Abstract
Introduction and objective
The cost implications associated with offloading outpatient surgery from hospitals to ASCs and the physician office remain poorly defined. Motivated by this, we determined whether payments for outpatient surgery vary by location of care.
Methods
Using national Medicare claims (1998 to 2006), we identified elderly patients, who underwent one of 22 common outpatient urologic procedures. For each procedure, we measured all relevant payments (in USD) made during 30-day claims window that encompassed the procedure date. We then categorized payment types (hospital, physician, and outpatient facility). Finally, we used multivariable regression to compare price-standardized payments across hospitals, ASCs, and the physician office.
Results
Average total payments for outpatient surgery episodes varied widely, from USD 200 for urethral dilation in the office to USD 5,688 for hospital-based shockwave lithotripsy. For all but two procedure groups, ASCs and the office were associated with lower overall episode payments than hospitals. For instance, average total payments for urodynamic procedures performed at ASCs were less than a third of those done in hospitals (P<0.001). Compared to hospitals, office-based prostate biopsies were nearly 75% less costly (P<0.001). Outpatient facility payments were the biggest driver of these differences.
Conclusions
These data support policies that encourage the provision of outpatient surgery in less resource-intensive settings.
Introduction
Nearly 53 million outpatient procedures are performed in the U.S. annually.1 While most of these procedures occurred traditionally in hospital outpatient departments, more and more are now being done in nonhospital-based facilities, such as freestanding ASCs and physician offices.2 In fact, the rate of ambulatory surgery visits to these facilities has increased by 300% over the last decade.3 Surgical care delivered in an ASC or the physician office has several advantages. Quicker case turnaround leads to less time in the healthcare setting,4 which may enhance patient satisfaction. Further, these facilities allow physicians greater administrative control over the practice environment, which allows for increased productivity.5
However, the cost implications for payers associated with offloading outpatient surgery from the hospital remain poorly defined. On one hand, ASCs and physician offices may be associated with lower costs per surgical episode. Unlike hospitals, which must maintain sufficient infrastructure to support inpatient care, these facilities furnish exclusively outpatient services and, thus, can provide streamlined treatment.6 Conversely, there are circumstances under which ASCs and physician offices might not be as cost-efficient. For instance, these facilities have less capacity than hospitals to manage unforeseen emergencies. If complications requiring postoperative admission and/or professional care occur frequently,7, 8 surgery at an ASC or in the physician office may be more expensive.
In this context, we used national Medicare claims to examine episode payments around 22 common outpatient urologic procedures. In addition to providing a detailed description of how payments are currently dispersed across hospitals, ASCs, and physician offices, we explored the extent to which different types of payments vary by the ambulatory care setting where a procedure is performed.
Methods
Subjects and databases
For our study, we used the 5% national sample of Medicare standard analytic files, including hospital inpatient, hospital outpatient, and carrier claims. We obtained all files for calendar years 1998 through 2006 from CMS. We excluded from our study population Medicare Advantage patients because services provided to them are not consistently captured in claims files. We also excluded patients less than 65 years of age and those not enrolled in Medicare parts A and B for six months before and after surgery.
We used HCPCS codes to identify patients within the carrier claims file undergoing endoscopic bladder, urethral, or ureteral surgery; microwave therapy for prostate enlargement; prostate biopsy; shockwave lithotripsy; urethral dilation; or urodynamic procedures (Appendix Table). We selected these procedures for two reasons: 1) all can be performed in hospitals, ASCs, or physician offices; and 2) they capture approximately 95% of outpatient procedures done by urologists.
Setting for ambulatory surgery
Through the unique Medicare provider number, we assigned all patients to the facility where their procedure was performed. Next, we constructed a three-level categorical variable, specifying the type of ambulatory care setting. To distinguish between procedures carried out at hospitals from those done in ASCs and the physician office, we used appropriate Place of Service codes from the carrier line item file.
Assessing episode payments for ambulatory surgery
We measured actual Medicare payments at the patient level. A fundamental step for defining our outcome was to decide which payments were reasonably attributed to the surgical episode. Consistent with MedPAC recommendations,9 we used a claims window, extracting payment data for all services from the date of surgery to 30 days after the index procedure. This timeframe allowed us to capture costs related to such things as postoperative complications and unexpected admissions before average payments got back to the preoperative “baseline.10” We standardized all payments to 2005 USD and price-adjusted them to account for regional differences in Medicare reimbursement.11
To better understand the source of any differences in payments, we also characterized the major component payments. Specifically, we measured hospital payments, payments for physician services, and outpatient facility payments. Hospital payments entailed those related to same-day admissions and hospitalizations occurring within 30 days. Payments for physician services included professional fees, as well as those for laboratory and imaging services. Facility payments for surgical services rendered at the physician office are “packaged.” Whereas Medicare collects separate facility claims from hospital- and ASC-based outpatient procedures, supplies and equipment payments for those procedures performed in the physician office are bundled into the practice expense component and paid via the physician fee schedule. Thus, under our accounting system, physician office facility payments are captured in the physician services component of total episode payments.
Statistical Analysis
For our initial analytic step, we made comparisons between patients based on the ambulatory setting where their procedure was performed. In particular, we examined differences between patients with respect to their age, gender, race (white, black, or other), comorbid status (assessed with an adaptation of the Charlson index12), and area of residence (Northeast, Midwest, South, or West), using appropriate parametric and nonparametric statistics. Next, we compared, by procedure type, episode payments for patients (both total and component) across ambulatory care settings. We accounted for case mix differences using multiple linear regression. Specifically, we adjusted our models for those patient characteristics described above. Because our payment data were positively skewed, we had to apply a logarithmic transformation to normalize them. Given the potential correlation of observations (i.e., patients clustered within facilities), we used robust variance estimators.13 To derive predicted payments, we had to retransform our predicted values back to their original scale.14
We carried out all analyses using the SAS statistical package (SAS, version 9.1; SAS Institute, Cary, NC). All tests were two-tailed, and we set the probability of Type 1 error at .05. The Institutional Review Boards of the University of California at Los Angeles and the University of Michigan approved this study.
Results
Over the study interval, 88% of the procedures examined were performed in an ASC or a physician office. As shown in Table 1, there were disproportionately more ambulatory surgery visits to these facilities among patients who resided in the South (p<.001). Women and black patients were less likely than men and white patients, respectively, to receive care at a nonhospital-based facility (P<0.001 for each comparison). In addition, the average Charlson score for a patient who underwent a procedure in an ASC or a physician office was lower than that for a patient treated at a hospital (P<0.001).
Table 1.
Differences in case mix across ambulatory care settings.
| Patient Characteristic | Ambulatory Care Setting
|
P-Value | ||
|---|---|---|---|---|
| HOPD (n=33,802) | ASC (16,798) | PO (233,971) | ||
|
| ||||
| Patient age, in years (SD) | 75.4 (6.8) | 74.9 (6.5) | 75.4 (6.7) | <0.001 |
|
| ||||
| Female, % | 38.2 | 31.5 | 33.8 | <0.001 |
|
| ||||
| Race, % | <0.001 | |||
| White | 89.6 | 91.0 | 90.2 | |
| Black | 7.7 | 7.2 | 5.6 | |
| Other | 2.7 | 1.8 | 4.2 | |
|
| ||||
| Charlson, % | <0.001 | |||
| 0 | 59.1 | 82.6 | 62.9 | |
| 1 | 23.1 | 9.4 | 22.3 | |
| 2 | 9.9 | 4.6 | 8.7 | |
| ≥3 | 7.9 | 3.4 | 6.1 | |
|
| ||||
| Area of residence, % | <0.001 | |||
| Northeast | 19.7 | 11.4 | 20.4 | |
| Midwest | 37.8 | 17.0 | 24.4 | |
| South | 34.2 | 59.1 | 38.5 | |
| West | 8.3 | 12.5 | 16.7 | |
Abbreviations: ASC, ambulatory surgery center; HOPD, hospital outpatient department; PO, physician office; SD, standard deviation.
Average unadjusted total payments for outpatient surgery episodes varied widely, from USD 200 for urethral dilation in a physician’s office to USD 5,688 for shockwave lithotripsy in a hospital. After accounting for case-mix differences, ASCs and physician offices were less costly than hospitals for all but two procedure groups (Table 2). For instance, average adjusted total payments for urodynamic procedures performed at ASCs were less than a third of those done in hospitals (P<0.001). Compared to hospitals, office-based prostate biopsies were nearly 75% less costly (P<0.001). While the physician office tended to be more cost-efficient than ASCs, the absolute magnitude of this difference was small (Table 2).
Table 2.
Predicted episode payments, stratified by ambulatory care setting.
| Procedure Type | Predicted 30-Day Payments, in USD (SD)† | ||
|---|---|---|---|
| HOPD | ASC | PO | |
| Urethral dilation | 578 (47) | 204 (27) | 94 (7) |
| Endoscopic bladder surgery | 908 (28) | 519 (14)* | 251 (11)** |
| Endoscopic urethral surgery | 1215 (47) | 577 (20)* | 338 (17)** |
| Urodynamics procedures | 1311 (78) | 407 (21)* | 152 (12)** |
| Prostate biopsy | 868 (42) | 521 (19)* | 222 (11)** |
| Endoscopic ureteral surgery | 2129 (149) | 634 (39)* | 413 (31)** |
| Microwave therapy | 3029 (208) | 2084 (118) | 3174 (357) |
| Shockwave lithotripsy | 4754 (417) | 943 (69)* | 1095 (77)** |
Abbreviations: ASC, ambulatory surgery center; HOPD, hospital outpatient department; PO, physician office; SD, standard deviation; USD, United States dollars.
All payments standardized to 2005 USD. Adjustments made for case mix, as well as regional differences in Medicare reimbursement.
Indicates that predicted 30-day payments for a given procedures performed at an ASC are significantly lower than those at a HOPD (P<0.05).
Indicates that predicted 30-day payments for a given procedures performed at a PO are significantly lower than those at a HOPD (P<0.05).
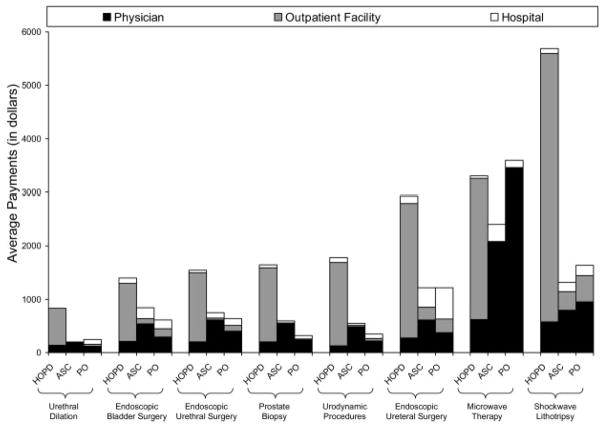
Outpatient facility payments were noted to be the biggest driver of the payment differences between hospitals and ASCs and the physician office (Figure 1). For example, outpatient facility payments accounted for 88% of the 30-day payments following shockwave lithotripsy in a hospital. Physician payments ranged from USD 117 (urethral dilation in a physician’s office) to USD 3,438 (microwave therapy in a physician’s office). Relative to hospitals, physician services constituted a larger proportion of average total payments at ASCs and physician offices.
Figure 1.
Differences in average total and component Medicare payments around episodes of urologic procedures across ambulatory care settings.
Abbreviations: ASC, ambulatory surgery center; HOPD, hospital outpatient department; PO, physician office.
Note: In the bar chart, black, grey, and white shading indicate average 30-day payments for physician, outpatient facility, and hospital services, respectively.
Discussion
Our findings indicate that average total payments around outpatient surgical episodes for urologic surgery vary by location of care. For comparable procedures, hospitals were associated with significantly higher 30-day payments than ASCs and the physician office. These differentials persisted even after case-mix adjustment. In fact, offloading 50% of the procedures examined from hospitals to ASCs would save the Medicare program nearly $66 million annually. While the physician office tended to be more cost-efficient than ASCs, the absolute magnitude of this difference was small. Outpatient facility payments were noted to be the biggest driver of the payment differences across ambulatory care settings.
To date, much of the literature on ambulatory surgical care in nonhospital-based facilities has focused on the issue of physician ownership and overuse.15, 16 Little work has examined their cost-efficiency. Prior studies characterizing overall episode payments have been limited to common inpatient procedures;10 however, few have examined payments related to outpatient procedures. Wynn and colleagues previously reported on payment differentials between ambulatory care settings for the facility-related components of care. Their results showed that payment rates for similar services varied among hospitals, ASCs, and the physician office, with the size of the differential varying by the service.17 Our findings suggest that these differences continue (and may even widen) well beyond the date of the index procedure, highlighting one of the advantages of ASCs and the physician office.
Our study must be considered in the context of several limitations. Several studies have compared the health status of patients treated across ambulatory care settings, demonstrating lower patient complexity at nonhospital-based facilities.18, 19 To the extent that low-risk patients are also less expensive to treat, our results might reflect patient clinical differences. We addressed this potential limitation in two ways. First, we performed case-mix adjustment using a well-developed approach to measure comorbidity. Second, because of potential heterogeneity between procedure groups, we also looked at total and component payments within them.
In addition, we based our analysis on Medicare claims data, and our results may not be generalizable to other payers. That said, the Medicare program accounts for 19% of total national spending on personal health services,20 making it the single largest payer in the U.S. Therefore, with regard to healthcare financing, as goes Medicare, so goes the nation. Finally, Medicare coverage for services provided in an ASC was recently changed.21 Since 2008, CMS has reimbursed facility fees for ASCs at two-thirds the rate of hospitals. Because our study was limited to claims through calendar year 2006, we could not assess the impact of this policy change on average 30-day payments. However, the differences that we observed across locations of care are likely to be more pronounced.
Limitations notwithstanding, our findings have possible implications for the Medicare program. If the observed differences among hospitals, ASCs, and physician offices in average total payments around outpatient surgical episodes are unjustified (i.e., due to inefficiencies rather than case mix, service, or content), CMS might base payment rates on costs in the least expensive setting. Alternatively, CMS may bundle reimbursements to facilities and physicians involved in care around an outpatient surgical episode into a single payment. Indeed the observed variation in outpatient facility payments suggests opportunities for improvement. Such a policy has been recommended by MedPAC for inpatient surgical procedures, in the hopes that it will help align providers around the common goal of improving quality and cost-efficiency.
Collectively, our data support policies that encourage the provision of outpatient surgical care in less resource-intensive settings. Moving forward, further research should consider how indirect costs are dispersed across hospitals, ASCs, and physician offices. Moreover, additional studies are needed to determine whether the savings accrued by ASCs’ lower episode costs are mitigated by increases in the total number of procedures associated with them.
Supplementary Material
Acknowledgments
Funding: This project was supported, in part, by grant number R01HS018726 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
References
- 1.Owings MF, Kozak LJ. Ambulatory and inpatient procedures in the United States, 1996. Vital Health Stat. 1998;13(139):1. [PubMed] [Google Scholar]
- 2.Winter A. Comparing the mix of patients in various outpatient surgery settings. Health Aff (Millwood) 2003;22:68. doi: 10.1377/hlthaff.22.6.68. [DOI] [PubMed] [Google Scholar]
- 3.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report. 2009;(11):1. [PubMed] [Google Scholar]
- 4.Berenson RA, Bodenheimer T, Pham HH. Specialty-service lines: salvos in the new medical arms race. Health Aff (Millwood) 2006;25:w337. doi: 10.1377/hlthaff.25.w337. [DOI] [PubMed] [Google Scholar]
- 5.Wolfson J, Walker G, Levin PJ. Freestanding ambulatory surgery: cost-containment winner? Healthc Financ Manage. 1993;47:26. [PubMed] [Google Scholar]
- 6.Casalino LP, Devers KJ, Brewster LR. Focused factories? Physician-owned specialty facilities. Health Aff (Millwood) 2003;22:56. doi: 10.1377/hlthaff.22.6.56. [DOI] [PubMed] [Google Scholar]
- 7.Chukmaitov AS, Menachemi N, Brown LS, Suanders C, Brooks RG. A comparative study of quality outcomes in freestanding ambulatory surgery centers and hospital-based outpatient departments: 1997–2004. Health Serv Res. 2008;43:1485. doi: 10.1111/j.1475-6773.2007.00809.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fleisher LA, Pasternak LR, Herbert R, Anderson GF. Inpatient hospital admission and death after outpatient surgery in elderly patients: importance of patient and system characteristics and location of care. Arch Surg. 2004;139:67. doi: 10.1001/archsurg.139.1.67. [DOI] [PubMed] [Google Scholar]
- 9.Medicare Payment Advisory Commission. [Accessed on May 25, 2011.];Report to the Congress: Improving incentives in the Medicare program. 2009 Available at: http://www.medpac.gov/documents/Jun09_EntireReport.pdf.
- 10.Birkmeyer JD, Gust C, Baser O, Dimick JB, Sutherland JM, Skinner JS. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res. 2010;45:1783. doi: 10.1111/j.1475-6773.2010.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don’t drive regional Medicare spending variations. Health Aff (Millwood) 2010;29:537. doi: 10.1377/hlthaff.2009.0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 13.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817. [Google Scholar]
- 14.Manning WG. The logged dependent variable, heteroscedasticity, and the retransformation problem. J Health Econ. 1998;17:283. doi: 10.1016/s0167-6296(98)00025-3. [DOI] [PubMed] [Google Scholar]
- 15.Hollingsworth JM, Ye Z, Stope SA, Krein SL, Hollenbeck AT, Hollenbeck BK. Opening of ambulatory surgery centers and procedure use in elderly patients: data from Florida. Arch Surg. 2011;146:187. doi: 10.1001/archsurg.2010.335. [DOI] [PubMed] [Google Scholar]
- 16.Hollingsworth JM, Krein SL, Ye Z, Kim HM, Hollenbeck BK. Urologist ownership of ambulatory surgery centers and urinary stone surgery use. Health Serv Res. 2009;44:1370. doi: 10.1111/j.1475-6773.2009.00966.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wynn BO, Hilborne LH, Hussey P, Sloss EM, Murphy E. Medicare payment differentials across ambulatory settings. RAND; Santa Monica, CA: Jul, 2008. [Accessed May 26, 2011.]. p. WR-602. Available at: http://www.rand.org/pubs/working_papers/2008/RAND_WR602.pdf. [PMC free article] [PubMed] [Google Scholar]
- 18.Sloss EM, Fung C, Wynn BO, eAshwood JS, Stoto MA. Further analyses of Medicare procedures provided in multiple ambulatory settings. RAND; Santa Monica, CA: May, 2006. [Accessed on May 26, 2011.]. p. WR-349. Available at: http://www.healthlawyers.org/SiteCollectionDocuments/Content/ContentGroups/Publications2/Health_Lawyers_Weekly2/Volume_4/Issue_432/MedPAC_rpt.pdf. [Google Scholar]
- 19.Wynn BO, Sloss EM, Pung C, Shugarman LR, Ashwood JS, Asch SM. Services provided in multiple ambulatory settings: a comparison of selected procedures. RAND; Santa Monica, CA: Nov, 2004. [Accessed on May 26, 2011.]. p. WR-157. Available at: http://www.eveia.com/RandMedPac2004.pdf. [Google Scholar]
- 20.The Henry J. Kaiser Family Foundation. [Accessed on May 26, 2011.];Medicare at a glance. Fact Sheet #1066-06.b. 2003 Available at: http://www.kff.org/medicare/upload/Medicare-At-A-Glance-Fact-Sheet-Fact-Sheet.pdf.
- 21.Centers for Medicare & Medicaid Services. Medicare program: Changes to the hospital outpatient prospective payment system and CY 2008 payment rates, the ambulatory surgical center payment system and CY 2008 payment rates, the hospital inpatient prospective payment system and FY 2008 payment rates; and payments for graduate medical education for affiliated teaching hospitals in certain emergency situations Medicare and Medicaid programs: hospital conditions of participation; necessary provider designations of critical access hospitals. Interim and final rule with comment period. Fed Regist. 2007;72:66579. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.