Abstract
Objectives. Medical marijuana laws (MMLs) have been suggested as a possible cause of increases in marijuana use among adolescents in the United States. We evaluated the effects of MMLs on adolescent marijuana use from 2003 through 2011.
Methods. We used data from the Youth Risk Behavior Survey and a difference-in-differences design to evaluate the effects of passage of state MMLs on adolescent marijuana use. The states examined (Montana, Rhode Island, Michigan, and Delaware) had passed MMLs at different times over a period of 8 years, ensuring that contemporaneous history was not a design confound.
Results. In 40 planned comparisons of adolescents exposed and not exposed to MMLs across states and over time, only 2 significant effects were found, an outcome expected according to chance alone. Further examination of the (nonsignificant) estimates revealed no discernible pattern suggesting an effect on either self-reported prevalence or frequency of marijuana use.
Conclusions. Our results suggest that, in the states assessed here, MMLs have not measurably affected adolescent marijuana use in the first few years after their enactment. Longer-term results, after MMLs are more fully implemented, might be different.
The presence of marijuana in the United States was first recorded in 1611 and the substance remained largely unregulated until the beginning of the 20th century (for a review of historical legislation on marijuana in the United States, see Pacula et al.1). Before the 20th century, marijuana was commonly prescribed by physicians for a variety of medical conditions. A rise in nonmedical marijuana use in the early part of the 20th century, coupled with societal reform on the recreational use of many substances (including alcohol), resulted in the first legislation aimed at regulating marijuana in the United States. Since then the legal status of marijuana has evolved; the drug became progressively more regulated through the 1970s, at which point marijuana was categorized as a Schedule I drug (illegal under federal law, with no currently accepted medical use) according to the Federal Controlled Substances Act.2
After the federal government classified marijuana as a Schedule I drug, states began passing their own legislation that addressed the medical use of marijuana.1 Most state legislation was specific to research programs or did not include provisions protecting physicians and patients from penalties, and as such these laws did not really promote the medical use of marijuana. California passed the first medical marijuana law (MML) that included broad protections for patients and physicians in 1996, and since then 17 states and the District of Columbia have passed MMLs.
MMLs typically contain legal provisions that cover 4 dimensions of medical marijuana regulation (Table 1). The first is the establishment of a state registry or identification cards for patients prescribed medical marijuana. The second dimension refers to state regulation of the practice of medicine (e.g., regulation of the patient–physician relationship, disease or condition limitations, and prohibition of disciplinary action or denial of privileges of a physician). Third, states can be arrayed according to their regulation of access to marijuana, including possession and cultivation limitations as well as retail–dispensary regulation. Finally, state MMLs are distinguished on the basis of affirmative defenses and legal protections for the medical marijuana patient, including protection from prosecution.
TABLE 1—
Medical Marijuana Laws Enacted in the United States, November 1996 Through May 2011
| Type of Provision |
|||||||
| State | Legislation | Effective Date | Registry/Identification Cards | Regulation of Practice of Medicine | Possession and Cultivation Limits | Dispensary/Retail | Affirmative Defenses/Legal Protections |
| California | California Compassionate Use Act of 1996, Cal. Health & Safety Code, §11362.5 (1996), Cal. Health & Safety Code, §§11362.7–11362.83 | November 6, 1996 (amended January 1, 2004) | Yes | Yes | Yes | Yes | Yes |
| Washington | Wash. Rev Code §§69.51A– 69.51A.901 (2007) | November 3, 1998 (amended November 2, 2008, and June 10, 2010) | No | Yes | Yes | No | Yes |
| Oregon | Ore. Rev Stat §475.300 (2007) | December 3, 1998 (amended 1999) | Yes | Yes | Yes | No | Yes |
| Alaska | Alaska Stat §§17.37.10–17.37.80 (2007) | March 4, 1999 | Yes | Yes | Yes | No | Yes |
| Maine | Me. Rev Stat Title 22 Health and Welfare, Ch. 558-C, Maine Medical Use of Marijuana Act | December 22, 1999 | Yes | Yes | Yes | Yes | Yes |
| Hawaii | Haw. Rev Stat §§329-121–329-128 (2008) | December 28, 2000 | Yes | Yes | Yes | No | Yes |
| Colorado | Colo. Const. art. XVIII, §14 (2001), Colo. Rev Stat §18-18-406.3 (2001), Colo. Rev Stat §25-1.5-106 (2003), Colo. Rev Stat §12-43.3 (2010) | June 1, 2001 | Yes | Yes | Yes | Yes | Yes |
| Nevada | Medical Use of Marijuana, ch. 453A, Nev. Rev Stat Ann. §§453A.010–810 (2011) | October 1, 2001 | Yes | Yes | Yes | No | Yes |
| Maryland | Md. Code Ann., Criminal Law §5-601(c)3(II) (2003) | January 1, 2003 | No | No | No | No | Yes |
| Vermont | Vt. Stat Ann. Title 18, §§4471–4474d (2003) | July 1, 2004 | Yes | Yes | Yes | Yes | Yes |
| Montana | Montana Medical Marijuana Act, Mont. Code Ann. §§50-46-101–210 (2010) | November 2, 2004 | Yes | Yes | Yes | Yes | Yes |
| Rhode Island | Edward O. Hawkins and Thomas C. Slater Medical Marijuana Act, R.I. Gen. Laws Ann. §§21-28.6-1–21-28.6-12 (2006) | January 3, 2006 | Yes | Yes | Yes | Yes | Yes |
| New Mexico | N.M. Stat Ann. §30-31C-1 (2007) | July 1, 2007 | Yes | Yes | Yes | Yes | Yes |
| Michigan | Mich. Comp. Law §§333.26421–333.26430 (2008) | December 4, 2008 | Yes | Yes | Yes | No | Yes |
| District of Columbia | District of Columbia Official Code, Title 7, Human Health Care and Safety, Subtitle G-ii, Chapter 16B, Use of Marijuana for Medical Treatment, D.C. Code §§7-1671.02–7-1671.13 (2010) | May 1, 2010 | Yes | Yes | Yes | Yes | Yes |
| New Jersey | N.J. Stat Ann. §24:6I (2010) | October 1, 2010 | Yes | Yes | Yes | Yes | Yes |
| Arizona | Ariz. Rev Stat §§36-2801–2819 | November 2, 2010 | Yes | Yes | Yes | Yes | Yes |
| Delaware | Delaware Medical Marijuana Act, SB 17 (not yet codified) | May 13, 2011 | Yes | Yes | Yes | Yes | Yes |
Concurrent with the gradual increase in state MMLs since 1996, national trends indicate declines in nonmedical marijuana use among adolescents from 1996 to 2008 followed by increases from 2008 to 2010.3 Some have suggested that passage of state MMLs may be contributing to recent increases in nonmedical marijuana use among adolescents, sparking a national debate regarding the legal status of marijuana. Moreover, noting the lag between the enactment of California’s MML in 1996 and the recent increases in adolescent marijuana use beginning in 2008, there may be a delayed effect of MMLs on adolescent marijuana use.
Theoretically, MMLs might make marijuana cheaper and more easily accessible to adolescents. The laws might reduce perceptions of the harmfulness or toxicity of marijuana and might increase the social acceptability of marijuana use. On the basis of such suppositions, MMLs might be expected to increase nonmedical marijuana use among adolescents. By contrast, the laws’ function of labeling marijuana as a medication for severely ill patients could reduce the perception of marijuana as a recreational drug, thus resulting in reduced nonmedical marijuana use among adolescents. Moreover, MMLs might not increase adolescents’ ease of access to marijuana if, as a result of minimal enforcement of marijuana prohibitions, the drug is already functionally decriminalized.
Early research on the potential impact of MML passage on marijuana use did not reveal any effects.4,5 A report from the Marijuana Policy Project Foundation evaluated marijuana use via multiple state and national surveys in 12 states that had passed MMLs subsequent to 1996 and showed either no change or statistically significant decreases in marijuana use after enactment of policies.6
In a recent study, Wall et al. used data from the National Survey on Drug Use and Health to compare the state-level prevalence of adolescent marijuana use from 2002 to 2008 in states with and without MMLs.7 Rates of marijuana use were significantly higher in states that enacted MMLs both before and after the policies had been enacted. The Wall et al. results highlighted the fact that states that eventually pass MMLs may differ in fundamental ways from those that do not pass such legislation. This preexisting cultural difference, rather than a causal link between MMLs and marijuana use, could account for higher rates of marijuana use.
To test this hypothesis, Harper et al.8 conducted further analyses of the same data used by Wall et al.,7 employing a difference-in-differences study design and aggregating state marijuana use rates by age (12–17 years, 18–25 years, ≥ 26 years). Results showed no evidence of a significant increase in marijuana use immediately after the enactment of MMLs in any of the 3 age groups.
Despite being a topic of continuing policy debate, the empirical literature on MML effects remains quite limited. We used a survey data set different from that used by Wall et al. and Harper et al. and analyzed data at the individual survey respondent level rather than aggregate reported statewide prevalence rates, providing additional statistical power to detect what might be quite small but important effects of MMLs on adolescent nonmedical marijuana use.
METHODS
Seventeen states and the District of Columbia have enacted MMLs since 1996 (Table 1). To ascertain the effects of MMLs on adolescent marijuana use, we treated enactment of these laws as a series of repeated natural experiments of a single conceptually similar intervention, even though specific legal provisions vary from state to state. States that eventually enact MMLs are particularly appropriate comparison states given that previous research has shown these states are more similar to one another in rates of adolescent marijuana use and perceptions of risk, even prior to passage of MMLs, than they are to states that have taken no action on MMLs.7
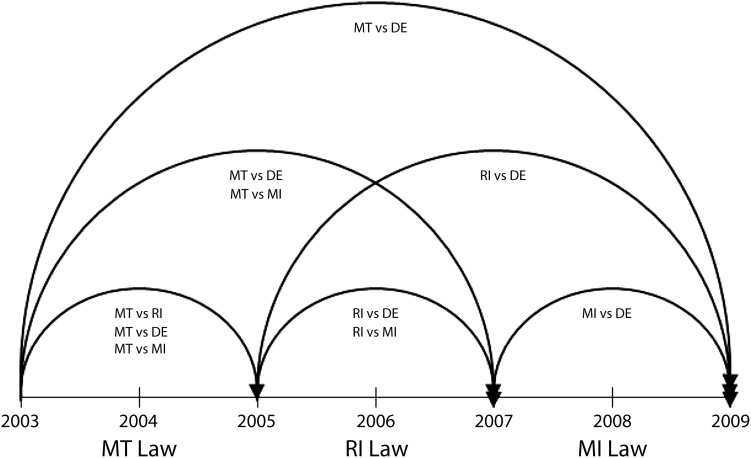
A comparison of states in Table 1 with states for which relevant Youth Risk Behavior Survey9 (YRBS) measures were available resulted in the selection of 4 focal study states: Montana, Rhode Island, Michigan, and Delaware. At different points in time, Rhode Island, Michigan, and Delaware served as untreated comparison states. The resulting “switching replications” design is illustrated in Figure 1.
FIGURE 1—
Planned comparisons for difference-in-differences analyses of states with medical marijuana laws: United States, 2003–2009.
Note. DE = Delaware; MI = Michigan; MT = Montana; RI = Rhode Island.
Data
Data were obtained from the YRBS. Data on marijuana use questions were available for both the focal states and their relevant comparison states from 2003 to 2009. Surveys were administered biennially with newly selected probability samples for each wave, providing repeated cross-sectional data.
In contrast to prior research that examined aggregate prevalence rates,7,8 we obtained individual-level YRBS data by state and year (n = 1814–4030). Analyses of individual-level observations rather than statewide rates allowed us to include individual-level covariates, increasing the study’s statistical power.
Variables
Demographic characteristics.
All adjusted analyses controlled for age, ethnicity, and gender, because marijuana use is known to vary by these demographic characteristics.10 Age was included as a continuous variable (range: 12–18 years). Ethnicity was coded as White, Black, Hispanic, or Other.
Outcome: adolescent marijuana use.
We evaluated adolescent lifetime marijuana use and past-month use via 2 questions from the YRBS.9 The distribution of responses for both of the questions was highly skewed. As a result, we dichotomized response options for both questions to reflect a yes or no response with respect to lifetime or past-month marijuana use. In a subgroup analysis limited to self-reported lifetime marijuana users, we used daily use yes–no and weekly use yes–no variables created from YRBS data on frequency of marijuana use in the past 30 days to examine frequency of marijuana use.
Predictor: medical marijuana legislation.
All of the study states had enacted an MML: Montana in 2004, Rhode Island in 2006, Michigan in 2008, and Delaware in 2011. Rhode Island, Michigan, and Delaware all served as comparison states at different points in time in a switching replications quasi-experimental design. To facilitate our difference-in-differences analyses, we created 2 MML indicator variables: an individual-level time indicator (coded 1 for participants surveyed after MML enactment and 0 for participants surveyed before enactment) and a state-level indicator variable distinguishing experimental versus comparison states (coded 1 for states that had passed MMLs and 0 for comparison states).
Analyses
We estimated regression models of the following form:
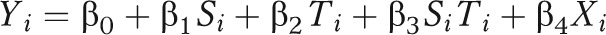 |
where Yi represents the outcome for participant i. Si is a state-level indicator (MML vs comparison) that captures state-level differences prior to MML passage. Ti, the individual-level indicator (survey completed pre-MML vs post-MML), captures the secular trend that would have occurred in the absence of MML enactment. The interaction term, SiTi, is interpreted as the difference between the MML state and the comparison state in the average change in adolescent marijuana use from the prepolicy time period to the postpolicy period. The difference-in-differences method assumes that the 2 states would have had identical trends in adolescent marijuana use if the MML had not been enacted (i.e., that the interaction term is 0). Xi represents a vector of control variables for participant i. Given the limitations of repeated cross-sectional data (i.e., unavailability of cohort data), the difference-in-differences approach is the strongest available method of identifying the causal effects of MMLs.11
We used the linear probability model for all analyses because the outcome variables were dichotomous. This model was used in lieu of a nonlinear regression model because of the difficulty in interpreting interaction terms in nonlinear difference-in-differences models; when a nonlinear model is used, the modeled interaction term loses its difference-in-differences interpretation and is no longer a reliable indicator of the magnitude or direction of the policy effect.12 To account for the complex survey design of the YRBS, we used the PROC SURVEYREG feature of SAS version 9.2 (SAS Institute, Cary, NC) to run all of our models.
Even after accounting for the nonindependence caused by the YRBS’s complex survey design, there could be a cohort effect such that Participants surveyed in the same year may respond more similarly to one another than they would to participants surveyed in other years (Figure 1). To account for this correlation, we treated survey year as an additional design stratum. A limitation of linear probability models is that they lead to heteroskedastic estimates of standard errors, potentially resulting in incorrect statistical inferences. Therefore, heteroskedastically robust jackknife standard errors were used to calculate all t statistics and P values. Another limitation of linear probability models is their potential to predict individual probabilities outside the range of 0–1. In this study, 7 of the covariate-adjusted models were found to predict values outside the 0–1 range. Our adjusted models predicting values outside the 0–1 range should not be interpreted directly, but the corresponding unadjusted models can be freely interpreted.
RESULTS
Results are reported separately for the effects of MMLs on the prevalence and frequency of adolescent marijuana use. Effects on prevalence were evaluated for the full sample, whereas effects on frequency were evaluated for a restricted sample of adolescents who reported ever having used marijuana.
Full Sample
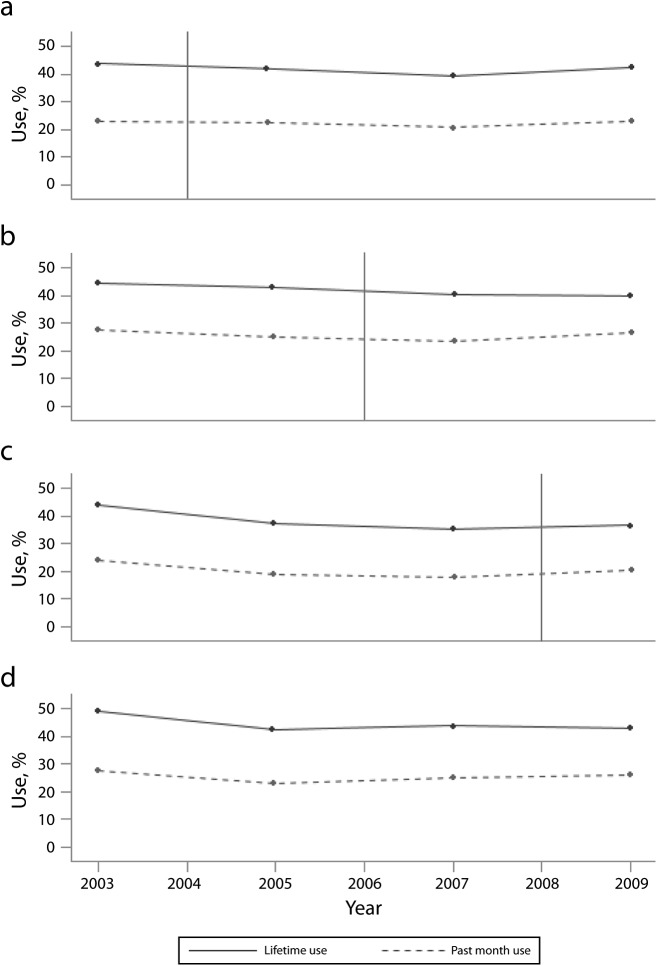
None of the models unadjusted for demographic characteristics revealed a statistically significant MML effect on the prevalence of either lifetime or 30-day marijuana use (Table 2), a result visually confirmed by the plot of marijuana use by survey year and state in Figure 2. The similarity in adolescent marijuana use trends across time and states is evident. After controlling for demographic factors, Montana showed a statistically smaller decrease than Delaware in the probability of lifetime marijuana use between 2003 and 2009 (B = 0.071, t250 = 2.21, P = .03). No other adjusted comparisons yielded a statistically significant difference (P < .05).
TABLE 2—
Results of Difference-in-Differences Models of Prevalence and Frequency of Marijuana Use: Youth Risk Behavior Survey, United States, 2003–2009
| Prevalence Data for Full Sample |
Frequency Data for Subsample |
|||||||
| Lifetime Use |
Monthly Use |
Weekly Use |
Daily Use |
|||||
| Comparison Period and Statesa | b (SE) | B (SE) | b (SE) | B (SE) | b (SE) | B (SE) | b (SE) | B (SE) |
| 2003–2005 | ||||||||
| Montana–Delaware (n = 11 623, n = 5213) | 0.044 (0.035) | 0.045 (0.029) | 0.037 (0.026) | 0.036 (0.023) | 0.031 (0.038) | 0.031 (0.037) | −0.004 (0.029) | −0.001b (0.028) |
| Montana–Michigan (n = 12 563, n = 5399) | 0.045 (0.044) | 0.038 (0.040) | 0.045 (0.030) | 0.041 (0.028) | 0.073 (0.042) | 0.069 (0.039) | 0.035 (0.036) | 0.035b (0.033) |
| Montana–Rhode Island (n = 10 034, n = 4319) | −0.007 (0.039) | −0.011b (0.033) | 0.019 (0.027) | 0.014 (0.022) | 0.033 (0.038) | 0.029 (0.037) | 0.007 (0.031) | 0.005 (0.030) |
| 2003–2007 | ||||||||
| Montana–Delaware (n = 12 486, n = 5478) | 0.001 (0.033) | 0.019 (0.028) | 0.002 (0.025) | 0.014 (0.024) | 0.022 (0.033) | 0.029 (0.032) | 0.009 (0.027) | 0.023b (0.027) |
| Montana–Michigan (n = 13 795, n = 5849) | 0.038 (0.041) | 0.032 (0.039) | 0.040 (0.030) | 0.040 (0.029) | 0.061 (0.040) | 0.065 (0.039) | 0.034 (0.035) | 0.037 (0.033) |
| 2003–2009 | ||||||||
| Montana–Delaware (n = 10 088, n = 4566) | 0.043 (0.039) | 0.071* (0.032) | 0.015 (0.029) | 0.030 (0.026) | −0.028 (0.037) | −0.023 (0.036) | −0.062* (0.029) | −0.044b (0.027) |
| 2005–2007 | ||||||||
| Rhode Island–Delaware (n = 9916, n = 4323) | −0.039 (0.033) | −0.037b (0.029) | −0.040 (0.026) | −0.038 (0.023) | −0.042 (0.040) | −0.050 (0.041) | 0.014 (0.032) | 0.018 (0.032) |
| Rhode Island–Michigan (n = 11 357, n = 4676) | −0.003 (0.040) | 0.000 (0.039) | −0.009 (0.027) | −0.006 (0.027) | −0.044 (0.043) | −0.048 (0.043) | −0.001 (0.033) | −0.001 (0.033) |
| 2005–2009 | ||||||||
| Rhode Island–Delaware (n = 10 699, n = 4323) | −0.033 (0.033) | −0.017b (0.024) | −0.017 (0.025) | −0.006 (0.020) | −0.028 (0.033) | −0.032 (0.033) | −0.031 (0.029) | −0.024 (0.028) |
| 2007–2009 | ||||||||
| Michigan–Delaware (n = 11 977, n = 5107) | 0.022 (0.032) | 0.025 (0.028) | 0.019 (0.023) | 0.023 (0.021) | 0.004 (0.034) | 0.009 (0.034) | −0.017 (0.024) | −0.011 (0.024) |
In parentheses, the first sample size listed is the full sample size, and the second one is the subsample size.
Model predicting outside the 0–1 range.
*P < .05.
FIGURE 2—
Marijuana use prevalence in (a) Montana, (b) Rhode Island, (c) Michigan, and (d) Delaware: Youth Risk Behavior Survey, 2003–2009.
Note. Vertical solid lines indicate years in which medical marijuana laws were enacted.
Thus, of the 20 models matching our 20 planned comparisons in the study design, only one yielded a statistically significant result, a finding that would be expected according to chance alone. Although some of the covariate-adjusted models indicated predicted probabilities outside the 0–1 range, results from corresponding covariate-free models produced similar results, with no significant MML effects evident. Examination of the (nonsignificant) estimates revealed no discernible pattern suggesting an effect on either self-reported lifetime marijuana use or self-reported use during the preceding 30 days.
A Restricted Sample of Marijuana Users
In the 20 comparison analyses conducted, only a single unadjusted model produced a statistically significant difference with respect to changes in frequency of marijuana use among self-reported users (Table 2). In the unadjusted model, Montana showed a statistically significant decrease in daily marijuana use between 2003 and 2009, as compared with the increase observed in Delaware over the same period (b = −0.063, t249 = −2.13, P = .03). Again, a single significant result in a set of 20 comparisons can be accounted for by chance alone.
Once more, although some of the covariate-adjusted models showed predicted probabilities outside the 0–1 range, results from corresponding covariate-free models produced similar results, with only the one significant MML effect evident. Finally, examination of the (nonsignificant) estimates revealed no discernible pattern suggesting an effect on frequency of marijuana use among self-reported users.
DISCUSSION
We found no evidence of intermediate-term effects of passage of state MMLs on the prevalence or frequency of adolescent nonmedical marijuana use in the states evaluated, with 2 minor exceptions. From 2003 through 2009, adolescent lifetime prevalence of marijuana use and frequency of daily marijuana use decreased significantly in Montana, as compared with a more modest decrease in lifetime prevalence and an increase in daily frequency observed in Delaware (Ps = .03). These 2 statistically significant findings do not appear to represent real effects. Our difference-in-differences study design involved 40 planned comparisons (before–after differences in treatment vs comparison states), and naturally 2 significant results (at the P < .05 level) of a possible 40 can be expected according to chance alone.
Moreover, the pattern is not consistent with an effect of MMLs. A significant effect was found for lifetime marijuana use but not past-month marijuana use. Self-reported lifetime use requires a much longer recall period than past-month use and is characterized by higher measurement error.13 Also, one would expect the 30-day use measure to be more sensitive than lifetime use to the effects of a change in MMLs, because most of the period covered by respondents’ lifetime reports occurred before passage of an MML.
Finally, the significant increase in daily marijuana use was observed for the comparison state of Delaware, which had not enacted an MML during the years under evaluation, whereas the frequency of daily marijuana use in Montana decreased. This is the opposite of what would be expected if MMLs had the deleterious effect of increasing the frequency of nonmedical marijuana use.
Conversely, the significant effects observed were found between the 2 states that differed the most on the timing of MML enactment, maximizing the length of the follow-up period. Hence, it is reasonable to suspect that enacting an MML may influence the prevalence and frequency of adolescent nonmedical marijuana use half a decade later, despite no evidence of more proximal effects. Resolving whether MMLs have longer-term effects on adolescent marijuana use that differ from the results observed to date will require future studies with follow-ups of longer duration.
According to a post hoc power analysis of our models focusing on the YRBS data set, an effect of MMLs on adolescent marijuana use would have to be in the range of 2.5 to 5 percentage points to be statistically detectable. As a comparison, the Monitoring the Future national survey revealed that adolescent reports of annual marijuana use increased from 21% in 2007 to 25% in 2011,3 a change that falls within the range of statistically detectable effects in our study.
Limitations
Our study is not without limitations. For example, we used self-reported data from nationally representative data sets; future research would benefit from multiple alternative sources of marijuana use (e.g., drug-related arrests and emergency room visits, parents’ reports) to provide additional perspectives on changing trends in marijuana use.14,15 Future research would also benefit from more precise data on the effects of MMLs on expected mechanisms or mediators between these laws and adolescent nonmedical use, such as marijuana markets (e.g., availability and cost of marijuana), norms and perceptions of marijuana use and its harmfulness, and frequency and intensity of marijuana use.
The details of MMLs and the implementation of specific components of these laws vary considerably from state to state, and such variations are likely to increase as additional states experiment with alternative approaches. For instance, of the states evaluated in this study, Michigan was the only one that did not set up a dispensary system. Medical marijuana dispensaries may make access to medical marijuana easier for both medical and nonmedical use.
Colorado’s MML went into effect in 2001, but restrictions on cultivation and distribution were relaxed much later, in 2009, resulting in more retail dispensaries. A recent Colorado study showed that 74% of adolescent patients in a substance abuse treatment program reported having used diverted medical marijuana.16 The situation in Colorado illustrates that MMLs are not static over time, and either more restrictive or less restrictive changes to the laws may be made subsequent to enactment.
Detailed implementation studies of processes within individual states are warranted to determine whether specific components of MMLs or alterations of MMLs within states are linked to increased diversion of marijuana to nonmedical use or changes in mental and physical health outcomes. In addition, some states already have, and others might implement, decriminalization policies, which might interact with MMLs in changing norms around and availability of marijuana. Outright legalization is also under active debate as a policy option. And some states may already have, or move toward, de facto legalization if existing prohibitions are unenforced. Lack of detailed implementation data on enforcement of various state marijuana legal provisions, marijuana markets and prices across states and over time, and actual physical accessibility of marijuana among young people is a clear limitation of our study and warrants more attention in future research.
Conclusions
Research on the effects of medical marijuana policies is in its early stages. Further studies on the influence of MMLs on marijuana use among adolescents are needed given associations between adolescent marijuana use and untoward outcomes such as unintentional injuries, emergency room visits, justice system involvement, and mental health and academic problems. Given the public health risks of widespread marijuana use, it is heartening that, in the states evaluated here, MMLs do not appear to have significantly increased the prevalence or frequency of adolescent marijuana use in the first few years after their enactment. However, the legal status of marijuana is continuing to evolve, with more lenient legislation potentially conveying considerable risks of deleterious public health outcomes. As such, the effects of marijuana policies on public health are deserving of continued close attention by public health scientists and practitioners.
Acknowledgments
This research was supported in part by the University of Florida (National Institutes of Health Clinical and Translational Science Institute award UL1 RR029890) and the Robert Wood Johnson Foundation’s Public Health Law Research Program, based at Temple University’s Beasley School of Law.
Note. This article is the sole responsibility of the authors and does not necessarily represent the views of the funders.
Human Participant Protection
This study involved secondary analyses of publicly available, deidentified data. Therefore, no institutional review board approval was needed.
References
- 1.Pacula RL, Chriqui JF, Reichmann DA, Terry-McElrath YM. State medical marijuana laws: understanding the laws and their limitations. J Public Health Policy. 2002;23(4):413–439. [PubMed] [Google Scholar]
- 2.US Department of Justice. Drug Enforcement Administration. Title 21 United States Code (USC) Controlled Substances Act. Available at: http://www.deadiversion.usdoj.gov/21cfr/21usc/index.html. Accessed February 11, 2013.
- 3.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2010. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2011. [Google Scholar]
- 4.Gorman DM, Huber JC., Jr Do medical cannabis laws encourage cannabis use? Int J Drug Policy. 2007;18(3):160–167. doi: 10.1016/j.drugpo.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Khatapoush S, Hallfors D. “Sending the wrong message”: did medical marijuana legalization in California change attitudes about and use of marijuana? J Drug Issues. 2004;34(4):751–770. [Google Scholar]
- 6.O’Keefe K, Earleywine M, Mirken B. Marijuana Use by Young People: The Impact of State Medical Marijuana Laws. Washington, DC: Marijuana Policy Project Foundation; 2008. [Google Scholar]
- 7.Wall MM, Poh E, Cerdá M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21(9):714–716. doi: 10.1016/j.annepidem.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22(3):207–212. doi: 10.1016/j.annepidem.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 9. Youth Risk Behavior Surveillance System. Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/yrbs. Accessed February 11, 2013.
- 10.Mayes LC, Suchman NE. Developmental pathways to substance abuse. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology, Volume 3: Risk, Disorder, and Adaptation. 2nd ed. Hoboken, NJ: John Wiley & Sons Inc; 2006. pp. 599–619. [Google Scholar]
- 11.Gangl M. Causal inference in sociological research. Annu Rev Sociol. 2010;36:21–47. [Google Scholar]
- 12.Athey S, Imbens GW. Identification and Inference in Nonlinear Difference-in-Differences Models. Stanford, CA: Stanford Institute for Economic Policy Research; 2002. [Google Scholar]
- 13.Bachman JG, O’Malley PM. When four months equal a year: inconsistencies in student reports of drug use. Public Opin Q. 1981;45(4):536–548. [Google Scholar]
- 14.Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol Bull. 1987;101(2):213–232. [PubMed] [Google Scholar]
- 15.Phares V, Compas BE, Howell DC. Perspectives on child behavior problems: comparisons of children’s self-reports with parent and teacher reports. Psychol Assess. 1989;1(1):68–71. [Google Scholar]
- 16.Salomonsen-Sautel S, Sakai JT, Thurstone C, Corley R, Hopfer C. Medical marijuana use among adolescents in substance abuse treatment. J Am Acad Child Adolesc Psychiatry. 2012;51(7):694–702. doi: 10.1016/j.jaac.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]