Abstract
Objectives. We examined primary and secondary syphilis cases among men who have sex with men (MSM) in California, and the association of methamphetamine use and Internet use to meet sex partners (Internet use) with number of sex partners.
Methods. We analyzed California surveillance data for MSM who were diagnosed with syphilis between 2004 and 2008, to assess differences in the mean number of sex partners by methamphetamine use and mutually exclusive groups of patients reporting Internet use (Internet users).
Results. Large proportions of patients reported methamphetamine use (19.2%) and Internet use (36.4%). From 2006 through 2008, Adam4Adam was the most frequently reported Web site statewide, despite temporal and regional differences in Web site usage. Methamphetamine users reported more sex partners (mean = 11.7) than nonmethamphetamine users (mean = 5.6; P < .001). Internet users reported more sex partners (mean = 9.8) than non-Internet users (mean = 5.0; P < .001). Multivariable analysis of variance confirmed an independent association of methamphetamine and Internet use with increased numbers of sex partners.
Conclusions. Higher numbers of partners among MSM syphilis patients were associated with methamphetamine and Internet use. Collaboration between currently stand-alone interventions targeting methamphetamine users and Internet users may offer potential advances in sexually transmitted disease control efforts.
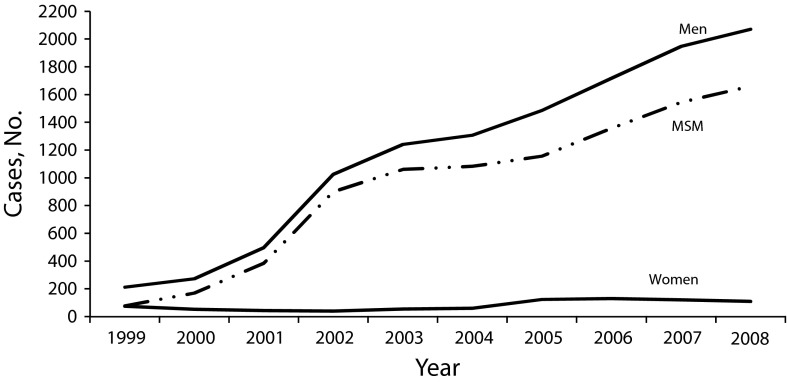
After decades of substantial progress in syphilis control, the number of primary and secondary syphilis cases in California increased each year from 1999 through 2008.1 Prior to 2000, syphilis in California had been primarily among heterosexual populations2,3; however, recent increases have been among men who have sex with men (MSM).1 Similar increases in infectious syphilis cases among MSM have been seen in other metropolitan areas across the United States.4–9
Increasing numbers of MSM have reported using the Internet to meet sex partners10–12 (hereafter referred to simply as “Internet use”); a meta-analysis by Liau et al. placed the figure at approximately 40%.13 Early studies examining the association between Internet use and sexual risk behavior found that MSM who reported seeking sex partners online were more likely to report both higher numbers of partners and more anonymous, unlocatable partners than MSM not seeking partners online.14,15 In San Francisco, an outbreak of syphilis among MSM was linked to seeking sex partners through an online chatroom.16 Several studies also found that individuals using the Internet to seek sex partners were at greater risk for sexually transmitted disease (STD) than individuals not seeking sex partners online.17–19 More recent research suggests that such Internet use is a general marker of individuals who already engage in or seek out high-risk sexual behavior; however, its independent contribution to increasing one’s risk of STD infection is unclear.20–23
An association between methamphetamine use and risky sexual behavior for STD/HIV transmission among MSM has been well documented. A cross-sectional study in San Francisco found that methamphetamine use, particularly in combination with sildenafil (Viagra), was associated with an increased risk of early syphilis infection among MSM seen at an STD clinic.17 Methamphetamine users are more likely than nonmethamphetamine users to report multiple and anonymous sex partners, STD coinfections, and more frequent unprotected anal intercourse with HIV sero-discordant partners or partners with unknown HIV status.24–27
Although methamphetamine use and Internet use have been associated with risky sexual behavior and risk of STD/HIV infection, few studies have examined the effect of these factors together.28,29 We describe the demographics and risk characteristics of MSM primary and secondary syphilis cases diagnosed in California between 2004 and 2008 and, in particular, the relationship of methamphetamine use and Internet use with reported number of sex partners within the year prior to syphilis diagnosis.
METHODS
California laws mandate that laboratories and health care providers report positive syphilis tests and suspected syphilis cases, respectively, to local health departments.30 The stages of syphilis cases were determined according to standard Centers for Disease Control and Prevention (CDC) public health surveillance case definitions.31 Individuals with infectious syphilis are contacted and interviewed by trained disease intervention specialists. Demographic, clinical, and self-reported risk behavior data, as well as information regarding the location of sex partners for the purposes of partner follow-up, are captured by disease intervention specialists using a standardized surveillance and case management form. These data are locally entered into an electronic surveillance database for weekly transmission to the California Department of Public Health. Since MSM make up the majority of syphilis cases in California, and several key variables of interest were dependent on patient self-report, analysis focused on interviewed MSM primary and secondary syphilis cases. To describe more recent and relevant changes in both reported Internet use and Web site trends, we focused on cases diagnosed between January 1, 2004, and December 31, 2008. To provide context for these focused analyses, we included a time trend of syphilis cases from 1999 (earliest year data available) to 2008.
Demographics
We examined frequencies of MSM cases by age, race/ethnicity, sexual orientation (bisexual vs MSM only), and stage of syphilis diagnosis. We classified males as MSM if they reported sex with only male partners in the 12 months prior to syphilis diagnosis, or as bisexual if they reported both male and female sex partners. If gender of sex partner was not available from the patient, information from health care providers was used, if available.
We stratified number of cases and estimated primary and secondary syphilis rates among MSM by 6 California regions, on the basis of residence at time of diagnosis: Northern, Bay Area, San Francisco, Central, Southern, and Los Angeles. To provide the denominator for calculating MSM rates, we used same-sex couple and gay, lesbian, and bisexual population estimates from the 2006 American Community Survey, which indicates that 15% of men in San Francisco are MSM, compared with 5.2% of men in all other California regions.32
Risk Characteristics
HIV status, venues used to meet sex partners, and number of sex partners during the critical period (the interval during which syphilis infection was most likely acquired; i.e., 3 months for primary syphilis and 6 months for secondary syphilis) were based on self-report. We also asked patients about use of specific drugs, including methamphetamines. We further examined the prevalence of methamphetamine use and Internet use in the year prior to syphilis diagnosis and stratified the results by region.
We asked patients reporting Internet use to name specific Web sites used to meet sex partners. Web sites reported by at least 10% of patients seeking sex partners online in any given year from 2004 through 2008 were referred to as “main sites.” We then classified patients into mutually exclusive groups of Internet users (hereafter referred to as “Internet user group”), depending on reported Web sites used. “Single main site” denotes reported exclusive use of a main site. “Multiple sites” denotes reported use of at least 1 main site, in addition to any other main or nonmain Web sites. “Other sites” denotes reported use of 1 or more nonmain Web site only. Patients who reported Internet use but did not name specific Web sites used were classified as “unknown.”
Statistical Analysis
We assessed demographic and risk characteristics using frequency distributions. We used t tests to assess significant differences in the mean number of sex partners for dichotomous variables. We used 1-way analysis of variance (ANOVA) to assess overall significant differences in mean number of sex partners among Internet user group patients and among single main site patients, as well as region.
We used multivariable ANOVA to assess differences in the mean number of sex partners by methamphetamine use and Internet use, adjusting for region. Model 1, which included all interviewed MSM cases, assessed differences by methamphetamine use and Internet use. We also examined HIV status as a potential confounder, given the high HIV coinfection rate among MSM syphilis cases.1 Model 2, which was restricted to cases reporting Internet use, assessed differences by methamphetamine use and Internet user group (single main site, multiple, other, unknown); this model excluded Northern and Central regions because of small numbers. Model 3, which was further restricted to single main site patients, assessed significant differences by methamphetamine use and specific main sites.
We set statistical significance at P < .05 for t test and ANOVA models and used a cutoff of P < .1 for potential interaction terms in the multivariable models. We used manual elimination to remove nonsignificant interactions and main effects in the multivariable models.
In addition to the mean, we assessed the median and the 75th and 95th percentiles to describe the distribution of the number of sex partners. In particular, we examined the 95th percentile to identify subgroups with particularly large numbers of sex partners, which are likely to have an important impact on disease transmission dynamics. We also assessed possible outlier numbers of reported sex partners. After closely examining the partner data, we chose a cutpoint of 200 sex partners to account for the effect of 9 individuals with 200 or more partners, who constituted only 0.15% of interviewed cases from 2004 to 2008 but whose inclusion resulted in an 86% increase in standard deviation (from 13.5 to 25.1). These 9 outliers were subsequently excluded from the multivariable ANOVA models because of their substantial influence on the mean and variance of sex partner estimates. All multivariate models were rerun to include these 9 outliers, with no effect on the key findings for methamphetamine use or Internet use, and only minor changes to the significance of interaction terms. We also excluded patients with missing sex partner data from all analyses related to number of sex partners. We conducted all statistical analyses using SAS version 9.1.3 (SAS Institute, Cary, NC).
RESULTS
The number of primary and secondary syphilis cases in California increased from 285 in 1999 to 1367 in 2004 and to 2179 in 2008 (Figure 1). Of the 9075 primary and secondary syphilis cases diagnosed between 2004 and 2008, 7440 (82.0%) were interviewed. Of those interviewed cases, 5925 (79.6%) were MSM. All further analyses were restricted to these interviewed MSM patients.
FIGURE 1—
Primary and secondary syphilis cases, by gender: California, 1999–2008.
Note. MSM = men who have sex with men.
The majority of these patients were diagnosed with secondary syphilis (71.0%), were White (51.4%), were HIV positive (58.9%, based on patients whose status was known), and reported sex with men only (91.7%; Table 1). The median age was 37 years (range = 14–75 years). The Internet was the most commonly reported venue used to meet sex partners (36.4%), and 19.2% of patients reported using methamphetamines in the year prior to syphilis diagnosis.
TABLE 1—
Characteristics of Interviewed Men Who Have Sex With Men (MSM) Diagnosed With Primary or Secondary Syphilis (n = 5925): California, 2004–2008
| Characteristic | No. (%) |
| Syphilis stage | |
| Primary | 1717 (29.0) |
| Secondary | 4208 (71.0) |
| Race/ethnicity | |
| White | 3046 (51.4) |
| Black | 608 (10.3) |
| Hispanic | 1813 (30.6) |
| Asian | 274 (4.6) |
| Other | 88 (1.5) |
| Unknown | 96 (1.6) |
| Sexual orientation | |
| Bisexual | 491 (8.3) |
| MSM only | 5434 (91.7) |
| HIV statusa | |
| Positive | 3257 (58.9) |
| Negative | 2273 (41.1) |
| Venues used to meet sex partners | |
| Internet | 2154 (36.4) |
| Bars and clubs | 1678 (28.3) |
| Bathhouses and sex clubs | 936 (15.8) |
| Streets | 319 (5.4) |
| Private parties | 326 (5.5) |
| Drug use in past year | |
| Methamphetamines | 1140 (19.2) |
| Poppers | 313 (5.3) |
| Ecstasy | 282 (4.8) |
| Erectile dysfunction drugs | 247 (4.2) |
| Cocaine | 221 (3.7) |
| No. of sex partners in interview period | |
| 1 | 1247 (21.1) |
| 2 | 1170 (19.8) |
| 3–4 | 1296 (21.9) |
| 5–9 | 905 (15.3) |
| 10–49 | 837 (14.1) |
| 50–99 | 100 (1.7) |
| 100–199 | 41 (0.7) |
| 200–499 | 5 (0.08) |
| ≥ 500 | 4 (0.07) |
| Missing | 320 (5.4) |
Note. The median age of patients was 37 years (range = 14–75 years). The median number of sex partners during the interview period was 3; for the 95th percentile, the number was 25.
A total of 395 patients did not know or refused to disclose their HIV status.
The majority of both primary and secondary patients reported 1 to 4 sex partners (67.7% and 60.6%, respectively), with a median of 3 sex partners, regardless of syphilis stage. The 95th percentile of number of sex partners was 25; a relatively small proportion of patients (0.85%) reported 100 or more sex partners, with 5 patients reporting 200 to 499 sex partners and 4 patients reporting more than 500 sex partners (Table 1).
Regionally, the majority of cases were diagnosed in the Los Angeles, Southern California, and San Francisco regions, with San Francisco having by far the highest estimated syphilis rate among MSM statewide (331.6 per 100 000 population; Table 2). Patients from the San Francisco, Central, and Southern regions reported the highest proportions of Internet use (44.5%, 41.5%, and 40.0%, respectively), and the highest proportions of methamphetamine use were reported from the San Francisco (26.6%) and Southern (23.3%) regions. Reported Internet use and methamphetamine use were low in Los Angeles and Northern California, compared with other regions (Table 2).
TABLE 2—
Internet and Methamphetamine Use Among Interviewed Primary and Secondary Syphilis Patients Who Were Men Who Have Sex With Men (MSM), by Region: California, 2004–2008
| Regiona | MSM With Syphilis, No. (%) | Syphilis Rateb per 100 000 | Internet Use, No. (%) | Methamphetamine Use, No. (%) | No. of Sex Partners,c Mean (95% CI) |
| Northern | 176 (3.0) | 33.5 | 46 (26.1) | 18 (10.2) | 4.9 (2.7, 7.0) |
| Bay Area | 545 (9.6) | 68.9 | 214 (37.9) | 107 (18.9) | 5.5 (4.7, 6.3) |
| San Francisco | 1046 (17.7) | 331.6 | 465 (44.5) | 278 (26.6) | 10.1 (9.1, 11.1) |
| Central | 82 (1.4) | 19.2 | 34 (41.5) | 15 (18.3) | 3.9 (2.8, 4.9) |
| Southern | 2002 (33.8) | 116.0 | 800 (40.0) | 467 (23.3) | 6.0 (5.5, 6.6) |
| Los Angeles | 2045 (34.6) | 164.6 | 589 (28.8) | 253 (12.4) | 6.5 (5.8, 7.1) |
Note. CI = confidence interval. Cases with outlier partner data (≥ 200 partners) are excluded. “Internet use” means use of Internet to meet sex partners.
Jurisdictions were as follows: Northern region: Alpine, Amador, Butte, Calaveras, Colusa, Del Norte, El Dorado, Glenn, Humboldt, Lake, Lassen, Mendocino, Modoc, Nevada, Placer, Plumas, Sacramento, San Joaquin, Shasta, Sierra, Siskiyou, Sutter, Tehama, Trinity, Yolo, and Yuba; Bay Area region: Alameda, Berkeley, Contra Costa, Marin, Napa, San Mateo, Santa Clara, Solano, and Sonoma; Central region: Fresno, Inyo, Kings, Madera, Mariposa, Merced, Mono, Monterey, San Benito, Santa Cruz, Stanislaus, Tuolumne, and Tulare; Southern region: Imperial, Kern, Long Beach, Orange, Pasadena, Riverside, San Bernardino, San Diego, San Luis Obispo, Santa Barbara, and Ventura.
We calculated the San Francisco rate using a 15.4% estimate of male population for the MSM population denominator. For all other regions, we used a 5.2% estimate of male population.
Sex partner statistics exclude cases with missing partner data.
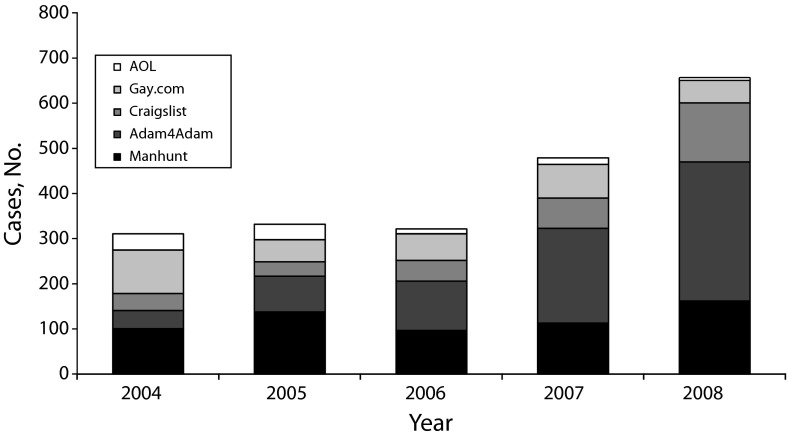
Five Web sites were reported by at least 10% of cases seeking sex partners online in any given year from 2004 through 2008: Adam4Adam.com, AOL.com, Craigslist.org, Gay.com, and Manhunt.net. Although AOL was more commonly reported from 2004 to 2005, reported use of this Web site decreased substantially in subsequent years. In 2004 and 2005, Manhunt was the most frequently reported Web site among cases seeking sex partners online, whereas Adam4Adam has been the most frequently reported Web site among MSM syphilis cases since 2006 (Figure 2).
FIGURE 2—
Reported Internet sites used to meet sex partners in past year among men who have sex with men diagnosed with primary and secondary syphilis: California, 2004–2008.
Note. Use of Internet sites is not mutually exclusive (i.e., individuals might have used > 1 site).
Web sites used to meet sex partners also differed by region. Among San Francisco cases, Manhunt (34.6%) was the most frequently reported Web site used, whereas relatively fewer cases reported using Adam4Adam (11.4%). By contrast, Adam4Adam was the most frequently reported Web site among patients in the Southern (51.1%) and Northern (38.8%) regions. Cases in the Bay Area and Central regions reported less use of Adam4Adam and Manhunt, compared with use of Gay.com and Craigslist (data not shown).
Internet Use and Methamphetamine Use (Model 1)
Of the 5916 patients diagnosed between 2004 and 2008, 1138 (19.2%) reported methamphetamine use and 2148 (36.3%) reported using the Internet to meet sex partners in the year prior to syphilis diagnosis (Table 3).
TABLE 3—
Bivariate and Multivariate Analysis of Number of Sex Partners Among Interviewed Men Who Have Sex With Men (MSM) Diagnosed With Primary or Secondary Syphilis, by Methamphetamine and Internet Use: California, 2004–2008
| Sex Partner Statisticsa |
|||||||||
| Model | Total No. | Meth Use, No. (%) | No. of Cases | No. of Sex Partners, Mean (95% CI) | Median | 75th Percentile | 95th Percentile | Bivariate Pb | Multivariate P |
| Overall | 5916 | 1138 (19.2) | 5596 | 6.8 (6.4, 7.2) | 3.0 | 6.0 | 25.0 | ||
| Model 1c | |||||||||
| Nonmeth users | 4778 | … | 4491 | 5.6 (5.3, 5.9) | 3.0 | 5.0 | 20.0 | < .001 | < .001 |
| Meth users | 1138 | 1138 (100.0) | 1105 | 11.7 (10.4, 13.0) | 5.0 | 10.0 | 50.0 | ||
| No Internet use | 3768 | 538 (14.3) | 3508 | 5.0 (4.6, 5.4) | 2.0 | 4.0 | 19.0 | < .001 | < .001 |
| Internet use | 2148 | 600 (27.9) | 2088 | 9.8 (9.1, 10.5) | 5.0 | 10.0 | 36.0 | ||
| Model 2d (Internet users only) | < .001 | .04 | |||||||
| Single site | 1082 | 280 (25.9) | 1056 | 8.2 (7.4, 9.1) | 4.0 | 8.0 | 30.0 | ||
| Multiple sites | 564 | 199 (35.3) | 554 | 14.1 (12.3, 15.8) | 7.0 | 15.0 | 50.0 | ||
| Other sites | 228 | 56 (24.5) | 222 | 9.1 (6.7, 11.5) | 4.0 | 8.0 | 40.0 | ||
| Unknown | 274 | 65 (23.7) | 256 | 7.8 (6.3, 9.3) | 4.0 | 8.0 | 24.0 | ||
| Single-site users | |||||||||
| Model 3e (single-site users only) | < .001 | < .001 | |||||||
| Adam4Adam | 424 | 124 (29.3) | 416 | 7.2 (6.1, 8.4) | 3.5 | 7.0 | 25.0 | ||
| Manhunt | 274 | 98 (35.8) | 266 | 12.0 (9.5, 14.4) | 5.0 | 10.0 | 50.0 | ||
| Craigslist | 168 | 25 (14.9) | 162 | 7.0 (5.4, 8.7) | 4.0 | 7.0 | 20.0 | ||
| Gay.com | 172 | 22 (12.8) | 171 | 5.6 (4.2, 7.0) | 3.0 | 6.0 | 16.0 | ||
| AOL.com | 44 | 11 (25.0) | 41 | 9.9 (4.1, 15.6) | 4.0 | 8.0 | 50.0 | ||
Note. CI = confidence interval; meth = methamphetamine.
Sex partner statistics exclude cases with missing sex partner data.
P values for bivariate analysis were determined by the t test and 1-way analysis of variance.
For model 1, results for only Internet use and meth use are displayed. Bivariate analysis included (1) meth use, (2) Internet use, and (3) region (P < .001). For multivariate analysis, additional variables retained in the final model were region (P < .001), Internet use and meth use interaction (P = .01), and meth use and region interaction (P < .001).
For model 2, results for only Internet user groups are displayed. Bivariate analysis included (1) meth use (P < .001), (2) Internet user groups, and (3) region (P < .001). For multivariate analysis, additional variables retained in the final model were meth use (P < .001), region (P < .001), Internet user group and region interaction (P = .002), and meth use and region interaction (P = .02). Model 2 excluded Northern and Central regions.
For model 3, results for only single main sites are displayed. Bivariate analysis included (1) meth use (P < .001), (2) single main sites, and (3) region (P = .059). For multivariate analysis, additional variables retained in the final model were single main sites and meth use interaction (P = .03), meth use and region interaction (P = .096), and nonsignificant-terms meth use (P = .26) and region (P = .18).
Methamphetamine users reported significantly more sex partners (mean = 11.7; 95% confidence interval [CI] = 10.4, 13.0) than did nonmethamphetamine users (mean = 5.6; 95% CI = 5.3, 5.9; P < .001). Patients reporting Internet use reported significantly more sex partners (mean = 9.8; 95% CI = 9.1, 10.5) than did those not reporting Internet use (mean = 5.0; 95% CI = 4.6, 5.4; P < .001; Table 3). Significant differences in mean number of sex partners were also found by region (P < .001), with San Francisco patients reporting the highest number of sex partners (mean = 10.1; 95% CI = 9.1, 11.1) and Central region patients reporting the least number of sex partners (mean = 3.9; 95% CI = 2.8, 4.9).
Model 1 indicated that methamphetamine use (P < .001), Internet use (P < .001), and region (P < .001) were independently associated with higher numbers of sex partners (Table 3). Interaction was observed between methamphetamine use and Internet use (P = .01): methamphetamine users had a larger difference in mean number of sex partners between Internet and non-Internet users (n = 5.9) than did nonmethamphetamine users (n = 3.6). Interaction was also observed between methamphetamine use and region (P < .001); for example, Los Angeles methamphetamine users reported an average of 9.1 more sex partners than did nonmethamphetamine users, whereas almost no difference was observed in the Central region.
Although bivariable analysis showed that HIV-positive patients (mean = 7.2) reported a significantly higher mean number of sex partners than either HIV-negative patients (mean = 6.6) or those whose HIV status was unknown or who refused to disclose it (mean = 5.1; P = .01), HIV infection (and related interaction terms) was nonsignificant in model 1 and was therefore excluded from further multivariable analyses.
Internet User Group and Methamphetamine Use (Model 2)
Of the 2148 patients reporting Internet use, 50.4% were classified as single-main-site users, 26.3% as multiple-site users, 10.6% as other-site users, and 12.8% as unknown (Table 3). Among multiple-site users, 56.9% reported using only the top 5 Web sites that met the 10% criteria (i.e., Adam4Adam, Manhunt, Craigslist, Gay.com, AOL). There were significant differences in the number of sex partners among Internet user group categories, as follows: single main site (mean = 8.2; 95% CI = 7.4, 9.1), multiple sites (mean = 14.1; 95% CI = 12.3, 15.8), other sites (mean = 9.1; 95% CI = 6.7, 11.5), and unknown (mean = 7.8; 95% CI = 6.3, 9.3; P < .001). Multiple-site users also reported the highest proportion of methamphetamine use among Internet user groups (35.3%), followed by single-site users (25.9%).
Model 2 indicated that methamphetamine use (P < .001), Internet user group (P = .04), and region (P < .001) remained independently associated with mean number of sex partners (Table 3). We found significant interaction between region and methamphetamine use (P = .02) and between Internet user group and region (P = .002).
Single Main Sites and Methamphetamine Use (Model 3)
Among the 1082 single-main-site users, Adam4Adam was the most frequently reported Web site (n = 424; 39.2%), followed by Manhunt (n = 274; 25.3%). Patients using Manhunt reported the most sex partners (mean = 12.0; 95% CI = 6.1, 8.4), followed by AOL.com (mean = 9.9; 95% CI = 4.1, 15.6) and Adam4Adam (mean = 7.2; 95% CI = 6.1, 8.4). Patients exclusively using Gay.com to meet sex partners reported the least number of sex partners (mean = 5.6; 95% CI = 4.2, 7.0; P < .001). Patients reporting exclusive use of Manhunt also reported the highest proportion of methamphetamine use (35.8%), followed by Adam4Adam users (29.3%). Patients using Gay.com reported the lowest proportion of methamphetamine use (25.0%; Table 3).
Model 3 showed that mean number of sex partners was significantly associated with single main site use (P < .001; Table 3). We found significant interaction between single main site use and methamphetamine use (P = .03); for example, among Manhunt.com users, those using methamphetamines reported an average of 9.2 more sex partners than those not using methamphetamines, whereas among Gay.com and AOL users, this difference was only 0.4 and 0.3 sex partners, respectively. We also observed regional differences in mean number of sex partners by methamphetamine use, ranging from 1.7 to 12.5 sex partners (P = .096; data not shown).
Ninety-Fifth Percentile
Beyond differences in the mean number of sex partners, we observed important findings related to STD transmission dynamics in the extreme distributions of number of sex partners; the 95th percentile of the number of sex partners was 50 among methamphetamine users compared with 20 among nonmethamphetamine users. Similarly, the 95th percentile among patients reporting Internet use was 40 sex partners, compared with 20 among patients not seeking sex partners online. Among single-main-site users, the highest 95th percentile of number of sex partners was among patients using Manhunt and AOL.com (50 sex partners each), although the latter was the least frequently reported Web site used (n = 44). The independent contributions of Internet use and methamphetamine use resulted in the highest mean and 95th percentile of number of sex partners among patients reporting both risk factors (mean = 14.5; 95% CI = 12.6, 16.4; 95th percentile = 50), compared with nonmethamphetamine users who did not report seeking sex partners online (mean = 4.4; 95% CI = 4.1, 4.7; 95th percentile = 15; data not shown). This relationship did not change when the 9 cases with 200 or more sex partners were included.
DISCUSSION
The number of infectious syphilis cases in California increased 629% between 1999 and 2008 and 58.5% between 2004 and 2008, with MSM accounting for a high proportion of cases during this period. Just more than one third of patients from 2004 to 2008 reported using the Internet to meet sex partners, demonstrating the importance of the Internet among MSM for partner selection and potential expansion of social and sexual networks. About one fifth of patients reported methamphetamine use, and its association with higher numbers of sex partners also points to the potentially important role it plays in sexual networks and increased likelihood of syphilis and other STD transmission.
Use of specific Web sites to meet sex partners varied over time. Use of commonly reported Web sites in 2004 decreased in subsequent years, whereas others (e.g., Adam4Adam and Manhunt) emerged as the most commonly reported Web sites statewide in recent years. Regional differences in reported use of particular Web sites indicate the need for Internet-specific interventions that incorporate an understanding of geographic Web site trends.
Our observation that patients meeting sex partners on emerging Web sites (e.g., Adam4Adam and Manhunt) were more likely to report higher proportions of methamphetamine use than users of other less commonly reported Web sites suggests the opportunity for targeted interventions that address drug use among individuals seeking sex partners online. It also points to the possibility of using Web sites as markers of network involvement and risky behavior, as recent research indicates that individuals with a tendency toward high-risk behaviors use the Internet to meet partners.20–23 Furthermore, our finding that Internet use and methamphetamine use were independently associated with higher numbers of sex partners in all models, and that persons reporting both methamphetamine use and Internet use had very high means and 95th percentiles of sex partners, suggests that individuals engaged in both activities may play an important role in ongoing disease transmission, particularly since the Internet offers an increasingly efficient, user-friendly, and expansive medium by which high-risk individuals can form new drug-related or sexual partnerships. Interventions should also consider how various Web site characteristics, such as free or low-cost membership, wide reach, partner and risk selection methods, and options for information disclosure, may appeal to different types of users with varying levels of risk-seeking behavior.33
Local health jurisdictions, particularly those with rising infectious syphilis rates, have developed innovative, Internet-based, public health interventions in response to increasing numbers of individuals seeking sex partners online. These interventions include e-mail partner notification, online health message boards, interactive chats, banner ads, and online laboratory slips for STD/HIV testing.34,35 One challenge to such interventions is the inability to geo-target advertising on some Web sites, thus disinclining health departments to pay for health messages or advertising not specific to their jurisdictions. Innovative drug treatment and harm reduction programs have also been developed to eliminate methamphetamine dependency and modify sexual risk behaviors that facilitate the spread of STD/HIV.36 Combining expertise and resources from these 2 intervention efforts could help address high-risk behaviors that contribute to STD infection. Additionally, new technology, such as smart mobile devices, provides individuals with constant access to the Internet and Web-based social and sexual networks. This, in conjunction with the rapid emergence of new social networking Web sites specifically suited to these new technologies, demands consistent communication with field staff and ongoing, systematic review of syphilis case interviews for development of effective and relevant interventions for reducing Internet-associated STD transmission.
Limitations
This analysis is subject to several limitations. Individuals were asked about Internet use and methamphetamine use in the past 12 months, whereas number of partners referred to the past 3 or 6 months. Although substantial changes in behavior within this relatively short time frame seem unlikely to be common, our data did not allow assessment of whether reported sex partners were in fact met online or through another venue. The proportion of MSM seeking sex partners online and using methamphetamines may also be underestimated, since all risk behavior data were based on self-report. However, field staff are skilled in developing rapport with persons they interview and are experienced in discussing stigmatized behaviors with sensitivity.
If the distribution of any of our key variables varied by syphilis stage, the differing time frames for primary vs secondary syphilis cases could have created a potential bias. We were further limited by our inability to extrapolate partner data from 3 to 6 months, or vice versa. Stratification of our variables of interest by syphilis stage did not yield any significant differences in the association with number of sex partners.
A small proportion of patients could not be located for interview, creating potential for bias, since noninterviewed and interviewed patients may differ with respect to key risk characteristics or sexual networks. In addition, methamphetamine use in Los Angeles was probably underestimated, as anecdotal field reports suggest that a higher proportion of patients used methamphetamines than the figure we were able to derive from the free-text drug use variable available for syphilis case interviews in Los Angeles.
Specific Internet Web sites used to meet sex partners are recorded as free text in the California syphilis surveillance and case management record, leaving room not only for misspelling and data entry errors but also for multiple Web sites being entered into a single, open-ended field. Although programming allowed for individual extraction and analysis of more commonly reported Web sites, the many less frequently reported “other” sites were not individually analyzed. In addition, these analyses did not take into account other venues where individuals may seek out sex partners, in addition to or instead of the Internet (e.g., bars and clubs, bathhouses and sex clubs, circuit parties).
Finally, the syphilis epidemic in California is primarily among non-Hispanic White MSM, and therefore our findings may not be generalizable to areas experiencing syphilis increases among heterosexual or different racial/ethnic communities.
Conclusions
Infectious syphilis in California continues to increase, particularly among MSM. Both methamphetamine use and Internet use are significantly associated with higher numbers of partners, indicating an important role in ongoing STD transmission. Collaboration between existing but currently stand-alone interventions for methamphetamine dependency and Internet use may offer potential advances in syphilis and other STD control efforts. Our analysis highlights the need for continuous monitoring of Internet venues that may be potential targets for successful intervention, given the nature of Web site use and the frequency with which Web sites fall in and out of popularity among MSM syphilis patients in California.
Acknowledgments
This work was conducted through the regular duty of authors employed at the California Department of Public Health, San Francisco Department of Public Health, Los Angeles County Department of Public Health, and Department of Medicine, University of California, Los Angeles. The work of authors from the California Department of Public Health was funded by the Centers for Disease Control and Prevention’s Comprehensive STD Prevention Systems (grant 5H25PS001379-04).
Human Participant Protection
No protocol approval was necessary for this study because routine surveillance data collected for public health purposes were used.
References
- 1.State of California Syphilis Elimination Surveillance Data. 2008. Sacramento, CA: California Dept of Public Health, STD Control Branch; 2009 [Google Scholar]
- 2.Continuing increase in infectious syphilis—United States. MMWR Morb Mortal Wkly Rep. 1988;37(3):35–38 [PubMed] [Google Scholar]
- 3.Current trends increases in primary and secondary syphilis—United States. MMWR Morb Mortal Wkly Rep. 1987;36(25):393–397 [PubMed] [Google Scholar]
- 4.D’Souza G, Lee JH, Paffel JM. Outbreak of syphilis among men who have sex with men in Houston, Texas. Sex Transm Dis. 2003;30(12):872–873 [DOI] [PubMed] [Google Scholar]
- 5.Primary and secondary syphilis among men who have sex with men—New York City, 2001. MMWR Morb Mortal Wkly Rep. 2002;51(38):853–856 [PubMed] [Google Scholar]
- 6.Primary and secondary syphilis—Jefferson county, Alabama, 2002–2007. MMWR Morb Mortal Wkly Rep. 2009;58(17):463–467 [PubMed] [Google Scholar]
- 7.Resurgent bacterial sexually transmitted disease among men who have sex with men—King County, Washington, 1997–1999. MMWR Morb Mortal Wkly Rep. 1999;48(35):773–777 [PubMed] [Google Scholar]
- 8.Peterman TA, Heffelfinger JD, Swint EB, Groseclose SL. The changing epidemiology of syphilis. Sex Transm Dis. 2005;32(10 suppl):S4–S10 [DOI] [PubMed] [Google Scholar]
- 9.Bronzan R, Echavarria L, Hermida J, Trepka M, Burns T, Fox K. Syphilis among men who have sex with men in Miami-Dade County, Florida [abstract P135]. Poster presented at: 2002 National STD Prevention Conference; March 4–7, 2002; San Diego, CA. Available at: http://www.cdc.gov/stdconference/2002/2002ConfAbPoster6.htm#P135. Accessed September 14, 2012
- 10.Ross MW, Rosser BR, McCurdy S, Feldman J. The advantages and limitations of seeking sex online: a comparison of reasons given for online and offline sexual liaisons by men who have sex with men. J Sex Res. 2007;44(1):59–71 [DOI] [PubMed] [Google Scholar]
- 11.Bull SS, McFarlane M. Soliciting sex on the Internet: what are the risks for sexually transmitted diseases and HIV? Sex Transm Dis. 2000;27(9):545–550 [DOI] [PubMed] [Google Scholar]
- 12.Rietmeijer CA, Bull SS, McFarlane M. Sex and the Internet. AIDS. 2001;15(11):1433–1434 [DOI] [PubMed] [Google Scholar]
- 13.Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sex Transm Dis. 2006;33(9):576–584 [DOI] [PubMed] [Google Scholar]
- 14.Horvath KJ, Rosser BR, Remafedi G. Sexual risk taking among young Internet-using men who have sex with men. Am J Public Health. 2008;98(6):1059–1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. JAMA. 2000;284(4):443–446 [DOI] [PubMed] [Google Scholar]
- 16.Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA. 2000;284(4):447–449 [DOI] [PubMed] [Google Scholar]
- 17.Wong W, Chaw JK, Kent CK, Klausner JD. Risk factors for early syphilis among gay and bisexual men seen in an STD clinic: San Francisco, 2002–2003. Sex Transm Dis. 2005;32(7):458–463 [DOI] [PubMed] [Google Scholar]
- 18.Elford J, Bolding G, Sherr L. Seeking sex on the Internet and sexual risk behaviour among gay men using London gyms. AIDS. 2001;15(11):1409–1415 [DOI] [PubMed] [Google Scholar]
- 19.Taylor M, Aynalem G, Smith L, Bemis C, Kenney K, Kerndt P. Correlates of Internet use to meet sex partners among men who have sex with men diagnosed with early syphilis in Los Angeles County. Sex Transm Dis. 2004;31(9):552–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jenness SM, Neaigus A, Hagan H, Wendel T, Gelpi-Acosta C, Murrill CS. Reconsidering the Internet as an HIV/STD risk for men who have sex with men. AIDS Behav. 2010;14(6):1353–1361 [DOI] [PubMed] [Google Scholar]
- 21.Al-Tayyib AA, McFarlane M, Kachur R, Rietmeijer CA. Finding sex partners on the Internet: what is the risk for sexually transmitted infections? Sex Transm Infect. 2009;85(3):216–220 [DOI] [PubMed] [Google Scholar]
- 22.Chiasson MA, Hirshfield S, Remien RH, Humberstone M, Wong T, Wolitski RJ. A comparison of on-line and off-line sexual risk in men who have sex with men: an event-based on-line survey. J Acquir Immune Defic Syndr. 2007;44(2):235–243 [DOI] [PubMed] [Google Scholar]
- 23.Ogilvie GS, Taylor DL, Trussler Tet al. Seeking sexual partners on the Internet: a marker for risky sexual behaviour in men who have sex with men. Can J Public Health. 2008;99(3):185–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colfax GN, Mansergh G, Guzman Ret al. Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: a venue-based comparison. J Acquir Immune Defic Syndr. 2001;28(4):373–379 [DOI] [PubMed] [Google Scholar]
- 25.Taylor MM, Aynalem G, Smith LV, Montoya J, Kerndt P. Methamphetamine use and sexual risk behaviors among men who have sex with men diagnosed with early syphilis in Los Angeles County. Int J STD AIDS. 2007;18(2):93–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garofalo R, Mustanski BS, McKirnan DJ, Herrick A, Donenberg GR. Methamphetamine and young men who have sex with men: understanding patterns and correlates of use and the association with HIV-related sexual risk. Arch Pediatr Adolesc Med. 2007;161(6):591–596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirshfield S, Remien RH, Walavalkar I, Chiasson MA. Crystal methamphetamine use predicts incident STD infection among men who have sex with men recruited online: a nested case–control study. J Med Internet Res. 2004;6(4):e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wohlfeiler D, Potterat JJ. Using gay men’s sexual networks to reduce sexually transmitted disease (STD)/human immunodeficiency virus (HIV) transmission. Sex Transm Dis. 2005;32(10 suppl):S48–S52 [DOI] [PubMed] [Google Scholar]
- 29.Toomey KE, Rothenberg RB. Sex and cyberspace-virtual networks leading to high-risk sex. JAMA. 2000;284(4):485–487 [DOI] [PubMed] [Google Scholar]
- 30. Title 17, California Code of Regulations, §2500, Reportable Diseases and Conditions.
- 31.Case definitions for infectious conditions under public health surveillance Centers for Disease Control and Prevention. MMWR Recomm Rep. 1997;46(RR-10):1–55 [PubMed] [Google Scholar]
- 32.Gates GJ. Same-sex couples and the gay, lesbian, bisexual population: new estimates from the American Community Survey. 2006. Available at: http://escholarship.org/uc/item/8h08t0zf. Accessed June 29, 2010
- 33.Wohlfeiler DHJ, Raymond HF, Kennedy T, McFarland W. How Can We Improve HIV and STD Prevention Online for MSM? Assessing the Preferences of Website Owners, Website Users, and HIV/STD Directors. Washington, DC: Foundation for AIDS Research; 2011 [Google Scholar]
- 34.Anderton JP, Valdiserri RO. Combating syphilis and HIV among users of Internet chatrooms. J Health Commun. 2005;10(7):665–671 [DOI] [PubMed] [Google Scholar]
- 35.Klausner JD, Levine DK, Kent CK. Internet-based site-specific interventions for syphilis prevention among gay and bisexual men. AIDS Care. 2004;16(8):964–970 [DOI] [PubMed] [Google Scholar]
- 36.Strona FV, McCright J, Hjord Het al. The acceptability and feasibility of the Positive Reinforcement Opportunity Project, a community-based contingency management methamphetamine treatment program for gay and bisexual men in San Francisco. J Psychoactive Drugs. 2006;(suppl 3):377–383 [DOI] [PubMed] [Google Scholar]