Abstract
Background
Emerging adulthood is a high-risk period for mental health problems and risk behaviors for youth generally and for physical health problems among those with type 1 diabetes.
Purpose
To examine whether adolescents’ relationships with parents and friends predict health and risk behaviors during emerging adulthood.
Method
Youth with and without diabetes were enrolled at average age 12 and followed for 7 years. Parent and friend relationship variables, measured during adolescence, were used to predict emerging adulthood outcomes: depression, risk behavior, and, for those with diabetes, diabetes outcomes.
Results
Parent relationship quality predicted decreased depressive symptoms and, for those with diabetes, decreased alcohol use. Parent control predicted increased smoking, reduced college attendance, and, for control participants, increased depressive symptoms. For those with diabetes, parent control predicted decreased depressive symptoms and better self-care. Friend relationship variables predicted few outcomes.
Conclusions
Adolescent parent relationships remain an important influence on emerging adults’ lives.
Keywords: Emerging adulthood, parent relationships, diabetes, risk and resistance framework
The transition to emerging adulthood is a relatively neglected area of research but an area that is coming to the forefront of both pediatric and adult research. Emerging adulthood is described as occurring between the ages of 18 and 25 (1, 2). It is the period of time that directly follows adolescence but occurs before many traditional adult responsibilities such as marriage, parenthood, and work are assumed. It is considered to be a high-risk period in terms of health behaviors and psychological distress (1). Lack of parental monitoring and freedom from the responsibilities of traditional adult roles provide opportunities to engage in risky behavior with few perceived consequences. This age group has the highest rate of alcohol usage (3), and the highest rate of depressive symptoms (2, 4). Emerging adulthood is an especially high-risk period for youth with a chronic illness, such as diabetes, as this is the time when youth assume responsibilities for a complex health regimen in which parents were often closely involved (5).
Yet, little is known about the predictors of health among emerging adults with type 1 diabetes. One reason for this lack of knowledge is that emerging adults with type 1 diabetes are difficult to locate and, therefore, difficult to study. They receive care from a variety of sources (6), and often receive less continuous care than when seen by pediatric providers. Thus, only a few studies have examined the psychological and physical well-being of emerging adults with type 1 diabetes. One cross-sectional study showed that adjustment to disease during adolescence predicted health outcomes during emerging adulthood, but adjustment to disease was measured retrospectively (7). The authors concluded that longitudinal data are needed.
There may be characteristics of childhood that protect from or heighten the risk of poor outcomes during emerging adulthood. From a clinical perspective, it is important to identify youth who are at risk for poor outcomes when they transition to emerging adulthood so that interventions can be set in place to address those risk factors. One of the few longitudinal studies conducted in this area found that behavioral problems during adolescence predicted poorer glycemic control 8 years later in young adulthood (8). Poor health during emerging adulthood is an important clinical outcome in and of itself, but also is significant because health and health behaviors during emerging adulthood may set in motion a pattern that pervades adulthood (9,10).
In this paper, we employ a risk and resistance framework (11) to understand the factors during adolescence that might play a role in the adjustment to the early stage of emerging adulthood among those with and without type 1 diabetes. We use longitudinal data to examine this issue. The risk and resistance framework is an expansion of the stress and coping model and has been used to understand how children adapt to chronic physical disorders (12, 13). Chronic physical disorders, such as diabetes, are conceptualized as an ongoing strain. Risk factors impede adjustment, whereas resistance factors facilitate adjustment. Here we focus on the social environment—specifically, the two sets of relationships that are critical to adolescents’ lives—relationships with family and friends (14). Risk factors would include conflictual or problematic interactions with network members, whereas resistance factors would include supportive aspects of these relationships. Below, we briefly review what is known about the influence of parents and peers on the health of both adolescents and emerging adults with and without diabetes.
Parent Relationships
There is a wealth of literature linking characteristics of family relationships to reduced risk behavior and good health outcomes among adolescents, including links of parental warmth and authoritative parenting to positive outcomes and links of parental neglect or lack of involvement and hostile parent-child relations to negative outcomes (15). One potentially problematic aspect of parent-child relationships is parent controlling behavior. Parent controlling behavior has been shown to interfere with youth’s development of autonomy and competence (16). Youth who perceive their parents as controlling have higher rates of delinquency, lower self-esteem, and increased depressive symptoms (16–18). In the area of diabetes, parent controlling behavior has been related to poor adherence, depressed mood, and lower diabetes self-efficacy (19,20). In this situation, parental control may interfere with the development of the skills needed by youth to manage their diabetes.
Despite the evidence for concurrent links of parent relationships to adolescent outcomes, there are fewer studies that have examined the links of parent relationships during adolescence to health outcomes during the transition to emerging adulthood. One longitudinal study showed that parent support during adolescence was associated with decreased depressive symptoms between the ages of 18 and 26 (21), and the link was stronger for females than males. Another study of 8 to 12-year-olds found that parenting quality in childhood predicted emerging adulthood outcomes that involved academic, social, and conduct domains 20 years later (22) but baseline levels of these outcomes were not statistically controlled. Among youth with diabetes, one study linked a positive family climate during middle adolescence (ages 14–16) to good glycemic control during young adulthood using trajectory analysis (ages 21–25; 23). Importantly, none of these studies examine the long-term effects of problematic parent relationships.
In this paper, we address whether supportive and conflictual relationships with parents during adolescence have long-term implications for health as youth transition to young adults. We predict that parent support will be beneficial and parent controlling behavior will be harmful to health. We examine whether those relations are the same for emerging adults with and without type 1 diabetes. Because parents are frequently involved in the daily behavioral regimen of taking care of diabetes throughout adolescence, we predict that parental influence on health outcomes will be more pronounced among emerging adults with than without diabetes.
Peer Relationships
Peer relationships take on increasing importance during adolescence (24,25); the peak age of peer influence is around age 14 (26). Supportive relationships with friends have been linked to a positive self-concept, social competence, psychological well-being, and fewer problems in school among adolescents (27–29). In the area of diabetes, a literature review on the implications of friend relationships for diabetes outcomes concluded that there was meager evidence that friend support was related to good diabetes outcomes but conflict with friends was a consistent, albeit infrequently explored, predictor of poor diabetes outcomes (30). In fact, one study found that friend support was related to poor diabetes outcomes (31). Researchers have not examined whether relationships with friends—supportive or conflictual—during adolescence predict health outcomes during emerging adulthood. Here we examine whether friend support and friend conflict during early adolescence predict emerging adulthood outcomes among youth with and without type 1 diabetes. Due to previous contradictory findings, we are unclear whether friend support will predict positive health outcomes, but we predict that friend conflict will predict negative health outcomes. We do not make differential predictions for youth with and without diabetes. Because specific friend relationships are more likely to change over the course of adolescence and emerging adulthood compared to parent relationships, we expect that the association of friend relationships to emerging adulthood outcomes will be less robust than that of parent relationships.
The Present Study
We examined whether parent relationships and friend relationships during early adolescence predicted adjustment to the earliest stage of emerging adulthood, the transition out of high school. We conducted a prospective study of teens with and without type 1 diabetes, enrolling them when they were average age 12 and following them for 7 years until average age 19 (one year after high school graduation). We examined two aspects of parent relationships—positive relationship quality and parental control, and two aspects of friend relationships—support and conflict, from the perspective of the adolescent and emerging adult. When possible, we controlled for the relevant adolescent outcome measure so that we were predicting changes in outcomes over time. We examined whether the implications of these risk and resistance factors for emerging adulthood outcomes (mental health, risk behavior) were moderated by diabetes status and sex. Because relationships are more central to the female than the male gender role (32), we predicted that associations may be stronger among females than males.
To the extent that early adolescent relationships with parents and friends predict emerging adulthood outcomes, one possibility is that these predictive effects are a function of current relationships with parents and friends. In fact, we have data on this sample in emerging adulthood that shows concurrent relations between parent support and good psychological well-being and between parent control and increased smoking/depression (33) as well as concurrent relations between friend conflict and risky health behaviors (e.g., alcohol and smoking) and poor psychological well-being (33). Thus, after identifying the parent and friend relationship variables from early adolescence that predict emerging adulthood outcomes, we ran a second set of analyses controlling for the corresponding current parent or friend relationship variable to determine if the early adolescent relationship variable uniquely predicted the emerging adult outcome. If the significance of the early adolescent relationship variable disappeared with the addition of the current relationship variable, we know that early relationship variables do not have unique predictive significance and that it is ongoing relationships with parents and friends that are implicated in health outcomes.
Method
Participant Recruitment
We recruited 132 adolescents with diabetes and 131 adolescents without diabetes into a longitudinal study when they were average age 12 (5th, 6th, 7th grades). Parents signed consent forms, and youth provided written assent. Adolescents with diabetes were recruited from a local Children’s Hospital. Of letters sent to 287 families, 171 were reached and determined to be eligible. Of the 171 families, 77% agreed to participate. The control group was recruited from health fairs in area malls soliciting volunteers and letters sent to randomly selected families from a local pediatric network of physicians. The two samples did not significantly differ in sex, age, or race but youth with diabetes had a lower social status and higher body mass index (BMI) than youth without diabetes. Further recruitment details have been described elsewhere (34). In-person interviews (Time 1 [T1]) were conducted in the hospital before or after a routine clinic appointment for youth with diabetes and in the homes for youth without diabetes.
We followed teens for between 6 and 8 years as they graduated from high school. We contacted them approximately one year after high school to complete the assessment (Time 2 [T2]). They were average age 19 and considered to be emerging adults. Because participants were now over 18, we reconsented them. Upon receipt of signed consent forms, we emailed participants a link to an on-line questionnaire, as they lived in a variety of places at this time. Of those enrolled in the study at T1, 89% (n = 117) of those with diabetes and 92% (n = 121) of those without diabetes completed the T2 on-line questionnaire. There were no differences in background variables or baseline psychosocial variables between those who did (n = 238) and did not (n = 25) participate in the T2 interview. (There was a trend indicating nonparticipants had a lower social status than participants, p = .07.) The demographic characteristics of the sample are shown in Table 1.
Table 1.
Demographic Characteristics
| Diabetes | Controls | |
|---|---|---|
| n = 117 | n = 121 | |
| sex | 53% female | 54% female |
| age (years) [T2] | M = 19.13 (SD = .40) | M = 19.01 (SD = .49) |
| race | 92% white | 93% white |
| ethnicity | 98% non-Hispanic | 97% non-Hispanic |
| social status* | M = 42.61 (SD =11.08) | M = 46.58 (SD =13.70) |
| body mass index* | M = 26.12 (SD =4.01) | M = 24.82 (SD =4.81) |
| diabetes duration (years) [T2] | M = 12.05 (SD =3.08) |
indicates a significant difference between diabetes and control groups, p < .05
Note: All variables are measured at T1 when participants were average age 12 except age and diabetes duration which are presented at T2 and noted as such.
T1 Interview (average age 12)
Background variables
We obtained data on participants’ sex, age, race, ethnicity, BMI (computed from height/weight measured by clinic staff for those with diabetes and measured by study staff for controls), and parents’ social status (35). For those with diabetes, we obtained diagnosis date and treatment regimen. At study start, the vast majority of youth were on multiple daily injections, with only 25% being on insulin pumps (by T2, this number rose to 59%).
Parent relationship
We measured the overall quality of the parent relationship with Kerr and Stattin’s (17) 8-item relationship quality measure for both mother and father. Items included “How often do you and your mom understand each other?” and “How often does your dad support and encourage you?” Adolescents rated the frequency of the same set of 8 items for mother and for father on a 1 (never) to 5 (very often) scale. Items were summed, and averages were taken for mother relationship quality and father relationship quality. Internal consistencies of the two scales were .80 and .87, respectively. Because the two indices were correlated (r =.38, p < .001), we averaged them to form an overall parent relationship quality index. In instances when there was no father (5% of cases), we used the mother relationship quality index.
We administered the 4-item “feeling controlled” by parents scale, also from Kerr and Stattin (17). Sample items are “Do you feel as though your parents control everything in your life?” and “Do you feel that your parents demand to know everything?” The internal consistency was .69. Participants responded on the same response scale as described above, and items were summed and then the average was taken.
Friend relationship
We administered the Berndt and Keefe (36) friendship questionnaire. This instrument contains six scales: companionship, intimacy, instrumental support, self-esteem enhancement, conflict, and dominance. Items are responded to on a 1 (never) to 5 (very often) scale and then summed and averaged into indices. Because the positive aspects of friendship were highly intercorrelated (r’s ranged from .47 to .72, p’s < .001), we standardized the four scales, summed them, and took the average to form an overall support index. The internal consistency of this index was .90. The two negative aspects of friendship (conflict and dominance) were correlated (r = .66, p = .001) but were unrelated to the positive aspects of friendship. Thus, we took the average of these two scales to form an overall friend conflict index. The internal consistency of this index was .82.
Depressive symptoms
Depressive symptoms were measured with the abbreviated form of the Children’s Depression Inventory (CDI; 37,38). The abbreviated CDI consists of 10 multiple choice items, is well-validated, has high internal consistency and high test-retest reliability. The internal consistency was .73. Items were summed, and the average was taken.
Diabetes outcomes
We administered the 14-item Self-Care Inventory (39,40) to youth with diabetes. This scale asks respondents to indicate how well they followed their physicians’ recommendations for glucose testing, insulin administration, diet, exercise, and other diabetes behaviors. This index reflects domains of self-care that have been regarded as important by the American Diabetes Association, and has been associated with glycemic control among adolescents (39,41,42). This instrument was updated by adding eight more contemporary items as described previously (43). The final 22 items were measured on a scale from 1 (never) to 5 (always/very often); negative items were reverse-coded, and then all were summed and averaged to create a final self-care index. Internal consistency for this index was .78.
Glycemic control was obtained from medical records and measured from hemoglobin A1c (HbA1c) by HPLC (Tosoh Instruments) with normal range of 4.6–6.1%. HbA1c values indicate the average blood glucose level over the past 2–3 months. The average HbA1c for the sample at T1 was 8.04 (SD = 1.31).
T2 Questionnaire (average age 19)
Health behaviors
To measure alcohol consumption and binge drinking, we used a series of questions from the Monitoring the Future Study (44). Participants were asked to indicate the number of times they drank more than a few sips of alcohol during the past month and were assigned either a 1 (had consumed any alcohol) or a 0 (had not consumed any alcohol). At T2, 52% of emerging adults had consumed alcohol. Consistent with the Monitoring the Future Study, binge drinking was defined as the consumption of five or more drinks of alcohol on a single occasion in the past month for males and four or more drinks of alcohol on a single occasion for females. We created a categorical variable, such that 1 represented one or more binges and 0 represented no binges in the past month. At T2, 34% of emerging adults had reported a binge.
We measured cigarette smoking with a question from the Monitoring the Future Study. We asked participants how often they had smoked cigarettes in the past 12 months. We created a dichotomous variable, such that 0 indicated never smoked in the past year and 1 indicated had ever smoked in the past year. At T2, 38% of emerging adults reported having smoked in the past year.
Depression
Depressive symptoms were measured by the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; 45). Participants indicated how often they experienced each symptom on a 0 (none of the time) to 3 (most of the time) scale. Items were summed to create a total score. We also used the conventional cutoff score of 16 to classify people as at elevated risk for clinical depression. This scale has well-established internal consistency and validity, and has been widely used with emerging adults. Internal consistency was .93.
Education
Participants were classified as full-time college students (75%) or not.
Diabetes outcomes
The same Self-Care Inventory used at T1 was used at T2 and had good internal consistency (α = .88). Glycemic control was measured using participants’ most recent HbA1c, which was requested from each participant’s current physician. We only had data available on HbA1c for 93 of the 117 emerging adults. Reasons for missing HbA1c data included participants not seeing a physician in the past year and seeing a physician but not having an HbA1c measured. We examined HbA1c as both a continuous variable and a dichotomous variable. The American Diabetes Association recommends that HbA1c be under 8.0 for children ages 6–12, under 7.5 for adolescents ages 13–19, and under 7.0 for adults over the age of 19 (46). Because we had so few youth who met the 7.5 criterion (n = 14), we categorized youth as less than 8.0 (n = 27) and 8.0 or over (n = 66).
Relationship variables
We had similar, but usually not identical, measures of parent and friend relationship variables at each wave of assessment. For T2, we created a parent relationship quality index based on items that measure closeness (e.g., how close are you to your parents) and self-disclosure (e.g., child disclosure of feelings [17]), as described in 32. The internal consistency was .89. The parent control measure was identical to that used at T1. We used three of the four subscales from T1 to reflect friend support at T2 (intimacy, instrumental support, esteem-enhancement); the fourth scale, companionship, was not used because it was not appropriate for emerging adults. We administered a measure of friend conflict more suited to adults (Test of Negative Social Exchange; 47). The internal consistencies for friend support and friend conflict were .94 and .93, respectively.
Results
Overview of the Analyses
We used multiple regression analysis to predict continuous outcomes and logistic regression analysis to predict categorical outcomes one year after high school graduation. For multiple regression analysis, we provided standardized betas, p values, and the increment to R2 for the step in the equation in which significant relationship predictor variables emerged. For logistic regression analysis, we provided unstandardized betas, standard errors, p values, and odds ratios for significant relationship predictor variables. Because there were health status differences in initial BMI and social status, we statistically controlled for these two variables in all analyses that involved both persons with and without type 1 diabetes. We controlled for baseline status of the dependent variable when available (i.e., depressive symptoms, self-care behavior, glycemic control) and whether or not the respondents were in college as college status could influence health outcomes. We entered these statistical control variables on the first step and friend support, friend conflict, parent relationship quality, and parent control on the second step. We also examined interactions with sex for all outcomes and interactions with health status (diabetes, control) for all but the diabetes-specific outcomes. Finally, to address the concern that early relationship variables are reflections of current relationship variables, we reran the analyses that showed significant effects for early adolescent relationship variables by including the corresponding T2 relationship measure.
Correlations Among Independent Variables
Correlations among the four T1 predictor variables ranged from non-significant to moderate, as shown in Table 2. Friend support and friend conflict were uncorrelated, and parent relationship quality and parent control were inversely related for both youth with diabetes and controls. For both groups, friend conflict was inversely related to parent relationship quality and positively correlated with parent control.
Table 2.
Correlations Among Predictor Variables
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. Parent Relationship Quality | -- | −.46** | .10 | −.36** |
| 2. Parent Control | -.45** | -- | .08 | .36** |
| 3. Friend Support | .21* | .02 | -- | −.05 |
| 4. Friend Conflict | −.42** | .15+ | −.08 | -- |
Note: Correlations for those with diabetes are above the diagonal; correlations for controls are below the diagonal;
p < .10;
p < .05;
p < .001
Although the measures were not identical in all cases, we also examined the correlation of the relationship variables across T1 and T2. Correlations were significant and modest: parent relationship quality (r = .36, p < .001); parent control (r = .19, p < .005); friend support (r = .32, p < .001); and friend conflict (r = .27, p < .001).
Depressive Symptoms
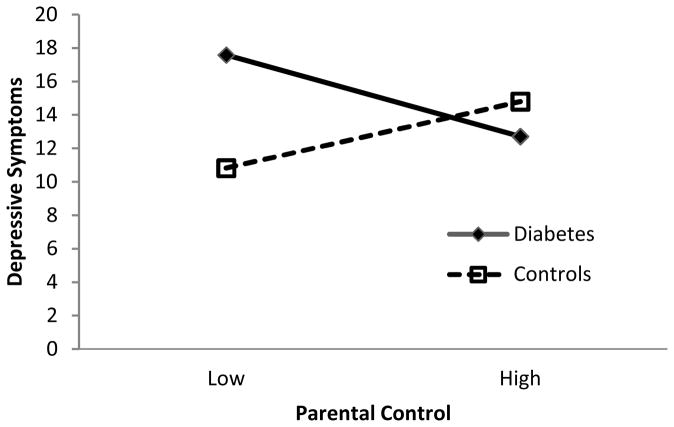
Although sex was a significant predictor of depressive symptoms (β = .18, p < .05; females higher), none of the interactions with sex were significant. Thus, these terms were dropped from the equation. We found a main effect of parent relationship quality (β = −.57, p < .05), such that better adolescent relationships with parents were associated with fewer depressive symptoms among emerging adults (change in R2 = .04). We also found a main effect of parent control (β = −.62, p < .05) that was qualified by an interaction with health status (β = .64, p < .01; change in R2 = .03). To examine the interaction, we used Aiken and West’s (48) simple slopes analysis. As shown in Figure 1, parent control during adolescence was related to less depressive symptoms among emerging adults for the diabetes group but more depressive symptoms among control emerging adults. Figure 1 also shows that depressive symptoms were higher among the diabetes than the healthy group only when parent control was low.
Figure 1.
Relation of T1 parent control to T2 depressive symptoms for emerging adults with and without diabetes.
Risk for Clinical Depression
We also examined elevated risk for clinical depression, using the standard CES-D cutoff of 16. One third (34%) of the sample scored at or above 16. Using logistic regression analysis, again sex was a significant predictor (B = −.91, SE = .30, p < .01; odds ratio = .40), but there were no interactions involving sex. Thus, these terms were dropped from the model. The only psychosocial variable to predict risk for clinical depression among emerging adults was the interaction between parent control and health status (B = 1.14, SE = .44; p < .01; odds ratio = 3.12). The form of the interaction was the same as that shown in Figure 1. Parent control was related to lower likelihood of being at risk for clinical depression among diabetes emerging adults (B = −.72, SE = .38, p = .06; odds ratio=.49) and unrelated to depression risk among control emerging adults (B = .36, SE = .28, p = .20; odds ratio = 1.44).
Alcohol
Among emerging adults, just over half (52%) said that they had consumed any alcohol over the past month. Logistic regression analysis revealed a main effect of parent relationship quality (B = −3.02, SE = 1.06; p < .01; odds ratio = .05) that was qualified by an interaction with health status (B = 1.73, SE = .66, p < .01; odds ratio = 5.64). Higher parent relationship quality during adolescence was related to a lower likelihood of alcohol consumption among emerging adults with diabetes (B = −1.33, SE = .49, p < .01; odds ratio = .27), but was unrelated to alcohol consumption among emerging adults without diabetes (B = .50, SE = .46, n.s.; odds ratio = 1.64). There were no effects involving participant sex and no effects involving friend relationships.
Among emerging adults, 34% of the sample had had at least one episode of binge drinking in the past month. There were no effects involving participant sex. There was a main effect of parent relationship quality (B = −2.59, SE = 1.11, p <.05; odds ratio = .08) that was qualified by an interaction with health status (B = 1.63, SE = .70, p < .05; odds ratio = 5.08) similar to the previous interaction. A better relationship with parents during adolescence was associated with a lower likelihood of binge drinking among emerging adults with diabetes (B = −.93, SE = .50, p = .06; odds ratio = .40) but was unrelated to binge drinking among emerging adults without diabetes (B = .66, SE = .51, p = .19; odds ratio = 1.94).
Smoking
Just over one-third (38%) of emerging adults had smoked cigarettes in the past year. Only parent control predicted smoking status (B = .59, SE = .21, p < .01; odds ratio = 1.80). Parent control during adolescence was related to a greater likelihood of smoking. There were no effects involving sex or health status.
College Attendance
Three-fourths (75%) of participants were attending college full-time. Although health status did not predict college attendance, those with a higher social status were more likely to attend college (B = .08, SE = .02, p < .001; odds ratio = 1.09). Among relationship predictors, more parent control during adolescence was related to lower likelihood of attending college (B = −.64, SE = .25, p < .01; odds ratio = .53). There were no interactions with sex or health status.
Diabetes Outcomes
Friend conflict during adolescence predicted poorer self-care behavior among emerging adults (β = −.25, p < .05), and parent control during adolescence was marginally associated with better self-care among emerging adults (β = .21, p = .06; increment to R2 was .08 for this step of the equation). None of the variables interacted with participant sex.
The only variable that predicted glycemic control was friend support (β = .21, p < .05), such that greater friend support during adolescence was related to poorer glycemic control among emerging adults (change in R2 = .06). There were no effects involving participant sex.
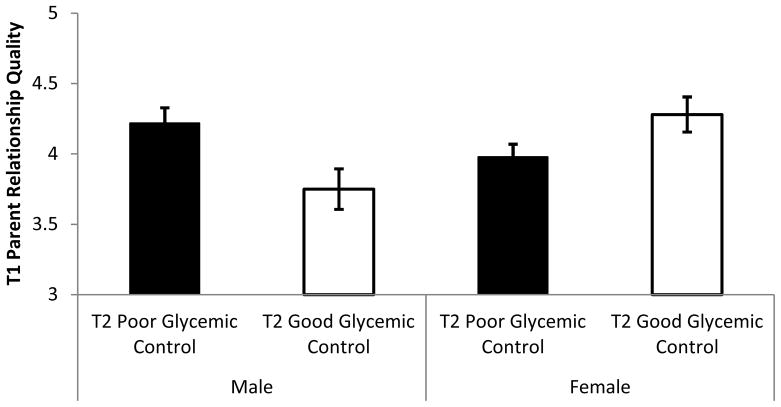
We also examined glycemic control as a dichotomous variable, with 8.0 and above representing poor control and below 8.0 representing better control. Consistent with findings using a continuous measure of HbA1c, greater friend support during adolescence was related to an increased likelihood of emerging adults being in the poor glycemic control group (B = 3.72, SE = 1.87, p < .05; odds ratio = 41.18). There also was a main effect of parent relationship quality (B = 7.10, SE = 3.09, p < .05) that was qualified by an interaction with sex (B = −3.52, SE = 1.75, p < .05; odds ratio = .03). The quality of parent relationships during adolescence was unrelated to glycemic control for female emerging adults (B = −.02, SE = .97, n.s.; odds ratio = .98), but a good parent relationship during adolescence was related to a higher likelihood of being in the poor glycemic control group for male emerging adults (B = 4.04, SE = 1.80, p < .05; odds ratio = 56.93). To depict this interaction more clearly, we present average parent relationship quality scores in adolescence for good and poor glycemic control groups among male and female emerging adults (see Figure 2).
Figure 2.
T1 relationship quality of males and females who had good versus poor glycemic control at T2.
Ruling out Concurrent Relationship Variables
An alternative explanation for these findings is that it is the endurance of parent and friend relationships from ages 12 to 19 that predict outcomes at the transition rather than specific parent and peer relationships when youth were age 12. Fortunately, we had parallel constructs of parent and peer relationships that we measured at the transition (33). Thus, we reran the analyses and added the T2 parallel construct of the T1 significant predictor to see if it accounted for the T1 effect. For example, if parent relationship quality at age 12 predicted the change in depressive symptoms between ages 12 and 19, we added parent relationship quality at age 19 to see if parent relationship quality at age 12, at age 19, or both predicted the change in depressive symptoms.
In most cases, the T2 measure of the relationship construct did not account for the effect of the T1 predictor. For both depressive symptoms and risk for clinical depression, the effects of the T1 variables remained significant but there was an additionally significant effect for T2 parent control. That is, beyond the effects of T1 parent control and the interaction of T1 parent control with health status, T2 parent control additionally predicted increases in depressive symptoms (β = .40, p < .05) and increases in risk for clinical depression (B = 1.34; SE = .65, p < .05). For smoking, alcohol consumption, and binge drinking, the T1 variables remained unchanged and the T2 variables were not significant with the exception of alcohol consumption. Here, beyond the T1 parent relationship quality by health status interaction, there was an additionally significant T2 parent relationship quality by health status interaction that paralleled the T1 interaction. For college status, the effect for T1 parent control remained significant and the effect for T2 parent control was not significant. For self-care behavior, T1 friend conflict remained significant and T2 friend conflict was not significant. For glycemic control, the effect of T1 friend support was diminished (p = .15) but the effect of T2 friend support was not significant. For glycemic control groups, the T1 parent relationship quality by sex effect was diminished (p = .15) but the T2 variables were not significant.
Discussion
The quality of early adolescents’ relationships with parents was a predictor of a lower level of depressive symptoms and, among youth with diabetes, lower rates of drinking alcohol and lower binge drinking in the early stage of emerging adulthood. These findings not only suggest that parent relationships continue to have an influence on emerging adulthood outcomes, but suggest that there is something about the parent-child relationship during early adolescence that may be protective years later. The findings for depressive symptoms held when controlling for earlier levels, and all of these findings held when controlling for concurrent measures of parent relationship quality. What is the mechanism that explains this resilience factor? High quality parent relationships during adolescence may provide youth with a sense of self-esteem and/or with coping skills that they can use to address the challenges that come with emerging adulthood. Early adolescence may be a critical period during which parent relationships have a unique influence on youth behavior. Future research should examine these possibilities.
The findings for parent control are consistent with previous literature (16–18) in suggesting that parent controlling behavior is associated with poor well-being and higher rates of risk behavior among youth. Here the outcomes are among emerging adults. Youth who reported feeling controlled by parents as adolescents were more likely to smoke, less likely to attend college, and, for those without diabetes, had higher rates of depressive symptoms and higher risk for clinical depression as emerging adults. One interpretation of these findings—at least in regard to risk behavior—is that early parent controlling behavior is ineffective. Parents may be reacting to early engagement in risk behavior or trying to keep their children from engaging in the risk behavior that the children end up engaging. This could be due to psychological reactance (49), the tendency to engage in a forbidden behavior when behavioral freedom is restricted. Or, parent controlling behavior during early adolescence could be a marker of another variable or a response to another variable that is responsible for the links of parent control to subsequent outcomes among emerging adults. One candidate is child externalizing behavior. Parents may be more controlling of youth who display greater acting out behavior. In this study, parents completed the Behavior Assessment for Children (50) at T1, which includes measures of child externalizing and internalizing behavior. We found that adolescent report of parent controlling behavior was related to parent report of adolescent externalizing behavior (r = .14, p < .05) but not internalizing behavior (r = .06, n.s.) at T1. Although this relation is significant, it is modest. Thus, it is also possible that parent controlling behavior in adolescence is associated with poor outcomes in emerging adulthood because parent control inhibits the autonomy youth need to establish to navigate adulthood.
However, parent controlling behavior was not clearly linked to poor outcomes among emerging adults with diabetes, which contradicts previous research (19,20). Adolescents with diabetes who perceived their parents as controlling had lower rates of depressive symptoms, lower risk for clinical depression, and better self-care behavior as emerging adults. Here, parent controlling behavior may reflect parent involvement. There is a large literature in the area of diabetes that shows parental involvement in self-care is beneficial for youth even during the later stages of adolescence (43). Emerging adults with diabetes who had parents who engaged in low levels of controlling behavior when they were adolescents had the highest rate of depressive symptoms as adults. Youth with diabetes may expect a higher level of parental involvement than other youth and be more likely to construe a lack of parental control as a lack of involvement in their lives. This explanation is somewhat speculative. The parental control measure is generic, meaning that it is not about parents controlling areas of diabetes but about feeling controlled by parents more generally. Because the measure is generic, it is possible that youth with and without diabetes construe the items differently. It will be important for future research to ask about parent control in specific domains and to understand the distinctions among parent control, monitoring, and involvement.
Friend relationships during early adolescence had little predictive value in terms of emerging adulthood outcomes. In one sense, this is not surprising as relationships with friends—and the friends themselves—are likely to change between early adolescence and emerging adulthood. It also may be that there is less variability in friend relationship variables than parent relationship variables as people presumably select network members who are supportive to be friends. The two findings that did emerge for friendship were both in the area of diabetes outcomes—friend support was associated with poorer glycemic control and friend conflict was associated with poorer self-care behavior. The finding for friend support may be surprising, but it is consistent with an earlier finding on this same sample during adolescence: friend support was related to poor glycemic control over four annual assessments during adolescence using multilevel modeling (31). A recent review of the literature on peer relationships and diabetes outcomes concluded that there was more evidence that peer conflict was harmful than that peer support was beneficial (30). Taken collectively, these finding suggest that friend support may be a marker of something that could detract from taking care of diabetes, such as sociability and/or vulnerability to peer influence. It also must be noted that the measures of support and conflict were general. For those with type 1 diabetes, general support from friends may not translate into friends who understand and support the restrictions imposed by diabetes.
We examined whether the association of relationship variables to outcomes differed between those with and without type 1 diabetes. We found some evidence to support our hypothesis of stronger relations for those with diabetes. Parent relationship quality was more strongly related to reduced alcohol consumption for those with than without diabetes, and parent controlling behavior was linked to some positive outcomes for those with diabetes—specifically decreased depressive symptoms and decreased risk for depression. Because parents are likely to have been closely involved in diabetes care throughout childhood, parental influence on youth’s behavior may be longer lasting in the case of diabetes.
We did not find any evidence that links to outcomes were stronger for females than males. In fact, one result directly contradicted this hypothesis. Good parent relationships during early adolescence were related to poorer glycemic control among male emerging adults but not female emerging adults. It is not obvious why a good relationship with parents during adolescence would be linked to a poor diabetes outcome years later for males. One possibility is that boys’ perception of a good relationship with parents during early adolescence reflects a relationship in which parents are permissive or offer too much independence. Parents may be less likely to monitor or involve themselves in boys’ than girls’ behavior, which then has unintended negative consequences years later. Research on children in general suggests that parents are less likely to supervise boys than girls (51) and more likely to leave them alone at a younger age than girls (52).
To understand the practical implications of this research, we return to the risk and resistance framework. Our findings lead to the conclusion that a good parent relationship during adolescence is a protective factor for emerging adults’ health and parent controlling behavior during adolescence is a risk factor for emerging adults’ health—except among youth with diabetes, in which case parent controlling behavior is partly protective. Health care professionals can use this information to identify early adolescents or even preadolescents who are at risk for poor outcomes as adults. Families with problematic parent-child relationships may be referred for individual or family counseling. There is already evidence of successful family-based interventions that focus on communication and parent-child relationships among youth with type 1 diabetes (53).
Before concluding, we note several study limitations. First, a relatively high proportion of the sample was Caucasian and middle class, which limits the generalizability of the findings. The association of family and friend relationships to outcomes may depend upon culture and social status. For example, parent involvement and parent controlling behavior may be perceived less negatively by people from other cultures. Second, despite the longitudinal nature of this study, we are unable to draw firm causal conclusions from these data. Although we examined the links of early relationship variables to changes in health outcomes over the 7 years for most outcomes, we did not have baseline data available on smoking or alcohol use because parents of 12-year-olds expressed sufficient discomfort with these questions that it would have affected our recruitment rate. Thus, the possibility remains that early levels of risky behavior may have preceded parent controlling behavior. Third, we did not collect information on comorbidities among those with diabetes, meaning that we are unable to rule out the possibility that other difficulties contributed to their health. Fourth, we were unable to examine the differences between mother and father relationship variables because we did not have separate measures of parent control. Although we had separate measures of mother and father relationship quality, we averaged the two so that we would not lose participants who did not have fathers from analyses. Future research should investigate the distinct contribution of characteristic of mother and father relationships to adolescents and emerging adults health. Finally, although we ruled out the possibility that the association of adolescent relationship variables to emerging adulthood outcomes were a function of concurrent relationship variables, we only had identical measures of one of the four relationship variables. Thus, some possibility remains that some of our findings tap a concurrent rather than an early relationship variable or are artifacts of using different measures.
In conclusion, these findings highlight the enduring importance of adolescent relationships—especially those with parents—for the health and risk behaviors of emerging adults. Despite the fact that there was some stability across adolescence and emerging adulthood in these relationship factors, adolescent relationship variables predicted changes in health outcomes between adolescence and emerging adulthood. And, these changes were not accounted for by concurrent relationship variables. This study contributes to a relative paucity of literature on the factors that influence the health and risk behavior of emerging adults generally and specifically those with type 1 diabetes. Because of this gap in knowledge, it is important to follow these participants as they further navigate the challenges of adulthood to study how the evolution of relationships with parents, romantic partners, and friends influence health and well-being. Understanding the involvement of early social factors in diabetes outcomes will help clinicians who care for those with type 1 diabetes to identify potential risk and resistance factors for health.
Acknowledgments
This work was supported by National Institutes of Health grant R01 DK60586. Portions of these data were presented at the March 2013 Meeting of the Society of Behavioral Medicine. We appreciate the support of the project manager, Pamela Snyder, and the research assistants, Abigail Vaughn and Jamie Vance, for their assistance on this project.
Footnotes
Conflict of Interest Statement: The authors have no conflict of interest to disclose.
Contributor Information
Vicki S. Helgeson, Carnegie Mellon University
Dianne K. Palladino, Carnegie Mellon University
Kerry A. Reynolds, The Rand Corporation
Dorothy Becker, Children’s Hospital of Pittsburgh.
Oscar Escobar, Children’s Hospital of Pittsburgh.
Linda Siminerio, University of Pittsburgh Medical Center.
References
- 1.Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–480. [PubMed] [Google Scholar]
- 2.Arnett JJ. Emerging adulthood: The winding road from the late teens through the twenties. New York: Oxford University Press; 2004. [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. [Accessibility verified April 8, 2013];Results from the 2010 national survey on drug use and health: Summary of national findings. 2011 Available at http://www.samhsa.gov/data/nsduh/2k10nsduh/2k10results.htm.
- 4.Kessler RC, Mickelson KD, Walters EE, Zhao S, Hamilton L. Age and depression in the MIDUS survey. In: Brim OG, Ryff CD, Kessler RC, editors. How healthy are we? A national study of well-being at midlife. Chicago, IL: University of Chicago Press; 2004. pp. 227–251. [Google Scholar]
- 5.Peters A, Laffel L. Diabetes care for emerging adults: Recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care. 2011;34:2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helgeson VS, Reynolds KA, Snyder PR, et al. Characterizing the transition from pediatric to adult care among emerging adults with Type 1 diabetes. Diabetic Med. doi: 10.1111/dme.12067. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wysocki T, Hough BS, Ward KM, Green LB. Diabetes mellitus in the transition to adulthood: Adjustment, self-care, and health status. J Dev Behav Pediatr. 1992;13:194–201. [PubMed] [Google Scholar]
- 8.Bryden KS, Neil A, Peveler RC, et al. Clinical and psychological course of diabetes from adolescence to young adulthood. Diabetes Care. 2001;24:1536–1540. doi: 10.2337/diacare.24.9.1536. [DOI] [PubMed] [Google Scholar]
- 9.Laska MN, Pasch KE, Lust K, Story M, Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prev Sci. 2009;10:376–386. doi: 10.1007/s11121-009-0140-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity. 2008;16:2205–2211. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 11.Wallander JL, Varni JW, Babani L, Banis HT, Wilcox KT. Family resources as resistance factors for psychological maladjustment in chronically ill and handicapped children. J Pediatr Psychol. 1989;14:157–173. doi: 10.1093/jpepsy/14.2.157. [DOI] [PubMed] [Google Scholar]
- 12.Wallander JL, Varni JW. Adjustment in children with chronic physical disorders: Programmatic research on a disability-stress-coping model. In: La Greca AM, Siegel LJ, Wallander JL, Walker CE, editors. Stress and coping in child health. New York: Guilford Press; 1992. pp. 279–298. [Google Scholar]
- 13.Wallander JL, Varni JW. Effects of pediatric chronic physical disorders on child and family adjustment. J Child Psychol Psyc. 1998;39:29–46. [PubMed] [Google Scholar]
- 14.Brown RT, Boeving A, LaRosa A, Carpenter LA. Health and chronic illness. In: Wolfe DA, Mash EJ, editors. Behavioral and emotional disorders in adolescents: Nature, assessment, and treatment. New York: Guilford Publications; 2006. pp. 505–531. [Google Scholar]
- 15.Collins WA, Steinberg L. Adolescent development in interpersonal context. In: Eisenberg N, editor. Handbook of child psychology. Vol. 3. Hoboken, NJ: Wiley; 2007. pp. 1003–1067. [Google Scholar]
- 16.Schiffrin HH, Liss M, Miles-McLean H, et al. Helping or hovering? The effects of helicopter parenting on college students’ well-being. [Accessibility verified April 8, 2013];J Child Fam Stud. 2013 Feb; Available at http://link.springer.com/article/2010.1007/s10826-10013-19716-10823/fulltext.html.
- 17.Kerr M, Stattin H. What parents know, how they know it, and several forms of adolescent adjustment: Further support for a reinterpretation of monitoring. Dev Psychol. 2000;36:366–380. [PubMed] [Google Scholar]
- 18.Nelson LJ, Padilla-Walker LM, Christensen KJ, Evans CA, Carroll JA. Parenting in emerging adulthood: An examination of parenting clusters and correlates. J Youth Adolescence. 2011;40:730–743. doi: 10.1007/s10964-010-9584-8. [DOI] [PubMed] [Google Scholar]
- 19.Butler JM, Skinner M, Gelfand D, Berg CA, Wiebe DJ. Maternal parenting style and adjustment in adolescents with type I diabetes. J Pediatr Psychol. 2007;32:1227–1237. doi: 10.1093/jpepsy/jsm065. [DOI] [PubMed] [Google Scholar]
- 20.Weissberg-Benchell J, Nansel T, Holmbeck G, et al. Generic and diabetes-specific parent-child behaviors and quality of life among youth with type 1 diabetes. J Pediatr Psychol. 2009;34:977–988. doi: 10.1093/jpepsy/jsp003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Needham BL. Reciprocal relationships between symptoms of depression and parental support during the transition from adolescence to young adulthood. J Youth Adolescence. 2008;37:893–905. [Google Scholar]
- 22.Masten AS, Burt KB, Roisman GI, et al. Resources and resilience in the transition to adulthood: Continuity and change. Dev Psychopathol. 2004;16:1071–1094. doi: 10.1017/s0954579404040143. [DOI] [PubMed] [Google Scholar]
- 23.Luyckx K, Seiffge-Krenke I. Continuity and change in glycemic control trajectories from adolescence to emerging adulthood. Diabetes Care. 2009;32:797–801. doi: 10.2337/dc08-1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fuligni AJ, Eccles JS, Barber BL, Clements P. Early adolescent peer orientation and adjustment during high school. Dev Psychol. 2001;37:28–36. [PubMed] [Google Scholar]
- 25.Larson RW, Verma S. How children and adolescents spend time across the world: Work, play, and developmental opportunities. Psychol Bull. 1999;125:701–736. doi: 10.1037/0033-2909.125.6.701. [DOI] [PubMed] [Google Scholar]
- 26.Berndt TJ. Developmental changes in conformity to peers and parents. Dev Psychol. 1979;15:608–616. [Google Scholar]
- 27.Anderman EM. School effects on psychological outcomes during adolescence. J Educ Psychol. 2002;94:795–809. [Google Scholar]
- 28.Ladd GW. Social competence and peer relations: Significance for young children and their service-providers. Early Child Serv. 2008;2:129–148. [Google Scholar]
- 29.Wentzel KR, McNamara CC. Interpersonal relationships, emotional distress, and prosocial behavior in middle school. J Early Adolescence. 1999;19:114–125. [Google Scholar]
- 30.Palladino DK, Helgeson VS. Friends or foes? A review of peer influence on self-care and glycemic control in adolescents with type 1 diabetes. J Pediatr Psychol. 2012;37:591–603. doi: 10.1093/jpepsy/jss009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Helgeson VS, Siminerio L, Escobar O, Becker D. Predictors of metabolic control among adolescents with diabetes: A 4-year longitudinal study. J Pediatr Psychol. 2009;34:254–270. doi: 10.1093/jpepsy/jsn079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spence JT, Helmreich RL. Masculinity and femininity: Their psychological dimensions, correlates, and antecedents. Austin, TX: University of Texas Press; 1978. [Google Scholar]
- 33.Helgeson VS, Palladino DK, Reynolds KA, et al. Relationships and health among emerging adults with and without type 1 diabetes. Health Psychol. doi: 10.1037/a0033511. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Helgeson VS, Snyder PR, Escobar O, Siminerio L, Becker D. Comparison of adolescents with and without diabetes on indices of psychosocial functioning for three years. J Pediatr Psychol. 2007;32:794–806. doi: 10.1093/jpepsy/jsm020. [DOI] [PubMed] [Google Scholar]
- 35.Hollingshead AB. Four factor index of social status. New Haven, CT: Yale University; 1975. [Google Scholar]
- 36.Berndt TJ, Keefe K. Friends’ influence on adolescents’ adjustment to school. Child Dev. 1995;66:1312–1329. [PubMed] [Google Scholar]
- 37.Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacol Bull. 1985;21:995–998. [PubMed] [Google Scholar]
- 38.Kovacs M. Children’s Depression Inventory (CDI): Technical manual. North Tonawanda, NY: Multi-Health Systems Inc; 2001. [Google Scholar]
- 39.La Greca AM, Swales T, Klemp S, Madigan S. Self care behaviors among adolescents with diabetes. Ninth Annual Sessions of the Society of Behavioral Medicine; Baltimore, MD. April 1988. [Google Scholar]
- 40.Lewin AB, LaGreca AM, Geffken GR, et al. Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: the Self-Care Inventory (SCI) J Pediatr Psychol. 2009;34:999–1007. doi: 10.1093/jpepsy/jsp032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Delamater A, Applegate B, Edison M, Nemery R. Increased risks for poor metabolic control in minority youths with type 1 diabetes. Diabetes. 1998;47:A326. [Google Scholar]
- 42.Greco P, LaGreca A, Ireland S, et al. Assessing adherence in IDDM: A comparison of two methods. Diabetes. 1990;40:A165. [Google Scholar]
- 43.Helgeson VS, Reynolds KA, Siminerio L, Escobar O, Becker D. Parent and adolescent distribution of responsibility for diabetes self-care: Links to health outcomes. J Pediatr Psychol. 2008;33:497–508. doi: 10.1093/jpepsy/jsm081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnston LD, O’Malley PM, Bachman JG, Shulenberg JE. Monitoring the future national survey results on drug use, 1975–2004: Volume II, College students and adults ages 19–45. Bethesda: National Institute on Drug Abuse; 2005. [Google Scholar]
- 45.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 46.American Diabetes Association. Standards of medical care in diabetes-2013. Diabetes Care. 2013;36:S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ruehlman LS, Karoly P. With a little flak from my friends: Development and preliminary validation of the Test of Negative Social Exchange (TENSE) Psychol Assessment. 1991;3:97–104. [Google Scholar]
- 48.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA US: Sage Publications, Inc; 1991. [Google Scholar]
- 49.Brehm JW. A theory of psychological reactance. Academic Press; 1966. [Google Scholar]
- 50.Reynolds CR, Kamphaus RW. Behavior Assessment System for Children. Circle Pines, MN: American Guidance Service; 1992. [Google Scholar]
- 51.Morrongiello BA, Klemencic N, Corbett M. Interactions between child behavior patterns and parental supervision: Implications for children’s risk of unintentional injury. Child Dev. 2008;79:627–638. doi: 10.1111/j.1467-8624.2008.01147.x. [DOI] [PubMed] [Google Scholar]
- 52.Morrongiello BA, Walpole B, McArthur BA. Young children’s risk of unintentional injury: A comparison of mothers’ and fathers’ supervision beliefs and reported practices. J Pediatr Psychol. 2009;34:1063–1068. doi: 10.1093/jpepsy/jsp011. [DOI] [PubMed] [Google Scholar]
- 53.Wysocki T, Harris MA, Buckloh LM, et al. Randomized trial of behavioral family systems therapy for diabetes: Maintenance of effects on diabetes outcomes in adolescents. Diabetes Care. 2007;30:555–560. doi: 10.2337/dc06-1613. [DOI] [PubMed] [Google Scholar]