Abstract
Objective
To assess racial/ethnic disparities in access to quality alcohol treatment services for risky drinking and alcohol problems in the United States, and to simulate strategies to narrow the gap.
Methods
Three-year longitudinal data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) were analyzed to examine the receipt of alcohol interventions in primary care and specialty treatment settings, consistent with published clinical guidelines. We compared US racial/ethnic minority and non-minority adults who were at-risk drinkers or had alcohol problems at baseline (N=9116). Simulation analyses projected how disparities in treatment services utilization might change if guidelines promoted care in more varied health and human service settings.
Results
Compared to whites, racial/ethnic minorities had two-thirds the odds of receiving an alcohol intervention over the three-year period (OR=0.62, 95%CI: 0.39–0.98). This disparity increased after adjusting for socioeconomic and clinical confounders (AOR=0.47, 95%CI: 0.28–0.80). The most pronounced disparities were observed among U.S.-born and foreign-born Hispanics (vs. whites). Simulation analyses suggested that these disparities could be partially mitigated by extending care to non-medical service venues.
Conclusions
Given limited capacity and barriers to using specialized addiction programs, current efforts to extend evidence-based alcohol interventions into medical settings address an important need. In doing so, however, racial/ethnic disparities in access to high-quality treatment are likely to increase. Partial solutions may be found in expanding the range and quality of alcohol-related services provided in alternative delivery sites, including faith-based and social service institutions.
INTRODUCTION
Although excessive alcohol consumption is the third leading cause of preventable death in the United States (1), only 11 percent of the 17.9 million Americans with an alcohol use disorder will receive treatment during any given year (2). Those that do will, on average, receive care 20 years following the onset of heavy drinking (3). There is thus a need for early intervention with the vast number of heavy drinkers in the general population at risk for severe alcohol problems, morbidity and mortality.
One reason for the large gap between those needing and receiving formal treatment is that very few people with an alcohol disorder think they should seek professional help (4). Another is that the demand for treatment far outstrips the supply. Even among the nation’s model addiction programs, patients are often wait-listed for 17–28 days (5, 6), and a long wait-list can result in a 50% drop-out rate before patients are even able to start treatment (7).
Both the lack of perceived need for treatment and the critical shortage of treatment slots are driving the current thrust of federal health policy to expand alcohol treatment beyond specialized settings and into mainstream medical care, particularly primary care (8–10). Backed by extensive data supporting the efficacy of primary care-based alcohol screening and brief intervention (11–15), the 2009 Patient Protection and Affordable Care Act (H.R. 3590 –111th Congress) includes provisions to integrate evidence-based alcohol intervention within patient-centered medical homes, and the 2008 Mental Health and Addiction Parity Act (H.R. 6983—110th Congress) requires that health plans cover alcohol treatment services at benefit levels commensurate with other medical services (16, 17). Further, private insurers, Medicaid and Medicare have developed billing codes that reimburse primary care providers for delivering alcohol interventions (18, 19).
While these efforts hold promise for reducing the alcohol-related health burden in the overall population, they also raise some question as to what impact this might have on existing disparities in alcohol problems. With the exception of some Asian American subgroups, US racial/ethnic minorities are at greater risk for alcohol dependence symptoms, negative drinking consequences and alcohol-related morbidity and mortality compared to whites (20–23). This might partly reflect racial disparities in substance use treatment access and utilization, but evidence of such disparities is modest, and even mixed (24–28).
There may be several reasons for this, one having to do with coercion into treatment. Racial/ethnic minorities are more likely than whites to be mandated to addiction treatment by the criminal justice system, and this can have the effect of reducing disparities in treatment use (29, 30). Another reason may be that treatment studies tend to focus only on the tip of the iceberg—people with severe and diagnosable alcohol problems who are likely to experience serious personal troubles because of their drinking, and to be pressured by spouses/partners, family and friends to seek help. Both can be strong motivators of treatment seeking (31, 32), and perhaps more so for racial/ethnic minorities who are more likely to experience tangible consequences due to their drinking. Finally, health insurance coverage appears to play a lesser role in determining use of addiction treatment than it does for other health-related services, possibly because specialty treatment is largely subsidized by public funding (33, 34).
Importantly, these mechanisms that increase access and use of specialized treatment by racial/ethnic minorities might not apply to alcohol services in medical settings. Indeed, minorities may be less likely to access evidence-based treatment in primary care because of the lack of health insurance (35). Also, because medically-based alcohol screening and brief intervention is largely intended for at-risk and non-dependent drinkers to prevent severe alcohol problems (8), legal coercion and social pressuring into these interventions seem less likely.
In our prior study it was observed that African Americans and Hispanics with risky drinking and alcohol use disorders were less likely to obtain primary care services than comparable whites (36) (Native Americans and Asians were excluded from those analyses due to small numbers). From this it followed that a national effort to expand treatment through evidence-based alcohol interventions in primary care could introduce sizeable racial differences in access to high-quality treatment services, and ultimately increase the burden of alcohol problems among minorities. The current study pursues this possibility further by examining disparities in the receipt of alcohol services. Here we conduct a stronger test of this hypothesis by using longitudinal data to model the actual receipt of an alcohol intervention from primary care and specialty programs over a three-year timeframe. We also examine how disparities in treatment receipt might be mitigated by expanding evidence-based alcohol intervention into alternative, non-medical venues such as churches, social services and family counseling agencies.
Methods
This analysis uses data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative, longitudinal survey of U.S. adults residing in household and non-institutional group quarters. Wave 1 data were collected in 2001–2 from 43,093 respondents, and Wave 2 data were collected from 34, 653 respondents in 2004–5, with a follow-up rate of 86.7% and a mean interval of roughly 3 years (36.6 months) between the two waves. The survey was administered through face-to-face, computer-assisted interviews. Approximately 16% of Hispanic respondents were interviewed in Spanish (37). (Additional information on the study’s design is provided by Grant and colleagues (38)). The current study analyzed data from the subset of respondents who met criteria for at-risk drinking or alcohol abuse at Wave 1 (N=9116). Alcohol dependent drinkers were excluded because the policy we focus on here—expanding treatment services by instituting alcohol screening and intervention in primary care—is not well-suited to treating dependent drinkers (8, 39). Given our concern with potential disparities in access to quality alcohol services, the analysis was restricted to non-dependent drinkers for whom these interventions have demonstrated effectiveness. The prospective, longitudinal design is an improvement over the more common approach of assessing lifetime treatment utilization, as the latter precludes assessment of temporal ordering and can mask long delays in obtaining treatment.
Following guidelines of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), at-risk drinkers were defined as men who consumed more than 4 drinks in a day or more than 14 drinks in a week, and women who consumed more than 3 drinks in a day or more than 7 drinks in a week during the 12 months prior to baseline (8). Alcohol abuse was defined as the presence of at least one of four diagnostic criteria during the 12 months prior to baseline, including hazardous alcohol use, social problems, legal problems, or failure to fulfill important roles due to one’s drinking (40), and was assessed using NIAAA’s Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV (AUDADIS-IV).
Measures
The key outcome was whether the respondent received an alcohol intervention during the 12 months prior to baseline and/or at any time during the three-year follow-up period. Our outcome measure was informed by NIAAA guidelines designed to promote best practices in screening, brief intervention, and referral to specialty treatment of people who are at-risk drinkers or have an alcohol use disorder (8). Respondents were coded as receiving an alcohol intervention if they received services for their drinking from a physician or mental health clinician (i.e., “a doctor, psychiatrist, psychologist, social worker”) or a specialty treatment program (detoxification, outpatient, inpatient, rehabilitation facility, or therapeutic community/halfway house), the two recommended sources of alcohol treatment services. Alcohol-related services received in alternative settings (i.e., Alcoholics Anonymous, family services/social service agency, emergency department, crisis center, employee assistance program, and from clergy) were also examined in separate analyses.
Racial/ethnic groups were categorized as non-Hispanic white, non-Hispanic black, foreign-born Hispanic, US-born Hispanic, Asian American/Pacific Islander, and Native American. Due to limited N, racial/ethnic minority groups were pooled in multivariate analyses. Selection of baseline covariates was informed by the extant literature and preliminary analyses indicating significant, bivariate associations with minority status and/or the key outcome. Final models adjusted for sex, age, education, income, health insurance, any prior lifetime alcohol treatment, and severity of need for alcohol intervention, including frequency of heavy drinking (defined as 5+/4+ drinks in a day for men/women) and negative consequences of drinking (interpersonal, legal, and/or role-related problems).
Analysis
Racial/ethnic group differences in demographic characteristics and severity of need at Wave 1 were assessed using chi-square tests and t-tests. To assess racial disparities in the receipt of an alcohol intervention, prospective analyses were conducted using logistic regression models adjusting for covariates. To assess whether expanding alcohol interventions into alternative service venues could potentially reduce racial disparities, logistic regression was used to estimate racial differences in services received from an expanded array of settings, including federally recommended clinical providers and specialty settings, as well as non-medical venues where study participants reported receiving alcohol counseling. STATA version 10 was used in all analyses to account for the complex survey design (41).
Results
Table 1 shows the characteristics of the sample of at-risk drinkers and persons with alcohol abuse. Racial/ethnic minorities constitute 23% of the overall sample, with African Americans comprising roughly one-third of the minority sample, and US-born and immigrant Hispanics each comprising one-fourth. Asian Pacific Islanders (APIs) and Native Americans each make up an additional 9%. Compared to whites, minorities were more likely to be male, younger, of lower socioeconomic status, and without health insurance. Minority respondents were also more likely than whites to drink heavily on a weekly basis or more often, and were two times more likely to experience negative drinking consequences.
Table 1.
Sample Characteristics (NESARC Wave 1, 2001–2)
| Variable | White (N=5,897)
|
Racial/ethnic minority (N=3,219)
|
F | df | p |
|---|---|---|---|---|---|
| Wtd. % | Wtd. % | ||||
| Demographics | |||||
| Racial/ethnic minority subgroup | n/a | n/a | |||
| African American | 32.1 | ||||
| US-born Hispanic | 25.1 | ||||
| Immigrant Hispanic | 25.1 | ||||
| Native American | 8.7 | ||||
| Asian/Pacific Islander | 8.9 | ||||
| Male | 58.1 | 66.2 | 32.7 | 1,65 | <.001 |
| Mean age ± SD | 39.9 ± .2 | 35.4 ± .3 | t = −11.6 | <.001 | |
| Education | 135.1 | 2.7,173.4 | <.001 | ||
| < HS grad | 6.9 | 25.5 | |||
| HS grad | 27.9 | 27.4 | |||
| Some college | 35.0 | 31.2 | |||
| College grad + | 30.2 | 15.9 | |||
| Income | 102.8 | 2.9,186.4 | <.001 | ||
| <20k | 15.4 | 31.1 | |||
| 20–40k | 23.8 | 30.1 | |||
| 40–60k | 20.2 | 17.7 | |||
| 60k+ | 40.6 | 21.1 | |||
| Health Insurance | 77.1 | 2.0,128.9 | <.001 | ||
| None | 16.4 | 32.3 | |||
| Public | 13.2 | 14.3 | |||
| Private | 70.4 | 53.4 | |||
| Severity of Need for Alcohol Intervention (at baseline) | |||||
| At-risk drinker | 97.2 | 96.2 | 5.09 | 1,65 | .027 |
| Alcohol abuse | 20.4 | 19.7 | .41 | 1,65 | .526 |
| Frequency of 5+/4+ drinks per day | 6.40 | 2.9,187.9 | <.001 | ||
| Never | 12.3 | 11.9 | |||
| Up to 11 time, past year | 41.3 | 35.9 | |||
| Monthly | 20.1 | 21.5 | |||
| Weekly or more | 26.3 | 30.7 | |||
| Negative consequences of drinking a | 3.0 | 6.3 | 34.8 | 1,65 | <.001 |
| Receipt of Alcohol Interventions | |||||
| Any lifetime alcohol intervention, prior to baseline b | 5.7 | 5.3 | .43 | 1,65 | .515 |
| Received alcohol intervention over the 3-year study period | 2.1 | 1.3 | 4.51 | 1,65 | .038 |
| Medically-based intervention only | 1.4 | 0.9 | 3.97 | 1,65 | .051 |
| Specialty treatment | 1.2 | 0.7 | 3.24 | 1,65 | .077 |
Note. df: design-based degrees of freedom
Negative consequences of drinking include the subset of alcohol abuse symptoms that relate to actual problems experienced due to drinking (interpersonal or legal problems, failure to fulfill roles and obligations). Hazardous drinking is excluded.
Includes specialty, medical, and non-medical providers
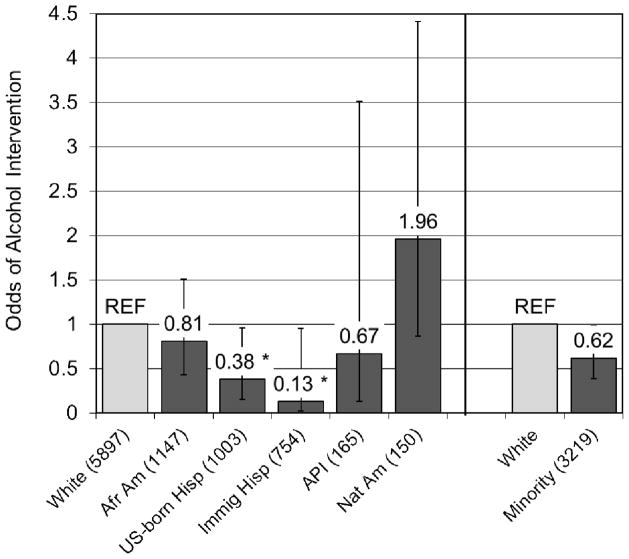
Despite indications of greater need for alcohol services, racial/ethnic minorities as a group were less likely to receive an alcohol intervention during the study period (see Table 1). Compared to whites, they had less than two-thirds the odds of receiving care (OR= 0.62, p<.05) (see Figure 1). African Americans and Asian/Pacific Islanders (APIs) both had lower odds relative to whites, although these were not statistically significant, and striking disparities were seen between Hispanics and whites (ORs = 0.38 and 0.13 for US-born and foreign-born Hispanics, respectively, p<.05). By contrast, Native Americans had nearly two times the odds of receiving an alcohol intervention compared to whites (OR=1.96), but this was non-significant due to their small numbers.
Figure 1. Racial/ethnic differences in the odds of receiving an alcohol intervention over 3 years (Reference group: white).
Note. Unweighted N shown in parentheses. * p <.05
Table 2 shows minority-white differences in the odds of receiving an alcohol intervention. In all cases, the minority-white disparity not only persisted but increased when we took into account group differences in demographic characteristics, severity of need for treatment, and prior treatment history (adjusted ORs ranged from 0.43 to 0.52, all p’s<.01).
Table 2.
Racial/ethnic disparities in the odds of receiving an alcohol intervention over 3 years
| Model | Racial/ethnic minority vs. white
|
||
|---|---|---|---|
| OR | 95% CI | p | |
| Unadjusted | .62 | .39 – .98 | .039 |
| Model 1a | .46 | .28 – .76 | .003 |
| Model 2b | .47 | .28 – .77 | .003 |
| Model 3c | .43 | .26 – .72 | .002 |
| Model 4d | .52 | .32 – .85 | .009 |
| Model 5e | .48 | .28 – .81 | .006 |
Base model: adjusted for sex, age, education, income, health insurance
Base model also adjusted for weekly 5+/4+ drinking
Base model also adjusted for negative consequences of drinking
Base model also adjusted for prior receipt of any alcohol treatment services
Fully adjusted model: adjusts for sex, age, education, income, health insurance, severity of need (weekly 5+/4+ drinking and negative drinking consequences), and any prior alcohol treatment
Alternative Venues for Alcohol Intervention
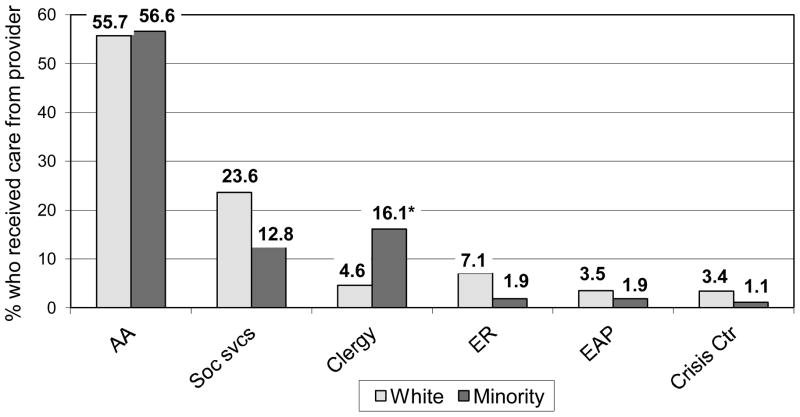
Given these disparities in services utilization, an important question for policymakers is whether evidence-based alcohol interventions should be extended beyond primary care to alternative settings, and whether doing so might help to reduce these disparities. Figure 2 shows alternative providers of alcohol counseling. Not surprisingly, Alcoholics Anonymous (AA) was by far the most commonly reported venue among white and minority drinkers. But because AA serves persons with severe alcohol problems who are already trying to become clean and sober, it is more appropriate as a complement to primary care-based intervention and specialty treatment rather than as an alternative site for screening and brief intervention (42, 43). Social service programs and clergy were the next most common sources of alcohol counseling. Racial/ethnic minorities were four times more likely than whites to receive alcohol counseling from clergy (16.1% vs 4.6%, p<.05). Additionally, 1–2% of minorities and 3–7% of whites received counseling from each of the following three sources: emergency departments, employee assistance programs, and crisis centers.
Figure 2. Non-medical providers of alcohol counseling received by at-risk drinkers and persons with alcohol abuse who used any alcohol services over 3 years.
Note. AA, Alcoholics Anonymous or other 12-step program; ER, Emergency Room; EAP, Employee Assistance Program
* p <.05
Table 3 presents the results of our analysis simulating the effects of expanding evidence-based alcohol intervention into these alternative settings (other than AA). While the estimated disparity in the receipt of an alcohol intervention changed very little for most groups, there was a 39% reduction in the disparity between US-born Hispanics and whites, from AOR=0.38 (0.15–0.96) to AOR=0.53 (0.26–1.09). U.S.-born Hispanics still have lower odds of obtaining care than whites, but the difference is no longer statistically significant.
Table 3.
Simulation: Estimated racial disparities in the receipt of an alcohol intervention when non-medical providers are included
| Racial/ethnic group (referent: white) | Currently recommended: Medical providers and specialty treatment
|
Hypothetical expansion to include non-medical providers a
|
Change in OR b | ||
|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | ||
| African American | .81 | .44 – 1.51 | .79 | .44 – 1.43 | 2.5% |
| US-born Hispanic | .38 | .15 – .96 * | .53 | .26 – 1.09 | −39% |
| Immigrant Hispanic | .13 | .02 – .95 * | .15 | .03 – .69 * | −15% |
| Asian/Pac Islander | .67 | .13 – 3.51 | .57 | .11 – 2.97 | 15% |
| Native American | 1.96 | .87 – 4.41 | 1.83 | .86 – 3.88 | 6.6% |
| Minority overall | .62 | .39 – .98 * | .63 | .43 – .93 * | −1.6% |
These include currently recommended providers (physicians, mental health clinicians and specialty treatment settings) and venues such as social services, clergy, ERs, Employee Assistance programs, and crisis centers
Calculated as (ORhyp − ORrec)/ORrec
p<.05
Discussion
In this study we considered what the widespread provision of evidence-based alcohol intervention in medical settings, especially primary care, might mean for racial/ethnic disparities in access to high-quality alcohol services. Results show that over a three-year period, racial/ethnic minorities as a group had roughly half the odds of receiving an alcohol intervention from primary care providers and/or specialty treatment programs compared to whites. This suggests that federal efforts to promote routine alcohol screening and intervention in primary care might not benefit racial/ethnic groups equally. Indeed, such efforts could have the unintended consequence of increasing disparities in access to quality treatment and, ultimately, exacerbating disparities in alcohol problems.
The most striking disparity was observed between whites and US- and foreign-born Hispanics, consistent with the results of our previous study based on the US National Alcohol Survey indicating that Hispanic at-risk and problem drinkers were far less likely to obtain primary care (36). Notably, Hispanics have some of the highest rates of heavy drinking and alcohol dependence, and low rates of dependence remission (44–47). Ensuring that they have access to high-quality early intervention is therefore important, especially for US-born Hispanics whose rates of alcohol disorder significantly exceed those of immigrant Hispanics (37, 48, 49).
While most efforts have focused on providing alcohol services in primary care settings, there is growing interest in a wider range of venues ranging from hospital emergency departments and hospital wards, to the criminal justice system and college settings (50). Our study results highlight the need to consider still other settings. Specifically, when our simulation analysis redefined the study outcome as the receipt of an alcohol intervention in primary care, specialty treatment or non-medical service setting, the disparity between US-born Hispanics and whites was reduced and no longer statistically significant.
Special consideration should be given to the role that social and family service agencies and clergy or faith-based organizations might play in promoting, linking and providing evidence-based alcohol interventions to minority communities, as these were common sources of alcohol counseling among minorities. Faith-based organizations have a long history of serving disadvantaged communities (51, 52), and churches have become increasingly involved in health promotion and intervention in African American and Latino communities (53). Their commitment to improving the welfare of their communities, and the trust and respect with which faith-based institutions are often held (54), may be critical to linking underserved minority populations with high-quality alcohol interventions.
Reaching Hispanic immigrants might require special efforts in light of the formidable barriers they face, including lack of health insurance, fear of mistreatment, limited English proficiency and logistical issues related to transportation and child care (55–59). Some health and social service agencies have successfully partnered with local bicultural and bilingual organizations to engage Hispanic immigrants in mental and physical health programs. This has been achieved partly through community building, enrichment and social support activities that appeal to broader individual and family interests (60). Of note, the involvement of local, volunteer promotoras de salud has been vital to such efforts to increase services utilization by these communities.
Several study limitations should be considered when interpreting the results presented here. First, the very low rates of treatment utilization during the study period, combined with relatively small samples of racial/ethnic minority subgroups, required that we pool minority groups in multivariate analyses. Such sample size issues are common to racial disparities research focused on treatment utilization and often motivate analyses of lifetime treatment use, which are associated with a different set of limitations as noted earlier. Another limitation was the lack of data on the respondent’s primary language and language of interview, which precluded analysis of Hispanic subgroup differences by language. Spanish-speaking Hispanics are far less likely than English-speaking Hispanics to access health care services generally (61). Interestingly, a recent study found that Spanish language/Hispanic social group preference predicted lower mental health services use, but was unrelated to alcohol or drug treatment utilization (62). Third, the NESARC does not distinguish among primary care providers, in particular community health centers which are a key source of health care for low-income, and uninsured and underinsured racial/ethnic minority populations (63). To the extent that evidence-based alcohol screening and intervention is integrated into routine care at community health clinics, these settings hold promise for mitigating disparities in treatment access and quality. Funding provided to federally qualified community health centers through the Affordable Care Act (ACA) might be instrumental in this regard (64). Further, increased insurance coverage under the ACA might also reduce disparities in access to medically-based alcohol intervention. Yet this might depend upon the presence of community health centers and their implementation of quality alcohol interventions. Even among persons with health insurance, racial disparities in the use of substance use treatment and other mental health services have been significant given the absence of a neighborhood health clinic (65). Finally, as noted earlier, the present analysis included persons with diagnosable alcohol abuse but excluded those with dependence, as primary care-based alcohol intervention appears less effective for the latter group. With the change to the DSM-5, alcohol abuse and dependence will no longer be distinguished and thus it is unclear how our study findings will translate. But if lower utilization among minorities is fundamentally related to logistical, attitudinal, and social barriers to primary care, it seems likely that racial disparities will persist.
CONCLUSIONS
It has recently been recognized that well-intentioned public health interventions might not benefit all segments of the general population, partly due to differential access to knowledge and health services (66–69). To offset the risk of unintended health disparities, policymakers must carefully consider whether innovations to improve health can be developed and disseminated in ways that increase, rather than detract from, health equity (70). The present study suggests that widespread implementation of evidence-based alcohol screening and intervention in primary care settings is another example of an innovation that can improve overall population health while also, potentially, exacerbating alcohol-related disparities. Efforts to adapt, link and disseminate these “state of the art” alcohol interventions to alternative, non-medical service settings, particularly those utilized by Hispanics, may be thus warranted.
Acknowledgments
This study was supported by funding from the National Institute on Alcohol Abuse and Alcoholism (grants R01 AA017197 and P50AA005595). An earlier version of this paper was presented at the 2012 Science on Eliminating Health Disparities Summit, National Institutes of Health, December 17–19, National Harbor, MD.
References
- 1.Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the United States, 2000. The Journal of the American Medical Association. 2004;291:1238–45. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Clark HW, Power AK, LeFauve CE, et al. Policy and practice implications of epidemiological surveys on co-occurring mental and substance use disorders. Journal of Substance Abuse Treatment. 2008;34:3–13. doi: 10.1016/j.jsat.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration, Center for Behavior Health Statistics and Quality. The TEDS Report: length of time from first use to adult treatment admission. Rockville, Md: 2011. [Google Scholar]
- 4.Edlund MJ, Booth BM, Feldman ZL. Perceived need for treatment for alcohol use disorders: results from two national surveys. Psychiatric Services. 2009;60:1618–28. doi: 10.1176/appi.ps.60.12.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCarty D, Gustafson DH, Wisdom JP, et al. The Network for the Improvement of Addiction Treatment (NIATx): enhancing access and retention. Drug and Alcohol Dependence. 2007;88:138–45. doi: 10.1016/j.drugalcdep.2006.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffman KA, Ford JH, II, Choi D, et al. Replication and sustainability of improved access and retention within the Network for the Improvement of Addiction Treatment. Drug and Alcohol Dependence. 2008;98:63–9. doi: 10.1016/j.drugalcdep.2008.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCarty D, McConnell KJ, Schmidt LA. Policies for the Treatment of Alcohol and Drug Use Disorders: a research agenda for 2010–2015. Greensboro, NC: Substance Abuse Policy Research Program (SAPRP), Robert Wood Johnson Foundation; [[Accessed: 2012-08-17]. 2009. Archived by WebCite® at http://www.webcitation.org/69zNUAUoi] [Google Scholar]
- 8.National Institute on Alcohol Abuse and Alcoholism. Rockville, Md: National Institute on Alcohol Abuse and Alcoholism; [accessed 12/11/09]. 2005. Helping patients who drink too much: a clinician’s guide. Updated 2005 Edition (NIH Publication No. 07-3769) [ http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. NIH Publication No. 07-3769. [Google Scholar]
- 9.Institute of Medicine. Broadening the Base of Treatment for Alcohol Problems. Washington, DC: National Academy Press; 1990. [PubMed] [Google Scholar]
- 10.McCarty D, Gustafson D, Capoccia VA, et al. Improving care for the treatment of alcohol and drug disorders. The Journal of Behavioral and Health Services and Research. 2009;36:52–60. doi: 10.1007/s11414-008-9108-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whitlock EP, Polen MR, Green CA, et al. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2004;140:557–68. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- 12.Ballesteros J, González-Pinto A, Querejeta I, et al. Brief interventions for hazardous drinkers delivered in pimary care are equally effective in men and women. Addiction. 2004;99:103–8. doi: 10.1111/j.1360-0443.2004.00499.x. [DOI] [PubMed] [Google Scholar]
- 13.Ballesteros J, Duffy JC, Querejeta I, et al. Efficacy of brief intervention for hazardous drinkers in primary care: systematic review and meta-analysis. Alcoholism: Clinical and Experimental Research. 2004;28:608–18. doi: 10.1097/01.alc.0000122106.84718.67. [DOI] [PubMed] [Google Scholar]
- 14.Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare healthcare sites: comparison at intake and 6 months later. Drug and Alcohol Dependence. 2009;99:280–95. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization Brief Intervention Study Group. A cross-national trial of brief interventions with heavy drinkers. American Journal of Public Health. 1996;86:948–55. doi: 10.2105/ajph.86.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Substance Abuse and Mental Health Services Administration. Overview of the affordable care act: what are the implications for behavioral health? [Accessed: 2012-08-16];SAMHSA News. 2010 18(3) Archived by WebCite® at http://www.webcitation.org/69y5LtLwy] [Google Scholar]
- 17.Substance Abuse and Mental Health Services Administration. Mental Health Parity and Addiction Equity Act. Rockville, MD: [Accessed: 2012-08-16]. 2011. Archived by WebCite® at http://www.webcitation.org/69y45E48Y] [Google Scholar]
- 18.Substance Abuse and Mental Health Services Administration. Screening, Brief Intervention, and Referral to Treatment (SBIRT) Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment; [Accessed: 2011-08-09]. 2011. Archived by WebCite® at http://www.webcitation.org/60ovK0sCj] [Google Scholar]
- 19.Substance Abuse and Mental Health Services Administration. Coding for SBI Reimbursement. Rockville, Md: Substance Abuse and Mental Health Services Administration; [accessed 08/8/13]. 2012. [ http://www.samhsa.gov/prevention/sbirt/coding.aspx. [Google Scholar]
- 20.Jones-Webb RJ, Hsiao C-Y, Hannan P, et al. Predictors of increases in alcohol-related problems among black and white adults: results from the 1984 and 1992 National Alcohol Surveys. American Journal of Alcohol and Drug Abuse. 1997;23:281–99. doi: 10.3109/00952999709040947. [DOI] [PubMed] [Google Scholar]
- 21.Mulia N, Ye Y, Greenfield TK, et al. Disparities in alcohol-related problems among white, black, and Hispanic Americans. Alcoholism: Clinical and Experimental Research. 2009;33:654–62. doi: 10.1111/j.1530-0277.2008.00880.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hilton J. Race and Ethnicity in Fatal Motor Vehicle Traffic Crashes 1999-2004. Washington, DC: National Center for Statistics and Analysis, National Highway Traffic and Safety Administration, U.S. Department of Transportation; [accessed 07/30/2010]. 2006. [ http://www-nrd.nhtsa.dot.gov/Pubs/809956.PDF. [Google Scholar]
- 23.Yoon Y-H, Yi H-Y. Liver Cirrhosis Mortality in the United States, 1970–2004 Surveillance Report #79. Arlington, VA: National Institue on Alcohol Abuse and Alcoholism; 2007. [Google Scholar]
- 24.Mojtabai R. Use of specialty substance abuse and mental health services in adults with substance use disorders in the community. Drug and Alcohol Dependence. 2005;78:345–54. doi: 10.1016/j.drugalcdep.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 25.Hatzenbuehler ML, Keyes KM, Narrow WE, et al. Racial/ethnic disparities in service utilization for individuals with co-occurring mental health and substance disorders in the general population: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69:1112–21. doi: 10.4088/jcp.v69n0711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keyes KM, Hatzenbuehler ML, Alberti P, et al. Service utilization difference for axis I psychiatric and substance use disorders between white and black adults. Psychiatric Services. 2008;59:893–901. doi: 10.1176/appi.ps.59.8.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmidt LA, Ye Y, Greenfield TK, et al. Ethnic disparities in clinical severity and services for alcohol problems: results from the National Alcohol Survey. Alcoholism: Clinical and Experimental Research. 2007;31:48–56. doi: 10.1111/j.1530-0277.2006.00263.x. [DOI] [PubMed] [Google Scholar]
- 28.Chartier KG, Caetano R. Trends in alcohol services utilization from 1991–1992 to 2001–2002: ethnic group differences in the U.S. population. Alcoholism: Clinical and Experimental Research. 2011;35:1485–97. doi: 10.1111/j.1530-0277.2011.01485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polcin DL, Beattie M. Relationship and institutional pressure to enter treatment: differences by demographics, problem severity, and motivation. Journal of Studies on Alcohol and Drugs. 2007;68:428–36. doi: 10.15288/jsad.2007.68.428. [DOI] [PubMed] [Google Scholar]
- 30.Cook BL, Alegría M. Racial-ethnic disparities in substance abuse treatment: the role of criminal history and socioeconomic status. Psychiatric Services. 2011;62:1273–81. doi: 10.1176/appi.ps.62.11.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Matzger H, Kaskutas LA, Weisner C. Reasons for drinking less and their relationship to sustained remission from problem drinking. Addiction. 2005;100:1637–46. doi: 10.1111/j.1360-0443.2005.01203.x. [DOI] [PubMed] [Google Scholar]
- 32.Room R, Matzger H, Weisner C. Sources of informal pressure on problematic drinkers to cut down or seek treatment. Journal of Substance Use. 2004;9:280–95. [Google Scholar]
- 33.Schmidt L, Greenfield TK, Mulia N. Unequal treatment: racial and ethnic disparities in alcoholism treatment services. Alcohol Research and Health. 2006;29:49–54. [PMC free article] [PubMed] [Google Scholar]
- 34.Weisner C, Matzger H, Tam TW, et al. Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. Journal of Studies on Alcohol. 2002;63:673–82. doi: 10.15288/jsa.2002.63.673. [DOI] [PubMed] [Google Scholar]
- 35.Schmidt L, Mäkelä P, Rehm J, et al. In: Alcohol: equity and social determinants; in Equity, Social Determinants and Public Health Programmes. Blas E, Kurup AS, editors. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 36.Mulia N, Schmidt LA, Ye Y, et al. Preventing disparities in alcohol screening and brief intervention: the need to move beyond primary care. Alcoholism: Clinical and Experimental Research. 2011;35:1557–60. doi: 10.1111/j.1530-0277.2011.01501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grant BF, Stinson FS, Hasin DS, et al. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:1226–33. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- 38.Grant BF, Goldstein RB, Chou SP, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Molecular Psychiatry. 2009;14:1051–66. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saitz R. Alcohol screening and brief intervention in primary care: absence of evidence for efficacy in people with dependence very heavy drinking. Drug and Alcohol Review. 2010;29:631–40. doi: 10.1111/j.1465-3362.2010.00217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 41.Stata Corporation. Stata Statistical Software: release 10.0. College Station, TX: Stata Corporation; 2007. [Google Scholar]
- 42.National Institute on Alcohol Abuse and Alcoholism. Helping Patients Who Drink Too Much. A clinician’s guide. Rockville, Md: National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health; 2005. [Google Scholar]
- 43.Willenbring ML. The past and future of research on treatment of alcohol dependence. Alcohol Research and Health. 2010;33:55–63. [PMC free article] [PubMed] [Google Scholar]
- 44.Chartier K, Caetano R. Ethnicity and health disparities in alcohol research. Alcohol Research and Health. 2010;33:152–60. [PMC free article] [PubMed] [Google Scholar]
- 45.Smith SM, Stinson FS, Dawson DA, et al. Race/ethnic differences in the prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36:987–98. doi: 10.1017/S0033291706007690. [DOI] [PubMed] [Google Scholar]
- 46.Dawson DA, Grant BF, Stinson FS, et al. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–92. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- 47.Grant JD, Vergés A, Jackson KM, et al. Age and ethnic differences in the onset, persistence and recurrence of alcohol use disorder. Addiction. 2011;107:756–65. doi: 10.1111/j.1360-0443.2011.03721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Burnam MA, Hough RL, Karno M, et al. Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. Journal of Health and Social Behavior. 1987;28:89–102. [PubMed] [Google Scholar]
- 49.Alegría M, Canino GJ, Stinson FS, et al. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and Non-Latino Whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67:56–65. doi: 10.4088/jcp.v67n0109. [DOI] [PubMed] [Google Scholar]
- 50.National Institute on Alcohol Abuse and Alcoholism. Brief interventions. Alcohol Alert. 2005;66:1–8. [Google Scholar]
- 51.Asomugha CN, Derose KP, Lurie N. Faith-based organizations, science, and the pursuit of health. Journal of Health Care for the Poor and Underserved. 2011;22:50–5. doi: 10.1353/hpu.2011.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Newlin K, Dyess SM, Allard E, et al. A methodological review of faith-based health promotion literature: advancing the science to expand delivery of diabetes education to black Americans. Journal of Religion and Health. 2012;51:1075–97. doi: 10.1007/s10943-011-9481-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.DeHaven MJ, Hunter IB, Wilder L, et al. Health programs in faith-based organisations: are they effective? American Journal of Public Health. 2004;94:1030–1036. doi: 10.2105/ajph.94.6.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nordtvedt M, Chapman LS. Health promotion in faith-based institutions and communities. American Journal of Health Promotion. 2011;25:TAHP1-12. doi: 10.4278/ajhp.25.4.tahp. [DOI] [PubMed] [Google Scholar]
- 55.Harari N, Davis M, Heisler M. Strangers in a strange land: health care experiences for recent Latino immigrants in Midwest communities. Journal of Health Care for the Poor and Underserved. 2008;19:1350–67. doi: 10.1353/hpu.0.0086. [DOI] [PubMed] [Google Scholar]
- 56.Betancourt JR, Green AR, Carrillo JE, et al. Barriers to health promotion and disease prevention in the Latino population. Clinical Cornerstone. 2004;6:16–29. doi: 10.1016/s1098-3597(04)80061-9. [DOI] [PubMed] [Google Scholar]
- 57.Bopp M, Fallon EA, Marquez DX. A faith-based physical activity intervention for Latinos: outcomes and lessons. American Journal of Health Promotion. 2011;25:168–71. doi: 10.4278/ajhp.090413-ARB-138. [DOI] [PubMed] [Google Scholar]
- 58.DeCamp LR, Choi H, Davis MM. Medical home disparities for Latino children by parental language of interview. Journal of Health Care for the Poor and Underserved. 2011;22:1151–66. doi: 10.1353/hpu.2011.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pacheco TL, Ramirez MA, Capitman JA. Policy barriers to health care access fuel discriminatory treatment: the role of Promotoras in overcoming malos tratos. Journal of Ambulatory Care Management. 2012;35:2–14. doi: 10.1097/JAC.0b013e31822c8d66. [DOI] [PubMed] [Google Scholar]
- 60.Glasnapp JD. Promising Practices in Mental Health Care Programs: A Look at The California Endowment’s Agricultural Worker Health Program Request for Proposal G,antees. Los Angeles, CA: The California Endowment; [Accessed: 2013-04-29]. 2004. Archived by WebCite® at http://www.webcitation.org/6GFMMfoD7. [Google Scholar]
- 61.Doty MM. Hispanic Patients’ Double Burden: Lack of Health Insurance and Limited English. New York: The Commonwealth Fund; 2003. [Google Scholar]
- 62.Keyes KM, Martins SS, Hatzenbuehler ML, et al. Mental health service utilization for psychiatric disorders among Latinos living in the United States: the role of ethnic subgroup, ethnic identity, and language/social preference. Social Psychiatry and Psychiatric Epidemiology. 2012;47:383–94. doi: 10.1007/s00127-010-0323-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Doty MM, Abrams MK, Hernandez SE, et al. Enhancing the Capacity of Community Health Centers to Achieve High Performance: Findings from the 2009 Commonwealth Fund National Survey of Federally Qualified Health Centers. New York: The Commonwealth Fund; [Accessed: 2013-04-29]. 2010. Archived by WebCite® at http://www.webcitation.org/6GFGg5jx1. [Google Scholar]
- 64.Shim RS, Koplan C, Langheim FJP, et al. Health care reform and integrated care: a golden opportunity for preventive psychiatry. Psychiatric Services. 2012;63:1231–33. doi: 10.1176/appi.ps.201200072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Alegría M, Lin J, Chen C-N, et al. The impact of insurance coverage in diminishing racial and ethnic disparities in behavioral health services. Health Services Research. 2013;47:1322–44. doi: 10.1111/j.1475-6773.2012.01403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Link BG. Epidemiological sociology and the social shaping of population health. Journal of Health and Social Behavior. 2008;49:367–84. doi: 10.1177/002214650804900401. [DOI] [PubMed] [Google Scholar]
- 67.Frohlich KL, Potvin L. The inequality paradox: the population approach and vulnerable populations. American Journal of Public Health. 2008;98:216–21. doi: 10.2105/AJPH.2007.114777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Capewell S, Graham H. Will cardiovascular disease prevention widen health inequalities? PLoS Medicine. 2010;7:e1000320. doi: 10.1371/journal.pmed.1000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lorenc T, Petticrew M, Welch V, et al. What types of interventions generate inequalities? evidence from systematic reviews. Journal of Epidemiology and Community Health. 2013;67:190–3. doi: 10.1136/jech-2012-201257. [DOI] [PubMed] [Google Scholar]
- 70.Korda RJ, Clements MS, Dixon J. Socioeconomic inequalities in the diffusion of health technology: uptake of coronary procedures as an example. Social Science and Medicine. 2011;72:224–9. doi: 10.1016/j.socscimed.2010.11.002. [DOI] [PubMed] [Google Scholar]