Abstract
Background
The single most important risk factor for postpartum maternal infection is cesarean section. Routine prophylaxis with antibiotics may reduce this risk and should be assessed in terms of benefits and harms.
Objectives
To assess the effects of prophylactic antibiotics compared with no prophylactic antibiotics on infectious complications in women undergoing cesarean section.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register (May 2009).
Selection criteria
Randomized controlled trials (RCTs) and quasi-RCTs comparing the effects of prophylactic antibiotics versus no treatment in women undergoing cesarean section.
Data collection and analysis
Two authors independently assessed the studies for inclusion, assessed risk of bias and carried out data extraction.
Main results
We identified 86 studies involving over 13,000 women. Prophylactic antibiotics in women undergoing cesarean section substantially reduced the incidence of febrile morbidity (average risk ratio (RR) 0.45; 95% confidence interval (CI) 0.39 to 0.51, 50 studies, 8141 women), wound infection (average RR 0.39; 95% CI 0.32 to 0.48, 77 studies, 11,961 women), endometritis (RR 0.38; 95% CI 0.34 to 0.42, 79 studies, 12,142 women) and serious maternal infectious complications (RR 0.31; 95% CI 0.19 to 0.48, 31 studies, 5047 women). No conclusions can be made about other maternal adverse effects from these studies (RR 2.43; 95% CI 1.00 to 5.90, 13 studies, 2131 women). None of the 86 studies reported infant adverse outcomes and in particular there was no assessment of infant oral thrush. There was no systematic collection of data on bacterial drug resistance. The findings were similar whether the cesarean section was elective or non elective, and whether the antibiotic was given before or after umbilical cord clamping. Overall, the methodological quality of the trials was unclear and in only a few studies was it obvious that potential other sources of bias had been adequately addressed.
Authors’ conclusions
Endometritis was reduced by two thirds to three quarters and a decrease in wound infection was also identified. However, there was incomplete information collected about potential adverse effects, including the effect of antibiotics on the baby, making the assessment of overall benefits and harms complicated. Prophylactic antibiotics given to all women undergoing elective or non-elective cesarean section is clearly beneficial for women but there is uncertainty about the consequences for the baby.
BACKGROUND
The single most important risk factor for postpartum maternal infection is cesarean section (Declercq 2007; Gibbs 1980). Women undergoing cesarean section have a five to 20-fold greater risk for infection and infectious morbidity compared with a vaginal birth. In Western countries the percentage of live births by cesarean section is around 22% (range 12.9% to 33.3%)(OECD 2007); in developing countries the overall rate is around 12% but varies widely by region (0.40% to 40%)(Thomas 2006). Infectious complications that occur after cesarean births are an important and substantial cause of maternal morbidity and are associated with a significant increase in hospital stay (Henderson 1995). Infections can affect the pelvic organs, the surgical wound, and the urinary tract.
Description of the condition
Infectious complications following cesarean birth include fever (febrile morbidity), wound infection, endometritis (inflammation of the lining of the uterus), and urinary tract infection. There can also occasionally be serious infectious complications including pelvic abscess (collection of pus in the pelvis), bacteremia (bacterial infection in the blood), septic shock (reduced blood volume due to infection), necrotizing fasciitis (tissue destruction in the uterine wall) and septic pelvic vein thrombophlebitis (inflammation and infection of the veins in the pelvis); sometimes these can lead to maternal mortality (Boggess 1996; Enkin 1989; Gibbs 1980; Leigh 1990).
Fever can occur after any operative procedure, and a low grade fever following a cesarean birth may not necessarily be a marker of infection (MacLean 1990). Without prophylaxis, the incidence of endometritis is reported to range from 20% to 85%; rates of wound infection and serious infectious complications as high as 25% have been reported (Enkin 1989). There has been no consistent application of a standard definition for endometritis nor wound infection, and surveillance strategies for the ascertainment of infections, especially following hospital discharge, vary widely (Baker 1995; Hulton 1992). Differences in ethnicity, socioeconomic status of the population studied will explain some of the variability in incidence, as will the use of different criteria to diagnose infection (Herbert 1999). Using the Centers for Disease Control (CDC) definitions for infection, the pooled mean rate of surgical site infections after cesarean section for US hospitals participating in the CDC and Prevention’s National Nosocomial Infections Surveillance System from January 1992 through June 2004 was 3.15%, ranging from 2.71% for low-risk patients to 7.53% for high-risk patients (NNIS 2004). These rates, when compared with infection rates following other surgical procedures that are collected as part of the NNIS system, are high. Given the number of cesarean sections performed, these rates translate into very large numbers of women with an infectious complication following birth, and significant costs and morbidity.
Factors that have been associated with an increased risk of infection and infectious morbidity among women who have a cesarean include emergency cesarean section, labor and its duration, ruptured membranes and the duration of rupture, the socioeconomic status of the woman, number of prenatal visits, vaginal examinations during labor, internal fetal monitoring, urinary tract infection, anemia, blood loss, obesity, diabetes, general anesthesia, development of subcutaneous hematoma, the skill of the operator and the operative technique (Beattie 1994; Desjardins 1996; Enkin 1989; Gibbs 1980; Killian 2001; Magann 1995; Olsen 2008; Webster 1988). The association of bacterial vaginosis with an increased incidence of endometritis following cesarean birth has also been reported (Watts 1990).
The most important source of micro-organisms responsible for post-cesarean section infection is the genital tract, particularly if the membranes are ruptured. Even in the presence of intact membranes, microbial invasion of the intrauterine cavity is common, especially with preterm labor (Watts 1992). Infections are commonly polymicrobial (caused by many organisms). Pathogens isolated from infected wounds and the endometrium include Escherichia coli and other aerobic gram negative rods, group B streptococcus and other streptococcus species, Enterococcus faecalis, Staphylococcus aureus and coagulase negative staphylococci, anaerobes (including Peptostreptococcus species and Bacteroides species), Gardnerella vaginalis and genital mycoplasmas (Martens 1995; Roberts 1993; Watts 1991). Although Ureaplasma urealyticum is very commonly isolated from the upper genital tract and infected wounds, it is unclear whether it is a pathogen in this setting (Roberts 1993). Wound infections caused by Staphylococcus aureus and coagulase negative staphylococci arise from contamination of the wound with the endogenous flora of the skin at the time of surgery (Emmons 1988).
Description of the intervention
Guidelines recommend the use of antibiotics with a relatively narrow spectrum of activity for prophylaxis based on factors such as cost, half life, safety and antimicrobial resistance and to avoid broad spectrum drugs that are usually reserved for treatment (Bratzler 2004). There are over 20 antibiotic regimens that have been compared for cesarean section prophylaxis. Some of these drugs have activity against a narrow range of potential pathogens (e.g. metronidazole, gentamicin), others specifically have additional anaerobic activity (e.g. cefoxitin and cefotetan), others have activity against Staphylococcus aureus (e.g. cefazolin) and yet others have an extended spectrum of coverage (e.g. meropenem). Details of the different antibiotic regimens for prophylaxis at cesarean section that have been compared and their effectiveness are included in another Cochrane review (Hopkins 1999).
There are differences in the route of administration of prophylactic antibiotics; for cesarean section the antibiotic is generally given intravenously. Usually a single dose is administered at the time of the procedure or multiple doses administered over a short period of time.
For cesarean section, prophylactic antibiotics are administered either before or after the cord is clamped (Classen 1992; Cunningham 1983; Wax 1997), although general guidelines for the prevention of surgical site infections recommend the antimicrobial dose is administered before the incision to achieve low infection rates (Bratzler 2004). A recent meta-analysis on the timing of perioperative antibiotics for cesarean delivery concluded that there was strong evidence that antibiotic prophylaxis that is given before skin incision decreases maternal infectious complications, without affecting the infant (Costantine 2008). However, it is argued that the timing of antibiotic administration may mask septic complications in the infant (Cunningham 1983). Additionally if the antibiotic is given before cord clamping, the baby will be exposed to the antibiotic via the placenta, and there may be exposure through breast milk if the antibiotic is given either before or after cord clamping, though the passage of antibiotic through the breast milk is thought to minimal (Enkin 1989). Because of the potential for adverse outcomes for the baby and the effect on maternal infectious complications, this review investigated the timing of antibiotic administration (see Subgroup analysis and investigation of heterogeneity).
How the intervention might work
General principles for the prevention of any surgical infection include sound surgical technique, skin antisepsis and antimicrobial prophylaxis (Owen 1994). Antibiotics administered prophylactically reduce the bacterial inoculum at the time of surgery and decrease the rate of bacterial contamination of the surgical site. An adequate antibiotic level in the tissue can augment natural immune defence mechanisms and help kill bacteria that are invariably in-oculated into the wound at the time of surgery (Talbot 2005).
Potential adverse effects of antibiotic prophylaxis
There are commonly identified adverse effects of antibiotic therapy which include gastrointestinal symptoms (nausea, vomiting or diarrhoea), skin rashes, thrush (candidiasis, which can affect both mother and baby) and joint pain (Dancer 2004). There can also occasionally be blood problems, kidney or liver damage (Dancer 2004; Westphal 1994) and anaphylaxis (a hypersensitivity reaction to a foreign substance leading to shock and collapse, which can be fatal).
Because there are some data that antibiotics reaching the baby during labor, or in the very early postnatal period, can affect the pattern of bacterial flora in the infant gut, with the potential to affect the baby’s developing immune system (Bedford Russell 2006), it is important to assess the impact of antibiotics given to the mother on the baby’s health.
Antibiotic prophylaxis may lead to increased drug resistant strains of bacteria which may be associated with infection. Resistant organisms may spread within the hospital and be associated with hospital-acquired drug resistant infections (Dancer 2004). These adverse effects cannot be assessed readily in randomized controlled trials, and additional research needs to be undertaken to assess the impact of prophylactic antibiotic use on the level of resistant bacteria, e.g. MRSA and C difficile in hospitals.
Why it is important to do this review
Surveys suggest that there is inconsistent and variable application of the use of prophylactic antibiotics at cesarean sections (Huskins 2001; Olsen 2008; Pedersen 1996). Prophylactic antibiotics have been shown, in previous versions of this review, to be effective in reducing febrile morbidity, endometritis, wound infection and urinary tract infection (Smaill 1995a; Smaill 1995b; Smaill 2002). In addition, both ampicillin and first generation cephalosporins appeared to have similar efficacy in reducing post-operative endometritis, and there did not appear to be any added benefit in utilizing a more broad spectrum agent or a multiple dose regimen (Hopkins 1999). However, it is important to update this evidence with more recent studies, to update the review methodology and also to address the question of whether increasing antimicrobial resistance has had an impact on the benefit of antibiotic prophylaxis.
The adverse effects of antibiotics for the woman and her infant and the potential for increased use of antimicrobial prophylaxis to contribute to the development of antimicrobial resistance are important considerations (Mallaret 1990; Shlaes 1997), as are the cost-effectiveness of different strategies (Mugford 1989). As well, it is important to assess any possible impact of maternal antibiotic treatment on the baby, as there is evidence that antibiotics given near or shortly after birth can affect the infant’s gut bacterial flora, with the potential to impact mucosal and systemic immune function (Bedford Russell 2006).
Particularly controversial is whether antibiotic treatment should be given to all mothers or only to those at greatest risk of infection (Ehrenkrans 1990; Gilstrap 1988; Howey 1990; Suonio 1989). Women undergoing cesarean section can be divided into low- and high-risk groups for infection. Women at high risk include those undergoing cesarean section after rupture of the membranes or onset of labor (ACOG 2003). We were interested to see if there was a difference in effectiveness depending on whether there is a high or low risk of infection. We performed a subgroup analysis based on whether the cesarean section was a planned procedure (elective) or whether there was active labor or ruptured membranes (non-elective).
It has been suggested that institutions with a low levels of baseline infections may see no impact of routine use of antibiotics, while institutions with high baseline infection rates may see a benefit. To explore this would require baseline measurements taken before randomization (e.g. data on infection rates over the previous year at the hospitals in the trial). It would not be valid to use a variable that arises after randomization for performing the stratification into high and low infection rates, such as the wound infection rates found in each trial’s control group. This could easily lead to spurious results, because of regression to the mean: there is a relationship between the control group event rate and the effect size, with larger treatment effects associated with higher control group event rates. A difference in treatment effects between high and low control group event rates would be expected and would not necessarily indicate a real difference (Gates 2008). Because we were interested to see if there was an effect of baseline risk of infection on outcomes, we looked for any information in the studies that described rates of infection before the intervention. This review will focus on whether antibiotics do more good than harm overall. A comparison of the effectiveness of different antibiotic regimens is covered in another Cochrane review (Hopkins 1999). Additional ways for trying to reduce post-cesarean infections (which may be the subject of future Cochrane reviews) include: skin preparation at cesarean section; double gloving or changing gloves (or both) before closure; peritoneal lavage; and vaginal antiseptic solution preparation.
OBJECTIVES
To determine, from the best evidence available, the effectiveness of prophylactic antibiotics compared with placebo, or no treatment, given to women when undergoing a cesarean section for reducing the incidence of febrile morbidity, wound infection, endometritis, urinary tract infection or any serious infectious complication, and to assess potential adverse effects and any impact on the infant, either short term or long term.
Comparisons between specific regimens will not be included in this version of the review; these have been assessed in another Cochrane review (Hopkins 1999) which is currently being updated.
METHODS
Criteria for considering studies for this review
Types of studies
All randomized controlled trials (RCTs) to evaluate the effects of prophylactic antibiotics in women undergoing cesarean section. Quasi-RCTs will also be included. We shall include cluster-RCTs should any be identified but cross-over trials are inappropriate for this question.
Types of participants
Women undergoing cesarean section, both elective and non-elective/emergency.
Types of interventions
Trials will be considered if they compare any prophylactic antibiotic regimen administered for cesarean section with placebo or no treatment.
Types of outcome measures
Primary outcomes
Maternal
Febrile morbidity (fever)
Wound infection (infection of the surgical incision)
Endometritis (inflammation of the lining of the womb)
Serious infectious complication (such as bacteremia, septic shock, septic thrombophlebitis, necrotizing fasciitis, or death attributed to infection)
Infant
Immediate adverse effects of antibiotics on the infant (unsettled, diarrhoea, rashes)
Oral thrush (candidiasis)
Secondary outcomes
Maternal
Urinary tract infection
Adverse effects of treatment on the woman (e.g. allergic reactions, nausea, vomiting, diarrhoea, skin rashes, thrush)
Length of stay in hospital
Infant
Length of stay in hospital
Long-term adverse effects (e.g. general health; frequency of visits to hospital)
Immune system development (using a validated scoring assessment)
Additional outcomes
Development of bacterial resistance
Cost
Search methods for identification of studies
Electronic searches
We contacted the Trials Search Co-ordinator to search the Cochrane Pregnancy and Childbirth Group’s Trials Register (May 2009).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co-ordinator and contains trials identified from:
quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL and MEDLINE, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co-ordinator searches the register for each review using the topic list rather than keywords.
Searching other resources
We searched the reference lists at the end of papers for further studies.
We did not apply any language restrictions.
Data collection and analysis
For the new studies identified since publication of the previous version of this review (Smaill 2002), two review authors have made the inclusion/exclusion decisions and undertaken data extraction independently, then conferred to agree. Had there been any disagreement, a third assessor would have been asked to decide. With the studies in the previous version of the review (Smaill 2002), one author (F Smaill) has done the data extraction twice; once originally for the previous version of this review and again now, eight years later, to check for accuracy. The following now describes the new methodology being used.
Selection of studies
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion. If required a third person would have been consulted to resolve any disagreements.
Data extraction and management
We designed a form to extract data. For eligible studies, we extracted the data independently using the agreed form. We resolved discrepancies through discussion or, if required, a third person would have been consulted. We entered the data into Review Manager software (RevMan 2008) and checked them for accuracy. When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Both review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). Any disagreement would have been resolved by discussion or by involving a third assessor.
1) Sequence generation (checking for possible selection bias)
We described for each included study the methods used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the methods as:
adequate (any truly random process, e.g. random number table; computer random number generator);
inadequate (any non random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear.
2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal the allocation sequence in sufficient detail and determined whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
adequate (e.g. telephone or central randomization; consecutively numbered sealed opaque envelopes);
inadequate (e.g. open random allocation; unsealed or non-opaque envelopes, alternation; date of birth);
unclear.
3) Blinding (checking for possible performance bias)
We described for each included study all the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We also provided information on whether the intended blinding was effective. Where blinding was not possible, we assessed whether the lack of blinding was likely to have affected outcomes and introduced bias. Blinding was assessed separately for different outcomes or classes of outcomes.
We assessed the methods as:
adequate, inadequate or unclear for participants;
adequate, inadequate or unclear for personnel;
adequate inadequate or unclear for outcome assessors;
where ‘adequate’ was when there was blinding or where we assessed that the outcome or the outcome measurement was not likely to have been influenced by lack of blinding.
4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We described for each included study and for each outcome or class of outcomes the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomized participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported or could be supplied by the trial authors, we re-included missing data in the analyses which we performed.
We discussed whether missing data greater than 20% might impact on outcomes acknowledging that with long-term follow up, complete data are difficult to attain.
5) Selective reporting bias
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
adequate (where it was clear that all of the study’s pre-specified outcomes and all expected outcomes of interest to the review have been reported);
inadequate (where not all the study’s pre-specified outcomes have been reported; one or more reported primary outcomes were not pre-specified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
unclear.
6) Other sources of bias
We described for each included study any important concerns we had about other possible sources of bias. This included potential sources of bias related to, for example, publication bias, whether the trial was stopped early and extreme baseline imbalance.
We assessed whether each study was free of other problems that could put it at risk of bias:
yes;
no;
unclear.
7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). These criteria suggest (1) high risk of bias is where plausible bias seriously weakens confidence in the results; (2) unclear risk of bias is where plausible bias raises doubts about the results; and (3) low risk of bias is where plausible bias is unlikely to seriously alter the results. With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it was likely to impact on the findings. We planned to explore the impact of the level of bias through undertaking sensitivity analyses - see Sensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we present results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we used the mean difference if outcomes were measured in the same way between trials. We used the standardized mean difference to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster-randomized trials
We would have included cluster-randomized trials (cluster-RCTs) in the analyses along with individually-randomized trials, had we identified any cluster-RCTs. Their sample sizes would have been adjusted using the methods described in Higgins 2008 using an estimate of the intracluster correlation co-efficient (ICC) derived from the trial (if possible), or from another source. If ICCs from other sources were used, this would have been reported and sensitivity analyses conducted to investigate the effect of variation in the ICC. If we had identified both cluster-RCTs and individually-randomized trials, we had planned to synthesise the relevant information. We would have considered it reasonable to combine the results from both if there was little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomization unit was considered to be unlikely.
We would have also acknowledged heterogeneity in the randomization unit and performed a separate meta-analysis.
Dealing with missing data
For included studies, levels of attrition were noted. We would have explored the impact of including studies with high levels of missing data in the overall assessment of treatment effect using sensitivity analysis.
For all outcomes analyses were carried out, as far as possible, on an intention-to-treat basis, i.e. we attempted to include all participants randomized to each group in the analyses. The denominator for each outcome in each trial was the number of participants with data, that is, the number randomized minus any participants whose outcomes were known to be missing (available case analysis). If more than 20% of participants were missing from an outcome we planned to explore by sensitivity analyses (see Sensitivity analysis).
Assessment of heterogeneity
We have assessed statistical heterogeneity in each meta-analysis using the T2 (tau-squared), I2 and Chi2 statistics. We have regarded heterogeneity as substantial if T2 was greater than zero and either I2 was greater than 30% or there was a low P-value (less than 0.10) in the Chi2 test for heterogeneity. Where we found heterogeneity and random-effects was used, we have reported the average risk ratio, or average mean difference or average standard mean difference.
Assessment of reporting biases
Where we suspected reporting bias (see Assessment of reporting biases), we attempted to contact study authors asking them to provide missing outcome data. Where this was not possible, and the missing data were thought to introduce serious bias, we planned to explore the impact of including such studies in the overall assessment of results by a sensitivity analysis.
Where there were 10 or more studies in a meta-analysis, we have investigated reporting biases (such as publication bias) using funnel plots. We have assessed funnel plot asymmetry visually. In a subsequent update of this review we shall include formal tests for funnel plot asymmetry and we plan to use the test proposed by Egger 1997 for continuous outcomes and the test proposed by Harbord 2006 for dichotomous outcomes.
Data synthesis
We have carried out statistical analysis using the Review Manager software (RevMan 2008). We have used fixed-effect meta-analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect, i.e. where trials were examining the same intervention and the trials’ populations and methods were judged sufficiently similar. If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we have used random-effects analysis to produce an overall summary, if this was considered clinically meaningful. If an average treatment effect across trials had not been clinically meaningful, we would not have combined heterogeneous trials. If we used random-effects analyses, the results have been presented as the average treatment effect and its 95% confidence interval.
Subgroup analysis and investigation of heterogeneity
We carried out the following subgroup analyses.
By type of surgery: (a) elective cesarean section; (b) non-elective cesarean section; and (c) mixed or not defined. (Rupture of membranes for more than six hours or the presence of labor was used to differentiate a non-elective cesarean section from an elective procedure.)
By time of administration: (a) before cord clamping; (b) after cord clamping; (c) not defined.
For fixed-effect meta-analyses, we used visual inspection with non-overlapping confidence intervals to indicate a statistically significant difference in treatment effect between the subgroups. We had planned to conduct subgroup analyses classifying whole trials by interaction tests as described by Deeks 2001 and will undertake these in a subsequent update of this review. For random-effects meta-analyses, we also used visual inspection with non-overlapping confidence intervals to indicate a statistically significant difference in treatment effect between the subgroups
Sensitivity analysis
We planned to carry out sensitivity analysis to explore the effect of trial quality for important outcomes in the review. Where there was a high risk of bias associated with a particular aspect of study quality, for example, quasi-RCTs where there is inadequate sequence generation and allocation concealment (Schultz 1995), we planned to explore this by sensitivity analysis (Higgins 2008).
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification.
Results of the search
The search of the Cochrane Pregnancy and Childbirth Group’s Trials Register identified 129 publications from 116 studies (13 studies had a second publication for the one study). Eighty-six studies were included (Characteristics of included studies), 20 were excluded (Characteristics of excluded studies) and 10 are awaiting classification, all because they are being translated (Characteristics of studies awaiting classification). We found no additional studies through searching reference lists.
Included studies
The 86 studies that met the inclusion criteria for this review enrolled over 13,000 women. For detailed information on the studies, see table of Characteristics of included studies. No study reported on baseline risk of infection before the intervention.
Setting
While the majority of the studies included in the review were conducted in industrial countries (e.g. US, Western Europe, Scandinavia, Canada and New Zealand), studies were reported from developing countries including Sudan, Nigeria, Tunisia, Kenya, Zimbabwe, and South Africa as well as Mexico, Greece, Turkey, Israel, the Middle East, China and Malaysia. Many of the studies included a majority of women who were identified as from a low socio-economic group, but other studies enrolled women who were not perceived to be at an increased risk of infection because of socio-economic status. Most studies adequately described the characteristics of the women who were enrolled, including details of the indication for cesarean section, mean duration of labor and membrane rupture and number of repeat sections. One study included information on the number of women who were HIV positive (Bagratee 2001). In no study were details on the incidence of bacterial vaginosis provided. No study reported baseline infection rates before the intervention.
Type of cesarean section
One objective of this review was to study the effect of prophylaxis in both elective and non-elective cesarean sections, and strict definitions of an elective and non-elective cesarean section were used by the authors of this review to categorize women and studies. In eleven studies (N = 2225), data on women undergoing an elective cesarean section were available (Adam 2005; Bagratee 2001; Duff 1982; Huam 1997; Jakobi 1994; Kolben 2001; Mahomed 1988; Rizk 1998; Shah 1998; Ujah 1992; Wu 1991). In 19 studies (N = 2229), there were data on non-elective procedures (Conover 1984; D’Angelo 1980; Elliott 1986; Freeman 1982; Fugere 1983; Gibbs 1981; Harger 1981; Hawrylyshyn 1983; Leonetti 1989; Moodley 1981; Ross 1984; Ruiz-Moreno 1991; Scarpignato 1982; Schedvins 1986; Tzingounis 1982; Weissberg 1971; Wong 1978; Work 1977; Young 1983). Three studies (N = 573) included both women having elective cesareans and non-elective cesareans (Dashow 1986; Jaffe 1984; Rothbard 1975). The remaining, and the majority of studies did not differentiate between an elective or non-elective procedure, or the definitions used were not consistent with those used in this review; these have been grouped as ‘both’ or ‘undefined’. Often a repeat section had been classified as elective by the study authors, but it was not always evident that all of these women were indeed not in labor and often the duration of membrane rupture was unclear. Fifty-two studies (N = 7765) were classified as undefined type of cesarean section (Adeleye 1981; Allen 1972; Apuzzio 1982; Bibi 1994; Bilgin 1998; Bourgeois 1985; Carl 2000; Chan 1989; Cormier 1989; De Boer 1989; Dillon 1981; Duff 1980; Engel 1984; Escobedo 1991; Gall 1979; Ganesh 1986; Gerstner 1980; Gibbs 1972; Gibbs 1973; Gordon 1979; Gummerus 1984; Hager 1983; Hagglund 1989; Ismail 1990; Jaffe 1985; Karhunen 1985; Kellum 1985; Kreutner 1978; Kristensen 1990; Lapas 1988; Levin 1983; Lewis 1990; Mallaret 1990; McCowan 1980; Miller 1968; Moro 1974; Morrison 1973; Ng 1992; Padilla 1983; Phelan 1979; Polk 1982; Reckel 1985; Rehu 1980; Roex 1986; Rudd 1981; Saltzman 1985; Stage 1982; Stiver 1983; Tully 1983; Turner 1990; Walss Rodriguez 1990; Yip 1997). One study reported both elective and emergency cesarean sections; the emergency sections, however, did not meet our definition of non-elective and these have been classified as “undefined” (Rouzi 2000).
Timing of antibiotic administration
Antibiotics for prophylaxis were administered intravenously either at the start of the operative procedure (“before cord”) or at or after clamping of the cord. In 36 studies (N = 5164), data on outcomes were available when the antibiotic had been administered before clamping of the cord (Adam 2005; Adeleye 1981; Allen 1972; Bibi 1994; Chan 1989; De Boer 1989; Duff 1980; Duff 1982; Freeman 1982; Gall 1979; Gerstner 1980; Gibbs 1972; Gibbs 1973; Hagglund 1989; Huam 1997; Jaffe 1984; Jaffe 1985; Kreutner 1978; Lapas 1988; Mahomed 1988; McCowan 1980: Miller 1968; Moodley 1981; Moro 1974; Morrison 1973; Ng 1992; Phelan 1979; Reckel 1985; Rehu 1980; Ross 1984; Rothbard 1975; Stage 1982; Turner 1990; Tzingounis 1982; Work 1977; Yip 1997). This was variably described as “pre-operatively”, “with induction of anaesthesia” or “before clamping of the cord”. In 43 studies (N = 7284) the antibiotic was administered at or after cord clamping (Apuzzio 1982; Bagratee 2001; Bourgeois 1985; Bilgin 1998; Carl 2000; Conover 1984; Cormier 1989; Dashow 1986; D’Angelo 1980; Dillon 1981; Elliott 1986; Engel 1984; Escobedo 1991; Fugere 1983; Ganesh 1986; Gibbs 1981; Gummerus 1984; Hager 1983; Harger 1981; Hawrylyshyn 1983; Ismail 1990; Jakobi 1994; Karhunen 1985; Kellum 1985; Kristensen 1990; Leonetti 1989; Levin 1983; Lewis 1990; Mallaret 1990; Polk 1982; Rizk 1998; Roex 1986; Rouzi 2000; Rudd 1981; Ruiz-Moreno 1991; Saltzman 1985; Shah 1998; Stiver 1983; Tully 1983; Walss Rodriguez 1990; Wong 1978; Wu 1991; Young 1983). Included in this group were studies where irrigation of the peritoneal or uterine cavity with an antibiotic containing solution was compared with either saline irrigation or no irrigation (Bourgeois 1985; Carl 2000; Conover 1984; Dashow 1986; Elliott 1986; Kellum 1985; Levin 1983; Lewis 1990; Rudd 1981; Wu 1991). There were six studies (N = 444) where there was insufficient information to know when the antibiotic had been administered, e.g. “operatively” or the results had been combined and these have been grouped together as “timing not defined” (Kolben 2001; Padilla 1983; Scarpignato 1982; Schedvins 1986; Ujah 1992; Weissberg 1971). In one study, results were available for antibiotic administration both before and after clamping of the cord (Gordon 1979).
Classes of antibiotics
The antimicrobial agents most often used in the trials included ampicillin, a first generation cephalosporin (usually cefazolin), a second generation cephalosporin (cefoxitin, cefotetan, cefamandole or cefuroxime), metronidazole, penicillins with an extended spectrum of activity (e.g. ticarcillin, mezlocillin or pipericillin), a beta-lactam/beta-lactamase inhibitor combination and an amino-glycoside-containing combination; see Characteristics of included studies for a classification of the antimicrobial agent used by antibiotic class. The penicillins have been divided into aminopenicilins (ampicillin), carboxypenicillins (carbenicillin, ticarcillin) or ureidopenicillins (mezlocillin, pipericillin). The second generation cephalosporins include the cefamycins (cefoxitin and cefotetan) that have extended anaerobic coverage. There was one study where the antimicrobial prophylaxis was administered by rectal suppository (De Boer 1989). The duration of the post-operative treatment course varied from a single intravenous dose (N = 22) to as long as a week. In a number of studies, antibiotics were continued for up to 24 hours following the procedure. While most studies were published in the 1980s, new studies have continued to be performed in the 1990s and the last study was published as recently as 2005. The next version of this review will include specific comparisons of the individual classes of antibiotics.
Assessing outcomes
The clinical criteria listed to define endometritis were consistent across trials. Febrile morbidity is a standard obstetrical outcome and was generally consistently reported although there was some variation in the exact criteria used for height of fever, interval between febrile episodes and interval from the operative procedure. Urinary tract infection generally meant a positive urine culture; symptoms related to the urinary tract were rarely required to be present. Wound infection usually was a clinical diagnosis and generally included induration, erythema, cellulitis or various degrees of drainage. A positive microbiological diagnosis was rarely required for the diagnosis of either wound infection or endometritis. There was no consistent approach to the definition of serious morbidity. For this review, all episodes of bacteremia have been classified as serious as have other complications such as pelvic abscess, pelvic thrombophlebitis and peritonitis. Some studies included other outcomes, e.g. need for additional antibiotic use and other infections, e.g. pneumonia. Some provided a measure of the fever as a ‘fever index’ which incorporated both the height of the fever and its duration. Where the duration of maternal hospital stay with its standard deviation was reported this has been included.
Side effects
Very few studies appeared to have consistently sought maternal side effects or neonatal/infant side effects and similarly it was the minority of studies that collected data on infectious complications after discharge.
Excluded studies
Of those studies excluded from the analysis, most were because either no clinical outcomes were reported or the specific outcomes of interest were not described. For some studies, although the trial was initially randomized, part-way through the study the placebo arm was dropped. Because results on the initially randomized part of the study were not available, these studies were not included in the analysis (See table of Characteristics of excluded studies for further details).
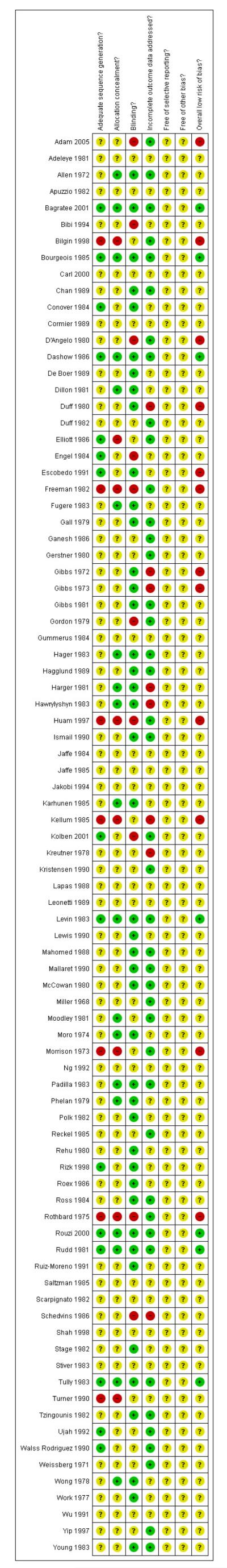
Risk of bias in included studies
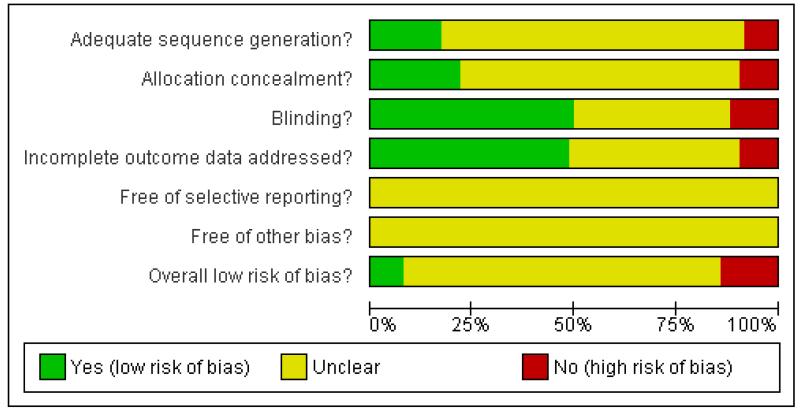
The methodological quality of the trials on the whole was unclear. This is mostly because the studies were undertaken a number of years ago, before the recent understanding of sources of bias in randomised controlled trials (Figure 1; Figure 2).
Figure 1. Methodological quality graph: review authors’ judgements about each methodological quality item presented as percentages across all included studies.
Figure 2. Methodological quality summary: review authors’ judgements about each methodological quality item for each included study.
Allocation
Seven studies assessed as adequate on sequence generation and allocation concealment (Bagratee 2001; Bourgeois 1985; Dashow 1986; Levin 1983; Rouzi 2000; Rudd 1981; Tully 1983). In 12 studies, the allocation concealment was adequate and although the randomization was unclear this was believed to be due to inadequate reporting rather than bias (Allen 1972; Dillon 1981; Fugere 1983; Hager 1983; Harger 1981; Hawrylyshyn 1983; Karhunen 1985; Moodley 1981; Moro 1974; Padilla 1983; Phelan 1979; Wong 1978). Seven studies were identified as quasi-RCTs (Bilgin 1998; Freeman 1982; Huam 1997; Kellum 1985; Morrison 1973; Rothbard 1975; Turner 1990).
Blinding
Approximately half of the studies (43/86) were placebo-controlled (which included the use of saline irrigation).
Incomplete outcome data
In most studies, all women who were initially randomized were included in the outcomes and an intention-to-treat analysis was performed. Dropouts were reported in about a quarter of studies but insufficient data were provided for them to be included in an intent-to-treat analysis. Where the group allocation of dropouts was not provided, there was the possibility that there may have been selective withdrawals from one or other of the groups. There were some studies where a discrepancy in the numbers allocated to the randomized groups, unlikely to have occurred by chance, was not accounted for. In most cases the numbers in the placebo group were smaller than those in the treatment group, raising the possibility of selective withdrawals not mentioned in the published report.
Selective reporting
This was unclear in all studies as we were unable to assess the trial protocols.
We undertook funnel plots for the primary outcomes to assess reporting bias, e.g. publication bias.
Other potential sources of bias
These were mostly unclear.
Effects of interventions
From the 86 studies included we have 14 meta-analyses.
1. Antibiotic prophylaxis versus no prophylaxis (Analyses 1.1 to 1.14)
Bearing in mind the lack of clarity regarding potential risk of bias for the included studies in this comparison, the overall findings were as follows.
Primary outcomes
There were reductions in all the maternal primary outcomes: febrile morbidity (average risk ratio (RR) 0.45; 95% confidence interval (CI) 0.39 to 0.51, 50 studies, 8141 women, random-effects [T2 = 0.09; Chi2 P = 0.0005; I2 = 45%], Analysis 1.1); wound infection (average RR 0.39; 95% CI 0.32 to 0.48, 77 studies, 11,961 women, random-effects [T2 = 0.14; Chi2 P = 0.04; I2 = 23%], Analysis 1.2); endometritis (RR 0.38; 95% CI 0.34 to 0.42, 79 studies, 12,142 women, Analysis 1.3) and serious infectious morbidity (RR 0.31; 95% CI 0.19 to 0.48, 31 studies, 5047 women, Analysis 1.4).
There were no data in any of the studies on the two infant primary outcomes of immediate adverse effects and infant thrush.
Secondary outcomes
There were reductions in both maternal urinary tract infection (RR 0.55; 95% CI 0.47 to 0.65, 61 studies, 9454 women, Analysis 1.7) and maternal length of stay in hospital (average mean difference (MD) −0.49; 95% CI −0.29 to −0.68, 17 studies, 3199 women, [T2 = 0.08; Chi2 P = 0.01; I2 = 49%], Analysis 1.9). Only 13 studies collected data on maternal adverse effects and suggested either an increase or no detectable effect (RR 2.43; 95% CI 1.00 to 5.90, 13 studies, 2131 women, Analysis 1.8).
There were no data in any of the studies on the other secondary outcomes.
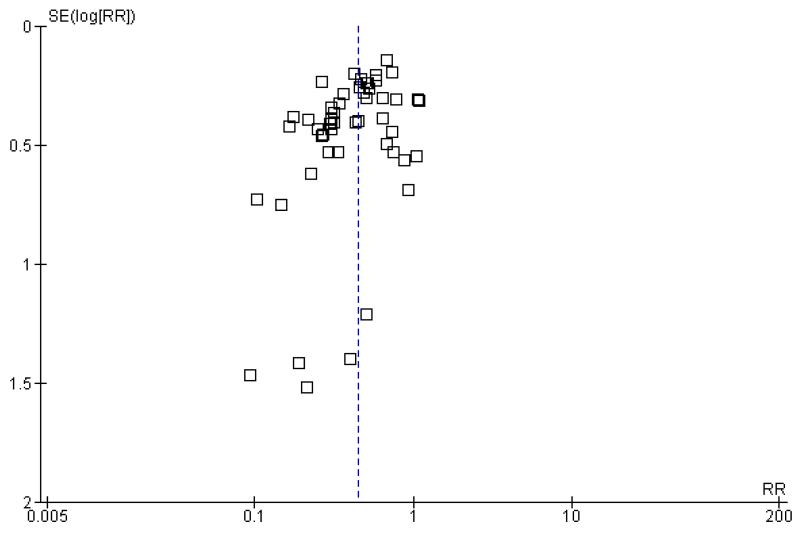
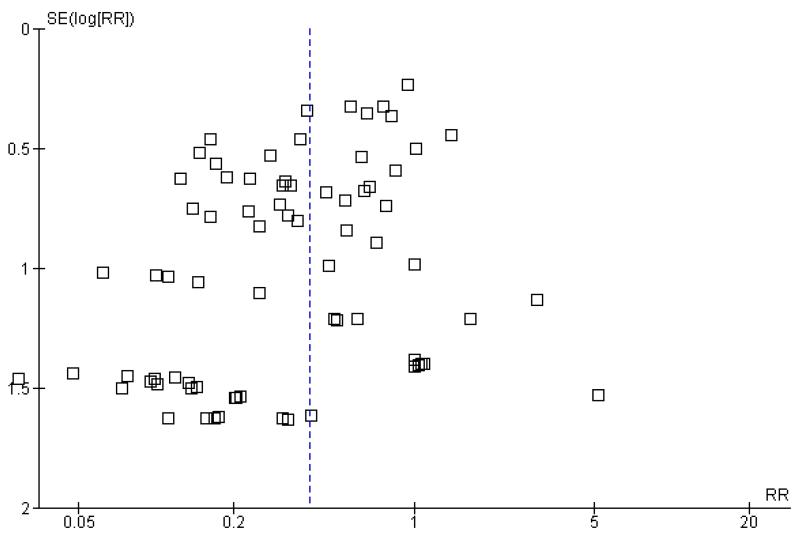
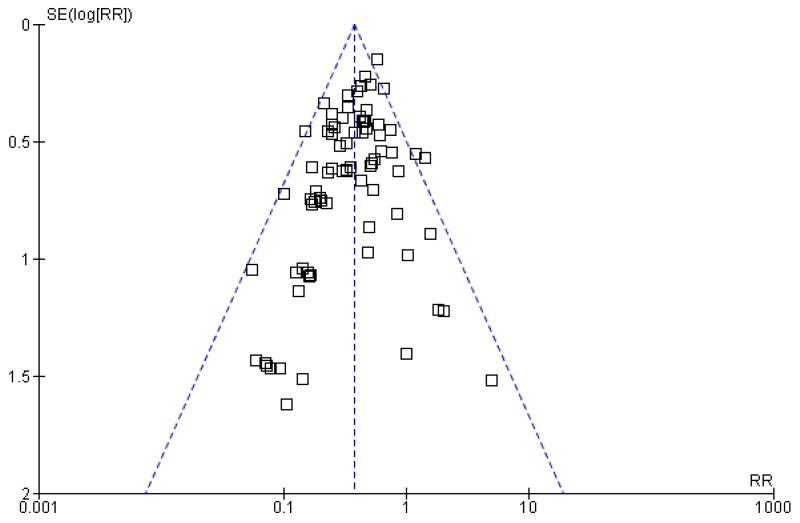
Reporting bias
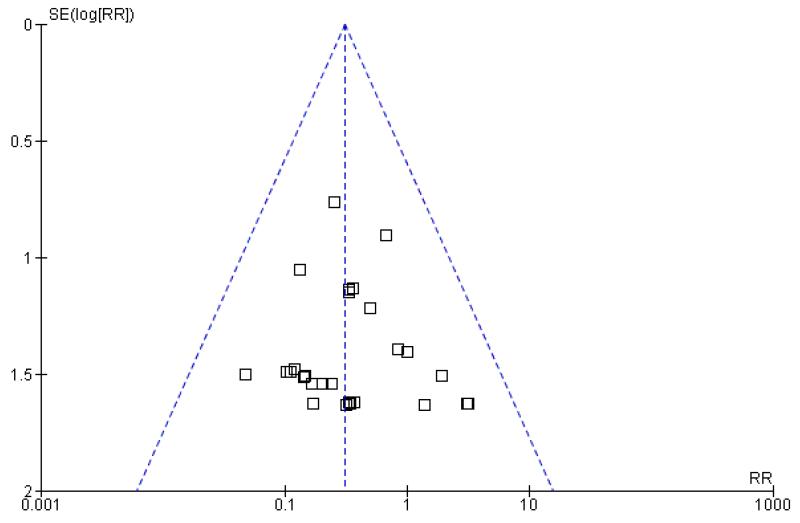
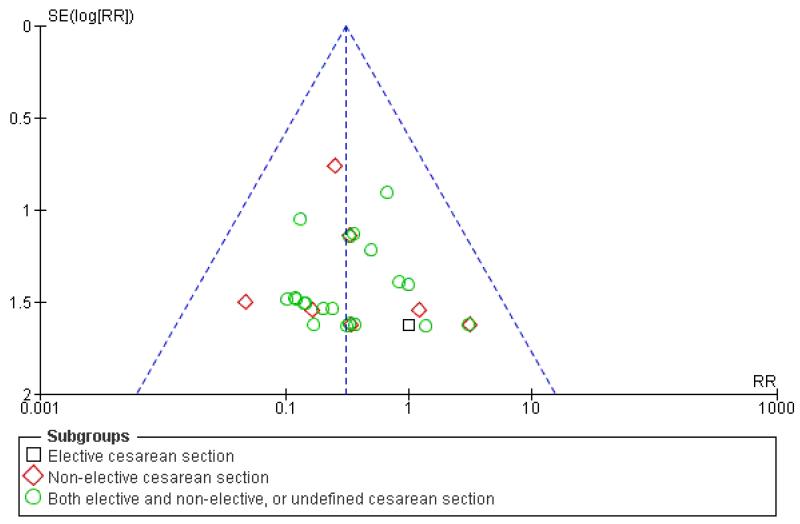
There was a potential for publication bias in the assessment of febrile morbidity, as judged by visual inspection of the funnel plot (Figure 3); however, we estimated that any reporting bias was unlikely to influence the results because of the large number of participants in the symmetrical part of the plot. There was no funnel plot asymmetry for the other primary outcomes (Figure 4; Figure 5; Figure 6).
Figure 3. Funnel plot of comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, outcome: 1.1 Maternal fever/febrile morbidity.
Figure 4. Funnel plot of comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, outcome: 1.2 Maternal wound infection.
Figure 5. Funnel plot of comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, outcome: 1.3 Maternal endometritis.
Figure 6. Funnel plot of comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, outcome: 1.4 Maternal serious infectious complications.
Study quality
We undertook a sensitivity analysis on the primary outcomes by study quality, omitting the seven quasi-RCTs (Bilgin 1998; Freeman 1982; Huam 1997; Kellum 1985; Morrison 1973; Rothbard 1975; Turner 1990). The overall findings remained very similar with reductions all the primary outcomes: febrile morbidity (average RR 0.46; 95% CI 0.40 to 0.53, 45 studies, 7323 women, random-effects [T2 = 0.09, Chi2 P = 0.001, I2 = 44%]; wound infection (average RR 0.41; 95% CI 0.33 to 0.50, 72 studies, 11,223 women, random-effects [T2 = 0.14, Chi2 P = 0.05, I2 = 23%); endometritis (RR 0.39; 95% CI 0.35 to 0.43, 73 studies, 11,274 women) and serious infectious morbidity remained the same as the main analysis contained no quasi-RCTs.
2. Antibiotic prophylaxis versus no prophylaxis, subgroups by type of cesarean section (Analyses 2.1 to 2.14)
We inspected the graphs visually and saw no difference in maternal febrile morbidity, wound infection or endometritis, and as well the confidence intervals for the summary estimates overlapped. These results suggest that there are benefits for the mother irrespective of whether the cesarean section is elective or emergency.There were insufficient data to assess any potential differential effect on maternal serious infectious complications. As above, there were no outcomes assessed on the infants in any of these studies.
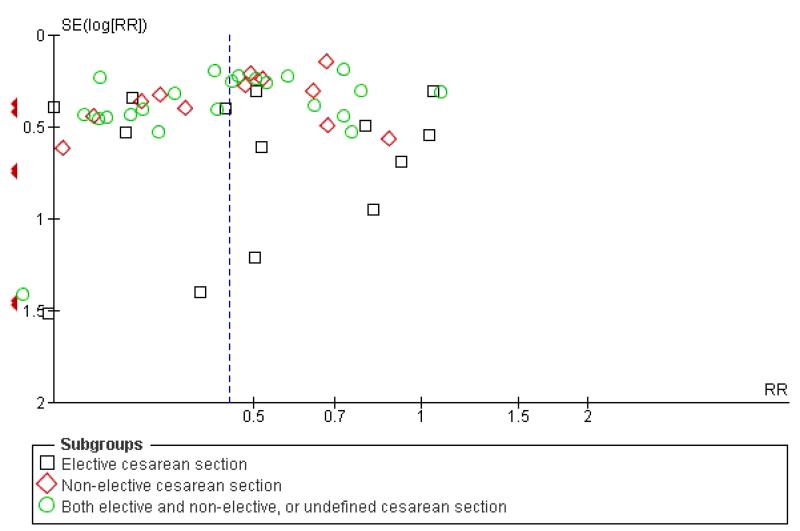
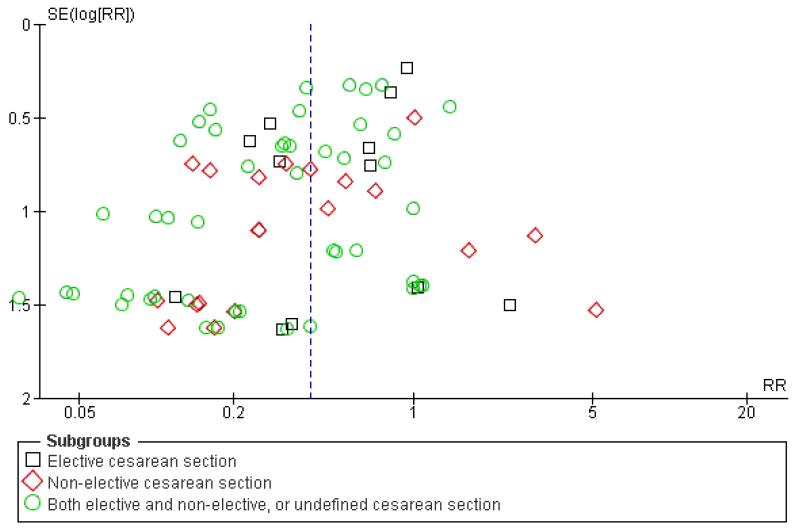
Reporting bias
As judged by a visual inspection of the funnel plot, there was a potential for publication bias in certain outcomes (e.g. febrile morbidity) (Figure 7; Figure 8; Figure 9; Figure 10).
Figure 7. Funnel plot of comparison: 1 Antibiotics versus no antibiotics - by type of cesarean section, outcome: 1.1 Maternal fever/febrile morbidity.
Figure 8. Funnel plot of comparison: 1 Antibiotics versus no antibiotics - by type of cesarean section, outcome: 1.2 Maternal wound infection.
Figure 9. Funnel plot of comparison: 1 Antibiotics versus no antibiotics - by type of cesarean section, outcome: 1.3 Maternal endometritis.
Figure 10. Funnel plot of comparison: 1 Antibiotics versus no antibiotics - by type of cesarean section, outcome: 1.4 Maternal serious infectious complications.
3. Antibiotic prophylaxis versus no prophylaxis, subgroups by timing of administration (Analyses 3.1 to 3.14)
We inspected the graphs visually and found no difference in maternal febrile morbidity, wound infection or endometritis, and as well the confidence intervals for the summary estimates overlapped. The results were similar for maternal serious infectious complication although there were insufficient data to conclude this with certainty. One of the reasons for looking at the different timing of administration was to assess any impact of antibiotic reaching the baby if given before cord clamping. However, none of the studies assessed outcomes on the baby.
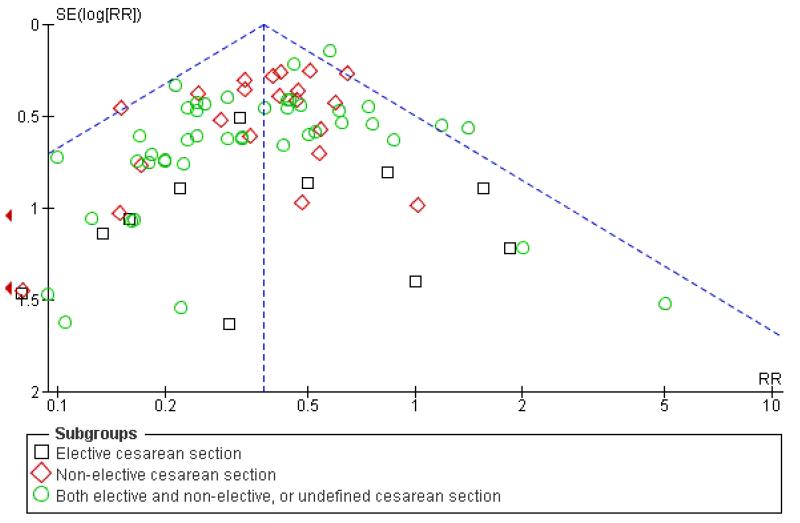
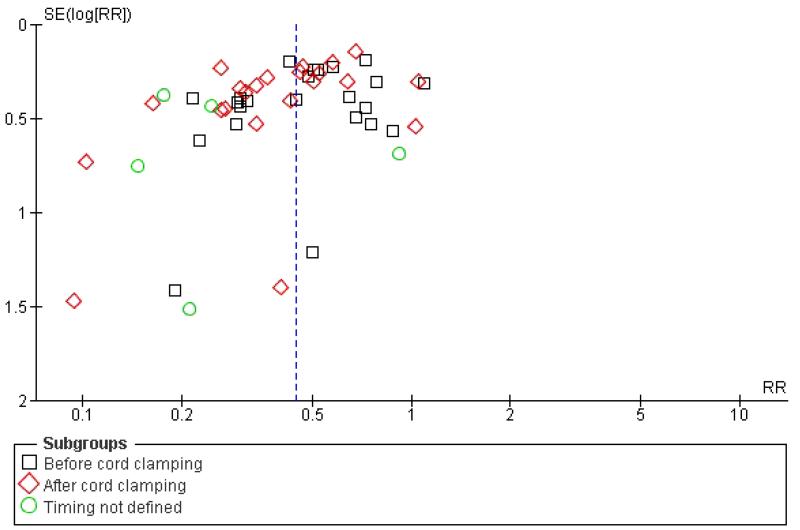
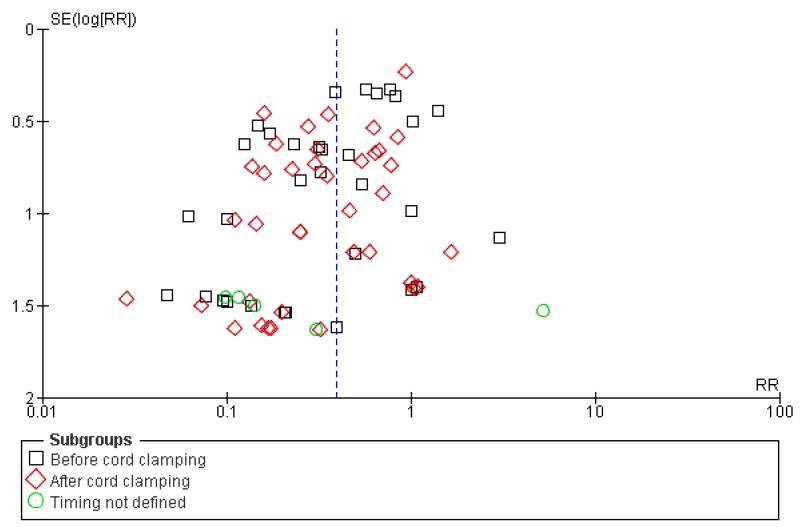
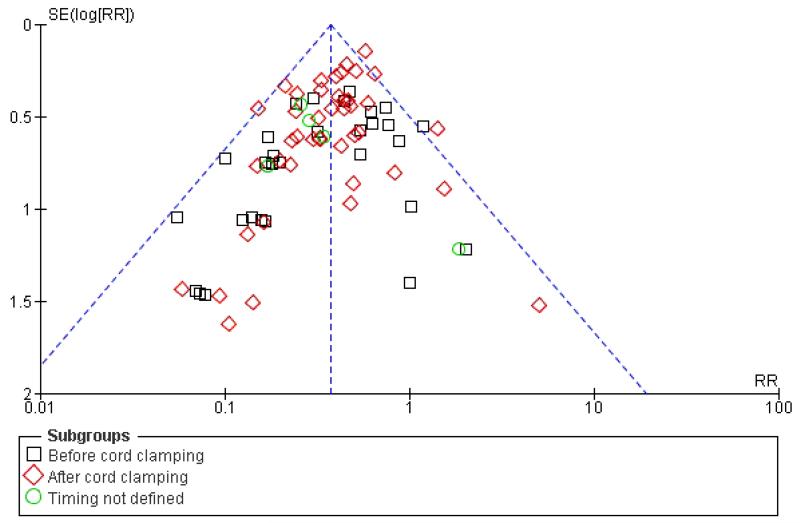
Reporting bias
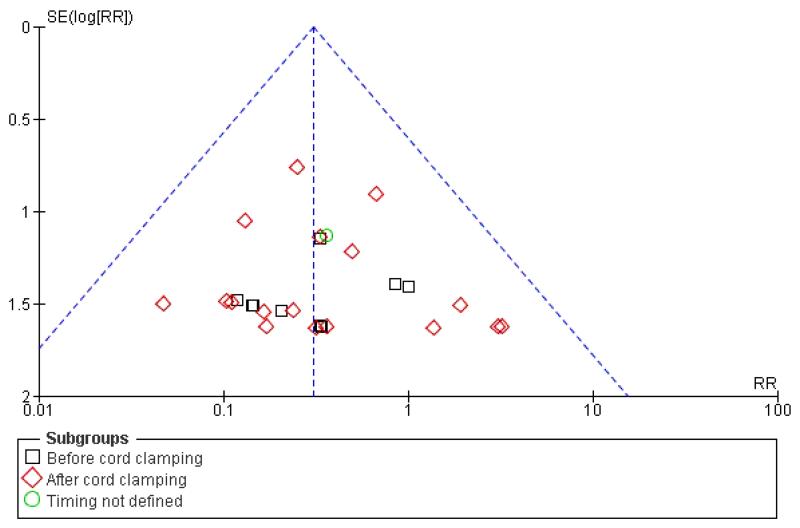
There was a potential for publication bias in the assessment of febrile morbidity as assessed by visual inspection of the funnel plot (Figure 11), while the other primary outcomes appeared to have funnel plot symmetry (Figure 12; Figure 13; Figure 14).
Figure 11. Funnel plot of comparison: 2 Antibiotics versus no antibiotics - by timing of administration, outcome: 2.1 Maternal fever/febrile morbidity.
Figure 12. Funnel plot of comparison: 2 Antibiotics versus no antibiotics - by timing of administration, outcome: 2.2 Maternal wound infection.
Figure 13. Funnel plot of comparison: 2 Antibiotics versus no antibiotics - by timing of administration, outcome: 2.3 Maternal endometritis.
Figure 14. Funnel plot of comparison: 2 Antibiotics versus no antibiotics - by timing of administration, outcome: 2.4 Maternal serious infectious complications.
Other considerations
Infant
Infant outcomes were infrequently reported. No study reported on any long-term adverse effects on the infant or effect of antibiotics on the infant immune system. In addition, no studies reported on the incidence of oral candidiasis (thrush) in babies which we had categorized as an adverse outcome.
Where Apgar scores were reported, there were no differences between the treatment and control groups (Adam 2005; Gordon 1979; Ng 1992; Rouzi 2000). One study collected information on birthweight, number of days in hospital, admission to neonatal intensive care, early neonatal death, respiratory distress syndrome and neonatal sepsis and there was no difference between the treatment and control groups (Rouzi 2000). Some authors stated there were no complications in the babies due to drug administration, without further details (Gordon 1979; Moodley 1981) and that the administration of antibiotics did not interfere with routine paediatric cultures (Gall 1979) or the evaluation of newborn sepsis (Duff 1980).
There were few neonatal deaths and where they were reported, no relationship to the administration of antibiotic was reported (Adam 2005; De Boer 1989).
Only one study reported on infant outcomes at four weeks and in that study the three infants who had complications were all in the control group (Gordon 1979).
Costs
Two studies reported on this outcome, but the data were in a format that we could not include in this review (Kristensen 1990; Mallaret 1990). See Characteristics of included studies table for details of costs.
Resistance
Changes in bacterial flora and the development of antibiotic resistant bacteria with the administration of antibiotics was not systematically collected in the studies included in this review, but several studies included detailed microbiological investigations, comparing the results of aerobic and anaerobic culture of the genital tract before and after the surgery and reporting on antimicrobial resistance in organisms associated with infection (Engel 1984; Fugere 1983; Gibbs 1981; Harger 1981; Ismail 1990; Karhunen 1985; Kreutner 1978; Miller 1968; Moro 1974; Rothbard 1975; Roex 1986; Stiver 1983).
There is a shift in the bacterial flora following the surgical procedure itself and return to the non-pregnant state and even in the control groups more gram positive aerobic organisms (including staphylococcal species and enterococci) were observed post-operatively (Engel 1984). Antibiotic prophylaxis was associated with increases in enterococci and gram-negative aerobic organisms (Engel 1984; Fugere 1983; Gibbs 1981; Kreutner 1978); cefazolin was associated with more anaerobic isolates (Engel 1984; Fugere 1983; Kreutner 1978) and cefoxitin and cefamandole with a decrease in anaerobic isolates (Engel 1984; Gibbs 1981).
Given that most regimens included a cephalosporin which has no activity against enterococci, it is not surprising that most studies reported significant increases in enterococcal colonization (Gibbs 1981; Ismail 1990; Stiver 1983). Harger reported that the isolates from infected sites in cefoxitin infected women showed a relative predominance of enterococci (Harger 1981). Ismail reported that enterococcal sepsis occurred in one patient and three others had significant enterococcal bacteriuria or urinary tract infection (Ismail 1990).
There were very few reports of resistant organisms developing following prophylaxis. No cefoxitin resistant strains of Enterobacteriaceae were isolated from stool samples after prophylaxis (Ismail 1990). In one study, there were more ampicillin resistant urinary tract infections when ampicillin was used for prophylaxis (9/17 versus 8/26) compared with control (Miller 1968). Rothbard reported one infection with an organism resistant to cephalothin and kanamycin used for prophylaxis (Rothbard 1975) and Duff reported an endometrial culture that grew Klebsiella pneumoniae resistant to ampicillin (Duff 1980). Engel reported urinary tract infections with mezlocillin resistant organisms (5/9) after mezlocillin prophylaxis and observed colonization with mezlocillin resistant strains of E. coli in cultures from the cervix (Engel 1984). In one study of cephalothin, all the organisms causing infection in the antibiotic group were described as sensitive to cephalothin in vitro (Moro 1974). In a study of cefoxitin prophylaxis, it was observed that the changes in endogenous flora were not associated with overgrowth of resistant pathogens, such as Pseudomonas, enterococci or Enterobacter (Roex 1986) and Karhunen reported no superinfections with resistant anaerobic organisms when tinidazole was used for prophylaxis (Karhunen 1985). Striver confirmed that there was no increase in nosocomial infection (Stiver 1983).
DISCUSSION
Summary of main result
In the 86 studies included in this review, the use of prophylactic antibiotics in women undergoing cesarean section substantially reduced the incidence of febrile morbidity, wound infection, endometritis, urinary tract infection, and serious infection after cesarean section. Whether considering only elective cesarean sections or non-elective cesarean section, the risk ratios for the effect of antibiotics is remarkably similar for the outcome of endometritis. There is a similar close clustering of risk ratios for the outcome of febrile morbidity between subgroups. Seventy-seven studies reported on the outcome of wound infection. Antibiotic treatment was associated with a statistically significant reduction in wound infection in both the elective and non-elective subgroups.
Using an episode of bacteremia and any other serious infectious morbidity as defined by the authors (except a prolonged febrile episode) as the definition of a serious outcome, antibiotic treatment was associated with a significant reduction for non-elective deliveries. A difference in serious outcomes could not be demonstrated for the elective deliveries. There were no deaths reported in any group.
Data were available on maternal length of stay for 17 studies. Overall, hospital stay was reduced in the antibiotic treated group and was significant in each of the subgroups. Duration of stay in the group receiving treatment ranged from 4.4 to 11.2 days, and for the no treatment group 5.2 to 12.1 days.
Febrile morbidity is common after cesarean section and was reduced with the use of prophylactic antibiotics. Few of these women will have positive bacterial cultures or a specific indication for antimicrobial treatment, but these women often have specimens collected and empiric antibiotic therapy started. This review could not address the costs of antibiotic prophylaxis. However, in those studies that did report the rate of the additional use of antibiotics or costs, or both, there were significant differences with more days of antibiotics being prescribed to the women who had not received prophylaxis. In the two studies that reported post-operative antibiotic costs, costs were lower in the group receiving prophylaxis compared with the control group (Kristensen 1990; Mallaret 1990).
No conclusions can be made from this review about the relative effectiveness of different antibiotic regimens (see review ‘Antibiotic prophylaxis regimens and drugs for cesarean section’ (Hopkins 1999)).
Description of studies
The women included in these trials varied greatly in their risk of infection, ranging from 0% to 61.30% for the outcome of endometritis. Similar wide variability in the incidence of the other outcomes (febrile morbidity, wound infection, urinary tract infection) was seen among the studies.
Because the estimate of the number of women needed to treat to prevent one infection will depend on the baseline risk of infection, fewer women undergoing an emergency section, where the risk of infection is higher, are needed to be treated to prevent an infectious outcome than women undergoing an elective procedure.
Adverse effects
Maternal side effects were not consistently collected nor reported. Overall, there were two episodes in the placebo or untreated group (0.2%) compared with 16 in the treated groups (1.3%) but the differences were not statistically significant. The most common side effect was rash, followed by phlebitis at the site of the intravenous infusion. There were no serious drug-related adverse events reported.
Infant outcomes were rarely systematically collected but when they were reported there was no evidence of any adverse effects associated with the administration of antibiotic. There is evidence that antibiotics given near or shortly after birth can affect the infant gut flora, with the potential to impact mucosal and systemic immune function (Bedford Russell 2006) but no study has prospectively examined the effect of any changes in flora on these or other outcomes. Oral yeast infection (thrush) was not an outcome reported in any of the included studies.
There were changes in bacterial flora with an increase in enterococcal colonization and examples of the development of antibiotic resistant bacteria with the administration of antibiotics, but few incidences where this was associated with infectious complications.
Generally the side effects of a single antibiotic dose are mild, but rarely serious allergic reactions can occur and be fatal. Although the risk of side effects reported in these studies was low, these data were incompletely collected, making it difficult to know accurately the incidence of the adverse effects of treatment. There are also unknown and unquantified effects of antibiotic use that include changing the normal maternal flora, effects on the presentation of infection in the infant, and the development of antimicrobial resistance. There is evidence that the cervicovaginal flora is altered in women undergoing cesarean section, whether antibiotics are used or not, but no problems with managing resistant organisms in this setting have been recognized (Galask 1987).
While increased use of antimicrobial prophylaxis may be one factor in increasing antimicrobial resistance (Shlaes 1997), there are no data supporting the contention that appropriate use of short course antimicrobial prophylaxis will cause significant bacterial resistance nor evidence that a policy of antibiotic prophylaxis for cesarean section has harmful effects that outweigh its benefits, even in those women perceived to be at low risk. Optimizing the choice and the duration of prophylactic antibiotic therapy is recommended as one strategy to prevent antimicrobial resistance (Shlaes 1997). Trends in antibiotic resistance should be monitored, reported and used to establish practice guidelines and monitor institutional policies. Susceptibility testing of significant bacterial isolates should guide antimicrobial therapy of individual women who develop infection despite prophylaxis.
Timing of antibiotic administration
A statistically significant reduction in all the primary outcomes (febrile morbidity, wound infection, endometritis, serious maternal outcomes) was seen whether the antibiotic was administered before the clamping of the cord or after clamping of the cord. There was no significant difference in the estimates for these outcomes by the timing of administration and the confidence intervals were overlapping. It has, however, been shown that the lowest risk of surgical wound infection is associated with antibiotics administered in the pre-operative period as compared with the perioperative or post-operative period (Classen 1992). Although a number of small studies did not show an increase in infectious outcomes when the antibiotic was administered after the cord was clamped (Cunningham 1983; Gordon 1979; Wax 1997), a recent meta-analysis of randomized controlled trials concluded that there was strong evidence that antibiotic prophylaxis given before skin incision decreased the incidence of postpartum endometritis and total infectious morbidities (Costantine 2008). Pre-operative administration of antibiotics did not significantly affect proven neonatal sepsis, suspected sepsis or neonatal intensive care unit admissions. In a retrospective study on the effect of a change in policy to administer prophylactic antibiotics before skin incision, the overall rate of surgical site infections fell from 6.2% to 2.5% (Kaimal 2008).
Quality of the evidence
Overall the methodological quality of the trials on the whole was unclear and there was the potential for publication bias. In only 8% of studies was it judged that the overall risk of bias was low (Bagratee 2001; Bourgeois 1985; Dashow 1986; Levin 1983; Rouzi 2000; Rudd 1981; Tully 1983). Most of the studies were undertaken in the 1970s and 1980s, before the recent understanding of sources of bias in randomised controlled trials and in most studies insufficient information was provided in the paper to adequately judge the risk of bias.
Consistency of the results
The results of the trials included in this review are, however, remarkably consistent, both in direction of effect and in effect size, despite some heterogeneity identified. Overall, the use of prophylactic antibiotics with cesarean section results in a major, clinically important, and statistically significant reduction in the incidence of episodes of febrile morbidity, wound infection, endometritis, urinary tract infection and serious infection after cesarean section.
Only the incidence of urinary tract infection in women undergoing an elective cesarean section was not statistically significant and there were too few serious infectious outcomes in women undergoing an elective cesarean section to analyse.
Agreement and disagreement with other studies or reviews
This review included in its definition of an elective cesarean section those women not in labor but with ruptured membranes for less than six hours, included studies that did not have a placebo arm and included studies that used antibiotic irrigation as well as systemic agents. A meta-analysis (Chelmow 2001) that used an expanded search strategy to identify additional relevant studies, and included only placebo-controlled studies of systemic antibiotics in women undergoing elective cesarean section who were non-laboring with intact membranes, showed a reduction in infections in this low-risk population and supports the conclusion of this review.
Implementation of findings
Inconsistent adherence to policies for administering antibiotic prophylaxis are reported (Huskins 2001; Mah 2001; Pedersen 1996) but simple quality improvement methods have been demonstrated to improve adherence with overall and timely administration of prophylaxis and reduce the infection rate (Weinberg 2001). It was also shown, in this study (Weinberg 2001) that a program that introduced a policy of universal prophylaxis for all women undergoing a cesarean section was more effective than one that required the obstetrician to decide whether a woman was high risk and mandated prophylaxis only for the high-risk women. In a prospective cohort study from a high-risk obstetrical unit in New York state, absence of antibiotic prophylaxis was identified by multiple logistic regression analysis as being independently associated with surgical site infection after cesarean section for both high-risk women and low-risk women and was identified as one of two modifiable factors (the other being fewer prenatal visits) (Killian 2001).
AUTHORS’ CONCLUSIONS
Implications for practice
Prophylactic antibiotics reduced the incidence of endometritis following both elective and non-elective cesarean section by two thirds to three quarters and the incidence of wound infection by up to three quarters. Postpartum febrile morbidity and the incidence of urinary tract infections are also decreased. Fewer serious complications were identified. The administration of prophylactic antibiotics before or after clamping of the cord for women undergoing cesarean section seemed equally effective. However, studies did not assess potential adverse effects on the baby and the rates of oral thrush were not reported. Obstetrical units should collect information on infection rates following cesarean section as an important quality indicator.
Implications for research
Further placebo controlled trials of the effectiveness of antibiotics with cesarean section are not ethically justified, but studies are needed to ascertain infant outcomes. Any future studies should use the list of outcomes identified here as a minimum data set and, in particular, include possible adverse effects on the infant. There should be research on methods to implement effective policies of prophylaxis for women undergoing cesarean section. Rates of infection following cesarean section are higher than for many other surgical procedures, even with a policy of uniform prophylaxis. Future research should look at interventions to reduce further the incidence of infection from that achieved with our current approach to antibiotic prophylaxis, e.g. the topical vaginal administration of metronidazole (Pitt 2001), the timing of antibiotic administration, whether there are advantages to an extended spectrum regimen (Tita 2009) and determine the role of surgical technique, pre- and intra-operative preparation and infection control policies on infection rates.
There is a theoretical opportunity for a cost-effective analysis to be performed in a unit where routine prophylactic antibiotics are not administered to women undergoing an elective cesarean section and where the risk of infection is very low, in an attempt to identify women at increased risk of infection in whom prophylaxis may be cost-effective. However, there is currently no evidence to support such a strategy. Because of local variation in practice and women, the results of such research will likely only be applicable to an individual unit and not generalizable.
There is a need for more information about the role of bacterial vaginosis and infectious complications following cesarean section, the significance of organisms such as Ureaplasma and whether these have implications for current prophylactic recommendations.
Better data on the safety of the intervention for the mother and infant are needed, particularly longer-term effects on the infant. Studies should be undertaken to determine what role antimicrobial prophylactic regimens have in the development of antimicrobial resistance. Research into the perceptions of the advantages and disadvantages of the intervention from the perspective of the woman and the healthcare provider will help define educational and research needs.
PLAIN LANGUAGE SUMMARY.
Routine antibiotics at cesarean section to reduce infection
Women undergoing cesarean section have a five to 20-fold greater chance of getting an infection compared with women who give birth vaginally. These infections can be in the organs within the pelvis, around the surgical incision and sometimes the urine. The infections can be serious, and very occasionally can lead to the mother’s death. The potential benefits of reducing infection for the mother need to be balanced against adverse effects such as nausea, vomiting, skin rash and rarely allergic reactions in the mother, and the risk of thrush and any effect of antibiotics on the ‘friendly’ gut bacteria in the baby. This review looked at whether antibiotics are effective at elective and emergency cesarean sections. It also studied the effect of giving the antibiotics before or after the cord is clamped. The review found 86 studies involving over 13,000 women. Routine use of antibiotics at cesarean section reduced the risk of fever and of wound, womb and urine infections in mothers. It also reduced the risk of serious complications of infections for the mothers. This was so whether the cesarean section was elective or emergency, and whether the antibiotics were given before or after clamping of the umbilical cord. However, none of the studies looked properly at possible adverse effects on the baby, for example, whether its use increased the risk of thrush. Similarly, it was unclear whether the routine use of antibiotics at cesarean section would contribute to increasing drug resistant strains of bacteria. Studies are needed on these two aspects of this intervention.
ACKNOWLEDGEMENTS
Justus Hofmeyr was an author on the previous versions of this review. He helped with writing of the Background section, identifying the studies for inclusion and with the data extraction of the original data. He also provided guidance on the updating of the review. Lei Dou helped with assessing the risk of bias in the studies in the previous version of the review (Smaill 2002).
We wish to thank Kate Barton, Caroline Brooke, Simon Claessens, Kornelia DeKorne, Violeta Dimova-Nikols, Rebecca Gainey, Alison Jenner, Agnieszka Kimball, Ben Lamy, Austin Leirvik, Melissa Slavick, Caroline Summers, Maria Tenorio, Jean Tsang, Kyle Wark and Elizabeth Whiteley for translating articles relevant to this review.
As part of the pre-publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group’s international panel of consumers and the Group’s Statistical Adviser.
Appendix
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | RCT, 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: Sept 2003 - April 2004. | |
| Setting: New Halfa Teaching Hospital, Eastern Sudan. | ||
| Inclusion criteria: planned elective CS (categorized as elective) | ||
| Exclusion criteria: antibiotics within 2 weeks; any visible infection; elevated temperature; allergic to antimicrobials; did not wish to participate | ||
| Interventions | Ceftriaxone 1 g IV at anesthetic induction vs no treatment. | |
| Outcomes | Post-operative febrile morbidity (oral temperature ≥ 38 °C twice at least 4 hours apart after first 24 hours | |
| Post-operative infections (endometritis, wound infection, pelvic abscess, peritonitis, other febrile morbidity (UTI, chest infection, malaria) | ||
| 2 perinatal deaths: 1 in each group due to respiratory distress and septicaemia due to imperforate anus | ||
| Notes | Developing country. | |
| Class of antimicrobial: third generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Patients were randomized.” |
| No additional details. | ||
| Allocation concealment? | Unclear | No information. |
| Blinding? | No | No blinding. |
| All outcomes | Not placebo-controlled. | |
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after randomization. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “The 2 groups were well matched at enrolment and there were no statistical differences in the admission variables.” |
| There was insufficient other information which to judge. | ||
| Overall low risk of bias? | No | Very little information provided, particularly around allocation concealment and it appears not placebo controlled |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: University College Hospital, Ibadan, Nigeria. Majority of patients from low socioeconomic class | ||
| Inclusion criteria: both elective and non-elective cesarean deliveries | ||
| Exclusion criteria: fever or obvious infection before operation | ||
| Interventions | Ampicillin 500 mg before operation and 250 mg 6 hourly for at least 7 days (IM until able to take orally) (N = 58) vs no antibiotics unless temperature 38 degrees C after the third post-operative day (N = 48). Both groups received curative doses of chloroquine | |
| Outcomes | Wound infection; UTI (not defined further); ’genital sepsis’ (not defined further: study group 5/58; control group 15/48) | |
| Notes | Prophylaxis continued for 7 days. | |
| Class of antibiotic: Aminopenicillin (ampicillin). | ||
| Subgroups | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | ‘Divided randomly into 2 groups.’ |
| No additional details. | ||
| Allocation concealment? | Unclear | No information was provided. |
| Blinding? | Unclear | Not placebo-controlled. |
| All outcomes | No additional details. | |
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. |
| All outcomes | No participants excluded; imbalance in group size not accounted for (58 vs 48) | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, parity and indications for CS |
| Overall low risk of bias? | Unclear | Very little information provided to assess risk of bias. |
| Methods | Randomized, placebo controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: August 1970 - January 1971. | |
| Setting: Johns Hopkins University, Baltimore, US; | ||
| Inclusion criteria: women undergoing CS (criteria not specified) | ||
| Exclusion criteria: evidence of clinical infection, history of penicillin allergy | ||
| Interventions | Cephalothin 1 g IV on call to operating room, further 2 g IV intra-operatively and every 6 hours for 48 hours, then 500 mg IM for additional 72 hours (N = 5) vs placebo (N = 7) | |
| Outcomes | Morbidity (temperature > 100.9°F twice, 6 hours apart after first 48 hours or other clinical signs of infection); not separated. For this review, the authors’ definition of morbidity has been classified as fever | |
| Notes | Part ofa larger randomized trial ofprophylactic antibiotics in gynecologic surgery; most patients (87%) were undergoing hysterectomy; only 12/300 patients enrolled underwent CS | |
| Class of antibiotic: first generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomized.” |
| No additional information. | ||
| Allocation concealment? | Yes | Randomized list ofplacebo or drug, kept in hospital pharmacy; code not broken until after patient classified as ‘morbid’ or ‘non-morbid’ |
| Blinding? | Yes | Described as “double-blind”. |
| All outcomes | Placebo-controlled. | |
| Incomplete outcome data addressed? | Yes | No loss to follow up. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | No information was provided. |
| Overall low risk of bias? | Unclear | Insufficient information to judge. |
| Methods | RCT: 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: October 1977 to June 1980. | |
| Setting: College Hospital, New Jersey, October. Women ‘predominantly black (90%) and socio-economically disadvantaged’ | ||
| Inclusion criteria: both elective and non-elective cesarean deliveries | ||
| Exclusion criteria: antibiotics within 2 weeks; pyrexia; any visible infection; penicillin allergy; known medical illness that might cause pyrexia; internal fetal scalp or uterine monitoring | ||
| Interventions | Ticarcillin 6 g IV within 15 minutes of cord clamping (N = 139) vs saline placebo (N = 120). Subset of 22 in each group received ticarcillin 3 g/saline 6-8 hours post-operatively or saline placebo (results similar so authors combined results with single-dose group). | |
| No post-operative antibiotics unless pyrexial > 38 degrees C after day 1 | ||
| Outcomes | Endomyometritis (pyrexia, uterine tenderness and no evidence of other infection) | |
| Notes | Authors’ definition of low and high risk not comparable to definitions for elective/non-elective used in this review | |
| Results for adolescent group (aged 15-18) reported in J Adolescent Health Care 1984;5: 163-166. In that study, incidence of endomyometritis in elective section: 0% for treatment vs 43% for placebo (numbers not given) | ||
| Class of antibiotic: aminopenicillin (ampicillin). | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | ‘Randomly divided into 2 groups.’ |
| Method not described. | ||
| Allocation concealment? | Unclear | No information. |
| Blinding? | Unclear | Placebo controlled (saline solution). |
| All outcomes | Described as “double-blind”, but Insufficient information to judge if there was blinding of study personnel | |
| Incomplete outcome data addressed? | Unclear | No loss of participants to follow up follow up and no participant excluded after analysis, however discrepancy in group numbers (139 vs 120) not accounted for ITT analysis. |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “The prophylaxis and placebo groups were essentially similar in regard to important demographic and obstetric parameters. There were no significant differences between the groups for any of the variables studied”. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Placebo controlled. |
| Methods | Randomized double-blind, placebo controlled; 2 parallel groups | |
| Participants | Dates of data collection: not reported. | |
| Setting: Durban, South Africa. | ||
| Inclusion criteria: women undergoing elective cesarean delivery | ||
| Exclusion: prior antibiotics within 2 weeks, allergy to penicillin or cephalosporin, rupture of membranes | ||
| Interventions | Cefoxitin (2 g IV after cord clamping) (N = 237) vs matching placebo (N = 238) | |
| Outcomes | Febrile morbidity (oral temperature >38°C twice 6 hours apart after first 24 hours) ; wound infection (wound cellulitis, erythema, discharge with or without fever); en-dometritis (fever, uterine tenderness, malodorous lochia); UTI (fever and positive urine culture); pneumonia; duration of hospital stay | |
| Notes | 11% were HIV positive; Staphylococcus aureus most common pathogen (43%) isolated | |
| Class of antibiotic: second generation cephalosporin (cefamycin) | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors‘ judgement | Description |
| Adequate sequence generation? | Yes | “…randomized…a computer-based allocation…” |
| Allocation concealment? | Yes | “…consecutively numbered sealed envelopes…” |
| Blinding? | Yes | Double-blind. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. It appeared to be an ITT analysis |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, parity, gestational age, weight and preoperative haemoglobin. There was insufficient other information which to judge |
| Overall low risk of bias? | Yes | The most important aspects appear to have low risk of bias. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: February to July 1991. | |
| Setting: Sousse Hospital, Tunisia. | ||
| Inclusion criteria: women undergoing elective CS or labor < 12 hours (categorized as ”both“ for this review” | ||
| Exclusion criteria: diagnosed amniotic infection; pyrexia >38°C; antibiotics within 3 days; allergy to beta lactam antibiotics; cardiac disease; diabetes | ||
| Interventions | Cephapirine 1 g IV with induction of anesthesia and 6 hours after operation, gentamycin 80 mg IM with induction, metronidazole 500 mg IV with induction (N = 133), vs no treatment (N = 136) | |
| Outcomes | Endometritis; wound infection; pyrexia only (> 38°C 48 hours after surgery): antibiotic 4/133 vs control 9/136; septicemia (0/133 vs 3/136, included as serious morbidity); duration of hospital stay (antibiotic 5.36 days vs control 6.21, P = 0.03, variance not given) | |
| Notes | Follow up at 30 days (86%). | |
| Translated from French. | ||
| Class of antibiotic: first generation cephalosporin, aminoglycoside and nitroimidazole (metronidazole) | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Allocation “by chance”. |
| Allocation concealment? | Unclear | Using random number table, patients allocated to treatment if the number is even, no treatment if the number is odd |
| Blinding? | No | Not placebo controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No losses or exclusions reported. It appears to be ITT analysis |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The groups were similar for age, parity, duration of labor and other risk factors. There was insufficient other information to judge |
| Overall low risk of bias? | Unclear | Overall unclear. |
| Methods | Quasi-RCT; 5 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Bursa, Turkey.. | ||
| Inclusion criteria: women undergoing CS due to acute fetal distress | ||
| Interventions | Ceftriaxone 1 g (N = 25) vs mezlocillin 2 g (N = 23) vs clindamycin 600 mg and amikacin 500 mg (N = 18) vs sulbactam ampicillin 1 g (N = 25) IV after clamping of the cord vs no treatment (N = 28) | |
| Outcomes | Wound infection (redness, tenderness, pain and purulent discharge); UTI (renal angle tenderness, fever, dysuria and pyuria); endometritis (vaginal spotting, purulent discharge with fever and pain) plus positive cultures | |
| Notes | Treatment groups combined. | |
| All wound infections were positive for coagulase negative staphylococcus | ||
| Class of antibiotic: third generation cephalosporin vs ureidopenicillin (mezlocillin) vs lincosamide (clindamycin) and aminoglycoside | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | No | “…according to the last digital of the patient’s file number…” |
| Allocation concealment? | No | “…according to the last digital of the patient’s file number…” |
| Blinding? | Unclear | Insufficient information provided. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. It appeared to be an ITT analysis |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 5 groups were comparable regarding maternal age, ruptured membranes, pelvic examinations, haemoglobin levels. Insufficient information to judge other aspects |
| Overall low risk of bias? | No | Quasi-RCT means it has high risk of bias. |
| Methods | RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: initiated March 1981. | |
| Setting: Charlottesville, Virginia, USA, almost all were indigent women | ||
| Inclusion criteria: both ‘low risk’ (labor < 6 hours) and ‘high risk’ (> 6 hours) women undergoing CS | ||
| Exclusion criteria: allergy to penicillin or cephalosporin; antibiotic use within 7 days; antibiotics required for other reasons; pyrexia >38° C; foul amniotic fluid. | ||
| Interventions | Irrigation of the uterus and peritoneal cavity with 2 g cefamandole in 1000 ml normal saline (N = 73), vs saline placebo (N = 75) vs no irrigation group (N = 44). As the objective of this review is to compare antibiotic with no antibiotic, rather than the effect of irrigation, only the first 2 groups are compared (double blind comparison) | |
| Outcomes | Metritis (pyrexia >38°C twice 8 hours apart, after 24 hours plus abnormal uterine tenderness, without another apparent source); duration of maternal stay (treatment 5. 29 days vs placebo 6.32 days, variance could not be calculated) | |
| Notes | Authors’ definition of low and high risk do not correspond to those used for elective/ non-elective in this review. | |
| No treated patients developed evidence of drug reaction. | ||
| There were no serious infections (pelvic abscess or phlebitis) in either group | ||
| Class of antibiotic: second generation cephalosporin. | ||
| Subgroup: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | ’A computer generated table of random numbers.” |
| Allocation concealment? | Yes | ”Assigned under the direction of the hospital pharmacy.” |
| Blinding? | Yes | Partially double blind placebo-controlled (3 groups: antibiotic irrigation, saline placebo irrigation, no irrigation). Physicians were unaware ofthe type ofirrigation used |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No loss to follow up reported. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The groups were comparable regarding gra-vidity, parity, maternal weight, hematocrit, etc. There was insufficient other information which to judge |
| Overall low risk of bias? | Yes | Good sequence generation, concealment allocation, blinding and complete outcome data |
| Methods | Randomly allocated (abstract only; no further details). | |
| Participants | Women undergoing high-risk CS (definition not provided; classified as not-defined). | |
| Setting: Texas, USA. | ||
| Interventions | Cefazolin 2 g in 1000 ml irrigation (N = 20) vs normal saline 1000 ml irrigation (N = 20) | |
| Outcomes | Wound infection, endometritis, UTI. | |
| Notes | Follow up 4-6 weeks post-operatively. | |
| Abstract only available. | ||
| Class of antibiotic: first generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | ‘…randomly allocated…’ |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | Normal saline irrigation used in control group; no additional details provided |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No information provided. |
| All outcomes | ||
| Free of selective reporting? | Unclear | No information provided. |
| Free of other bias? | Unclear | No information provided. |
| Overall low risk of bias? | Unclear | Abstract only, not enough information provided. |
| Methods | Randomized, placebo-controlled trial; 4 parallel groups (3 treatment, 1 placebo) | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: October 1986 to February 1987. | |
| Setting: Prince ofWales Hospital, Hong Kong; mostly suburban or rural Chinese women of lower or middle class | ||
| Inclusion criteria: all women undergoing CS. | ||
| Exclusion criteria: receiving antibiotics; pyrexia >37.4°C; diagnosed infection; increased risk of infection, e.g. diabetes; known sensitivity to the antibiotics | ||
| Interventions | IV at time of induction of anesthesia: ampicillin 1 g (N = 96); ampicillin 1 g and metronidazole 500 mg (N = 104); ampicillin 1 g and sulbactam 500 mg (N = 99), vs placebo (normal saline) (N = 101). Results of the 3 treatment groups combined | |
| Outcomes | Febrile morbidity (oral temperature of more than 38°C at least twice after day 1); wound infection (induration, serosanguinous discharge or dehiscence with purulent discharge) ; UTI (positive culture); genital tract infection (pain and uterine tenderness, purulent uterine discharge with microbiological confirmation); any infection anywhere (antibiotic 75/299 vs placebo 28/101); post-operative antibiotic use (22/299 vs 9/101) | |
| Notes | Only moderate or prolonged febrile morbidity (as defined) included | |
| Class of antibiotic: Aminopenicillin (ampicillin), nitroimidazole (metronidazole), beta-lactam/beta-lactamase inhibitor | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “list of random numbers consulted by nurse.” |
| No additional information. | ||
| Allocation concealment? | Unclear | “list of random numbers consulted by nurse.” |
| Blinding? | Yes | Double blind’ randomized trial (the anesthetist was not blind) |
| All outcomes | ||
| Placebo (normal saline). | ||
| “All doctors and nurses looking after the patients were ignorant of the drug given until the end of the study.” | ||
| Incomplete outcome data addressed? | Yes | No loss to follow up |
| All outcomes | No participants excluded | |
| ITT analysis | ||
| Free of selective reporting? | Unclear | Insufficient information to judge |
| Free of other bias? | Unclear | The groups were comparable regarding age, parity, primary CS, indication for CS, urinary catheterization and vaginal examination before operation. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Sequence generation and concealment allocation are unclear. |
| Methods | RCT; 4 parallel groups | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: March to November 1982. | |
| Setting: Naval Hospital, San Diego, California. | ||
| Inclusion criteria: women at increased risk of post-CS endometritis (in labor or with ruptured membranes). Classified as non-elective for this review | ||
| Exclusion criteria: allergy to penicillin or cephalosporins; antibiotic use within 48 hours; separate indication for use of antibiotics; temperature >38 degrees C; chorioamnionitis; pyuria | ||
| Interventions | Administration by irrigation of uterus and peritoneal cavity with 2g cefoxitin in 500ml saline (N = 37), vs 500ml normal saline (N = 23), or IV after clamping of the umbilical cord, cefoxitin 2g (N = 31) vs saline (N = 33). Irrigation and IV groups combined for this review | |
| Outcomes | Endometritis (febrile morbidity and uterine tenderness); total infection-related morbidity (cefoxitin 10/68 vs saline 14/56); fever index; duration of IV antibiotics; additional antibiotics; days in hospital (no difference, variance not given) | |
| Notes | 1 woman developed an allergic reaction to cefoxitin (acute pruritic rash). | |
| There were 2 episodes of bacteraemia (both in placebo groups); there were no episodes of septic pelvic thrombophlebitis nor drainage of pelvic abscess in either group | ||
| Class of antibiotic: second generation cephalosporin (cefamycin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | ”Each patient was designated to receive either normal saline or cefoxitin based on a computer generated table of random numbers“ |
| Allocation to irrigation or IV prophylaxis based on last digit of social security number | ||
| Allocation concealment? | Unclear | No information was provided. |
| Blinding? | Yes | Double blind, placebo controlled. |
| All outcomes | “Both antibiotic and normal saline were packaged identically to ensure that the administration was blinded | |
| Incomplete outcome data addressed? | Unclear | No losses and no exclusions were reported. |
| All outcomes | Imbalance in randomized groups not accounted for (irrigation: cefoxitin 37 vs saline 23; overall 68 vs 56) ITT analysis. | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 4 groups were comparable regarding age, gravidity, parity, duration of pregnancy, socioeconomic status, maternal weight, hours in labor, length of ruptured membranes, and other potential risk factors. Insufficient additional information to judge |
| Overall low risk of bias? | Unclear | Overall insufficient information on which to judge. |
| Methods | Randomized trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Hopital Pellegrin, Bordeaux, France. | ||
| Inclusion criteria: women undergoing CS; both elective and non-elective deliveries | ||
| Exclusion criteria: allergy to beta-lactam antibiotics; pyrexia; indication for antibiotics | ||
| Interventions | Cefotetan 2 g after clamping of umbilical cord (N = 55) vs no antibiotic (N = 55) | |
| Outcomes | Endometritis; urinary infection; local complications (classified as wound infection); fever only (cefotetan 0/55 vs control 6/55); antibiotic therapy (10/55 vs 25/55); mean days in hospital (10.0 vs 10.2, no variance given) | |
| Notes | Translated from French. | |
| Class of antibiotic: second generation cephalosporin (cefamycin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “randomized.” |
| Allocation concealment? | Unclear | Allocated by sealed envelopes. |
| Blinding? | Unclear | Not placebo controlled. No additional information provided. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No losses or exclusions reported: analysis appears to be ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | There were no significant differences between the groups for risk factors for infection. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Overall unclear. |
| Methods | RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not stated. | |
| Setting: Cleveland, Ohio, USA. | ||
| Inclusion criteria: women in labor with ruptured membranes requiring internal monitoring (non-elective delivery) | ||
| Exclusion criteria: evidence of infection; penicillin or cephalosporin allergy | ||
| Interventions | Short course cefazolin (1g IV 6 hourly for 24 hours, N = 24); long course (cefazolin 1g IV for 8 or more doses and cephalexin 500mg orally 6 hourly for 5 days, N = 25); vs no prophylactic antibiotics. Short and long courses combined for this review Administered after umbilical cord clamping. | |
| Outcomes | Endometritis and/or wound infection (antibiotic 12/49 vs control 20/31) | |
| Notes | It was possible to deduce the rate of endometritis alone, but not wound infection, for this review. | |
| 1 late infectious complication (wound dehiscence) in control group | ||
| Drug class: first generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | ‘Randomly assigned’, no details given. |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | No | No blinding of participant or clinician; not placebo controlled |
| All outcomes | Insufficient information to judge whether there was blinding of outcome assessor | |
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after analysis. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | There were no statistical differences among the 3 groups for potential risk factors. |
| There was insufficient other information which to judge | ||
| Overall low risk of bias? | No | Mostly unclear but with no blinding. |
| Methods | Randomized, placebo-controlled trial; 5 parallel groups (4 treatment, 1 control) | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: December 1982 to May 1984. | |
| Setting: Madigan Army Medical Centre, Tacoma, Washington, USA | ||
| Inclusion criteria: all women undergoing CS. | ||
| Exclusion criteria: penicillin or cephalosporin allergy; antibiotic therapy; known infectious process | ||
| Interventions | Irrigation during CS with 2 g of either cephapirin sodium (N = 79), cefamandole nafate (N = 70), moxalactam disodium (N = 64) or ampicillin sodium (N = 70), vs saline (N = 77). A vitamin was added to each solution for disguise. The antibiotic groups have been considered together in this review | |
| Outcomes | Fever (>38°C twice 6 hours apart, excluding the first 24 hours); endomyometritis (pyrexia >37.8°C, uterine tenderness and pelvic peritoneal irritation without other localising signs of irritation; UTI (positive culture); wound infection; fever index; all infection-related morbidity; therapeutic antibiotics; mean post-operative days (variance not given) | |
| Notes | 3 episodes of pelvic thrombophlebitis (all in treated groups). | |
| Results were given for all women and women in labor, both high risk (corresponding to the category of non-elective deliveries) and all labor. The data for elective deliveries were deduced from these | ||
| Class of antibiotic: first generation cephalosporin vs second generation cephalosporin vs carbapenem vs aminopenicillin (ampicillin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated numbers using the mixed congruential method |
| Allocation concealment? | Yes | “The pharmacy to assign each patient to 1 of 5 groups.” |
| Blinding? | Yes | Double blind placebo controlled trial. A vitamin was added to each solution for disguise |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No loss to follow up. |
| All outcomes | No participant excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The mean level of gravidity of the placebo group was higher than that of the cephapirin group. There was insufficient other information which to judge |
| Overall low risk of bias? | Yes | The most important aspects are with low risk of bias. |
| Methods | Randomized, double blind, placebo-controlled; 2 parallel groups | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: December 1983 to June 1985. | |
| Setting: Chogoria Hospital, Kenya. | ||
| Inclusion criteria: all patients undergoing CS. | ||
| Exclusion criteria: clinical infection. | ||
| Interventions | Metronidazole 1 g rectal suppository 10-45 minutes before and 8 hours after procedure (N = 91) vs placebo suppository (N = 91) | |
| Outcomes | Fever (> 37.9°C on at least 1 occasion); wound infection; mean febrile days (0.56 for treatment vs 1.23 for control), hospital days, any antibiotic use (18/91 vs 23/91) | |
| Notes | Elective CS not defined. | |
| No adverse events on mother or babies noted. | ||
| There was 1 grade 3 wound (defined as deep pelvic abscess or evidence of local or generalized peritonitis) in the treatment group as compared with 3 in the placebo group (classified as serious infectious morbidity) | ||
| Class of antibiotic: nitroimidazole (metronidazole). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “…randomized…” |
| Allocation concealment? | Unclear | No information was provided. |
| Blinding? | Yes | Double-blind. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | 7/189 patients initially randomized were not included in analysis because suppositories were incorrectly administered As treated analysis performed. |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, parity, duration of labor, duration ruptured membranes, number of vaginal examinations, etc. There was insufficient other information to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: September 1979 and April 1980. | |
| Setting: Children’s Hospital of Buffalo, USA; | ||
| Inclusion criteria: all women undergoing CS (1 third elective) | ||
| Exclusion: evidence of active infection, penicillin or cephalosporin allergy; recent antibiotic treatment | ||
| Interventions | Cefoxitin 2 g IV (N = 46) vs saline placebo (N = 55) after clamping the umbilical cord and at 4 and 10 hours post-operatively | |
| Outcomes | Febrile morbidity (temperature > 38 °C twice 6 hours apart after first 24 hours); en-dometritis (fever, uterine tenderness, leukocytosis); wound infection (fever, cellulitis, ex-udate); maternal length of stay | |
| Notes | No serious life-threatening infection in either group; no drug-related adverse-effects | |
| Class of antibiotic: second generation cephalosporin (cefamycin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Numbered packages…” “The random code was broken at the end of the study.” No further information provided. |
| Allocation concealment? | Yes | Randomized by pharmacy. |
| Blinding? | Yes | Double-blind, placebo-controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| 9/110 ‘packages’ not included (either damaged or patients failed to meet inclusion criteria) | ||
| imbalance in group size (46-placebo vs 55-cefoxitin) not explained | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, status, race, obesity, obstetric factors and indication for surgery |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: October 1976 and March 1977. | |
| Setting: Walter Reed Army Medical Center, Washington DC. | ||
| Inclusion criteria: all women undergoing either primary or repeat CS (44% elective) | ||
| Exclusion criteria: penicillin allergy; chorioamnionitis prior to surgery | ||
| Interventions | Ampicillin 1 g IV prior to surgery and 6 and 12 hours post-operatively (N = 26) vs placebo (N = 31) | |
| Outcomes | Febrile morbidity (> 100.3 °F twice 6 hours apart after first 24 hours); endomyometri-tis (fever, uterine and abdominal tenderness, purulent lochia); UTI (positive culture); wound infection (induration, erythema and warmth with purulent drainage); need for antibiotics (treatment 3/26 vs placebo 13/31); maternal hospital stay (6.03 vs 6.9; no variance given) | |
| Notes | Class of antibiotic: aminopenicillin (ampicillin). | |
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “In a … randomized manner.” |
| Not further described, prepared by hospital pharmacy. | ||
| Allocation concealment? | Unclear | Prepared by the hospital pharmacy. |
| Blinding? | Yes | Double-blind, placebo controlled. |
| All outcomes | The pharmacist was the only individual with access to the treatment protocol | |
| Incomplete outcome data addressed? | No | No losses to follow up were reported. 23/80 excluded because of errors in dispensation of medication |
| All outcomes | Analysis was not ITT; data from excluded patients could not be re-included | |
| Free of selective reporting? | Unclear | Insuffient information to judge. |
| Free of other bias? | Unclear | “There is a notable difference in the division of repeat sections between groups”. |
| There was insufficient other information which to judge | ||
| Overall low risk of bias? | No | Unclear sequence generation and concealment allocation, along with high exclusions |
| Methods | Randomized placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: January 1970 to June 1980. | |
| Setting: Washington, DC. US. | ||
| Inclusion criteria: women undergoing CS who were not in labor and did not have ruptured membranes (elective) | ||
| Interventions | Ampicillin 1 g 30 min prior to surgery and at 4 and 8 hours post-operatively (N = 42) vs placebo solution (N = 40) | |
| Outcomes | Febrile morbidity (> 100.4 °F twice 6 hours apart after the first 24 hours); endomy-ometritis (fever, uterine and adnexal tenderness, purulent lochia); UTI; wound infection (induration, erythema and warmth with purulent drainage); need for antibiotics (treatment 1/42 vs placebo 6/40); maternal hospital stay (4.3 vs 4.6; no variance given) | |
| Notes | No life-threatening infection related complications nor bacteremic episodes in either group | |
| Class of antibiotic: aminopenicillin (ampicillin). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Randomized. |
| No further information. | ||
| Allocation concealment? | Unclear | No information was provided. |
| Blinding? | Unclear | Described as “double-blind”. Placebo-controlled: “placebo solution”. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No loss to follow up. |
| All outcomes | No participant excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, race, gravidity, parity and socioeconomic status. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 4 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Letterman Army Medical Center, California; Womack Army Community Hospital, North Carolina | ||
| Inclusion criteria: women in active labor or ruptured membranes and at least 1 digital vaginal examination (categorized as non-elective in this review although duration of membrane rupture not stated) | ||
| Exclusion criteria: allergy to penicillin or cephalosporin, fever > 37.7°C with suspicion of chorioamnionitis; antibiotic use within 2 weeks | ||
| Interventions | Cefoxitin 2g IV after clamping the cord, repeated every 6 hours for 48 hours (N = 39) vs uterine and peritoneal lavage with 2 g cefoxitin after delivery of the placenta (N = 42) vs irrigation plus IV therapy (N = 38) vs no therapy (N = 39). The three treatment groups have been combined in this review | |
| Outcomes | Febrile morbidity (> 37.9 °C twice 6 hours apart after first 24 hours); endometritis (fever and uterine tenderness); UTI (positive culture); wound infection (including fever, cellulitis and exudate); hospital stay (treatment 4.86 vs control 5.2; variance could not be calculated) | |
| Notes | 3 episodes of septicemia reported in control group vs none in treatment groups. | |
| No antibiotic reactions reported. | ||
| Class of antibiotic: second generation cephalosporin (cefamycin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “Randomized… using a table of random numbers…” |
| Allocation concealment? | No | “Randomization into 1 of 4 groups was performed by using a table of random numbers,” |
| Blinding? | Unclear | Not placebo-controlled. |
| All outcomes | Clinician was not blinded. | |
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded form the analysis. ITT analysis. | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 4 groups were comparable regarding age, parity, gestational age, rupture of membrane, labor, vaginal examination. Insufficient other information to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: August 1980 - August 1981. | |
| Setting: Nordwest Hospital, Frankfurt, West Germany. | ||
| Inclusion criteria: women undergoing CS. | ||
| Exclusion criteria: severe penicillin allergy, renal insufficiency, antibiotic use, amniotic infection | ||
| Interventions | Mezlocillin 4 g and oxacillin 2 g every 8 hours after clamping of the cord for 3 doses (N = 50) vs no treatment (N = 50) | |
| Outcomes | Endometritis, UTIs, wound infections. | |
| Notes | Detailed pre- and post- antibiotic microbiological cultures were performed; there were fewer gram positive cocci and more gram negative rods in cervical cultures of the treated group; more break-through infections in the treated group were with mezlocillin-resistant organisms | |
| Class of antibiotic: penicillinase-resistant penicillin (oxacillin) and ureidopenicillin (mezlocillin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | ’…a computerised list of randomization… |
| Allocation concealment? | Unclear | ’…a computerised list of randomization… ” |
| No additional information | ||
| Blinding? | No | Control group received no treatment. Single blinded. Women did not know their allocation but clinicians did so this may have introduced bias in assessing some outcomes |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | Although there is no report of losses or exclusions and analysis appears to be ITT, there is insufficient detail to assess this |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “Both groups were statistically homogenous” but there is insufficient other data to assess this |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Double blind, RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Date of data collection: March 1985 - August 1986. | |
| Setting: Mexico. | ||
| Inclusion criteria: women undergoing CS (labor < 12 hours, membrane rupture < 12 hours, < 7 vaginal exams) | ||
| Exclusion: any antibiotic within 2 weeks, fever, clinical evidence of infection | ||
| Interventions | Ampicillin 1 g IV every six hours × 3 then 1 g every 6 hours × 7 days (N = 23) vs ampicillin 1 g every 6 hours × 3 doses then placebo (N = 37) vs placebo (N = 31). Antibiotics administered after surgery, within 2 hours of the procedure | |
| Outcomes | Fever > 38 °C × 2 at least 6 hours apart after first 24 hours; endometritis (temperature > 38 °C, purulent lochia, pain on internal examination); wound infection (increased warmth, size or colour of wound, or purulent secretions); urine infection (dysuria and positive culture) | |
| Notes | Paper was not written in English. | |
| No explanation provided for unequal size groups. | ||
| Class of antibiotic: Aminopenicillin (ampicillin). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “…by computerized tables…” |
| Allocation concealment? | Unclear | Assignment to treatment group was performed using the computer card which is attached to the file |
| No additional information was provided. | ||
| Blinding? | Yes | Double-blind.matching placebo doses. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | 3 were lost to follow up 3 patients excluded for inadequate follow up (group allocation not provided).and no exclusions were reported. The analysis was ITT with the available data |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | No information provided on which to make a judgement. |
| Overall low risk of bias? | No | Allocation concealment is unclear and no explanation provided for unequal size groups and no explanation provided for unequal size groups |
| Methods | Quasi-RCT, 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: Jan 1979 - May 1980. | |
| Setting: Riverside Osteopathic Hospital, Michigan, USA. | ||
| Inclusion criteria: women at high risk (defined as presence of labor) undergoing CS | ||
| Exclusion criteria: oral temperature > 38° C any time prior to surgery; antibiotic use within 2 weeks prior to admission; refusal to participate; repeat elective CS; compelling indication for antibiotics in the judgement of the physician | ||
| Interventions | Either cefazolin (N = 28) 1 G IV within 1 hour prior to surgery, then 5 and 12 hours after operation for total of 3 doses, or carbenicillin (N = 34) 2G IV within 1hr prior to surgery then 6 and 12 hours after operation for a total of 3 doses or no treatment | |
| Outcomes | Febrile morbidity (oral temperature > 38 °C twice at least 6 hours apart after the first 24 hours); wound infection (fever, cellulitis, and/or exudate); endometritis (fever, uterine tenderness and foul discharge, or fever and a positive culture with uterine tenderness and no other apparent cause); UTI (fever, urinary tract symptoms and/or positive culture >100,000 organisms/ml if pre-operative culture negative); pulmonary infection (fever with abnormal chest x-ray and/or physical signs of consolidation); undetermined (persistent fever with no discernible signs of infection) | |
| Notes | Results of 2 antibiotic groups reported together. | |
| Class ofantimicrobial: first generation cephalosporin vs carboxypenicillin (carbenicillin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | No | “By random distribution of the last digit of their hospital number.” |
| Allocation concealment? | No | Allocation based on case record number. |
| Blinding? | No | No blinding. |
| All outcomes | Not placebo controlled. | |
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after randomization. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “Lack of any significant differences between the two groups confirmed adequate randomization.” |
| Insufficient other information to judge. | ||
| Overall low risk of bias? | No | Quasi-RCT give high risk of bias. |
| Methods | Randomized, placebo-controlled trial; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: September 1980 to November 1981. | |
| Setting: Hopital Saint-Luc, Montreal, Canada. | ||
| Inclusion criteria: women undergoing non-elective CS. | ||
| Exclusion criteria: not in labor with intact membranes, allergy to cephalosporins, antibiotic use within 48 hours, fever, ruptured membranes for > 36 hours | ||
| Interventions | Cefoxitin 2 g IV (N = 30) vs cefazolin 1 g IV (N = 30) vs placebo (N = 29) at clamping of the cord and at 6 and 12 hours later. Both treatment groups have been combined | |
| Outcomes | Endometritis, wound infection, UTI (symptoms or two successive positive cultures) septicemia, pelvic abscess, pelvic thrombophlebitis. Follow up at 6 weeks. No side effects observed | |
| Notes | There were no serious infections in any of the groups. | |
| In the placebo and cefazolin groups there was no increase in aerobic bacterial colonization of the cervix after 4 days but there was an increase in colonization by anaerobes; the opposite occurred in the group receiving cefoxitin | ||
| Class of antibiotic: first generation cephalosporin vs second generation cephalosporin (cefamycin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Randomized; method not described. |
| Allocation concealment? | Yes | “A number (1 to 90) identified the boxes. The number was allocated randomly to a box.” |
| An envelope containing the randomization code was available in case of adverse reactions | ||
| Blinding? | Yes | Described as “double blind”. |
| All outcomes | Placebo-controlled: “vitamin solution with a similar colour as the other preparations” | |
| Incomplete outcome data addressed? | Unclear | No loss to follow up. |
| All outcomes | 1 patient in the control group was excluded from analysis as no cultures were performed As treated analysis performed. | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The groups were comparable regarding demographic characters. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT, 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not stated. | |
| Setting: Duke Universtiy Medical Center, North Carolina, USA | ||
| Inclusion criteria: all women undergoing either a repeat CS or in labor | ||
| Exclusion: clinical infection, ruptured membranes for >12 hours, prior antibiotics within 48 hours, renal or hepatic disease | ||
| Interventions | Cefazolin 1 g IM pre-operatively (on call to the operating room) and cephalothin 2 g IV at 6, 12, and 24 hours after first dose (N = 46) vs placebo (N = 49) | |
| Outcomes | Wound infection (cellulitis, purulent exudate, intraperitoneal abscess or peritonitis); endometritis; UTI; maternal hospital stay | |
| Notes | No minor side effects (rash or pruritus) or major reactions (anaphylaxis) observed. | |
| 4 women (all in control group) had septicemia [counted as serious morbidity] | ||
| Class of antimicrobial: first generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomized.” |
| Method not described. | ||
| Allocation concealment? | Unclear | No information was provided. |
| Blinding? | Yes | Described as “double-blind”. |
| All outcomes | Placebo controlled. | |
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after randomization. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, racial distribution, parity, number of catheterizations or length of time of indwelling catheter. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, placebo controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Date of data collection: November 1983 and December 1984. | |
| Setting: University Hospital, New Jersey; ; lower socioeconomic class (90% black) | ||
| Inclusion criteria: women < 21 years old undergoing CS. | ||
| Exclusion: antibiotic use within 2 weeks; active infection or fever at delivery; penicillin or sulfa allergy; internal fetal monitoring | ||
| Interventions | Trimethoprim 240 mg and sulfamethoxazole 1200 mg IV after clamping of cord (N = 29) vs placebo (N = 28) | |
| Outcomes | Endomyometritis (fever [> 100.3°F twice within 24 hours after first day], uterine tenderness, absence of another focus); UTI (fever and positive culture); wound infection (fever, abnormal appearing wound with cellulitis or a wound draining purulent material) | |
| Notes | Authors’ definition of high risk not comparable with that used in this review. | |
| The incidence of UTI and wound infection was similar between the groups (numbers not given) | ||
| Class of antibiotic: sulfonamide/trimethoprim. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | ‘Randomly divided.’ |
| No further details provided. | ||
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | Placebo-controlled. |
| All outcomes | No further information. | |
| Incomplete outcome data addressed? | Yes | No loss to follow up reported. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, gravidity, vaginal examinations, duration of labor and duration of rupture of membranes, elective repeat CS. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: August 1979 and April 1980. | |
| Setting: Universitats-Frauenklinik Wien, Austria. | ||
| Inclusion criteria: women undergoing CS. | ||
| Interventions | IV metronidazole 500 mg before induction of anesthesia and 12 and 24 hours post-operatively, then rectal suppository × 4 days (N = 53) vs no treatment (N = 50) | |
| Outcomes | Fever (> 38°C on 2 subsequent days); wound infection; endometritis; additional use of antibiotics (treatment 13/53 vs control 22/50); maternal hospital days | |
| Notes | Full translation pending. | |
| Class of antibiotic: Nitroimidazole (metronidazole). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “…randomized…’ (no further details provided in translation) |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | Not placebo-controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. It appears to be an ITT analysis |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | Insufficient information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Random allocation is presumed although method not described. | |
| Participants | Dates of data collection: November 1971 and April 1972. | |
| Setting: University of Pennsylvania. | ||
| Inclusion criteria: women undergoing primary CS or repeat section | ||
| Exclusion criteria: penicillin allergy, fever in labor. | ||
| Interventions | Ampicillin 1 g, methicillin 1 g and kanamycin 0.5 g IM 15-30 minutes before, and at 2 and 8 hours after delivery (N = 33) vs placebo (N = 28) | |
| Outcomes | Endometritis (fever and uterine tenderness or fever and pathogenic organism without other cause); UTI; wound infection (fever, cellulitis and exudate); morbidity [fever > 100 °F in 2 separate 24 hour periods after first postpartum day or positive post-operative urine culture of > 100,000 colonies/ml] (treatment 9/33 vs placebo 17/28); UTI (fever and urinary tract symptoms or a single significant culture with or without fever); maternal hospital stay (6.5 vs 6.9 days; no variance given) | |
| Notes | 2 serious infections: 1 pelvic abscess in treatment group, 1 septicemia in placebo group. | |
| Authors’ definitions of repeat and primary section not consistent with those used for elective/non-elective in this review | ||
| Class of antibiotic: aminopenicillin (ampicillin), penicillinase-resistant penicillin (me- thicillin), aminoglycoside | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “…the patient randomization.” |
| Random allocation is presumed although method not described. | ||
| Allocation concealment? | Unclear | Insufficient details provided. |
| Blinding? | Yes | Placebo-controlled; study described as double-blind. |
| All outcomes | “The materials were prepared by the pharmacy service in coded identical vials, containing identically appearing solutions.” No specific statement to confirm adequate blinding of study personnel | |
| Incomplete outcome data addressed? | No | No loss of participants to follow up. |
| All outcomes | 17 patients “were eliminated from the study, 6 for errors in giving the study medications, 5 for penicillin allergies, 3 for fever in labor, 2 for being started on ampicillin prophylaxis, and 1 for cesarean hysterectomy” | |
| Analysis done on included patients; no data available to incorporate data on patients eliminated | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “The patient randomization is statistically acceptable.” |
| Insufficient other information to judge. | ||
| Overall low risk of bias? | No | There is uncertainty around the sequence generation ad concealment allocation, and the high loss of data (17/61 = 28%) would suggest high risk of bias |
| Methods | Random allocation is presumed although method not described. | |
| Participants | Dates of data collection: August 1972 to February 1973. | |
| Setting: University of Pennsylvania. | ||
| Inclusion criteria: women undergoing CS. | ||
| Exclusion criteria: penicillin allergy, fever in labor. | ||
| Interventions | Ampicillin 1 g and kanamycin 0.5 g IM 15 to 30 minutes before, and at 2 and 8 hours after delivery (N = 34) vs placebo (N = 34) | |
| Outcomes | Endometritis (fever and uterine tenderness or fever and pathogenic organism without other cause); UTI; wound infection (fever, cellulitis and exudate; any grade); morbidity [fever > 100°F in two separate 24 hour periods after first postpartum day or positive post-operative urine culture of > 100,000 colonies/ml] (treatment 8/34 vs placebo 22/34) | |
| Notes | 1 pelvic abscess in placebo group. | |
| Authors’ definitions of repeat and primary section not comparable to those used for elective/non-elective in this review, categorized as ‘both’ | ||
| Class of antibiotic: aminopenicillin (ampicillin), aminoglycoside | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomization of patients is acceptable.” |
| Random allocation of patients is assumed but method not described | ||
| Allocation concealment? | Unclear | Insufficient details provided. |
| Blinding? | Yes | Placebo-controlled; study described as double-blind. |
| All outcomes | “The materials were prepared by the pharmacy service in coded identical vials, containing identically appearing solutions.” No specific statement to confirm adequate blinding of study personnel | |
| Incomplete outcome data addressed? | No | “25 patients were eliminated because of penicillin allergy, fever in labor, errors in giving the medication, etc. None was used as a control.” |
| All outcomes | An ITT analysis was not performed and the data cannot be re-included | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “Randomization of patients is acceptable”. |
| The groups were comparable regarding age, rupture of membranes, indication for CS and anemia | ||
| Insufficient other information to judge. | ||
| Overall low risk of bias? | No | There is uncertainty around the sequence generation ad concealment allocation, and the high loss of data (25/68 = 37%) would suggest high risk of bias |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: October 1978 and July 1979. | |
| Setting: Robert B Green Memorial Hospital, Texas, US; patients indigent and predominantly Mexican-American | ||
| Inclusion criteria: women in labor with rupture of membranes (non-elective) | ||
| Exclusion criteria: infection, antibiotics within prior 3 days, allergy to penicillin or cephalosporin; no consent | ||
| Interventions | Cefamandole 2 g IV after cord clamping, and at 4 and 8 hours post-operatively (N = 50) vs identical appearing placebo (N = 50) | |
| Outcomes | Endomyo(para)metritis; wound infection; maternal hospital stay; records reviewed 6 weeks to 6 months after discharge. 4 episodes of bacteremia (1 in treatment group, 3 in placebo) have been categorized as serious outcomes | |
| Notes | No incidence of pelvic abscess or septic thrombophlebitis in either group. | |
| Increase in Enterobacteriacae and enterococci and decrease in gram positive anaerobes and nonpathogens in prophylactic group. | ||
| No adverse clinical or laboratory results attributable to treatment | ||
| Class of antibiotic: second generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomized.” |
| No further information. | ||
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Double-blind, identical-appearing placebo. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses to follow up. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, parity, race, gestational age, weight, indications for CS, anesthesia, etc. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT, 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of collection: enrolment started November 1976. | |
| Setting: San Bernadino county and University of California at Los Angeles Medical Centers; primarily indigent cases | ||
| Inclusion criteria: women undergoing CS. | ||
| Exclusion: emergency section, penicillin allergy, fever > 38 degrees C, on antibiotics; declined to participate | ||
| Interventions | Ampicillin 1 g IV 15-30 minutes before surgery and at 2 and 8 hours post-operatively (N = 38) vs ampicillin 1 g IV immediately after cord clamping and at 2 and 8 hours post-operatively (N = 40) vs no antibiotic (N = 36). Outcomes of both treatment groups combined | |
| Outcomes | Endometritis; wound infection; UTI; maternal hospital stay (5.1 and 4.7 for pre- and post-administration of antibiotics respectively vs 6.0 for no treatment, variance not given) | |
| Notes | Although emergency CSs were excluded, the women enrolled did not conform to our definition of an elective section. | |
| Information on neonatal morbidity collected; there were 2 infants with definite infections in mothers who received no antibiotics and 1 infection in an infant where antibiotics were given after cord clamping | ||
| Class of antibiotic: aminopenicillin (ampicillin). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “at random.” |
| Method not described. | ||
| Allocation concealment? | Unclear | No information. |
| Blinding? | No | No blinding “…because of the different modes of administering the antibiotics, a double-blind study was not possible” Not placebo controlled. |
| All outcomes | ||
| “The investigator was not intimately involved with the post-operative care … and the pediatricians did not know into which group the mothers had been placed.” | ||
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after randomization. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | Insufficient information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | ‘Randomly divided’ (no details provided); placebo-controlled | |
| Participants | Dates of data collection: December 1981 to August 1982. | |
| Setting: School of Midwifery, Helsinki, Finland. | ||
| Inclusion criteria: women undergoing CS; elective CSs not included but definition not provided | ||
| Exclusion: antibiotics prior to procedure. | ||
| Interventions | Metronidazole 500 mg IV after cutting of cord (N = 109) vs placebo (N = 110) | |
| Outcomes | Wound infection, endometritis, sepsis (temperature > 38.5°C and bacteremia). | |
| Notes | Translated from German. | |
| Class of antibiotic: nitroimidazole (metronidazole). | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomly” divided into 2 groups. |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | No details provided. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No losses or exclusions reported; it appears the analysis was ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The groups were comparable in respect of social status, age, parity, duration of pregnancy, primary section/repeat section, axillary temperature before the procedure, localization of skin incision, number of am-nioscopes. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Overall unclear. |
| Methods | Randomized, placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Central Baptist Hospital, Lexington, Kentucky, US. | ||
| Inclusion criteria: women undergoing primary, non-elective CS (while it appears most women were in labor and/or had ruptured membranes it is unclear whether all patients fulfilled our criteria for non-elective) | ||
| Exclusion: antibiotic use within 7 days, penicillin or cephalosporin allergy | ||
| Interventions | Cefamandole 500 mg IV immediately after the cord was clamped, again in the recovery room and two more doses 6 hours apart (N = 43) vs identical-appearing placebo (N = 47) | |
| Outcomes | Infectious morbidity (fever > 100.3°F twice 6 hours apart after first 24 hours); endomy-ometritis (fever, uterine tenderness, and positive culture from endometrium); wound infection, UTI; maternal duration of stay (treatment 5.1 days vs placebo 5.4; not significant, no variance given) | |
| Notes | There was 1 episode of bacteremia in the control group. | |
| Class of antibiotic: second generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Randomized. No further information. |
| Allocation concealment? | Yes | “according to pre-numbered envelopes maintained in the central pharmacy.” |
| Blinding? | Yes | Described as “double-blind”. |
| All outcomes | Placebo-controlled: “identical appearing, equal volume solution” | |
| Incomplete outcome data addressed? | Yes | No loss to follow up. |
| All outcomes | No participant excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, race, parity, weight, type of anesthesia, operating time or pre-operative hematocrit. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, placebo controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collections: July 1983 and December 1986. | |
| Setting: University Hospital, Lund, Sweden. | ||
| Inclusion criteria: women undergoing emergency CS (during labor and/or after rupture of membranes [duration not specified]); categorized as “both” for this review | ||
| Exclusion criteria: fever > 38°C, given antibiotics, chemotherapy or immunosuppressive therapy in prior 3 weeks, allergy to cephalosporins, alcohol or drug abuse, chronic disease of cardiovascular, renal, hepatic or gastrointestinal system, severe anemia | ||
| Interventions | Cefuroxime 1.5 g IV at the start of the operation and 12 hours later (N = 80) vs saline placebo (N = 80) | |
| Outcomes | Endometritis (fever > 38°C twice at least 1 hour apart, after the first post-operative day, and increased tenderness of the uterus); wound infection (redness, tenderness, increased heat and edema of wound); UTI | |
| Notes | There were no cases of septicemia or abscess formation observed in either group. | |
| Only 55% of women had ruptured membranes (number > 6 hours not stated) and 77% were in labor; these definitions do not meet our criteria for non-elective section, categorized as ‘both’ | ||
| Class of antibiotic: second generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “…a pre-set randomized series in a double-blind manner…” |
| Allocation concealment? | Unclear | “…a pre-set randomized series in a double-blind manner…” |
| Blinding? | Yes | Described as “double-blind”. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. It appears to be an ITT analysis |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, parity, previous CS, complications during pregnancy and gestational age at the operation. There is Insufficient information to judge overall |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not stated. | |
| Setting: Pittsburgh, Pennsylvania, US. | ||
| Inclusion criteria: women undergoing CS after labor or rupture of membranes (method section unclear as to duration of ruptured membranes; it has been assumed that all women were in labor) | ||
| Exclusion criteria: elective CS without labor; already receiving antibiotics; fever or other evidence of infection; allergy to penicillin or cephalosporins; requiring endocarditis prophylaxis | ||
| Interventions | Cefoxitin 2 g IV after cord clamping, and at 6 and 12 hours after initial dose (N = 196) vs matching mannitol and riboflavin placebo (N = 196) | |
| Outcomes | Febrile morbidity (fever > 37.9°C twice at least 4 hours apart after first post-operative day); endomyometritis (fever > 38°C with uterine tenderness, maternal white blood cell count > 15000/cu mm, malodorous lochia and no apparent cause for fever); UTI; incision infection (purulent drainage with induration and tenderness); additional antibiotic therapy (treatment 26/196 vs placebo 68/190) | |
| Notes | Increase in enterococci and decrease in Staphylococcus aureus, various streptococci, E. coli and a variety of anaerobes from infected sites in prophylactic group compared with placebo | |
| Class of antibiotics: second generation cephalosporin (cefamycin) | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomized.” |
| No further information. | ||
| Allocation concealment? | Yes | “The hospital pharmacy prepared coded vials.” |
| Blinding? | Yes | Double-blind, identical appearing placebo. |
| All outcomes | ||
| Incomplete outcome data addressed? | No | Insufficient information to judge. |
| All outcomes | ||
| Free of selective reporting? | Unclear | No loss to follow up reported. 14/400 women initially randomized not included in final analysis (errors in protocol, 2 allergic to penicillin after first dose given and 2, who received cefoxitin, for infusion-related reactions); insufficient data provided to perform ITT analysis |
| Free of other bias? | Unclear | The 2 groups were comparable regarding demographic and obstetric variables and indications for CS. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: July 1980 to June 1981. | |
| Setting: Mount Sinai Hospital, Toronto, Canada. | ||
| Inclusion criteria: women undergoing CS (at ‘high’ risk because of ruptured membranes in active labor); classified as ‘non-elective’ | ||
| Exclusion criteria: febrile, antibiotic use in prior 24 hours; allergy to penicillin or cephalosporin; significant hepatic or renal disease | ||
| Predominantly private, middle-class and in their late 20s. | ||
| Interventions | Cefoxitin 2 g IV at time of cord clamping (N = 64) vs cefoxitin 2 g at time of cord clamping and at 4 and 8 hours post-operatively (N = 60) vs identical-appearing placebo; both treatment groups combined in this analysis | |
| Outcomes | Febrile morbidity (> 38°C twice at least 8 hours apart, after first post-operative day); endometritis (fever, foul, excessive lochia or uterine tenderness); UTI (fever and positive culture); wound infection (fever, cellulitis or exudate with positive cultures) | |
| Notes | No adverse drug reactions in cefoxitin groups, no septicemia in any group; 4 patients in placebo group were considered seriously ill (although do not fit the criteria for serious morbidity in this review) compared to none in treatment groups | |
| Antibiotic class: Second generation cephalosporin (cefamycin) | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “…randomized.” |
| Method not described. | ||
| Allocation concealment? | Yes | “…randomly packaged in identical vials coded from 1 to 200.” |
| Blinding? | Yes | “…double-blinded, placebo-controlled.” “The medication and an identical appearing placebo were prepared prior to the study and … packaged in identical vials….The attending physician was unaware of what regimen his patient received and the code numbers were revealed only after the study was completed.” |
| All outcomes | ||
| Incomplete outcome data addressed? | No | No loss of participants to follow up. |
| All outcomes | 7 patients were excluded after having entered the study. 1 patient was excluded because of an error in mixing and administering the IV injections; 6 patients were excluded because they became febrile within 8 hours of operation and required immediate antibiotic therapy Not ITT analysis. Data from excluded patients could not be re-included in the analysis | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 3 groups were comparable regarding age, parity, gestational age, duration of labor, duration of ruptured membranes, number of vaginal examinations, use of internal fetal monitoring or post-operative haemoglobin.There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Quasi-RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: September 1994 - April 1995 | |
| Setting: University Hospital, Kuala Lumpur, Malaysia. | ||
| Inclusion criteria: elective CS. | ||
| Exclusion criteria: allergic to penicillin, evidence of infection, premature rupture of membranes, receiving antibiotics prior to CS | ||
| Interventions | Augmentin (amoxicillin-clavulanic acid)1.2G IV either at the time general anesthesia was induced or after epidural block vs no treatment | |
| Outcomes | Febrile morbidity (fever > 38°C twice at least 4 hrs apart after the first 24 hrs); wound sepsis (defined and graded as a) erythema and/or induration, b) serous oozing, c) presence of pus, d) wound dehiscence); UTI (routine midstream urine on 3rd post-operative day > 100,000 organisms/ml); endometritis (fever, uterine tenderness and foul smelling lochia) ; pneumonia (cough, fever and/or radiographic evidence of pulmonary consolidation) | |
| Notes | Class of antibiotic: beta-lactam/beta-lactamase inhibitor combination | |
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | No | “Alternately allocated to either antibiotic group or control group.” |
| Allocation concealment? | No | Allocation based on alternate number. |
| Blinding? | No | No blinding. |
| All outcomes | Not placebo controlled. | |
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after analysis. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “Both the study groups and control group were comparable in terms of patient characteristics and operative variables.” Insufficient other information to judge. |
| Overall low risk of bias? | No | Quasi-RCT and no blinding means that there is high risk of bias |
| Methods | Double-blind, randomized, placebo-controlled; 2 parallel groups | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: University of Illinois College of Medicine, Chicago, US (large, inner city hospital); majority of subjects black (40%) or Hispanic (60%) | ||
| Inclusion criteria: undergoing CS. | ||
| Exclusion: preoperative fever, antibiotics within 1 week, membranes ruptured >36 hours, evidence of chorioamnionitis, penicillin or cephalosporin allergy | ||
| Interventions | Cefoxitin 2 g after cord clamped and at 4 and 8 hours (N = 74) vs placebo (N = 78) | |
| Outcomes | Endometritis (fever and uterine tenderness or fever and pathologic organism without other focus); wound infection (fever, cellulitis and exudate); UTI (fever and symptoms or positive culture) | |
| Notes | In the placebo group there were 8 episodes of serious morbidity (6 cases of sepsis; 1 pelvic abscess; 1 episode of pelvic thrombophlebitis) compared with 1 in the treated group (1 episode of sepsis). | |
| Routine post-operative cultures were performed: enterococci were isolated from 30/68 cases who received cefoxitin vs 15/74 who received placebo; there was no change in the rate of cefoxitin resistance in Enterobacteriaceae from the stool after prophylaxis | ||
| Class of antibiotic: second generation cephalosporin (cefamycin) | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “… randomized…” |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Double-blind. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. The analysis appeared to be ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | Insufficient information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT, 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: March - October 1982. | |
| Setting: A Meir General Hospitla, Kfar Sava, Israel. | ||
| Inclusion criteria: patients undergoing CS, classified as “no-labor” if cesarean was performed before onset of labor and “labor” if occurred after onset of labor | ||
| Exclusion criteria: evidence of infection, known allergy to penicillin, antibiotic therapy during the previous 2 weeks | ||
| Interventions | Mezlocillin 2 g IV 30 minutes before surgery, then 4 and 9 hours after surgery vs placebo IV 30 minutes before surgery, then 4 and 9 hours after surgery | |
| Outcomes | Febrile morbidity (2 oral temperatures > 38°C at least 4 hours apart after the first 24 hours); endometritis (fever and uterine tenderness with or without a positive lochial culture and no other apparent cause of fever); UTI (> 105 colonies/ml after a negative pre-operative culture); wound infection (fever, cellulitis, exudate and tenderness) | |
| Notes | Class of antibiotic: ureidopenicillin (mezlocillin). | |
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Patients were randomly assigned.” |
| Method not described. | ||
| Allocation concealment? | Unclear | No information. |
| Blinding? | Unclear | Placebo controlled. |
| All outcomes | Insufficient information to judge whether there was blinding of study personnel | |
| Incomplete outcome data addressed? | Unclear | 7 patients were excluded for errors in following the protocol |
| All outcomes | ||
| Excluded patients not included in analysis; data cannot be imputed | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “The groups did not differ significantly in obstetrical variables…indications for CS were similar in both groups.” Insufficient other information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized placebo-controlled trial: 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not stated. | |
| Setting: Kfar-Sava, Israel. | ||
| Inclusion criteria: women undergoing CS. | ||
| Exclusion: women with active infection, allergy to penicillin and antibiotic treatment within 2 weeks | ||
| Interventions | Mezlocillin 5 g IV during 30 minutes prior to surgery (N = 38) vs placebo (N = 40) | |
| Outcomes | Febrile morbidity (> 38°C twice at least 4 hours apart after first 24 hours post-operative) ; endometritis (fever and uterine tenderness); UTI (single culture of > 100,000 bacteria/ml); wound infection (redness, cellulitis, tenderness and exudate from incision) | |
| Notes | Authors’ definition of emergency not consistent with definitions used in this review (classified as ‘both/undefined’) | |
| Class of antibiotic: ureidopenicillin (mezlocillin). | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “…randomly assigned…” (method not stated). |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | Placebo was used in the control group but no details provided |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | It is unclear whether all patients randomized were included in the analysis but no losses or exclusions were reported. It appeared to be an ITT analysis |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, parity, rupture of membranes, duration of ruptured membranes, number of vaginal examinations, duration of anesthesia, and indications for CS. There is Insufficient information to judge overall |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection; not reported. | |
| Setting: Rambam Medical Center, Haifa, Israel. | ||
| Inclusion criteria: low risk women requiring cesarean delivery (elective procedure, duration of membrane rupture < 3 hours, no more than 2 vaginal examinations) | ||
| Exclusion: required a drug other than cefazolin for prophylaxis, fever, membrane rupture > 24 hours | ||
| Interventions | Cefazolin 1 g after clamping of the cord (N = 167) vs no treatment (N = 140) | |
| Outcomes | Febrile morbidity (fever > 37.7°C twice at least 4 hours apart after first 24 hours); endometritis (fever, uterine tenderness and abnormal lochia); UTI (fever and positive culture); wound infection (fever, cellulitis or exudate with positive culture); therapeutic antibiotic use (treatment group 6.5% vs 20% in control group, P < 0.001) | |
| Notes | Although some women were in labor at the time of the procedure (mean duration of labor 53 and 44 minutes in the 2 groups), the study population so closely resembles the criteria for elective CS used in this review that the results have been included in the ‘elective’ category | |
| Class of antibiotic: first generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Randomized by computer program to 1 of 2 groups at time of their first antenatal visit |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | Not placebo-controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No losses to follow up. |
| All outcomes | No participant excluded. | |
| Imbalance in group size not accounted for (likely because randomization occurred at first antenatal visit and not all patients randomized were enrolled) | ||
| ITT analysis performed. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The groups were comparable regarding socioeconomic level, weight, gestational age, post-operative haemoglobin and operation time. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: May 1982-August 1983. | |
| Setting: South Saimaa Central Hospital, Lappeenranta, Finland | ||
| Inclusion criteria: initially all women undergoing CS (N = 80); thereafter women undergoing non-elective (ruptured membranes) section (N = 72) | ||
| Interventions | Tinidazole 500 mg IV at cord clamping (N = 75) vs identical placebo (N = 77) | |
| Outcomes | Febrile morbidity (> 38°C on 2 post-operative days, excluding the first); endometritis (fever, foul lochia or uterine tenderness); wound infection (fever, cellulitis or exudate); UTI (fever and positive culture) | |
| Notes | Authors’ definition of non-elective (ruptured membranes) and elective (unruptured membranes) not consistent with the definitions used in this review; classified in this review as ‘both’. | |
| Newborn infants observed for effects of tinidazole (although data not given) | ||
| Class of antibiotic: nitroimidazole (tinidazole). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | ‘Randomized according to a code.’ |
| Allocation concealment? | Yes | “Identical vials … coded from 1 to 160.” |
| Blinding? | Yes | Placebo-controlled, double blind. |
| All outcomes | “The code was first opened when the study was completed.” | |
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. |
| All outcomes | 8 women excluded: 4 because they were febrile before the operation, 4 because of mistakes in administration; data not provided to perform ITT analysis | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, weight, gestational age, etc. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: September 1982-September 1983. | |
| Setting: University of Mississippi Medical Center, | ||
| Inclusion criteria: women undergoing non-elective CS (including prolonged ruptured membranes and prolonged labor, as well as general risk factors such as poor nutrition and poverty) | ||
| Exclusion: current antibiotics, known infectious process, allergy to cephalosporins | ||
| Interventions | Cefamandole 2 g in 800 ml saline irrigation during the procedure (N = 84) vs saline irrigation (N = 86) vs no treatment (N = 92) | |
| As the objective of this review is to compare antibiotic with no antibiotic, rather than the effect of irrigation, the 2 irrigation groups are compared | ||
| Outcomes | Febrile morbidity (> 100.6°F twice 6 hours apart after first post-operative day); serious morbidity (fever and endomyometritis or abscess requiring IV antibiotics for resolution) | |
| Notes | Authors’ definition of high risk does not correspond to that used for non-elective in this review, classified as ‘both’. | |
| The outcome of serious morbidity included endomyometritis and is classified as endometritis in this review | ||
| Class of antibiotic: second generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | No | Randomized by last digit ofhospital admission number to no irrigation, antibiotic irrigation or saline irrigation |
| Allocation concealment? | No | No additional information provided. |
| Blinding? | Unclear | Placebo-controlled (normal saline irrigation). |
| All outcomes | No further information provided. | |
| Incomplete outcome data addressed? | No | No loss to follow up or exclusion ofpartici-pants reported, but follow up given for only 77/84 of treatment and 53/86 of placebo group for outcome of serious infection, without explanation |
| All outcomes | ||
| No evidence ITT analysis was performed. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 3 groups were comparable regarding operative indicators, duration of labor, etc. |
| There was insufficient other information which to judge | ||
| Overall low risk of bias? | No | Quasi-RCT gives high risk of bias. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: January 1996 - December 1997. | |
| Setting:Technical University of Munich. Munich, Germany. | ||
| Inclusion criteria: elective CS. | ||
| Exclusion criteria: evidence ofpre-existing infections, labor, rupture ofmembranes, oral temperature > 37.5°C, antibiotic therapy within 72 hr or surgery, immune deficiency, known allergic reaction to cephalosporins, age <18 years | ||
| Interventions | 2 g cefotiam IV intraoperative vs no treatment. | |
| Outcomes | Febrile morbidity (oral temperature of > 38°C twice on at lease 2 occasions 24 h apart or > 38.5°C on 1 occasion after the first 24 hours); wound infection (purulent material at site of incision), endometritis (fever, uterine tenderness and offensive lochia), UTI (> 100,000 bacteria/ml of midstream urine in patients with symptoms (urgency, dysuria, frequency) | |
| Notes | Drug class: third generation cephalosporin. | |
| Unable to confirm whether drug given after clamping of cord. | ||
| Class of antibiotic: second generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “according to a computer generated random assignment.” |
| Allocation concealment? | Unclear | Insufficient information to judge. |
| Blinding? | No | No blinding. |
| All outcomes | Not placebo controlled. | |
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after randomization. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “No significant difference was detected between the 2 groups for age, gestational age, health insurance status, body mass index, kind of anesthesia, duration of surgery, or additional pregnancy risk factors.” Insufficient other information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: November 1975-June 1976. | |
| Setting: Medical University Hospital of South Carolina; | ||
| Inclusion criteria: all women undergoing CS (51/97 not in labor; 61/97 without ruptured membranes) | ||
| Exclusion criteria: signs of infection, allergy to penicillin or cephalosporin, antibiotics within 2 weeks; lack of consent | ||
| Interventions | Cefazolin 1 g IV pre-operatively and at 2 and 8 hours post-operatively (N = 48) vs similar volume of placebo (N = 49) | |
| Outcomes | Febrile morbidity (> 100.3oF twice on any of first 10 postpartum days after the first) ; endometritis (fever and uterine tenderness, or fever and pathogen from endometrium without other cause); UTI (fever or positive culture and symptoms); wound infection (fever, cellulitis and/or exudate) | |
| Notes | Aerobic isolates unchanged, fewer anaerobes in patients given placebo; most pathogens isolated were resistant to cefazolin whether treatment or placebo given. | |
| There were 2 episodes of septicemia (both in placebo group). | ||
| Class of antibiotic: first generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | ‘Random allocation.’ |
| No additional information. | ||
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | “A similar volume of placebo” was administered to the control group |
| All outcomes | No additional information. | |
| Incomplete outcome data addressed? | No | No loss to follow up reported. |
| All outcomes | 6 women initially randomized not included in analysis (non-adherence or noninfec-tious complications) | |
| ITT analysis not performed; could not re-include data. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding race, age and type of CS. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection:February 1987-March 1988. | |
| Setting: Odense University Hospital, Denmark. | ||
| Inclusion criteria: women undergoing non-elective CS (58/201 without labor; 65/201 without ruptured membranes) | ||
| Exclusion: fever, antibiotics within 7 days, penicillin or cephalosporin allergy | ||
| Interventions | Cefuroxime 750 mg IV after cord clamping (N = 102) vs no treatment (N = 99) | |
| Outcomes | Febrile morbidity (> 37.9°C twice at least 6 hours apart after first post-operative day) ; endometritis (fever, uterine tenderness and abnormal lochia); wound infection (fever, cellulitis and/or purulent discharge); UTI; cost of post-operative antibiotics (treatment $US0.69 vs control $US7.47); maternal hospital stay (treatment 8.1 vs control 8.0, no variance given) | |
| Notes | No woman had a severe infection such as pelvic abscess or septic pelvic thrombophlebitis | |
| Class of antibiotic: second generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “…randomly…” |
| No further information. | ||
| Allocation concealment? | Unclear | Paper reports using envelopes containing empty vial or vial containing treatment |
| Blinding? | Unclear | Not placebo controlled. |
| All outcomes | “Patients, attending physicians, and study coordinators were blind with regard to group assignments.” | |
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. The analysis appears to be by ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding epidemiologic and obstetric data. However, there is Insufficient information overall |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Double blind, placebo controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Athens, Greece. | ||
| Inclusion criteria: women undergoing elective or non-elective CS. Age range 17-40 years Exclusion criteria: allergy to metronidazole, amnionitis, and pyrexia | ||
| Interventions | Metronidazole 500 mg IV 2 hours or immediately preoperatively, 500 mg intraopera-tively, 1000 mg 8 hours post-operatively (N = 50), vs placebo (N = 50) | |
| Outcomes | Wound infection; endometritis; inadequate wound healing (metronidazole 1/50 vs placebo 8/50); mean temperature (36.8°C SD 1.02 vs 37.6, 1.03); duration of hospital stay. | |
| Notes | Although the authors are not identical and the presentation of the data makes direct comparisons difficult, the description of the 2 studies cited is so similar that it is presumed the 2 citations refer to the same patient population | |
| Translated from Bulgarian. | ||
| Class of antibiotic: nitroimidazole (metronidazole). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Women were divided into 2 groups; no further details available |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | Placebo given to control group; described as “double blind”. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No information available (pending full translation). |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | There was no significant difference in parity and age between the groups. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Unclear. |
| Methods | Randomized placebo controlled trial; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dats of data collection: not reported. | |
| Setting: Jersey City Medical Center, New Jersey; predominantly lower socio-economic indigent women Inclusion criteria: women | ||
| undergoing primary CS after onset of labor (corresponds to the definition of non-elective) | ||
| Exclusion: febrile or infected, allergy to pipericillin. | ||
| Interventions | Pipericillin 4 g peri-operatively (N = 50) vs pipericillin 4 g peri-operatively and at 4 and 8 hours post-operatively (N = 50) vs placebo (N = 50); both treatment groups combined in analysis | |
| Outcomes | Febrile morbidity (> 38.0°C twice at least 6 hours apart after first post-operative day) ; endometritis (fever, tender uterus and purulent lochia); hospital stay (no significant difference, variance not given) | |
| Notes | Use of saline or antibiotic lavage not allowed. | |
| No adverse reactions reported with treatment. | ||
| Class of antibiotic: ureidopenicillin (pipericillin). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “…randomly divided…” |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | Described as blinded. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No losses or exclusions were reported. The analysis appears to be by ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 3 groups were comparable regarding number of vaginal exams, haemoglobin levels and other risk factors. However, there was insufficient information to judge overall |
| Overall low risk of bias? | Unclear | Unclear. |
| Methods | RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: February to June 1982. | |
| Setting: Kaiser-Permanente Medical Center-Santa Clara, California | ||
| Inclusion criteria: all women undergoing CS (39/128 repeat section) | ||
| Exclusion: fever or infection, allergy to antibiotics. | ||
| Interventions | Cefoxitin 2 g in 1 L saline irrigation (N = 41) vs cephapirin 2 g in 1 L saline irrigation (N = 44) vs identical appearing placebo saline irrigation (N = 43) after delivery of the placenta; both treatment groups combined in the analysis | |
| Outcomes | UTI (positive culture); wound infection (purulent wound discharge with or without wound separation); endometritis (fever > 100.4°F after first post-operative day, uterine tenderness, foul smelling lochia without other source) | |
| Notes | Follow up for 8 weeks. | |
| 1 patient in placebo group developed septic pelvic thrombophlebitis and septic pulmonary emboli, classified as a serious complication | ||
| Class of antibiotic: first generation cephalosporin or second generation cephalosporin (cefamycin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “Sequenced randomly by lottery method.” |
| Allocation concealment? | Yes | “1 milliliter of multivitamin infusion was added to create an identical appearance of all solutions .… and bags sequenced randomly … used in numerical order.” |
| Blinding? | Yes | “Patients, physicians, operative room personnel and data collectors were… blinded to the group assignment.” |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No loss to follow up reported. |
| All outcomes | 4 patients were eliminated from the statistical analysis because ofdeviations from the protocol of irrigation technique Not ITT analysis. Data could not be re-included in the analysis | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | There were no statistically significant differences in mean gestational age, mean number of vaginal examination or mean duration of ruptured membranes between groups. There was insufficient other information which to judge |
| Overall low risk of bias? | Yes | There is low risk of bias for the 4 major components. |
| Methods | Random, double-blind, placebo-controlled trial; 2 parallel groups | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection:July 1985-January 1986. | |
| Setting: Louisiana State University Hospital; 90% indigent population | ||
| Inclusion criteria: women undergoing elective and non-elective CS (definitions of elective and emergency CS not provided; results combined in the analysis) | ||
| Exclusion: antibiotic use within 2 weeks, allergy to penicillin | ||
| Interventions | Ticarcillin 5 g in 1200 ml saline irrigation (N = 112) vs saline irrigation (N = 100) Results of the second part of the study (cefoxitin vs ticarcillin) not included | |
| Outcomes | Febrile morbidity (> 100.3°F twice at least 4 hours apart after first post-operative day); endomyometritis, wound infection, UTI, septicaemia, maternal hospital stay (treatment 4.5 vs placebo 5.4, no variance given) | |
| Notes | Definition of elective and non-elective CS not provided. | |
| There were 3 episodes of septicaemia in those women undergoing emergency section (2 in the control group and 1 in the placebo group) | ||
| Class of antibiotic: carboxypenicillin (ticarcillin). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “… in a random double-blind manner.” |
| No additional information provided. | ||
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Double blind. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear |
|
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | In Part 1, the duration of labor was significantly longer in the ticarcillin group than in the saline group. There is insufficient information to assess overall bias |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Double blind, placebo controlled trail; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: November 1986 and March 1987. | |
| Setting: University of Zimbabwe; patients enrolled between | ||
| Inclusion criteria: all women undergoing elective CS (before onset of labor or rupture of membranes; corresponds to our definition of elective) | ||
| Interventions | Crystalline penicillin 2 MU and chloramphenicol 500 mg pre-operatively “before going to theatre” ( N = 115) vs matching placebo (N = 117) | |
| Outcomes | Fever (> 37.9oC twice at least 4 hours apart after first post-operative day); wound sepsis (graded as abnormal erythema and/or induration, oozing wound without frank pus or pus formation); endomyometritis (fever, uterine tenderness and foul-smelling lochia), pelvic abscess formation, bacteraemia; maternal hospital stay (treatment 5.43 vs placebo 6.18, variance not given) | |
| Notes | No woman developed pelvic abscess nor required a laparotomy. | |
| Class of antibiotic: penicillin and chloramphenicol. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “… randomized…” |
| Allocation concealment? | Unclear | “…a randomized list…” |
| Blinding? | Yes | Double blind. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. Analysis appears to be ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The groups were comparable regarding age, pre-operative weight, parity, previous CS, gestational age, and pre-operative haemoglobin. Insufficient information overall |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: July 1986-December 1987. | |
| Setting: Grenoble, France. | ||
| Inclusion criteria: ‘low-risk’ women, undergoing CS (27% in labor) | ||
| Exclusion: allergy to beta-lactam antibiotics, receipt of antibiotics within 3 days; ruptured membranes >12 hours; fever, amniotic infection | ||
| Interventions | Cefotetan 1 g IV at the time of cord clamping (N = 136) vs placebo injection (N = 130) | |
| Outcomes | Endometritis, wound infection (includes superficial wound infection and deep abscess), septicaemia; additional antibiotic use (10/136 in treatment group vs 19/130 in placebo) ; antibiotic costs; maternal hospital stay | |
| Notes | There was 1 episode of septicaemia in the placebo group. | |
| Class of antibiotic: second generation cephalosporin (cefamycin) | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “…randomized by drawing of lots.” |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Double blind, placebo-controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. Analysis appears to be ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups reported as comparable regarding demographic values. Insufficient additional information |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: June - September 1979. | |
| Setting: National Women’s Hospital, Auckland, New Zealand. | ||
| Inclusion criteria: all women undergoing CS (8/73 were repeat) | ||
| Exclusion: already on antibiotics. | ||
| Interventions | Metronidazole 500 mg IV prior to incision and metronidazole 2 g suppository at end of surgery (N = 35) vs matching placebo infusion and suppository (N = 38) | |
| Outcomes | Fever (> 37.9°C within 14 days of delivery); wound infection, endometritis, UTI, major complication (return to theatre or hospitalised >10 days because of post-operative morbidity); need for antibiotic therapy (treatment 13 vs placebo 10); fever index (257 degree hours vs 165 hours) | |
| Notes | 1 major complication (not infectious) in each group (bleeding from lower segment in 1, major deep vein thrombosis extending into iliac veins in another) | |
| Drug class: nitroimidazole (metronidazole). | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomized.” |
| No additional information. | ||
| Allocation concealment? | Unclear | No information was provided. |
| Blinding? | Yes | Double-blind, placebo-controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses to follow up reported. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The groups were comparable regarding age and weight. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT: 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not specified. | |
| Setting: Durban, South Africa. | ||
| Inclusion criteria: all patients undergoing CS. | ||
| Exclusion criteria: women with pre-existing UTI. | ||
| Interventions | Ampicillin 500 mg IM pre-operatively and 8 hourly for 48 hours followed by 500 mg orally 8 hourly for 4 days (N = 150) vs no treatment for first 48 hours then oral placebo 8 hourly for 4 days (N = 150) | |
| Outcomes | UTI (culture positive), intra-uterine infection not defined further, classified as endometri-tis), wound infection | |
| Notes | Fewer postpartum urinary isolates in treated group were sensitive to ampicillin (8/17 vs 18/26). | |
| In the control group, 3 women developed pelvic abscesses (included as serious morbidity) and 1 patient required hysterectomy for secondary postpartum haemorrhage following severe E. coli intrauterine infection | ||
| Class of antibiotic: aminopenicillin (ampicillin). | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “on a random basis.” |
| Method not described. | ||
| Allocation concealment? | Unclear | Insufficient information to judge. |
| Blinding? | Unclear | Partly placebo controlled: “an oral placebo was given after 48 hours” |
| All outcomes | ||
| Insufficient information to judge whether there was blinding of study personnel | ||
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after randomization. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | insufficient information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, controlled trial; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: University of Natal, Durban, South Africa. | ||
| Inclusion criteria: women undergoing emergency CS (ruptured membranes for > 6 hours and < 20 hours; corresponds to our definition of non-elective) | ||
| Exclusion criteria: prior antibiotic therapy, fever > 37.2°C, fetal tachycardia of > 160/minute. | ||
| Interventions | Lincomycin 600 mg (N = 20) vs metronidazole 500 mg (N = 20) vs placebo (N = 20) IV 2 hours pre-operatively and 8 hourly for 48 hours; both treatment groups are combined for the analysis | |
| Outcomes | Wound discharge/abscess formation, puerperal sepsis (> 37.9°C twice in first 48 hours or > 37.5°C from 2nd post-operative day), septicaemia, UTI. | |
| Notes | Authors’ definition of puerperal sepsis has been classified as fever. | |
| No complications of drug administration reported in mothers or babies; no rash, diarrhoea nor nausea | ||
| Class of antibiotic: Lincosamide (lincomycin). | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Randomized. |
| No further information provided. | ||
| Allocation concealment? | Yes | “…using unmarked code-numbered separate boxes.“ |
| Blinding? | Unclear | Described as “double-blind” placebo-controlled. |
| All outcomes | ||
| Drug to be given was “in unmarked boxes in the original packing” | ||
| Incomplete outcome data addressed? | Yes | No losses to follow up. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | No information was provided. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Norfold General Hospital, Virginia; both private (N = 70) and clinic (N = 78) women included | ||
| Inclusion criteria: all women undergoing CS (49/148 were repeat procedure; 57/148 were not in labor) | ||
| Exclusion: membranes ruptured > 24 hours. | ||
| Interventions | Cephalothin 2 g IV 15-30 minutes prior to surgery and 1 g every 6 hours for 36 hours, then cephalexin 500 mg orally every 6 hours until 5th post-operative day (N = 74) vs identical appearing placebo (N = 74) | |
| Outcomes | Fever (> 100.3°F twice after 48 hours); endometritis (fever, uterine tenderness, foul-smelling or abnormal lochia and positive cultures); UTI, wound infection; maternal hospital stay (treatment 6.2 vs placebo 7.5, no variance given) | |
| Notes | All bacterial isolates in treatment group were sensitive to cephalothin | |
| Class of antibiotic: first generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Assigned in a random manner.” |
| No further information provided. | ||
| Allocation concealment? | Yes | All preparations supplied by the pharmacy had a code number known only by the pharmacy |
| Blinding? | Yes | Double blind, placebo controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. |
| All outcomes | 52/200 excluded for various reasons, including 14 because of protocol violations ITT analysis performed on available data. | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | No information was provided. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Quasi-RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: City of Memphis Hospitals, Tennessee; indigent women, many obstetric and metabolic complications | ||
| Inclusion criteria: all women undergoing CS. | ||
| Exclusion criteria: febrile or infected. | ||
| Interventions | Aqueous penicillin 10 MU every 8 hours and kanamycin 500 mg IM every 12 hours pre-operatively and for 3 days post-operatively (N = 115) vs no treatment (N = 115) | |
| Outcomes | Fever (> 100.9°F after second post-operative day), severe pelvic infection (treatment 27% vs control 7%); ‘free of infectious morbidity’ (3.6 vs 6.8 days); maternal hospital stay (5.4 vs 8.8 days, no variance given) | |
| Notes | No adverse drug reactions reported; no evidence of development of resistance reported. Unable to ascertain from description of study incidence of endometritis or wound infection; inadequate description of nature of severe pelvic infections (not included as outcome in analysis). | |
| 2 groups of women were studied retrospectively (N = 75); methods nor results do not specifically describe results of this group and it is unclear whether they have been included in the overall results | ||
| Class of antibiotic: penicillin and aminoglycoside. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | No | Alternate allocation to treatment or no treatment. |
| Allocation concealment? | No | “…every other patient.” |
| Blinding? | Unclear | Not placebo-controlled. |
| All outcomes | No further information provided. | |
| Incomplete outcome data addressed? | Yes | No loss to follow up. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding gravidity, parity, age and operative indica-tors.There was insufficient other information which to judge |
| Overall low risk of bias? | No | Quasi-RCT suggests high risk of bias. |
| Methods | RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: March-August 1991. | |
| Setting: Ipoh, Malaysia. | ||
| Inclusion criteria: women undergoing CS. | ||
| Exclusions: hypersensitivity to 1 of antibiotics; presence of infection or fever; on antibiotics; multiple pregnancy | ||
| Interventions | Cefoperazone 1g every 12 hours × 3 (N = 71) vs ampicillin 500mg every 6 hours × 4 (N = 74) at induction of anesthesia vs no treatment (N = 77); both treatment groups combined for data analysis | |
| Outcomes | Wound infection (inflammation over wound with serous or purulent discharge); any antibiotics post-operatively (cefoperazone vs ampicillinvs no treatment: 6.6% vs 16.2% vs 25.7%). Hospital stay: ampicillin vs no treatment 5.57 days (SD 1.43) vs 6.5 days (SD 3.67) | |
| Notes | Author’s definition of emergency not consistent with criteria used in this review; classified as both/undefined | |
| Class of antibiotic: third generation cephalosporin or aminopenicillin (ampicillin) | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “… randomized…” |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | No information provided. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | 2 patients excluded (1 from cefoperazone group, 1 from no treatment group); on treatment analysis performed |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 3 groups were comparable regarding age, race, parity, gestational age, etc. But insufficient information overall |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, double-blind, placebo-controlled trial; two parallel arms | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Johns Hopkins Hospital, Baltimore, US. | ||
| Inclusion criteria: all women undergoing CS (35/71 were a repeat section) | ||
| Exclusion: fever, membrane rupture > 24 hours, penicillin allergy, lack of consent | ||
| Interventions | Ampicillin 2 g pre-operatively (N = 34) vs similar-appearing placebo (N = 37) | |
| Outcomes | Fever (> 37.0°C twice at least 6 hours apart after first post-operative day); endometritis, UTI, wound infection, bacteraemia, pelvic abscess, maternal hospital stay | |
| Notes | The authors definition of primary and repeat are different from those used in this review and have not been analysed separately; most women for repeat section were in early labor at the time the operation was performed | |
| Study medications were administered pre-operatively when possible, however transit time delays resulted in patients receiving medication after the surgical procedure had started | ||
| There was 1 pelvic abscess in the placebo group; there were 3 episodes of bacteraemia (1 Klebsiella spp. in treatment group, 2 group B streptococcal infections in placebo); combined for outcome of serious morbidity | ||
| Class of antibiotic: aminopenicillin (ampicillin). | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomly assigned.” |
| Method not described. | ||
| Allocation concealment? | Yes | “The medication code was kept in the pharmacy.” |
| Blinding? | Yes | “… or a similar appearing placebo… all solutions were prepared (in the pharmacy).” |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after randomization. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “There were no statistically significant differences in (the epidemiologic and obstetric variables in the two groups) when the study and placebo groups were compared.” |
| Insufficient other information to judge. | ||
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, placebo controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: July-December 1976. | |
| Setting: Naval Regional Medical Center, Portmouth, Virginia, US | ||
| Inclusion criteria: all women undergoing CS (46/122 were a repeat section). The authors’ definition of primary and repeat do not correspond to definitions of elective and non-elective used in this review (repeat sections included women in labor with ruptured membranes). The results for these two categories have been combined in this review | ||
| Exclusion criteria: allergy to penicillin or cephalosporin, infection or receiving antibiotics | ||
| Interventions | Cefazolin 500 mg IV 30 minutes before and 500 mg at 2 and 1 g at 8 hours after delivery (N = 61) vs matching placebo (N = 61) | |
| Outcomes | Endometritis (fever and uterine tenderness or fever and pathogenic organism); UTI (fever and symptoms, or positive culture); wound infection (fever, cellulitis and exudate) ; maternal hospital stay (treatment 5.5 days vs placebo 5.7 days, no variance given) | |
| Notes | 2 women developed serious complications as stated by the authors: 1 in treatment group developed septic pelvic thrombophlebitis; 1 given placebo developed pneumonia and endoparametritis (both included in outcome of serious morbidity) | |
| Class of antibiotic: first generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomly.” |
| No further information. | ||
| Allocation concealment? | Yes | “All preparations supplied had a code number known only by the pharmacy.” |
| Blinding? | Yes | Described as double-blind. |
| All outcomes | “All materials appeared similar in solution.” | |
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. 8 women excluded for mistakes in protocol (no further details) could not be included in ITT analysis |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, height, weight, etc. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: July 1978-October 1980. | |
| Setting: Brigham and Women’s Hospital, Boston, Massachusetts, US | ||
| Inclusion criteria: all women undergoing CS (other than repeat section); criteria do not correspond with our definition of non-elective | ||
| Exclusion: active infection, fever, membranes ruptured > 36 hours, antibiotic therapy within 2 weeks, renal disease, allergy to penicillin or cephalosporin | ||
| Interventions | Cefazolin 2 g after cord clamped (N = 146) and at 4 and 8 hours after first dose vs matching placebo (N = 132) | |
| Outcomes | Fever (oral temperature > 100.3 degrees Fahrenheit on any of 2 of first 10 post-operative days); UTI, wound infection (only pus-draining included in outcome of wound infection); endometritis (fever, tenderness on pelvic examination, abnormal discharge) ; pelvic abscess; septic pelvic thrombophlebitis, bacteraemia; subsequent antibiotic use (23% for placebo vs 12% for treatment) | |
| Notes | Outcome of fever and minor wound infection combined (11/146 for treatment vs 13/ 132 for placebo). | |
| 4 episodes of bacteraemia, all in placebo group. | ||
| 1 episode of rash and 1 episode of phlebitis reported in treatment group vs none in control. | ||
| Data collected at 6 weeks on 259/266 patients; 35% of infections diagnosed after discharge | ||
| Class of antibiotic: first generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomly allocated.” |
| No further information. | ||
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Double blind; placebo-controlled. |
| All outcomes | “Participants, their physicians and all investigators were unaware of the assignment throughout the study.” | |
| Incomplete outcome data addressed? | Unclear | 12 participants withdrawn (8 treatment, 4 placebo) and started on therapeutic antibiotics by the surgeon because the operation had been prolonged or was complicated or the preoperative specimen of urine disclosed significant bacteriuria Results on participants excluded could not be re-included in ITT analysis |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, body mass index, proportion on private service, etc. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Hanover, Germany. | ||
| Inclusion criteria: women undergoing CS. | ||
| Interventions | Mezlocillin 2 g IV half hour pre-operatively then every 8 hours × 4 (N = 70) vs no treatment (N = 70) | |
| Outcomes | Wound infection (inflammation with or without exudation); endometritis (fever and tenderness of the uterus or fever with pathogens from the cervical canal); UTI (> 100, 000 bacteria/ml) | |
| Notes | 1 episode of allergic skin reaction occurred with the injection of mezlocillin | |
| Class of antibiotic: ureidopenicillin (mezlocillin). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “… randomized…” |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | No information provided. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | 1 drop-out (no treatment) reported. Analysis appears to be ITT. |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, height, weight, and risk of wound infection. But risk of endometritis was not in balance in the 2 groups. Insufficient information overall |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: September 1977-January 1978. | |
| Setting: State Maternity Hospital, Helsinki, Finland. | ||
| Inclusion criteria: all women undergoing CS. | ||
| Exclusion criteria: allergic to penicillin, clindamycin or gentamicin; emergency section | ||
| Interventions | 10 million units benzyl penicillin IV (N = 46) vs 500 mg clindamycin IV and 80 mg gentamicin IM (N = 42) vs glucose solution placebo (N = 40) IV by infusion starting 30 minutes before operation and stopping 4 hours after. Results of both treatment groups combined | |
| Outcomes | Endometritis (fever, uterine tenderness and foul-smelling vaginal discharge); wound infection (all grades combined); hospital stay (treatment 7.7 vs 7.7 placebo; no variance given) | |
| Notes | Data from a fourth group that consisted ofpatients allergic to 1 ofthe drugs or undergoing an emergency section have not been included | |
| Drug class: penicillin or lincosamide (clindamycin) and aminoglycoside | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Assigned at random … in bottles containing code numbers.” |
| No further information provided. | ||
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Placebo-controlled. |
| All outcomes | “the code was kept secret for persons performing the operations and observing the patients in the post-operative period.” | |
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. |
| All outcomes | Two women excluded after initial randomization. | |
| ITT analysis with available data. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The first 3 groups were comparable regarding number of amnioscopic examinations, number of vaginal examination, duration of labor and duration of intrauterine monitoring. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT: 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Women undergoing elective CS (absence of labor and before rupture of membranes). | |
| Exclusion: allergy to penicillin or cephalosporin, prior antibiotic therapy within 7 days. | ||
| Setting: United Arab Emirates. | ||
| Interventions | Cefuroxime 1.5 g after clamping of the cord vs no treatment. | |
| Outcomes | Febrile morbidity (temperature of > 38°C after first 48 hours); endometritis (uterine tenderness and offensive lochia with fever and no other source); wound infection (erythema, induration or purulent discharge); UTI (> 100,000 bacteria/ml) | |
| Notes | Majority of patients were indigent; follow up at 6 weeks. | |
| Class of antibiotic: second generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “…a computer generated number scheme…” |
| Allocation concealment? | Unclear | Although “…randomization code and the mode of intervention was only known to the anesthesiology staff…” there is still insufficient information to judge allocation concealment |
| Blinding? | Yes | Not placebo controlled, but “patient and study co-ordinators unaware of group allocation” |
| All outcomes | ||
| The mode of intervention was only known to the anesthesiology staff. So those assessing outcomes were not aware of allocation | ||
| Incomplete outcome data addressed? | Unclear | No losses or exclusions were reported. Analysis appears to be ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, parity, weight, gestational age and indication for cesarean. Insufficient information overall |
| Overall low risk of bias? | Unclear | Mostly unclear, particularly allocation concealment. |
| Methods | Randomized, placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: April 1983-October 1984. | |
| Setting: Academisch Ziekenhuis der Vrije Universiteit, Amsterdam, The Netherlands | ||
| Inclusion criteria: all women undergoing CS (77/129 were elective sections) | ||
| Exclusion: active infection, antibiotics within 7 days, allergy to penicillin or cephalosporin, impaired liver or renal function | ||
| Interventions | Cefoxitin 2 g (N = 64) vs matching placebo (N = 65) IV bolus immediately following clamping of the cord and at 6 and 12 hours later | |
| Outcomes | Febrile morbidity (> 38°C for at least 24 hr after first 24 hr); endometritis (fever, fetid lochia and/or uterine tenderness on pelvic examination); wound infection (palpable induration, wound dehiscence and/or pus drained); UTI (positive culture), bacteraemia | |
| Notes | 1 episode of Staphylococcus aureus bacteraemia (in cefoxitin group) not considered life-threatening (included in outcome of serious morbidity). No serious antibiotic side effects reported in cefoxitin-treated group; 1 patient in cefoxitin group developed diarrhoea | |
| Class of antibiotic: second generation cephalosporin (cefamycin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | ‘Randomly allocated.’ No further information. |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Placebo-controlled: “matching placebo”. |
| All outcomes | Described as “double blind”. | |
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. |
| All outcomes | 21 women were excluded: 2 had fever prior to surgery, 2 because of a known allergy to penicillins; 8 women excluded because of protocol failures and 9 women for intraoperative complications (not defined further) Not ITT analysis. | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding demographic, obstetric and operative fac-tors.There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Addenbrooke’s Hospital, Cambridge, UK. | ||
| Inclusion criteria: women undergoing emergency CS (in active labor with membrane rupture) | ||
| Exclusion criteria: pyrexia; antibiotic use within 2 weeks. | ||
| Interventions | Metronidazole 500 mg (N = 57) vs placebo (N = 58) IV infusion at start of procedure; post-operatively metronidazole or placebo suppository twice daily for 5 days | |
| Outcomes | Pyrexia (> 38°C twice 4 hours apart after first 24 hours); wound infection; endometritis (heavy, offensive lochia and pyrexia); UTI; antibiotic use (15/57 in treatment group vs 20/58 in control group) | |
| Notes | 1 woman in the control group developed a pelvic abscess. | |
| Length of admission not significantly different between the 2 groups (mean 7.4, SD 2. 3 days). | ||
| No adverse reactions occurred. | ||
| Class of antibiotic: Nitroimidazole (metronidazole). | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomized, sequential basis.” |
| No further information. | ||
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Double-blind, placebo controlled. |
| All outcomes | “Antibiotic … was provided without access to the ‘trial code.”’ | |
| Incomplete outcome data addressed? | Yes | No loss to follow up. |
| All outcomes | No participant excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | Comparison of the 2 groups showed similar risk factors.There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Quasi-RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: New York Medical College, New York, US. | ||
| Inclusion criteria: all women undergoing CS (divided into “no labor” and “labor” groups which correspond to the definitions of elective/non-elective used in this review | ||
| Exclusion criteria: fever, antibiotic use within 2 weeks, ruptured membranes > 2 hours, major penicillin allergy | ||
| Interventions | Cephalothin 2 g IV and kanamycin 1 g IM at induction of anesthesia, then cephalothin 2 g IV q6hrs × 8 doses and kanamycin 500 mg IM q12 hr × 4 doses (N = 47) vs no treatment (N = 53) | |
| Outcomes | Febrile morbidity (temperature greater that 100.4°F orally on 2 consecutive days, excluding the first post-operative day); endometritis (fever, uterine tenderness and positive culture or fever and pathogenic organism); UTI, wound infection (fever and cellulitis or exudate). Data available on elective (defined as no labor) and non-elective (defined as presence of labor) | |
| Notes | No difference in average duration of hospital stay between groups (data not shown). | |
| 1 woman (treatment group) developed endometritis with organism resistant to cephalothin and kanamycin | ||
| Class of antibiotic: first generation cephalosporin and animoglycoside | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | No | Randomized “…using the last digit of their hospital chart number” to treatment or no treatment |
| Allocation concealment? | No | “…using the last digit of their hospital chart number.” |
| Blinding? | No | Not placebo controlled. |
| All outcomes | No further information provided. | |
| Incomplete outcome data addressed? | Yes | No loss to follow up. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, parity, ethnic background or type of anesthesia. There was insufficient other information which to judge |
| Overall low risk of bias? | No | Quasi-RCT suggests high risk of bias. |
| Methods | Randomized placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Jeddah, Saudi Arabia. | ||
| Inclusion criteria: women undergoing CS (both elective and emergency) | ||
| Exclusions: use of antibiotics, fever or signs of infection; allergy to penicillin or cephalosporin | ||
| Interventions | Cefazolin 1 g after clamping of the cord (N = 221) vs matching placebo (N = 220) | |
| Outcomes | Febrile morbidity (> 38°C twice 4 hours apart after first 24 hours); endometritis (fever, uterine tenderness and abnormal lochia); wound infection (fever, cellulitis or exudate with positive culture); UTI (fever and positive urine culture); pneumonia, bacteraemia, pelvic abscess, unexplained fever, therapeutic antibiotics, length of post-operative stay | |
| Notes | Definition of emergency section (unscheduled) did not correspond to the definition of non-elective section used in this review; these patients have been analysed in the “both or not-defined” group. Women undergoing elective section included women with scheduled section and with intact membranes and have been analysed in the “elective” group. | |
| There were no significant differences in the fetal outcomes reported (definitions not consistent with those for this review; no serious side effects with cefazolin | ||
| Class of antibiotic: first generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “…computer-generated randomization…” |
| Allocation concealment? | Yes | “…each indistinguishable minibag was given a code number in the department of pharmaceutical care.” There was, however, no information on how the codes were used and whether there was sequential opening |
| Blinding? | Yes | Triple blind. “Both the experimental drug and placebo were indistinguishable.” |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. Analysis appeared to be by ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding maternal characteristics and emergency and elective CS. Insufficient information overall |
| Overall low risk of bias? | Yes | Mostly low risk of bias. |
| Methods | RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: Tripler Army Medical Center, Honolulu, Hawaii, US. | ||
| Inclusion criteria: all women undergoing CS (19/60 women had ruptured membranes > 6 hours; 40/60 were in active labor) | ||
| Exclusion: known infection, currently on antibiotics, allergic to penicillin or cephalosporin | ||
| Interventions | Cefamandole 2 g in 800 ml normal saline irrigation (N = 30) vs irrigation with 800 ml normal saline (N = 30). Non-irrigation control group (N = 30) not included in analysis | |
| Outcomes | Endomyometritis (fever, unusual uterine and parametrial tenderness without evidence of other source of infection); maternal length of stay | |
| Notes | Length ofhospital stay for the control group included results from both the no irrigation group and the placebo irrigation group (5.37 days vs 4.53 for treatment group) | |
| Class of antibiotic: second generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Randomly allocated using table of random numbers. |
| Allocation concealment? | Yes | Randomly allocated by hospital pharmacy. |
| Blinding? | Yes | Double-blind, placebo-controlled. |
| All outcomes | Vitamin solution added to make placebo visually identical; physicians and patients blinded to treatment | |
| Incomplete outcome data addressed? | Yes | No losses were reported. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 3 groups were comparable regarding age, parity, weight and socioeconomic background. Insufficient information overall |
| Overall low risk of bias? | Yes | Mostly low risk of bias. |
| Methods | Randomized, placebo-controlled; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting:Hospital Central Militar, Mexico city, Mexico. Women predominantly (78%) of low socioeconomic level | ||
| Inclusion criteria: women in active labor undergoing CS. | ||
| Exclusion: elective CS, evidence of infection, antibiotic use within 8 days, metronidazole intolerance, lack of consent | ||
| Interventions | Metronidazole 1 g IV (N = 50) vs identical appearing placebo (N = 50) immediately after cord clamping | |
| Outcomes | Endometritis (purulent and/orfoul odour lochia); wound infection (wound edges tender, red and swollen, or frank pus or sanguino-purulent material exuded); UTI (bacteria seen in sediment); maternal hospital stay | |
| Notes | Class of antibiotic: Nitroimidazole (metronidazole). | |
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “… randomized…” |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Double blind. |
| All outcomes | Identical appearing placebo. | |
| Incomplete outcome data addressed? | Unclear | No losses or exclusions were reported. Appears to be ITT analysis |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups reported as comparable regarding age and parity, etc. Insufficient information overall |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Participants | Dates of data collection:Not specified. | |
| Setting: Fairfax Hospital, Virginia, US. Women predominantly private | ||
| Inclusion: criteria: high-risk women undergoing CS (in active labor and/or ruptured membranes > 4 hours); not consistent with the criteria for non-elective in this review: | ||
| classified as “both/undefined” in this review Exclusion: active infection, fever, antibiotic use within 3 days, allergy to penicillin or cephalosporins | ||
| Interventions | Ceftizoxime 2 g (N = 50) vs placebo (N = 49) IV at time of cord clamping | |
| Outcomes | Febrile morbidity (oral temperature > 37.9°C twice at least 8 hr apart, after first 24 hr); endometritis (fever and foul lochia or uterine tenderness); UTI (fever and positive culture); wound infection (fever, abnormal-looking wound, surrounded by cellulitis and/or draining purulent material) | |
| Notes | Class of antibiotic: third generation cephalosporin. | |
| There was 1 drug reaction (maculopapular rash) in the treatment group. | ||
| Women followed up at 6 weeks. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “randomized.” Method not described. |
| Allocation concealment? | Unclear | No information. |
| Blinding? | Unclear | Placebo controlled. |
| All outcomes | Described as “double-blinded” but insufficient information to judge whether there was adequate blinding of study personnel | |
| Incomplete outcome data addressed? | Unclear | No loss of participants to follow up. |
| All outcomes | 1 patient was removed from the study when she became febrile in the delivery room, not included in ITT analysis | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “The groups were comparable. No significant differences were observed between the 2 groups with respect to maternal age, parity, gestational age, duration of labor, duration of ruptured membranes or use of internal fetal monitoring. There were no significant differences regarding indication for CS”. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: November 1981-March 1982. | |
| Setting: University of Parma, Parma, Italy. | ||
| Inclusion criteria: women undergoing emergency CS (58/60 women in spontaneous labor; classified as non-elective) | ||
| Exclusion criteria: allergy to penicillin or cephalosporins; severe renal disease, history of pelvic infections | ||
| Interventions | Cefuroxime 750 mg IM 30-60 minutes before surgery and 8 and 16 hours after (short term)(N = 20) vs 750 mg 3 times a day for 5 days (first dose being given post-operatively after the woman had returned to the ward) (long term) (N = 20) vs no treatment (N = 20). The results of both treatment groups have been combined | |
| Outcomes | Fever (> 100.3°F twice 6 hr apart); endometritis (fever and uterine tenderness); maternal stay (treatment 7.1 vs control 7.9 days, no variance given) | |
| Notes | Note: the group given long-term prophylaxis received the first dose after return to the ward | |
| Class of antibiotic: second generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Randomly assigned. |
| No further information. | ||
| Allocation concealment? | Unclear | No information was provided. |
| Blinding? | Unclear | Not placebo controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No losses to follow up reported. |
| All outcomes | 1 woman was excluded because of an allergic reaction to cefuroxime | |
| Could not be re-included in ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 3 groups were comparable.There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | All sections unclear. |
| Methods | Randomized trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: November 1983-October 1984. | |
| Setting: Sodersjukhuset, Stockholm, Sweden. | ||
| Inclusion criteria: women with rupture of membranes for > 6 hours (equivalent to non-elective group) | ||
| Exclusion criteria: fever or foul smell of amniotic fluid. | ||
| Interventions | Cefuroxime 1.5 g IV q8 hr for 24 hours, starting immediately before or during the operation, followed by oral cefadroxil 500 mg twice daily for 6 days (N = 26) vs no treatment (N = 27) | |
| Outcomes | Endometritis (marked uterine tenderness with or without a foul discharge with fever at least twice); wound infection (redness, tenderness, induration and pus in the wound); UTI (positive culture) | |
| Notes | Data provided (but not included) for a second control group eligible for inclusion but not randomized. | |
| Numbers not provided to calculate mean maternal length of stay for the 2 randomized groups | ||
| Class of antibiotic: second generation cephalosporin, then first generation cephalosporin | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | ‘Randomly referred.’ |
| No other information provided. | ||
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | No | Not placebo controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | No | No loss to follow up reported. |
| All outcomes | 11 patients “should have been given prophylactic treatment according to the study design but received no antibiotics and … formed a second control group” Not ITT analysis. | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, parity, previous CS, duration of labor and membrane rupture. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 4 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: not reported. | |
| Setting: United Arab Emirates. | ||
| Inclusion criteria: women undergoing elective CS (definition not provided) | ||
| Exclusion: hypersensitivity to penicillin or cephalosporin; prior antibiotic therapy within 3 days; hepatorenal insufficiency; positive cultures or definite evidence of infection | ||
| Interventions | Pipericillin 4 g IV after the cord was clamped (N = 48) vs cephradine 500 mg plus metronidazole 500 mg both IV after the cord was clamped and every 8 hours × 2 (N = 47) vs piperacillin 2 g IV after clamping of the cord and 2 g every 8 hours × 2 (N = 52) vs no treatment (N = 51) | |
| Outcomes | Febrile morbidity (fever > 38°C twice 4 hours apart after first day); endometritis (uterine and parametrial tenderness, foul smelling vaginal discharge); wound infection (local induration and tenderness with wound exudate) | |
| Notes | 3 women who developed drug reactions were excluded from study (1 from each of the treatment groups). Late morbidity evaluated at 4-6 weeks | |
| Class of antibiotic: Ureidopenicillin (pipericillin). | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “… randomized…” |
| Allocation concealment? | Unclear | “…consecutively numbered sealed envelopes…” but as sequence generation was unclear, so allocation concealment will be unclear |
| Blinding? | Unclear | No information was provided. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No losses were reported but 14 women were excluded (8/147 from treatment groups, 6/51 from control group). It was an ITT analysis but with available outcome data |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | Insufficient information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, placebo controlled trial; 2 parallel groups (2:1 active:placebo randomization) | |
| Unit of randomization: individual. | ||
| Part of a larger study looking at prophylaxis also in gynaecologic surgery | ||
| Participants | Dates of data collection: July 1976-June 1978. | |
| Setting: 14 US centres. | ||
| Inclusion criteria: all women undergoing CS (46% in labor). | ||
| Exclusion criteria: infection, allergy to penicillin or cephalosporins | ||
| Interventions | Cephradine 1 g IV (N = 133) vs placebo (N = 66) within 1 hour prior to surgery, repeated at 4 hours | |
| Outcomes | Febrile morbidity (oral temperature > 37.7°C twice 4 hours apart, after first 48 hours) ; endometritis (uterine tenderness, fever and purulent discharge), wound infection (increased local tenderness, redness or swelling); UTI (positive culture); maternal length of stay (treatment 5.8 days vs placebo 7.57 days; P < 0.05, variance not given) | |
| Notes | Class of antibiotic: first generation cephalosporin. | |
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Randomly allocated. |
| No additional information. | ||
| Allocation concealment? | Unclear | Investigator provided with Individually. randomized block of patient numbers |
| Blinding? | Yes | Patients and investigators blind to allocation throughout the study Placebo-controlled. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. |
| All outcomes | Drop-outs in CS women not stated (overall: 11/319 from treated group, 8/172 from placebo group As treated analysis performed. | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age and other risk factors.There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, placebo-controlled trial; 3 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collectin: no reported. | |
| Setting: 5 centres in Canada. | ||
| Inclusion criteria: all women in labor or with ruptured membranes (duration of ruptured membranes not stated; mean duration 9.97 hours; included in both category) | ||
| Interventions | Cefoxitin 2 g (N = 124) vs cefazolin 1 g (N = 120) vs placebo (N = 117) infused IV immediately after cord clamped and 6 and 12 hours later. Results of both treatment groups combined | |
| Outcomes | Febrile morbidity (oral temperature > 37.9°C twice at least 6 hours apart after first 24 hours); wound infection (redness, induration, tenderness and/or purulent discharge from the incision line); endometritis/parametritis (uterine and/or adnexal tenderness with fever) UTI (dysuria or pyuria and positive culture); need for antibiotic therapy (11% for treatment groups vs 27% for placebo); maternal length of stay (7.3 and 7.4 days for treatment groups vs 7.9 for placebo) | |
| Notes | Side effects documented: 2 infusion-related hypotensive episodes (1 with cefazolin, 1 with placebo that necessitated withdrawal from study); 6 episodes of phlebitis (5 in treated, 1 in placebo group); 1 episode of angioedema (placebo patient). Data provided on antibiotic resistance in wound isolates and screening cervical cultures. 1 episode of bacteraemia (in placebo group); 1 episode of septic shock (in cefazolin-treated group); both outcomes included as serious morbidity. | |
| Follow up at 6 weeks. | ||
| Class of antibiotic: first generation cephalosporin or second generation cephalosporin | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomily assigned.” |
| No additional information. | ||
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | Described as “double-blind”. |
| All outcomes | No details provided on placebo. | |
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. |
| All outcomes | 7 women (1 in treatment, 6 in placebo group) initially randomized but results not included, 6 because they failed to receive all 3 doses, 1 because of hypotensive episode with first dose As-treated analysis performed. | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 3 groups were comparable regarding age, parity, gravidity, etc.There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | All unclear. |
| Methods | Randomized, placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization: individual placebo-controlled; double-blind | ||
| Participants | Dates of data collection: September 1978-June 1980. | |
| Setting: Beth Israel Hospital, Boston, Massachusetts, US. | ||
| Inclusion criteria: women undergoing primary CS (inclusion criteria not consistent with the definition of non-elective CS used in this review) | ||
| Exclusion criteria: < 18 years of age, membranes ruptured > 35 hours, allergy to penicillin or cephalosporin, fever, infection or antibiotic use, significant underlying cardiac, renal or hepatic disease, unable to provide consent | ||
| Interventions | Cefoxitin 2 g IV immediately after the cord was clamped and at 4 and 8 hours (N = 52) vs matched placebo (mannitol with riboflavin) (N = 61) | |
| Outcomes | Febrile morbidity (oral temperature > 37.9°C twice at least 6 hours apart after first 24 hours); UTI (positive culture); wound infection (purulence, cellulitis or dehiscence); endometritis (fever, uterine tenderness, abnormal lochia); septicaemia (positive blood culture in a clinically septic patient); additional antibiotic use (8 in treatment group vs 12 in placebo) | |
| Notes | Both episodes of septicaemia occurred in the placebo group. | |
| Class of antibiotic: second generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Randomized as determined by table of random numbers. |
| Allocation concealment? | Yes | Sequential study numbers. |
| Blinding? | Yes | Randomization was blind to both patients and investigators. |
| All outcomes | ||
| Placebo controlled: (mannitol with ri-boflavin). | ||
| Incomplete outcome data addressed? | Yes | No loss to follow up reported. |
| All outcomes | 14 women (7 in each group) initially randomized were later excluded (all doses not administered, antibiotic therapy prior to surgery, antibiotic following surgery, incorrect dose schedule, infection prior to surgery, drug code broken for possible allergy | |
| As treated analysis performed. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, body mass index, gravidity, frequency of fetal monitoring, number of vaginal examinations, duration of labor, duration of ruptured membranes, duration of surgery and indications for CS. There was insufficient other information which to judge |
| Overall low risk of bias? | Yes | Low risk of bias for the 4 main elements of the assessment. |
| Methods | Quasi-RCT, 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection; not reported. | |
| Setting: Hammersmith Hospital (N = 102) and Northwick Park Hospital (N = 99), London, England | ||
| Inclusion criteria: women undergoing CS (both elective and emergency) | ||
| Exclusion: on antibiotics, adverse reaction to penicillin or cephalosporin, pyrexia > 37.5 degrees C in labor, known vaginal pathogen, or suspected intrauterine infection | ||
| Interventions | Cephradine 2 g IV after induction of anesthesia and 1 g 6 and 12 hours after the operation (N = 101) vs no treatment (N = 100) | |
| Outcomes | Puerperal infection (temperature > 37.5°C after 24 hours); endometritis (pyrexia with uterine or adnexal tenderness); wound infection (purulent discharge or erythema, induration and serous discharge with positive culture); UTI (> 100,000 colony forming units in urine culture); length of hospital stay (7.63 for treatment group, 7.18 for control group [SD not provided]) | |
| Notes | Definitions of elective and emergency procedure, nor separate outcomes for each group, provided. | |
| Follow up completed 1987. | ||
| Class of antibiotic: first generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | No | “…alternate patients…” |
| Allocation concealment? | No | “…alternate patients…” |
| Blinding? All outcomes | Unclear | No information was provided. |
| Incomplete outcome data addressed? | Unclear | No losses or exclusions were reported. Analysis appears to be ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable with respect to age, social class, single mother, weight, previous CS, the mode of onset of labor, the use of electronic fetal monitoring, the type of CS, gestational age, birthweight or the perinatal outcome. Insufficient information overall |
| Overall low risk of bias? | Unclear | Quasi-RCT indicates high risk of bias. |
| Methods | Randomized, placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Date of data collection: not reported. | |
| Setting: Alexandra Maternity Hospital, Athens, Greece. | ||
| Inclusion criteria: women in labor (non-elective). | ||
| Exclusion criteria: acute bleeding due to abruptio placentae, established infection | ||
| Interventions | Cefuroxime 750 mg IV 1 hour or less before surgery and every 8 hours for 72 hours (N = 46) vs matching placebo (comparable in appearance and viscosity) (N = 50) | |
| Outcomes | Febrile morbidity (oral temperature of > 100.3°F twice 6 hours apart) and infection of endometrium, urinary tract and wound (not defined); results of duration of maternal stay only provided for febrile patients | |
| Notes | No patients had any major complications from the use of cefuroxime | |
| Class of antibiotic: second generation cephalosporin. | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Selected in a random manner.” |
| No additional information. | ||
| Allocation concealment? | Unclear | No information was provided. |
| Blinding? | Yes | Described as “double-blind”. |
| All outcomes | Placebo-controlled: “the placebo was comparable to cefuroxime in both appearance and viscosity of solution” | |
| Incomplete outcome data addressed? | Yes | No loss to follow up. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | Insufficient information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT, 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: August 1989 - July 1990. | |
| Setting: Jos Universtiy Teaching Hospitla, Jos, Nigeria. | ||
| Inclusion criteria: healthy women scheduled for elective CS. | ||
| Exclusion criteria: labor, premature rupture of membranes, uncontrolled diabetes melli-tus, sickle cell disease | ||
| Interventions | Augmentin (amoxicillin-clavulanic acid) 1.2 g IV intraoperatively by the anesthetist vs placebo (10 cc normal saline) | |
| Outcomes | Febrile morbidity, wound erythema or induration, seropurulent discharge, pneumonia | |
| Notes | Developing country. | |
| Class of antibiotic:Beta-lactam/beta-lactamase inhibitor combination | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “Using a random list of numbers.” |
| Allocation concealment? | Unclear | “Randomization was performed by the nurse in charge of the antenatal ward using a random number list.” |
| Blinding? | Unclear | Placebo-controlled. |
| All outcomes | Insufficient information to judge whether there was blinding of study personnel | |
| Incomplete outcome data addressed? All outcomes | Yes | No loss of participants to follow up. |
| No participant excluded after randomization. | ||
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “They were well matched for the (patient characteristics) considered .. and equally well matched for (preoperative, intraoperative and post-operative) variables.” Insufficient information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear and allocation concealment not adequate. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: July 1-September 1988. | |
| Setting: Coah, Mexico. | ||
| Inclusion criteria: women undergoing urgent CS. | ||
| Exclusion: fever, chorioamnionitis, penicil weeks lin allergy, antibiotic treatment in prior 2 | ||
| Interventions | Ampicillin 2 g IV every 4 hours × 3 after cl; amping of cord (N = 59) vs no treatment | |
| Outcomes | Febrile syndrome; wound infection; abdominal wall abscess; endometritis | |
| Notes | No definitions of outcomes provided. | |
| Class of antibiotic: Aminopenicillin (ampicillin). | ||
| Subgroups: | ||
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Allocated “in random form” using a random table. |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | Not placebo-controlled. No additional information provided. |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No losses or exclusions were reported. Analysis appears to be ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | Insufficient information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT: 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: Not specified. | |
| Setting: Miami, Florida, US. Mostly low-income or indigent Negro women from ghetto areas of large metropolitan area | ||
| Inclusion criteria: women undergoing primary CS after the onset of labor | ||
| Exclusion criteria: none specified. | ||
| Interventions | Penicillin G 2 million units IV every 4 hours and kanamycin 500 mg IM every 12 hours as soon as it was decided to perform a CS, at the time of operation or immediately postoperatively and continued for a minimum of 3 days post-operatively (N = 40) vs no treatment (N = 40) | |
| Outcomes | Febrile morbidity (temperature of > 100.3°F on any 2 days after first 24 hours); UTI, endometritis and wound infection (not defined); maternal length of stay (treatment 5.8 days vs 8.7 days for control group, no variance given) | |
| Notes | 1 patient receiving penicillin had a drug rash on the third day | |
| Class of antibiotic: penicillin and aminoglycoside. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “selected at random.” |
| Allocation concealment? | Unclear | Insufficient information to judge. |
| Blinding? | Unclear | No blinding. |
| All outcomes | Not placebo controlled. | |
| Incomplete outcome data addressed? | Yes | No loss of participants to follow up. |
| All outcomes | No participant excluded after randomization. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | “The clinical material in both groups was identical.” Insufficient other information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection: January 1975-January 1977. | |
| Setting: Los Angeles County-University of Southern California Medical Center, Los Angeles, California, US, 87% Hispanic or Black | ||
| Inclusion criteria: women in labor with ruptured membranes who underwent internal fetal monitoring (classified as non-elective) | ||
| Exclusion: fever, other antibiotic use, penicillin allergy. | ||
| Interventions | Cefazolin 1 g IV after the cord was clamped and at 4-6 hours and 10-12 hours postoperatively (N = 48) vs placebo (N = 45) | |
| Outcomes | Standard temperature morbidity, endomyometritis, abdominal wound infection, urinary infections (no definitions provided for any outcomes) | |
| Notes | 2 women were said to develop a serious infection: 1 (cefazolin group) developed septic thrombophlebitis and is included as a serious outcome; the other (placebo group) was treated with antibiotics for prolonged fever (judged not to be a serious outcome for this review) | |
| Class of antibiotic: first generation cephalosporin. | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomized to numbered packages.” No further information. |
| Allocation concealment? | Yes | “… the agents having been randomized to numbered packages by the pharmacy department.” |
| Blinding? | Yes | Double blind study, placebo controlled; similar quantity of placebo given |
| All outcomes | ||
| The physician caring for the patient did not know which agent his patient received | ||
| Incomplete outcome data addressed? | Unclear | No loss to follow up reported. |
| All outcomes | 7 women initially randomized not included in final analysis because they did not meet all the criteria (allocated group unknown) ITT analysis not performed. | |
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 patient groups reported as similar. Insufficient information overall |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | RCT; 2 parallel groups. | |
| Unit of randomization: individual. | ||
| Participants | Dates of data collection; not reported. | |
| Setting: University of Michigan Medical Center, Ann Arbour, Michigan, US | ||
| Inclusion criteria: women in labor. | ||
| Exclusion criteria: acute bleeding due to abruptio placentae, infection on treatment; abnormal renal function, penicillin allergy | ||
| Interventions | Cephalothin 2 g IV within 1 hour of operation and at 4 and 8 hours after (N = 40) vs comparable appearing placebo (N = 40) | |
| Outcomes | Febrile morbidity (oral temperature > 100.3°F twice 6 hours apart); infection of endometrium, urinary tract and wound (definitions not provided); fever index (40 degree hours for treatment group vs 83 for placebo group) | |
| Notes | Class of antibiotic: first generation cephalosporin. | |
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Selected in random …manner”. No further information provided. |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Yes | Double blind, placebo controlled. |
| All outcomes | “The placebo was comparable to the cephalothin in both appearance and viscosity of solution.” | |
| Incomplete outcome data addressed? | Unclear | No loss to follow up or exclusion of participants after randomization described, but results of only 80/85 participants reported Insufficient detail to know if the analysis was ITT. |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable, but insufficient information overall |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized into 3 groups (irrigation vs systemic treatment vs no treatment) | |
| Participants | Dates of data collection: May 1988 - August 1989. | |
| Setting: Beijing, China. | ||
| Inclusion criteria: women undergoing both elective (N = 112) and non-elective (N = 105) CS. Only women undergoing an elective CS were randomized to treatment or no treatment and have been included in analysis | ||
| Interventions | Local irrigation with ampicillin 6 g after delivery of the placenta (N = 39) vs penicillin 5. 6 MU and gentamicin 240,000 U IV immediately after surgery and penicillin 1.6 MU and gentamicin 160,000 U per day IM × 3 days (N = 41) vs no treatment (N = 32). Treatment groups combined | |
| Outcomes | Endometritis (presence of any 2 of following: temperature above 37.5° C, uterine tenderness, foul vaginal discharge); abdominal wound infection (cellulitis with small amount ofexudate within 2 months ofoperation); uterine incision infection (associated with late postpartum haemorrhage); fever index | |
| Notes | Women undergoing non-elective sections randomized to either treatment group (not included in this review) | |
| Class of antibiotic: Penicillin and aminoglycoside or aminopenicillin (ampicillin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “… randomized…” |
| Allocation concealment? | Unclear | No information provided. |
| Blinding? | Unclear | No information provided. |
| All outcomes | ||
| Incomplete outcome data addressed? | Unclear | No losses or exclusions were reported. Analysis appears to be ITT |
| All outcomes | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | Insufficient information to judge. |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, placebo controlled; 2 parallel groups. | |
| Participants | Date of data collection: not reported. | |
| Setting: Prince of Wales Hospital, Hong Kong. | ||
| Inclusion criteria: women undergoing CS. | ||
| Exclusion criteria: penicillin allergy, current antibiotic use, fever, receipt of steroid injection | ||
| Interventions | Augmentin 1.2 g (amoxycillin sodium 1000 mg and clavulanate potassium 200 mg) in 10 ml saline (N = 160) vs saline placebo (N = 160) | |
| Outcomes | Febrile morbidity (2 oral temperatures > 37.9°C at least 6 hours apart after first 24 hours); bacteriuria at day 3 (classified in this review as UTI); wound infection (purulent discharge, cellulitis, tenderness and wound abscess requiring incision and drainage); endometritis (fever, pelvic pain, uterine tenderness, purulent vaginal discharge without signs of infection in the lower genital tract); duration of hospital stay | |
| Notes | Sub-rectus Redivac drain routinely inserted. | |
| Class ofantibiotic: Beta-lactam/beta-lactamase inhibitor combination | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomized.” |
| No further information reported. | ||
| Allocation concealment? | Unclear | Assigned by the anesthetist in a randomized, double-blind manner; placebo-controlled |
| Blinding? | Unclear | Placebo-controlled (10 ml normal saline). Described as “double-blind”. Treatment assigned by anesthetist |
| All outcomes | ||
| Incomplete outcome data addressed? | Yes | No loss to follow up reported. |
| All outcomes | No patients excluded from analysis. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age, weight, parity, duration oflabor, birth-weight, etc. There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
| Methods | Randomized, placebo-controlled trial; 2 parallel groups. | |
| Unit of randomization; individual. | ||
| Participants | Dates of data collection: May 1978-July 1979. | |
| Setting: Los Angeles County-University of Southern California Medical Center, Los Angeles, California, US. | ||
| Predominantly (91%) Hispanic or Black. | ||
| Inclusion criteria: women in labor with an intrauterine pressure catheter and fetal scalp electrode (non-elective) | ||
| Exclusion criteria: fever, significant systemic disease. | ||
| Interventions | Cefoxitin 1 g IV at time of cord clamping and at 4 and 8 hours (N = 50) vs matching placebo (N = 50) | |
| Outcomes | Endomyometritis, abdominal wound infection, serious complications; duration of maternal hospital stay (treatment 5.1 days vs control 5.9 days, not statistically significant, no variance given) | |
| Notes | 1 case of septic pelvic thrombophlebitis occurred in the treatment group; there were 8 episodes of bacteremia in the control group vs 1 in the treatment group; both outcomes combined under serious morbidity | |
| Class of antibiotic: second generation cephalosporin (cefamycin) | ||
Subgroups:
|
||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | “Randomly assigned.” |
| No additional information. | ||
| Allocation concealment? | Unclear | No information was provided. |
| Blinding? | Yes | Placebo-controlled; “similarly appearing placebo”. |
| All outcomes | ||
| “the physician team did not know which medication the patient was to receive.” | ||
| Incomplete outcome data addressed? | Yes | No loss to follow up reported. |
| All outcomes | No participants excluded. | |
| ITT analysis. | ||
| Free of selective reporting? | Unclear | Insufficient information to judge. |
| Free of other bias? | Unclear | The 2 groups were comparable regarding age and race.There was insufficient other information which to judge |
| Overall low risk of bias? | Unclear | Mostly unclear. |
C: centigrade
CS: cesarean section
hr: hour/hours
IM: intramuscularly
ITT: intention to treat
IV: intravenously
MU: million units
q 6 hrs: every 6 hours
SD/sd: standard deviation
vs: versus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Andrews 2003 | All participants received prophylaxis with cefotetan after cord clamping and were then randomized to receive doxycycline plus azithromycin vs placebo |
| Cormier 1988 | Did not include women undergoing cesarean section. |
| Creatsas 1980 | Not relevant to this review. Ampicillin or gentamycin given prior to cesarean section in women with intrauterine infection, to measure transplacental transfer. No control group, and no clinical outcomes given |
| De Palma 1980 | Women at high risk (membranes ruptured for more than 6 hours) initially were randomized to early treatment (ie prophylactic therapy continued for 4 days) vs standard treatment (i.e. treatment only started when infection apparent). When the results were compared midway through the study, standard therapy was abandoned. The results for the 2 groups prior to abandoning the no treatment group could not be obtained from the paper |
| Elliott 1982 | Only the first 42 women were randomized to placebo or active treatment; after that a significant difference was observed between the placebo and treated groups and the placebo arms were discontinued. Further women were randomized to 2 different active treatments. The data for the first part of the study (with only the first 42 women) are not available from the published paper |
| Harrigill 2003 | Women were randomized to normal saline intraabdominal irrigation vs no irrigation. All patients received cefazolin at the time of cord clamping |
| Itskovitz 1979 | Not all women were randomly allocated to treatment or no treatment. 150 women were assigned at random to each of the 2 wings of the department according to the day of their admission, each wing receiving women on alternate days. In both wings, of the last 50 women every second woman served as a control. 50 women in 1 wing received IV cephalothin or oral cephalexin, 50 women in the other wing received IV or oral ampicillin. The first 50 women enrolled were all treated; separate results for the last 100 women (who were alternately allocated therapy or no treatment) are not available |
| Kreutner 1979 | After approximately 70% of the planned study population had been randomized to placebo or 1 of 2 active treatment groups, an unacceptably high morbidity rate in the placebo group was confirmed and the placebo arm was discontinued. Further women were randomized to two different active treatments. The data for the first part of the study when women were randomized to treatment or placebo are not available from the published paper |
| Louie 1982 | Eligible women were in active labor with ruptured membranes. While this study initially included a placebo control group, this group was dropped after 30 women had been enrolled on the basis ofethical considerations about assigning women to a non-treatment group in which the likelihood of morbidity was high. Only 7 women (out of a total of 195 women entered) were randomized to placebo, separate results on the initial part of the study not available. The placebo (7) and treatment groups (188) were very imbalanced making a meaningful comparison between groups impossible |
| Pawelec 1994 | Abstract only; unable to confirm random allocation and method of allocation to no treatment group; data for separate outcomes of endometritis and wound infection not provided |
| Petersen 1985 | No numerical data. |
| Pitt 2001 | Women were randomized to receive intravaginal metronidazole or placebo gel during labor; most, but not all patients also received 1 prophylactic dose of cefazolin after cord clamping |
| Roex 1987 | No clinical outcomes. |
| Sanchez-Ramos 1999 | Patients were randomized to metronidazole gel intravaginally or matching placebo, but most patients also received prophylactic antibiotics after cord clamping |
| Sengupta 1976 | In this study, in which women were alternately allocated to antibiotic prophylaxis or no treatment, the women enrolled were undergoing both gynaecological and obstetrical surgery. Rates ofinfectious complications are given for all abdominal surgery (cesarean section, abdominal hysterectomy and laparotomy). Data specifically on the women who underwent cesarean section are, however, not available from the published study |
| Skryten 1988 | Abstract only. Rates for all post-operative infection morbidity and clinically significant genital tract-related infections (wound infections, endometritis) and abscess formation (septicemia) combined; rates for individual outcomes not provided |
| Spreafico 1987 | Results combined from 3 time periods. In only 1 period did it appear women were randomized to antibiotic therapy or no treatment; results just for this period not available in published report |
| Voto 1986 | All women received antibiotics (randomized to cefoxitin after cord clamping and then every fours hours x 2 or oral ampicillin 2 g daily x 7 days); no clinical outcomes reported |
| Wallace 1984 | This was not a randomized trial of antibiotic prophylaxis. 3 distinct groups of women were studied: 1 group was part of randomized trial that compared extracorporeal cesarean section with prophylactic antibiotic; the second group received extracorporeal cesarean section and no antibiotics; the third group received extracor-poreal cesarean section with antibiotics (the decision to administer antibiotics in the latter 2 groups was at the discretion of the physician) |
| Wells 1994 | Absolute numbers cannot be calculated from data provided in abstract; no published version of this study identified |
IV: intravenous
vs: versus
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Being translated. |
DATA AND ANALYSES
Comparison 1. Antibiotic prophylaxis versus no antibiotic prophylaxis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Maternal febrile morbidity/fever | 50 | 8141 | Risk Ratio (M-H, Random, 95% CI) | 0.45 [0.39, 0.51] |
| 2 Maternal wound infection | 77 | 11961 | Risk Ratio (M-H, Random, 95% CI) | 0.39 [0.32, 0.48] |
| 3 Maternal endometritis | 79 | 12142 | Risk Ratio (M-H, Fixed, 95% CI) | 0.38 [0.34, 0.42] |
| 4 Maternal serious infectious complications | 31 | 5047 | Risk Ratio (M-H, Fixed, 95% CI) | 0.31 [0.19, 0.48] |
| 5 Infant immediate adverse effects | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 6 Infant oral thrush | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 7 Maternal urinary tract infection | 61 | 9454 | Risk Ratio (M-H, Fixed, 95% CI) | 0.55 [0.47, 0.65] |
| 8 Maternal adverse effects | 13 | 2131 | Risk Ratio (M-H, Fixed, 95% CI) | 2.43 [1.00, 5.90] |
| 9 Maternal days in hospital | 17 | 3199 | Mean Difference (IV, Random, 95% CI) | −0.49 [−0.68, −0.29] |
| 10 Infant days in hospital | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 11 Infant long-term adverse effects | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 12 Infant’s immune system development | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 13 Development of bacterial resistance | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 14 Costs | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
Comparison 2. Antibiotics versus no antibiotics - subgroup by type of cesarean section.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Maternal febrile morbidity/fever | 50 | 8141 | Risk Ratio (M-H, Random, 95% CI) | 0.45 [0.40, 0.51] |
| 1.1 Elective cesarean section | 15 | 2433 | Risk Ratio (M-H, Random, 95% CI) | 0.50 [0.37, 0.68] |
| 1.2 Non-elective cesarean section | 15 | 1951 | Risk Ratio (M-H, Random, 95% CI) | 0.41 [0.31, 0.52] |
| 1.3 Both elective and non-elective, or undefined cesarean section | 24 | 3757 | Risk Ratio (M-H, Random, 95% CI) | 0.46 [0.38, 0.55] |
| 2 Maternal wound infection | 77 | 11961 | Risk Ratio (M-H, Random, 95% CI) | 0.40 [0.33, 0.49] |
| 2.1 Elective cesarean section | 15 | 2433 | Risk Ratio (M-H, Random, 95% CI) | 0.62 [0.44, 0.88] |
| 2.2 Non-elective cesarean section | 20 | 2458 | Risk Ratio (M-H, Random, 95% CI) | 0.41 [0.27, 0.63] |
| 2.3 Both elective and non-elective, or undefined cesarean section | 46 | 7070 | Risk Ratio (M-H, Random, 95% CI) | 0.35 [0.27, 0.46] |
| 3 Maternal endometritis | 79 | 12142 | Risk Ratio (M-H, Fixed, 95% CI) | 0.38 [0.34, 0.42] |
| 3.1 Elective cesarean section | 14 | 2398 | Risk Ratio (M-H, Fixed, 95% CI) | 0.39 [0.24, 0.65] |
| 3.2 Non-elective cesarean section | 21 | 2537 | Risk Ratio (M-H, Fixed, 95% CI) | 0.40 [0.33, 0.47] |
| 3.3 Both elective and non-elective, or undefined cesarean section | 48 | 7207 | Risk Ratio (M-H, Fixed, 95% CI) | 0.36 [0.32, 0.42] |
| 4 Maternal serious infectious complications | 31 | 5047 | Risk Ratio (M-H, Fixed, 95% CI) | 0.31 [0.20, 0.48] |
| 4.1 Elective cesarean section | 4 | 545 | Risk Ratio (M-H, Fixed, 95% CI) | 1.01 [0.04, 24.21] |
| 4.2 Non-elective cesarean section | 7 | 923 | Risk Ratio (M-H, Fixed, 95% CI) | 0.31 [0.14, 0.69] |
| 4.3 Both elective and non-elective, or undefined cesarean section | 22 | 3579 | Risk Ratio (M-H, Fixed, 95% CI) | 0.30 [0.17, 0.52] |
| 5 Infant immediate adverse effects | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 5.1 Elective cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 5.2 Non-elective cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 5.3 Both elective and non-elective, or undefined cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 6 Infant oral thrush | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 6.1 Elective cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 6.2 Non-elective cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 6.3 Both elective and non-elective, or undefined cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 7 Maternal urinary tract infection | 61 | 9454 | Risk Ratio (M-H, Fixed, 95% CI) | 0.56 [0.48, 0.65] |
| 7.1 Elective cesarean section | 11 | 1832 | Risk Ratio (M-H, Fixed, 95% CI) | 0.90 [0.55, 1.48] |
| 7.2 Non-elective cesarean section | 17 | 2148 | Risk Ratio (M-H, Fixed, 95% CI) | 0.41 [0.29, 0.57] |
| 7.3 Both elective and non-elective, or undefined cesarean section | 37 | 5474 | Risk Ratio (M-H, Fixed, 95% CI) | 0.58 [0.48, 0.70] |
| 8 Maternal adverse effects | 13 | 2131 | Risk Ratio (M-H, Fixed, 95% CI) | 2.43 [1.00, 5.90] |
| 8.1 Elective cesarean section | 2 | 235 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 8.2 Non-elective cesarean section | 5 | 808 | Risk Ratio (M-H, Fixed, 95% CI) | 2.86 [0.61, 13.31] |
| 8.3 Both elective and non-elective, or undefined cesarean section | 6 | 1088 | Risk Ratio (M-H, Fixed, 95% CI) | 2.23 [0.75, 6.63] |
| 9 Maternal days in hospital | 17 | 3199 | Mean Difference (IV, Random, 95% CI) | −0.49 [−0.68, −0.29] |
| 9.1 Elective cesarean section | 5 | 1065 | Mean Difference (IV, Random, 95% CI) | −0.45 [−0.71, −0.19] |
| 9.2 Non-elective cesarean section | 3 | 586 | Mean Difference (IV, Random, 95% CI) | −0.45 [−0.77, −0.13] |
| 9.3 Both elective and non-elective, or undefined cesarean section | 10 | 1548 | Mean Difference (IV, Random, 95% CI) | −0.54 [−0.88, −0.19] |
| 10 Infant days in hospital | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 10.1 Elective cesarean section | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 10.2 Non-elective cesarean section | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 10.3 Both elective and non-elective, or undefined cesarean section | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 11 Infant long-term adverse effects | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 11.1 Elective cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 11.2 Non-elective cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 11.3 Both elective and non-elective, or undefined cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 12 Infant’s immune system development | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 12.1 Elective cesarean section | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 12.2 Non-elective cesarean section | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 12.3 Both elective and non-elective, or undefined cesarean section | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 13 Development of bacterial resistance | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 13.1 Elective cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 13.2 Non-elective cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 13.3 Both elective and non-elective, or undefined cesarean section | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 14 Costs | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 14.1 Elective cesarean section | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 14.2 Non-elective cesarean section | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 14.3 Both elective and non-elective, or undefined cesarean section | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
Comparison 3. Antibiotics versus no antibiotics - subgroup by timing of administration.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Maternal febrile morbidity/fever | 50 | 8141 | Risk Ratio (M-H, Random, 95% CI) | 0.45 [0.39, 0.51] |
| 1.1 Before cord clamping | 23 | 3195 | Risk Ratio (M-H, Random, 95% CI) | 0.51 [0.43, 0.60] |
| 1.2 After cord clamping | 22 | 4555 | Risk Ratio (M-H, Random, 95% CI) | 0.43 [0.35, 0.52] |
| 1.3 Timing not defined | 5 | 391 | Risk Ratio (M-H, Random, 95% CI) | 0.25 [0.14, 0.44] |
| 2 Maternal wound infection | 77 | 11961 | Risk Ratio (M-H, Random, 95% CI) | 0.39 [0.32, 0.48] |
| 2.1 Before cord clamping | 35 | 4978 | Risk Ratio (M-H, Random, 95% CI) | 0.40 [0.30, 0.55] |
| 2.2 After cord clamping | 38 | 6598 | Risk Ratio (M-H, Random, 95% CI) | 0.39 [0.30, 0.51] |
| 2.3 Timing not defined | 5 | 385 | Risk Ratio (M-H, Random, 95% CI) | 0.29 [0.07, 1.24] |
| 3 Maternal endometritis | 79 | 12142 | Risk Ratio (M-H, Fixed, 95% CI) | 0.38 [0.34, 0.42] |
| 3.1 Before cord clamping | 31 | 4410 | Risk Ratio (M-H, Fixed, 95% CI) | 0.33 [0.27, 0.41] |
| 3.2 After cord clamping | 44 | 7323 | Risk Ratio (M-H, Fixed, 95% CI) | 0.40 [0.35, 0.46] |
| 3.3 Timing not defined | 5 | 409 | Risk Ratio (M-H, Fixed, 95% CI) | 0.30 [0.18, 0.50] |
| 4 Maternal serious infectious complications | 31 | 5047 | Risk Ratio (M-H, Fixed, 95% CI) | 0.31 [0.19, 0.48] |
| 4.1 Before cord clamping | 12 | 1639 | Risk Ratio (M-H, Fixed, 95% CI) | 0.27 [0.11, 0.67] |
| 4.2 After cord clamping | 18 | 3337 | Risk Ratio (M-H, Fixed, 95% CI) | 0.32 [0.18, 0.55] |
| 4.3 Timing not defined | 1 | 71 | Risk Ratio (M-H, Fixed, 95% CI) | 0.36 [0.04, 3.32] |
| 5 Infant immediate adverse effects | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 5.1 Administered before cord clamping | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 5.2 Administered after cord clamping | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 5.3 Timing of administration not defined | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 6 Infant oral thrush | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 6.1 Administered before cord clamping | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 6.2 Administered after cord clamping | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 6.3 Timing of administration not defined | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 7 Maternal urinary tract infections | 61 | 9454 | Risk Ratio (M-H, Fixed, 95% CI) | 0.55 [0.47, 0.64] |
| 7.1 Before cord clamping | 28 | 3828 | Risk Ratio (M-H, Fixed, 95% CI) | 0.57 [0.46, 0.71] |
| 7.2 After cord clamping | 30 | 5276 | Risk Ratio (M-H, Fixed, 95% CI) | 0.55 [0.43, 0.71] |
| 7.3 Timing not defined | 4 | 350 | Risk Ratio (M-H, Fixed, 95% CI) | 0.36 [0.18, 0.75] |
| 8 Maternal adverse effects | 13 | 2131 | Risk Ratio (M-H, Fixed, 95% CI) | 2.43 [1.00, 5.90] |
| 8.1 Before cord clamping | 2 | 339 | Risk Ratio (M-H, Fixed, 95% CI) | 2.96 [0.12, 71.38] |
| 8.2 After cord clamping | 8 | 1617 | Risk Ratio (M-H, Fixed, 95% CI) | 2.44 [0.88, 6.75] |
| 8.3 Timing not defined | 3 | 175 | Risk Ratio (M-H, Fixed, 95% CI) | 2.17 [0.24, 19.70] |
| 9 Maternal days in hospital | 17 | 3199 | Mean Difference (IV, Random, 95% CI) | −0.49 [−0.68, −0.29] |
| 9.1 Before cord clamping | 6 | 1000 | Mean Difference (IV, Random, 95% CI) | −0.63 [−1.18, −0.09] |
| 9.2 After cord clamping | 9 | 2093 | Mean Difference (IV, Random, 95% CI) | −0.40 [−0.58, −0.23] |
| 9.3 Timing not defined | 2 | 106 | Mean Difference (IV, Random, 95% CI) | −0.87 [−1.53, −0.20] |
| 10 Infant days in hospital | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 10.1 Administration before cord clamping | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 10.2 Administration after cord clamping | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 10.3 Timing of administration not defined | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 11 Infant long-term adverse effects | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 11.1 Administered before cord clamping | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 11.2 Administered after cord clamping | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 11.3 Timing of administration not defined | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 12 Infant’s immune system development | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 12.1 Administration before cord clamping | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 12.2 Administration after cord clamping | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 12.3 Timing of administration not defined | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 13 Develoment of bacterial resistance | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 13.1 Administered before cord clamping | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 13.2 Administered after cord clamping | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 13.3 Timing of administration not defined | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 14 Costs | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 14.1 Administration before cord clamping | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 14.2 Administration after cord clamping | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 14.3 Timing of administration not defined | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
Analysis 1.1. Comparison 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, Outcome 1 Maternal febrile morbidity/fever.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis
Outcome: 1 Maternal febrile morbidity/fever
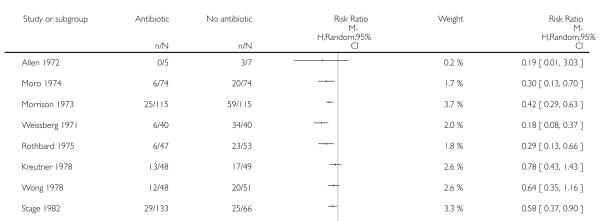 |
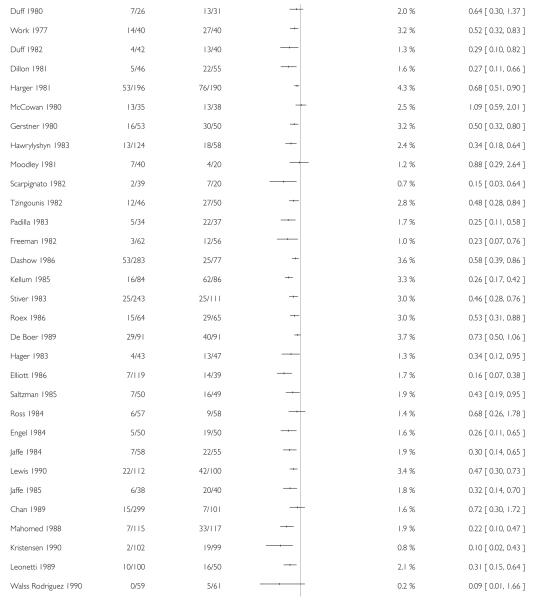 |
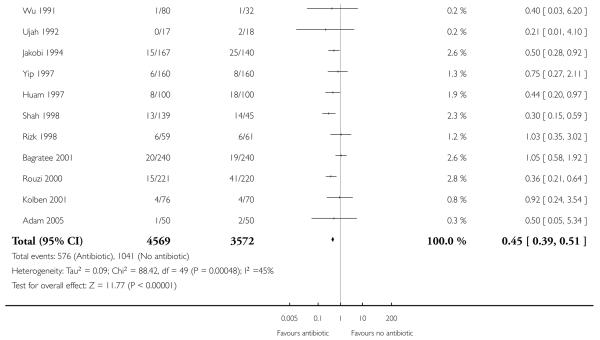 |
Analysis 1.2. Comparison 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, Outcome 2 Maternal wound infection.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis
Outcome: 2 Maternal wound infection
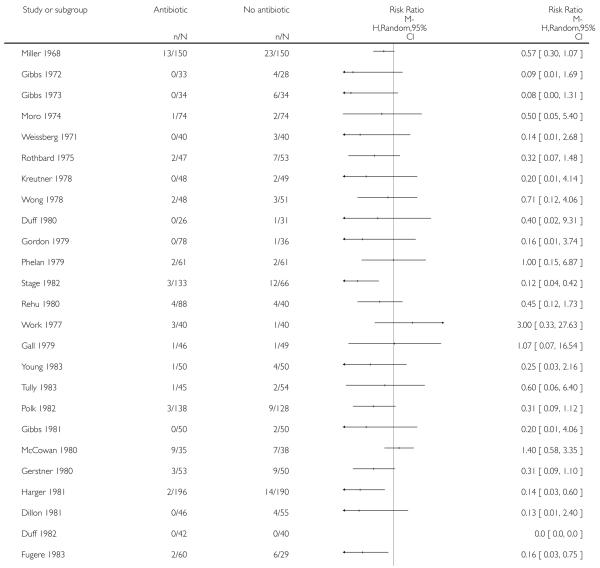 |
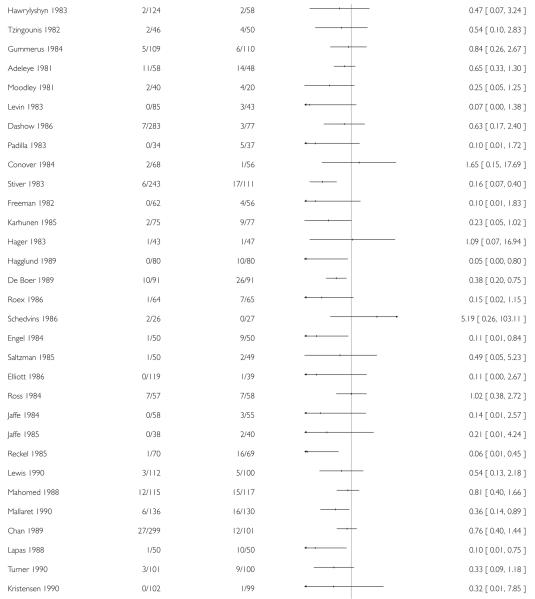 |
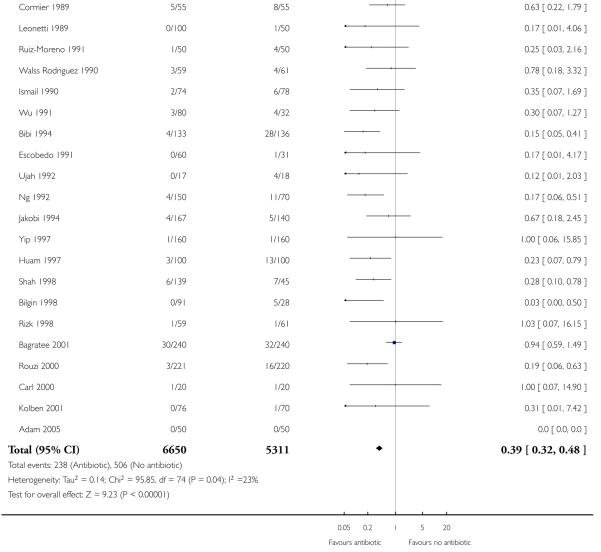 |
Analysis 1.3. Comparison 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, Outcome 3 Maternal endometritis.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis
Outcome: 3 Maternal endometritis
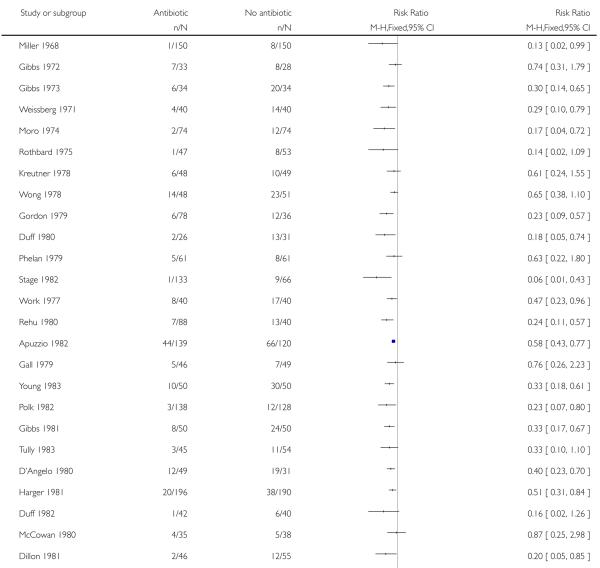 |
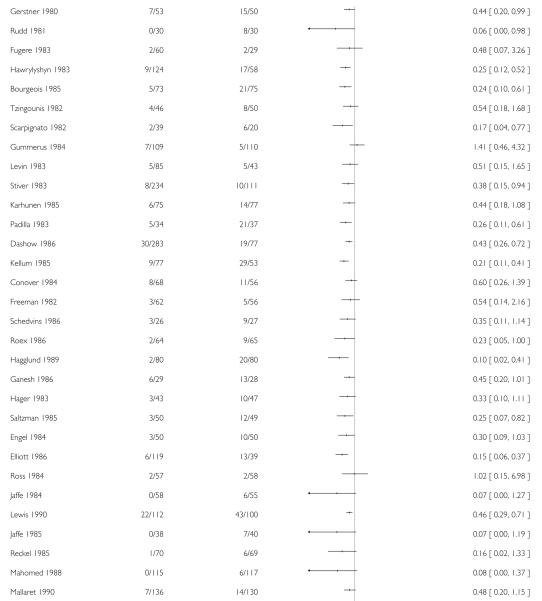 |
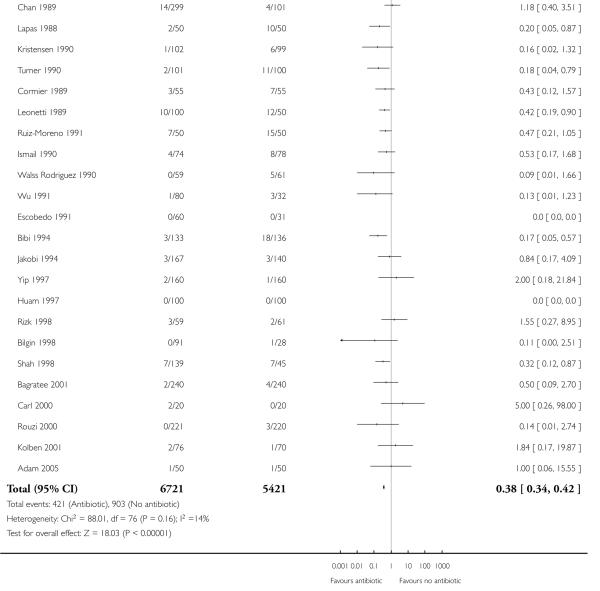 |
Analysis 1.4. Comparison 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, Outcome 4 Maternal serious infectious complications.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis
Outcome: 4 Maternal serious infectious complications
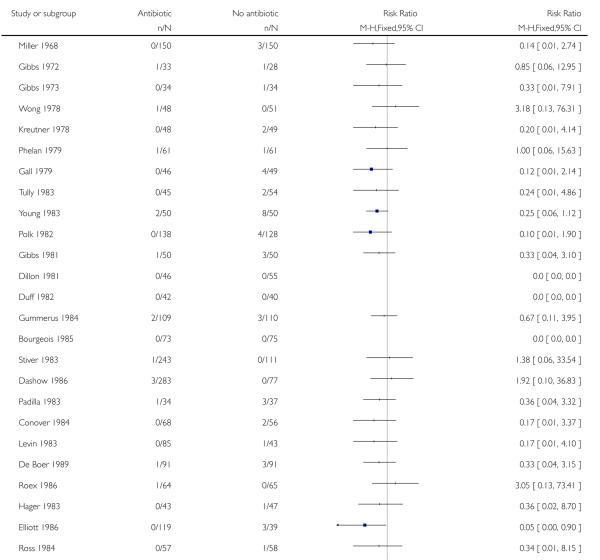 |
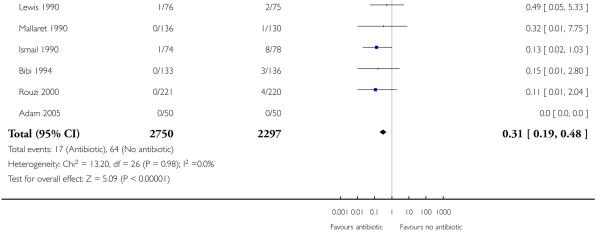 |
Analysis 1.7. Comparison 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, Outcome 7 Maternal urinary tract infection.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis
Outcome: 7 Maternal urinary tract infection
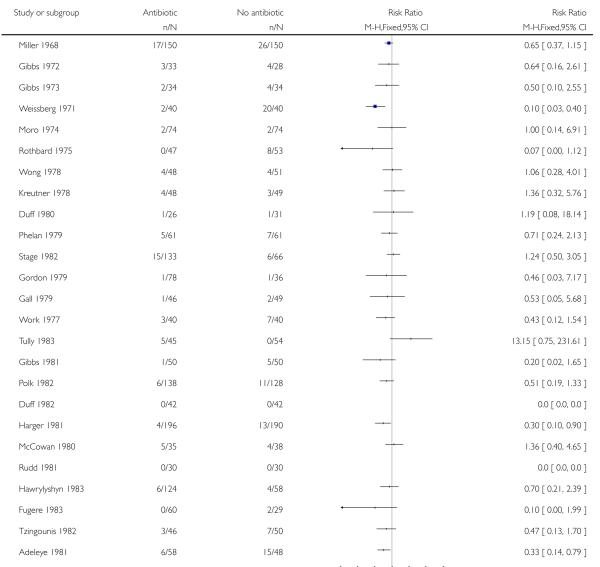 |
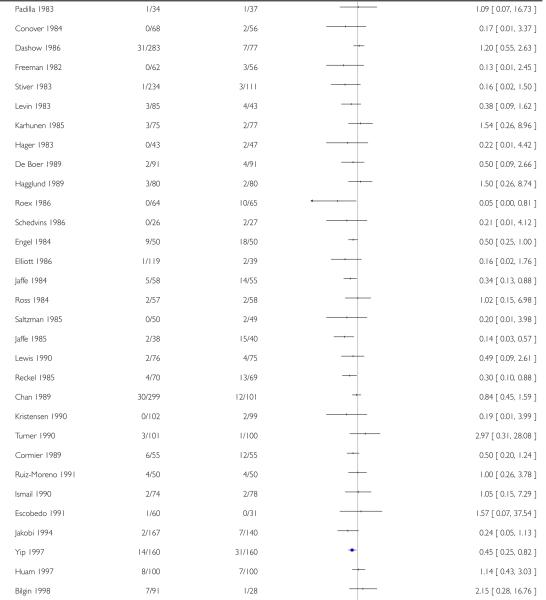 |
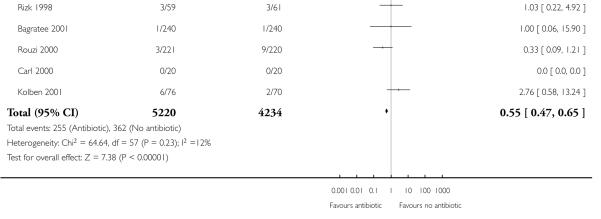 |
Analysis 1.8. Comparison 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, Outcome 8 Maternal adverse effects.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis
Outcome: 8 Maternal adverse effects
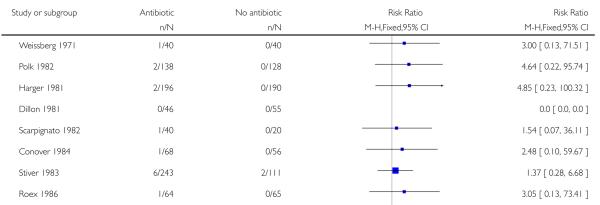 |
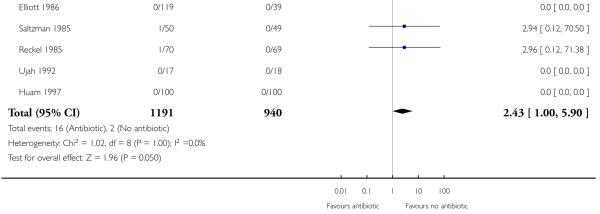 |
Analysis 1.9. Comparison 1 Antibiotic prophylaxis versus no antibiotic prophylaxis, Outcome 9 Maternal days in hospital.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 1 Antibiotic prophylaxis versus no antibiotic prophylaxis
Outcome: 9 Maternal days in hospital
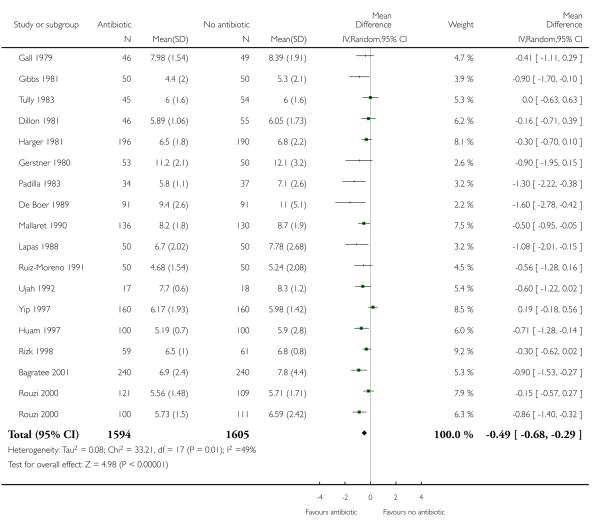 |
Analysis 2.1. Comparison 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section, Outcome 1 Maternal febrile morbidity/fever.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section
Outcome: 1 Maternal febrile morbidity/fever
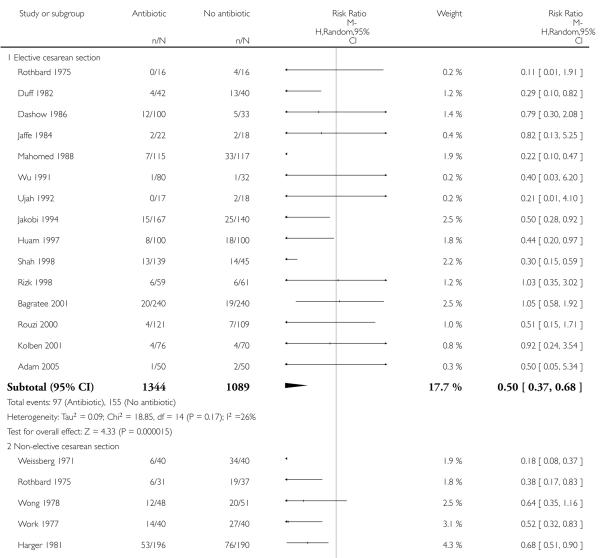 |
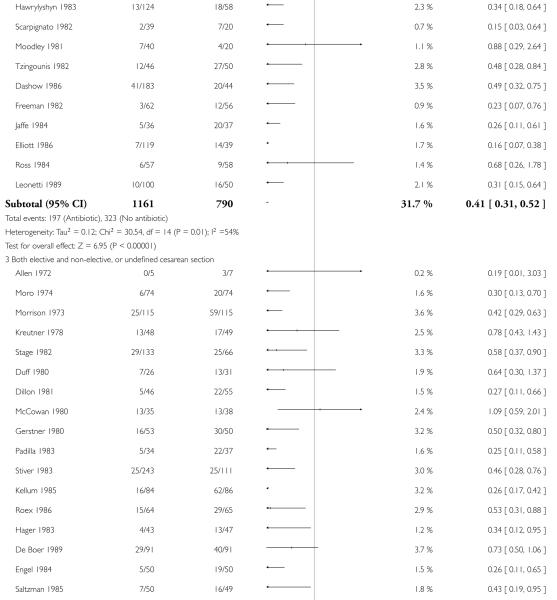 |
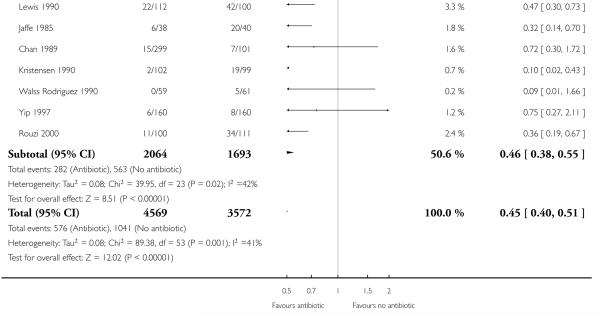 |
Analysis 2.2. Comparison 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section, Outcome 2 Maternal wound infection.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section
Outcome: 2 Maternal wound infection
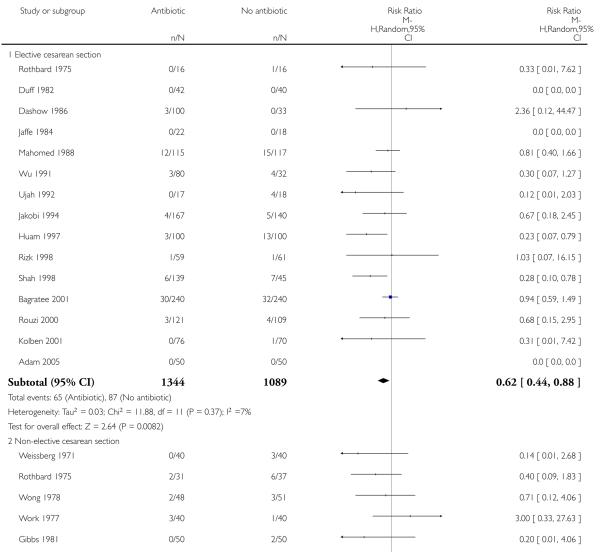 |
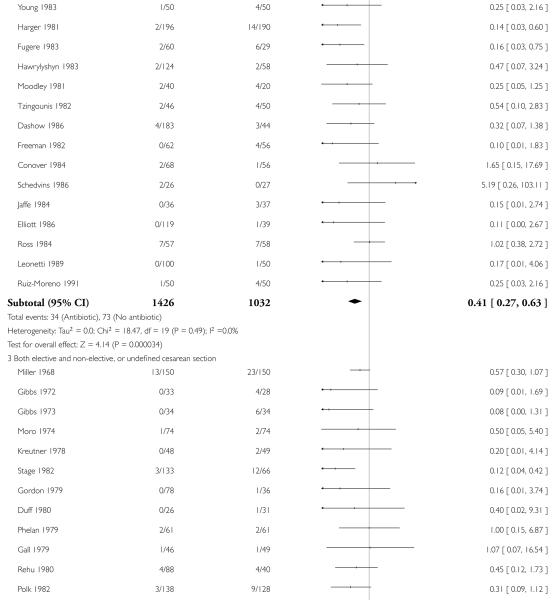 |
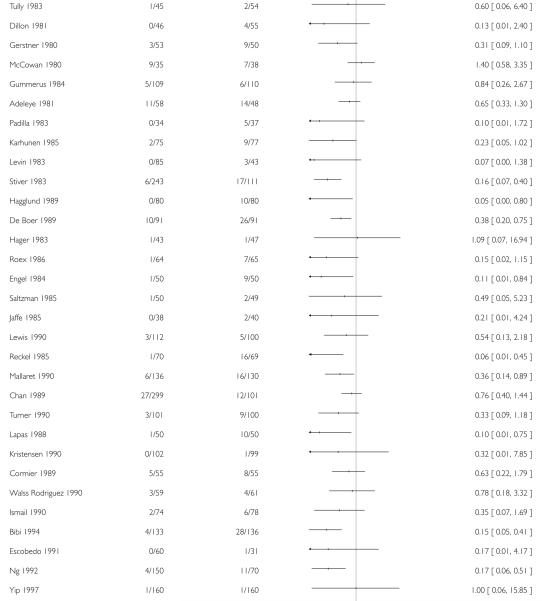 |
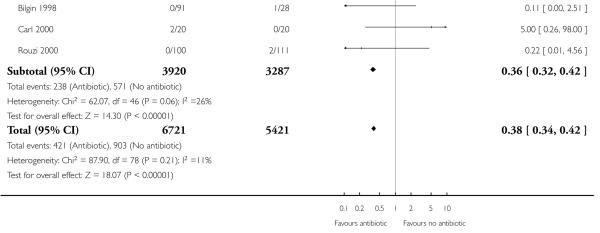 |
Analysis 2.3. Comparison 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section, Outcome 3 Maternal endometritis.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section
Outcome: 3 Maternal endometritis
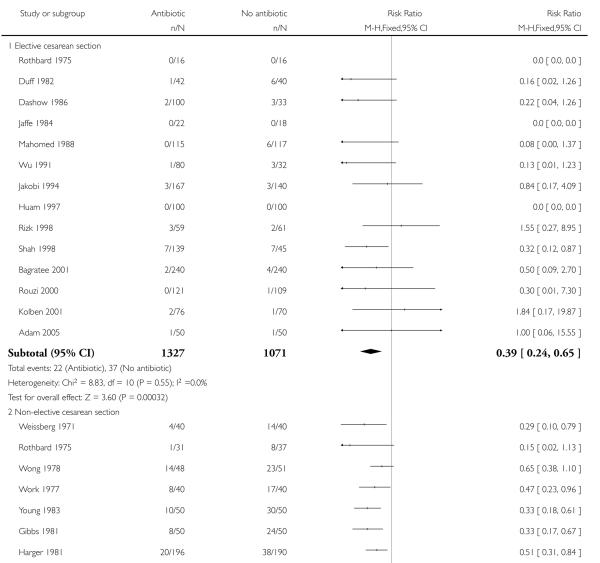 |
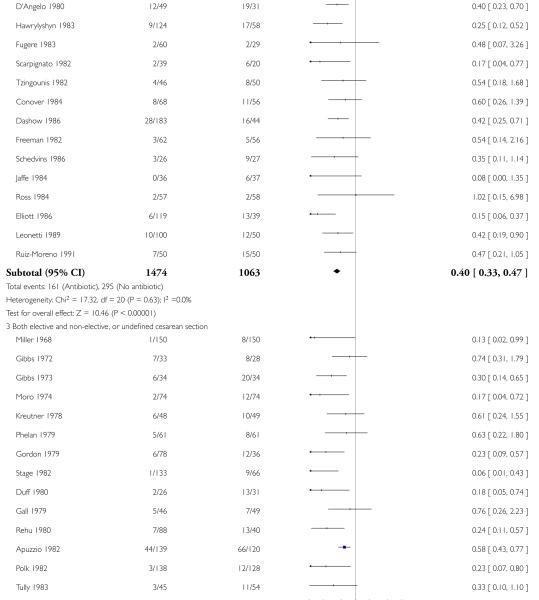 |
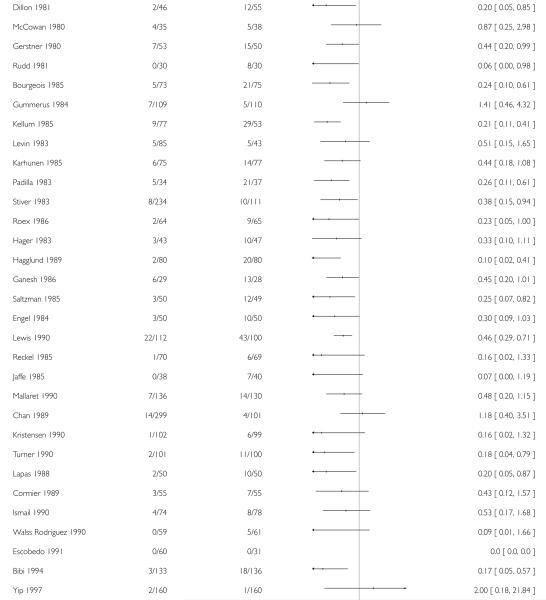 |
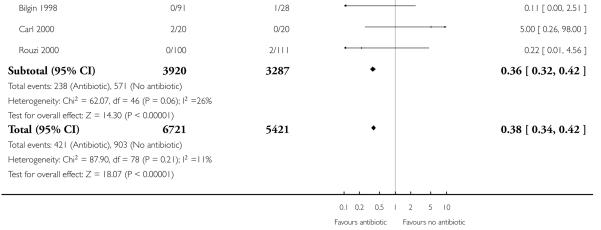 |
Analysis 2.4. Comparison 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section, Outcome 4 Maternal serious infectious complications.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section
Outcome: 4 Maternal serious infectious complications
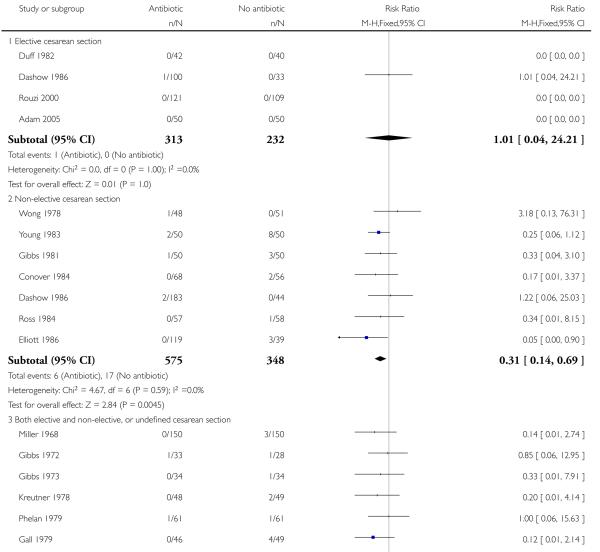 |
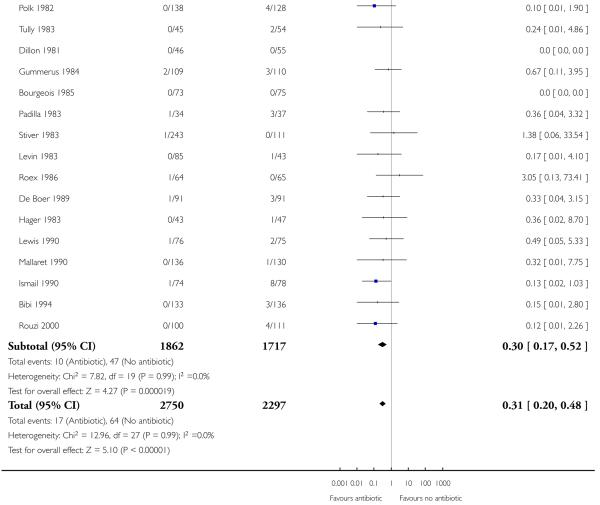 |
Analysis 2.7. Comparison 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section, Outcome 7 Maternal urinary tract infection.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section
Outcome: 7 Maternal urinary tract infection
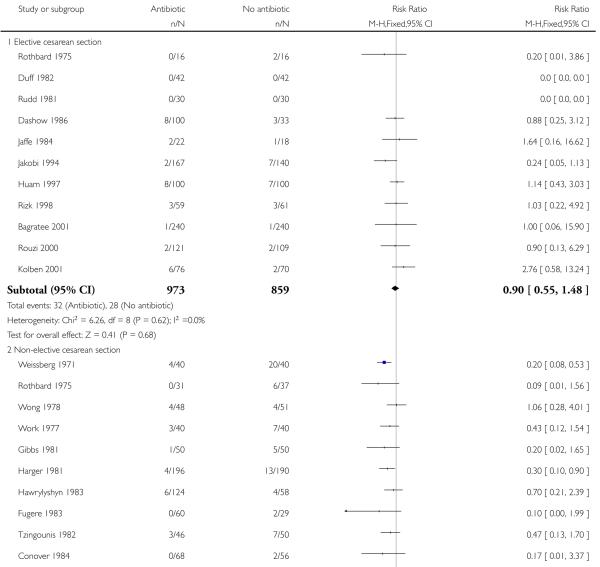 |
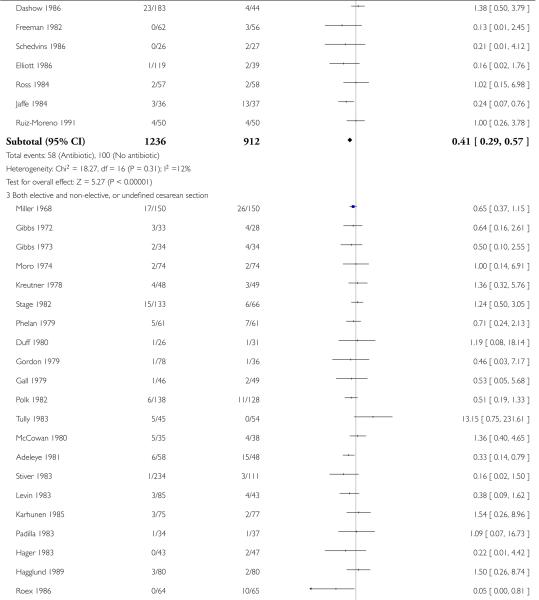 |
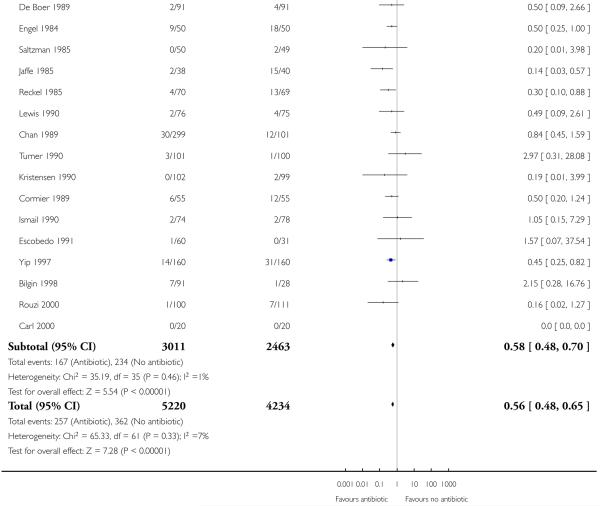 |
Analysis 2.8. Comparison 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section, Outcome 8 Maternal adverse effects.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section
Outcome: 8 Maternal adverse effects
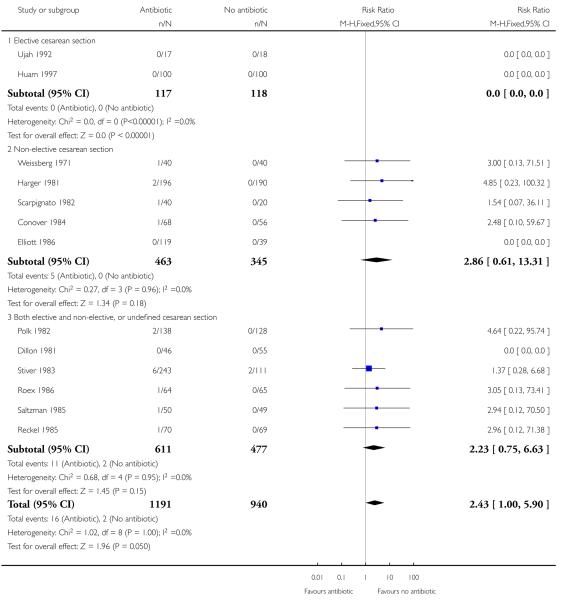 |
Analysis 2.9. Comparison 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section, Outcome 9 Maternal days in hospital.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 2 Antibiotics versus no antibiotics - subgroup by type of cesarean section
Outcome: 9 Maternal days in hospital
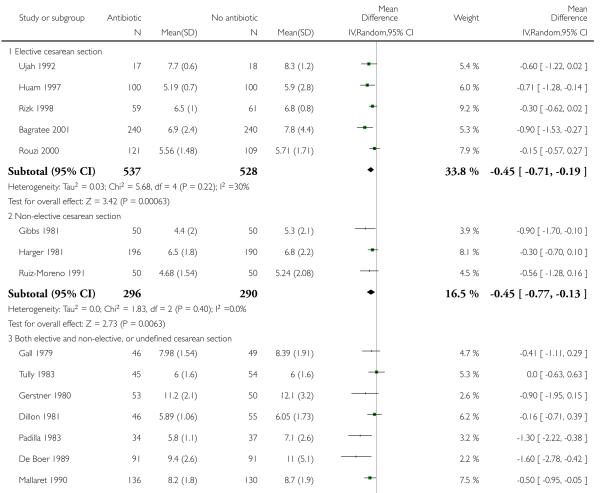 |
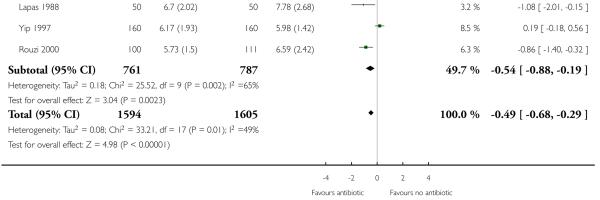 |
Analysis 3.1. Comparison 3 Antibiotics versus no antibiotics - subgroup by timing of administration, Outcome 1 Maternal febrile morbidity/fever.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 3 Antibiotics versus no antibiotics - subgroup by timing of administration
Outcome: 1 Maternal febrile morbidity/fever
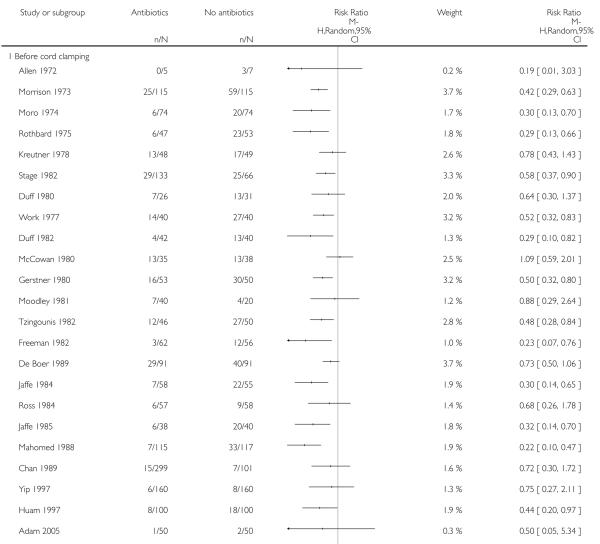 |
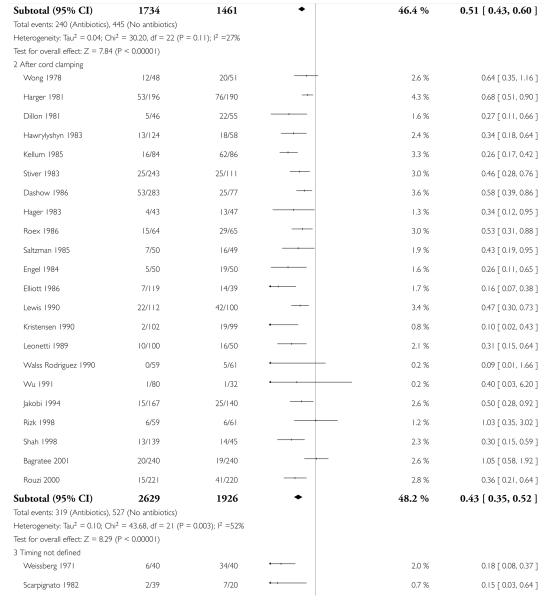 |
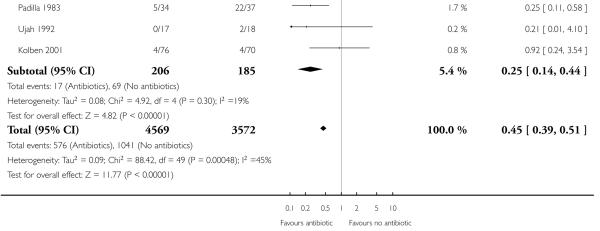 |
Analysis 3.2. Comparison 3 Antibiotics versus no antibiotics - subgroup by timing of administration, Outcome 2 Maternal wound infection.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 3 Antibiotics versus no antibiotics - subgroup by timing of administration
Outcome: 2 Maternal wound infection
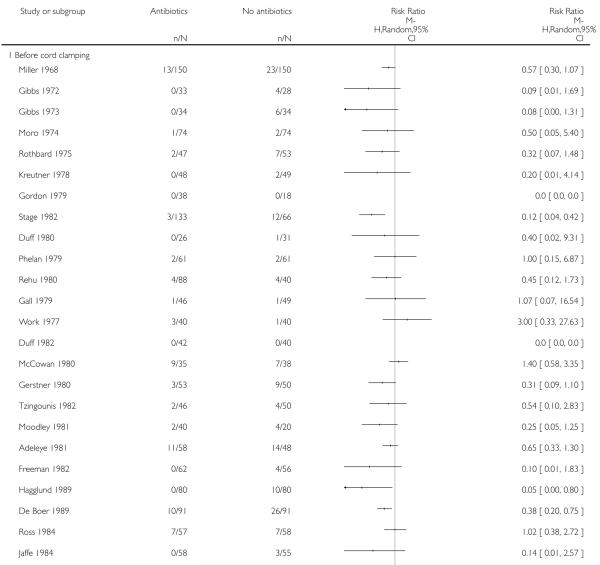 |
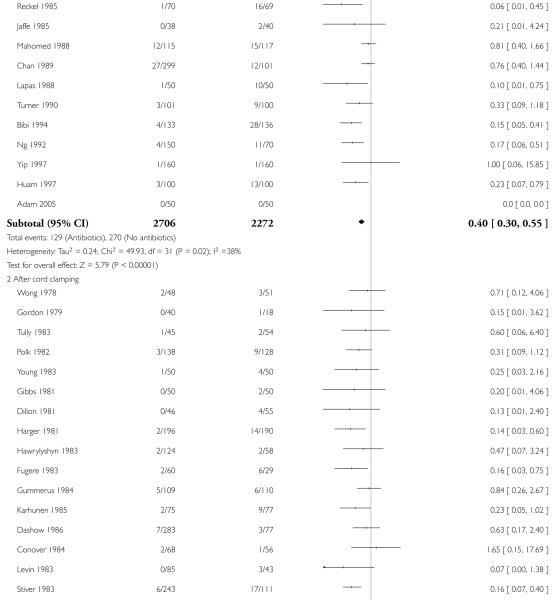 |
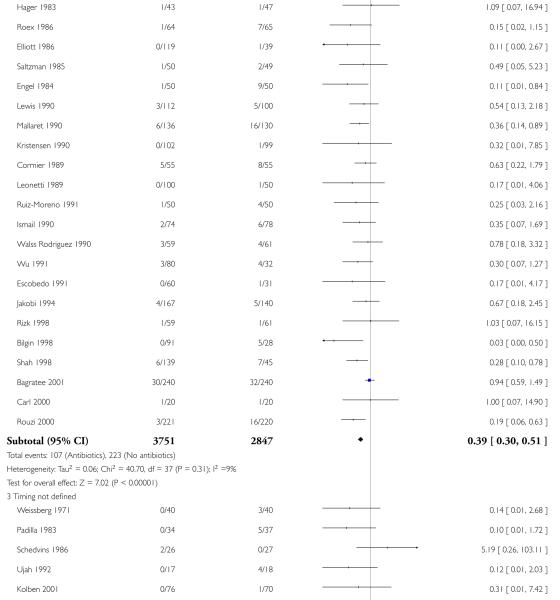 |
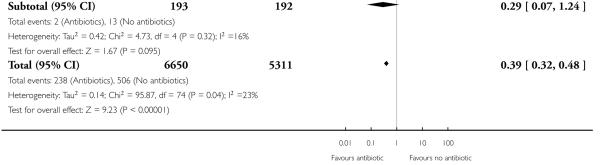 |
Analysis 3.3. Comparison 3 Antibiotics versus no antibiotics - subgroup by timing of administration, Outcome 3 Maternal endometritis.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 3 Antibiotics versus no antibiotics - subgroup by timing of administration
Outcome: 3 Maternal endometritis
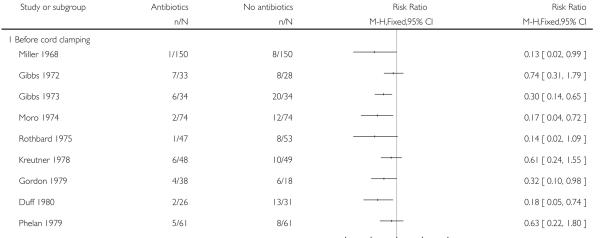 |
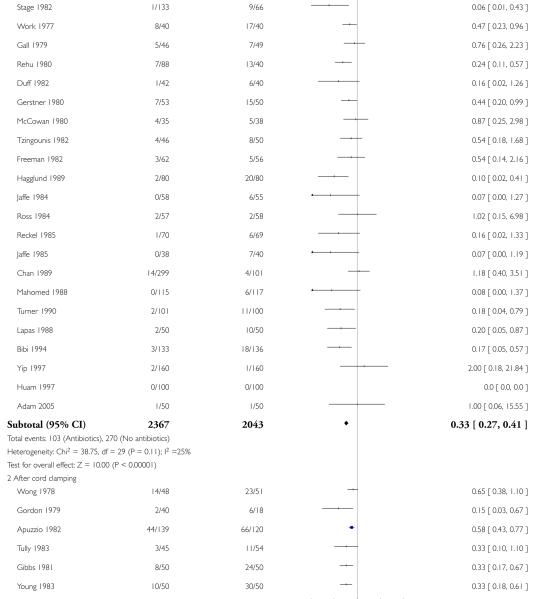 |
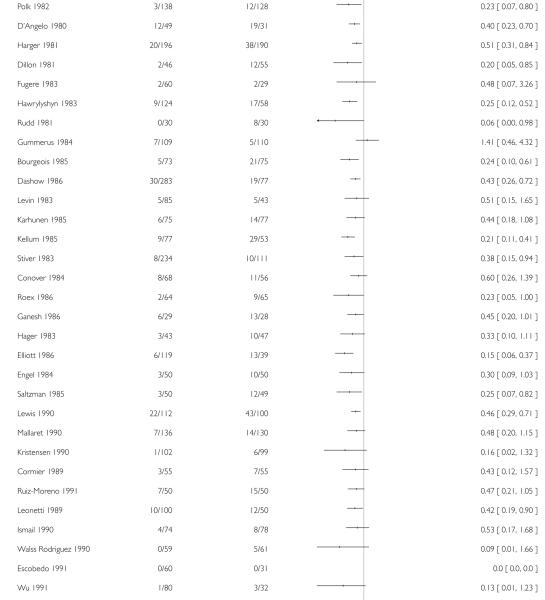 |
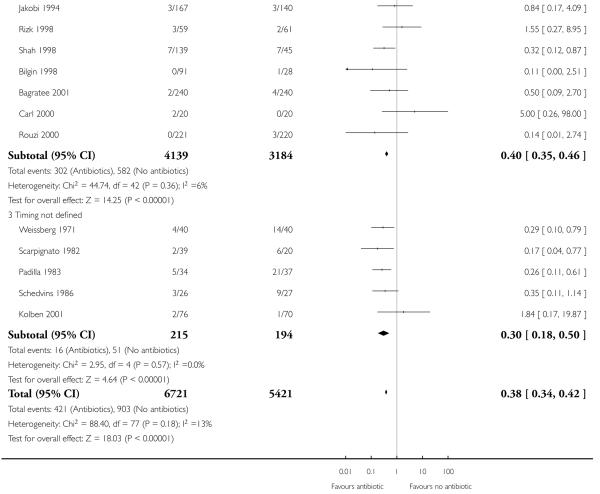 |
Analysis 3.4. Comparison 3 Antibiotics versus no antibiotics - subgroup by timing of administration, Outcome 4 Maternal serious infectious complications.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 3 Antibiotics versus no antibiotics - subgroup by timing of administration
Outcome: 4 Maternal serious infectious complications
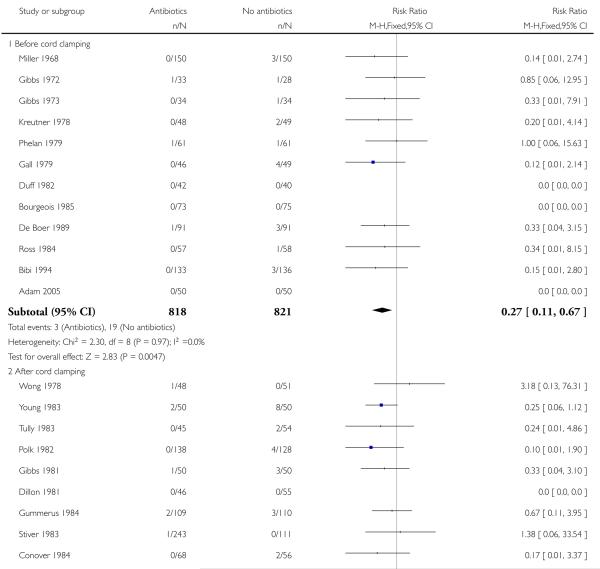 |
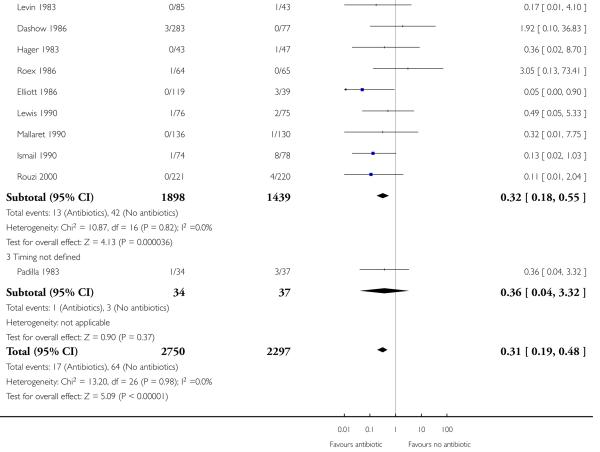 |
Analysis 3.7. Comparison 3 Antibiotics versus no antibiotics - subgroup by timing of administration, Outcome 7 Maternal urinary tract infections.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 3 Antibiotics versus no antibiotics - subgroup by timing of administration
Outcome: 7 Maternal urinary tract infections
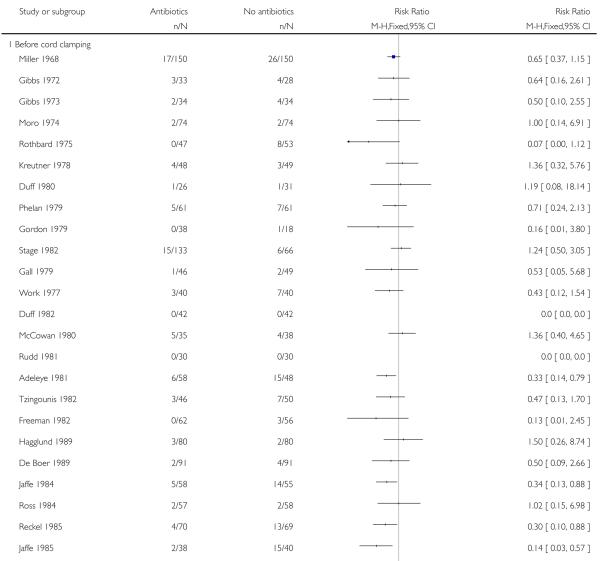 |
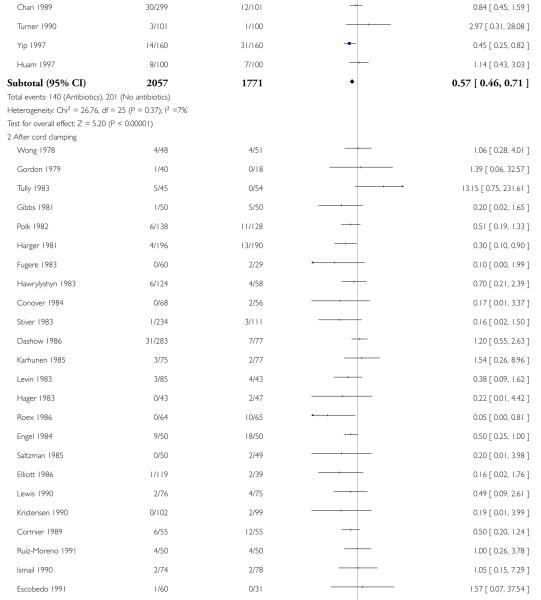 |
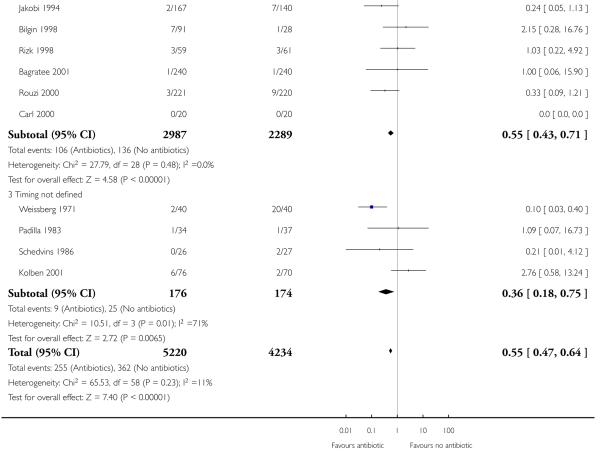 |
Analysis 3.8. Comparison 3 Antibiotics versus no antibiotics - subgroup by timing of administration, Outcome 8 Maternal adverse effects.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 3 Antibiotics versus no antibiotics - subgroup by timing of administration
Outcome: 8 Maternal adverse effects
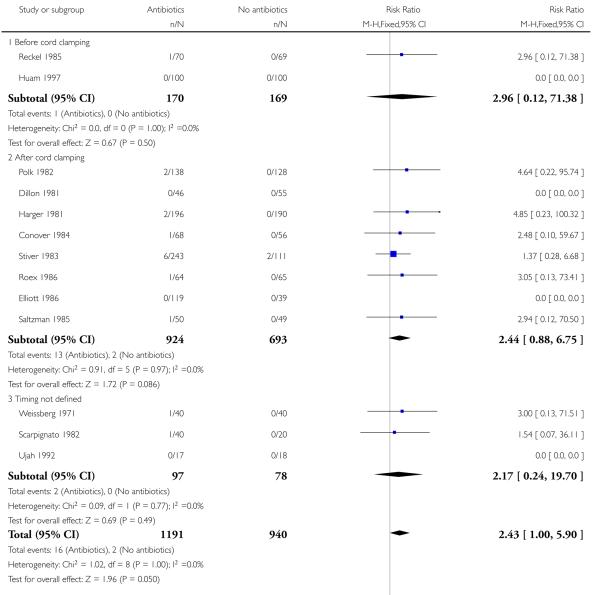 |
Analysis 3.9. Comparison 3 Antibiotics versus no antibiotics - subgroup by timing of administration, Outcome 9 Maternal days in hospital.
Review: Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section
Comparison: 3 Antibiotics versus no antibiotics - subgroup by timing of administration
Outcome: 9 Maternal days in hospital
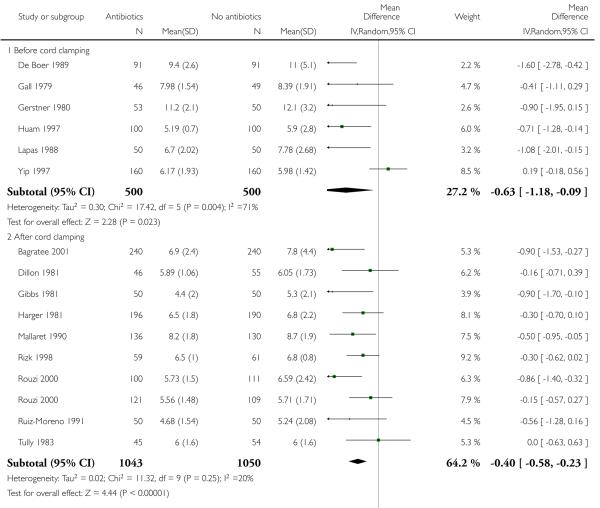 |
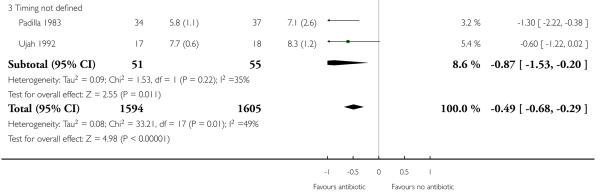 |
FEEDBACK
Griffin, July 1999
Summary
It has been stated that manual removal of the placenta during cesarean section increases the risk of endometritis, when compared to cord traction for placental delivery. Occlusive dressings also increase wound healing and decrease the risk of wound infection. Would it be better to adopt these simple measures first and then trial antibiotic therapy again?
Summary of comments from Chris Griffin, July 1999.
Reply
Infection following cesarean section may be reduced by the use of cord traction to remove the placenta and occlusive wound dressings. Most trials of prophylactic antibiotic therapy do not specify the methods of placental removal and wound care, and may represent a mixture of various methods. Given the clinically important reduction of infection with antibiotic use in general, support for a policy of not using antibiotics would require evidence from randomized trials that in the context of placental removal by cord traction and occlusive wound dressings, antibiotic therapy confers no additional benefit.
Contributors
Summary of response from Fiona Smaill and Justus Hofmeyr, October 1999.
WHAT’S NEW
Last assessed as up-to-date: 5 November 2009.
| Date | Event | Description |
|---|---|---|
| 31 May 2009 | New search has been performed | Search updated. Five new trials included (Adam 2005; Freeman 1982; Huam 1997; Jaffe 1984; Kolben 2001). |
| 18 May 2009 | New citation required but conclusions have not changed | New review team substantially updated this review. |
HISTORY
Protocol first published: Issue 4, 2008
Review first published: Issue 1, 2010
| Date | Event | Description |
|---|---|---|
| 3 January 2008 | Amended | Converted to new review format. |
| Added a note about the updating of the review. | ||
| 5 March 2002 | New search has been performed | Fifteen additional trials have been added to the review. The overall conclusion remains unchanged. Antibiotic prophylaxis will reduce infectious complications following both an elective and non-elective cesarean section |
| 30 June 1999 | Feedback has been incorporated | Added feedback from Chris Griffin and response from authors. |
Footnotes
DECLARATIONS OF INTEREST
None known.
SOURCES OF SUPPORT
Internal sources
- University of the Witwatersrand, South Africa.
- The University of Liverpool, UK.
External sources
- UNDP/UNFPA/WHO/World Bank (HRP), Switzerland.
- The University of Liverpool, UK.
NIHR NHS Cochrane Collaboration Programme Grant Scheme award for NHS-prioritised centrally-managed, pregnancy and childbirth systematic reviews: CPGS02
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
We have used fixed-effect Mantel-Haenszel meta-analysis for combining data because the Handbook suggests it is more commonly used (Higgins 2008).
We have modified the wording in the methods sections for Assessment of heterogeneity, Assessment of reporting biases and Data synthesis to update them with the new methods being used by the group, developed in conjunction with the Group’s Statistician, Simon Gates, and Richard Riley. We have used these new methods in the review.
Medical Subject Headings (MeSH)
*Antibiotic Prophylaxis [adverse effects]; Bacterial Infections [* prevention & control]; Cesarean Section [* adverse effects]; Endometritis [* prevention & control]; Postoperative Complications [* prevention & control]; Randomized Controlled Trials as Topic; Surgical Wound Infection [prevention & control]; Urinary Tract Infections [prevention & control]
MeSH check words
Female; Humans; Pregnancy
Editorial group: Cochrane Pregnancy and Childbirth Group.
Publication status and date: New, published in Issue 1, 2010.
Review content assessed as up-to-date: 5 November 2009.
References to studies included in this review
* Indicates the major publication for the study
- Adam 2005.Adam I, Adam ES, Gerais AS. Randomized trial of ceftriaxone prophylaxis in elective cesarean section. Saudi Medical Journal. 2005;26(3):500–1. [published data only] [PubMed] [Google Scholar]
- Adeleye 1981.Adeleye JA, Osinusi BO. The use of prophylactic antibiotics in caesarean sections. Singapore Journal of Obstetrics and Gynaecology. 1981;12:29–34. [published data only] [Google Scholar]
- Allen 1972.Allen JL, Rampone JF, Wheeless CR. Use of a prophylactic antibiotic in elective major gynecologic operations. Obstetrics & Gynecology. 1972;39:218–24. [published data only] [PubMed] [Google Scholar]
- Apuzzio 1982.Appuzzio JJ, Ganesh VV, Pelosi MA, Frisoli G. The effect of prophylactic antibiotics on risk factors for endomyometritis in adolescent patients undergoing cesarean section. Journal of Adolescent Health Care. 1984;5:163–6. doi: 10.1016/s0197-0070(84)80036-4. [published data only] [DOI] [PubMed] [Google Scholar]
- *; Apuzzio JJ, Reyelt C, Pelosi M, Sen P, Louria DB. Prophylactic antibiotics for cesarean section: comparison of high- and low-risk patients for endomyometritis. Obstetrics and Gynecology. 1982;59:693. [published data only] [PubMed] [Google Scholar]
- Bagratee 2001.*; Bagratee J, Moodley J, Kleinschmidt I, Zawilski W. A randomized controlled trial of antibiotic prophylaxis in elective caesarean section. BJOG: an international journal of obstetrics and gynaecology. 2001;108:143–8. doi: 10.1111/j.1471-0528.2001.00042.x. [DOI] [PubMed] [Google Scholar]
- Bagratee JS, Moodley J. Antibiotic prophylaxis in elective caesarean section. Women’s Health - into the new millenium; Proceedings of the 4th International Scientific Meeting of the Royal College of Obstetricians and Gynaecologists; Cape Town South Africa. 1999 Oct 3-6; p. 6. 1999. [published data only] [Google Scholar]
- Bibi 1994.Bibi M, Megdiche H, Ghanem H, Sfaxi I, Nouira M, Essaidi H, et al. Antibiotic prophylaxis in a priori cesarean sections without a high risk of infection [L’antibioprophylaxie dans les cesariennes a priori sans ‘haut risque infectieux’] Journal de Gynecologie, Obstetrique et Biologie de la Reproduction (Paris) 1994;23:451–5. [published data only] [PubMed] [Google Scholar]
- Bilgin 1998.Bilgin T, Ozan H, Dirgen A, Esmer A. Comparison of four different antibiotics as prophylaxis in caesarean section. Journal of Obstetrics and Gynaecology. 1998;18(6):546–7. doi: 10.1080/01443619866309. [published data only] [DOI] [PubMed] [Google Scholar]
- Bourgeois 1985.Bourgeois FJ, Pinkerton JA, Andersen W, Thiagarajah S. Antibiotic irrigation prophylaxis in the high-risk cesarean section patient. American Journal of Obstetrics and Gynecology. 1985;153:197–201. doi: 10.1016/0002-9378(85)90113-9. [published data only] [DOI] [PubMed] [Google Scholar]
- Carl 2000.Carl SH, Hampton R. Normal saline pelvic and intrauterine irrigation in the high-risk cesarean section (CS) patient as a safe and cost-effective method of infection prophylaxis. American Journal of Obstetrics and Gynecology. 2000;182(1 Pt 2):S96. [published data only] [Google Scholar]
- Chan 1989.Chan ACW, Leung AKL, Chin RKH, Chang AMZ. Single dose prophylactic antibiotics in caesarean sections. Australian and New Zealand Journal of Obstetrics and Gynaecology. 1989;29:107–9. doi: 10.1111/j.1479-828x.1989.tb01696.x. [published data only] [DOI] [PubMed] [Google Scholar]
- Conover 1984.Conover WB, Moore TR. Comparison of irrigation and intravenous antibiotic prophylaxis at cesarean section. Obstetrical and Gynecological Survey. 1984;39:692–3. [PubMed] [Google Scholar]
- *; Conover WB, Moore TR. Comparison of irrigation and intravenous antibiotic prophylaxis at cesarean section. Obstetrics and Gynecology. 1984;63:787–91. [published data only] [PubMed] [Google Scholar]
- Cormier 1989.Cormier P, Leng JJ. Antibiotic prophylaxis after caesarean section [Antibioprophylaxie lors des cesariennes] Journal de Gynecologie, Obstetrique et Biologie de la Reproduction. 1991;20:600. [Google Scholar]
- *; Cormier P, Leng JJ, Janky E, Duthil B, Brouste V. Prevention of infectious complications after cesarean section by the use of cefotetan. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction (Paris) 1989;18:388–92. [published data only] [PubMed] [Google Scholar]
- D’Angelo 1980.D’Angelo LJ, Sokol RJ. Short- vs long-course prophylactic antibiotic treatment in cesarean section patients. Obstetrics & Gynecology. 1980;55:583–6. [published data only] [PubMed] [Google Scholar]
- Dashow 1986.Dashow EE, Read JA, Coleman FH. Randomized comparison of five irrigation solutions at cesarean section. Obstetrics & Gynecology. 1986;68:473–8. [published data only] [PubMed] [Google Scholar]
- De Boer 1989.De Boer CN, Thornton JG. Prophylactic short course rectal metronidazole for cesarean section. A double-blind controlled trial of a simple low cost regimen. International Journal of Gynecology & Obstetrics. 1989;28:103–7. doi: 10.1016/0020-7292(89)90468-2. [published data only] [DOI] [PubMed] [Google Scholar]
- Dillon 1981.Dillon WP, Seigel MS, Lele AS, O’Leary JA. Evaluation of cefoxitin prophylaxis for cesarean section. International Journal of Gynecology & Obstetrics. 1981;19:133–9. doi: 10.1016/0020-7292(81)90052-7. [published data only] [DOI] [PubMed] [Google Scholar]
- Duff 1980.Duff P, Park RC. Antibiotic prophylaxis for cesarean section in a military population. Military Medicine (Washington DC) 1980;145:377–81. [published data only] [PubMed] [Google Scholar]
- Duff 1982.Duff P, Smith PN, Keiser JF. Antibiotic prophylaxis in low-risk cesarean section. Journal of Reproductive Medicine. 1982;27:133–8. [published data only] [PubMed] [Google Scholar]
- Elliott 1986.Elliott JP, Flaherty JF. Comparison of lavage or intravenous antibiotics at cesarean section. Obstetrics & Gynecology. 1986;67:29–32. [published data only] [PubMed] [Google Scholar]
- Engel 1984.*; Engel K, Amir-Moazami B, Karschnia R, Hahn T. Advantages and hazards of preventing infection following cesarean section--clinical and bacteriologic results of a high-dosage treatment with mezlocillin and oxacillin short-term preventive following clamping of the umbilical cord [Nutzen und Gefahren der Infektionsprophylaxe bei der Sectio caesarea—-klinische und bakteriologische Ergebnisse einer hochdosierten Kurzzeitprophylaxe nach dem Abnabeln mit Mezlocillin und Oxacillin.] Geburtshilfe und Frauenheilkunde. 1984;44(3):162–70. doi: 10.1055/s-2008-1036872. [DOI] [PubMed] [Google Scholar]
- Engel K, Karschnia R. Bacterial flora changes resulting from antimicrobial treatment. Journal of Obstetrics and Gynaecology. 1986;6:6–8. [published data only] [Google Scholar]
- Escobedo 1991.Escobedo Lobaton JM, Rodriguez Hinojosa DE, Kistner Garza AM, Benavides de Anda L. Prophylactic use of antibiotics in cesarean section [Uso profilactico de antibioticos en operacion cesarea] Ginecologia y Obstetricia de Mexico. 1991;59(1):35–8. [published data only] [PubMed] [Google Scholar]
- Freeman 1982.Freeman GM. The efficacy of prophylactic antibiotics in high-risk patients undergoing cesarean section. Journal of the American Osteopathic Association. 1982;81(9):610–5. [published data only] [PubMed] [Google Scholar]
- Fugere 1983.Fugere P, Turgeon P, Boucher M, Verschelden G, Lemay M. Use of cephalosporins in antibiotic prophylaxis in women undergoing nonelective caesarean section [Utilisation des cephalosporines comme antibioprophylaxie lors de cesariennes] Canadian Medical Association Journal. 1983;129:132–5. [published data only] [PMC free article] [PubMed] [Google Scholar]
- Gall 1979.Gall SA. The efficacy of prophylactic antibiotics in caesarean section. American Journal of Obstetrics and Gynecology. 1979;134:506–11. doi: 10.1016/0002-9378(79)90830-5. [published data only] [DOI] [PubMed] [Google Scholar]
- Ganesh 1986.Ganesh V, Apuzzio JJ, Dispenziere B, Patel K, Bergen B, Louria DB. Single-dose trimethoprim-sulfamethoxazole prophylaxis for cesarean section. American Journal of Obstetrics and Gynecology. 1986;154:1113–4. doi: 10.1016/0002-9378(86)90768-4. [published data only] [DOI] [PubMed] [Google Scholar]
- Gerstner 1980.Gerstner G, Kofler E, Huber J. Perioperative metronidazol-prophylaxis for cesarean section. Zeitschrift fur Geburtshilfe und Perinatologie. 1980;184:418–23. [published data only] [PubMed] [Google Scholar]
- Gibbs 1972.Gibbs RS, De Cherney AH, Schwarz RH. Prophylactic antibiotics in cesarean section: a double-blind study. American Journal of Obstetrics and Gynecology. 1972;114:1048–53. doi: 10.1016/0002-9378(72)90867-8. [published data only] [DOI] [PubMed] [Google Scholar]
- Gibbs 1973.Gibbs RS, Hunt JE, Schwarz RH. A follow-up study on prophylactic antibiotics in cesarean section. American Journal of Obstetrics and Gynecology. 1973;117:419–22. doi: 10.1016/0002-9378(73)90050-1. [published data only] [DOI] [PubMed] [Google Scholar]
- Gibbs 1981.Gibbs RS, St Clair PJ, Castillo MS, Castaneda YS. Bacteriologic effects of antibiotic prophylaxis in high-risk cesarean section. Obstetrics & Gynecology. 1981;57:277–82. [published data only] [PubMed] [Google Scholar]
- Gordon 1979.Gordon HR, Phelps D, Blanchard K. Prophylactic cesarean section antibiotics: maternal and neonatal morbidity before or after cord clamping. Obstetrics & Gynecology. 1979;53:151–6. [published data only] [PubMed] [Google Scholar]
- Gummerus 1984.Gummerus M. Perioperative short-term prophylaxis of puerperal infections following caesarean section with metronidazol. Geburtshilfe und Frauenheilkunde. 1984;44:570–2. doi: 10.1055/s-2008-1036304. [published data only] [DOI] [PubMed] [Google Scholar]
- Hager 1983.Hager WD, Williamson MM. Effects of antibiotic prophylaxis on women undergoing nonelective cesarean section in a community hospital. Journal of Reproductive Medicine. 1983;28:687–90. [published data only] [PubMed] [Google Scholar]
- Hagglund 1989.Hagglund L, Christensen KK, Christensen P, Westrom L, Ingemarsson I. Reduced rate of postoperative infections in emergency cesarean section after two doses of cefuroxim perioperatively. Acta Obstetricia et Gynecologica Scandinavica. 1989;68:201–4. doi: 10.3109/00016348909020989. [published data only] [DOI] [PubMed] [Google Scholar]
- Harger 1981.Harger JH, English DH. Selection of patients for antibiotic prophylaxis in cesarean sections. American Journal of Obstetrics and Gynecology. 1981;141:752–8. doi: 10.1016/0002-9378(81)90699-2. [published data only] [DOI] [PubMed] [Google Scholar]
- Hawrylyshyn 1983.Hawrylyshyn PA, Bernstein EP, Papsin FR. Short-term antibiotic prophylaxis in high-risk patients followingcesarean section. American Journal of Obstetrics and Gynecology. 1983;145:285–9. doi: 10.1016/0002-9378(83)90712-3. [published data only] [DOI] [PubMed] [Google Scholar]
- Huam 1997.Huam SH, Lim JM, Raman S. Single-dose antibiotic prophylaxis in women undergoing elective caesarean section. Medical Journal of Malaysia. 1997;52:3–7. [published data only] [PubMed] [Google Scholar]
- Ismail 1990.Ismail MA, Nelson KE, Larson P, Moses VK. Selective effect of cefoxitin prophylaxis on post-cesarean-section microbial flora. Journal of Reproductive Medicine. 1990;35:168–74. [published data only] [PubMed] [Google Scholar]
- Jaffe 1984.Jaffe R, Loebel R, Altaras M, Ben Aderet N. Perioperative mezlocillin prophylaxis in cesarean section. Clinical Therapeutics. 1984;6(4):467–74. [published data only] [PubMed] [Google Scholar]
- Jaffe 1985.Jaffe R, Altaras M, Cohen I, Ben-Aderet N. Single-dose mezlocillin prophylaxis in emergency cesarean section. Clinical Therapeutics. 1985;7(4):507–11. [published data only] [PubMed] [Google Scholar]
- Jakobi 1994.Jakobi P, Weissman A, Sigler E, Margolis K, Zimmer EZ. Post-cesarean section febrile morbidity. Journal of Reproductive Medicine. 1994;39:707–10. [published data only] [PubMed] [Google Scholar]
- Karhunen 1985.Karhunen M, Koskela O, Teisala K, Suikkari AM, Mattila J. Prophylaxis and treatment of anaerobic infections following caesarean section with tinidazole. Chemotherapy. 1985;31:228–36. doi: 10.1159/000238341. [published data only] [DOI] [PubMed] [Google Scholar]
- Kellum 1985.Kellum RB, Roberts WE, Harris JB, Khansur N, Morrison JC. Effect of intrauterine antibiotic lavage after cesarean birth on postoperative morbidity. Journal of Reproductive Medicine. 1985;30:527–9. [published data only] [PubMed] [Google Scholar]
- Kolben 2001.Kolben M, Mandoki E, Ulm K, Freitag K. Randomized trial of cefotiam prophylaxis in the prevention of postoperative infectious morbidity after elective cesarean section. European Journal of Clinical Microbiology and Infectious Diseases. 2001;20:40–2. doi: 10.1007/s100960000365. [published data only] [DOI] [PubMed] [Google Scholar]
- Kreutner 1978.Kreutner AK, Del Bene VE, Delamar D, Huguley V, Harmon PM, Mitchell KS. Perioperative antibiotic prophylaxis in cesarean section. Obstetrics & Gynecology. 1978;52:279–84. [published data only] [PubMed] [Google Scholar]
- Kristensen 1990.Kristensen GB, Beiter EC, Mather O. Single-dose cefuroxime prophylaxis in non-elective cesarean section. Acta Obstetricia et Gynecologica Scandinavica. 1990;69:497–500. doi: 10.3109/00016349009013325. [published data only] [DOI] [PubMed] [Google Scholar]
- Lapas 1988.*; Lapas KA, Todorov I. Comparative double-blind study of intravenous metronidazole vs placebo in preventing infection after cesarean section. Akusherstvo i Ginekologiia. 1988;27:46–9. [published data only] [PubMed] [Google Scholar]
- Lappas CA, Leonardopoulos J. Double-blind comparative study of metronidazole iv vs placebo in the prophylaxis of sepsis following cesarean section. Archives of Gynecology. 1985;237(Suppl 1):279. [published data only] [Google Scholar]
- Leonetti 1989.Leonetti HB, Yun H, O’Leary JA, Greenberg AL. Single vs multiple dose piperacillin in high risk primary cesarean section. American Journal of Gynecologic Health. 1989;3:195–8. [published data only] [Google Scholar]
- Levin 1983.Levin DK, Gorchels C, Andersen R. Reduction of post-cesarean section infectious morbidity by means of antibiotic irrigation. American Journal of Obstetrics and Gynecology. 1983;147:273–7. doi: 10.1016/0002-9378(83)91110-9. [published data only] [DOI] [PubMed] [Google Scholar]
- Lewis 1990.Lewis DF, Otterson WN, Dunnihoo DR. Antibiotic prophylactic uterine lavage in cesarean section: a double-blind comparison of saline, ticarcillin, and cefoxitin irrigation in indigent patients. Southern Medical Journal. 1990;83:274–6. doi: 10.1097/00007611-199003000-00004. [published data only] [DOI] [PubMed] [Google Scholar]
- Mahomed 1988.Mahomed K. A double-blind randomized controlled trial on the use of prophylactic antibiotics in patients undergoing elective caesarean section. British Journal of Obstetrics and Gynaecology. 1988;95:689–92. doi: 10.1111/j.1471-0528.1988.tb06531.x. [published data only] [DOI] [PubMed] [Google Scholar]
- Mallaret 1990.Mallaret MR, Blatier JF, Racinet C, Fauconnier J, Favier M, Micoud M. Economic benefit of using antibiotics prophylactically in cesarean sections with little risk of infection. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction (Paris) 1990;19:1061–4. [PubMed] [Google Scholar]
- *; Racinet C, Mallaret MR, Favier M, Berthet J, Morel I, Fauconnier J, et al. Antibiotic prophylaxis in cesarean sections without high risk of infection. Presse Medicale. 1990;19:1755–8. [published data only] [PubMed] [Google Scholar]
- McCowan 1980.McCowan L, Jackson P. The prophylactic use of metronidazole in caesarean section. New Zealand Medical Journal. 1980;92:153–5. [published data only] [PubMed] [Google Scholar]
- Miller 1968.Miller RD, Crichton D. Ampicillin prophylaxis in caesarean section. South African Journal of Obstetrics and Gynaecology. 1968;6:69–70. [published data only] [Google Scholar]
- Moodley 1981.Moodley J, Zeeman DJ. Prophylactic and antimicrobial therapy using lincomycin in patients undergoing emergency caesarean section. South African Medical Journal. 1981;59:911–3. [published data only] [PubMed] [Google Scholar]
- Moro 1974.Moro M, Andrews M. Prophylactic antibiotics in cesarean section. Obstetrics & Gynecology. 1974;44:688–92. [published data only] [PubMed] [Google Scholar]
- Morrison 1973.Morrison JC, Coxwell WL, Kennedy BS, Schreier PC, Wiser WL, Fish SA. The use of prophylactic antibiotics in patients undergoing cesarean section. Surgery, Gynecology and Obstetrics. 1973;136:425–8. [published data only] [PubMed] [Google Scholar]
- Ng 1992.Ng NK. The role of prophylactic antibiotics in caesarean section - a randomized trial. Medical Journal of Malaysia. 1992;47:273–9. [published data only] [PubMed] [Google Scholar]
- Padilla 1983.Padilla SL, Spence MR, Beauchamp PJ. Single-dose ampicillin for cesarean section prophylaxis. Obstetrics & Gynecology. 1983;61:463–6. [published data only] [PubMed] [Google Scholar]
- Phelan 1979.Phelan JP, Pruyn SC. Prophylactic antibiotics in cesarean section: a double-blind study of cefalozin. American Journal of Obstetrics and Gynecology. 1979;133:474–8. doi: 10.1016/0002-9378(79)90279-5. [published data only] [DOI] [PubMed] [Google Scholar]
- Polk 1982.Polk BF, Krache M, Phillippe M, Munoz A, Hutchinson D, Miao L, et al. Randomized clinical trial of perioperative cefoxitin in preventing maternal infection after primary cesarean section. American Journal of Obstetrics and Gynecology. 1982;142:983–7. doi: 10.1016/0002-9378(82)90779-7. [published data only] [DOI] [PubMed] [Google Scholar]
- Reckel 1985.Reckel J, Scheele R. Perioperative antibiotic prophylaxis in cesarean section [Perioperative Antibiotikaprophylaxe bei Kaiserschnitt] Der Klinikarzt. 1985;14:1054–65. [published data only] [Google Scholar]
- Rehu 1980.Rehu M, Jahkola M. Prophylactic antibiotics in caesarean section: effect of a short preoperative course of benzyl penicillin or clindamycin plus gentamicin on postoperative infectious morbidity. Annals of Clinical Research. 1980;12:45–8. [published data only] [PubMed] [Google Scholar]
- Rizk 1998.Rizk DEE, Nsanze H, Mabrouk MH, Mustafa N, Thomas L, Kumar M. Systemic antibiotic prophylaxis in elective cesarean delivery. International Journal of Gynecology & Obstetrics. 1998;61(3):245–51. doi: 10.1016/s0020-7292(98)00062-9. [published data only] [DOI] [PubMed] [Google Scholar]
- Roex 1986.Roex AJM, Puyenbroek JI, Maclaren DM, Arts NFTh. Short-term antibiotic prophylaxis for caesarean section [Kortdurende antibioticum profylaxe bij de section Caesarea] Nederland Tijdschrift voor Obstetrie en Gynaecologie. 1987;100:105. [Google Scholar]
- *; Roex AJM, Puyenbroek JI, MacLaren DM, Van Geijn HP, Arts NFT. A randomized clinical trial of antibiotic prophylaxis in cesarean section: maternal morbidity, risk factors and bacteriological changes. European Journal of Obstetrics & Gynecology and Reproductive Biology. 1986;22:117–24. doi: 10.1016/0028-2243(86)90055-9. [published data only] [DOI] [PubMed] [Google Scholar]
- Ross 1984.Ross L, Mason P, Barnet-Lamb M, Robinson RE, Warren R. Prophylactic metronidazole in patients with ruptured membranes undergoing emergency caesarean section. Journal of Obstetrics and Gynaecology. 1984;5:32–5. [published data only] [Google Scholar]
- Rothbard 1975.Rothbard MJ, Mayer W, Wystepek A, Gordon M. Prophylactic antibiotics in cesarean section. Obstetrics & Gynecology. 1975;45:421–4. [published data only] [PubMed] [Google Scholar]
- Rouzi 2000.Rouzi AA, Khalifa F, Ba’aqeel H, Al-Hamdan HS, Bondagji N. The routine use of cefazolin in cesarean section. International Journal of Gynecology and Obstetrics. 2000;69:107–12. doi: 10.1016/s0020-7292(99)00225-8. [published data only] [DOI] [PubMed] [Google Scholar]
- Rudd 1981.Long WH, Rudd EG, Dillon MB. Intrauterine irrigation with cefamandole nafate solution at cesarean section: a preliminary report. American Journal of Obstetrics and Gynecology. 1980;138:755–8. doi: 10.1016/s0002-9378(16)32731-4. [DOI] [PubMed] [Google Scholar]
- *; Rudd EG, Long WH, Dillon MB. Febrile morbidity following cefamandole nafate intrauterine irrigation during cesarean section. American Journal of Obstetrics and Gynecology. 1981;141:12–6. doi: 10.1016/0002-9378(81)90667-0. [published data only] [DOI] [PubMed] [Google Scholar]
- Ruiz-Moreno 1991.Ruiz-Moreno JA, Garcia-Rojas JM, Lozada-Leon JD. Prevention of post cesarean infectious morbidity with a single dose of intravenous metronidazole. International Journal of Gynecology & Obstetrics. 1991;34:217–20. doi: 10.1016/0020-7292(91)90352-6. [published data only] [DOI] [PubMed] [Google Scholar]
- Saltzman 1985.Saltzman DH, Eron LJ, Kay HH, Sites JG. Single-dose antibiotic prophylaxis in high-risk patients undergoing cesarean section. Obstetrics & Gynecology. 1985;65:655–7. [published data only] [PubMed] [Google Scholar]
- Scarpignato 1982.Scarpignato C, Caltabiano M, Condemi V, Mansani FE. Short-term vs long-term cefuroxime prophylaxis in patients undergoing emergency cesarean section. Clinical Therapeutics. 1982;5:186–92. [published data only] [PubMed] [Google Scholar]
- Schedvins 1986.Schedvins K, Moberg PJ. Prevention of postoperative infection in cesarean section after rupture of the membranes. International Journal of Gynecology & Obstetrics. 1986;24:165–8. doi: 10.1016/0020-7292(86)90093-7. [published data only] [DOI] [PubMed] [Google Scholar]
- Shah 1998.Shah S, Mazher Y, John IS. Single or triple dose piperacillin prophylaxis in elective cesarean section. International Journal of Gynecology & Obstetrics. 1998;62(1):23–9. doi: 10.1016/s0020-7292(98)00063-0. [published data only] [DOI] [PubMed] [Google Scholar]
- Stage 1982.Stage AH, Glover DD, Vaughan JE. Low-dose cephradine prophylaxis in obstetric and gynecologic surgery. Journal of Reproductive Medicine. 1982;27:113–9. [published data only] [PubMed] [Google Scholar]
- Stiver 1983.*; Stiver HG, Forward KR, Livingstone RA, Fugere P, Lemay M, Verschelden G, et al. Multicenter comparison of cefoxitin vs cefazolin for prevention of infectious morbidity after nonelective cesarean section. American Journal of Obstetrics and Gynecology. 1983;145:158–63. doi: 10.1016/0002-9378(83)90483-0. [DOI] [PubMed] [Google Scholar]
- Stiver HG, Forward KR, Tyrrell DL, Krip G, Livingstone RA, Fugere P, et al. Comparative cervical microflora shifts after cefoxitin or cefazolin prophylaxis against infection following cesarean section. American Journal of Obstetrics and Gynecology. 1984;149(7):718–21. doi: 10.1016/0002-9378(84)90109-1. [published data only] [DOI] [PubMed] [Google Scholar]
- Tully 1983.Tully JL, Klapholz H, Baldini LM, Friedland GH. Perioperative use of cefoxitin in primary cesarean section. Journal of Reproductive Medicine. 1983;28:827–32. [published data only] [PubMed] [Google Scholar]
- Turner 1990.Turner MJ, Egan DM, Qureshi WA, Skehan M, Black A, Darrell JH, et al. Use of cephradine prophylaxis of infection after caesarean section: stepwise logistic regression analysis of relevant factors. Journal of Obstetrics and Gynaecology. 1990;10:204–9. [published data only] [Google Scholar]
- Tzingounis 1982.Tzingounis V, Makris N, Zolotas J, Michalas S, Aravantinos D. Cefuroxime prophylaxis in caesarean section. Pharmatherapeutica. 1982;3:140–3. [published data only] [PubMed] [Google Scholar]
- Ujah 1992.Ujah I, Olarewaju R. The use of prophyactic Augmentin in elective caesarean section in Jos University teaching hospital; Proceedings of 26th British Congress of Obstetrics and Gynaecology; Manchester, UK. 1992 July 7-10; p. 484. 1992. [Google Scholar]
- *; Ujah IAO, Olarewaju RS, Otubu JAM. Prophylactic amoxicillin-clavulanic acid in elective cesarean section. Current Therapeutic Research, Clinical and Experimental. 1992;52(5):647–51. [published data only] [Google Scholar]
- Walss Rodriguez 1990.Walss Rodriguez R, Avila Esparza M. Prophylactic antimicrobial therapy in cesarean section [Antibioticoterapia profilactica en operacion cesarea] Ginecologia y Obstetricia de Mexico. 1990;58:79–83. [published data only] [Google Scholar]
- Weissberg 1971.Weissberg SM, Edwards NL, O’Leary JA. Prophylactic antibiotics in cesarean section. Obstetrics & Gynecology. 1971;38:290–3. [published data only] [PubMed] [Google Scholar]
- Wong 1978.Wong R, Gee CL, Ledger WJ. Prophylactic use of cefazolin in monitored obstetric patients undergoing cesarean section. Obstetrics & Gynecology. 1978;51:407–11. doi: 10.1097/00006250-197804000-00004. [published data only] [DOI] [PubMed] [Google Scholar]
- Work 1977.Work BA., Jr. Role of preventive antibiotics in patients undergoing cesarean section. South African Medical Journal. 1977;70:44–5. doi: 10.1097/00007611-197710001-00012. [published data only] [DOI] [PubMed] [Google Scholar]
- Wu 1991.Wu Y. Prevention of post-operative infection by using antibiotics of 217 cases of cesarean section. Chinese Journal of Obstetrics and Gynecology. 1992;27:73–5. [PubMed] [Google Scholar]
- *; Wu Y, Zhan L, Jing Y. Prevention of post-operative infection by uterine and intraperitoneal irrigation with ampicillin during cesarean section. International Journal of Experimental and Clinical Chemotherapy. 1991;4(3):132–6. [published data only] [Google Scholar]
- Yip 1997.Yip SK, Lau TK, Rogers MS. A study on prophylactic antibiotics in cesarean sections - is it worthwhile? Acta Obstetricia et Gynecologica Scandinavica. 1997;76(6):547–9. doi: 10.3109/00016349709024581. [published data only] [DOI] [PubMed] [Google Scholar]
- Young 1983.Young R, Platt L, Ledger W. Prophylactic cefoxitin in cesarean section. Surgery, Gynecology and Obstetrics. 1983;157:11–4. [published data only] [PubMed] [Google Scholar]
References to studies excluded from this review
- Andrews 2003.Andrews WW, Hauth JC, Cliver SP, Savage K, Goldenberg RL. Randomized clinical trial of extended spectrum antibiotic prophylaxis with coverage for ureaplasma urealyticum to reduce post-cesarean delivery endometritis. Obstetrics & Gynecology. 2003;101(6):1183–9. doi: 10.1016/s0029-7844(03)00016-4. [published data only] [DOI] [PubMed] [Google Scholar]
- Cormier 1988.Cormier Ph, Leng JJ, Janky E, Brouste V, Duthil B. Antibiotic prophylaxis with cefotetan in the prevention of post-partum and post-abortum infectious complications in endo-uterine investigations [Prevention par l’utilization du cefotetan des complications infectieuses du post-partum et du post-abortum dans les manoevres endo-manoeuvres uterines] Revue Francaise de Gynecologie et d Obstetrique. 1988;83:829–32. [published data only] [PubMed] [Google Scholar]
- Creatsas 1980.Creatsas G, Pavlatos M, Lolis D, Kaskarelis D. Ampicillin and gentamicin in the treatment of fetal intrauterine infections. Journal of Perinatal Medicine. 1980;8:13–8. doi: 10.1515/jpme.1980.8.1.13. [published data only] [DOI] [PubMed] [Google Scholar]
- De Palma 1980.De Palma RT, Leveno KJ, Cunningham FG, Pope T, Kappus SS, Roark ML, et al. Identification and management of women at high risk for pelvic infection following cesarean section. Obstetrics & Gynecology. 1980;55:185S–192S. doi: 10.1097/00006250-198003001-00047. [published data only] [DOI] [PubMed] [Google Scholar]
- Elliott 1982.Elliott JP, Freeman RK, Dorchester W. Short versus long course of prophylactic antibiotics in cesarean section. American Journal of Obstetrics and Gynecology. 1982;143:740–4. doi: 10.1016/0002-9378(82)90002-3. [published data only] [DOI] [PubMed] [Google Scholar]
- Harrigill 2003.Harrigill K, Miller H, Haynes D. The effect of intra-abdominal irrigation at cesarean section on maternal morbidity. American Journal of Obstetrics and Gynecology. 2000;182(1 Pt 2):S161. doi: 10.1016/s0029-7844(02)02466-3. [DOI] [PubMed] [Google Scholar]
- *; Harrigill KM, Miller HS, Haynes DE. The effect of intraabdominal irrigation at cesarean delivery on maternal morbidity: a randomized trial. Obstetrics & Gynecology. 2003;101:80–5. doi: 10.1016/s0029-7844(02)02466-3. [published data only] [DOI] [PubMed] [Google Scholar]
- Itskovitz 1979.Itskovitz J, Paldi E, Katz M. The effect of prophylactic antibiotics on febrile morbidity following cesarean section. Obstetrics & Gynecology. 1979;53:162–5. [published data only] [PubMed] [Google Scholar]
- Kreutner 1979.Kreutner AK, Del Bene VE, Delamar D, Bodden JL, Loadholt CB. Perioperative cephalosporin prophylaxis in cesarean section: effect on endometritis in the high-risk patient. American Journal of Obstetrics and Gynecology. 1979;134:925–35. doi: 10.1016/0002-9378(79)90868-8. [published data only] [DOI] [PubMed] [Google Scholar]
- Louie 1982.Louie TJ, Binns BAO, Baskett TF, Ross J, Koss J. Cefotaxime, cefazolin, or ampicillin prophylaxis of febrile morbidity in emergency cesarean sections. Clinical Therapeutics. 1982;5:83–96. [published data only] [PubMed] [Google Scholar]
- Pawelec 1994.Pawelec M, Michalik T, Robaczynski J. One-dose administration of Mandol in the prevention of infectionafter caesarean section; Proceedings of 14th European Congress of Perinatal Medicine; Helsinki, Finland. 1994 June 5-8; p. 389. 1994. [published data only] [Google Scholar]
- Petersen 1985.Petersen C, Brautigam HH. Short-term peri-operative prophylaxis with cefotaxim in gynaecological and obstetric surgery. Deutsche Medizinische Wochenschrift. 1985;110:1369–74. doi: 10.1055/s-2008-1069012. [published data only] [DOI] [PubMed] [Google Scholar]
- Pitt 2001.Pitt C, Sanchez-Ramos L, Kaunitz A. Adjunctive intravaginal metronidazole for the prevention of postcesarean endometritis: a randomized controlled trial. Obstetrics & Gynecology. 2001;98:745–50. doi: 10.1016/s0029-7844(01)01517-4. [published data only] [DOI] [PubMed] [Google Scholar]
- Roex 1987.Roex AJM, Van Loenen AC, Puyenbroek JI, Arts NFT. Secretion of cefoxitin in breast milk following short-term prophylactic administration in caesarean section. European Journal Obstetrics & Gynecology and Reproductive Biology. 1987;25:299–302. doi: 10.1016/0028-2243(87)90140-7. [published data only] [DOI] [PubMed] [Google Scholar]
- Sanchez-Ramos 1999.Sanchez-Ramos L, Pitt C, Delke I, Gaudier FL. Preoperative administration of intravaginal metronidazole for the prevention of post-cesarena endometritis: a randomized double-blind trial. American Journal of Obstetrics and Gynecology. 1999;180(1 Pt 2):S:81. [published data only] [Google Scholar]
- Sengupta 1976.Sengupta BS, Wynter HH, Hall JS, Ramchander R, Alexis A, Zamah N, et al. Prophylactic antibiotic in elective gynaecological and obstetrical major surgery. International Journal of Gynecology & Obstetrics. 1976;14:417–24. doi: 10.1002/j.1879-3479.1976.tb00077.x. [published data only] [DOI] [PubMed] [Google Scholar]
- Skryten 1988.Skryten A. The efficacy of perioperative cefoxitin prophylaxis in preventing infectious morbidity after nonelective cesarean section; 12th FIGO World Congress of Gynecology and Obstetrics; Brazil. 1988 October 23-28; p. 713. 1988. [published data only] [Google Scholar]
- Spreafico 1987.Spreafico P, Scian A, Epis A, Vassen L, Bonazzi C, Lovotti M. Cesarean section: antibiotic prophylaxis with ceftezole. Chemotherapia. 1987;6(2S):613–6. [published data only] [PubMed] [Google Scholar]
- Voto 1986.Voto LS, Benolief LA, Muniz AA, Trepat A, Balsechi EE, Margulies M. Prophylaxis of post-cesarean section puerperal infection with the ue of cefoxitin antibiotics [Profilaxis de la infeccion puerperal post-cesarea medianta el uso del antibiotico cefoxitina] Obstetricia y Ginecologia Latino-Americanas. 1986;44:419–24. [published data only] [Google Scholar]
- Wallace 1984.Wallace RL, Eglinton GS, Yonekura ML, Wallace TM. Extraperitoneal cesarean section: a surgical form of infection prophylaxis? American Journal of Obstetrics and Gynecology. 1984;148:172–7. doi: 10.1016/s0002-9378(84)80171-4. [published data only] [DOI] [PubMed] [Google Scholar]
- Wells 1994.Wells M, McCullough W, Rymer J. Antibiotic prophylaxis in emergency caesarean section. International Journal of Gynecology & Obstetrics. 1994;46:77. [published data only] [Google Scholar]
References to studies awaiting assessment
- Ahued 1994.Ahued Ahued RA, Leal del Rosal JA, Rocha del Valle G, Sereno Colo JA. The efficacy of sulbactam-ampicillin in preventing postoperative infections in gynecology and obstetrics. A comparative open study [Eficacia de sulbactam/ampicilina en la profilaxis de infecciones postquirurgicas en gineco-obstetricia. Estudio abierto comparativo] Ginecologia y Obstetricia de Mexico. 1994;62(9):282–4. [published data only] [PubMed] [Google Scholar]
- Battarino 1988.Battarino O, Battarino A. Short-term antibiotic prophylaxis in cesarean section [La profilassi antibiotica short-time nel taglio cesareo] Minerva Ginecologica. 1988;40:563–7. [published data only] [PubMed] [Google Scholar]
- Garcia 1992.Garcia MH, Garcia I, Doyague MJ, Luna S, Velasco MJ, Lanchares JL, et al. Incidence of urinary infection and other infectious complications in antibiotic prophylaxis of cesaran section with ultra-short schedule. III [Incidencia de infección urinaria y otras complicaciones infecciosas en la profilaxis antibiótica de la cesárea con pauta ultracorta. III] Tokoginecologia Practica. 1992;51(7):349–56. [Google Scholar]
- García MHH, Lajas JA, Velasco MJ, Doyague MJ, Luna S, García A, et al. Incidence of endometritis and infection of surgical wound in antibiotic prophylaxis of cesarean section with ultra-short shedule. II [Incidencia de endometritis e infección en la herida oporatoria en la profilaxis antibiótica de la cesárea con pauta ultracorta. II] Tokoginecologia Practica. 1992;51:340–8. [published data only] [Google Scholar]
- Heilmann 1984.Heilmann L, Tauber PF. Short-term prevention with cefoxitin in cesarean section [Kurzzeitprophylaxe mit Cefoxitin beim Kaiser-schnitt] Geburtshilfe und Frauenheilkunde. 1984;44:792–5. doi: 10.1055/s-2008-1036521. [published data only] [DOI] [PubMed] [Google Scholar]
- Krasnodebski 1997.Krasnodebski J, Stolecki M. A single dose of antibiotic - as a prophylaxis during cesarean section. Ginekologia Polska. 1997;68:30–5. [published data only] [PubMed] [Google Scholar]
- Lemus 2005.Lemus Rocha R, Garcia Gutierrez LB, Basavilvazo Rodriguez MA, Cruz Avelar A, Peralta Pedrero ML, Hernandez Valencia M. Incidence of infected surgical wound and prophylaxis with cefotaxime in cesarean section. Ginecologia y Obstetricia de Mexico. 2005;73(10):537–43. [published data only] [PubMed] [Google Scholar]
- Magro 1983.Magro B, Franchi I, Chehade A, Berti MA, Coppi G. A controlled clinical study of cefuroxim for antimicrobial prophylaxis during obstetric and gynecological surgery [Studio clinico controllato del cefuroxim nella profilassi antimicrobia durante gli interventi chirurgici in ostetricia e ginecologia] Clinica Terapeutica. 1983;105(3):209–14. [published data only] [PubMed] [Google Scholar]
- Oestreicher 1987.Oestreicher M, Oestreicher S, Dudenhausen JW. Prospective study on the question of single-dose antibiotic prophylaxis for primarily indicated abdominal cesarean section(translation) Zeitschrift fur Geburtshilfe und Perinatologie. 1987;191:12–4. [published data only] [PubMed] [Google Scholar]
- Sokolowski 1989.Sokolowski VH, Canzler E, Brotzmann C. Influence of vagimid prophylaxis on course of puerperium and healing of the wound after caesarean section in comparison with a control group. Zentralblatt fur Gynakologie. 1989;111:461–5. [published data only] [PubMed] [Google Scholar]
- Sziller 1994.Sziller I, Karovits J, Erdosi F, Beke A, Oszoli G. Postoperative infectious morbidity after perioperative ampicillin / sulbactam prophylaxis in women undergoing elective caesarean section. Magyar Norvosok Lapja. 1994;57:101–4. [published data only] [Google Scholar]
Additional references
- ACOG 2003.American College of Obstetricians and Gynecologists ACOG practice bulletin number 47, October 2003: prophylactic antibiotics in labor and delivery. Obstetrics & Gynecology. 2003;102:875–82. doi: 10.1016/s0029-7844(03)00984-0. [DOI] [PubMed] [Google Scholar]
- Baker 1995.Baker C, Luce J, Chenoweth C, Friedman C. Comparison of case-finding methodologies for endometritis after cesarean section. American Journal of Infection Control. 1995;23:27–33. doi: 10.1016/0196-6553(95)90005-5. [DOI] [PubMed] [Google Scholar]
- Beattie 1994.Beattie PG, Rings TR, Hunter MF, Lake Y. Risk factors for wound infection following caesarean section. Australian and New Zealand Journal of Obstetrics and Gynaecology. 1994;34:398–402. doi: 10.1111/j.1479-828x.1994.tb01256.x. [DOI] [PubMed] [Google Scholar]
- Bedford Russell 2006.Bedford Russell A, Murch S. Could peripartum antibiotics have delayed health consequences for the infant? BJOG: an international journal of obstetrics and gynaecology. 2006;113:758–65. doi: 10.1111/j.1471-0528.2006.00952.x. [DOI] [PubMed] [Google Scholar]
- Boggess 1996.Boggess KA, Watts DH, Hillier SL, Krohn MA, Benedetti TJ, Eschenbach DA. Bacteremia shortly after placental separation during cesarean delivery. Obstetrics & Gynecology. 1996;87:779–84. doi: 10.1016/0029-7844(96)00037-3. [DOI] [PubMed] [Google Scholar]
- Bratzler 2004.Bratzler DW, Houck PM. Antimicrobial prophylaxis for surgery: an advisory statement from the national surgical infection prevention project. CID. 2004;38:1706–15. doi: 10.1086/421095. [DOI] [PubMed] [Google Scholar]
- Chelmow 2001.Chelmow D, Rueehli MS, Huang E. Prophylactic use of antibiotics for nonlaboring patients undergoing cesarean delivery with intact membranes: a meta-analysis. American Journal of Obstetrics and Gynecology. 2001;184(4):656–61. doi: 10.1067/mob.2001.111303. [DOI] [PubMed] [Google Scholar]
- Classen 1992.Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. New England Journal of Medicine. 1992;326(5):281–6. doi: 10.1056/NEJM199201303260501. [DOI] [PubMed] [Google Scholar]
- Costantine 2008.Costantine MM, Rahman M, Ghulmiyah L, Byers BD, Longo M, Wen T, et al. Timing of perioperative antibiotics for cesarean delivery: a metaanalysis. American Journal of Obstetrics and Gynecology. 2008;199(3):301.e1–301.e6. doi: 10.1016/j.ajog.2008.06.077. [DOI] [PubMed] [Google Scholar]
- Cunningham 1983.Cunningham FG, Leveno KJ, DePalma RT, Roark M, Rosenfeld CR. Perioperative antimicrobials for cesarean delivery: before or after cord clamping. Obstetrics & Gynecology. 1983;62(2):151–4. [PubMed] [Google Scholar]
- Dancer 2004.Dancer SJ. How antibiotics can make us sick: the less obvious adverse effects of antimicrobial chemotherapy. Lancet Infectious Diseases. 2004;6:611–9. doi: 10.1016/S1473-3099(04)01145-4. [DOI] [PubMed] [Google Scholar]
- Declercq 2007.Declercq E, Barger M, Cabral HJ, Evans SR, Kotelchuck M, Simon C, et al. Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstetrics & Gynecology. 2007;109(3):669–77. doi: 10.1097/01.AOG.0000255668.20639.40. [DOI] [PubMed] [Google Scholar]
- Deeks 2001.Deeks JJ, Altman DG, Bradburn MJ, Statistical methods. for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Davey Smith G, Altman DG, editors. Systematic reviews in health care: meta-analysis in context. BMJ Books; London: 2001. [Google Scholar]
- Desjardins 1996.Desjardins C, Diallo HO, Audet-Lapointe P, Harel F. Retrospective study of post-cesarean endometritis. 1992-1993. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction. 1996;25:419–23. [PubMed] [Google Scholar]
- Egger 1997.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrenkrans 1990.Ehrenkranz NJ, Blackwelder WC, Pfaff SJ, Poppe D, Yerg DE, Kaslow RA. Infections complicating low-risk cesarean sections in community hospitals: efficacy of antimicrobial prophylaxis. American Journal of Obstetrics and Gynecology. 1990;162:337–43. doi: 10.1016/0002-9378(90)90381-g. [DOI] [PubMed] [Google Scholar]
- Emmons 1988.Emmons SL, Krohn M, Jackson M, Eschenbach DA. Development of wound infections among women undergoing cesarean section. Obstetrics & Gynecology. 1988;72:559–64. [PubMed] [Google Scholar]
- Enkin 1989.Enkin MW, Enkin E, Chalmers I, Hemminki E. Prophylactic antibiotics in association with caesarean section. In: Chalmers I, Enkin MW, Keirse MJNC, editors. Effective care in pregnancy and childbirth. Oxford University Press; Oxford: 1989. pp. 1246–69. [Google Scholar]
- Galask 1987.Galask RP. Changing concepts in obstetric antibiotic prophylaxis. American Journal of Obstetrics and Gynecology. 1987;157(2):491–7. doi: 10.1016/s0002-9378(87)80201-6. [DOI] [PubMed] [Google Scholar]
- Gates 2008.Gates S. Comparing outcomes by differing incidence of baseline data. 2008. Personal communication. [Google Scholar]
- Gibbs 1980.Gibbs RS. Clinical risk factors for puerperal infection. Obstetrics & Gynecology. 1980;55:178S–183S. doi: 10.1097/00006250-198003001-00045. [DOI] [PubMed] [Google Scholar]
- Gilstrap 1988.Gilstrap LC. Prophylactic antibiotics for cesarean section and surgical procedures. Journal of Reproductive Medicine. 1988;33:588–90. [PubMed] [Google Scholar]
- Harbord 2006.Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Statistics in Medicine. 2006;25:3443–57. doi: 10.1002/sim.2380. [DOI] [PubMed] [Google Scholar]
- Henderson 1995.Henderson E, Love EJ. Incidence of hospital-acquired infections associated with caesarean section. Journal of Hospital Infection. 1995;29:245–55. doi: 10.1016/0195-6701(95)90271-6. [DOI] [PubMed] [Google Scholar]
- Herbert 1999.Herbert PR, Reed G, Entman SS, Mitchel EF, Berg C, Griffin M. Serious maternal morbidity after childbirth: prolonged hospital stays and readmissions. Obstetrics & Gynecology. 1999;94(6):942–7. doi: 10.1016/s0029-7844(99)00419-6. [DOI] [PubMed] [Google Scholar]
- Higgins 2008.The Cochrane Collaboration Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1. 2008 [updated September 2008] Available from www.cochrane-handbook.org.
- Hopkins 1999.Hopkins L, Smaill F. Antibiotic prophylaxis regimens and drugs for cesarean section. Cochrane Database of Systematic Reviews. 1999;(2) doi: 10.1002/14651858.CD001136. DOI: 10.1002/14651858.CD001136. [DOI] [PubMed] [Google Scholar]
- Howey 1990.Howie PW, Davey PG. Prophylactic antibiotics and caesarean section. BMJ. 1990;300:2–3. doi: 10.1136/bmj.300.6716.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulton 1992.Hulton LJ, Olmsted RN, Treston-Aurand J, Craig CP. Effect of postdischarge surveillance on rates of infectious complications after cesarean section. American Journal of Infection Control. 1992;20:198–201. doi: 10.1016/s0196-6553(05)80146-4. [DOI] [PubMed] [Google Scholar]
- Huskins 2001.Huskins WC, Ba-Thike K, Festin MR, Limpongsanurak S, Lumbiganon P, Peedicayil A, et al. An international survey of practice variation in the use of antibiotic prophylaxis in cesarean section. International Journal of Gynecology & Obstetrics. 2001;73(2):141–5. doi: 10.1016/s0020-7292(01)00365-4. [DOI] [PubMed] [Google Scholar]
- Kaimal 2008.Kaimal AJ, Zlatnik MG, Cheng YW, Thiet MP, Connatty E, Creedy P, et al. Effect of a change in policy regarding the timing of prophylactic antibiotics on the rate of postcesarean delivery surgical-site infections. American Journal of Obstetrics and Gynecology. 2008;199(3):310.e1–31.e5. doi: 10.1016/j.ajog.2008.07.009. [DOI] [PubMed] [Google Scholar]
- Killian 2001.Killian CA, Graffunder EM, Vinciguerra TJ, Venezia RA. Risk factors for surgical-site infections following cesarean section. Infection Control and Hospital Epidemiology. 2001;22:613–7. doi: 10.1086/501831. [DOI] [PubMed] [Google Scholar]
- Leigh 1990.Leigh DA, Emmanuel FX, Sedgwick J, Dean R. Post-operative urinary tract infection and wound infection in women undergoing caesarean section: a comparison of two study periods in 1985 and 1987. Journal of Hospital Infection. 1990;15:107–16. doi: 10.1016/0195-6701(90)90119-9. [DOI] [PubMed] [Google Scholar]
- MacLean 1990.MacLean AB. Puerperal pyrexia. In: MacLean AB, editor. Clinical Infection in Obstetrics and Gynecology. Blackwell Scientific Publications; Oxford: 1990. pp. 195–209. [Google Scholar]
- Magann 1995.Magann EF, Washburne JF, Harris RL, Bass JD, Duff WP, Morrison JC. Infectious morbidity, operative blood loss, and length of the operative procedure after cesarean delivery by method of placental removal and site of uterine repair. Journal of the American College of Surgeons. 1995;181:517–20. [PubMed] [Google Scholar]
- Mah 2001.Mah MW, Pyper AM, Oni GA, Memish ZA. Impact of antibiotic prophylaxis on wound infection after cesarean section in a situation of expected high risk. American Journal of Infection Control. 2001;29(2):85–8. doi: 10.1067/mic.2001.111372. [DOI] [PubMed] [Google Scholar]
- Martens 1995.Martens MG, Kolrud BL, Faro S, Maccato M, Hammill H. Development of wound infection or separation after cesarean delivery. Prospective evaluation of 2,431 cases. Journal of Reproductive Medicine. 1995;40:171–5. [PubMed] [Google Scholar]
- Mugford 1989.Mugford M, Kingston J, Chalmers I. Reducing the incidence of infection after caesarean section: implications of prophylaxis for hospital resources. BMJ. 1989;299:1003–6. doi: 10.1136/bmj.299.6706.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NNIS 2004.NNIS A report from the NNIS System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. American Journal of Infection Control. 2004;2004;32(8):470–85. doi: 10.1016/S0196655304005425. [DOI] [PubMed] [Google Scholar]
- OECD 2007.Organization for Economic Co-operation and Development . Health at a Glance 2007: OECD Indicators. Organisation for Economic Co-operation and Development; [accessed 31 October 2009]. http://www.oecd.org/document/11/0,3343,en.2649.33929.16502667.1.1.1.37407,00.html [Google Scholar]
- Olsen 2008.Olsen MA, Butler AM, Willer DM, Devkota P, Gross GA, Fraser VJ. Risk factors for surgical site infection after low transverse cesarean section. Infection Control and Hospital Epidemiology. 2008;29:477–84. doi: 10.1086/587810. [DOI] [PubMed] [Google Scholar]
- Owen 1994.Owen J, Andrews WW. Wound complications after cesarean sections. Clinical Obstetrics and Gynecology. 1994;37:842–55. doi: 10.1097/00003081-199412000-00009. [DOI] [PubMed] [Google Scholar]
- Pedersen 1996.Pedersen TK, Blaakaer J. Antibiotic prophylaxis in cesarean section. Acta Obstetricia et Gynecologica Scandinavica. 1996;75:537–9. doi: 10.3109/00016349609054667. [DOI] [PubMed] [Google Scholar]
- RevMan 2008.RevMan The Cochrane Collaboration . Review Manager (RevMan). 5.0. The Nordic Cochrane Centre: The Cochrane Collaboration; Copenhagen: 2008. [Google Scholar]
- Roberts 1993.Roberts S, Maccato M, Faro S, Pinell P. The microbiology of post-cesarean wound morbidity. Obstetrics & Gynecology. 1993;81:383–6. [PubMed] [Google Scholar]
- Schultz 1995.Schultz KF. Subverting randomization in controlled trials. JAMA. 1995;274:1456–8. [PubMed] [Google Scholar]
- Shlaes 1997.Shlaes DM, Gerding DN, John JJ, Craig WA, Bornstein DL, Duncan RA, et al. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the prevention of antimicrobial resistance in hospitals. Clinical Infectious Diseases. 1997;25:584–99. doi: 10.1086/513766. [DOI] [PubMed] [Google Scholar]
- Suonio 1989.Suonio S, Saarikoski S, Vohlonen I, Kauhanen O. Risk factors for fever, endometritis and wound infection after abdominal delivery. International Journal of Gynecology and Obstetrics. 1989;29:135–42. doi: 10.1016/0020-7292(89)90843-6. [DOI] [PubMed] [Google Scholar]
- Talbot 2005.Talbot TR, Kaiser AB. Postoperative infections and antimicrobial prophylaxis. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 6th Edition Elsevier Inc; Philadelphia: 2005. pp. 3533–47. [Google Scholar]
- Thomas 2006.Thomas J. Rates of cesarean delivery in developing countries suggest unequal access. International Family Planning Perspectives. 2006;32(2):105. [Google Scholar]
- Tita 2009.Tita ATN, Rouse DJ, Blackwell S, Saade GR, Spong CY, Andrews WW. Emerging concepts in antibiotic prophylaxis for cesarean delivery. Obstetrics & Gynecology. 2009;113:675–82. doi: 10.1097/AOG.0b013e318197c3b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts 1990.Watts DH, Krohn MA, Hillier SL, Eschenbach DA. Bacterial vaginosis as a risk factor for post-cesarean endometritis. Obstetrics & Gynecology. 1990;75:52–8. [PubMed] [Google Scholar]
- Watts 1991.Watts DH, Hillier SL, Eschenbach DA. Upper genital tract isolates at delivery as predictors of post-cesarean infection among women receiving antibiotic prophylaxis. Obstetrics & Gynecology. 1991;77:287–92. doi: 10.1097/00006250-199102000-00026. [DOI] [PubMed] [Google Scholar]
- Watts 1992.Watts DH, Krohn MA, Hillier SL, Eschenbach DA. The association of occult amniotic fluid infection with gestational age and neonatal outcome among women in preterm labor. Obstetrics & Gynecology. 1992;79:351–7. doi: 10.1097/00006250-199203000-00005. [DOI] [PubMed] [Google Scholar]
- Wax 1997.Wax JR, Hersey K, Philput C, Wright MS, Nichols KV, Eggleston MK, et al. Single dose cefazolin prophylaxis for postcesarean infections: before vs after cord clamping. Journal of Maternal Fetal Medicine. 1997;6(1):61–5. doi: 10.1002/(SICI)1520-6661(199701/02)6:1<61::AID-MFM13>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Webster 1988.Webster J. Post-caesarean wound infection: a review of the risk factors. Australian and New Zealand Journal of Obstetrics and Gynaecology. 1988;28:210–7. doi: 10.1111/j.1479-828x.1988.tb01664.x. [DOI] [PubMed] [Google Scholar]
- Weinberg 2001.Weinberg M, Fuentes JM, Ruiz AI, Lozano FW, Angel E, Gaitan H, et al. Reducing infections among women undergoing cesarean section in Columbia by means of continuous quality improvement methods. Archives of Internal Medicine. 2001;161:2357–65. doi: 10.1001/archinte.161.19.2357. [DOI] [PubMed] [Google Scholar]
- Westphal 1994.Westphal JF, Vetter D, Brogard JM. Hepatic side-effects of antibiotics. Journal of Antimicrobial Chemotherapy. 1994;33:387–401. doi: 10.1093/jac/33.3.387. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Smaill 1995a.Smaill F, The Cochrane Collaboration . Prophylactic antibiotics for elective Caesarean section [revised 06 May 1993] In: Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP, Crowther C, editors. The Cochrane Pregnancy and Childbirth Database [database on disk and CDROM] 2. Update Software; Oxford: 1995a. Pregnancy and Childbirth Module. [Google Scholar]
- Smaill 1995b.Smaill F. Prophylactic antibiotics in Caesarean section (all trials) [revised 03 August 1994] In: Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP, Crowther C, The Cochrane Collaboration, editors. The Cochrane Pregnancy and Childbirth Database [database on disk and CDROM] 2. Update Software; Oxford: 1995b. Pregnancy and Childbirth Module. [Google Scholar]
- Smaill 2002.Smaill F, Hofmeyr GJ, Smaill FM. Antibiotic prophylaxis for cesarean section. Cochrane Database of Systematic Reviews. 2002;(3) doi: 10.1002/14651858.CD000933. DOI: 10.1002/14651858.CD000933. [DOI] [PubMed] [Google Scholar]