Abstract
Introduction:
National Health Information System plays an important role in ensuring timely and reliable access to Health information, which is essential for strategic and operational decisions that improve health, quality and effectiveness of health care. In other words, using the National Health information system you can improve the quality of health data, information and knowledge used to support decision making at all levels and areas of the health sector. Since full identification of the components of this system – for better planning and management influential factors of performanceseems necessary, therefore, in this study different attitudes towards components of this system are explored comparatively.
Methods:
This is a descriptive and comparative kind of study. The society includes printed and electronic documents containing components of the national health information system in three parts: input, process and output. In this context, search for information using library resources and internet search were conducted, and data analysis was expressed using comparative tables and qualitative data.
Results:
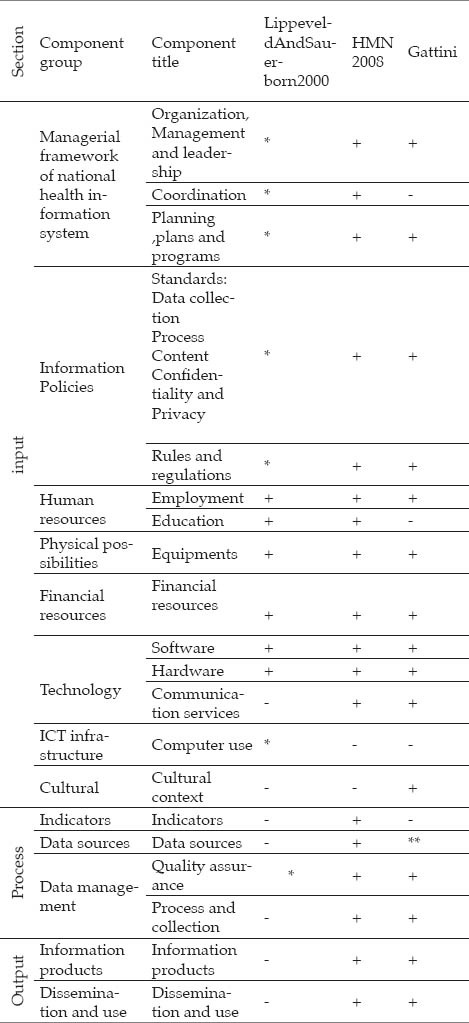
The findings showed that there are three different perspectives presenting the components of national health information system Lippeveld and Sauerborn and Bodart model in 2000, Health Metrics Network (HMN) model from World Health Organization in 2008, and Gattini’s 2009 model. All three models outlined above in the input (resources and structure) require components of management and leadership, planning and design programs, supply of staff, software and hardware facilities and equipment. Plus, in the “process” section from three models, we pointed up the actions ensuring the quality of health information system, and in output section, except for Lippeveld Model, two other models consider information products and use and distribution of information as components of the national health information system.
Conclusion:
the results showed that all the three models have had a brief discussion about the components of health information in input section. But Lippeveld model has overlooked the components of national health information in process and output sections. Therefore, it seems that the health measurement model of network has a comprehensive presentation for the components of health system in all three sections-input, process and output.
Keywords: National Health Information System, components of the National Health Information System, model
1. INTRODUCTION
Health information system, in any country, is one of the fundamental parts of health system, which provides required information for decision makers working in health sector at the national or local level, and is used to codify and oversee policies, evaluate effects of interference, and to choose priorities.
In addition, using health information system, researchers, consultants and everyone else needing health information can gain access to correct and reliable data (1). In other words, national health information infrastructures mean enhancement to the quality of data as well as health knowledge in all levels and areas of health sector (2). Establishment of those required infrastructures, as a basic part of implementing health information system throughout the country, has been suggested to be essential for developing the health care. On the other hand, health information systems perform measurements in healtheconomy territory, along with providing required information for decision makers and policymakers. Systematic monitoring over health care expenses, for example, favors the conditions to envision necessary savings without sacrificing the quality of the service (3). Therefore, we can say, promotion of heath, quality and effectiveness of health care calls for instant and complete access to all information about the patient and supporting decision making through national health information infrastructures (2). International reports and consultants’ experiences showed that, in many cases, decision makers are not using documentary-based information (4) and the scarcity of information resources and data processing is considered to be one of the basic barriers of development planning in the countries (5). One reason for inaccessibility to precise and accurate statistics and information in developing countries is the lack of coordination between users and producers of information as well as investors in health information system, which is required for gathering, analyzing and distributing information. As a consequence, decision makers are unable to understand the problems and needs, monitoring the improvements, evaluating interference effect, making documentary-based decisions about health policies, planning programs and allocating resources (6). In addition, in some countries, health information system is influenced by poor quality of management and lack of resources (7).
Also, in our country, Iran, the lack of vital information required for making decision leads to problems related to health system, and health information system is one suggested solutions- among othersto help remove concerns and challenges respective to health care providing systems, both private and public (8). In country’s amendment programs of health system, one currently existent problem was attributed to is sues concerning health information system. The lack of national health accounts, utilizing the resources, seasonal illness and death in the country, insurance coverage, information showing the amount of money that the patients need to pay and how it should be paid, as well as information about private sector, are stumbling blocks to implementing health information system in Iran. In order to remove the above problems, in the Fourth Development Plan, the Health Information System is considered (9, 10). By the same token, the Parliament Health Commission- in order to regard justice in health proiding system, provide effective and efficient health care and reform health system structure- announced that one of its important goals would be to revolutionize the health information system (11).
Implementing health information system and establishing required infrastructure, in every country, calls for well-studied, precise planning, along with managing the human resources, logistics, software, hardware and finances (12). With considering the necessity a national health information system in the country, this study was aimed to compare proposed models in order to help create a system or, in another words, a national health information system. To avoid costly errors and rework in creating and running the national health information system, necessarily we have to take advantage of other countries’ experiences, when planning.
2. REVIEW METHODS
This research is a comparative and descriptive type of study. The society of research consisted of printed and electronic documents containing components of the national health information system in three categories: Input, process and Output. Inputs refers to all kinds of resources including human, finances, cultural bedrock, technology and communication and information technology, information policies, management framework of health information system, as well as physical facilities. Process includes indexes and information resources and data management, such as data gathering, coding, data flow, communication, calculation and quality assurance measures. Output includes produced information and using and spreading the information. To do so, we used library resources and internet browsing to look for information. Data was analyzed using comparative tables and descriptive data.
3. RESULTS
According to the findings, there are three models proposed for national health information system. The first model, developed by Lippeveld, Sauerborn and Bodart in 2000, defines national health information system as a set of organized components and measures aimed to produce information, which will make managerial decision making improve, in all levels of health care. This model, recognizes the “national health information systems, as an organized set of connected components which are divided into two groups: Information process and Health information system management and Health information system management resources into the information process cycle, which includes stages such as gathering, transferring, processing, analyzing and using of information.
In this model, the managerial structure of health information system is divided into two components resources and organizational rules - as bellow (Figure 1)
Figure 1.
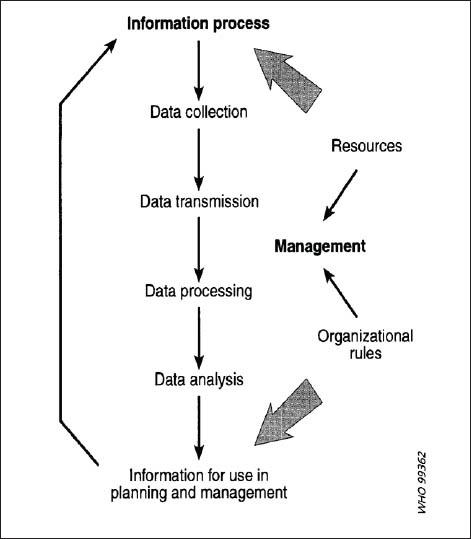
Managerial structure of NHIS
Resources
Employees
Employee training
Logistics of health information system and facility distribution
Software and hardware
Finances
B- Organizational rules
Health information system management
Data gathering standards
Rules for data and reports transferring and processing
Confidentiality and privacy
The amount of use of computers
Supply and distribution of resources and equipment
Quality assurance measures of health information system
Role of private sector and how to interact with them (13).
Health Metrics Network (HMN) model, developed by world Health Organization in 2008, recognizes the national health system as a composite of different interacting components, which help produce better information and improve the decision making process. In this model, “health information system” includes six different parts, which constitute three overall divisions- input, process and output- as described below:
Inputs:
-
1)
Health information system resources
- Coordination and leading
- Health information system’s information policies
- Human resources and finances
- Health information system infrastructures
Process:
-
2)
Indexes
- Heaith informat ion territories
- Defining the principal indexes
-
3)
Information resources (Health information system renources)
- Institute-based date
- Population-based data
-
4)
Data management Data management
- Ensuring quality of the data
- Gathering and data processing
Output:
-
5)
Information products (changing data into information)
-
6)
Use and publication (use of information in decision making)
In this model, however, information resources were defined as a component of the “process” part, and all kinds of data resources related to health were divided into two groups- Institution-based and population-based- as below:
A- Institution-based data
Personal documents such as patients’ medical case and records
Documents indicating provided services
Documents related to resources population-based data
Censuses
Registry of vital events
Investigations in populations
Here are data resources for national health information system model quoted from WHO “health metrics network”(14). (Figure 2).
Figure 2.
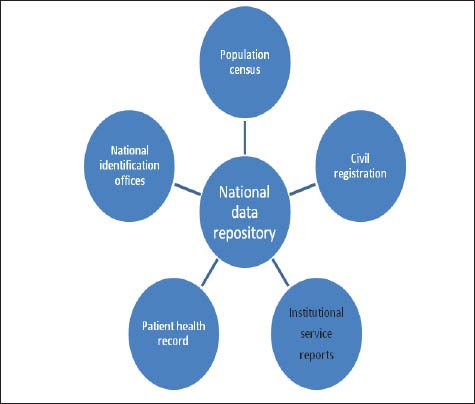
“Health Metrics Network” quoted by WHO
The last model of national health information system was presented by Gattini in 2009. Gattini defines the national health information system as “an integrated and organized network of resources and processes at the national level which contribute to a nationwide creation and communication of health related information, consist of certain information systems maintained by variety of programs in offices and institutes and interact with each other across the country.”
Coordination, in this network, is done by a “National health authority” and its main goal is to backup evidence-based decisions in health section. Its final goal, however, is to maintain and improve health in the society. In this model, the structure and process of health information system from a systematic perspective spective are described as Figure 3.
Figure 3.
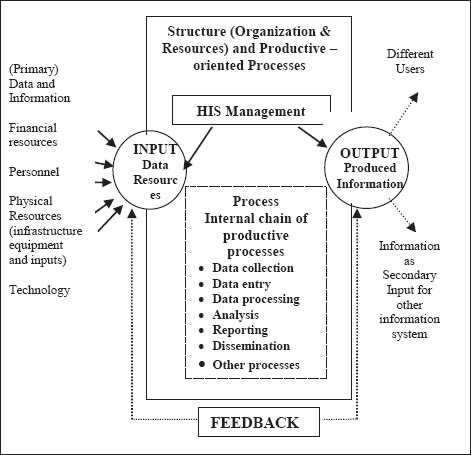
Perspective of structure and process of NHIS
In Gattini’s model, in addition to finances, employees, physical resources, technology and data and information are also considered as Input of national health information system. Plus, this model divides the components of national health information system into two parts- structure and performance- as below (Table 1):
Table 1.
Comparative review of components of National health Information System. *Organization rules part. **Inputs section
Structure:
-
1)
Institutional component:
- Managerial framework of national health information system
- Policies, plans, legislated regulations and management
- Organizing and management
- Establishing a cultural bedrock for using information in decision making
- Finances, human and physical resources
-
2)
Technological component:
- Equipment (hardware)
- Software
- Communication structure and related services
Performance:
-
3)
Functional components:
- Data and information production (gathering, processing, analyzing and reporting)
- Publishing and exchanging data and information
- Information management and information system (15)
4. DISCUSSION
Management framework of health information system is one of the national health information system inputs that all of the models have expressed it. In many studies, Information systems success is related to how well the IS interface with the organizational and users environments (16). Findings of a study about evaluation frameworks for health information systems shows that having the right user attitude and skills base together with good leadership, IT friendly environment and good communication can have positive influence on the system adoption (17).
The Lippeveld and Sauerborn and also HMN model coordination marked as a part of management framework of national health information system. Experience of the Papua New Guinea has showed that central coordination of systems design is essential to make sure that information systems are aligned with government priorities and can deliver the information required by managers (18). Analyzing the problem of unsustainable health information system in less-developed economics like Mozambique identified that the development of the different subsystems by different foreign experts within different departments of MoH in Mozambique was a result of a lack of coordination leading to fragmentation (19). Number of publications also identified the current structure of health care organizational systems as a barrier for health information technology adoption (20).
Standards are the backbone of technological progress. They enable parts to fit together, assure consistency over time, and facilitate communication. Standards are “pre-requisites to the joining of information from many separate computer sources to produce a whole that is greater than the sum of its parts. They are means by which we are able to combine data from different sources and there- by generate value from raw data through analysis (10). The main purpose of the national health information system is to develop nationwide framework (database) that facilitates the exchange of diffuse health information, currently available only in local databases and information systems that often are not able to communicate with each other (21). Lippeveld and Sauerborn refer to standards of data collection, process and transfer of data, confidentiality and privacy as inputs of health information system, while in model of health metrics and Gattini model, this information policy are given under Content standards. More over each of three mentioned models accept the necessity of rules and regulations for health information system. Health care messaging standards should be used for data interchange. Common vocabulary standard and required data elements for public health surveillance databases are required to enable effective sharing of data. Without a common vocabulary, data from local systems cannot be analyzed to detect emerging health threats. Government coordination and support for consensus standardization and low-cost distribution of common vocabularies for health event detection, prevention, and intervention are a fundamental aspect of a national health information infrastructure (22).
One of important inputs of health information system is human resources which include the employment and staff education. All of mentioned three models look considerably to staff training, but Gattini model ignores this element. The training and competences of healthcare professionals as the end- users operating a specific application are key factors in health information technology adoption (20). Human resource is one of the important barriers for implementation of the health information system. The great resistance of physicians and other healthcare professionals to accept and use health information systems and electronic medical records is probably one of the major barriers that delayed the adoption and successful implementation of such systems. The analysis of the human barriers could reveal a lot of factors related directly to the beliefs, attitudes and behaviors of healthcare professionals such as the ability to learn over time, computer knowledge and typing proficiency, understanding and believing in HIS and EMR systems, motivation and personal initiative to explore and use the systems and user-developed strategies and workarounds to solve minor difficulties (23). The researcher suggests that teaching and training should be developed and implemented as a course or a subject of the formal undergraduate as well as post graduate medical education programs (17). All of three models explain the physical possibility and equipments of health information systems. Lippeveld and Sauerborn refer to amount of using computers, but two other models don’t refer to this element. Gattini pays attention to forming of cultural context in decision making, but two other models ignore the cultural aspects.
The process of a national health information system includes indicators, data sources and data managements. The indicators are only given at health metrics model. Data sources at Gattini and Lippeveld and Sauerborn models are at the inputs part, and health metrics model pays attention to it at process section.
Quality assurance in the Lippeveld and Sauerborn model is given in the organizational rules but in the other models this element is mentioned in the process section. Out put of an health information system includes information products, dissemination and use. This elements are given in the health metrics and Gattini models, but Lippeveld and Sauerborn model ignores it. Yusof’s study identified that use of result information is one of the measurement indicators of an information system (17).
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Csiki IE. Bucharest: The institute of public health; 2003. Description of the national Health information system in Romania. [Google Scholar]
- 2.Yasnoff W, Humphreys MJ, Overhage M. A consensus action agenda for achieving the national health information infrastructure Journal of American Medicatical information association. 2004;11:332–338. doi: 10.1197/jamia.M1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Varga S, Stevanovic R, Mauher M. Founding and development of the Croatian health information system. Acta Med Croatica. 2005;59(3):191–999. [PubMed] [Google Scholar]
- 4.Addor V, Dumitrescu A. Increasing the use of health data and information by decision-makers in Europe: the role of national health information system. European Journal of public health. 2004;14(4) [Google Scholar]
- 5.Avgerou C. Information systems for development planning. International journal of information management. 2013;13(4):260–273. [Google Scholar]
- 6.WHO publication; 2006. WHO Health Metrics Network. [Google Scholar]
- 7.Chaulagai CN, Moyo CM, Koot J. Health Policy journal. Oxford Univ Press; 2005. Design and implementation of a health management information system in Malawi. [DOI] [PubMed] [Google Scholar]
- 8.Jamshidi A. Health reforms in Iran”[Persian] available at: http://www.atgci.org/hmdc/healthsystem reform.ppt .
- 9.Mc Connel H. International efforts in implementing national healyh information infrastructure and electronic health records. World hospital health services. 40(1):39–40. [PubMed] [Google Scholar]
- 10.De Detmar Building the national health information infrastructure for personal health, health care services, public health, and research. BMC Medical Informatics and Decision Making. 2003;3(1) doi: 10.1186/1472-6947-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tehran: The fourth national development plan of Islamic Republic of Iran, Information Technology part; 2005. Persian. [Google Scholar]
- 12.Ministry of Health and Medical education, “Strategic plan of TAKFAB in the fourth economic, social and economic plan of Iran” Tehran. 2004 [Google Scholar]
- 13.Lippeveldn T, Sauerborn R, Bodart C. WHO publication; 2000. Design and implementation of health information systems. [Google Scholar]
- 14.second edition. Geneva: WHO publication; 2008. Health Metrics Network. Framework and standards for country health information system. [Google Scholar]
- 15.Gattinin CH. Brazil: Technical Series on Information for Decision- Making; 2009. Improving the Structure and Performance of National Health Information Systems, Operational Approach and Strategic Recommendations. [Google Scholar]
- 16.Brender J, Ammenwerth E, Nykanen P, Talmon J. Factors influencing success and failure of health information system. Methods of information in medicine. 2006;75(1):125–136. [PubMed] [Google Scholar]
- 17.Yusuf MM, Kuljis J, Papazafeiropoulou A, Stergioulas LK. An evaluation framework for health information systems: human, organization and technology - fit factors (HOT-fit) Int J Med. Inform. 2008;77(6):386–398. doi: 10.1016/j.ijmedinf.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 18.Cibulskis RE, Hiawalyer G. Development of a National Health Information System in Papua New Guinea. Available from: http://www.hsph.harvard.edu .
- 19.Kimaro H, Nhampossa J. Analyzing the Problem of Unsustainable Health Information Systems in Less-Developed Economies: Case Studies From Tanzania and Mozambique. Information Technology for Development journal. 2005;11:273–298. [Google Scholar]
- 20.Lluch M. Healthcare professionals’ organisational barriers to health information technologies - A literature review. Int J Med. Inform. 2011;80:849–862. doi: 10.1016/j.ijmedinf.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Aaviksoo A. National Health Information System. Health Policy Monitor, October. 2005. Available at: http://www.hpm.org/survey/ee/a6/3 .
- 22.Tang PC. AMIA Advocates National Health Information System in Fight against National Health Threats. J Am Med Inform Assoc. 2002;l9:123–124. doi: 10.1197/jamia.M1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khalifa M. Vol. 21. The 3rd International Conference on Current and Future Trends of Information and Communication Technologies in Healthcare (ICTH). Proceedings Computer Science; 2013. Barriers to Health Information Systems and Electronic Medical Records Implementation: A Field Study of Saudi Arabian Hospitals; pp. 335–342. [Google Scholar]


