Abstract
Objective
We examined trends from 1977–2010 in calorie, macronutrient, and food group intake among US adults 55 and older.
Design
Cross-sectional time series.
Setting
A nationally representative sample of the US non-institutionalized population.
Participants
Older Americans aged ≥55 years (n=18,603) from four surveys of dietary intake in 1977–1978, 1989–1991, 1994–1996, and 2005–2010.
Measurements
Dietary intake was assessed using one 24-hour recall. Multivariable linear regression models were used to determine adjusted per capita mean energy and macronutrient intake for each survey year. Interactions were used to examine differences by race/ethnicity, gender, and generation. The top five food group contributors to total calorie intake were identified for each year.
Results
Mean total calorie intake increased significantly among older Americans from 1977–2010. Increases in carbohydrate intake (43% to 49% of total calories) were coupled with decreases in total fat intake (from 40% to 34%) while saturated fat (11%) remained constant. Corresponding shifts in food group intake were observed, as red meat intake greatly declined while bread and grain desserts became dominant calorie sources. Calorie intake was significantly higher for whites compared to blacks from 1994–2010. Cohort analysis indicated a shift from decreasing caloric intake with age to relatively stable calorie intake despite increasing age in more recent cohorts.
Conclusion
Increases in total calorie intake from 1977–2010, coupled with the finding that more recent generations did not show the expected age-related decrease in caloric consumption, raise concerns about obesity risk among older Americans. Additionally, despite declines across time in total fat intake, saturated fat intake continues to exceed recommendations and shifts toward increased consumption of grain-based desserts suggest that high discretionary calorie intake by older Americans might make it difficult to meet nutrient requirements while staying within energy needs.
Keywords: older adults, energy intake, macronutrients, food groups
Introduction
Older adults comprise one of the fastest growing age groups of the US population, and their number is expected to double from 40.2 million to 88.5 million by 2050 (1,2). In this important segment of the population, the prevalence of obesity significantly increased between 1960 and 1994 and continued to increase between 1999 and 2010 among older men aged 65 years and over (2,3). By 2007–2010, over one third of adults ≥65 were obese, with obesity prevalence highest (40.8%) among adults aged 65–74 years (2,4). This rise in obesity is concerning given the shifts in the age distribution of the US population. In older adults, obesity increases the risk of many chronic conditions such as diabetes, hypertension, and cardiovascular disease and is also associated with chronic pain (5). Both aging and obesity result in increased health care costs, with Medicare expenses approximately 34% higher for obese individuals (6).
Concurrent with this rise in obesity, diets among all Americans have shifted unfavorably toward higher total calorie intake, increased consumption of sweetened beverages, and more frequent snacking (7–10). In contrast, examination of energy intake prior to the mid-1990s found that calorie intake for older Americans was inadequate to meet energy needs, and increases from 1977 to 1996 were much smaller relative to other age groups (10–12). The contribution of salty snacks, soft drinks, and pizza to total energy intake, as well as increases in these food groups between 1977 and 1996, were also notably smaller for adults >60 compared to younger adults (10). Additional food group shifts from high-fat to low-fat meat and dairy were documented among adults ≥65 between 1977 and 1987 (11). The number of snacking occasions and total energy from snacks increased among adults >60 between 1977 and 2006; in contrast to younger adults, snacking was shown to be an important contributor to both adequate energy and micronutrient intake (9,13,14).
However, limited information is available on current dietary trends after the mid-1990s specifically among older Americans. To our knowledge, up-to-date trends in energy intake using nationally representative data are not available. Energy requirements decline as individuals age for reasons including decreased physical activity and lean mass (15). Although numerous studies confirm the corresponding decrease in calorie intake with increasing age, few studies have examined whether these declines persist in the current obesogenic food environment (16–18). Monitoring recent cohorts of older adults for increased susceptibility to secular trends is needed to anticipate sharp rises in the prevalence of obesity and other nutritionally related non-communicable diseases as these cohorts age.
As diet is a key modifiable risk factor for obesity and related chronic diseases, understanding trends in dietary intake among this expanding segment of the population is essential. Thus, the goal of this study is describe changes in energy, macronutrient, and food group intake among US adults aged 55 years and older from 1977–2010. Trends in energy intake are compared by age group (55–64, 65–74, and ≥75 years of age), race/ethnicity, gender, and generation. Results of this analysis can help inform policy and nutritional interventions by identifying dietary components of concern as well as vulnerable subpopulations of older adults that these efforts should focus upon.
Methods
Dietary Intake
This cross-sectional study included 18,603 older adults aged 55 and older from four nationally representative US surveys of dietary intake: 5,537 participants from the 1977–1978 Nationwide Food Consumption Survey (NFCS77); 3,521 participants from the 1989–1991 Continuing Survey of Food Intakes by Individuals (CSFII89); 3,851participants from the 1994–1996 Continuing Survey of Food Intakes by Individuals (CSFII94); and 5,694 participants from the 2005–2006, 2007–2008 and 2009–2010 National Health and Nutrition Examination Surveys (NHANES05). These studies used self-weighting, multistage, stratified area probability samples of civilian, non-institutionalized US population. Details about the sampling design and data collection methodology used by each survey have been published previously (19–24). This secondary data analysis was exempt from institutional review board approval.
NFCS77 and CSFII89 collected one in-person interviewer-administered 24-hour recall and a two-day self-administered food intake record for a total of 3 consecutive days of dietary intake. CSFII94 collected two nonconsecutive in-person interviewer-administered 24-hour recalls. NHANES05 collected two nonconsecutive 24-hour recalls, the first by trained interviewer in the Mobile Examination Center and a second by telephone 3–10 days later. To ensure that data collection methodology was comparable across surveys, only the first day of dietary intake was used. Dietary recalls for all surveys were linked with food composition tables for the corresponding time period that are all based on the United States Department of Agriculture (USDA) Nutrient Data Base for Standard Reference, which further ensures survey comparability.
Food Grouping System
Foods and beverages were classified into 57 mutually exclusive, nutritionally meaningful groups (42 food groups and 15 beverage groups) using the University of North Carolina at Chapel Hill food grouping system (25). Our approach begins with the nine USDA food groupings and breaks them down into more detailed groups in a systematic method based on nutrient composition, dietary behaviors, and consumption patterns, with beverages classified separately based on their effects on satiety and weight gain (26,27). A complete description of food and beverage groups is provided in Supplementary Table 1.
Statistical Analysis
Analyses were performed using survey commands within Stata (version 12, 2011, StataCorp, College Station, TX) to account for complex survey design. Survey weights provided by the USDA were used to account for differential probabilities of selection and non-response and were normalized to a comparable scale across years. Linear regression was used to compute mean daily intake of total calories and percentage of calories from carbohydrates, protein, total fat, and saturated fat for each survey year, adjusted for gender, race-ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, and other race/ethnicities), education (less than high school, high school, some college, and college degree), and household income (≤130%, 131–299%, ≥300% of the federal poverty level) for all adults ≥ 55 years of age and by age groups (55–64, 65–74, and ≥75 years). Trends in saturated fat intake were examined only from 1989–91 to 2005–10 because fat subtypes were not measured in NFCS77. Adjusted mean intake was also calculated for each race-ethnic group, and interactions of time and race were tested using a Wald “chunk” test to determine if changes across time differed by race-ethnicity, with significance set at P<0.05. Interactions by gender were examined using the same approach. Pairwise difference testing was conducted using t-tests, and P<0.01 was considered statistically significant. For each survey, mean calorie intake from each food and beverage group was calculated, and groups were ranked to identify the top food group contributors to total calories for each year.
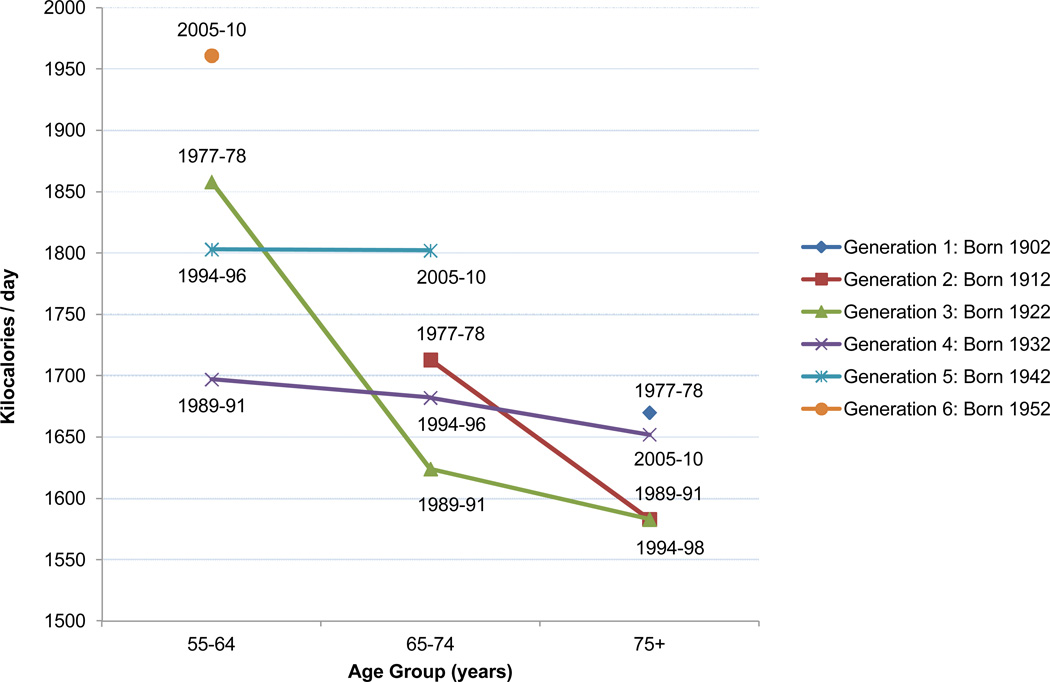
Because of changes in the US food environment and lifestyles within the latter half of the 20th century, we hypothesized that declines in total energy intake that occur with increasing age might differ for generations born in earlier years (Generation 1, born approximately in 1902 and age ≥75 in 1977–78) compared to generations born in later years (Generation 6, born approximately in 1952 and age 55–64 in 2005–10, see Figure 2). To examine these cohort effects, linear regression was used to regress total energy intake on age group, generation, and an interaction of age group and generation. Chunk tests of the interaction terms were used to test whether decreases in total calories that occur with increasing age are different for earlier vs later generations.
Figure 2.
Changes in total energy intake with increasing age among older Americans by generationa
a Data for adults aged 55 years and older from the Nationwide Food Consumption Survey (NFCS) 1977–1978 (n=5,337), Continuing Survey of Food Intakes by Individuals (CSFII) 1989–1991 (n=3,521), CSFII 1994–1996 (n=3,851), and the National Health and Nutrition Examination Survey (NHANES) 2005–2010 (n=5,694). Multivariable linear regression models were used to estimate per capita mean energy intake for each age group and survey year, adjusting for gender, race/ethnicity, household income, and education. Changes in energy intake with increasing age were significantly different across generations (P for interaction <0.05).
Results
The distribution of age group, gender, race/ethnicity, household income, and education was significantly different (P<0.01) across survey years, reflecting the shifting demographics among older adults (Table 1).
Table 1.
Distribution of sociodemographic characteristics among older Americans, 1977–2010a
| NFCS 1977–1978 n=5537 |
CSFII 1989–1991 n=3521 |
CSFII 1994–1996 n=3851 |
NHANES 2005–2010 n=5694 |
|
|---|---|---|---|---|
| Age Groups (%)b | ||||
| Youngest Old (55–64 years) | 48.6 | 40.3 | 40.6 | 46.5 |
| Middle Old (65–74 years) | 34.1 | 35.8 | 34.8 | 30.6 |
| Oldest Old (≥75 years) | 17.3 | 23.9 | 24.6 | 22.9 |
| Male (%) | 42.0 | 43.3 | 43.2 | 45.6 |
| Race/ethnicity (%) | ||||
| Non-Hispanic White | 87.0 | 83.9 | 82.6 | 79.7 |
| Non-Hispanic Black | 10.1 | 9.9 | 10.9 | 9.3 |
| Mexican American | 2.2 | 4.5 | 1.5 | 4.4 |
| Other | 0.7 | 1.6 | 5.0 | 6.5 |
| Household incomec | ||||
| 0–130% | 22.8 | 19.4 | 17.2 | 16.8 |
| 131–299% | 38.9 | 31.9 | 36.0 | 33.0 |
| ≥300% | 38.3 | 48.7 | 46.8 | 50.3 |
| Education | ||||
| Less than high school | 39.7 | 32.4 | 30.4 | 21.5 |
| High school degree | 30.2 | 34.1 | 34.9 | 27.0 |
| Some college | 15.5 | 15.4 | 16.6 | 25.7 |
| Bachelor’s degree or higher | 14.6 | 18.0 | 18.2 | 25.8 |
Data for adults aged 55 years and older from the Nationwide Food Consumption Survey (NFCS) 1977–1978, Continuing Survey of Food Intakes by Individuals (CSFII) 1989–1991, CSFII 1994–1996, and the National Health and Nutrition Examination Survey (NHANES) 2005–2010. The distribution of age group, gender, race/ethnicity, household income, and education were significantly different across survey years (P<0.01).
Weighted percentages have been adjusted to be nationally representative.
Household income expressed as percentage of the Federal Poverty Level.
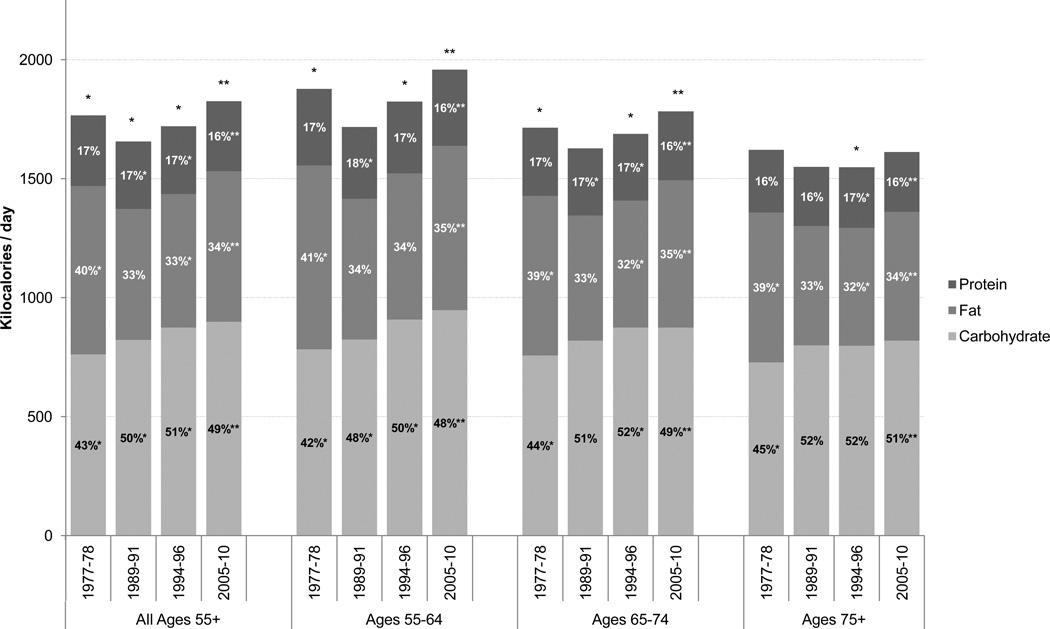
Among all adults ≥55 years of age, mean total calorie intake was significantly higher in 2005–10 (1841 kcal/d) compared to 1977–78 (1768 kcal/d), although a significant decrease was observed between 1977–78 and 1989–91 (Figure 1, p <0.01). These differences in calorie intake across time were also observed among 55–64 and 65–74 year olds, while total calorie intake in the oldest age group remained relatively constant across time. Comparing across age groups, mean total calorie consumption was significantly lower for older age groups at most time points, with adults ≥75 years of age having the lowest intake for all survey years.
Figure 1.
Adjusted per capita energy intake and macronutrient density among older Americans, 1977–2010a
*Data is significantly different than the subsequent survey year, P<0.01.
**Data is significantly different from 1977–1978, P<0.01.
a Data for adults aged 55 years and older from the Nationwide Food Consumption Survey (NFCS) 1977–1978 (n=5537), Continuing Survey of Food Intakes by Individuals (CSFII) 1989–1991 (n=3521), CSFII 1994–1996 (n=3851), and the National Health and Nutrition Examination Survey (NHANES) 2005–2010 (n=5694). Multivariable linear regression models were used to estimate per capita mean energy intake and percentage calories from protein, fat, and carbohydrate, adjusting for age group (for ages 55+), gender, race/ethnicity, household income, and education.
The percentage of calories from carbohydrates significantly increased from 43% in 1977–78 to 51% in 1994–96, then declined slightly to 49% in 2005–10 (p<0.01). In substitution, fat intake significantly decreased from 40% of total calories in 1977–78 to 34% in 2005–10; however, in the most recent time span from 1994–96 to 2005–10, a small but significant increase in fat was observed (p<0.01). Saturated fat intake among all age groups did not change from 1989–91 to 2005–10, staying at 11% in both years (results not shown). The percentage of calories from protein remained relatively constant across the survey years. Trends across time in macronutrient density among each individual age group were similar to those observed for all adults ≥55.
Among both non-Hispanic whites and blacks, similar trends of decreasing calorie intake from 1977–78 to 1989–91 and subsequent increases by 2005–10 were observed (Table 2). From 1994–2010, calorie intake was significantly lower for blacks compared to whites. In contrast, total calorie intake among Mexican Americans decreased sharply between 1977–78 and 2005–10 by 173 kcal/d, despite an increase between 1994–96 and 2005–10. Mexican Americans had the highest level of calorie intake in 1977–78, yet the lowest in 2005–10.
Table 2.
Total energy intake among older Americans by race/ethnicity and gender, 1977–2010a
| NFCS 1977–78 n =5537 |
CSFII 1989–91 n = 3521 |
CSFII 1994–96 n =3851 |
NHANES 2005–10 n = 5694 |
P valueb | |
|---|---|---|---|---|---|
| Race-ethnicity | |||||
| Non-Hispanic white | 1775 ± 16 | 1652 ± 23 | 1734 ± 17† | 1864 ± 18†‡ | 0.00 |
| Non-Hispanic black | 1696 ± 46§ | 1641 ± 78 | 1616 ± 49† | 1774 ± 28† | 0.15 |
| Mexican-American | 1924 ± 80§ | 1767 ± 175 | 1612 ± 93 | 1751 ± 34‡ | 0.05 |
| Gender | |||||
| Men | 2085 ± 26∥ | 1885 ± 35∥ | 2015 ± 22∥ | 2141 ± 27∥ | 0.13 |
| Women | 1524 ± 15∥ | 1472 ± 20∥ | 1485 ± 17∥ | 1609 ± 14∥ | 0.00 |
Data for adults aged 55 years and older from the Nationwide Food Consumption Survey (NFCS) 1977–1978, Continuing Survey of Food Intakes by Individuals (CSFII) 1989–1991, CSFII 1994–1996, and the National Health and Nutrition Examination Survey (NHANES) 2005–2010. Multivariable linear regression models were used to estimate per capita mean energy intake among each race-ethnic group and among each gender, adjusting for age group, gender, race/ethnicity, household income, and education where appropriate.
P value from t test for significant difference between 1977–78 and 2005–10 for the specified race-ethnic group or gender.
Significant difference between non-Hispanic whites and non-Hispanic blacks for the specified survey year.
Significant difference between non-Hispanic whites and Mexican Americans for the specified survey year.
Significant difference between non-Hispanic blacks and Mexican Americans for the specified survey year.
Significant difference between men and women for the specified survey year.
Total calorie intake significantly increased by a similar amount among men and women from 1977–2010, despite significantly lower absolute intake among women (Table 2). Interaction tests were significant, reflecting the greater decrease in calories between 1977–78 and 1989–91 among men compared to women.
Trends in total energy intake were significantly different across generations (P for interaction <0.05), as earlier generations experienced declines in intake with increasing age while more recent generations maintained a relatively stable level of intake from age 55 onward (Figure 2).
Examining contributions of specific food groups to total calorie intake for all age groups, red meat decreased from being the #1 contributor in 1977–78 to #7 in 2005–10 (Table 3; rankings for all food groups shown in Supplementary Table 2). Bread surpassed red meat to become the main source of calories from 1989–91 to 2005–10, although its percentage contribution to total intake actually declined during this time span as diets became more diverse. Calories from grain desserts increased across time, and this food group remained a top 5 contributor for all survey years.
Table 3.
Major sources of energy among older Americans, 1977–2010a
| #1 Source |
#2 Source |
#3 Source |
#4 Source |
#5 Source |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Survey Yearb | #1 Source | %c | Mean ± SEd (kcal) |
#2 Source | % | Mean ± SE (kcal) |
#3 Source | % | Mean ± SE (kcal) |
#4 Source | % | Mean ± SE (kcal) |
#5 Source | % | Mean ± SE (kcal) |
| NFCS 1977–78 | Red meate | 11.7 | 222 ± 6.7 | Breadsf | 9.8 | 161 ± 2.6 | Grain dessertsg | 6.0 | 118 ± 3.6 | Processed meath | 6.2 | 113 ± 3.4 | Coffee/teai | 4.8 | 79 ± 1.7 |
| CSFII 1989–91 | Breads | 9.2 | 139 ± 3.1 | Grain desserts | 6.3 | 116 ± 5.7 | Milkj | 5.6 | 85 ± 3.2 | Red meat | 5.1 | 84 ± 4.7 | Starchy vegetablesk | 4.4 | 71 ± 3.5 |
| CSFII 1994–96 | Breads | 9.1 | 144 ± 2.1 | Grain desserts | 7.1 | 134 ± 3.9 | Red meat | 4.6 | 78 ± 3.0 | Fruitl | 4.7 | 74 ± 1.9 | Processed meat | 4.2 | 72 ± 2.6 |
| NHANES 2005–10 | Breads | 7.6 | 136 ± 3.9 | Grain desserts | 6.8 | 134 ± 4.2 | Fruit | 4.2 | 71 ± 1.8 | Milk | 3.8 | 69 ± 2.9 | Dairy dessertsm | 3.3 | 64 ± 2.9 |
Data for adults aged 55 years and older from the Nationwide Food Consumption Survey (NFCS) 1977–1978 (n=5,537), Continuing Survey of Food Intakes by Individuals (CSFII) 1989–1991 (n=3,521), CSFII 1994–1996 (n=3,851), and the National Health and Nutrition Examination Survey (NHANES) 2005–2010 (n=5,694).
Per capita energy intake for each year: NFCS 1977–78: 1,768 kcal; CSFII 1989–91: 1,652 kcal; CSFII 1994–96: 1,716 kcal; NHANES 2005–10: 1,841 kcal.
Mean per-person percent of total calorie intake provided by each food group for given survey year.
Per capita total calories provided by each food group for given survey year. Values are mean calories (kcal) ± standard error (SE).
Includes beef, pork, lamb, and organ meats.
Includes yeast breads and rolls.
Includes grain-based desserts such as cookies, pastries, cakes, and pies.
Includes processed meat and poultry.
Includes coffee and tea (combined with milk, cream, and/or sweeteners) and coffee beverages.
Includes whole, 2%, 1%, and nonfat milk (plain, chocolate, or flavored).
Includes starchy vegetables and starchy vegetable dishes but excludes french fries and other fried potatoes.
Includes fresh, frozen, canned, or dried fruit.
Includes dairy-based desserts such as ice cream, sherbet, frozen yogurt, and pudding.
Discussion
This analysis helps fill the major research gap in the literature describing current trends in dietary intake among older Americans. A trend toward overall higher calorie diets across the past three decades was observed, as well as significant increases in carbohydrate intake coupled with decreases in total fat but not saturated fat intake. Corresponding shifts in food group intake were observed, as red meat intake greatly declined while bread and grain desserts became the dominant calorie sources. Total calorie intake was significantly higher for whites compared to blacks from 1994–96 onward, while increases in energy intake from 1977–78 to 2005–10 were similar among men and women. By examining differences by generation, this analysis uniquely found that individuals born before 1930 experienced a decline in calorie intake with increasing age, but individuals born after that period maintained a relatively constant level of intake.
Previous studies observed a small but statistically significant increase in total calorie intake among adults >60 between 1977 and 1996 (10,28). Our study found a similar pattern for adults ≥55. However, we uniquely show that from 1994–96 to 2005–10, a more substantial increase in energy intake occurred among older adults, demonstrating a trend toward increased calorie intake over time similar to that of younger age groups. Mean energy intake by gender in 2005–10 was similar to recommended amounts for sedentary older adults, but may exceed these guidelines in light of potential underreporting (29–31). While previous studies focus upon dietary deficiency and undernutrition among older adults, our findings of increased energy intake suggest that future research should examine the role of diet in obesity, chronic disease risk, and quality of life for this age group (12,13,17,18).
Decreases in energy intake between 1977–78 and 1989–91 were consistently observed among all adults ≥55 years and in stratified analysis by age group (among 55–64 and 65–74 year olds), by race-ethnicity, and by gender. Previous studies suggest that these changes reflect real shifts in consumption, changes in the food supply, and differences in survey methodology (11,32). Shifts away from whole milk and higher-fat red meats and increased consumption of lower-fat products between 1977–1991 have been documented (11,33). Changes in the food supply during this time span include increased trimming of visible fat from meat products at the retail level and industry changes in livestock breeding, which result in beef and pork with lower fat content (11,32,33). Although changes in interview procedures, food coding, and weight conversion methods were introduced after the NFCS77, results of the 1988 Bridging Study suggest that the effects of these changes on macronutrient and food group intake were minimal (32,34). If declines in energy intake were due to methodological differences in dietary assessment across surveys, then trends would likely be similar for all age groups. However, a previous study using these same surveys found a significant increase in total energy among adults aged 19–39 years and no change among adults 40–59 years, suggesting that the decrease in energy intake we observed among older adults between 1977–78 and 1989–91 reflects real changes in consumption, rather than an artifact of survey methodology changes (10).
The significant decrease in calories from fat between 1977–2010 and substitution with increased carbohydrate were also previously observed during earlier time periods (11). Corresponding to the changes in macronutrient intake, we observed shifts in food group intake as red meat was replaced by carbohydrate-rich foods such as bread and grain desserts. In agreement, Nielsen et al also found decreases between 1977–78 and 1994–96 in medium- and high-fat beef and pork intake for adults ≥60 (10). Our study builds upon this evidence by showing that the trend toward decreased red meat consumption continued from 1994–96 to 2005–10. Saturated fat intake did not decline from 1977–2010 and remained above recommendations, suggesting that increases in grain-based desserts might offset decreases in red meat (29). Increased consumption of grain-based desserts, which are main contributors to both added sugar and solid fat, may help explain why over 80% of older Americans exceed discretionary energy allowances (29,35).
Prior examination of differences in energy intake by race-ethnicity in 1976–1980 and 1988–1991 found that among older adults, African Americans and Mexican Americans tended to have lower caloric intakes than whites (18,36). However, while we observed a similar pattern in 1994–96 and 2005–10, our data indicated that Mexican-Americans had the highest intake in 1977–78 and 1989–91. This conflicting result is likely explained by differences in classification of ethnicity among surveys used in this analysis. The NFCS77 and CSFII89 distinguish only between Hispanics and non-Hispanics; however, Mexican Americans were the predominant group of Hispanics in this time period (19,20,37). CSFII94 and NHANES05 further differentiate origin among Hispanics, which allows study specifically of Mexican Americans, but over-sampling of only Mexican Americans prohibits study of all Hispanics (21,38). Because dietary patterns may differ among Hispanics of different origin and degree of acculturation, further studies of changes in dietary intake among Hispanics are needed (39). The lack of differential changes in total energy intake from 1977–2010 by gender is in agreement with previous studies (11).
The age-related decline in energy intake among older adults which results from both physiological impairment, such as decreased appetite, and non-physiological causes, including medical and social factors, is well-documented (16–18). To determine whether this phenomenon persists despite overall increases in calorie intake among Americans, we uniquely examined changes in energy intake from age 55 to ≥75 by generation. While the age-related decline was observed for individuals born before 1930, more recent generations no longer exhibited this same pattern. Because even slight excesses in calorie intake are sufficient to explain the rising prevalence of obesity, our finding supports the need for further studies, specifically using cohort data, to confirm these results (40,41).
Limitations
Differences in dietary assessment methodology across surveys are a primary limitation. This analysis used only the first day of dietary recall to maximize comparability in collection method (24-hour recall) and administration mode (in-person interviews). Multiple pass methodology was introduced in CSFII94 to maximize recall and automated in NHANES05 (21,42). This additional probing potentially increased the accuracy of data collection and could explain the observed increases in dietary consumption between 1994–96 and 2005–10 (42,43). However, no studies have examined the impact of these methodological changes.
One important limitation is the use of self-reported dietary intake, as underreporting potentially varies across foods groups and is associated with obesity (30,44–46). However, some studies suggest that underreporting is overestimated among older adults when single cutpoints are used for all age groups and because undereating is difficult to distinguish from underreporting (30,45). Changes in population-level factors associated with dietary intake can influence temporal trends (47). Although our analysis adjusts for sociodemographic characteristics, we were unable to adjust for weight status because comparable measurements were not collected for all surveys. Thus, another possible explanation for the decrease in energy intake between 1977–78 and 1989–91 might be an increase in underreporting as consequence of increased obesity prevalence (3,48,49).
Conclusion
Increases in total calorie intake from 1977–2010, coupled with the finding that more recent generations did not show the expected age-related decrease in caloric consumption, raise concerns about obesity risk in older Americans. Additionally, despite total fat declines across time, saturated fat intake continues to exceed recommendations and shifts toward increased consumption of grain desserts may potentially make it difficult for older Americans to meet nutrient requirements while staying within their lower total calorie needs (15). It remains unclear the extent to which the changes in the diets of older Americans contributed to the rise in obesity during this time span. Future studies should continue to monitor dietary trends in this rapidly growing segment of the US population, with particular focus on examining the association between dietary habits with nutrition-related chronic disease.
Supplementary Material
Acknowledgements
We wish to thank the National Institutes of Health (5T32DK007686-19 and 5R24HD050924), the Honors Carolina-Senior Thesis Research Grant, and the William W. and Ida W. Taylor Honors Mentored Research Fellowship for financial support. This research was funded in part by a Summer Undergraduate Research Fellowship from the Office for Undergraduate Research at the University of North Carolina at Chapel Hill. We also wish to thank Dr. Phil Bardsley for exceptional assistance with data management and programming and Ms. Frances L. Dancy for administrative assistance.
Footnotes
Conflict of interest:
We declare that we have no conflict of interest.
List of author contributions:
All authors participated in the overall design of the study, interpretation of results, and drafting of the manuscript. RJ and JP completed all data analysis.
Contributor Information
Rachel Johnston, Email: rajohnst@live.unc.edu.
Jennifer M. Poti, Email: poti@unc.edu.
W.R. Kenan, Jr., Email: popkin@unc.edu.
References
- 1.US Department of Health and Human Services. Older Adults. [Accessed January 2013];HealthyPeople.gov. 2012 http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=31.
- 2.Fakhouri TH, Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among older adults in the United States, 2007–2010. NCHS data brief. 2012:1–8. [PubMed] [Google Scholar]
- 3.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord. 1998;22:39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 5.Decaria JE, Sharp C, Petrella RJ. Scoping review report: obesity in older adults. Int J Obes (Lond) 2012;36:1141–1150. doi: 10.1038/ijo.2012.29. [DOI] [PubMed] [Google Scholar]
- 6.Lakdawalla DN, Goldman DP, Shang B. The health and cost consequences of obesity among the future elderly. Health Aff (Millwood) 2005;24(Suppl 2):W5R30–W5R41. doi: 10.1377/hlthaff.w5.r30. [DOI] [PubMed] [Google Scholar]
- 7.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977–1998. JAMA. 2003;289:450–453. doi: 10.1001/jama.289.4.450. [DOI] [PubMed] [Google Scholar]
- 8.Nielsen SJ, Popkin BM. Changes in beverage intake between 1977 and 2001. Am J Prev Med. 2004;27:205–210. doi: 10.1016/j.amepre.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Piernas C, Popkin BM. Snacking increased among U. S. adults between 1977 and 2006. J Nutr. 2010;140:325–332. doi: 10.3945/jn.109.112763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nielsen SJ, Siega-Riz AM, Popkin BM. Trends in energy intake in U. S. between 1977 and 1996: similar shifts seen across age groups. Obes Res. 2002;10:370–378. doi: 10.1038/oby.2002.51. [DOI] [PubMed] [Google Scholar]
- 11.Popkin BM, Haines PS, Patterson RE. Dietary changes in older Americans, 1977–1987. Am J Clin Nutr. 1992;55:823–830. doi: 10.1093/ajcn/55.4.823. [DOI] [PubMed] [Google Scholar]
- 12.Ryan AS, Craig LD, Finn SC. Nutrient intakes and dietary patterns of older Americans: a national study. J Gerontol. 1992;47:M145–M150. doi: 10.1093/geronj/47.5.m145. [DOI] [PubMed] [Google Scholar]
- 13.Zizza CA, Arsiwalla DD, Ellison KJ. Contribution of snacking to older adults' vitamin, carotenoid, and mineral intakes. J Am Diet Assoc. 2010;110:768–772. doi: 10.1016/j.jada.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Zizza CA, Tayie FA, Lino M. Benefits of snacking in older Americans. J Am Diet Assoc. 2007;107:800–806. doi: 10.1016/j.jada.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 15.Bernstein M, Munoz N. Academy of N, Dietetics Position of the Academy of Nutrition and Dietetics: food and nutrition for older adults: promoting health and wellness. J Acad Nutr Diet. 112:1255–1277. doi: 10.1016/j.jand.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 16.Hays NP, Roberts SB. The anorexia of aging in humans. Physiol Behav. 2006;88:257–266. doi: 10.1016/j.physbeh.2006.05.029. [DOI] [PubMed] [Google Scholar]
- 17.Drewnowski A, Evans WJ. Nutrition, physical activity, and quality of life in older adults: summary. J Gerontol A Biol Sci Med Sci. 2001;56(Spec No 2):89–94. doi: 10.1093/gerona/56.suppl_2.89. [DOI] [PubMed] [Google Scholar]
- 18.Wakimoto P, Block G. Dietary intake, dietary patterns, and changes with age: an epidemiological perspective. J Gerontol A Biol Sci Med Sci. 2001;56(Spec No 2):65–80. doi: 10.1093/gerona/56.suppl_2.65. [DOI] [PubMed] [Google Scholar]
- 19.Rizek R. The 1977–78 Nationwide Food Consumption Survey. Fam Econ Rev. 1978;4:3–7. [Google Scholar]
- 20.US Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group. Continuing Survey of Food Intakes by Individuals 1989–91 and Diet and Health Knowledge Survey 1989–91. Beltsville, MD: 1991. [Accessed May 2009]. http://www.ars.usda.gov/Services/docs.htm?docid=14393. [Google Scholar]
- 21.US Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group. Continuing Survey of Food Intakes by Individuals 1994–96 and Diet and Health Knowledge Survey 1994–96. Beltsville, MD: 1996. [Accessed May 2009]. http://www.ars.usda.gov/Services/docs.htm?docid=14531. [Google Scholar]
- 22.US Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group, and US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed September 2012];National Health and Nutrition Examination Survey 2005–2006. 2006 http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/nhanes05_06.htm.
- 23.US Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group, and US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. National Health and Nutrition Examination Survey 2007–2008. Hyattsville, MD: 2008. [Accessed September 2012]. http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/nhanes07_08.htm. [Google Scholar]
- 24.US Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group, and US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed September 2012];National Health and Nutrition Examination Survey 2009–2010. 2010 http://www.cdc.gov/nchs/nhanes/nhanes2009-2010/nhanes09_10.htm.
- 25.Popkin BM, Haines PS, Siega-riz AM. Dietary patterns and trends in the United States: the UNC-CH approach. Appetite. 1999;32:8–14. doi: 10.1006/appe.1998.0190. [DOI] [PubMed] [Google Scholar]
- 26.Mourao D, Bressan J, Campbell W, Mattes R. Effects of food form on appetite and energy intake in lean and obese young adults. Int J Obes. 2007;31:1688–1695. doi: 10.1038/sj.ijo.0803667. [DOI] [PubMed] [Google Scholar]
- 27.Mattes RD. Dietary compensation by humans for supplemental energy provided as ethanol or carbohydrate in fluids. Physiol Behav. 1996;59:179–187. doi: 10.1016/0031-9384(95)02007-1. [DOI] [PubMed] [Google Scholar]
- 28.Wright J, Kennedy-Stephenson J, Wang C, McDowell M, Johnson C. Trends in intake of energy and macronutrients–United States, 1971–2000. JAMA. 2004;291:1193–1194. [Google Scholar]
- 29.US Department of Agriculture, US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. Washington, DC: US Government Printing Office; 2010. [Google Scholar]
- 30.Livingstone MB, Black AE. Markers of the validity of reported energy intake. J Nutr. 2003;133(Suppl 3):895S–920S. doi: 10.1093/jn/133.3.895S. [DOI] [PubMed] [Google Scholar]
- 31.Poslusna K, Ruprich J, de Vries JH, Jakubikova M, van't Veer P. Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr. 2009;101(Suppl 2):S73–S85. doi: 10.1017/S0007114509990602. [DOI] [PubMed] [Google Scholar]
- 32.Guenther PM, Perloff BP, Vizioli TL., Jr Separating fact from artifact in changes in nutrient intake over time. J Am Diet Assoc. 1994;94:270–275. doi: 10.1016/0002-8223(94)90367-0. [DOI] [PubMed] [Google Scholar]
- 33.Popkin BM, Siega-Riz AM, Haines PS, Jahns L. Where's the fat? Trends in U. S. diets 1965–1996. Prev Med. 2001;32:245–254. doi: 10.1006/pmed.2000.0807. [DOI] [PubMed] [Google Scholar]
- 34.Guenther PM, Perloff BP. Effects of procedural differences between 1977 and 1987 in the Nationwide Food Consumption Survey on estimates of food and nutrient intakes: results of the USDA 1988 Bridging Study. Washington, DC: US Department of Agriculture, Human Nutrition Information Service; 1990. [Google Scholar]
- 35.Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. J Nutr. 2010;140:1832–1838. doi: 10.3945/jn.110.124826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McDowell MA, Briefel RR, Alaimo K, Bischof AM, Caughman CR, et al. Energy and macronutrient intakes of persons ages 2 months and over in the United States: Third National Health and Nutrition Examination Survey, Phase 1, 1988–91. Advance data. 1994:1–24. [PubMed] [Google Scholar]
- 37.Gibson C, Jung K. Historical census statistics on population totals by race 1790 to 1990, and by Hispanic origin, 1970 to 1990, for the United States, regions, divisions, and states. Working Paper Series No. 56. Appendix D-1, D-3, and D-4. Washington, DC: Population Division, US Census Bureau; 2002. [Google Scholar]
- 38.US Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group, and US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed February 2013];Analytic note regarding 2007–2010 survey design changes and combining data across other survey cycles. 2008 http://www.cdc.gov/nchs/data/nhanes/analyticnote_2007-2010.pdf.
- 39.Arandia G, Nalty C, Sharkey JR, Dean WR. Diet and acculturation among Hispanic/Latino older adults in the United States: a review of literature and recommendations. J Nutr Gerontol Geriatr. 2012;31:16–37. doi: 10.1080/21551197.2012.647553. [DOI] [PubMed] [Google Scholar]
- 40.Swinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr. 2009;90:1453–1456. doi: 10.3945/ajcn.2009.28595. [DOI] [PubMed] [Google Scholar]
- 41.Hall KD, Sacks G, Chandramohan D, Chow CC, Wang YC, et al. Quantification of the effect of energy imbalance on bodyweight. Lancet. 2011;378:826–837. doi: 10.1016/S0140-6736(11)60812-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.US Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group, and US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed Februrary 2013];National Health and Nutrition Examination Survey 2003–2004 MEC In-person Dietary Interviewers Procedure Manual. 2004 http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/DIETARY_MEC.pdf.
- 43.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88:324–332. doi: 10.1093/ajcn/88.2.324. [DOI] [PubMed] [Google Scholar]
- 44.Tooze JA, Vitolins MZ, Smith SL, Arcury TA, Davis CC, et al. High levels of low energy reporting on 24-hour recalls and three questionnaires in an elderly low-socioeconomic status population. J Nutr. 2007;137:1286–1293. doi: 10.1093/jn/137.5.1286. [DOI] [PubMed] [Google Scholar]
- 45.Shahar DR, Yu B, Houston DK, Kritchevsky SB, Newman AB, et al. Misreporting of energy intake in the elderly using doubly labeled water to measure total energy expenditure and weight change. J Am Coll Nutr. 2010;29:14–24. doi: 10.1080/07315724.2010.10719812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bazelmans C, Matthys C, De Henauw S, Dramaix M, Kornitzer M, et al. Predictors of misreporting in an elderly population: the 'Quality of life after 65' study. Public Health Nutr. 2007;2007;10:185–191. doi: 10.1017/S1368980007246774. [DOI] [PubMed] [Google Scholar]
- 47.Duffey KJ, Popkin BM. Energy density, portion size, and eating occasions: contributions to increased energy intake in the United States, 1977–2006. PLoS Med. 2011;8:e1001050. doi: 10.1371/journal.pmed.1001050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heitmann BL, Lissner L, Osler M. Do we eat less fat, or just report so? Int J Obes Relat Metab Disord. 2000;24:435–442. doi: 10.1038/sj.ijo.0801176. [DOI] [PubMed] [Google Scholar]
- 49.Hirvonen T, Mannisto S, Roos E, Pietinen P. Increasing prevalence of underreporting does not necessarily distort dietary surveys. Eur J Clin Nutr. 1997;51:297–301. doi: 10.1038/sj.ejcn.1600397. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.