Abstract
Although smoking deprivation is often used in laboratory studies to induce urges to smoke cigarettes, the optimal length of deprivation has not been established. Previous research showed that overnight abstinence from cigarettes led to high baseline urge to smoke that potentially masked alcohol’s acute effects on urge to smoke (Kahler et al., 2012). The current study examined whether alcohol’s effects on smoking urge were more pronounced when a shorter length of smoking deprivation was used (i.e., 3 hour instead of overnight abstinence). Using a balanced placebo design for alcohol administration, we found that participants experienced a significant increase in self-reported urge to smoke when administered alcohol after a 3-hour smoking deprivation (N=32), whereas this effect was smaller and nonsignificant when smokers were required to be abstinent overnight (N = 96). Research on factors that heighten smoking urges may find stronger effects if a 3-hour deprivation is used compared to using overnight abstinence.
Keywords: alcohol, urge, smoking, balanced placebo design
1. Introduction
Relapse to smoking often occurs in the context of alcohol consumption (Borland, 1990; Kahler, Spillane & Metrik, 2010), although the reasons for this are not clear. To understand the links between acute alcohol intoxication and subsequent smoking, laboratory studies have been developed. These studies, which measure how alcohol and other experimental factors impact urge to smoke, typically use a smoking deprivation period prior to alcohol administration or another experimental manipulation to ensure that participants are not sated (Ashare & McKee, 2012; Colby et al., 2004; Cooney et al., 2003; Leeman et al., 2010; Harrison, Coppola & McKee, 2009; Kahler et al., 2012; Palfai et al., 2000). However, the optimal length of smoking deprivation to use in such studies has not been established. There is reason to believe the length of smoking deprivation may influence results, with longer periods of deprivation potentially resulting in a ceiling effect (Kahler et al., 2009; Kahler et al., 2012); that is, if participants are already experiencing a near-maximal level of urge to smoke, there may be little room for additional increments to that urge. For example, previous studies demonstrated an acute effect of alcohol on smoking urge in the context of a 3-hour smoking deprivation (McKee et al., 2006; McKee et al. 2009), whereas a laboratory study requiring overnight smoking abstinence did not find a significant acute pharmacologic or expectancy effect of alcohol on cigarette urge (Kahler et al., 2012).
We know of no attempts to compare directly the effects of alcohol on urge to smoke following 3 hr vs. overnight cigarette abstinence. Establishing the optimal period of smoking abstinence is important for the design of future lab studies on alcohol’s impact on smoking as well as other acute experimental procedures aimed at eliciting smoking urges. In addition, this knowledge can inform models of how alcohol use contributes to smoking lapse at different stages of a smoking cessation attempt.
1.1. Aims and Hypotheses
We conducted a study mirroring that of Kahler et al. (2012) using 3 hr instead of overnight abstinence. We compared the acute effects of alcohol on self-reported urge to smoke cigarettes in the new sample relative to the effects in the Kahler et al. (2012) study. We hypothesized that the sample using a short abstinence period (3 hr) would show lower levels of initial urge to smoke and greater increases in urge following alcohol administration.
2. Method
2.1. Participants
The Brown University Institutional Review Board approved this study. Inclusion and exclusion criteria and procedures were identical to those used in Kahler et al. (2012), except for length of nicotine deprivation. Participants were community members who met the following inclusion criteria: 21 to 65 years of age, smoking 10–30 cigarettes a day, a carbon monoxide (CO) level >10 ppm, current heavy drinking (≥5 drinks per occasion for men, ≥4 drinks for women) at least twice a month, and reported no history or intention to seek alcohol treatment. Exclusion criteria were: using nicotine replacement therapy or other tobacco product, planning to quit smoking in the next month, incapable of abstaining from alcohol for 24 h without significant withdrawal symptoms, current affective disorder or psychotic symptoms; illicit drug use on more than four occasions in the past 4 weeks, current pregnancy or nursing, medical issues or medications contraindicated for alcohol consumption, weighing greater than 250 lbs, and prior knowledge about study procedures or contact with study participants.
Those who met eligibility criteria completed a single experimental session (n=32). During informed consent, participants were informed that the study evaluated effects of alcohol on smoking behavior and that they would be randomly assigned to consume a beverage containing alcohol or a nonalcoholic beverage.
2.2. Design
Complete details on study design are presented in Kahler et al. (2012). In both studies we used a 2×2 balanced placebo design crossing alcohol administration (0.4 g/kg of alcohol or placebo) with beverage content instructions (told alcohol or told placebo). Designs differed only in length of deprivation period (3 vs. 15 hours), and we performed analyses on the combined sample of the current study and Kahler et al 2012 sample, using length of deprivation as an independent variable in these analyses. Research assistants were blind to the alcohol content of the beverage.
2.3. Procedure
Participants completed interview and self-report assessments including demographics, diagnostic interview, and smoking and alcohol use questions. Participants were instructed to refrain from drinking alcohol for 24 h prior to both sessions, confirmed by a zero breath alcohol concentration (BrAC) per an Alco-Sensor IV (Intoximeters, Inc., St Louis, MO, USA) upon arrival. Participants were instructed not to eat any solid foods within 4 h or drink any liquids within 2 h prior to the session. In Kahler et al. (2012), participants were instructed to abstain from smoking overnight before the session, which was verified by a reduction in carbon monoxide levels of at least 50% relative to baseline. In the current study, participants were allowed to smoke ad libitum prior to the session, were provided a small meal, and then smoked in the lab, exactly 3 hours before alcohol administration. All sessions occurred in a ventilated smoking room with a one-way mirror window.
Participants completed measures of urge to smoke immediately prior to beverage administration (Time 1), and a second measure of urge to smoke 42 minutes after starting drinking (Time 2). Participants who received alcohol received a drink that contained a 5:1 ratio of fresh tonic/vodka, and those who received placebo received a drink that contained 5:1 ratio of fresh tonic/flat tonic (0.0 g/kg). Participants had to consume each of three drinks over 15 total minutes (5 minutes per drink).
2.4. Measures
2.4.1
Demographic and substance use characteristics were assessed using a self-report measure.
2.4.2
Alcohol dependence was measured via Structured Clinical Interview for DSM-IV (SCID; First et al., 1995).
2.4.3
Urge to smoke was assessed using the Brief Questionnaire of Smoking Urges (Cox, Tiffany, & Christen, 2001). This well-validated measure includes 10 items that assess urges to smoke for either positive reinforcement (Factor 1) or negative reinforcement (Factor 2). Previous work has shown that Factor 1 is more strongly affected by alcohol administration than Factor 2 (King & Epstein, 2005; Kahler et al., 2012), so it was selected for analysis in this study.
2.5. Data Analysis Plan
Baseline differences in demographic and substance use characteristics between the current study and the Kahler et al. (2012) sample were run using independent samples t-tests and chi-square tests. To test the effect of deprivation period on urge to smoke, we ran regression analyses with the combined sample (Kahler et al., 2012 and the 3 hr sample), covarying Time 1 B-QSU. We included length of deprivation, the dummy-coded main effect of received alcohol vs. received placebo, and the dummy-coded main effect of told alcohol vs. told placebo as predictors of change in B-QSU from Time 1 to Time 2. We also included the interactions between length of deprivation and both told alcohol and received alcohol. We then ran regression analyses within each sample to determine whether Time 1 B-QSU, receiving alcohol or being told alcohol had an effect on urge to smoke.
3. Results
3.1. Participant characteristics
Participants in the 3 hr sample were, on average, 38.5 years old (SD=13.9), had received 13.7 years of education (SD=2.1), smoked 18 cigarettes smoked per day (SD=5.6), drank 43.8% of the prior 90 days (SD=26.8%), drank 6 drinks per drinking day (SD=3.3), and were mostly White (81.3%), not married or cohabiting (71.9%), and employed (56%). This sample was very similar to the Kahler et al. (2012) sample, differing significantly only in terms of current DSM-IV alcohol dependence (0% in current sample; 7.3% in Kahler et al., 2012). However, this variable was not correlated with our outcome variable, so it was excluded from all further analyses. No participants reported feeling deceived by the beverage they drank.
3.2. Urge to smoke
In the combined sample, Time 1 urge to smoke significantly predicted Time 2 urge to smoke. The interaction of length of deprivation and receiving alcohol approached significance, which indicated that the effect of receiving alcohol on urge to smoke was stronger in the short deprivation sample compared to the long deprivation sample (see Table 1).
Table 1.
Linear regression predicting urge to smoke
| Predictor | B | SE (B) | sr2 | p |
|---|---|---|---|---|
| Combined Sample (N=128) | ||||
| Time 1 Urge | .92 | .07 | .61 | <.01 |
| Told Alcohol | .17 | .33 | <.01 | .62 |
| Received Alcohol | .62 | .33 | .01 | .06 |
| Long Deprivation | .01 | .33 | <.01 | .96 |
| Told Alcohol × Long Deprivation | −.35 | .38 | <.01 | .40 |
| Received Alcohol × Long Deprivation | −.75 | .38 | .01 | .052 |
| Kahler et al., 2012 sample (N=96) | ||||
| Time 1 Urge | .95 | .08 | <.01 | |
| Told Alcohol | −.15 | .20 | .52 | |
| Received Alcohol | −.13 | .20 | .42 | |
| Current Study (N=31) | ||||
| Time 1 Urge | .85 | .10 | <.01 | |
| Told Alcohol | .18 | .26 | .50 | |
| Received Alcohol | .59 | .27 | .035 | |
Note. Told Alcohol, Received Alcohol, and Long Deprivation are dummy coded, 0 vs. 1. Label describes participants with a value of 1. Total R2 in combined sample=.634. Total R2 in Kahler et al. (2012) sample=.583. Total R2 in 3 hr study=.746.
When examining the samples separately, among those participants who experienced long deprivation (Kahler et al., 2012), Time 1 urge to smoke predicted greater Time 2 urge, but having received alcohol or been told alcohol did not significantly predict Time 2 urge. In the 3 hr sample, having been told alcohol did not significantly predict urge, but both Time 1 urge and receiving alcohol significantly predicted greater Time 2 urge.
4. Discussion
Previously, we found that there was no effect of having been told alcohol or having received alcohol on urge to smoke in a balanced placebo design (Kahler et al., 2012). We speculated that this was because participants had abstained from smoking overnight, which contributed to ceiling effects on urge at the time of the experimental session. Using the same balanced placebo design, we shortened the length of deprivation to only 3 hours and found that self-reported urge to smoke at Time 1 was lower for those participants who underwent the shorter deprivation period as compared to those with overnight abstinence. We hypothesized that these lower baseline urge ratings would result in greater effects of alcohol on urge to smoke. Indeed, we found that in the 3 hr sample, having received alcohol was associated with greater urge to smoke.
This finding has methodological implications. There are several laboratory methods that intend to elicit smoking urge (e.g., cue reactivity, stress paradigms), and there is variability in how long participants are asked to abstain from smoking prior to experimental sessions. This is the first paper of which we are aware to provide empirical evidence for researchers regarding how length of smoking deprivation period influences the consequences of experimental manipulations such as alcohol administration.
In addition to methodological implications, these findings suggest that urge might be a mechanism by which alcohol exerts its effects on smoking relapse. There have been several laboratory based studies that provide evidence that alcohol consumption contributes to increases in urge to smoke among smokers (Burton & Tiffany, 1997; Businelle et al., 2013; Epstein et al., 2007; King, McNamara, Conrad & Cao, 2009), and urge to smoke has been shown to mediate the link between alcohol use and smoking relapse (Hendricks, Delucchi, Humfleet, & Hall, 2012). The current study is the first to provide support for the pharmacological, and not expectancy, effects of alcohol being the mechanism that contributes to urge to smoke, which may ultimately contribute to smoking relapse.
There are also potential clinical implications. For individuals early in a quit attempt (those who have recently smoked), urge may be more susceptible to fluctuations following alcohol consumption; it also may be that when people have been abstinent from cigarettes long enough that craving begins to diminish, alcohol rekindles the urge to smoke. However, these participants were not attempting to quit smoking. In order to determine the clinical relevance of this phenomenon it would be useful for future work to focus on collecting event-level data in order to determine how urge fluctuates early in a quit attempt when alcohol is consumed. One study using ecological momentary assessment found that urge to smoke was a significant predictor of smoking lapse after at least 24 hours of smoking abstinence (Holt et al., 2012); these findings could be replicated and extended to include the influence of alcohol on urge and subsequent relapse.
There also may be value in examining the extent to which individuals are responding to the expectancy versus pharmacologic effects of smoking prior to alcohol administration, as it may be possible to administer nicotine in another way (e.g., nicotine gum) prior to alcohol consumption in order to limit expectancy effects of alcohol while managing the high levels of urge that accompany long deprivation.
4.1. Limitations
Although this study had several strengths, there are limitations worth noting. The sample size of participants who experienced the short deprivation period was small (n=32), which limited our ability to look for potential moderators of alcohol’s effects. For example, we previously found that women were more sensitive than men to the expectancy effects of alcohol and its contribution to smoking lapse (Kahler et al., 2012); however, examining gender as a moderator of the current findings would lead to overly small cell sizes. In addition, the current study used a quasi-experimental design lacking randomization to short vs. long smoking deprivation; we did not test higher doses of alcohol, there may be limited generalizability of the vodka-tonic beverage, and we did not use a sample of smokers who wished to quit, which may have influenced results.
4.2. Conclusions
The findings of the current study are relevant for methodology of laboratory-based studies of smoking, and provide evidence that a shorter deprivation period prior to experimental manipulation might result in greater effects on smoking urge. Second, the pharmacologic and not expectancy effects of alcohol may be the mechanism by which alcohol use leads to smoking urge.
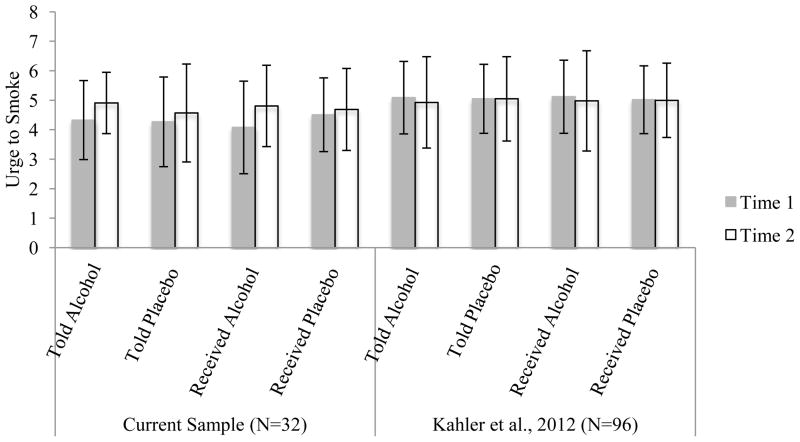
Figure 1.
Self-reported urge to smoke across conditions in balanced placebo design
Note: Time 1=immediately drink administration, 3 hrs after last cigarette; Time 2=42 minutes after drink administration began; cells reflect averages irrespective of crossed condition (e.g., told alcohol average takes into account those who received alcohol and placebo).
Highlights.
Previous work from our laboratory found no effect of alcohol on urge to smoke.
We hypothesized that this was due to a ceiling effect of urge after overnight smoking deprivation.
The current study used an identical design with only 3 hours of smoking deprivation.
Participants who received alcohol experienced an increase in urge to smoke.
3 hours of smoking deprivation appears useful in studies of alcohol’s effect on smoking variables
Acknowledgments
Role of Funding Source
This study was funded by the National Institute on Alcohol Abuse and Alcoholism grant R01AA016978 to Dr. Kahler, by a Senior Research Career Scientist award from the Department of Veterans Affairs to Dr. Rohsenow, by T32 AA007459 from the National Institute of Alcohol Abuse and Alcoholism; and by K08 DA029094 from the National Institute on Drug Abuse awarded to Nichea Spillane.
Footnotes
Contributors
Authors Kahler and Day designed this study and author Kahler designed, wrote the protocol, and collected the data for the laboratory study. Author Rohsenow contributed to the design, interpretation, and writing. Author Kahler undertook the statistical analysis, and author Day and wrote the first draft of the manuscript, with editing by all authors. All authors contributed to and have approved the final manuscript.
Conflict of Interest
The authors have no conflicts of interest to report. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ashare RL, McKee SA. Effects of varenicline and bupropion on cognitive processes among nicotine-deprived smokers. Experimental And Clinical Psychopharmacology. 2012;20(1):63–70. doi: 10.1037/a0025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R. Slip-ups and relapse in attempts to quit smoking. Addictive Behaviors. 1990;15:235–245. doi: 10.1016/0306-4603(90)90066-7. [DOI] [PubMed] [Google Scholar]
- Burton SM, Tiffany ST. The effect of alcohol consumption on craving to smoke. Addiction. 1997;92(1):15–26. doi: 10.1111/j.1360-0443.1997.tb03634.x. [DOI] [PubMed] [Google Scholar]
- Businelle MS, Lam CY, Kendzor DE, Cofta-Woerpel L, McClure JB, Cinciripini PM, Wetter DW. Alcohol consumption and urges to smoke among women during a smoking cessation attempt. Experimental And Clinical Psychopharmacology. 2013;21(1):29–37. doi: 10.1037/a0031009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colby SM, Rohsenow DJ, Monti PM, Gwaltney CJ, Gulliver SB, Abrams DB, Sirota AD. Effects of tobacco deprivation on alcohol cue reactivity and drinking among young adults. Addictive Behaviors. 2004;29(5):879–892. doi: 10.1016/j.addbeh.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Cooney JL, Cooney NL, Pilkey DT, Kranzler HR, Oncken CA. Effects of nicotine deprivation on urges to drink and smoke in alcoholic smokers. Addiction. 2003;98(7):913–921. doi: 10.1046/j.1360-0443.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- Cox LS, Tiffany ST, Christen AG. Evaluation of the brief questionnaire of smoking urges (QSU-brief) in laboratory and clinical settings. Nicotine Tob Res. 2001;3(1):7–16. doi: 10.1080/14622200020032051. [DOI] [PubMed] [Google Scholar]
- Epstein AM, Sher TG, Young MA, King AC. Tobacco chippers show robust increases in smoking urge after alcohol consumption. Psychopharmacology. 2007;190(3):321–329. doi: 10.1007/s00213-006-0438-8. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- Harrison ER, Coppola S, McKee SA. Nicotine deprivation and trait impulsivity affect smokers’ performance on cognitive tasks of inhibition and attention. Experimental And Clinical Psychopharmacology. 2009;17(2):91–98. doi: 10.1037/a0015657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks PS, Delucchi KL, Humfleet GL, Hall SM. Alcohol and marijuana use in the context of tobacco dependence treatment: Impact on outcome and mediation of effect. Nicotine & Tobacco Research. 2012;14(8):942–951. doi: 10.1093/ntr/ntr312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt LJ, Litt MD, Cooney NL. Prospective analysis of early lapse to drinking and smoking among individuals in concurrent alcohol and tobacco treatment. Psychology Of Addictive Behaviors. 2012;26(3):561–572. doi: 10.1037/a0026039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Metrik J, Spillane NS, Leventhal AM, McKee SA, Tidey JW, Rohsenow DJ. Sex differences in stimulus expectancy and pharmacologic effects of a moderate dose of alcohol on smoking lapse risk in a laboratory analogue study. Psychopharmacology. 2012;222(1):71–80. doi: 10.1007/s00213-011-2624-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Leventhal AM, Colby SM, Gwaltney CJ, Kamarck TW, Monti PM. Hostility, cigarette smoking, and responses to a lab-based social stressor. Experimental and Clinical Psychopharmacology. 2009;17(6):413. doi: 10.1037/a0017690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Spillane NS, Metrik J. Alcohol use and initial smoking lapses among heavy drinkers in smoking cessation treatment. Nicotine & Tobacco Research. 2010;12:781–785. doi: 10.1093/ntr/ntq083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Epstein AM. Alcohol Dose-Dependent Increases in Smoking Urge in Light Smokers. Alcoholism: Clinical And Experimental Research. 2005;29(4):547–552. doi: 10.1097/01.ALC.0000158839.65251.FE. [DOI] [PubMed] [Google Scholar]
- King A, McNamara P, Conrad M, Cao D. Alcohol-induced increases in smoking behavior for nicotinized and denicotinized cigarettes in men and women. Psychopharmacology. 2009;207(1):107–117. doi: 10.1007/s00213-009-1638-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman RF, McKee SA, Toll BA, Krishnan-Sarin S, Cooney JL, Makuch RW, O’Malley SS. Risk factors for treatment failure in smokers: Relationship to alcohol use and to lifetime history of an alcohol use disorder. Nicotine & Tobacco Research. 2008;10(12):1793–1809. doi: 10.1080/14622200802443742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman RF, O’Malley SS, White MA, McKee SA. Nicotine and food deprivation decrease the ability to resist smoking. Psychopharmacology. 2010;212(1):25–32. doi: 10.1007/s00213-010-1902-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA. Developing human laboratory models of smoking lapse behavior for medication screening. Addiction Biology. 2009;14(1):99–107. doi: 10.1111/j.1369-1600.2008.00135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA, Harrison ER, Shi J. Alcohol expectancy increases positive responses to cigarettes in young, escalating smokers. Psychopharmacology. 2010;210(3):355–364. doi: 10.1007/s00213-010-1831-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA, Krishnan-Sarin S, Shi J, Mase T, O’Malley SS. Modeling the effect of alcohol on smoking lapse behavior. Psychopharmacology. 2006;189(2):201–210. doi: 10.1007/s00213-006-0551-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA, Sinha R, Weinberger AH, Sofuoglu M, Harrison ER, Lavery M, Wanzer J. Stress decreases the ability to resist smoking and potentiates smoking intensity and reward. Journal Of Psychopharmacology. 2011;25(4):490–502. doi: 10.1177/0269881110376694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palfai TP, Monti PM, Ostafin B, Hutchison K. Effects of nicotine deprivation on alcohol-related information processing and drinking behavior. Journal Of Abnormal Psychology. 2000;109(1):96–105. doi: 10.1037/0021-843X.109.1.96. [DOI] [PubMed] [Google Scholar]
- Sayette MA, Martin CS, Wertz JM, Perrott MA, Peters AR. The effects of alcohol on cigarette craving in heavy smokers and tobacco chippers. Psychology Of Addictive Behaviors. 2005;19(3):263–270. doi: 10.1037/0893-164X.19.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Fischer LA, Paty JA, Gnys M, Hickcox M, Kassel JD. Drinking and smoking: a field study of their association. Ann Behav Med. 1994;16:203–209. [Google Scholar]
- Shiffman S, Gwaltney CJ, Balabanis MH, Liu KS, Paty JA, Kassel JD, Gnys M. Immediate antecedents of cigarette smoking: An analysis from ecological momentary assessment. Journal Of Abnormal Psychology. 2002;111(4):531–545. doi: 10.1037/0021-843X.111.4.531. [DOI] [PubMed] [Google Scholar]
- Van Zundert RP, Kuntsche E, Engels RE. In the heat of the moment: Alcohol consumption and smoking lapse and relapse among adolescents who have quit smoking. Drug And Alcohol Dependence. 2012;126(1–2):200–205. doi: 10.1016/j.drugalcdep.2012.05.016. [DOI] [PubMed] [Google Scholar]