Abstract
Objectives
To determine women's knowledge of contraceptive effectiveness.
Study Design
We performed a cross-sectional analysis of a contraceptive knowledge questionnaire completed by 4,144 women enrolled in the Contraceptive CHOICE Project prior to receiving comprehensive contraceptive counseling and choosing their method. For each contraceptive method, women were asked “what percentage would get pregnant in a year: <1%, 1-5%, 6-10%, >10%, don't know.”
Results
Overall, 86% of subjects knew the annual risk of pregnancy was >10% if no contraception is used. More than 45% of women overestimate the effectiveness of depo-medroxyprogesterone acetate, pills, patch, ring, and condoms. After adjusting for age, education and contraceptive history, women who chose the intrauterine device (IUD) [RRadj=6.9, 95% CI: 5.6-8.5] or implant [RRadj = 5.9, 95% CI 4.7-7.3] were significantly more likely to accurately identify the effectiveness of their method compared to women who chose either the pill, patch, or ring.
Conclusions
This cohort demonstrated significant knowledge gaps regarding contraceptive effectiveness and over-estimated the effectiveness of pills, patch, ring, DMPA, and condoms.
Keywords: Contraception effectiveness, Contraception failure, Contraception knowledge
Introduction
Many factors influence women's decisions regarding contraceptive methods.1, 2 Knowledge of a contraceptive method's effectiveness can be an important factor in a woman's choice of method.1, 2 General contraceptive knowledge varies widely across populations with notable disparities among minority and younger populations who have less awareness and understanding of various contraceptive methods.1-3 Multiple studies have evaluated women's knowledge of a specific contraceptive method, such as the intrauterine device (IUD),1, 2, 4 or evaluated the knowledge of women in countries outside the United States5, 6.
Among women using reversible contraception, most choose less effective methods such as condoms (26%) and oral contraceptive pills (45%).7 Reliance on less effective methods contributes to the fact that nearly half of all pregnancies in the United States are unintended.8 Recently published data from the National Survey of Family Growth show an increase in the use of long-acting reversible contraceptives (LARC) which include IUDs and implants.7, 9 LARC are not only the most effective methods, but appear to provide the highest satisfaction and rate of continuation among users.10
Promoting use of the most effective contraceptive methods requires an assessment of what women who desire reversible contraception know about the effectiveness of the available methods. The primary objective of this analysis was to determine the knowledge of contraceptive effectiveness among a cohort of St. Louis women enrolled in the Contraceptive CHOICE Project. Our secondary objective was to assess whether women choosing LARC methods had better knowledge regarding the effectiveness of their own method prior to contraceptive counseling compared to women who chose the pill, patch, or ring.
Materials and Methods
The Contraceptive CHOICE Project (CHOICE) is a prospective cohort study developed to promote the use of LARC methods in the St. Louis region. The methods for CHOICE have been previously published,11 but a brief description is provided below. The CHOICE protocol was approved by the Washington University in St. Louis School of Medicine Human Research Protection Office prior to the initiation of recruitment.
CHOICE is a convenience sample of women in St. Louis City and County who desire reversible contraception. The primary objective of CHOICE is to promote the use of LARC and provide no-cost contraception to a large number of women in the St. Louis region in an effort to reduce unintended pregnancies. Participants are recruited from clinics serving women at high risk for unintended pregnancy and sexually transmitted infections (STIs), as well as from the local community through word-of-mouth. Recruitment occurs via general awareness about the CHOICE Project through general and reproductive health clinics, referring healthcare providers, newspaper reports, and study flyers. Inclusion criteria for CHOICE include: 1) age 14-45 years; 2) willing to start a new reversible contraceptive method (may have used the chosen method previously, but not their current method of contraception); 3) no desire to conceive for at least 12 months; 4) sexually active with a male partner (or an intent to be active in the next 6 months); 5) reside in or seek clinical services at designated recruitment sites in the St. Louis region; and 6) ability to consent in English or Spanish. Women were excluded if they had a hysterectomy or sterilization procedure in the past.
All potential CHOICE participants are read a short standardized script regarding LARC methods at the time of eligibility screening, regardless of whether or not they enroll in the project.11 This script states “one of [the] objectives [of the study] is to be sure women are aware of all contraceptive options, especially the most effective, reversible, long-acting methods. These methods include intrauterine contraception and the subdermal implant.” Women who choose to participate may then enroll the day they hear the script or to up to 30 days later, or they will be rescreened for eligibility if greater than 30 days have passed. All enrolled participants complete a written contraceptive knowledge questionnaire prior to receiving comprehensive contraceptive counseling and selecting their contraceptive method. All reversible contraceptive methods are presented during contraceptive counseling; contraceptive method effectiveness, common side effects, risks and benefits are described so that participants can make an informed decision.
The contraceptive knowledge questionnaire asks participants to indicate the typical use failure rate of each contraceptive method. They were given a written questionnaire which stated: “we would like to get your best guess about how successful you think birth control methods are at preventing pregnancy. For each method of birth control, please tell us how many women you think would get pregnant, in a year, while using this method. What percentage (or number of women out of 100) do you think would get pregnant in a year using each method below?” The response categories are: <1%, 1-5%, 6-10%, >10%, and don't know. Participants are asked the effectiveness of the IUD, implant, depo-medroxyprogesterone acetate (DMPA), oral contraceptive pills, contraceptive patch, vaginal contraceptive ring, condoms, natural family planning (NFP) method, sterilization, and using “nothing” for contraception. Typical use failure rates as quoted in Table 112 were used to define the correct answers and were categorized as “correct,” “overestimate,” “underestimate,” and “don't know.”
Table 1.
Typical use failure rates of selected contraceptive methods
| Contraceptive method | Percent of women experiencing an unintended pregnancy (contraceptive failure) within the first year of typical use |
|---|---|
| No method (Nothing) | 85 |
| Spermicides | 28 |
| Natural family planning | 24 |
| Condom (male & female) | 18-21 |
| Diaphragm | 12 |
| Combined and progestin-only pills | 9 |
| Contraceptive patch | 9 |
| Vaginal contraceptive ring | 9 |
| Depo-medroxyprogesterone acetate (DMPA) | 6 |
| IUD | 0.2-0.8 |
| Implanon | 0.5 |
| Sterilization (male & female) | 0.15-0.5 |
Adapted from Trussell J. Contraceptive failure in the United States. Contraception 2011;83:397-404
All women enrolled in the Contraceptive CHOICE Project from the study launch in August 2007 through December 2009 were eligible to be included in this analysis. Demographic and reproductive characteristics of the study participants are obtained using a staff- administered questionnaire during the enrollment session and are described with frequencies, percentages, means, and standard deviations for appropriate data type. Baseline covariates among different contraceptive method users were compared using chi-square for categorical variables, as well as ANOVA for continuous normally distributed variables. Normality was assessed by evaluating the histogram of continuous variables. Participants’ responses were evaluated for the entire cohort before analyzing them by the method of contraception they chose after completing contraceptive counseling. We then assessed the likelihood of correctly estimating effectiveness of chosen method with univariate analysis using chi-square. We evaluated the association of participant's reported contraceptive history on their knowledge of contraceptive effectiveness. We assessed the likelihood of correctly estimating the effectiveness of their chosen method with multivariable Poisson regression with robust error variance adjusted for age, education and prior method use. We also performed the analyses of contraceptive effectiveness knowledge by chosen baseline contraceptive method. Because the published failure rates for the combination hormonal contraceptive patch and vaginal ring are the same as oral contraceptive pills, we chose to group users of these methods together as pill/patch/ring users. Additionally, because users of pill/patch/ring represent the largest proportion of women using reversible contraception in the US,7 they served as the referent group for this multivariable regression analysis.
Results
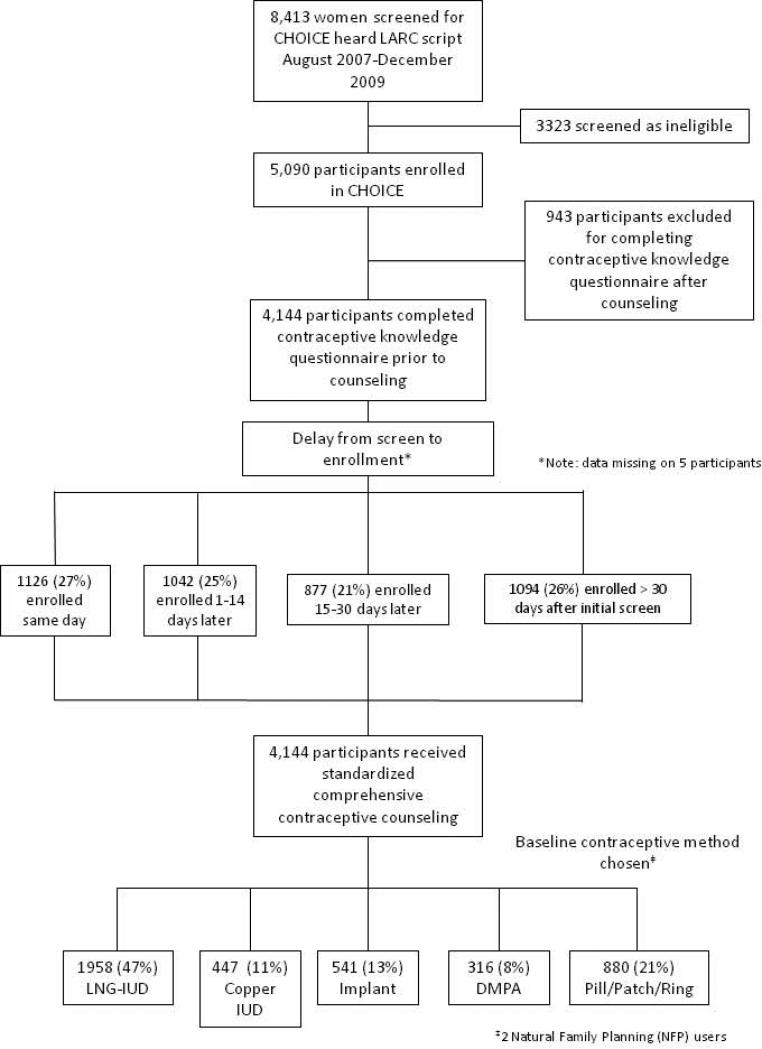
Of the 8,413 women screened for eligibility, 5,090 participants were eligible and enrolled in CHOICE between August 2007 and December 2009. (See Figure 1) Of the women enrolled, 4,144 (81%) completed the baseline contraceptive knowledge tool prior to contraceptive counseling. The time from screening to enrollment and completion of the knowledge tool was distributed relatively equally between same day, within 1-14 days, 15-30 days and greater than 30 days. Overall, 71% of participants chose LARC; 47% chose the levonorgestrel IUD (LNG-IUD), 11% chose the copper IUD, and 13% chose the contraceptive implant. Oral contraceptive pills (either combination or progestin-only) were chosen by 10% of women, 8% chose DMPA, 9% chose the vaginal ring and 2% chose the contraceptive patch. We observed statistically significant differences in most of the demographic and baseline characteristics of the participants when grouped by chosen baseline contraceptive method (Table 2). Overall, the mean age of participants at the time of enrollment was 25.2 years (SD 5.8). Participants who chose the copper IUD tended to be older and more educated compared to other methods, whereas users of the implant were younger and less likely to have attended or completed college. More than half of participants reported difficulty paying for necessities or receive government support and only 41% reported they had private health insurance. The majority of participants (59%) reported they wanted two or fewer children.
Figure 1.
Participant flow from screening to enrollment and baseline contraceptive method chosen
Table 2.
Baseline Characteristics of Cohort Stratified by Chosen Contraceptive Method
| All users (n=4144)‡ Mean (SD) | LNG-IUD (n=1958) Mean (SD) | Copper IUD (n=447) Mean (SD) | Implant (n=541) Mean (SD) | DMPA (n=316) Mean (SD) | Pill/Patch/Ring (n=880) Mean (SD) | |
|---|---|---|---|---|---|---|
| Age at enrollment* | 25.2 (5.8) | 25.8 (5.7) | 28.1 (6.2) | 23.0 (5.9) | 24.5 (5.9) | 24.0 (4.8) |
| Age first had sex* | 16.3 (2.5) | 16.2 (2.4) | 16.3 (3.1) | 15.7 (2.2) | 15.9 (2.1) | 16.8 (2.5) |
| % | % | % | % | % | % | |
| Education* | ||||||
| Less than high school/High school | 37.3 | 35.5 | 29.8 | 57.3 | 52.4 | 27.7 |
| Some college | 41.6 | 43.6 | 41.2 | 32.2 | 38.1 | 44.7 |
| College/Grad degree | 21.0 | 21.0 | 29.1 | 10.5 | 9.5 | 27.6 |
| Hispanic Ethnicity* | 5.0 | 4.2 | 7.4 | 8.0 | 2.2 | 4.7 |
| Race* | ||||||
| Black | 50.9 | 50.9 | 39.0 | 58.3 | 72.7 | 44.9 |
| White | 41.5 | 42.3 | 51.3 | 33.3 | 21.6 | 46.9 |
| Other | 7.5 | 6.8 | 9.6 | 8.4 | 5.7 | 8.2 |
| Marital status* | ||||||
| Never married | 59.5 | 55.6 | 45.7 | 64.9 | 63.0 | 70.7 |
| Married/Living with Partner | 34.0 | 37.8 | 42.6 | 29.7 | 26.9 | 26.5 |
| Separated/Divorced/Widowed | 6.5 | 6.6 | 11.7 | 5.4 | 10.1 | 2.8 |
| Monthly individual income* | ||||||
| None | 19.0 | 17.2 | 17.3 | 29.9 | 22.7 | 15.6 |
| $1-800 | 32.5 | 30.6 | 29.7 | 35.3 | 34.2 | 35.7 |
| $801-1600 | 29.8 | 31.5 | 28.8 | 24.4 | 28.8 | 30.3 |
| $1601+ | 18.8 | 20.8 | 24.1 | 10.4 | 14.4 | 18.4 |
| Insurance* | ||||||
| None | 45.3 | 43.2 | 44.6 | 44.0 | 59.0 | 46.4 |
| Private | 41.4 | 42.4 | 43.0 | 31.1 | 31.7 | 47.9 |
| Public | 13.3 | 14.4 | 12.4 | 24.9 | 9.2 | 5.6 |
| Government support/Trouble paying for basic necessities*§ | 58.9 | 61.5 | 58.7 | 64.3 | 65.2 | 47.5 |
| Gravidity* | ||||||
| 0 | 27.0 | 19.5 | 22.6 | 30.1 | 24.7 | 44.9 |
| 1 | 22.2 | 20.1 | 14.5 | 29.8 | 24.1 | 25.3 |
| 2 | 18.3 | 21.8 | 17.7 | 14.0 | 16.1 | 14.4 |
| 3+ | 32.5 | 38.7 | 45.2 | 26.1 | 35.1 | 15.3 |
| Parity* | ||||||
| 0 | 45.6 | 35.5 | 36.5 | 49.0 | 48.4 | 69.3 |
| 1 | 25.2 | 28.7 | 22.1 | 27.0 | 21.5 | 19.1 |
| 2 | 18.1 | 22.5 | 22.1 | 14.6 | 17.7 | 8.4 |
| 3+ | 11.2 | 13.3 | 19.2 | 9.4 | 12.3 | 3.2 |
| Number of children desired* | ||||||
| Don't Know | 2.6 | 2.5 | 2.5 | 2.0 | 1.6 | 3.6 |
| 0 | 7.5 | 7.3 | 10.3 | 8.6 | 6.6 | 5.2 |
| 1 | 13.0 | 12.8 | 13.9 | 12.6 | 12.7 | 11.9 |
| 2 | 38.8 | 38.1 | 34.7 | 38.3 | 35.4 | 39.6 |
| 3+ | 40.6 | 39.3 | 38.7 | 38.5 | 43.7 | 39.7 |
| History of STI** | 33.7 | 35.1 | 31.1 | 34.4 | 42.7 | 28.1 |
| Lifetime sexual partners* | ||||||
| 0-1 | 9.3 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 |
| 2-4 | 26.8 | 26.9 | 20.1 | 32.0 | 28.8 | 26.1 |
| 5-9 | 32.4 | 32.5 | 31.1 | 29.2 | 36.4 | 33.2 |
| 10-19 | 19.6 | 21.0 | 21.9 | 14.4 | 17.1 | 19.5 |
| 20+ | 11.9 | 11.3 | 18.6 | 11.3 | 11.1 | 10.3 |
| Sexual partners last 30 days* | ||||||
| 0 | 19.4 | 19.0 | 16.8 | 25.0 | 17.4 | 18.9 |
| 1 | 73.6 | 74.9 | 77.2 | 68.6 | 72.5 | 72.6 |
| 2+ | 7.0 | 6.1 | 6.0 | 6.5 | 10.1 | 8.5 |
| Any unintended pregnancies† | 91.3 | 91.1 | 91.6 | 89.7 | 89.8 | 93.8 |
Note: due to rounding some columns exceed 100%
Statistically significant finding p<0.05
Public Assistance: current receipt of food stamps, WIC, welfare or unemployment; Trouble Paying Basic Expenses: transportation, housing, health or medical care, or food
History of STI: self-reported of history of chlamydia, gonorrhea, syphilis, trichomoniasis, genital herpes, human papillomavirus or human immunodeficiency virus
Among women who reported history of pregnancy (n=3017)
2 Participants chose the natural family planning as their baseline contraceptive method
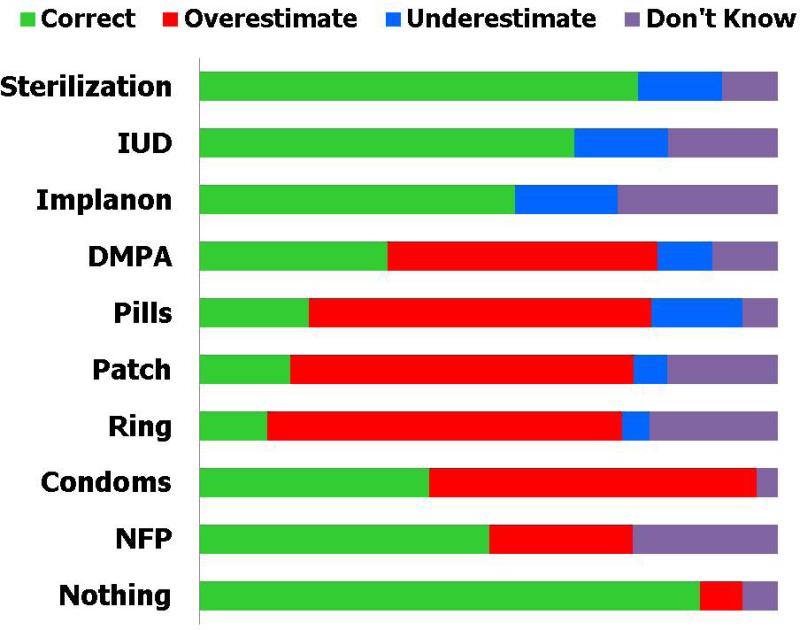
Most participants (86%) correctly estimated the annual chance of pregnancy using no contraception. The structure of the question regarding contraceptive effectiveness did not make it possible to “overestimate” the effectiveness of sterilization, IUDs and implants, yet only 76%, 65% and 55%, respectively, correctly identified the effectiveness of these methods. Similarly, participants could not “underestimate” the percentage of women who would experience a contraceptive failure in a year using condoms, natural family planning or no contraception. Figure 2 demonstrates the most common mistake was to overestimate the effectiveness (underestimate the risk of failure) of DMPA, pill, patch, ring, condoms or NFP. Among the entire cohort, less than 1 in 5 participants could correctly identify the typical risk of contraceptive failure for the pill, patch or ring. The proportion of all participants who correctly identified the effectiveness of DMPA, condoms, and natural family planning methods was 33%, 40%, and 50% respectively. The overestimation of the effectiveness of non-LARC methods was considerable with 47%, 57%, and 60% overestimating the effectiveness of DMPA, condoms and pill/patch/ring, respectively. When we stratified participants by baseline chosen method (LARC vs. non-LARC), the results were similar to those presented in Figure 2. While women who chose LARC methods were more likely to know the effectiveness of those methods, they were not more knowledgeable about non-LARC method failure rates. Finally, we assessed whether there was an association between time from screening to contraceptive knowledge assessment and correct estimates; no such relationship was found.
Figure 2.
Knowledge of contraceptive effectiveness among all participants (n=4,144)
Women who chose IUDs were most likely to correctly estimate the effectiveness of their chosen method. Seventy-two percent of women who chose IUDs correctly identified the IUD failure rate compared to 53% of women who did not choose IUDs (p<0.01). Sixty-two percent of participants who chose the implant correctly estimated its effectiveness. Only 22% of DMPA users correctly identified their method's effectiveness, whereas participants who chose pill/patch/ring users were least likely to be correct (12%). Upon adjusting for age, education and prior method use, women who chose IUDs were nearly seven times (adjusted relative risk (RRadj)=6.9; 95% confidence interval (CI) 5.6-8.5) more likely to correctly identify the failure rate of their chosen method than women who chose the pill/patch/ring (Table 3). Women who chose the implant were almost six times more likely (RRadj=5.9; 95% CI 4.7-7.3), and women who chose DMPA were twice as likely (RRadj=2.0; 95% CI 1.5-2.7) to correctly estimate the effectiveness of their method compared to women who chose pill, patch, or ring.
Table 3.
Knowledge of Effectiveness of Chosen Contraceptive Method (n=4,144)
| Contraceptive Method Chosen | n | % of Cohort using this method | % Correctly Estimated Effectiveness of Chosen Method | RRadj (95% CI) Correct Estimation of Chosen Method† |
|---|---|---|---|---|
| LNG-IUD | 1,958 | 47.5 | 72.2 | 6.9 (5.6-8.5) |
| Copper IUD | 447 | 10.8 | 72.8 | 7 (5.7-8.7) |
| Implant | 541 | 13.1 | 61.7 | 5.9 (4.7-7.3) |
| DMPA | 316 | 7.7 | 22.2 | 2.0 (1.5-2.7) |
| Pill/Patch/Ring | 880 | 20.9 | 11.8 | Reference |
Multivariable model Poisson regression with robust error variance adjusted for age, education and prior method use
Comment
In our study of knowledge of contraceptive effectiveness, most women overestimated the effectiveness of the oral contraceptive pill, the contraceptive patch, the ring, DMPA and condoms. Women who chose LARC methods were more likely to know the effectiveness of their chosen method than those who chose less effective methods, but they were not more knowledgeable about non-LARC method failure rates. This suggests these women highly value contraceptive effectiveness. In fact, studies have shown that women prioritize effectiveness, safety and ease of use when choosing a contraceptive method.1, 2 Women who chose less effective methods (e.g., pill, patch, or ring) also heard the short script regarding contraceptive effectiveness and nevertheless chose a non-LARC method. While their overestimation of the effectiveness of the non-LARC methods may demonstrate less a priori knowledge, these participants still selected these methods following comprehensive contraceptive counseling. Thus, there may be other reasons this group is reluctant to use LARC methods other than contraceptive effectiveness.
Unintended pregnancy continues to be an epidemic13 in the US and will require a multifaceted approach to lower this rate. Despite past uncertainty regarding the influence of clinicians’ counseling,14 there is recent evidence that counseling can increase contraceptive use and potentially decrease the rate of unintended pregnancy.15, 16 When discussing various contraceptive options for women, it is important to emphasize the difference between typical and perfect-use failure rates. As demonstrated in this analysis, nearly 60% of participants overestimated the typical effectiveness of pills, patch, ring and condoms. These four methods require significantly more user adherence creating potential for less than perfect use. We cannot ignore the impact of media and direct-to-consumer advertising on women's knowledge of contraceptives which usually present perfect-use failure rates.17 It is possible that women overestimate the effectiveness of these methods as a result of the Food and Drug Administration's requirement that manufacturer's messages include only data from the package label where perfect use failure rates are cited. However, women's typical use is more variable and the failure rates are significantly higher.12 Whereas, for LARC methods, typical use and perfect use failure rates are equivalent.
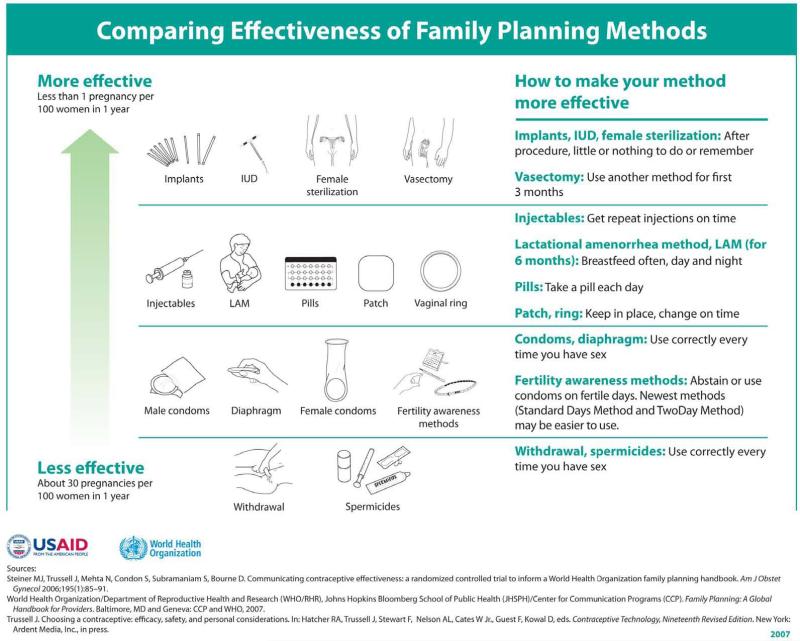
The overestimation of the effectiveness of the most commonly used contraceptives, pills and condoms, warrants attention and highlights the need for better methods to convey contraceptive effectiveness. Accurate information from healthcare providers is essential to helping women choose the best contraceptive method for them. A recent Cochrane review of strategies to communicate contraceptive effectiveness found limited evidence regarding which counseling tools work best.3 Steiner, et al, showed that a World Health Organization (WHO) developed chart of contraceptive effectiveness stratified by “average” (typical) versus “correct and consistent use” (perfect use) was significantly more difficult for women to understand.18 The most recently published WHO chart of contraceptive effectiveness (Figure 3) uses a continuum of typical use effectiveness to demonstrate the difference between the more effective and less effective methods.19
Figure 3.
Comparing typical effectiveness of family planning methods19
A strength of this report is that it is one of the largest assessments of women's prior knowledge of contraceptive effectiveness in the US. Women enrolled in CHOICE are similar to reproductive-aged women nationally represented in the National Survey of Family Growth and the Behavioral Risk Factor Surveillance System.20 Specifically, the women included in the current analysis similarly report a desire for 2 or fewer children which will require reliance on an effective contraceptive method for over 30 years given the reproductive lifespan of American women.21 However, there are limitations to this study. All participants heard a short statement which described IUDs and implants as “the most effective, reversible, long-acting methods” prior to their enrollment. It is difficult to estimate the influence of this short script on our results. While the script may have increased awareness and knowledge of the low failure rate of LARC methods, it is still important to note that over one-third of participants could not correctly identify the correct failure rate for IUDs and implants. More importantly, the overestimation of the effectiveness of the most commonly used reversible contraceptives—pill, patch, ring and DMPA—reinforces the need for better education about contraception. The higher rate of LARC use in CHOICE compared with national use estimates may reflect the influence of our script introducing LARC methods on women's choice of baseline method, but there are other factors that could contribute. Some of the participants in CHOICE were referred from other reproductive health providers who may have advised their patients of the higher effectiveness and ease of use of LARC, thus increasing the demand for these methods. The comprehensive contraceptive counseling and lack of cost and access barriers to LARC methods could be related to increased use. Given the high prevalence of prior unintended pregnancy among the women enrolled, it is possible CHOICE participants value effectiveness of their chosen contraceptive method more than the average woman in the US.
In conclusion, although sexually experienced and aware of the risk of pregnancy, participants in the Contraceptive CHOICE Project demonstrated significant knowledge gaps regarding contraceptive effectiveness. Women who selected IUDs and implants had greater knowledge of the effectiveness of their chosen method than women who selected other methods. In order to increase the use of highly-effective contraception and potentially decrease the rate of unintended pregnancy, we must improve education about typical use contraceptive effectiveness. The American College of Obstetricians and Gynecologists has stated that use of LARC methods has the potential to reduce unintended pregnancy rates and should be offered as first-line contraceptive options.22 Clinicians, public health officials, and educators need to provide comprehensive counseling and universal access to all contraceptive methods so that women may choose the best method that will reduce their risk for unintended pregnancy.
Acknowledgments
The Contraceptive CHOICE Project is funded by an Anonymous Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presentation information: A preliminary version of this analysis was presented as a poster at “Reproductive Health 2010” sponsored jointly by the Society of Family Planning, Association of Reproductive Health Professionals and Planned Parenthood Federation of America, Atlanta, GA, September 22-26, 2010.
DISCLOSURE: The authors report no conflicts of interest.
References
- 1.FORREST JD. U.S. women's perceptions of and attitudes about the IUD. Obstet Gynecol Surv. 1996;51:S30–4. doi: 10.1097/00006254-199612000-00012. [DOI] [PubMed] [Google Scholar]
- 2.STANWOOD NL, BRADLEY KA. Young pregnant women's knowledge of modern intrauterine devices. Obstet Gynecol. 2006;108:1417–22. doi: 10.1097/01.AOG.0000245447.56585.a0. [DOI] [PubMed] [Google Scholar]
- 3.LOPEZ LM, STEINER MJ, GRIMES DA, SCHULZ KF. Strategies for communicating contraceptive effectiveness. Cochrane Database Syst Rev. 2008:CD006964. doi: 10.1002/14651858.CD006964.pub2. [DOI] [PubMed] [Google Scholar]
- 4.HLADKY KJ, ALLSWORTH JE, MADDEN T, SECURA GM, PEIPERT JF. Women's knowledge about intrauterine contraception. Obstet Gynecol. 117:48–54. doi: 10.1097/AOG.0b013e318202b4c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DELBANCO S, LUNDY J, HOFF T, PARKER M, SMITH MD. Public knowledge and perceptions about unplanned pregnancy and contraception in three countries. Fam Plann Perspect. 1997;29:70–5. [PubMed] [Google Scholar]
- 6.MUULA AS. Trends in contraceptive knowledge and use among adolescent married women in Malawi. Croat Med J. 2008;49:561–3. doi: 10.3325/cmj.2008.4.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MOSHER WD, JONES J. Use of Contraception in the United States: 1982-2008. National Center for Health Statistics. Vital Health Statistics. 2010:23. [PubMed] [Google Scholar]
- 8.FINER LB, HENSHAW SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 9.KAVANAUGH ML, JERMAN J, HUBACHER D, KOST K, FINER LB. Characteristics of women in the United States who use long-acting reversible contraceptive methods. Obstet Gynecol. 2011;117:1349–57. doi: 10.1097/AOG.0b013e31821c47c9. [DOI] [PubMed] [Google Scholar]
- 10.PEIPERT JF, ZHAO Q, ALLSWORTH JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117:1105–13. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.SECURA GM, ALLSWORTH JE, MADDEN T, MULLERSMAN JL, PEIPERT JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203:115, e1–7. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.TRUSSELL J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.HENSHAW SK. Unintended pregnancy and abortion in the USA: Epidemiology and public health impact. In: Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD, editors. Management of Unintended and Abnormal Pregnancy: Comprehensive Abortion Care. Wiley-Blackwell; Oxford: 2009. [Google Scholar]
- 14.MOOS MK, BARTHOLOMEW NE, LOHR KN. Counseling in the clinical setting to prevent unintended pregnancy: an evidence-based research agenda. Contraception. 2003;67:115–32. doi: 10.1016/s0010-7824(02)00472-9. [DOI] [PubMed] [Google Scholar]
- 15.HARPER CC, BROWN BA, FOSTER-ROSALES A, RAINE TR. Hormonal contraceptive method choice among young, low-income women: how important is the provider? Patient Educ Couns. 2010;81:349–54. doi: 10.1016/j.pec.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LEE JK, PARISI SM, AKERS AY, BORRERRO S, SCHWARZ EB. The impact of contraceptive counseling in primary care on contraceptive use. J Gen Intern Med. 2011;26:731–6. doi: 10.1007/s11606-011-1647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.SUFRIN CB, ROSS JS. Pharmaceutical industry marketing: understanding its impact on women's health. Obstet Gynecol Surv. 2008;63:585–96. doi: 10.1097/OGX.0b013e31817f1585. [DOI] [PubMed] [Google Scholar]
- 18.STEINER MJ, TRUSSELL J, MEHTA N, CONDON S, SUBRAMANIAM S, BOURNE D. Communicating contraceptive effectiveness: A randomized controlled trial to inform a World Health Organization family planning handbook. Am J Obstet Gynecol. 2006;195:85–91. doi: 10.1016/j.ajog.2005.12.053. [DOI] [PubMed] [Google Scholar]
- 19.STEINER MJ, TRUSSELL J, JOHNSON S. Communicating contraceptive effectiveness: an updated counseling chart. Am J Obstet Gynecol. 2007;197:118. doi: 10.1016/j.ajog.2007.03.049. [DOI] [PubMed] [Google Scholar]
- 20.KITTUR ND, SECURA GM, PEIPERT JF, MADDEN T, FINER LB, ALLSWORTH JE. Comparison of contraceptive use between the Contraceptive CHOICE Project and state and national data. Contraception. 83:479–85. doi: 10.1016/j.contraception.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.GUTTMACHER I. Fulfilling the Promise: Public Policy and U.S. Family Planning Clinics The Alan Guttmacher Institute New York. The Alan Guttmacher Institute (AGI); 2000. [Google Scholar]
- 22.ACOG Committee Opinion no. 450: Increasing use of contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2009;114:1434–8. doi: 10.1097/AOG.0b013e3181c6f965. [DOI] [PubMed] [Google Scholar]