan P, Anderson I, Gülmezoglu AM, Temmerman M, et al. Advancing social and economic development by investing in women’s and children’s health: a new global investment framework. Lancet. 2013;11:S0140-6736(13)62231-X. doi: 10.1016/S0140-6736(13)62231-X. [DOI] [PubMed] [Google Scholar]
- 10.World health report 2006: working together for health Geneva: World Health Organization; 2006. Available from: http://www.who.int/whr/2006 [accessed 20 January 2014].
- 11.Anand S, Bärnighausen T. Health workers and vaccination coverage in developing countries: an econometric analysis. Lancet. 2007;369:1277–85. doi: 10.1016/S0140-6736(07)60599-6. [DOI] [PubMed] [Google Scholar]
- 12.Humphreys G. Vaccination: rattling the supply chain [news]. Bull World Health Organ. 2011;89:324–5. doi: 10.2471/BLT.11.030511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sabot O, Yadav P, Zaffran M. Maximizing every dose and dollar: the imperative of efficiency in vaccine delivery (NBAR Impact & Innovation Series) Seattle: The National Bureau of Asian Research; 2011. Available from: http://www.nbr.org/downloads/pdfs/CHA/CHA_MazimizingEveryDoseandDollar.pdf [accessed 20 January 2014].
- 14.Zaffran M, Vandelaer J, Kristensen D, Melgaard B, Yadav P, Antwi-Agyei KO, et al. The imperative for stronger vaccine supply and logistics systems. Vaccine. 2013;31(Suppl 2):B73–80. doi: 10.1016/j.vaccine.2012.11.036. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization [Internet]. Global Vaccine Action Plan 2011–2020. Geneva: WHO; 2013. Available from: http://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/ [accessed 20 January 2014].