Abstract
Objective
A nighttime dip in blood pressure is associated with decreased risk of cardiovascular morbidity and mortality. We examined whether personality traits predict nighttime dipping blood pressure.
Methods
A community-based sample of 2,848 adults from Sardinia (Italy) completed the Revised NEO Personality Inventory and 7.34-years later (SD=0.87) were examined with 24-hour ambulatory blood pressure monitoring. The primary analyses examined the associations of personality traits with continuous and categorical measures of mean arterial, systolic and diastolic blood pressure nighttime dipping.
Results
Agreeableness and conscientiousness were associated with more nocturnal blood pressure dipping (β = .05, p=.025 and β = .07, p<.001, respectively) and lower systolic blood pressure at night (β = -.045, p=.018 and β = -.032; p=.072, respectively). Non-dippers were particularly more impulsive (p=.009), less trusting (p=.004), and less self-disciplined (p=.001), but there was no significant association between nocturnal dipping blood pressure and trait anxiety (p=.78) or depression (p=.59). The associations were stronger when comparing extreme dippers (nighttime drop ≥ 20%) to reverse dippers (nighttime increase in blood pressure). Indeed, scoring 1 SD higher on conscientiousness was associated with about 40% reduced risk of reverse dipping (OR = 1.43, CI = 1.08-1.91).
Conclusions
We found evidence that reduced nighttime blood pressure dipping is associated with antagonism and impulsivity related traits but not with measures of emotional vulnerability. The strongest associations were found with conscientiousness, a trait that may have broad impact on cardiovascular health.
Keywords: Ambulatory Blood Pressure Monitoring, Circadian Rhythm, Dipping, Impulsivity, Conscientiousness, Trust, Personality, Systolic blood pressure, Cardiovascular
Introduction
There is increasing recognition that circadian patterns of blood pressure (BP) are associated with cardiovascular health. In healthy individuals, BP tends to drop during the first few hours of sleep followed by a surge in the morning (1). This dip in nocturnal BP, relative to daytime BP, is typically assessed with a 24-hour ambulatory blood pressure monitor (ABPM). A pattern of nocturnal non-dipping BP (defined as a drop of less than 10%) has been associated with target-organ damage, vascular events, and cardiovascular mortality (2-6). The cardiovascular risk associated with non-dipping has been found in both normotensive and hypertensive subjects (7).
Several factors contribute to non-dipping BP, including lower depth and quality of sleep, lower level of activity during the day, ethnicity, higher sympathetic nervous system arousal, renal dysfunction, and endocrine conditions (1, 3, 8-10). Psychological factors have also been linked to a non-dipping pattern, including depression (11), anxiety (12), and anger and hostility-related traits (13, 14). These traits are obvious candidates because they are also associated with other cardiovascular risk factors, cardiovascular events, and mortality (15-20).
There is growing evidence, however, that other personality traits are relevant to health and longevity (21-30). In particular, traits related to conscientiousness are associated with health outcomes with effects that are similar or stronger than those for traits most often considered in cardiovascular research. This study aims to extend the research on psychological correlates of non-dipping BP by examining systematically a full spectrum of personality traits organized under the five major dimensions of personality. These five traits are defined as neuroticism (the tendency to experience emotional distress, anxiety, and depression), extraversion (sociable, out-going, full of energy and with a positive outlook), openness (creative, unconventional, curious, sensitive to feelings and aesthetics), agreeableness (a tendency to trust, cooperate, and please others; antagonism is the opposite pole of this trait), and conscientiousness (a measure of self-control, order, discipline, and industriousness)(31). We examined the association between personality traits and BP dipping, both as a continuous measure and as categorical classifications. We also examined the association between personality factors and mean nighttime BP to complement past research that focused on daytime BP. The study was conducted in a large, community-based sample from a genetically homogeneous population in Sardinia, Italy. The personality traits assessed at baseline were used to prospectively predict BP nocturnal dipping measured about seven years later.
Methods
Participants
Participants were part of the SardiNIA project, an ongoing multidisciplinary study of the genetic and environmental basis of complex traits and age-related processes (32). Participants were from a cluster of four towns in the Ogliastra province of Sardinia, Italy. The population in this rural region is characterized by a relatively low level of genetic admixture and a high proportion of long-lived individuals (33). The current study included 2,848 participants who completed the personality questionnaire and the 24-hour ABPM. Most of the personality data were collected during the first wave of assessment (2001 to 2004) and most of the ABPM data were collected during the third wave of assessment (2008 to 2012). Prior to each assessment, participants provided written informed consent. The research protocol and the consent form were approved by local institutional review boards in Italy and the United States (including the MedStar Research Institute Institutional Review Board in Baltimore and the Florida State University Human Subjects Committee in Tallahassee).
Measures - Personality Assessment
Participants completed the Italian version of the Revised NEO Personality Inventory (NEO-PI-R)(31). The NEO-PI-R is a 240-item questionnaire that assesses 30 facets, six for each of the five major dimensions of personality. Participants filled out the self-report questionnaire (90%) or chose to have the questionnaire read by a trained Sardinian psychologist (10%). A variable (test administration) that indicated this difference in the administration of the NEO-PI-R was used as a covariate in the analyses. Raw scores were standardized as T scores (M = 5, SD = 1) using combined-sex norms reported in the manual (31). In this sample, the NEO-PI-R factor structure shows good congruence with the normative structure and the internal consistencies for the five dimensions ranged from 0.80 to 0.87. Individual differences in personality traits are generally consistent across measurement occasions. Indeed, for the five major dimensions assessed by the NEO-PI-R, the test-retest correlations have been found to range from 0.78 to 0.85 over an average interval of 10 years (34).
Measures – Nocturnal blood pressure dipping
A SpaceLabs 90207 (SpaceLabs Redmond, WA) device was used to monitor ambulatory BP over 24 hours. A cuff of appropriate size was placed on the left arm by a nurse who explained the procedure to the participants and performed measurement tests. The compliance with the ABPM was generally good. BP was measured at 20-min intervals from 6:00AM to 10:00PM and at 40-min intervals during the nighttime. ABPM readings were screened to reduce measurement errors. Individuals with fewer than 31 valid readings during the day or fewer than 9 during the night were not included in the analyses.
Day-time BP means were calculated as the average of all valid readings after 6:00AM until 10:00PM. Nighttime averages included readings from 10:00PM to 6:00AM. The percent reduction in nighttime BP was calculated with the formula: [(daytime BP - nighttime BP)/daytime BP] × 100. We report the results for mean arterial pressure (MAP=1/3 systolic BP + 2/3 diastolic BP) because by combining the systolic and diastolic BP measures, the MAP is likely to be more accurate than either measure alone(9). However, given that different measures of BP have been used in previous studies, we present the associations between personality and nocturnal BP dipping based on MAP, systolic, and diastolic BP. According to conventional criteria, individuals were classified as dippers if the dipping ratio was ≥ 10%, and as a non-dipper otherwise. In follow-up analyses, participants were further classified as extreme dippers (BP decline ≥ 20%), dippers (BP decline between 10% and 20%), non-dippers (BP decline between 0% and 10%), and reverse dippers or risers (higher nighttime than daytime BP)(6, 35).
Statistical analyses
Univariate differences in sample characteristics were tested using chi-square or ANOVA, as appropriate. Linear and logistic regressions were used to evaluate whether personality traits were associated with dipping status, either as a continuous or categorical variable, respectively. We also examined whether the association between personality and dipping status was different for hypertensive versus normotensive individuals by testing the interaction of the five broad factors with hypertension, defined as ABPM mean day systolic/diastolic ≥ 130/85 and/or night systolic/diastolic ≥ 120/70 mm Hg (36) and/or treatment with anti-hypertensive drugs. Finally, we used linear regression to examine whether the five personality factors were associated with mean nighttime systolic and diastolic BP. All analyses were controlled for age, sex, education, antihypertensive medication, season (BP tends to be lower in the summer: 21-June to 21-September), time interval, cigarette smoking, obesity (body mass index (BMI) ≥30; based on staff assessed weight and height), diabetes, and personality test administration. The significance level was set at p < 0.05, two-tailed. No correction for multiple testing was done to avoid inflated type 2 errors (37). The analyses were run using the SPSS software version 20 (IBM SPSS Statistics).
Results
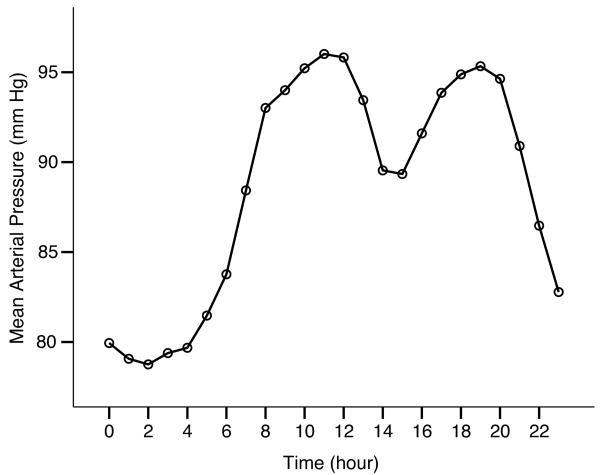
As detailed in Table 1, the sample included 60% women and age ranged from 19 to 90 years (M = 50.62; SD = 15.37) at the time of ABPM assessment. Personality traits were assessed from 3 to 10 years earlier (time interval: M = 7.34, SD = 0.87). After screening, there was an average of 56.56 (SD = 4.7) BP readings per participant, for a total of 161,069 BP assessments across all participants. Figure 1 collapses data across all individuals and plots the mean assessments by hour, starting from midnight. The pattern in this sample confirms an average nighttime dip in BP, with a nadir at about 2 AM and a peak at about 11 AM. On average, there was a 12% dip in MAP at night (M=12.25, SD = 6.60). About 35% of participants had less than 10% MAP dipping at night and were classified as non-dippers. Roughly 4% were reverse dippers and 11% were extreme dippers. As reported in Table 1, compared to dippers, the non-dippers were older (p = 0.050), less educated (p = 0.020), more likely to be obese (p = 0.020), diabetic (p < 0.001), and on hypertensive medications (p < 0.001). Basic univariate analyses also indicated that non-dippers scored lower on agreeableness (p = 0.041) and conscientiousness (p = 0.004). There were no significant differences between dippers and non-dippers on sex (p = 0.22), current smoking (p = 0.44), former smoking (p = 0.50), and time interval between the personality and the ABPM assessment (p = 0.25).
Table 1. Descriptive statistics for the total sample and separately for dippers and non-dippers.
| Total (N=2848) |
Dippers (N=1843) |
Non-dippers (N=1005) |
|
|---|---|---|---|
| Age, y | 50.62 (15.37) | 50.20 (14.55) | 51.39 (16.74)* |
| Time interval, y | 7.34 (0.87) | 7.33 (0.86) | 7.37 (0.89) |
| Sex, female, n (%) | 1718 (60%) | 1127 (61%) | 591 (59%) |
| Education –None | 76 (3%) | 41 (2%) | 35 (4%)* |
| –Elementary | 518 (18%) | 313 (17%) | 205 (20%) |
| –Junior high | 1252 (44%) | 829 (45%) | 423 (42%) |
| –High school | 754 (27%) | 497 (27%) | 257 (26%) |
| –University | 248 (9%) | 163 (9%) | 85 (8%) |
| Current smoker, n (%) | 475 (17%) | 300 (16%) | 175 (17%) |
| Former smoker, n (%) | 713 (25%) | 454 (25%) | 259 (26%) |
| BMI | 25.97 (4.62) | 25.84 (4.53) | 26.19 (4.78)* |
| Obese, n (%) | 511 (18%) | 308 (17%) | 203 (20%)* |
| Diabetes, n (%) | 117 (4%) | 54 (3%) | 63 (6%)* |
| Anti-hypertensive drugs | 560 (20%) | 315 (17%) | 245 (24%)* |
| MAP, day, mm Hg | 92.49 (8.72) | 93.52 (8.41) | 90.59 (8.95)* |
| MAP, night, mm Hg | 81.03 (8.74) | 78.47 (7.50) | 85.72 (8.90)* |
| MAP Dipping, % | 12.25% | 16.03% | 5.34%* |
| Systolic , day, mm Hg | 122.09 (11.73) | 122.86 (11.50) | 120.69 (12.03)* |
| Systolic, night, mm Hg | 110.63 (11.93) | 107.43 (10.36) | 116.50 (12.39)* |
| Systolic Dipping, % | 9.28% | 12.47% | 3.44%* |
| Diastolic , day, mm Hg | 76.83 (8.12) | 78.00 (7.76) | 74.67 (8.34)* |
| Diastolic, night, mm Hg | 65.48 (7.90) | 63.45 (6.97) | 69.21 (8.16)* |
| Diastolic Dipping, % | 14.60% | 18.59% | 7.26%* |
| Neuroticism | 5.54 (0.90) | 5.53 (0.90) | 5.56 (0.90) |
| Extraversion | 4.84 (0.88) | 4.86 (0.88) | 4.81 (0.88) |
| Openness | 4.63 (0.98) | 4.64 (0.96) | 4.62 (1.02) |
| Agreeableness | 4.71 (0.94) | 4.74 (0.93) | 4.66 (0.95)* |
| Conscientiousness | 4.94 (0.94) | 4.97 (0.92) | 4.87 (0.98)* |
Notes: The values are mean and (SD) if not specified as number of participants and percentages. Except for personality traits, all variables were assessed at the time of ambulatory blood pressure measurement. MAP = Mean arterial pressure. Univariate differences in sample characteristics were tested using chi-square or ANOVA, as appropriate.
p < .05.
Fig. 1.
Table 2 shows the association between personality and the continuous measures of nighttime BP dipping, controlling for the covariates. The results were similar across the measures of MAP, systolic and diastolic dipping in BP. Scoring higher in conscientiousness and agreeableness was associated with more nighttime BP dipping. The logistic regressions yielded similar results (Table 2): every standard deviation higher score in either conscientiousness or agreeableness was associated with a more than 10% reduced risk of being a non-dipper. The results were similar when all five traits were tested simultaneously (conscientiousness: OR = 0.88, CI = 0.80-0.97; agreeableness: OR = 0.90, CI = 0.82-0.99). The results were also similar when dippers vs. non-dippers were categorized using systolic (conscientiousness: OR = 0.88, CI = 0.80-0.95; agreeableness: OR = 0.93, CI = 0.85-1.01) or diastolic BP (conscientiousness: OR = 0.90, CI = 0.82-0.98; agreeableness: OR = 0.85, CI = 0.77-0.99).
Table 2.
Personality traits predicting nighttime blood pressure dipping 7 years later.
| Personality traits | Dipping MAP Beta | Dipping Systolic Beta | Dipping Diastolic Beta | Non-dipper (Dipping MAP<10%) Odds Ratios (95%CI) |
|---|---|---|---|---|
| N: Neuroticism | -0.03 | -0.04^ | -0.03 | 1.05 (0.95-1.14) |
| E: Extraversion | 0.02 | 0.01 | 0.03 | 0.95 (0.86-1.04) |
| O: Openness | 0.00 | 0.01 | -0.01 | 1.03 (0.94-1.12) |
| A: Agreeableness | 0.05* | 0.04^ | 0.04^ | 0.89 (0.81-0.97)* |
| C: Conscientiousness | 0.07* | 0.06* | 0.07* | 0.87 (0.80-0.95)* |
| N1: Anxiety | 0.01 | 0.01 | 0.00 | 0.96 (0.87-1.05) |
| N2: Angry Hostility | -0.03 | -0.03 | -0.02 | 1.07 (0.98-1.16) |
| N3: Depression | -0.01 | -0.03 | -0.01 | 1.02 (0.93-1.11) |
| N4: Self-consciousness | -0.02 | -0.02 | -0.01 | 1.01 (0.93-1.09) |
| N5: Impulsiveness | -0.05* | -0.05* | -0.05* | 1.10 (1.01-1.21)* |
| N6: Vulnerability | -0.04* | -0.03^ | -0.04^ | 1.05 (0.98-1.14) |
| E1: Warmth | 0.04^ | 0.03 | 0.03^ | 0.94 (0.86-1.02) |
| E2: Gregariousness | 0.04^ | 0.02 | 0.03 | 0.92 (0.85-1.00) |
| E3: Assertiveness | 0.01 | 0.01 | 0.01 | 0.94 (0.85-1.04) |
| E4: Activity | 0.03^ | 0.02 | 0.04* | 0.92 (0.84-1.01) |
| E5: Excitement-Seeking | -0.03 | -0.03 | -0.02 | 1.05 (0.95-1.15) |
| E6: Positive Emotions | 0.00 | 0.00 | 0.00 | 1.03 (0.96-1.12) |
| O1: Fantasy | -0.01 | 0.00 | 0.00 | 1.07 (0.98-1.17) |
| O2: Aesthetics | 0.00 | 0.01 | -0.01 | 1.03 (0.94-1.13) |
| O3: Feelings | -0.02 | -0.02 | -0.02 | 1.07 (0.98-1.16) |
| O4: Actions | 0.02 | 0.03 | 0.02 | 0.93 (0.86-1.01) |
| O5: Ideas | -0.02 | 0.00 | -0.03 | 1.00 (0.92-1.09) |
| O6: Values | 0.01 | 0.03 | 0.00 | 1.01 (0.92-1.11) |
| A1: Trust | 0.05* | 0.05* | 0.05* | 0.87 (0.81-0.94)* |
| A2: Straightforwardness | 0.02 | 0.02 | 0.01 | 0.94 (0.87-1.03) |
| A3: Altruism | 0.04^ | 0.03 | 0.03^ | 0.95 (0.88-1.04) |
| A4: Compliance | 0.02 | 0.02 | 0.02 | 0.97 (0.90-1.04) |
| A5: Modesty | 0.02 | 0.01 | 0.02 | 0.93 (0.85-1.02) |
| A6: Tender-mindedness | 0.00 | 0.00 | 0.00 | 0.98 (0.91-1.07) |
| C1: Competence | 0.05* | 0.04* | 0.05* | 0.89 (0.82-0.97)* |
| C2: Order | 0.06* | 0.05* | 0.06* | 0.90 (0.83-0.98)* |
| C3: Dutifulness | 0.07* | 0.06* | 0.06* | 0.88 (0.81-0.96)* |
| C4: Achievement Striving | 0.03 | 0.02 | 0.04^ | 0.94 (0.87-1.03) |
| C5: Self-Discipline | 0.06* | 0.05* | 0.06* | 0.90 (0.82-0.98)* |
| C6: Deliberation | 0.03 | 0.03 | 0.03^ | 0.94 (0.88-1.02) |
Note. Dipper N=1843; Non-Dipper N=1005. The standardized Beta coefficients are from linear regressions with personality predicting continuous dipping variables. The Odds Ratios are from logistic regression predicting the risk of non-dipping vs. dipping. Regression analyses controlling for age, sex, education, antihypertensive medication use, season, time interval, cigarette smoking, obesity, diabetes, and type of personality test administration. MAP = Mean arterial pressure. 95% CI = 95% Confidence Interval.
P < 0.05;
P < 0.10.
Table 2 further presents the results for the 30 facets that compose the broader personality factors. Among the facets of neuroticism, impulsiveness was associated with a reduced nocturnal BP fall, but there was no significant association between BP dipping and either trait anxiety or depression. For agreeableness, only the trust facet was related to nighttime dipping BP. Instead, almost all facets of conscientiousness were associated with dipping BP pattern, including the facets of competence (effective, prepared, capable), order (organized, neat, methodical), dutifulness (reliable, responsible, dependable), and self-discipline (motivated, self-control).
We further tested whether the association between personality and BP dipping differed between those with or without hypertension. None of the interactions between the five personality factors and hypertension status were significant, which suggests that the associations between personality traits and BP dipping were not significantly different across normotensive and hypertensive participants.
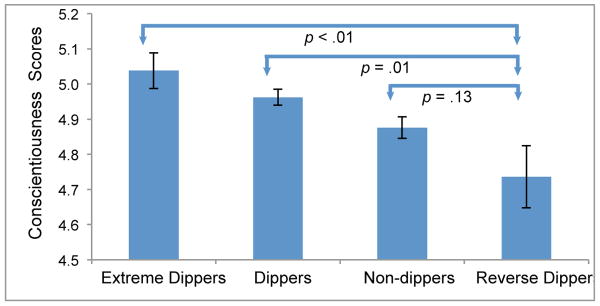
Some studies suggest that among non-dippers, those with a more extreme pattern are at even greater risk. These studies have found that reverse dippers, those with BP higher at night than during the day, are at greatest risk (6). In Figure 2, we present the covariate-adjusted mean conscientiousness scores for the four groups classified according to their dipping pattern. The level of conscientiousness was significantly and progressively lower from the extreme dippers to the reverse dippers. A logistic regression indicated that 1 SD lower score on conscientiousness was associated with a more than 40% increased risk of being a reverse dipper as compared to extreme dippers (OR = 1.43, CI = 1.08-1.91).
Fig. 2.
Finally we examined whether the five major dimensions of personality were associated with mean nighttime BP. In regression models that included all covariates, we found no significant associations between diastolic BP and the five major factors. However, those scoring higher on agreeableness (Beta = -0.045; p=0.018) and conscientiousness (Beta = -0.032; p=0.072) had slightly lower mean systolic BP at night. These associations were slightly stronger in models that did not include potential mediators, such as smoking, obesity and diabetes, as covariates (e.g., conscientiousness: Beta = -0.037; p=0.039).
Discussion
In a large community-based sample, we examined whether personality traits prospectively predicted circadian BP patterns seven years later. The results indicated that scoring lower on agreeableness and conscientiousness was associated with blunted nocturnal BP dipping, a risky pattern for cardiovascular morbidity and mortality. Logistic regressions indicated that 1 SD lower score on conscientiousness or agreeableness was associated with roughly 10% increased risk of non-dipping. These effects were generally stronger for conscientiousness and when comparing more extreme dipping patterns. Indeed, scoring 1 SD lower on conscientiousness was associated with about 40% increased risk of being a reverse dipper (i.e., those with higher nocturnal BP) as compared to extreme dippers (i.e., those with a ≥20% nocturnal decrease in BP). The association between personality and nighttime dipping was net of the effect of demographic variables, antihypertensive medication use, and other cardiovascular risk factors such as smoking and obesity. Personality shared similar associations with dipping among hypertensive and normotensive individuals, which indicates that personality traits are linked to a risky day/night BP pattern not only among those with hypertension. These associations are most likely driven by elevated systolic BP at night among those with lower agreeableness and lower conscientiousness, given that these traits were associated with nighttime but not daytime BP.
Thus, the results of this study suggest a link between personality traits, the physiology of sleep, and cardiovascular function. Evidence from other studies provides some clues to the mechanism underlying this pattern of associations. Regarding circadian preferences, it is intriguing that those who score high on conscientiousness, and to a lesser extent high agreeableness, are more likely to be morning type (38) and have a diurnal preference (39, 40). Furthermore, students with lower conscientiousness reported not getting enough sleep (41) and worse sleep quality (42). Thus, individuals who are less conscientious are more likely to go to sleep later at night, to have less regular sleep patterns, and to get fewer hours of sleep, which may contribute to the reduced nocturnal BP dipping (10) and elevated BP at night. Future studies could examine whether variability in sleep stages relates to both personality and BP dipping. This could be relevant because BP tends to rise during the rapid eye movement (REM) stage as compared to non-REM sleep. Other correlates of potential relevance could be the delta wave increase during sleep, renal function, and growth hormone secretion. In addition to physiological and sleep related patterns, the lifestyle of these individuals is likely to contribute to the observed reduced nocturnal BP fall. For example, there is strong evidence that individuals who score low on conscientiousness tend to be more sedentary (43), as also reflected by lower peak aerobic capacity (44), and engage in other behaviors with unfavorable health and social consequences (45, 46).
The analyses at the facet level indicate that almost all components of conscientiousness are linked to the dipping pattern. In contrast, for agreeableness the effect was all driven by trust. As the name indicates, this facet measures the tendency to believe that others are well-intentioned and honest (31). Those who score low on this trait are wary, assume the worse in others, and tend to be cynical and skeptical. These individuals may have a harder time to trust others, which may keep their BP from dipping at night. Among the facets that compose neuroticism, we found a reduced nocturnal BP dipping for those who are most impulsive. It is worth noting that impulsiveness is related to obesity, smoking, and a worse immune and metabolic profile (22, 46-48). Contrary to expectation, no significant association was found between the nocturnal BP dipping pattern and the traits depression and anxiety. Previous studies have examined concurrent emotional states (11, 12) more than trait dispositions and this may contribute to the different results.
The findings regarding neuroticism-related traits raise a broader issue. Cardiovascular research most often focuses on emotion-related states and traits such as anger, hostility, anxiety, and depression (14, 18). As discovered in this study, other traits are likely to be linked to cardiovascular health, with effects that might be even stronger. Most prominent in this and a growing number of studies is the role of conscientiousness. In addition to a non-dipping pattern, individuals with low levels of conscientiousness are likely to have other risk factors for cardiovascular health, including cigarette smoking and other substance use (23, 46), sedentary behavior (43), obesity (22, 49), inflammation (48, 50), dyslipidemia (51), and metabolic syndrome (24). In long-term prospective studies, low conscientiousness is also associated with a number of health outcomes (52, 53), such as Alzheimer's disease (25), and mortality (26, 54-56). Less is known about whether conscientiousness predicts cardiovascular events, such as stroke. However, prospective studies indicate that low conscientiousness is associated with increased risk for cardiovascular mortality (30, 54, 55). Given this pattern of associations, cardiovascular research should consider the domain of conscientiousness and its facets, along with the more traditional psychological risk factors.
This study had several strengths. We obtained a comprehensive assessment of the five-factor model of personality and 24-hour ABPM roughly seven years later to examine the association between psychological traits and circadian BP pattern. The sample is perhaps the largest to date to test such associations. Furthermore, the study provides data from a community-based sample, which complements data from clinical populations. The sample is also from a homogeneous population, which may reduce potential biases due to genetic admixture. Although the associations were robust and mostly consistent with a broader literature, the effect sizes were relatively modest. For any specific individual, knowing their personality profile can allow only weak predictions of their dipping status. However, these effects were based on long term prospective analyses and concurrent associations are possibly stronger. Besides eventual prognostic value, these results are informative on the broader links between personality traits, circadian patterns, and cardiovascular health. Among the limitations of this study was the lack of a diary or other tools to assess each individual's sleep/wake pattern. The lack of sleep logs is likely to increase noise in the analyses. To test the robustness of the reported associations, in supplementary analyses, we restricted the BP assessments to when most people are likely to be awake (9:00AM to 8:59PM) and asleep (1:00AM to 4:59 AM). With this more restricted time-frame, we found essentially the same associations, with conscientiousness (OR = 0.88, CI = 0.79-0.97) and agreeableness (OR = 0.90, CI = 0.81-1.00) predicting non-dipping BP. Another limitation is the possibility that we have missed important confounders, such as co-morbid conditions or social variables such as income (57). Given that multiple tests were performed, there is an increased risk of false positive results. Before reaching firm conclusions, these findings need to be replicated in independent samples. Furthermore, repeated measures of ABPM would be useful to test the robustness of the BP nocturnal dipping pattern and to test whether changes in dipping status are related to psychological traits. Because of the study's design and the typical high stability of personality traits (34), we framed this study with personality as predictor of dipping pattern. It is possible, however, that circadian variation in BP influences psychological traits and functioning.
In summary, this research suggests that personality dispositions are related to circadian patterns in BP and supports more research on how conscientiousness and other personality traits can help improve the lifestyle and cardiovascular risk profile of patients and the general population. Low conscientiousness is a key indicator of risky behaviors and lifestyles. In the clinical setting, assessing conscientiousness may help identify individuals at greater risk. Low conscientiousness may worsen cardiac prognosis and may be a barrier to treatment adherence. Indeed, conscientiousness predicts adherence to medical regimens (58), such as adherence to anti-hypertensive medication (59), cholesterol lowering treatment (60), and post-transplant medication adherence (61). Motivational interventions that deal with specific plans for treatment regimens may be particularly useful for individuals low in conscientiousness.
Abbreviations
- ABPM
ambulatory blood pressure monitoring
- BP
blood pressure
- BMI
body mass index
- MAP
mean arterial pressure
- NEO-PI-R
Revised NEO Personality Inventory
- REM
rapid eye movement
Footnotes
Conflicts of Interest and Source of Funding: This research was supported in part by the Intramural Research Program of the NIH, National Institute on Aging. The authors have no financial or other conflict of interests to declare.
References
- 1.Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. The New England journal of medicine. 2006;354:2368–74. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 2.Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–9. doi: 10.1097/00004872-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Pickering TG, Kario K. Nocturnal non-dipping: what does it augur? Current opinion in nephrology and hypertension. 2001;10:611–6. doi: 10.1097/00041552-200109000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Cuspidi C, Giudici V, Negri F, Sala C. Nocturnal nondipping and left ventricular hypertrophy in hypertension: an updated review. Expert review of cardiovascular therapy. 2010;8:781–92. doi: 10.1586/erc.10.29. [DOI] [PubMed] [Google Scholar]
- 5.Verdecchia P, Schillaci G, Gatteschi C, Zampi I, Battistelli M, Bartoccini C, Porcellati C. Blunted nocturnal fall in blood pressure in hypertensive women with future cardiovascular morbid events. Circulation. 1993;88:986–92. doi: 10.1161/01.cir.88.3.986. [DOI] [PubMed] [Google Scholar]
- 6.Fagard RH, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Night-day blood pressure ratio and dipping pattern as predictors of death and cardiovascular events in hypertension. Journal of human hypertension. 2009;23:645–53. doi: 10.1038/jhh.2009.9. [DOI] [PubMed] [Google Scholar]
- 7.Hermida RC, Ayala DE, Mojon A, Fernandez JR. Blunted Sleep-Time Relative Blood Pressure Decline Increases Cardiovascular Risk Independent of Blood Pressure Level-The “Normotensive Non-dipper” Paradox. Chronobiology international. 2012 doi: 10.3109/07420528.2012.701127. [DOI] [PubMed] [Google Scholar]
- 8.Matthews KA, Kamarck TW, HH M, Strollo PJ, Owens JF, Buysse DJ, Lee L, Reis SE. Blood pressure dipping and sleep disturbance in African-American and Caucasian men and women. American journal of hypertension. 2008;21:826–31. doi: 10.1038/ajh.2008.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Birkenhager AM, van den Meiracker AH. Causes and consequences of a non-dipping blood pressure profile. Neth J Med. 2007;65:127–31. [PubMed] [Google Scholar]
- 10.Sherwood A, Routledge FS, Wohlgemuth WK, Hinderliter AL, Kuhn CM, Blumenthal JA. Blood pressure dipping: ethnicity, sleep quality, and sympathetic nervous system activity. American journal of hypertension. 2011;24:982–8. doi: 10.1038/ajh.2011.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scuteri A, Spalletta G, Cangelosi M, Gianni W, Assisi A, Brancati AM, Modestino A, Caltagirone C, Volpe M. Decreased nocturnal systolic blood pressure fall in older subjects with depression. Aging clinical and experimental research. 2009;21:292–7. doi: 10.1007/BF03324918. [DOI] [PubMed] [Google Scholar]
- 12.Kayano H, Koba S, Matsui T, Fukuoka H, Toshida T, Sakai T, Akutsu Y, Tanno K, Geshi E, Kobayashi Y. Anxiety Disorder Is Associated With Nocturnal and Early Morning Hypertension With or Without Morning Surge - Ambulatory Blood Pressure Monitoring. Circ J. 2012;76:1670–7. doi: 10.1253/circj.cj-11-1085. [DOI] [PubMed] [Google Scholar]
- 13.Pavek K, Taube A. Personality characteristics influencing determinacy of day and night blood pressure and heart rate. Blood Pressure. 2009;18:30–5. doi: 10.1080/08037050902812648. [DOI] [PubMed] [Google Scholar]
- 14.Thomas KS, Nelesen RA, Dimsdale JE. Relationships between hostility, anger expression, and blood pressure dipping in an ethnically diverse sample. Psychosomatic medicine. 2004;66:298–304. doi: 10.1097/01.psy.0000126196.82317.9d. [DOI] [PubMed] [Google Scholar]
- 15.Sutin AR, Scuteri A, Lakatta EG, Tarasov KV, Ferrucci L, Costa PT, Jr, Schlessinger D, Uda M, Terracciano A. Trait antagonism and the progression of arterial thickening: women with antagonistic traits have similar carotid arterial thickness as men. Hypertension. 2010;56:617–22. doi: 10.1161/HYPERTENSIONAHA.110.155317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boyle SH, Michalek JE, Suarez EC. Covariation of psychological attributes and incident coronary heart disease in U.S. Air Force veterans of the Vietnam war. Psychosomatic medicine. 2006;68:844–50. doi: 10.1097/01.psy.0000240779.55022.ff. [DOI] [PubMed] [Google Scholar]
- 17.Roest AM, Martens EJ, Denollet J, de Jonge P. Prognostic association of anxiety post myocardial infarction with mortality and new cardiac events: a meta-analysis. Psychosomatic medicine. 2010;72:563–9. doi: 10.1097/PSY.0b013e3181dbff97. [DOI] [PubMed] [Google Scholar]
- 18.Albus C. Psychological and social factors in coronary heart disease. Ann Med. 2010;42:487–94. doi: 10.3109/07853890.2010.515605. [DOI] [PubMed] [Google Scholar]
- 19.Raikkonen K, Matthews KA, Flory JD, Owens JF, Gump BB. Effects of optimism, pessimism, and trait anxiety on ambulatory blood pressure and mood during everyday life. Journal of personality and social psychology. 1999;76:104–13. doi: 10.1037//0022-3514.76.1.104. [DOI] [PubMed] [Google Scholar]
- 20.Penninx BW, Beekman AT, Honig A, Deeg DJ, Schoevers RA, van Eijk JT, van Tilburg W. Depression and cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry. 2001;58:221–7. doi: 10.1001/archpsyc.58.3.221. [DOI] [PubMed] [Google Scholar]
- 21.Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, Houts R, Poulton R, Roberts BW, Ross S, Sears MR, Thomson WM, Caspi A. A gradient of childhood self-control predicts health, wealth, and public safety. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:2693–8. doi: 10.1073/pnas.1010076108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sutin AR, Ferrucci L, Zonderman AB, Terracciano A. Personality and obesity across the adult life span. Journal of personality and social psychology. 2011;101:579–92. doi: 10.1037/a0024286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turiano NA, Whiteman SD, Hampson SE, Roberts BW, Mroczek DK. Personality and substance use in midlife: Conscientiousness as a moderator and the effects of trait change. J Res Pers. 2012;46:295–305. doi: 10.1016/j.jrp.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sutin AR, Costa PT, Jr, Uda M, Ferrucci L, Schlessinger D, Terracciano A. Personality and metabolic syndrome. Age (Dordr) 2010;32:513–9. doi: 10.1007/s11357-010-9153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Terracciano A, Iacono D, O'Brien RJ, Troncoso JC, An Y, Sutin AR, Ferrucci L, Zonderman AB, Resnick SM. Personality and resilience to Alzheimer's disease neuropathology: a prospective autopsy study. Neurobiology of aging. 2013;34:1045–50. doi: 10.1016/j.neurobiolaging.2012.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson RS, Mendes de Leon CF, Bienias JL, Evans DA, Bennett DA. Personality and mortality in old age. The journals of gerontology Series B, Psychological sciences and social sciences. 2004;59:P110–6. doi: 10.1093/geronb/59.3.p110. [DOI] [PubMed] [Google Scholar]
- 27.Andersen SL, Sun JX, Sebastiani P, Huntly J, Gass JD, Feldman L, Bae H, Christiansen L, Perls TT. Personality Factors in the Long Life Family Study. The journals of gerontology Series B, Psychological sciences and social sciences. 2012 doi: 10.1093/geronb/gbs117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sutin AR, Zonderman AB, Uda M, Deiana B, Taub DD, Longo DL, Ferrucci L, Schlessinger D, Cucca F, Terracciano A. Personality traits and leptin. Psychosomatic medicine. 2013;75:505–9. doi: 10.1097/PSY.0b013e3182919ff4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benedict RH, Schwartz CE, Duberstein P, Healy B, Hoogs M, Bergsland N, Dwyer MG, Weinstock-Guttman B, Zivadinov R. Influence of personality on the relationship between gray matter volume and neuropsychiatric symptoms in multiple sclerosis. Psychosomatic medicine. 2013;75:253–61. doi: 10.1097/PSY.0b013e31828837cc. [DOI] [PubMed] [Google Scholar]
- 30.Jokela M, Pulkki-Raback L, Elovainio M, Kivimaki M. Personality traits as risk factors for stroke and coronary heart disease mortality: pooled analysis of three cohort studies. Journal of behavioral medicine. 2013 doi: 10.1007/s10865-013-9548-z. [DOI] [PubMed] [Google Scholar]
- 31.Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- 32.Pilia G, Chen WM, Scuteri A, Orrú M, Albai G, Dei M, Lai S, Usala L, Lai M, Loi P, Mameli C, Vacca L, Deiana M, Masala M, Cao A, Najjar SS, Terracciano A, Nedorezov T, Sharov A, Zonderman AB, Abecasis G, Costa PT, Lakatta E, Schlessinger D. Heritability of Cardiovascular and Personality Traits in 6,148 Sardinians. PloS Genetics. 2006;2:e132. doi: 10.1371/journal.pgen.0020132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poulain M, Pes GM, Grasland C, Carru C, Ferrucci L, Baggio G, Franceschi C, Deiana L. Identification of a geographic area characterized by extreme longevity in the Sardinia island: the AKEA study. Experimental gerontology. 2004;39:1423–9. doi: 10.1016/j.exger.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 34.Terracciano A, Costa PT, Jr, McCrae RR. Personality plasticity after age 30. Personality and Social Psychology Bulletin. 2006;32:999–1009. doi: 10.1177/0146167206288599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ivanovic BA, Tadic MV, Celic VP. To dip or not to dip? The unique relationship between different blood pressure patterns and cardiac function and structure. Journal of human hypertension. 2013;27:62–70. doi: 10.1038/jhh.2011.83. [DOI] [PubMed] [Google Scholar]
- 36.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker Boudier HAJ, Zanchetti A. 2007 Guidelines for the management of arterial hypertension - The task force for the management of arterial hypertension of the European society of hypertension (ESH) and of the European society of cardiology (ESC) Eur Heart J. 2007;28:1462–536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 37.Perneger TV. What's wrong with Bonferroni adjustments. BMJ. 1998;316:1236–8. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tonetti L, Fabbri M, Natale V. Relationship between Circadian Typology and Big Five Personality Domains. Chronobiology international. 2009;26:337–47. doi: 10.1080/07420520902750995. [DOI] [PubMed] [Google Scholar]
- 39.Hogben AL, Ellis J, Archer SN, von Schantzi M. Conscientiousness is a predictor of diurnal preference. Chronobiology international. 2007;24:1249–54. doi: 10.1080/07420520701791596. [DOI] [PubMed] [Google Scholar]
- 40.Walker RJ, Kribs ZD, Christopher AN, Shewach OR, Wieth MB. Age, the Big Five, and time-of-day preference: A mediational model. Pers Indiv Differ. 2014;56:170–4. [Google Scholar]
- 41.Raynor DA, Levine H. Associations Between the Five-Factor Model of Personality and Health Behaviors Among College Students. J Am Coll Health. 2009;58:73–81. doi: 10.3200/JACH.58.1.73-82. [DOI] [PubMed] [Google Scholar]
- 42.Williams PG, Moroz TL. Personality vulnerability to stress-related sleep disruption: Pathways to adverse mental and physical health outcomes. Pers Indiv Differ. 2009;46:598–603. [Google Scholar]
- 43.Rhodes RE, Smith NE. Personality correlates of physical activity: a review and meta-analysis. Br J Sports Med. 2006;40:958–65. doi: 10.1136/bjsm.2006.028860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Terracciano A, Schrack JA, Sutin AR, Chan W, Simonsick EM, Ferrucci L. Personality, metabolic rate and aerobic capacity. PloS one. 2013;8:e54746. doi: 10.1371/journal.pone.0054746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bogg T, Roberts BW. Conscientiousness and health-related behaviors: a meta-analysis of the leading behavioral contributors to mortality. Psychological bulletin. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- 46.Terracciano A, Lockenhoff CE, Crum RM, Bienvenu OJ, Costa PT., Jr Five-Factor Model personality profiles of drug users. BMC Psychiatry. 2008;8:22. doi: 10.1186/1471-244X-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sutin AR, Milaneschi Y, Cannas A, Ferrucci L, Uda M, Schlessinger D, Zonderman AB, Terracciano A. Impulsivity-related traits are associated with higher white blood cell counts. Journal of behavioral medicine. 2012;35:616–23. doi: 10.1007/s10865-011-9390-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sutin AR, Terracciano A, Deiana B, Naitza S, Ferrucci L, Uda M, Schlessinger D, Costa PT., Jr High Neuroticism and low Conscientiousness are associated with interleukin-6. Psychol Med. 2010;40:1485–93. doi: 10.1017/S0033291709992029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Terracciano A, Sutin AR, McCrae RR, Deiana B, Ferrucci L, Schlessinger D, Uda M, Costa PT., Jr Facets of personality linked to underweight and overweight. Psychosomatic medicine. 2009;71:682–9. doi: 10.1097/PSY.0b013e3181a2925b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mottus R, Luciano M, Starr JM, Pollard MC, Deary IJ. Personality traits and inflammation in men and women in their early 70s: the lothian birth cohort 1936 study of healthy aging. Psychosomatic medicine. 2013;75:11–9. doi: 10.1097/PSY.0b013e31827576cc. [DOI] [PubMed] [Google Scholar]
- 51.Sutin AR, Terracciano A, Deiana B, Uda M, Schlessinger D, Lakatta EG, Costa PT., Jr Cholesterol, triglycerides, and the Five-Factor Model of personality. Biological psychology. 2010;84:186–91. doi: 10.1016/j.biopsycho.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chapman BP, Roberts B, Lyness J, Duberstein P. Personality and Physician-Assessed Illness Burden in Older Primary Care Patients Over 4 Years. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2012 doi: 10.1016/j.jagp.2012.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sutin AR, Zonderman AB, Ferrucci L, Terracciano A. Personality Traits and Chronic Disease: Implications for Adult Personality Development. The journals of gerontology Series B, Psychological sciences and social sciences. 2013 doi: 10.1093/geronb/gbt036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hagger-Johnson G, Sabia S, Nabi H, Brunner E, Kivimaki M, Shipley M, Singh-Manoux A. Low conscientiousness and risk of all-cause, cardiovascular and cancer mortality over 17 years: Whitehall II cohort study. Journal of psychosomatic research. 2012;73:98–103. doi: 10.1016/j.jpsychores.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Terracciano A, Löckenhoff CE, Zonderman AB, Ferrucci L, Costa PT., Jr Personality predictors of longevity: Activity, emotional stability, and conscientiousness. Psychosomatic medicine. 2008;70:621–7. doi: 10.1097/PSY.0b013e31817b9371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kern ML, Friedman HS. Do conscientious individuals live longer? A quantitative review. Health Psychology. 2008;27:505–12. doi: 10.1037/0278-6133.27.5.505. [DOI] [PubMed] [Google Scholar]
- 57.Brummett BH, Babyak MA, Siegler IC, Shanahan M, Harris KM, Elder GH, Williams RB. Systolic blood pressure, socioeconomic status, and biobehavioral risk factors in a nationally representative US young adult sample. Hypertension. 2011;58:161–6. doi: 10.1161/HYPERTENSIONAHA.111.171272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Axelsson M, Brink E, Lundgren J, Lotvall J. The influence of personality traits on reported adherence to medication in individuals with chronic disease: an epidemiological study in West Sweden. PloS one. 2011;6:e18241. doi: 10.1371/journal.pone.0018241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Quine L, Steadman L, Thompson S, Rutter DR. Adherence to anti-hypertensive medication: proposing and testing a conceptual model. British journal of health psychology. 2012;17:202–19. doi: 10.1111/j.2044-8287.2011.02034.x. [DOI] [PubMed] [Google Scholar]
- 60.Stilley CS, Sereika S, Muldoon MF, Ryan CM, Dunbar-Jacob J. Psychological and cognitive function: predictors of adherence with cholesterol lowering treatment. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2004;27:117–24. doi: 10.1207/s15324796abm2702_6. [DOI] [PubMed] [Google Scholar]
- 61.Dobbels F, Vanhaecke J, Dupont L, Nevens F, Verleden G, Pirenne J, De Geest S. Pretransplant predictors of posttransplant adherence and clinical outcome: an evidence base for pretransplant psychosocial screening. Transplantation. 2009;87:1497–504. doi: 10.1097/TP.0b013e3181a440ae. [DOI] [PubMed] [Google Scholar]