Abstract
Ligation of the TNF receptor family co-stimulatory molecule OX40 (CD134) with an agonist anti-OX40 mAb enhances antitumor immunity by augmenting T cell differentiation as well as turning off the suppressive activity of the FoxP3+CD4+ regulatory T cells (Treg). In addition, antibody-mediated blockade of the checkpoint inhibitor CTLA-4 releases the “brakes” on T cells to augment tumor immunotherapy. However, monotherapy with these agents have limited therapeutic benefit particularly against poorly immunogenic murine tumors. Therefore, we examined whether the administration of agonist anti-OX40 therapy in the presence of CTLA-4 blockade would enhance tumor immunotherapy. Combined anti-OX40/anti-CTLA-4 immunotherapy significantly enhanced tumor regression and the survival of tumor-bearing hosts in a CD4 and CD8 T cell-dependent manner. Mechanistic studies revealed that the combination immunotherapy directed the expansion of effector T-bethigh/Eomeshigh granzyme B+ CD8 T cells. Dual immunotherapy also induced among distinct populations of Th1 (IL-2, IFNγ) and, surprisingly, Th2 (IL-4, IL-5, and IL-13) CD4 T cells exhibiting increased T-bet and Gata-3 expression. Furthermore, IL-4 blockade inhibited the Th2 response, while maintaining the Th1 CD4 and effector CD8 T cells that enhanced tumor-free survival. These data demonstrate that refining the global T cell response during combination immunotherapy can further enhance the therapeutic efficacy of these agents.
Introduction
The generation of potent cytotoxic CD8 T cells capable of destroying tumors requires T cell receptor (TCR) stimulation along with the provision of co-stimulatory signals (1). Previous studies have shown that ligation of the tumor necrosis factor receptor (TNFR) family co-stimulatory receptor OX40 (CD134) on T cells can significantly enhance antitumor immunity against various tumor types, including melanoma, breast, and prostate cancer (2). Mechanistic studies have revealed that OX40 ligation with an agonist anti-OX40 mAb boosts cytokine production and the expression of pro-survival molecules associated with enhanced T cell expansion, differentiation, and the generation of long-lived memory cells (3–5). OX40 ligation has also been shown to augment or inhibit the expansion and suppressive activity of CD4+CD25+FoxP3+ regulatory T cells (Treg) depending on several factors, including the cytokine milieu present during stimulation (6–9).
CTLA-4 is a negative regulatory protein that serves as a checkpoint inhibitor to limit T cell responses by attenuating T cell proliferation and cytokine production. In tumor-bearing hosts, inhibition of CTLA-4 improves antitumor immunity by releasing the “brakes” on T cells (10). CTLA-4 blockade was shown to improve the overall survival in patients with metastatic (stage IV) melanoma highlighting the efficacy of this cancer immunotherapy (11). Current studies are investigating whether CTLA-4 blockade has similar benefits for patients with breast, lung, or prostate cancer (12–15).
OX40 and CTLA-4 are both up-regulated on CD4 and CD8 T cells shortly after TCR stimulation and are constitutively expressed on Treg (16–18). Treatment with an agonist anti-OX40 mAb or CTLA-4 blockade has distinct and overlapping functional effects on different T cell compartments. For example, both anti-OX40 therapy and CTLA-4 blockade enhance the expansion and production of cytokines by naïve CD4 T cells (4, 10). However, anti-OX40 therapy drives significantly greater formation of long-lived memory CD4 T cells (19). OX40 ligation has been shown to augment CD8 T cell expansion and effector differentiation through a combination of CD8 T cell direct and indirect pathways. Studies have revealed that during priming CTLA-4 blockade indirectly enhances CD8 T cell effector function through cell-extrinsic effects on the responding CD8 T cells (20–24). OX40 and CTLA-4 are constitutively expressed on Treg and anti-OX40 therapy or CTLA-4 blockade has been shown to alleviate Treg suppression, although there are reports that under certain conditions OX40 ligation can drive Treg expansion (6–9, 18, 25, 26).
Pre-clinical data have shown that monotherapy with anti-OX40 or anti-CTLA-4 has limited therapeutic efficacy against many tumor types, suggesting that combination immunotherapy likely will be required to generate optimal therapeutic responses. We hypothesized that OX40 ligation in the presence of CTLA-4 blockade would augment tumor immunotherapy by simultaneously increasing the number and function of effector CD4 and CD8 T cells, while relieving the inhibitory effects of Treg. Indeed, recent work demonstrated that combined anti-OX40/anti-CTLA-4 therapy in the presence of repeated intratumoral vaccination with the TLR ligand CpG improved antitumor immunity in a murine lymphoma model (27). Therapeutic efficacy of this regimen was associated with increased IFNγ expression by T cells and a concomitant reduction in the frequency of Treg in the tumor. However, this study the authors only examined the effects of combination therapy versus CpG alone; there was no comparison of the effects of single versus dual therapy, or analysis of the effects on CD8 T cell differentiation and the impact on the cytokine milieu. In the current study, we demonstrate that in tumor-bearing mice the combined anti-OX40/anti-CTLA-4 regimen improves the limited therapeutic efficacy of monotherapy by augmenting the Th1/Th2 CD4 and effector CD8 T cell responses. In addition, limiting Th2 CD4 T cells via IL-4 blockade further enhances tumor immunotherapy. These data provide insight into the mechanisms by which the combined anti-OX40/anti-CTLA-4 immunotherapy drives potent polyclonal effector T cells responses and suggest that the clinical combination of these agents may offer a novel means of boosting tumor immunotherapy in patients with cancer.
Materials and Methods
Mice
Wild-type C57BL/6 mice were purchased from Jackson Labs (Bar Harbor, ME). OT-I Thy1.1 TCR Tg and POET-1 Tg mice (28) were bred in our facility. All mice were bred and maintained under specific pathogen-free conditions in the Providence Portland Medical Center animal facility. Experimental procedures were performed according to the NIH Guide for the Care and Use of Laboratory Animals.
Lymphocyte isolation and analysis
Peripheral (axillary, brachial, and inguinal) lymph nodes were harvested and processed to obtain single cell suspensions. ACK lysing buffer (Lonza, Walkersville, MD) was added for 5 min at RT to lyse red blood cells. Cells were rinsed with RPMI 1640 medium containing 10% FBS (10% cRPMI), 1M HEPES, non-essential amino acids, sodium pyruvate (Lonza), and pen-strep glutamine (Invitrogen, Grand Island, NY). For flow cytometry analysis, cells were incubated for 30 min at 4° C with: Ki-67 FITC, FoxP3 eFluor 450, granzyme B PE, CD3 eFluor 710, CD4 V500, CD4 FITC, CD8 eFluor 605, CD8 PE-Cy7, Thy1.1 eFluor 450, KLRG-1 APC, CD25 Alexa Fluor 700, IL-2 PE, IL-2 Alexa Fluor 700, IL-4 FITC, IL-5 PE, IL-13 eFluor 710, TNF-α PE-Cy7, IFNγ APC, Bcl-6 PE, Eomes eFluor 710, T-bet PE-Cy7, Gata-3 eFluor 660, and Fixable Viability Dye eFluor 780. All antibodies were obtained from eBioscience (San Diego, CA), BD Biosciences (San Jose, CA), BioLegend (San Diego, CA), or Invitrogen. Flow cytometry plots were gated on viable CD3+ T cells excluding doublets. For intracellular staining, cells were fixed and permeabilized with the FoxP3 Staining Buffer Set (eBioscience). For intracellular cytokine production, lymphocytes were stimulated with 5 μg/ml plate-bound anti-CD3 (clone 2C11) or SPAS-1 (SNC9-H8; STHVNHLHC) peptide in 10% cRPMI with 1 μl/ml of brefeldin A containing Golgi-Plug solution (BD Biosciences) for 4h at 37° C prior to intracellular staining. Cells were analyzed with an LSR II flow cytometer using FACSDiva software (BD Biosciences).
Cytokine production multiplex ELISA
CD4 or CD8 T cells were purified by cell sorting (B220/CD11b/MHC II−) and 2×106 cells/well were stimulated with media or plate-bound anti-CD3 (2 μg/ml) in 24-well plates. Supernatants were collected after 24h and cytokine expression was determined using a FlowCytomix Th1/Th2/Th17 kit (eBioscience). Cytokine expression levels were visualized with a heatmap using the Genesis software package (29). Cytokine expression levels were log2 transformed and shown in a yellow/red (low/high) scale.
Tumor challenge and TIL isolation
7.5×105 (for monotherapy or combination therapy) or 1×106 TRAMP-C1 (for tumor harvest and IL-4 blockade) murine prostate tumor cells or 1×106 MCA-205 murine sarcoma cells were injected (day 0; sq) into male C57BL/6 mice. TRAMP-C1 and MCA-205 cells were kindly provided by Dr. Andy Weinberg (EACRI, Portland, OR). TRAMP-C1-mOVA tumor cells were generated in our laboratory and described previously (20). 2×106 TRAMP-C1-mOVA cells were injected (day 0; sq) into male POET-1 Tg mice. All cell lines were tested and confirmed to be Mycoplasma-free using the MycoAlert detection kit (Lonza). TRAMP-C1 tumor-bearing mice received rat IgG (200 μg; Sigma), anti-OX40 (250 μg; clone OX86; BioXCell, Lebanon, NH), and/or anti-CTLA-4 (200 μg; clone 9D9; BioXCell) mAb at the indicated time points. All mAbs were verified to be endotoxin-free and injected ip into recipient mice. T cells were depleted with anti-CD4 (clone GK1.5) and/or anti-CD8 (clone 53-6.72) mAb on day 3, 10, and 17 (200 μg) post-tumor inoculation. For IL-4 blockade, anti-IL-4 mAb (clone 11B.11) was given every 2–3 days (200 μg; ip) for 3 weeks (NCI Biological Resources Branch Preclinical Repository, Frederick, MD). Tumor growth (area) was assessed every 2–3 days with micro-calipers and mice were sacrificed when tumors reached >150 mm2. Tumor infiltrating lymphocytes (TIL) were harvested by dissection of tissue into small fragments followed by digestion in 1 mg/ml collagenase (Invitrogen), 100 μg/ml hyaluronidase (Sigma), and 20 mg/ml DNase (Sigma) in PBS for 30 min at RT. Following filtration through nylon mesh, lymphocytes were stained and analyzed by flow cytometry as described.
Adoptive transfer and activation of OT-I T cells
Single cell suspensions were prepared from the spleens of OT-I Thy1.1 TCR Tg mice. OT-I T cells were purified by negative selection using the Dynal mouse CD8 cell isolation kit (Invitrogen, Carlsbad, CA) and injected (iv; day 0) in 200 μl of PBS into TRAMP-C1-mOVA tumor-bearing POET-1 Tg mice. Mice were then treated with 100 μg anti-OX40 (clone OX86) or control rat IgG Ab (day 0, 1), and/or 200 μg anti-CTLA-4 mAb (clone 9D9; day 0, 2, 4).
Treg functional assay
TRAMP-C1 tumor-bearing mice received anti-OX40 mAb or rat Ig (d4, 8) +/− anti-CTLA-4 mAb (d4, d6, d8). Eight or 9 days later (d12 or d13 post-tumor implantation), lymph nodes were harvested and CD4+CD25+ Treg (CD8/B220/CD11b/MHC II−) were isolated by cell sorting (>99% purity). Treg were seeded in triplicate at 5×104 cells/well in 96-well round-bottom plates previously coated with plate-bound anti-CD3/anti-CD28 (2 μg/ml; overnight). Naïve responder CD8 cells (Teff) were prepared from wild-type mice using the Dynal CD8 T cell negative selection kit (Invitrogen), CFSE-labeled, and 5×104 cells/well were added to triplicate wells containing media (positive control) or Treg. 2×105 irradiated (3,000 rads) T-cell depleted (Dynal beads, Invitrogen) accessory cells were added to all wells. Cells were harvested after 72h, stained for CD8, and the extent of CFSE dilution in the CD8 responder cells was determined.
Statistical analysis
Statistical significance was determined using one-way ANOVA (for comparisons among 3 or more groups; with Tukey correction for multiple comparisons), student’s t-test (for comparisons between 2 groups; two-tailed), or Kaplan-Meier survival and log-rank (Mantel-Cox) test (for tumor survival studies) using GraphPad Prism software (GraphPad, San Diego, CA); P-value of <0.05 was considered significant; *P<0.05, **P<0.01; ***P<0.001.
Results
Agonist anti-OX40 therapy in the presence of CTLA-4 blockade augments the antitumor response
TRAMP-C1 prostate or MCA-205 sarcoma tumors were implanted into cohorts of wild-type mice. Four (TRAMP-C1) or eight (MCA-205) days later, tumor-bearing mice were treated with control Ab (rat IgG), agonist anti-OX40 mAb, blocking anti-CTLA-4 mAb, or combined anti-OX40/anti-CTLA-4 therapy. Monotherapy with anti-OX40 or anti-CTLA-4 had limited effects on tumor growth or survival, but the combined immunotherapy significantly enhanced tumor regression and survival (Fig. 1A–1C). The therapeutic efficacy was T cell-dependent as CD4 and/or CD8 T cell-depletion prior to the initiation of therapy abrogated the survival benefit of the combined anti-OX40/anti-CTLA-4 immunotherapy (Fig. 1D).
Figure 1. Agonist anti-OX40 therapy in the presence of CTLA-4 blockade augments tumor immunotherapy.
A–C) 7.5×105 TRAMP-C1 prostate or 1×106 MCA-205 sarcoma tumor cells were implanted into wild-type mice (d0; n=15 and 14/group, respectively). Tumor-bearing mice were treated with rat IgG, anti-OX40, and/or anti-CTLA-4 mAb. Treatment was initiated four (TRAMP-C1) or eight (MCA-205) days post-tumor inoculation and the extent of A) tumor growth (data indicates the number of tumor-free/total) and survival of B) TRAMP-C1 or C) MCA-205 tumor-bearing mice were determined. D) Cohorts of mice received 1×106 TRAMP-C1 tumors (d0) along with anti-CD4, anti-CD8, or anti-CD4/CD8 depleting mAb (d3, d10, d17; n=14/group). All mice were treated with anti-OX40/anti-CTLA-4 therapy (as in (A)) and survival was determined. Data are representative of cumulative results from 2 to 3 independent experiments.
Combined anti-OX40/anti-CTLA-4 therapy boosts CD4 and CD8 T cell expansion and differentiation, but does not alter the ratio of T effector to Treg or the Treg suppressor function
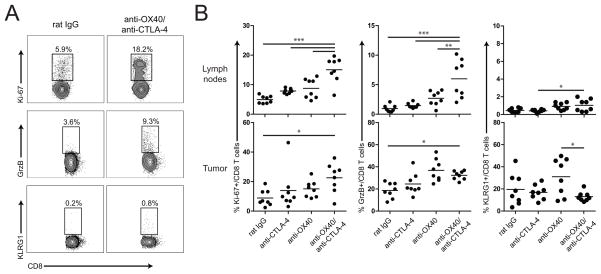
We characterized the phenotypic and functional response of the CD8 T effector, CD4 T effector, and CD4 Treg cells isolated from the lymph nodes and tumors following combination immunotherapy. Dual anti-OX40/anti-CTLA-4 therapy enhanced significantly the proliferation and effector function of the CD8 T cells as characterized by the expression of Ki-67 and granzyme B, respectively (Fig. 2A, B). We observed in the lymph nodes low levels of expression of KLRG-1, a marker of terminal differentiation and senescence in activated T cells (30, 31), regardless of treatments (<2% KLRG-1+/total CD8 T cells; Fig. 2B). KLRG-1 expression was markedly increased on tumor-infiltrating CD8 T cells (~20–30% KLRG-1+/total CD8 T cells; Fig. 2B); however, there was a trend towards lower KLRG-1 expression on CD8 T cells present in the tumors of anti-OX40/anti-CTLA-4 treated mice, which corresponded with a higher proliferative index (Fig. 2B; % Ki-67+/CD8 T cells in the tumor). These data suggest that anti-OX40/anti-CTLA-4 therapy may help retain the proliferative capacity of tumor-reactive T cells by limiting their terminal differentiation into KLRG-1+ CD8 T cells.
Figure 2. Combined anti-OX40/anti-CTLA-4 therapy boosts CD8 T cell expansion and differentiation.
Cohorts of mice received 1×106 TRAMP-C1 tumors (d0) along with anti-OX40/rat IgG (d17, d21) in the presence or absence of CTLA-4 blockade (d17, d19, d21). Eight days later (d25 post-tumor implantation), A, B) lymph nodes and B) tumors were harvested and the extent of CD8 T cell proliferation (Ki-67) and differentiation (granzyme B, KLRG-1) were determined by flow cytometry. Graphs are representative of the results obtained from A) individual mice or B) cumulative data (n=8/group) from two independent experiments. *P<0.05, **P<0.01, ***P<0.001
We evaluated the effects of combined anti-OX40/anti-CTLA-4 immunotherapy on effector and regulatory CD4 T cells. Analogous to its effects on CD8 T cells, dual therapy increased the proliferation (Ki-67) of effector FoxP3−CD4+ T cells as compared to the other groups (Fig. 3A, B). While the frequency of FoxP3+CD4 T cells in the lymph nodes increased, the frequency of Treg within the tumor did not change following combination immunotherapy (Fig. 3C, D). Similarly, total cell numbers were relatively unchanged among the treatment groups (Supplemental Fig. 1). Other studies have demonstrated that CTLA-4 blockade augments tumor immunotherapy in part by increasing the ratio of effector to regulatory T cells (25, 32). We analyzed the effect of anti-OX40/anti-CTLA-4 therapy on the effector to Treg ratio in tumor-bearing mice. Mono- or dual-therapy did not increase the ratio of effector CD8 or CD4 T cells to Treg; instead, there was a slight decrease in the Teff/Treg ratio in the lymph nodes (Fig. 4A, 4B). To investigate whether the combination immunotherapy abrogated the suppressive activity of Treg, CD4+CD25+ T cells were isolated by cell sorting from tumor-bearing hosts treated with either the control Ab (rat IgG), anti-OX40, anti-CTLA-4, or combined anti-OX40/anti-CTLA-4. Titrated numbers of Treg were co-cultured with CFSE-labeled CD8 T cells and the extent of proliferation was determined after 72 hrs. Treg isolated from mice receiving either monotherapy or combination immunotherapy exhibited comparable suppressor function (Fig. 4C), indicating that the therapeutic efficacy of dual immunotherapy was not due to an abrogation of suppressor Treg function.
Figure 3. Effects of anti-OX40/anti-CTLA-4 therapy on effector and regulatory CD4 T cells.
Cohorts of TRAMP-C1 tumor-bearing mice were treated with anti-OX40 and/or anti-CTLA-4 (as in Fig. 2). Eight days later (d25 post-tumor implantation), lymph nodes and tumors were harvested and the phenotype of A) FoxP3− effector CD4 T cells and C) FoxP3+ regulatory CD4 T cells were determined by flow cytometry. A, C) Graphs depict representative data from the lymph nodes of individual mice. A, B) The extent of proliferation (Ki-67) of FoxP3−CD4+ T cells was assessed. C, D) The frequency of FoxP3+ Treg/total CD4 T cells and proliferation (Ki-67) of FoxP3+CD4+ T cells was determined. Graphs are representative of the results obtained from A, C) individual mice or B, D) cumulative data (n=8/group) from two independent experiments. *P<0.05, **P<0.01, ***P<0.001
Figure 4. Effects of anti-OX40/anti-CTLA-4 therapy on regulatory T cell accumulation and suppressor function.
A–D) Cohorts of TRAMP-C1 tumor-bearing mice were treated with anti-OX40 and/or anti-CTLA-4 (as in Fig. 2). Eight days post-treatment, lymph nodes and tumors were harvested and the ratio (based upon total cell numbers) of A) CD8 T cells or B) effector FoxP3−CD4+ T cells to FoxP3+CD4+ Treg cells was determined. C) In additional cohorts of mice, CD4+CD25+ T cells were isolated from the lymph nodes by cell sorting and then co-cultured with naïve CFSE-labeled responder CD8 T cells. Cells were harvested 72 hours later and the extent of CFSE dilution was determined by flow cytometry. D) TRAMP-C1 tumor-bearing mice were treated as above and 8 days later the % ICOS+ and ratio of ICOS+ CD4 Teff:Treg cells were determined by flow cytometry. Graphs depict the A, B, D) mean+/−SD (n=4–5/group) or C) mean+/−SEM (n=3/group) from one of two independent experiments. *P<0.05, ***P<0.001
Studies have revealed an integral role for the co-stimulatory molecule, ICOS, in mediating the antitumor efficacy of anti-CTLA-4 in mice. ICOS expression was associated with increased effector function among CD4 and CD8 T cells (33). Anti-CTLA-4 therapy led to a transient increase in ICOS-expressing T cells, which may serve as a prognostic factor for increased long-term survival (34–36). We investigated ICOS expression following anti-OX40/anti-CTLA-4 therapy in TRAMP-C1 tumor-bearing mice, and found a significant increase in ICOS-expressing CD4 Teff and Treg with a higher ratio of ICOS+ Teff:Treg following combination immunotherapy (Fig. 4D). No changes in ICOS expression were detected in the CD8 T cell compartment (data not shown). These data suggest that dual therapy augments ICOS expression, although further studies are needed to determine whether ICOS directly affects the function of CD4 Teff and Treg following anti-OX40/anti-CTLA-4 therapy.
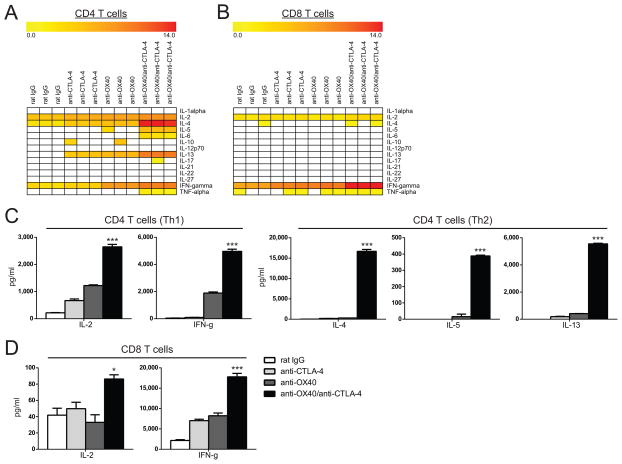
Agonist anti-OX40 therapy plus CTLA-4 blockade enhances CD4 and CD8 T cell cytokine production and generates distinct subsets of Th1 and Th2 CD4 T cells
TRAMP-C1 tumor-bearing mice were treated with the combined immunotherapy and the CD4 or CD8 T cells from the lymph nodes were purified by cell sorting and cytokine secretion was determined by multiplex ELISA following re-stimulation (24 hrs) with plate-bound anti-CD3 mAb. We observed a striking increase in the magnitude and breadth of cytokine production in the CD4 T cell compartment following combined immunotherapy including a significant increase in Th1 (IFNγ, IL-2) and, surprisingly, Th2 (IL-4, IL-5, IL-13) cytokines (Fig. 5A, 5C). Dual therapy also led to a significant increase in IL-2 and IFNγ production by the effector CD8 T cells (Fig. 5B, 5D).
Figure 5. Agonist anti-OX40 therapy plus CTLA-4 blockade enhances Th1 and Th2 cytokine production.
A–D) Cohorts of TRAMP-C1 tumor-bearing mice were treated with anti-OX40 (d4, d8) and/or CTLA-4 blockade (d4, d6, d8). Eight days later (d12 post-tumor implantation), CD4 and CD8 T cells were purified from the lymph nodes by cell sorting. Following stimulation for 24 hrs (with plate-bound anti-CD3), supernatants were collected and cytokine levels from A) CD4 or B) CD8 T cells were determined using a multiplex ELISA. Total cytokine levels (pg/ml) were log2 transformed and visualized with a heatmap (white squares indicate cytokines were not detected). C, D) Graphs depict the mean+/−SEM (n=3/group) from one of two independent experiments. *P<0.05, ***P<0.001
We investigated whether the combined therapy generated distinct Th1/Th2 subsets, or created multi-functional CD4 T cells as was shown in mice receiving anti-OX40 plus chemotherapy-induced lymphopenia (37). Cytokine expression was determined by intracellular cytokine staining (ICS) and flow cytometry and revealed distinct populations of CD4 T cells within the effector (FoxP3−) compartment; a Th1 subset containing IFNγ+ cells and a Th2 subset with IL-4+IFNγ− cells that included the IL-5+ and IL-13+ subset (Fig. 6A). No cytokine production was detected among the FoxP3+CD4+ T cells (data not shown). Combination immunotherapy also boosted the frequency and total number of cytokine-producing CD4 and CD8 T cells (Fig. 6C, 6D). Although NKT cells can also produce copious amounts of IL-4 (38, 39), anti-OX40/anti-CTLA-4 therapy did not increase the number of NKT cells nor did it elicit NKT cell-specific IL-4 production (data not shown).
Figure 6. Altered transcriptional programming of T cell following combination immunotherapy.
A–F) Cohorts of mice received 1×106 TRAMP-C1 tumor cells (d0) and then were treated with rat IgG/anti-OX40 (d4, d8) and/or anti-CTLA-4 (d4, d6, d8). Eight days later, lymph nodes were harvested and A-D) cells were re-stimulated with plate-bound anti-CD3 (4h) and the expression of the indicated cytokines was determined by flow cytometry. E–F) Cells were harvested as described above and expression (% and MFI) of the indicated transcription factors (Bcl-6, T-bet, Eomes, and Gata-3) was determined directly ex vivo by flow cytometry. Dot plots depict the data from individual mice and bar graphs depict the mean+/−SD (n=3–5/group) from one of two independent experiments. *P<0.05, **P<0.01, ***P<0.001
To determine whether the combined anti-OX40/anti-CTLA-4 therapy could augment the expansion of Ag-specific CD8 T cells, OVA-specific OT-I T cells were transferred into TRAMP-C1-mOVA tumor-bearing mice along with rat IgG, anti-CTLA-4, and/or anti-OX40 therapy. Seven days later, the Ag-specific CD8 T cell response was determined. The combination therapy increased significantly the expansion (% OT-I+/CD8) and differentiation (% grzB+/OT-I) of Ag-specific OT-I T cells in tumor-bearing mice (Suppl. Fig. 2A). SPAS-1 is an endogenous tumor-Ag expressed in TRAMP-C1 prostate tumor cells (40). We determined the frequency and function of prostate tumor (SPAS-1)-specific CD8 T cells in the TRAMP-C1 tumor-bearing mice. The combined anti-OX40/anti-CTLA-4 therapy boosted the frequency and total number of endogenous effector (IFNγ+) SPAS-1-specific CD8 T cells (Suppl. Fig. 2B).
T cell differentiation is regulated by the master transcription factors Bcl-6, T-bet, Eomes, and Gata-3. IFNγ-induced T-bet promotes Th1 differentiation; IL-4 induced Gata-3 favors Th2 development. Similarly, reciprocal expression of Bcl-6 and T-bet controls CD8 T cell differentiation; the less differentiated cells are Bcl-6high/T-betlow, while the terminal effector cells are Bcl-6low/T-bethigh (41, 42). Our data revealed that the dual anti-OX40/anti-CTLA-4 therapy led to increased T-bet and Gata-3-expressing CD4 T cells (Fig. 6E), which reflected increased Th1/Th2 cytokine production (Fig. 6C). We examined the co-expression of T-bet and Gata-3 among the different treatment groups and found that the combination therapy increased Gata-3 expression primarily in the T-betneg population (Suppl. Fig. 3). T-bethigh and Eomeshigh effector CD8 T cells were generated following combination immunotherapy (Fig. 6F).
Given the striking increase in Th2 cytokines, particularly IL-4, following anti-OX40/anti-CTLA-4 therapy, we asked whether the IL-4-producing Th2 CD4 T cells were beneficial or detrimental to the generation of antitumor immunity. Pilot studies demonstrated that the efficacy of combination therapy was reduced at higher tumor doses (data not shown). Therefore, we increased the initial dose of TRAMP-C1 tumors (to 1×106) and then treated tumor-bearing mice with rat IgG, anti-CTLA-4, anti-OX40, and/or anti-IL-4 mAb. IL-4 blockade was sufficient to abrogate the induction of the Th2 CD4 T cell response in tumor-bearing mice, while maintaining Th1 and effector CD8 T cells (Fig. 7A and 7B, respectively). More importantly, the inclusion of IL-4 blockade led to a striking increase in survival (Fig. 7D), while anti-IL-4 alone, or in combination with either anti-CTLA-4 or anti-OX40 monotherapy, had no effect (Fig. 7C).
Figure 7. IL-4 blockade limits Th2 differentiation following combined anti-OX40/anti-CTLA-4 therapy, while maintaining Th1 and effector CD8 T cells responses that enhance anti-tumor immunity.
A–D) Cohorts of mice received 1×106 TRAMP-C1 tumor cells (d0) and then were treated with anti-OX40 (d4, d8) and anti-CTLA-4 (d4, d6, d8) in the presence or absence of anti-IL-4 mAb (every 2–3 days starting on day 3 post-tumor inoculation). A-B) Eight days later (d12 post-tumor inoculation), lymph nodes were harvested and cells were re-stimulated with plate-bound anti-CD3 (4h) and the expression of the indicated cytokines was determined by flow cytometry. C, D) Tumor-bearing mice received anti-OX40/anti-CTLA-4 +/−anti-IL-4 mAb (as in (A)) and the survival of tumor-bearing mice was determined (n=12–17/total per group). A, B) Data depict the mean+/−SD (n=3–5/group) from one of two independent experiments. C, D) Data are representative of cumulative results from 2–3 independent experiments. *P<0.05, **P<0.01, ***P<0.001
Discussion
Studies have shown that anti-CTLA-4 or anti-OX40 mAb monotherapy can improve antitumor immunity (2, 10). CTLA-4 blockade significantly improved survival in patients with metastatic melanoma, highlighting the therapeutic potential of cancer immunotherapy (11). Despite these successes, only a fraction of patients benefited, suggesting that combination immunotherapy may help generate a more potent and broadly effective response. For example, pre-clinical studies have shown that repeated intratumoral vaccination with CpG in the presence of anti-OX40/anti-CTLA-4 therapy enhanced antitumor immunity in a murine lymphoma model (27). These data revealed an increase in IFNγ+ T cells in the tumors of mice receiving combination therapy.
In the current study, we demonstrated that combined anti-OX40/anti-CTLA-4 immunotherapy enhanced the survival of mice with TRAMP-C1 (prostate) or MCA-205 (sarcoma) tumors (Fig. 1A–1C) through a T cell-dependent mechanism (Fig. 1D). Dual anti-OX40/anti-CTLA-4 therapy resulted in a robust increase in effector CD4 and CD8 T cell expansion and differentiation (Fig. 2, 3), including a striking increase in cytokine production, including Th1 (IFNγ, IL-2) and Th2 (IL-4, IL-5, IL-13) cytokines (Fig. 5). OX40 ligation has been shown to promote either Th1 or Th2 responses, depending upon the cytokine milieu present during the priming of naïve CD4 T cells and the strength of TCR stimulation (43–45). Recent data from Hirschhorn-Cymerman et al., also identified strong Th1 and Th2-cytokine secretion following agonist anti-OX40 therapy in conjunction with lymphodepletion (with cyclophosphamide) and adoptive transfer of melanoma-specific (Trp1 TCR Tg) CD4 T cells (37), suggesting that combination therapy may direct the development of a novel bi-functional Th1/Th2-like population of CD4 T cells. Work from Villarino et al. highlighted the development of IL-13-producing Th1 and Th17 CD4 T cell subsets, even in the absence of IL-4Rα signaling (46). In contrast, our data showed that the combined anti-OX40/anti-CTLA-4 therapy led to the generation of distinct Th1 and Th2 CD4 T cell subsets (Fig. 6A), not bi-functional Th1/Th2 cells. The explanations for these disparate results are unclear, but may reflect differences in the complexity of boosting the endogenous polyclonal CD4 T cell compartment (the current study) versus the use of adoptively transferred TCR Tg CD4 T cells with a higher affinity for cognate antigen (37). Indeed, recent work showed that low affinity TCR stimulation preferentially leads to increased IL-4 production among CD4 T cells (47).
Anti-OX40 or anti-CTLA-4 monotherapy has also been shown to increase the formation of IL-17-producing CD4 T cells in murine models and in PBMC of patients with metastatic melanoma (48). However, we did not detect significant levels of IL-17 among any of the treatment groups (Fig. 5A), suggesting that increased IL-17 production was not responsible for the therapeutic efficacy we observed in the current study. Other groups have shown that OX40 ligation in the presence of IL-4 and TGF-β can induce CD4 differentiation into IL-9-producing Th9 cells (49). Although we detected high levels of IL-4 following dual immunotherapy (Fig. 5C), TGF-β and IL-9 were undetectable in any of the treatment groups (data not shown).
Along with the potent effects of combination immunotherapy on effector CD4 and CD8 T cell proliferation and differentiation (Fig. 2, 3), we also observed an expansion of Treg post-treatment (Fig. 3C, 3D). Reports have demonstrated that OX40 or CTLA-4-specific monotherapy can shift effector to regulatory T cell ratios in favor of effector cell expansion, relieve the inhibitory effects of Treg, reduce FoxP3 expression on Treg, and in certain circumstances, induce Treg apoptosis (7, 25, 50). However, our studies showed that single or dual anti-OX40/anti-CTLA-4 immunotherapy did not alter the effector CD8 or CD4 T cell to Treg ratios in the tumor (Fig. 4A and 4B, respectively), inhibit the suppressor function of Treg (Fig. 4C), reduce FoxP3 expression, or induce Treg apoptosis (data not shown) (51). Thus, it appears that the main effects of the therapy are through increasing the extent of cytokine-producing effector T cells, rather than inhibiting Treg function. The explanation for these differences remains unclear, but may reflect the different model systems utilized for these studies (e.g., cell lines, timing of tissue harvest). Another possibility is that in our study immune therapy was given in the absence of vaccination, while other groups administered anti-CTLA-4 mAb with a GM-CSF or FLT3-ligand-secreting vaccine (32, 52). When anti-CTLA-4 was used as a monotherapy in the absence of vaccination, no changes were seen in the Teff:Treg ratio (53). Notably, we did detect a significant increase in ICOS expression among Teff and Treg CD4 T cells following the combination therapy (Fig. 4D), although the functional consequence of this remains to be determined.
Recent work showed that combination immunotherapy with agonist anti-OX40 and anti-4-1BB mAbs favored the formation of T-bethigh/Eomeshigh CD4 T cells with enhanced effector function (54). Although we observed an increase in T-bethigh CD4 T cells, no differences were observed in Eomes expression following anti-CTLA-4/anti-OX40 therapy (Fig. 6E), suggesting that T-bet, rather than Eomes, up-regulation, was likely the main driver of effector CD4 T cells differentiation in this model system. Given that the IL-4-dependent induction of Th2 cells reduce, rather than promote, the therapeutic efficacy of the dual anti-OX40/anti-CTLA-4 therapy (Fig. 7D), it appears that directing the extent of Th1/Th2 responses may be an important consideration when translating these therapies into the clinic. We also found that anti-OX40/anti-CTLA-4 therapy induced the formation of T-bethigh/Eomeshigh CD8 T cells (Fig. 6F). Since a high T-bet:Eomes ratio is associated with increased effector CD8 T cell differentiation (42), it remains unclear whether the co-expression of these two transcription factors represents a transient or a long-lived stable population of effector/effector-memory CD8 T cells or a more central memory-like subset. Additional studies will be needed to clarify the role of transcriptional regulation of the CD8 T cell compartment in generating optimal tumor immunotherapy.
Th2-derived IL-4 can promote macrophage polarization towards an M2 phenotype, which in turn enhances tumor progression (55, 56). Similarly, tumor-induced myeloid-derived suppressor cells (MDSC) can also suppress T cell function to limit antitumor immunity (57, 58). Currently, we are examining whether IL-4 affects the expansion and/or suppressive activity of M2 macrophages or MDSC in TRAMP-C1 tumor-bearing mice receiving dual therapy. However, recent work has shown that MDSC accumulate slowly over a period of several weeks in TRAMP-C1 tumor-bearing mice (59). Thus, it is unlikely that potential changes in MDSC function significantly affected the ability of anti-OX40/anti-CTLA-4 therapy to enhance tumor regression as therapeutic efficacy was observed by 10–14 days post-treatment (Fig. 1A).
Despite the ability of combination immunotherapy to augment tumor regression, treatment of large well-established tumors remains challenging due to the induction of tumor-specific tolerance and immune-suppression. Given that the combined anti-OX40/anti-CTLA-4 therapy was able to boost Ag-specific CD8 T cell responses (Suppl. Fig. 2), it will be of great interest to investigate whether the inclusion of tumor-specific vaccination will facilitate the expansion of polyclonal tumor-reactive effector T cells capable of further enhancing tumor regression, particularly at later stages of disease. In summary, these data demonstrate that agonist anti-OX40 therapy in conjunction with CTLA-4 blockade improves the limited therapeutic efficacy of monotherapy to elicit potent antitumor immunity and provide the rationale to study the activity of combination regimens such as anti-OX40/anti-CTLA-4 therapy in clinical trials.
Supplementary Material
Acknowledgments
We thank the EACRI Vivarium for excellent technical assistance, our colleagues at the EACRI for helpful discussions and critical reading of the manuscript, and Mr. Dan Haley (EACRI Flow Cytometry Core Facility) for his assistance with cell sorting.
Grant support: V Foundation V Scholar Award, the Safeway Foundation, the Providence Portland Medical Foundation, and the NIH (5R00CA136678)
Footnotes
Potential Conflicts of Interest: None
References
- 1.Williams MA, Bevan MJ. Effector and memory CTL differentiation. Annu Rev Immunol. 2007;25:171–92. doi: 10.1146/annurev.immunol.25.022106.141548. [DOI] [PubMed] [Google Scholar]
- 2.Sugamura K, Ishii N, Weinberg AD. Therapeutic targeting of the effector T-cell co-stimulatory molecule OX40. Nat Rev Immunol. 2004;4:420–31. doi: 10.1038/nri1371. [DOI] [PubMed] [Google Scholar]
- 3.Redmond WL, Ruby CE, Weinberg AD. The role of OX40-mediated co-stimulation in T-cell activation and survival. Crit Rev Immunol. 2009;29:187–201. doi: 10.1615/critrevimmunol.v29.i3.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Croft M. Control of immunity by the TNFR-related molecule OX40 (CD134) Annu Rev Immunol. 2010;28:57–78. doi: 10.1146/annurev-immunol-030409-101243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watts TH. TNF/TNFR family members in costimulation of T cell responses. Annu Rev Immunol. 2005;23:23–68. doi: 10.1146/annurev.immunol.23.021704.115839. [DOI] [PubMed] [Google Scholar]
- 6.Piconese S, Valzasina B, Colombo MP. OX40 triggering blocks suppression by regulatory T cells and facilitates tumor rejection. J Exp Med. 2008;205:825–39. doi: 10.1084/jem.20071341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vu MD, Xiao X, Gao W, Degauque N, Chen M, Kroemer A, et al. OX40 costimulation turns off Foxp3+ Tregs. Blood. 2007;110:2501–10. doi: 10.1182/blood-2007-01-070748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.So T, Croft M. Cutting edge: OX40 inhibits TGF-beta- and antigen-driven conversion of naive CD4 T cells into CD25+Foxp3+ T cells. J Immunol. 2007;179:1427–30. doi: 10.4049/jimmunol.179.3.1427. [DOI] [PubMed] [Google Scholar]
- 9.Ruby CE, Yates MA, Hirschhorn-Cymerman D, Chlebeck P, Wolchok JD, Houghton AN, et al. Cutting Edge: OX40 agonists can drive regulatory T cell expansion if the cytokine milieu is right. J Immunol. 2009;183:4853–7. doi: 10.4049/jimmunol.0901112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Egen JG, Kuhns MS, Allison JP. CTLA-4: new insights into its biological function and use in tumor immunotherapy. Nat Immunol. 2002;3:611–8. doi: 10.1038/ni0702-611. [DOI] [PubMed] [Google Scholar]
- 11.Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.May KF, Jr, Gulley JL, Drake CG, Dranoff G, Kantoff PW. Prostate cancer immunotherapy. Clin Cancer Res. 2011;17:5233–8. doi: 10.1158/1078-0432.CCR-10-3402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vonderheide RH, LoRusso PM, Khalil M, Gartner EM, Khaira D, Soulieres D, et al. Tremelimumab in combination with exemestane in patients with advanced breast cancer and treatment-associated modulation of inducible costimulator expression on patient T cells. Clin Cancer Res. 2010;16:3485–94. doi: 10.1158/1078-0432.CCR-10-0505. [DOI] [PubMed] [Google Scholar]
- 14.Calabro L, Danielli R, Sigalotti L, Maio M. Clinical studies with anti-CTLA-4 antibodies in non-melanoma indications. Semin Oncol. 2010;37:460–7. doi: 10.1053/j.seminoncol.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Lynch TJ, Bondarenko I, Luft A, Serwatowski P, Barlesi F, Chacko R, et al. Ipilimumab in combination with paclitaxel and carboplatin as first-line treatment in stage IIIB/IV non-small-cell lung cancer: results from a randomized, double-blind, multicenter phase II study. J Clin Oncol. 2012;30:2046–54. doi: 10.1200/JCO.2011.38.4032. [DOI] [PubMed] [Google Scholar]
- 16.Taraban VY, Rowley TF, O’Brien L, Chan HT, Haswell LE, Green MH, et al. Expression and costimulatory effects of the TNF receptor superfamily members CD134 (OX40) and CD137 (4-1BB), and their role in the generation of anti-tumor immune responses. Eur J Immunol. 2002;32:3617–27. doi: 10.1002/1521-4141(200212)32:12<3617::AID-IMMU3617>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 17.Gramaglia I, Weinberg AD, Lemon M, Croft M. Ox-40 ligand: a potent costimulatory molecule for sustaining primary CD4 T cell responses. J Immunol. 1998;161:6510–7. [PubMed] [Google Scholar]
- 18.Takeda I, Ine S, Killeen N, Ndhlovu LC, Murata K, Satomi S, et al. Distinct roles for the OX40-OX40 ligand interaction in regulatory and nonregulatory T cells. J Immunol. 2004;172:3580–9. doi: 10.4049/jimmunol.172.6.3580. [DOI] [PubMed] [Google Scholar]
- 19.Evans DE, Prell RA, Thalhofer CJ, Hurwitz AA, Weinberg AD. Engagement of OX40 enhances antigen-specific CD4(+) T cell mobilization/memory development and humoral immunity: comparison of alphaOX-40 with alphaCTLA-4. J Immunol. 2001;167:6804–11. doi: 10.4049/jimmunol.167.12.6804. [DOI] [PubMed] [Google Scholar]
- 20.Redmond WL, Gough MJ, Charbonneau B, Ratliff TL, Weinberg AD. Defects in the Acquisition of CD8 T Cell Effector Function after Priming with Tumor or Soluble Antigen Can Be Overcome by the Addition of an OX40 Agonist. J Immunol. 2007;179:7244–53. doi: 10.4049/jimmunol.179.11.7244. [DOI] [PubMed] [Google Scholar]
- 21.Bansal-Pakala P, Halteman BS, Cheng MH, Croft M. Costimulation of CD8 T cell responses by OX40. J Immunol. 2004;172:4821–5. doi: 10.4049/jimmunol.172.8.4821. [DOI] [PubMed] [Google Scholar]
- 22.Gattinoni L, Ranganathan A, Surman DR, Palmer DC, Antony PA, Theoret MR, et al. CTLA-4 dysregulation of self/tumor-reactive CD8+ T cell function is CD4+ T cell-dependent. Blood. 2006;108:3818–23. doi: 10.1182/blood-2006-07-034066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shrikant P, Khoruts A, Mescher MF. CTLA-4 blockade reverses CD8+ T cell tolerance to tumor by a CD4+ T cell- and IL-2-dependent mechanism. Immunity. 1999;11:483–93. doi: 10.1016/s1074-7613(00)80123-5. [DOI] [PubMed] [Google Scholar]
- 24.Pedicord VA, Montalvo W, Leiner IM, Allison JP. Single dose of anti-CTLA-4 enhances CD8+ T-cell memory formation, function, and maintenance. Proc Natl Acad Sci U S A. 2011;108:266–71. doi: 10.1073/pnas.1016791108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peggs KS, Quezada SA, Chambers CA, Korman AJ, Allison JP. Blockade of CTLA-4 on both effector and regulatory T cell compartments contributes to the antitumor activity of anti-CTLA-4 antibodies. J Exp Med. 2009;206:1717–25. doi: 10.1084/jem.20082492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xiao X, Gong W, Demirci G, Liu W, Spoerl S, Chu X, et al. New Insights on OX40 in the Control of T Cell Immunity and Immune Tolerance In Vivo. J Immunol. 2012;188:892–901. doi: 10.4049/jimmunol.1101373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Houot R, Levy R. T-cell modulation combined with intratumoral CpG cures lymphoma in a mouse model without the need for chemotherapy. Blood. 2009;113:3546–52. doi: 10.1182/blood-2008-07-170274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lees JR, Charbonneau B, Swanson AK, Jensen R, Zhang J, Matusik R, et al. Deletion is neither sufficient nor necessary for the induction of peripheral tolerance in mature CD8+ T cells. Immunology. 2006;117:248–61. doi: 10.1111/j.1365-2567.2005.02293.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sturn A, Quackenbush J, Trajanoski Z. Genesis: cluster analysis of microarray data. Bioinformatics. 2002;18:207–8. doi: 10.1093/bioinformatics/18.1.207. [DOI] [PubMed] [Google Scholar]
- 30.Joshi NS, Cui W, Chandele A, Lee HK, Urso DR, Hagman J, et al. Inflammation directs memory precursor and short-lived effector CD8(+) T cell fates via the graded expression of T-bet transcription factor. Immunity. 2007;27:281–95. doi: 10.1016/j.immuni.2007.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Voehringer D, Koschella M, Pircher H. Lack of proliferative capacity of human effector and memory T cells expressing killer cell lectinlike receptor G1 (KLRG1) Blood. 2002;100:3698–702. doi: 10.1182/blood-2002-02-0657. [DOI] [PubMed] [Google Scholar]
- 32.Curran MA, Montalvo W, Yagita H, Allison JP. PD-1 and CTLA-4 combination blockade expands infiltrating T cells and reduces regulatory T and myeloid cells within B16 melanoma tumors. Proc Natl Acad Sci U S A. 2010;107:4275–80. doi: 10.1073/pnas.0915174107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fu T, He Q, Sharma P. The ICOS/ICOSL pathway is required for optimal antitumor responses mediated by anti-CTLA-4 therapy. Cancer Res. 2011;71:5445–54. doi: 10.1158/0008-5472.CAN-11-1138. [DOI] [PubMed] [Google Scholar]
- 34.Chen H, Liakou CI, Kamat A, Pettaway C, Ward JF, Tang DN, et al. Anti-CTLA-4 therapy results in higher CD4+ICOShi T cell frequency and IFN-gamma levels in both nonmalignant and malignant prostate tissues. Proc Natl Acad Sci U S A. 2009;106:2729–34. doi: 10.1073/pnas.0813175106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liakou CI, Kamat A, Tang DN, Chen H, Sun J, Troncoso P, et al. CTLA-4 blockade increases IFNgamma-producing CD4+ICOShi cells to shift the ratio of effector to regulatory T cells in cancer patients. Proc Natl Acad Sci U S A. 2008;105:14987–92. doi: 10.1073/pnas.0806075105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Di Giacomo AM, Calabro L, Danielli R, Fonsatti E, Bertocci E, Pesce I, et al. Long-term survival and immunological parameters in metastatic melanoma patients who responded to ipilimumab 10 mg/kg within an expanded access programme. Cancer Immunol Immunother. 2013;62:1021–8. doi: 10.1007/s00262-013-1418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hirschhorn-Cymerman D, Budhu S, Kitano S, Liu C, Zhao F, Zhong H, et al. Induction of tumoricidal function in CD4+ T cells is associated with concomitant memory and terminally differentiated phenotype. J Exp Med. 2012;209:2113–26. doi: 10.1084/jem.20120532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smyth MJ, Godfrey DI. NKT cells and tumor immunity--a double-edged sword. Nat Immunol. 2000;1:459–60. doi: 10.1038/82698. [DOI] [PubMed] [Google Scholar]
- 39.Godfrey DI, Hammond KJ, Poulton LD, Smyth MJ, Baxter AG. NKT cells: facts, functions and fallacies. Immunology today. 2000;21:573–83. doi: 10.1016/s0167-5699(00)01735-7. [DOI] [PubMed] [Google Scholar]
- 40.Fasso M, Waitz R, Hou Y, Rim T, Greenberg NM, Shastri N, et al. SPAS-1 (stimulator of prostatic adenocarcinoma-specific T cells)/SH3GLB2: A prostate tumor antigen identified by CTLA-4 blockade. Proc Natl Acad Sci U S A. 2008;105:3509–14. doi: 10.1073/pnas.0712269105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhu J, Yamane H, Paul WE. Differentiation of effector CD4 T cell populations (*) Annu Rev Immunol. 2010;28:445–89. doi: 10.1146/annurev-immunol-030409-101212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kaech SM, Cui W. Transcriptional control of effector and memory CD8+ T cell differentiation. Nat Rev Immunol. 2012;12:749–61. doi: 10.1038/nri3307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Flynn S, Toellner KM, Raykundalia C, Goodall M, Lane P. CD4 T cell cytokine differentiation: the B cell activation molecule, OX40 ligand, instructs CD4 T cells to express interleukin 4 and upregulates expression of the chemokine receptor, Blr-1. J Exp Med. 1998;188:297–304. doi: 10.1084/jem.188.2.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ohshima Y, Yang LP, Uchiyama T, Tanaka Y, Baum P, Sergerie M, et al. OX40 costimulation enhances interleukin-4 (IL-4) expression at priming and promotes the differentiation of naive human CD4(+) T cells into high IL-4-producing effectors. Blood. 1998;92:3338–45. [PubMed] [Google Scholar]
- 45.Rogers PR, Croft M. CD28, Ox-40, LFA-1, and CD4 modulation of Th1/Th2 differentiation is directly dependent on the dose of antigen. J Immunol. 2000;164:2955–63. doi: 10.4049/jimmunol.164.6.2955. [DOI] [PubMed] [Google Scholar]
- 46.Gallo E, Katzman S, Villarino AV. IL-13-producing Th1 and Th17 cells characterize adaptive responses to both self and foreign antigens. Eur J Immunol. 2012;42:2322–8. doi: 10.1002/eji.201142227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Milner JD, Fazilleau N, McHeyzer-Williams M, Paul W. Cutting edge: lack of high affinity competition for peptide in polyclonal CD4+ responses unmasks IL-4 production. J Immunol. 2010;184:6569–73. doi: 10.4049/jimmunol.1000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.von Euw E, Chodon T, Attar N, Jalil J, Koya RC, Comin-Anduix B, et al. CTLA4 blockade increases Th17 cells in patients with metastatic melanoma. J Transl Med. 2009;7:35. doi: 10.1186/1479-5876-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xiao X, Balasubramanian S, Liu W, Chu X, Wang H, Taparowsky EJ, et al. OX40 signaling favors the induction of T(H)9 cells and airway inflammation. Nat Immunol. 2012;13:981–90. doi: 10.1038/ni.2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hirschhorn-Cymerman D, Rizzuto GA, Merghoub T, Cohen AD, Avogadri F, Lesokhin AM, et al. OX40 engagement and chemotherapy combination provides potent antitumor immunity with concomitant regulatory T cell apoptosis. J Exp Med. 2009;206:1103–16. doi: 10.1084/jem.20082205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Redmond WL, Triplett T, Floyd K, Weinberg AD. Dual anti-OX40/IL-2 therapy augments tumor immunotherapy via IL-2R-mediated regulation of OX40 expression. PLoS ONE. 2012;7:e34467. doi: 10.1371/journal.pone.0034467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Curran MA, Allison JP. Tumor vaccines expressing flt3 ligand synergize with ctla-4 blockade to reject preimplanted tumors. Cancer Res. 2009;69:7747–55. doi: 10.1158/0008-5472.CAN-08-3289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holmgaard RB, Zamarin D, Munn DH, Wolchok JD, Allison JP. Indoleamine 2,3-dioxygenase is a critical resistance mechanism in antitumor T cell immunotherapy targeting CTLA-4. J Exp Med. 2013;210:1389–402. doi: 10.1084/jem.20130066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Qui HZ, Hagymasi AT, Bandyopadhyay S, St Rose MC, Ramanarasimhaiah R, Menoret A, et al. CD134 plus CD137 dual costimulation induces Eomesodermin in CD4 T cells to program cytotoxic Th1 differentiation. J Immunol. 2011;187:3555–64. doi: 10.4049/jimmunol.1101244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coussens LM, Zitvogel L, Palucka AK. Neutralizing tumor-promoting chronic inflammation: a magic bullet? Science. 2013;339:286–91. doi: 10.1126/science.1232227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. J Clin Invest. 2012;122:787–95. doi: 10.1172/JCI59643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Condamine T, Gabrilovich DI. Molecular mechanisms regulating myeloid-derived suppressor cell differentiation and function. Trends Immunol. 2011;32:19–25. doi: 10.1016/j.it.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sica A, Bronte V. Altered macrophage differentiation and immune dysfunction in tumor development. J Clin Invest. 2007;117:1155–66. doi: 10.1172/JCI31422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rigamonti N, Capuano G, Ricupito A, Jachetti E, Grioni M, Generoso L, et al. Modulators of arginine metabolism do not impact on peripheral T-cell tolerance and disease progression in a model of spontaneous prostate cancer. Clin Cancer Res. 2011;17:1012–23. doi: 10.1158/1078-0432.CCR-10-2547. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.