Abstract
Background:
Plantar fasciitis is the most common cause of heel pain. Extracorporeal shock wave therapy (ESWT) is an alternative treatment for refractory cases of plantar fasciitis. Studies also demonstrated that ESWT may be an appropriate treatment for myofascial trigger points. This study was designed to evaluate its effectiveness by comparing the ESWT of Gastrocnemius/Soleus (gastroc-soleus) trigger points and heel region with the ESWT of the heel region alone.
Materials and Methods:
The study was carried out among 40 patients with a clinical diagnosis of plantar fasciitis, divided randomly to case (n = 20) and control (n = 20) groups. The case group received ESWT for the heel region and for the gastroc-soleus trigger points. The control group received ESWT just for the heel region. The protocol was the same in both groups and they were treated for three sessions every week. The pain score (100 mm visual analog score [VAS]) and the modified Roles and Maudsley score was evaluated before the first session and eight weeks after the last session.
Results:
Eight weeks after the last session, although the mean VAS had decreased significantly in both groups, this decrement was more significant in the case group. (P = 0.04). According to the modified Roles and Maudsley score, there was a significant improvement in both the case (P < 0.001) and control (P = 0.01) groups, eight weeks after treatment, but there were significantly better results in the case group.
Conclusion:
The combination of ESWT for both plantar fasciitis and gastroc-soleus trigger points in treating patients with plantar fasciitis is more effective than utilizing it solely for plantar fasciitis.
Keywords: Extracorporeal shock wave therapy, plantar fasciitis, trigger points
INTRODUCTION
Plantar fasciitis is the most common cause of inferior heel pain, and may account for up to 15% of all foot symptoms requiring professional care among adults. Plantar fasciitis affects women slightly more often than men.[1] The incidence peaks between the ages of 40 and 60 years.[2] Increased bodyweight and work on hard surfaces are the risk factors.[3,4,5] Reduced range of ankle dorsiflexion is associated with plantar fasciitis,[3] as are calf and hamstring tightness.[6]
A great variety of therapies have been reported for the treatment of plantar fasciitis, including local steroid injections, platelet-rich plasma, intralesional botulinum toxin A (BTX-A), extracorporeal shock wave therapy, and a combination of all of these treatments with stretching exercises of the gastrocnemius and soleus muscles, or the plantar fascia.[7,8,9,10,11,12,13,14] Additionally, the effectiveness of trigger point needling in relieving plantar heel pain has been shown in some studies.[15,16,17] Some studies have also demonstrated that ESWT may be an appropriate treatment for myofascial trigger points.[18,19]
As there is a lack of studies evaluating the effectiveness of ESWT of the gastroc-soleus trigger points in the treatment of plantar fasciitis, we designed this study to evaluate its effectiveness by comparing ESWT of the gastroc-soleus trigger points and heel region with the ESWT of the heel region alone.
MATERIALS AND METHODS
This study is a randomized, placebo-controlled trial, which was carried out from March 2012 to November 2012, among 40 patients, with a clinical diagnosis of plantar fasciitis, referred to the Outpatient Clinics of Kashani University Hospital, Isfahan, Iran [Figure 1]. The patients who met the following inclusion criteria were included into the study: (1) Patients who had heel pain felt it localized to the site of the insertion of the plantar fascia and intrinsic muscles on the medial calcaneal tuberosity on the anterior-medial aspect of the heel for at least six months. (2) Patients who had at least one gastroc-soleus trigger point concomitantly. (3) Patients who did not respond to conservative treatments for at least three months. (4) Patients who were between 20 and 60 years of age, and had signed the informed consent form.
Figure 1.
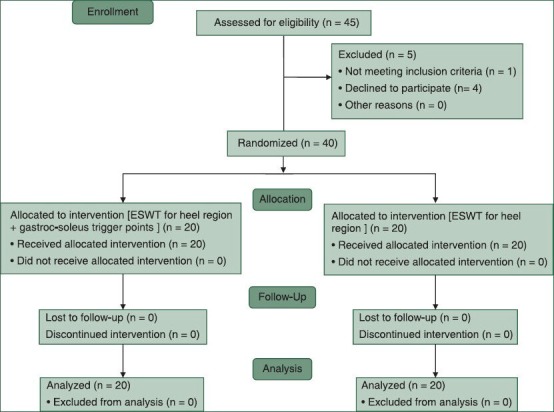
CONSORT 2010 Flow Diagram of randomized clinical trial: number of participants screened, randomized, and retained and analyses
Exclusion criteria of the study were: (1) Dysfunction of the knee or ankle, local arthritis, generalized polyarthritis, rheumatoid arthritis, ankylosing spondylitis, and Reiter syndrome. (2) Neurologic abnormalities. (3) Bleeding tendency (hereditary or acquired). (4) Nerve entrapment syndromes such as the tarsal tunnel syndrome. (5) Previous operation on the heel. (6) Pregnancy. (7) Evidences of infection in the lower limbs. (8)Medical history of tumor. (9) Patients who had received local corticosteroid injection within 12 weeks.
The patients were divided randomly into case (n = 20) and control (n = 20) groups. The case group received extracorporeal shock wave therapy (ESWT) (3000 shock waves/session of 0.2 mJ/mm2) for the heel region and (400 shock waves/session of 0.2 mj/mm2 per each trigger point) for the gastroc-soleus trigger points. The control group received ESWT (3000 shock waves/session of 0.2 mj/mm2) for just the heel region. The protocol was the same in both groups and they were treated for three sessions every week. The Duolith SD1 shock wave machine was used and shock waves were applied to the site of maximum local tenderness.
The pain score (100 mm visual analog score [VAS]) and the modified Roles and Maudsley score were evaluated before the first session and eight weeks after the last session. The modified Roles and Maudsley score was a patient-administered scoring system (see table A on bmj.com).[20]
The article has been submitted and registered in www.clinicaltrial.gov as RCT number: NCT01786057.
Statistical analysis
Statistical analyses were performed using the statistical package for social sciences (SPSS) statistical package version 13.0 (SPSS Inc., Chicago, IL, USA). Independent sample t-test or Mann–Whitney U-test, paired t-test or Repeated Measure ANOVA test, and the Chi Chi-square test were used to assess the differences between stages, as appropriate. A P-value less than 0.05 was considered significant.
RESULTS
Among 45 patients who had plantar fasciitis, five patients did not pass the screening protocol because they refused treatment (four patients), or were withdrawn because of violation of the selection criteria at entry (one patient).
A total number of 40 patients were investigated after taking anamnesis and a thorough physical examination. In case group there were seven males (35%) and 13 females (65%) and the control group had six males (30%) and 14 females (70%). According to gender there was no significant difference between the two groups.
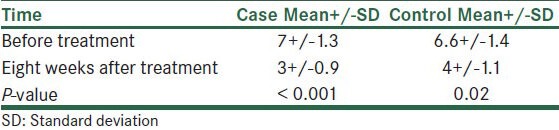
The results showed that the mean VAS scores did not differ significantly before treatment between the case and control groups (P < 0.001). Eight weeks after the last session, the mean VAS was significantly lower in the case group (P < 0.05). Although the mean VAS had decreased significantly in both groups, this decrement was more significant in the case group. (P = 0.04) [Table 1].
Table 1.
Comparison of the visual analog scale scores before and after treatment within the case and control groups
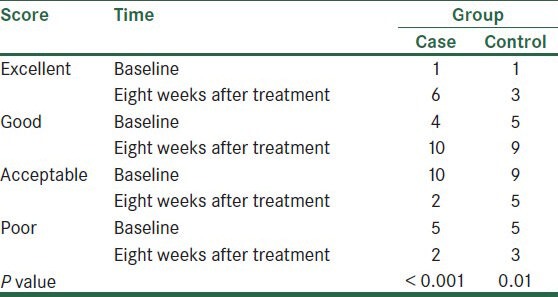
According to the modified Roles and Maudsley score, there was no significant difference between the baseline scores of the two groups (P = 0.86). The results revealed that there was a significant improvement in both groups eight weeks after the last session, but the Wilcoxon test showed significantly better results in the case group [Table 2].
Table 2.
Comparison of results of modified Roles and Maudsley score before and eight weeks after treatment in the case and control groups
Power analysis demonstrated that a sample size of 20 plantar fasciitis groups would be necessary to show that ESWT for both the gastroc-soleous trigger points and the heel region was more accurate than ESWT for the heel region solely. (α = 0.05; β = 0.80). Here, the power of the test means the probabilityof rejecting the null hypothesis, given that the alternative hypothesis is true. The result is a decision regarding the sample size at a given α level (0.05) and statistical power (0.80).
DISCUSSION
As we have described, in recent years, several treatment options, including dry needling, injection of therapeutic medications (local anesthetics, steroids, botulinum toxin A), and ESWT have been studied for plantar fasciitis treatment.[7,8,9,10,11,12,13,14,15,16,17] The local steroid injection is an alternative treatment, which is commonly used for refractory plantar fasciitis. It has been shown that it may cause plantar fascia rupture, fat pad atrophy, lateral plantar nerve injury secondary to injection, and calcaneal osteomyelitis.[21,22] During the past decade, ESWT has been used increasingly worldwide, and based on some well-controlled trials, it has been recently approved by the food and drug administration (FDA) for treatment of plantar fasciitis in the United States of America.[23]
It is a relatively safe procedure and can be considered before any surgical treatment. It may be preferable to try it before a local steroid injection.[24] Its proposed mechanism is cavitation of the deep tissue, which causes micro rupture of capillaries, leakage of the chemical mediators, and promotion of neovascularization of the damaged tissue.[25] A study demonstrated that ESWT contributes to healing and pain reduction in plantar fasciitis, and ultrasound imaging is able to depict the morphological changes related to plantar fasciitis as a result of this therapy.[26]
A quasi-experimental trial using 1% lidocaine injections for the myofascial trigger points, has found a reduction in pain, when combined with physical therapy.[19] Two trials have investigated the effectiveness of trigger point needling in relieving plantar heel pain.[15,16] Another study shows that trigger point dry needling by improving the severity of heel pain, can be used as a good alternative option before proceeding to more invasive therapies of plantar fasciitis, despite the insignificant effect on the range of motion of the ankle joint.[17]
In this study we compared the effectiveness of ESWT for both the heel region and gastroc-soleus trigger points with ESWT just for the heel region. As the results showed, although both VAS and the modified Roles and Maudsley score had improved in both groups, the results were significantly better in the case group compared to the control group. This difference could be due to the fact that the myofascial trigger points of the calf muscles played an important role in pain perception and functional impairment of patients with plantar fasciitis. The improvement in both groups was consistent with the other studies that examined the effectiveness of ESWT in plantar fasciitis.
Indeed, as we performed this study to evaluate the effectiveness of ESWT for gastroc-soleus trigger points in plantar fasciitis, we did not compare the different methods for applying that (e.g., radial vs. focus). Further studies are recommended to find out the mechanisms of action of ESWT on gastroc-soleus trigger points during the treatment of plantar fasciitis, along with comparing the different methods, to find the best method and dosage.
On the basis of our findings, in summary, it can be stated that a combination of ESWT for both plantar fasciitis and gastroc-soleus trigger points in treating patients with plantar fasciitis is more effective than utilizing it solely for plantar fasciitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Riddle DL, Pulisic M, Sparrow K. Impact of demographic and impairment related variables on disability associated with plantar fasciitis. Foot Ankle Int. 2004;25:311–7. doi: 10.1177/107110070402500506. [DOI] [PubMed] [Google Scholar]
- 2.Tu P, Bytomski JR. Diagnosis of heel pain. Am Fam Physician. 2011;84:909–16. [PubMed] [Google Scholar]
- 3.Irving DB, Cook JL, Menz HB. Factors associated with chronic plantar heel pain: A systematic review. (23-4).J Sci Med Sport. 2006;9:11–22. doi: 10.1016/j.jsams.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for plantar fasciitis: A matched case-control study. J Bone Joint Surg Am. 2003;85-A:872–7. doi: 10.2106/00004623-200305000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Werner RA, Gell N, Hartigan A, Wiggerman N, Keyserling WM. Risk factors for plantar fasciitis among assembly plant workers. PM R. 2010;2:110–6. doi: 10.1016/j.pmrj.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Labovitz JM, Yu J, Kim C. The role of hamstring tightness in plantar fasciitis. Foot Ankle Spec. 2011;4:141–4. doi: 10.1177/1938640010397341. [DOI] [PubMed] [Google Scholar]
- 7.DiGiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, et al. Plantar fasciaspecific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year of follow-up. J Bone Joint Surg Am. 2006;88:1775–81. doi: 10.2106/JBJS.E.01281. [DOI] [PubMed] [Google Scholar]
- 8.Glazer JL. An approach to the diagnosis and treatment of plantar fasciitis. Phys Sports Med. 2009;37:74–9. doi: 10.3810/psm.2009.06.1712. [DOI] [PubMed] [Google Scholar]
- 9.Placzek R, Deuretzbacher G, Meiss AL. Treatment of chronic plantar fasciitis with botulinum toxin A: Preliminary clinical results. Clin J Pain. 2006;22:190–2. doi: 10.1097/01.ajp.0000169674.34191.0e. [DOI] [PubMed] [Google Scholar]
- 10.Rompe JD, Cacchio A, Well L, Jr, Furia JP, Haist J, Reiners V, et al. Plantar fascia specific stretching versus radial shock-wave therapy as initial treatment of plantar fasciopathy. J Bone Joint Surg Am. 2010;92:2514–22. doi: 10.2106/JBJS.I.01651. [DOI] [PubMed] [Google Scholar]
- 11.Sampson S, Gerhardt M, Mandelbaum B. Platelet rich plasma injection grafts for musculoskeletal injuries: A review. Curr Rev Musuculoskelet Med. 2008;1:165–74. doi: 10.1007/s12178-008-9032-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seyler TM, Smith BP, Marker DR, Ma J, Shen J, Smith TL, et al. Botulinum neurotoxin as a therapeutic modality in orthopaedic surgery: More than twenty years of experience. J Bone Joint Surg Am. 2008;90:133–45. doi: 10.2106/JBJS.H.00901. [DOI] [PubMed] [Google Scholar]
- 13.Soomekh DJ. Using platelet-rich plasma in the foot and ankle. Foot Ankle Spec. 2010;3:88–90. doi: 10.1177/1938640010364483. [DOI] [PubMed] [Google Scholar]
- 14.Tsai WC, Hsu CC, Chen CP, Chen MJ, Yu TY, Chen YJ. Plantar fasciitis treated with local steroid injection: Comparison between sonographic and palpation guidance. J Clin Ultrasound. 2006;34:12–6. doi: 10.1002/jcu.20177. [DOI] [PubMed] [Google Scholar]
- 15.Tillu A, Gupta S. Effect of acupuncture treatment on heel pain due to plantar fasciitis. Acupunct Med. 1998;16:66–8. [Google Scholar]
- 16.Perez-Millan R, Foster L. Low frequency electroacupuncture in the management of refractory plantar fasciitis. Acupunct Med. 2001;13:1–6. [Google Scholar]
- 17.Eftekhar-Sadat B, Babaei-Ghazani A, Zeinolabedinzadeh V. Evaluation of dry needling in patients with chronic heel pain due to plantar fasciitis. Foot (Edinb) 2012 Nov 28; doi: 10.1016/j.foot.2012.09.003. pii: S0958-2592(12)00107-1. [DOI] [PubMed] [Google Scholar]
- 18.Müller-Ehrenberg H, Licht G. Diagnosis and therapy of myofascial pain syndrome with focused shock waves (ESWT) Medizinisch Orthopädische Technik. 2005;5:1–6. [Google Scholar]
- 19.Ji HM, Kim HJ, Han SJ. Extracorporeal shock wave therapy in myofascial pain syndrome of upper trapezius. Ann Rehabil Med. 2012;36:675–80. doi: 10.5535/arm.2012.36.5.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roles NC, Maudsley RH. Radial tunnel syndrome: Resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br. 1972;54:499–508. [PubMed] [Google Scholar]
- 21.Acevedo JI, Beskin JL. Complications of plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1998;19:91–7. doi: 10.1177/107110079801900207. [DOI] [PubMed] [Google Scholar]
- 22.Sellman JR. Plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1994;15:376–81. doi: 10.1177/107110079401500706. [DOI] [PubMed] [Google Scholar]
- 23.Henney JE. From the food and drug administration: Shock wave for heel pain. JAMA. 2000;284:2711. doi: 10.1001/jama.284.21.2711-jfd00010-2-1. [DOI] [PubMed] [Google Scholar]
- 24.Hyer CF, VanCourt R, Block A. Evaluation of ultrasound-guided extracorporeal shock wave therapy in the treatment of chronic plantar fasciitis. J Foot Ankle Surg. 2005;44:137–43. doi: 10.1053/j.jfas.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Tahririan MA, Motififard M, Tahmasebi MN, Siavashi B. Plantar fasciitis. J Res Med Sci. 2012;17:799–804. [PMC free article] [PubMed] [Google Scholar]
- 26.Vahdatpour B, Sajadieh S, Bateni V, Karami M, Sajjadieh H. Extracorporeal shock wave therapy in patients with plantar fasciitis. A randomized, placebo-controlled trial with ultrasonographic and subjective outcome assessments. J Res Med Sci. 2012;17:834–8. [PMC free article] [PubMed] [Google Scholar]


