Abstract
Background
Anemia is associated with decreased functional capacity, reduced quality of life, and worsened outcomes among patients with heart failure (HF) due to reduced left ventricular ejection fraction (HFREF). We sought to evaluate the independent effect of anemia on clinical outcomes among those with HFREF.
Hypothesis
Anemia is associated with cardiovascular events in patients with heart failure.
Methods
The HF‐ACTION trial was a prospective, randomized trial of exercise therapy vs usual care in 2331 patients with HFREF. Patients with New York Heart Association class II to IV HF and left ventricular ejection fractions of ≤35% were recruited. Hemoglobin (Hb) was measured up to 1 year prior to entry and was stratified by quintile. Anemia was defined as baseline Hb <13 g/dL and <12 g/dL in men and women, respectively. Hemoglobin was assessed in 2 models: a global prediction model that had been previously developed, and a modified model including variables associated with anemia and the studied outcomes.
Results
Hemoglobin was available at baseline in 1763 subjects (76% of total study population); their median age was 59.0 years, 73% were male, and 62% were Caucasian. The prevalence of anemia was 515/1763 (29%). Older age, female sex, African American race, diabetes, hypertension, and lower estimated glomerular filtration rates were all more frequent in lower Hb quintiles. Over a median follow‐up of 30 months, the primary outcome of all‐cause mortality or all‐cause hospitalization occurred in 78% of those with anemia and 64% in those without (P < 0.001). The secondary outcomes of all‐cause mortality alone,cardiovascular (CV) mortality or CV hospitalization, and CV mortality or HF hospitalization occurred in 23% vs 15%, 67% vs 54%, and 44 vs 29%, respectively (P < 0.001). Heart failure hospitalizations occurred in 36% vs 22%, and urgent outpatient visits for HF exacerbations occurred in 67% and 55%, respectively (P < 0.001). For the global model, there was an association observed for anemia and all‐cause mortality or hospitalization (adjusted hazard ratio [HR]: 1.15, 95% confidence interval [CI]: 1.01‐1.32, P = 0.04), but other outcomes were not significant at P < 0.05. In the modified model, the adjusted HR for anemia and the primary outcome of all‐cause mortality or all‐cause hospitalization was 1.25 (95% CI: 1.10‐1.42, P < 0.001). There were independent associations between anemia and all‐cause death (HR: 1.11, 95% CI: 0.87‐1.42, P = 0.38), CV death or CV hospitalization (HR: 1.16, 95% CI: 1.01‐1.33, P = 0.035), and CV death and HF hospitalization (HR: 1.27, 95% CI: 1.06‐1.51, P = 0.008).
Conclusions
Anemia modestly is associated with increased rates of death, hospitalization, and HF exacerbation in patients with chronic HFREF. After adjusting for other important covariates, anemia is independently associated with an excess hazard for all‐cause mortality and all‐cause hospitalization. Anemia is also associated with combinations of CV death and CV/HF hospitalizations as composite endpoints.
Introduction
Both heart failure (HF) and chronic kidney disease (CKD) are increasing in prevalence as the population ages, and both conditions have been associated with anemia of chronic disease.1, 2 Common risk factors for both CKD and HF include obesity, metabolic syndrome, diabetes mellitus (DM), and hypertension, some of which are commonly linked with the development of anemia.3, 4, 5, 6 Previous HF studies have consistently reported an association between reduced estimated glomerular filtration rates (eGFR), anemia, elevated levels of B‐type natriuretic peptide, and increased HF mortality.7, 8, 9 Anemia, even in the absence of renal disease, has also been associated with adverse clinical outcomes; however, the impact of HF, anemia, and CKD, alone or in combination, on mortality, adverse events, and hospitalization rates, remains of clinical interest.10 It is not certain whether the adverse effect of anemia on clinical outcomes is independent of its impact on other comorbid conditions. Of note, anemia in HF may be dynamic; when hemoglobin (Hb) rises, there have been favorable changes in left ventricular (LV) mass and improved symptoms.11 We sought to evaluate the impact of baseline anemia on the composite outcome of all‐cause death and all‐cause hospitalization and various cardiovascular (CV) and HF outcomes among patients with chronic systolic HF participating in the Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training (HF‐ACTION) trial.
Methods
Setting
Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training (HF‐ACTION) was a prospective, randomized trial of aerobic exercise training in patients who were medically stable, with New York Heart Association (NYHA) classes II to IV HF and measured left ventricular ejection fraction (LVEF) ≤35%. Recruitment criteria and methods for HF‐ACTION have been reported elsewhere.12, 13 Major exclusion criteria were comorbidities that may have precluded moderate‐ to vigorous‐intensity exercise (eg, peritoneal or hemodialysis) and major CV events within the last 6 months. The trial was designed to evaluate the composite primary endpoint of all‐cause mortality and all‐cause hospitalization over a median follow‐up of 30 months in patients who were optimally medically managed and underwent medically supervised and home‐based exercise training as compared with controls who received usual care.13 Primary and secondary endpoints were adjudicated by a clinical endpoints committee. Once a subject incurred 1 hospitalization for HF, subsequent hospitalizations were not reviewed by the endpoints committee and were classified according to the indication by the principal investigator.
Study Sample
A total of 2331 subjects were recruited from April 2003 through February 2007 at 82 sites within the United States, Canada, and France; however, the study sample was reduced because 568 subjects had no measured Hb recorded at baseline. The remaining 1763 subjects (76% of the total trial population) served as the study sample, providing complete data for analysis.
Laboratory Measures and Calculation of Glomerular Filtration Rate
Hemoglobin and serum creatinine (SCr) were obtained from the reported values from the study sites recorded within 1 year prior to trial enrollment and performed by the local laboratory at each center. Detailed methods for local measurement of Hb and SCr were not available. Anemia was defined as a baseline Hb <13 g/dL in men and <12 g/dL in women (World Health Organization definition).14 Estimated glomerular filtration rates (mL/min/1.73 m2) were calculated using the 4‐variable Levey Modification of Diet in Renal Disease formula (186.3 × [SCr − 1.154] × [age − 0.203]); calculated values were multiplied by 0.742 for women and by 1.21 for African Americans.15
Statistical Analysis
Statistical analyses were performed by the data coordinating center (Duke Clinical Research Institute, Durham, NC) using SAS software version 9.2 (SAS Institute Inc., Cary, NC). Baseline characteristics were reported as medians with 25th and 75th percentiles, or counts and proportions, as appropriate. The primary composite endpoint was all‐cause mortality or hospitalization. Prespecified secondary endpoints were all‐cause mortality, CV mortality or CV hospitalization, and CV mortality or HF hospitalization. Cumulative event rates were calculated using the Kaplan‐Meier method. Time zero for censoring was the time of randomization. Relative risks were expressed as hazard ratios (HR) with 95% confidence intervals (CI) and were calculated using the Cox proportional hazards model. Two modeling approaches were taken. Model 1 was created a priori to predict each of the 4 main clinical endpoints using the entire 2331 subjects recruited into HF‐ACTION with the goal of creating an adjustment model. For this method, included variables were identified via a bootstrapped backward selection algorithm of a Cox proportional hazards model with the C‐index used to choose the best model for each outcome (see Supporting Information, Appendix, in the online version of this article). This approach evaluated 61 candidate variables (including Hb) and was done independent and before the current analysis. This analysis did not identify Hb as a strong predictor of outcomes. After reviewing Model 1 results and the included covariates, it was decided to create a model (Model 2) that focused on evaluating specifically whether anemia was a predictor of outcomes and included only the 1763 subjects with actual, nonimputed Hb values. Model 2 used variables found to be differentially associated with Hb (Table 1) and known to be clinical confounders for HF, including age, African American vs other race, female sex, DM, ischemic etiology of HF, LVEF, and eGFR. Other variables in the HF‐ACTION database excluded from Model 2 were those believed to result from anemia or related to other included variables (exercise‐performance variables, quality of life, and symptom scores), variables known to be confounded by indication (eg, β‐blocker and diuretic dosage, use of nitrates), biologic representations of the same construct (eg, SCr and blood urea nitrogen, where renal‐filtration function is represented by eGFR), and those with no biologic plausibility (randomization allocation, site of randomization). The univariate relationship of the continuous variables in this set (age, LVEF, eGFR) with each outcome was checked for linearity of the log HR, and piecewise linear splines were used as transformations when appropriate in Model 2. A 2‐tailed P value <0.05 was considered statistically significant.
Table 1.
Baseline Characteristics by Quintile of Hb
| Total, n = 1763 | Q1 of Hb, n = 373 | Q2 of Hb, n = 355 | Q3 of Hb, n = 339 | Q4 of Hb, n = 357 | Q5 of Hb, n = 339 | |
|---|---|---|---|---|---|---|
| Hb, g/dL, median (Q1, Q3) | 13.5 (12.3, 14.6) | 11.4 (10.7, 11.8) | 12.7 (12.4, 12.9) | 13.5 (13.4, 13.7) | 14.4 (14.2, 14.6) | 15.6 (15.2, 16.1) |
| Age, y, median (Q1, Q3) | 59 (51, 68) | 60 (52, 70) | 61 (54, 70) | 60 (51, 69) | 58 (50, 66) | 57 (60, 65) |
| Sex, F, n (%) | 480 (27) | 160 (43) | 132 (37) | 95 (28) | 69 (19) | 24 (7) |
| Race, n (%) | ||||||
| Black or African American | 571 (33) | 175 (48) | 138 (39) | 98 (30) | 89 (25) | 71 (21) |
| White | 1069 (62) | 178 (48) | 195 (55) | 213 (65) | 249 (71) | 234 (71) |
| Other | 93 (5) | 15 (4) | 21 (6) | 18 (5) | 13 (4) | 26 (8) |
| Hypertension, n (%) | 1068 (61) | 257 (69) | 206 (58) | 196 (58) | 201 (56) | 208 (62) |
| DM, n (%) | 569 (32) | 148 (40) | 121 (34) | 108 (32) | 102 (29) | 90 (27) |
| COPD, n (%) | 198 (11) | 37 (10) | 43 (12) | 39 (12) | 43 (12) | 36 (11) |
| Prior MI, n (%) | 746 (42) | 159 (43) | 158 (45) | 132 (39) | 156 (44) | 141 (42) |
| PVD, n (%) | 132 (7.5) | 32 (8.6) | 27 (7.6) | 28 (8.3) | 24 (6.7) | 21 (6.2) |
| Prior CABG, n (%) | 458 (26) | 110 (29) | 104 (29) | 78 (23) | 85 (24) | 81 (24) |
| BMI, kg/m2, median (Q1, Q3) | 30 (26, 35) | 29 (25, 35) | 30 (26, 35) | 29 (25, 34) | 30 (26, 35) | 30 (27, 36) |
| Resting HR, bpm, median (Q1, Q3) | 70 (63, 77) | 70 (64, 78) | 69 (61, 76) | 70 (63, 76) | 70 (62, 76) | 71 (64, 78) |
| Systolic BP, mm Hg, median (Q1, Q3) | 110 (100, 126) | 110 (100, 128) | 110 (100, 124) | 110 (100, 126) | 110 (100, 124) | 112 (104, 124) |
| Diastolic BP, mm Hg, median (Q1, Q3) | 70 (60, 78) | 68 (60, 76) | 70 (60, 78) | 70 (60, 80) | 70 (60, 78) | 71 (64, 80) |
| NYHA class, n (%) | ||||||
| II | 1119 (63) | 196 (53) | 225 (63) | 223 (66) | 243 (68) | 232 (68) |
| III/IV | 644 (37) | 177 (47) | 130 (37) | 116 (34) | 114 (32) | 107 (32) |
| Angina class, n (%) | ||||||
| No angina | 1455 (83) | 308 (83) | 287 (81) | 279 (82) | 297 (83) | 284 (84) |
| I | 166 (9) | 29 (8) | 38 (11) | 36 (11) | 30 (8) | 33 (10) |
| II–IV | 140 (8) | 35 (9) | 29 (8) | 24 (7) | 30 (8) | 22 (6) |
| HF etiology, ischemic, n (%) | 923 (52) | 206 (55) | 207 (58) | 168 (50) | 177 (50) | 165 (49) |
| LVEF, %, median (Q1, Q3) | 25 (20, 30) | 25 (20, 30) | 25 (20, 30) | 24 (20, 30) | 24 (20, 30) | 24 (21, 30) |
| ACEI and/or ARB, n (%) | 1665 (94) | 349 (94) | 336 (95) | 317 (94) | 336 (94) | 327 (96) |
| β‐Blocker, n (%) | 1666 (94) | 348 (93) | 337 (95) | 326 (96) | 332 (93) | 323 (95) |
| Loop diuretic, n (%) | 1396 (79) | 333 (89) | 274 (77) | 266 (78) | 275 (77) | 248 (73) |
| Nitrate, n (%) | 446 (25) | 113 (30) | 81 (23) | 86 (25) | 89 (25) | 77 (23) |
| CCB, n (%) | 123 (7) | 32 (9) | 27 (8) | 22 (6) | 19 (5) | 23 (7) |
| Spironolactone/eplerenone, n (%) | 798 (45) | 172 (46) | 146 (41) | 155 (46) | 166 (46) | 159 (47) |
| Digoxin, n (%) | 798 (45) | 166 (44) | 159 (45) | 153 (45) | 177 (50) | 143 (42) |
| SCr, mg/dL, median (Q1, Q3) | 1.2 (1.0, 1.5) | 1.3 (1.0, 1.7) | 1.2 (0.9, 1.5) | 1.2 (1.0, 1.5) | 1.2 (1.0, 1.4) | 1.2 (1.0, 1.4) |
| eGFR, median (Q1, Q3) | 67 (51, 81) | 59 (44, 76) | 67 (50, 82) | 66 (53, 80) | 68 (55, 82) | 71 (56, 83) |
| BUN, median (Q1, Q3) | 20 (15, 28) | 23 (16, 35) | 20 (15, 29) | 20 (16, 27) | 20 (15, 25) | 20 (15, 26) |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; BMI, body mass index; BP, blood pressure; BUN, blood urea nitrogen; CABG, coronary artery bypass graft surgery; CCB, calcium channel blocker; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; F, female; Hb, hemoglobin; HF, heart failure; HR, heart rate; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NA, not available; NYHA, New York Heart Association; PVD, peripheral vascular disease; Q, quintile; SCr, serum creatinine.
Quintiles of Hb are defined as follows: Q1, ≤12.1 g/dL; Q2, 12.1 < Hb ≤13.1 g/dL; Q3, 13.1 < Hb ≤13.9 g/dL; Q4, 13.9 < Hb ≤14.9 g/dL; Q5, >14.9 g/dL.
Figure 1.
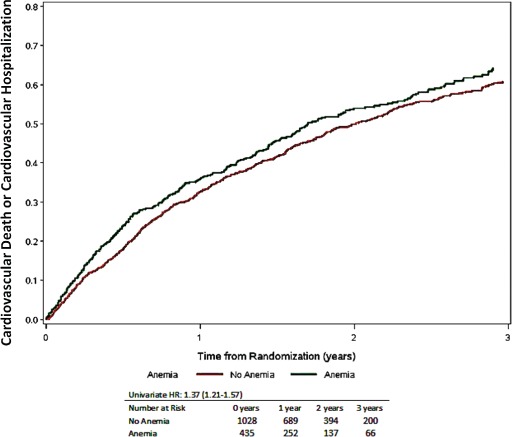
Time to CV mortality or CV hospitalization, stratified by the presence or absence of anemia. Numbers at risk include only those with nonmissing covariates (total is <1763). Abbreviations: CV, cardiovascular; HR, hazard ratio.
Results
Baseline Characteristics
Selected demographics for the study sample (n = 1763) were as follows: median age 59 years (range, 19–90 years), 73% male, 62% Caucasian, 33% African American, and 5% other races (Table 1). The overall prevalence of anemia was 30.1% and 26.9% in men and women, respectively. The median Hb was 15.6 g/dL for quintile (Q) 5 compared with 11.4 g/dL for Q1. At baseline, we found that in patients with HFREF, reduced Hb was more frequent among the expected conditions, including older age, female sex, African Americans, DM, hypertension, and mildly reduced renal‐filtration function. In the lowest quintile of Hb, the median eGFR was 59 mL/kg/1.73 m2, with an interquartile range of 44–76 mL/kg/1.73 m2. Thus, nearly all subjects were above critical levels of renal dysfunction. The most striking contrast was a prevalence of DM corresponding to 40% in Hb Q1 compared with 27% in Hb Q5.
Adverse Events
The median follow‐up times for those with and without anemia were 30 and 31 months, respectively (P = 0.594). Table 2 displays selected adverse events reported by site investigators over the course of the trial according to the presence of anemia. These adverse events were not adjudicated by the endpoints committee nor adjusted for confounding variables. With the exception of transient ischemic attack, adverse events were more frequent for those with anemia. The fraction of subjects with ≥1 selected adverse CV event was 49% and 37% for those with and without anemia, respectively.
Table 2.
Selected Adverse Outcomes According to Presence or Absence of Anemia
| All | Anemia | No Anemia | |
|---|---|---|---|
| N | 1763 | 515 | 1248 |
| Follow‐up, mo, median (25th and 75th percentiles) | 30 (19, 42) | 30 (18, 43) | 31 (20, 42) |
| Prespecified adverse CV events, n (%) | |||
| Worsening HF | 518 (29) | 200 (39) | 318 (25) |
| UA | 138 (7.8) | 51 (9.9) | 87 (7.0) |
| Serious arrhythmia | 261 (15) | 82 (16) | 179 (14) |
| Stroke | 52 (2.9) | 22 (4.3) | 30 (2.4) |
| TIA | 30 (1.7) | 7 (1.4) | 23 (1.8) |
| Any of the above events | 711 (40) | 253 (49) | 458 (37) |
Abbreviations: CV, cardiovascular; HF, heart failure; TIA, transient ischemic attack; UA, unstable angina.
Prespecified Primary and Secondary Outcomes in the Trial
Kaplan‐Meier curves demonstrating the time to first event are shown in Figure 2 for all‐cause mortality or all‐cause hospitalization as a composite. Kaplan‐Meier curves for the prespecified primary and secondary endpoints are shown in Figures 3 through 4. Individual trial outcomes and unadjusted/adjusted HRs for subjects with and without anemia are shown in Table 3. Over the median follow‐up of 30 months, all‐cause mortality or all‐cause hospitalization occurred in 78% vs 64%, and all‐cause mortality alone occurred in 23% vs 15% among patients with and without anemia, respectively (P < 0.001 for both). Cardiovascular mortality or CV hospitalization and CV mortality or HF hospitalization occurred in 67% vs 54%, and 44% vs 29%, respectively (P < 0.001) in those with and without anemia. Heart failure hospitalizations occurred in 36% vs 22%, and urgent outpatient visits for HF exacerbations in 67% vs 55%, in the anemia vs no‐anemia groups, respectively (P < 0.001 for both). The results from univariate and multivariate adjustment Models 1 and 2 are shown in Table 3. For Model 1, the adjusted HR for anemia and the primary outcome of all cause mortality or all‐cause hospitalization was 1.15 (95% CI: 1.01‐1.32, P = 0.042). The adjusted HRs for anemia and the prespecified secondary outcomes were 0.99 (95% CI: 0.77–1.27, P = 0.919) for all‐cause death, 1.22 (95% CI: 0.97–1.30, P = 0.120) for CV death or CV hospitalization, and 1.20 (95% CI: 0.99–1.44, P = 0.060) for CV death and HF hospitalization. For the modified model designed to evaluate anemia as a predictor of outcomes, the adjusted HR for anemia and the primary outcome of all‐cause mortality or all‐cause hospitalization was 1.25 (95% CI: 1.10–1.42, P < 0.001). The adjusted HRs for anemia and the prespecified secondary outcomes were 1.11 (95% CI: 0.87–1.42, P = 0.385) for all‐cause death, 1.16 (95% CI: 1.01–1.33, P = 0.035) for CV death or CV hospitalization, and 1.27 (95% CI: 1.06–1.51, P = 0.008) for CV death and HF hospitalization. All of these analyses demonstrated attenuation of the measure of association with adjustment, and this attenuation was greater for the global model (Model 1) than when adjusting for specific confounders of the anemia and outcomes association using Model 2 (ie, age, African American vs other race, female sex, DM, ischemic etiology of HF, LVEF, and eGFR).
Figure 2.
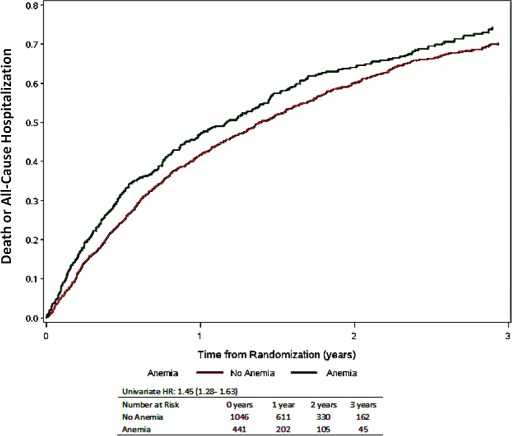
Time to all‐cause mortality or all‐cause hospitalization stratified by the presence or absence of anemia. Numbers at risk include only those with nonmissing covariates (total is <1763).
Figure 3.
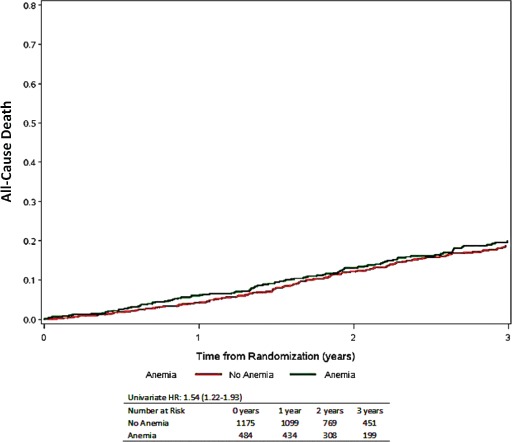
Time to all‐cause mortality stratified by the presence or absence of anemia. Numbers at risk include only those with nonmissing covariates (total is <1763). Abbreviations: AC, all‐cause; HR, hazard ratio.
Figure 4.
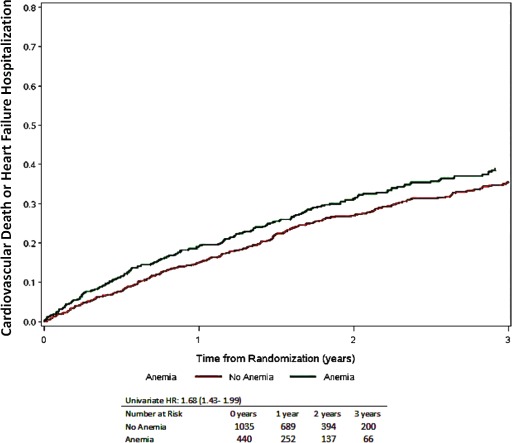
Time to CV mortality or HF hospitalization, stratified by the presence or absence of anemia. Numbers at risk include only those with nonmissing covariates (total is <1763). Abbreviations: CV, cardiovascular; HF, heart failure; HR, hazard ratio.
Table 3.
Trial Outcomes According to the Presence or Absence of Anemia
| All | Anemia | No Anemia | Univariate (Unadjusted) | Model 1 Adjusted | Model 2 Adjusted | ||||
|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | HR (95% CI) | P Value | ||||
| N | 1763 | 515 | 1248 | ||||||
| Follow‐up, mo, median (IQR) | 30 (19–42) | 30 (18–43) | 31 (20–42) | 0.594 | |||||
| Trial outcomes | |||||||||
| All‐cause mortality or all‐cause hospitalization | 1203 (68) | 401 (78) | 802 (64) | 1.45 (1.28–1.63) | <0.001 | 1.15 (1.01–1.32) | 0.042 | 1.25 (1.10–1.42) | <0.001 |
| All‐cause mortality | 308 (17) | 118 (23) | 190 (15) | 1.54 (1.22–1.93) | <0.001 | 0.99 (0.77–1.27) | 0.919 | 1.11 (0.87–1.42) | 0.385 |
| CV mortality or CV hospitalization | 1021 (58) | 343 (67) | 678 (54) | 1.37 (1.21–1.57) | <0.001 | 1.22 (0.97–1.30) | 0.120 | 1.16 (1.01–1.33) | 0.035 |
| CV mortality or HF hospitalization | 590 (33) | 227 (44) | 363 (29) | 1.68 (1.43–1.99) | <0.001 | 1.20 (0.99–1.44) | 0.060 | 1.27 (1.06–1.51) | 0.008 |
| CV mortality | 261 (15) | 97 (19) | 164 (13) | 1.46 (1.14–1.88) | 0.003 | 0.93 (0.71–1.23) | 0.619 | 1.09 (0.83–1.43) | 0.527 |
| All‐cause hospitalization | 1150 (65) | 387 (75) | 763 (61) | 1.46 (1.29–1.65) | <0.001 | 1.16 (1.01–1.33) | 0.040 | 1.27 (1.12–1.45) | <0.001 |
| CV hospitalization | 950 (54) | 320 (62) | 630 (50) | 1.37 (1.20–1.57) | <0.001 | 1.12 (0.96–1.30) | 0.138 | 1.17 (1.02–1.35) | 0.03 |
| HF hospitalization | 464 (26) | 186 (36) | 278 (22) | 1.79 (1.49–2.15) | <0.001 | 1.25 (1.02–1.54) | 0.032 | 1.33 (1.09–1.61) | 0.005 |
| ED or urgent clinic visit for HF exacerbation | 1033 (59) | 346 (67) | 687 (55) | 1.40 (1.25–1.57) | <0.001 | 1.21 (1.04–1.40) | 0.012 | 1.20 (1.05–1.38) | 0.008 |
Abbreviations: CI, confidence interval; CV, cardiovascular; ED, emergency department; HF, heart failure; HR, hazard ratio; IQR, interquartile range.
Adjusted HRs are derived from adjustment models 1 and 2 described in the Methods section.
Discussion
The current analysis provides a unique opportunity to evaluate the relationship of anemia to outcomes in stable HF patients with preserved eGFR. In general, all the unadjusted HRs for trial endpoints were elevated for those with anemia. There were no indications of competing risks given the similar follow‐up times for those with and without anemia (median 30 months for each; Table 2). For both the original predictive model developed for the primary endpoint and the modified model, anemia was associated with the primary endpoint of time to all‐cause mortality or hospitalization. Although the associations with other trial outcomes were nonsignificant in the global model, these associations were evident for the primary and secondary outcomes when the model was modified to be more specific to an evaluation of anemia. These data are consistent with the notion that anemia, even in those with only mildly reduced or normal renal function, is an elevated risk state for patients with HFREF and represents a complicated clustering of modulators that are related to CV mortality or hospitalization.16 Anemia may be both a contributor and a result of HF as a chronic disease state. Reduced Hb is associated with impaired oxygen delivery, salt and water retention, and chronic volume overload, which may exacerbate HF symptoms.17 It has been reported in clinical trials and observational studies that patients with the lowest Hb values have higher physician‐assigned NYHA class and worse HF symptoms.17 Additionally, anemia has been consistently associated with higher rates of hospitalization for HF and other causes as well as all‐cause mortality in those with HF.18, 19 Anemia can be considered a manifestation of the chronic cardiorenal syndrome, where either the HF worsens kidney function (type 2) or vice versa (type 4).20 In cardiorenal syndromes, anemia may play a role in reducing oxygen delivery, thus impairing myocardial contractility and systolic performance.21 In addition, increased LV mass is commonly associated with anemia and progressive renal failure and may be related to the impairment of cellular transport of electrolytes and oxygen, which affects mechanical and metabolic functions.22 Chronic kidney disease and HF have been associated with increased levels of hepcidin‐25, which inhibits the ferroportin transporter and blocks iron transport from the gut and at many somatic levels.23 Also, reduced renal mass is associated with relative deficiency of erythropoietin, which is partially responsible for the predictable decline in erythroid mass as renal function declines. Moreover, deficient levels of erythropoietin may directly influence LV remodeling and HF.24 Lastly, anemia is associated with increased markers of inflammation and oxidative stress.25, 26 Collectively, these pathologic changes may be responsible for the higher morbidity and mortality associated with anemia in HFREF that we reported in HF‐ACTION and has been observed in other studies.17
This study adds to the literature in demonstrating that anemia, even at higher levels of eGFR at baseline, is independently associated with an array of adverse outcomes including cardiac and all‐cause hospitalization, emergency department or urgent clinic visit for HF exacerbation, and death due to HF or other cardiac causes.
We recognize that both renal‐filtration function and older age are important confounders in the relationship between anemia and poor outcomes.16, 27 Herzog and colleagues found that, among Medicare recipients not on dialysis, the annual mortality rate was 4% for those with no HF, CKD, or anemia. The mortality rate was 8% for anemia or CKD, 13% for HF, and 23% for all 3 conditions in the same patient population.28 The annual mortality rate in HF ACTION was <10%, suggesting selection bias for the trial significantly reduced generalizability and may have reduced the relative impact of anemia on survival. Thus, both in community populations and clinical trials, senescent decline in both bone marrow and renal function may play a role in cardiac adverse events precipitating hospitalization, and in some circumstances, contributing to death.29, 30
Our findings suggested that investigator reported adverse events related to the heart were more frequent in those with anemia. Finally, the triad of older age, anemia, and reduced renal function may identify a particularly frail population that is more prone to medication adverse events, complications with invasive procedures, and a greater susceptibility to event‐driven mortality over the natural history of HF.31, 32
Study Limitations
Our study has all the limitations of a post hoc analysis from a large randomized trial. Selection bias for entry into the trial of exercise training yielded a younger and more robust group of HF patients able to exercise, which may not represent those commonly seen in clinical practice. We did not have baseline Hb or SCr values on all the subjects in the trial; thus, this is a subgroup that has both measures recorded on the case report form up to 1 year prior to randomization. We did not have a background history of prior anemia or its treatments, including iron or erythrocyte‐stimulating agents. Because subjects were restricted to having systolic HF, we cannot generalize our findings to those with more modestly reduced LVEF (36%–45%) or to those with preserved systolic function. Hemoglobin and SCr values were obtained from clinical records and not measured in a core laboratory. Thus, differences in assay types and standardization probably contributed to variation in eGFR. Furthermore, we did not measure arterial blood gases, serum iron indices, folate, vitamin B12, or erythropoietin precluding the etiology of anemia. Lastly, we did not have measures of iron transport, inflammation, and oxidative stress or other biomarkers to elucidate the pathophysiologic mechanisms relating chronic failure of the heart, bone marrow, and kidneys.33
The current analysis provides results from 2 models, which both have limitations. Model 1 was derived a priori from the complete cohort. Hemoglobin values were missing in 24% of the cases and were imputed in order to be included in the preconstructed global model (Model 1). Derived variables integrating information such as eGFR or anemia as defined as a disease state in this paper were not considered at the time Model 1 was created. Model 1 also did not allow clinical refinement for multicollinearity and did not exclude potential symptomatic outcomes of anemia as predictors. Additionally, since Model 1 had a large number of predictor variables relative to the number of outcomes, it was subject to overfitting and overadjustment.34 Whereas Model 2 addressed some of the shortcomings of Model 1, it excluded known predictors of clinical outcomes in HF featured in other HF‐ACTION papers, including peak oxygen uptake (VO2), quality of life, medication treatment, and detailed echocardiographic measures.35 Model 2 was created based upon univariate findings and after Model 1 results were known. Both models have the limitation of unknown or unmeasured confounders that may account for the association between anemia and the clinical outcomes reported.36
Conclusion
Anemia is associated with increased rates of death, hospitalization, and HF exacerbation in outpatients with chronic HFREF and with both preserved and decreased renal filtration function. After adjusting for other important covariates, anemia is independently associated with an excess hazard for all‐cause mortality and all‐cause hospitalization. Anemia is also associated with combinations of CV death and CV/HF hospitalizations as composite endpoints.
Supporting information
Appendix S1.
This work was funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health. The authors acknowledge the HF‐ACTION Trial and Amgen, Inc., for partial support of statistical analyses and manuscript preparation and finalization. Dr. Kilpatrick is an employee and stockholder of Amgen, Inc., which provided funding for this analysis. ClinicalTrials.gov identifier: NCT00047437.
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1. McCullough PA, Philbin EF, Spertus JA, et al. Confirmation of a heart failure epidemic: findings from the Resource Utilization Among Congestive Heart Failure (REACH) Study. J Am Coll Cardiol. 2002;39:60–69. [DOI] [PubMed] [Google Scholar]
- 2. Szczech LA, Harmon W, Hostetter TH, et al. World Kidney Day 2009: problems and challenges in the emerging epidemic of kidney disease. J Am Soc Nephrol. 2009;20:453–455. [DOI] [PubMed] [Google Scholar]
- 3. Whaley‐Connell AT, Sowers JR, Stevens LA, et al; Kidney Early Evaluation Program Investigators. CKD in the United States: Kidney Early Evaluation Program (KEEP) and National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2008;51(4 suppl 2):S13–S20. [DOI] [PubMed] [Google Scholar]
- 4. Whaley‐Connell AT, Sowers JR, McFarlane SI, et al; Kidney Early Evaluation Program Investigators. Diabetes mellitus in CKD: Kidney Early Evaluation Program (KEEP) and National Health and Nutrition and Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2008;51(4 suppl 2):S21–S29. [DOI] [PubMed] [Google Scholar]
- 5. Artham SM, Lavie CJ, Patel HM, et al. Impact of obesity on the risk of heart failure and its prognosis. J Cardiometab Syndr. 2008;3:155–161. [DOI] [PubMed] [Google Scholar]
- 6. Zalesin KC, Franklin BA, Miller WM, et al. Impact of obesity on cardiovascular disease. Endocrinol Metab Clin North Am. 2008;37:663–684. [DOI] [PubMed] [Google Scholar]
- 7. McFarlane SI, Chen SC, Whaley‐Connell AT, et al.; Kidney Early Evaluation Program Investigators. Prevalence and associations of anemia of CKD: Kidney Early Evaluation Program (KEEP) and National Health and Nutrition Examination Survey (NHANES) 1999‐2004. Am J Kidney Dis. 2008. Apr;51(4 Suppl 2):S46‐55. [DOI] [PubMed] [Google Scholar]
- 8. Wu AH, Omland T, Wold Knudsen C, et al; Breathing Not Properly Multinational Study Investigations. Relationship of B‐type natriuretic peptide and anemia in patients with and without heart failure: a substudy from the Breathing Not Properly (BNP) Multinational Study. Am J Hematol. 2005;80:174–180. [DOI] [PubMed] [Google Scholar]
- 9. Smith GL, Lichtman JH, Bracken MB, et al. Renal impairment and outcomes in heart failure: systematic review and meta‐analysis. J Am Coll Cardiol. 2006;47:1987–1996. [DOI] [PubMed] [Google Scholar]
- 10. McCullough PA, Lepor NE. Piecing together the evidence on anemia: the link between chronic kidney disease and cardiovascular disease. Rev Cardiovasc Med. 2005;(6 suppl 3):S4–S12. [PubMed] [Google Scholar]
- 11. Anand I, McMurray JJ, Whitmore J, et al. Anemia and its relationship to clinical outcome in heart failure. Circulation. 2004;110:149–154. [DOI] [PubMed] [Google Scholar]
- 12. Whellan DJ, O'Connor CM, Lee KL, et al; HF‐ACTION Trial Investigators. Heart failure and a controlled trial investigating outcomes of exercise training (HF‐ACTION): design and rationale. Am Heart J. 2007;153:201–211. [DOI] [PubMed] [Google Scholar]
- 13.O'Connor CM, Whellan DJ, Lee KL, et al; HF‐ACTION Investigators. Efficacy and safety of exercise training in patients with chronic heart failure: HF‐ACTION randomized controlled trial. JAMA. 2009;301:1439–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. de Benoist B, McLean E, Egli I, et al, eds. Worldwide Prevalence of Anaemia, 1993–2005. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 15. Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. [DOI] [PubMed] [Google Scholar]
- 16. McCullough PA, Franklin BA, Leifer E, et al. Impact of reduced kidney function on cardiopulmonary fitness in patients with systolic heart failure. Am J Nephrol. 2010;32:226–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McCullough PA, Lepor NE. The deadly triangle of anemia, renal insufficiency, and cardiovascular disease: implications for prognosis and treatment. Rev Cardiovasc Med. 2005;6:1–10. [PubMed] [Google Scholar]
- 18. von Haehling S, van Veldhuisen DJ, Roughton M, et al. Anaemia among patients with heart failure and preserved or reduced ejection fraction: results from the SENIORS study. Eur J Heart Fail. 2011;13:656–663. [DOI] [PubMed] [Google Scholar]
- 19. Hamaguchi S, Tsuchihashi‐Makaya M, Kinugawa S, et al; JCARECARD Investigators. Anemia is an independent predictor of long‐term adverse outcomes in patients hospitalized with heart failure in Japan: a report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARECARD). Circ J. 2009;73:1901–1908. [DOI] [PubMed] [Google Scholar]
- 20. Ronco C, McCullough P, Anker SD, et al; for the Acute Dialysis Quality Initiative (ADQI) consensus group. Cardio‐renal syndromes: report from the consensus conference of the Acute Dialysis Quality Initiative. Eur Heart J. 2010;31:703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Weisensee D, Schnaars Y, Schoeppe W, et al. Potential uremic toxins modulate energy metabolism of cardiac myocytes in vitro. Exp Nephrol. 1997;5:194–200. [PubMed] [Google Scholar]
- 22. Yerkey MW, Kernis SJ, Franklin BA, et al. Renal dysfunction and acceleration of coronary disease. Heart. 2004;90:961–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kato A. Increased hepcidin‐25 and erythropoietin responsiveness in patients with cardio‐renal anemia syndrome. Future Cardiol. 2010;6:769–771. [DOI] [PubMed] [Google Scholar]
- 24. Smith K, Semple D, Bhandari S, et al. Cellular basis of uraemic cardiomyopathy: a role for erythropoietin? Eur J Heart Fail. 2009;11:732–738. [DOI] [PubMed] [Google Scholar]
- 25. van der Zee S, Baber U, Elmariah S, et al. Cardiovascular risk factors in patients with chronic kidney disease. Nat Rev Cardiol. 2009;6:580–589. [DOI] [PubMed] [Google Scholar]
- 26. Kovesdy CP, Kalantar‐Zadeh K. Review article: Biomarkers of clinical outcomes in advanced chronic kidney disease. Nephrology (Carlton). 2009;14:408–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hawkins S, Wiswell R. Rate and mechanism of maximal oxygen consumption decline with aging: implications for exercise training. Sports Med. 2003;33:877–888. [DOI] [PubMed] [Google Scholar]
- 28. Herzog CA, Muster HA, Li S, et al. Impact of congestive heart failure, chronic kidney disease, and anemia on survival in the Medicare population. J Card Fail. 2004;10:467–472. [DOI] [PubMed] [Google Scholar]
- 29. Anderson S, Halter JB, Hazzard WR, et al; workshop participants. Prediction, progression, and outcomes of chronic kidney disease in older adults. J Am Soc Nephrol. 2009;20:1199–1209. [DOI] [PubMed] [Google Scholar]
- 30. Shlipak MG, Katz R, Kestenbaum B, et al. Clinical and subclinical cardiovascular disease and kidney function decline in the elderly. Atherosclerosis. 2009;204:298–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Franklin BA. Survival of the fittest: evidence for high‐risk and cardioprotective fitness levels. Curr Sports Med Rep. 2002;1:257–259. [DOI] [PubMed] [Google Scholar]
- 32. McCullough PA. Why is chronic kidney disease the “spoiler” for cardiovascular outcomes? J Am Coll Cardiol. 2003;41:725–728. [DOI] [PubMed] [Google Scholar]
- 33. Stenvinkel P, Carrero JJ, Axelsson J, et al. Emerging biomarkers for evaluating cardiovascular risk in the chronic kidney disease patient: how do new pieces fit into the uremic puzzle? Clin J Am Soc Nephrol. 2008;3:505–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. O'Connor CM, Whellan DJ, Wojdyla D, et al. Factors related to morbidity and mortality in patients with chronic heart failure with systolic dysfunction: the HF‐ACTION predictive risk score model. Circ Heart Fail. 2012;5:63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Enders CK. Applied Missing Data Analysis New York, NY: Guilford Press; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1.


