Abstract
Systemic administration of human umbilical cord blood (HUCB) mononuclear cells (MNC) following middle cerebral artery occlusion (MCAO) in the rat reduces infarct size and, more importantly, restores motor function. The HUCB cell preparation is composed of immature T-cells, B-cells, monocytes and stem cells. In this study we examined whether the beneficial effects of HUCB injection were attributable to one of these cell types. Male Sprague Dawley rats underwent permanent MCAO followed 48 hours later by intravenous administration of HUCB MNC preparations depleted of either CD14+ monocytes, CD133+ stem cells, CD2+ T-cells or CD19+ B cells. Motor function was measured prior to MCAO and 30 days post-stroke. When CD14+ monocytes were depleted from the HUCB MNC, activity and motor asymmetry were similar to the MCAO only treated animals. Monocyte depletion prevented HUCB cell treatment from reducing infarct size while monocyte enrichment was sufficient to reduce infarct size. Administration of monocyte-depleted HUCB cells did not suppress Iba1 labeling of microglia in the infarcted area relative to treatment with the whole HUCB preparation. These data demonstrate that the HUCB monocytes provide the majority of the efficacy in reducing infarct volume and promoting functional recovery.
Keywords: cord blood, cerebral ischemia, monocytes, behavior, infarct, microglia
INTRODUCTION
Despite great progress in the prevention, diagnosis and understanding of the pathophysiological mechanisms of stroke, it is the fourth leading cause of death and the leading cause of disability worldwide (Roger et al., 2011). Still, our advancement toward developing new therapeutic agents has been limited. Currently, only the thrombolytic agent, tissue plasminogen activator (TPA), is approved by the U.S. Food and Drug Administration (FDA) for the acute (urgent) treatment of ischemic stroke, which accounts for 85% of all strokes. TPA is only effective within 4.5 hours of the onset of stroke and resolves ischemia by dissolving the clot. With this narrow therapeutic window, only 2–3% of all stroke patients are able to benefit from the use of TPA.
Cell therapy has garnered attention over the last 20 years, and could substantially expand the treatment window. The earliest studies used fetal tissue to examine the ability of transplanted cells to repair stroke-damaged brain by replacing the dead neurons (Mampalam et al., 1988; Tonder et al., 1989). The first cell therapy to reach clinical trials for a treatment of lacunar ischemic strokes was the hNT or LBS Neurons, a cell-line developed from a teratocarcinoma (Kondziolka et al., 2000). Since that time much of the focus has been on stem cell therapies encompassing embryonic, neural (and other somatic stem cells), and, more recently, induced pluripotent stem cells (see (Sladek and Bjugstad, 2011) for a recent commentary). Our understanding of the repair mechanisms that underlie the therapeutic benefits associated with cell therapy have evolved from simple neural repair to include trophic support (Kern et al., 2011), inhibition of inflammation (Yang et al., 2010), as well as stimulation of angiogenesis and endogenous neurogenesis (Taguchi et al., 2004).
The first published report of HUCB MNC intravenous administration as a treatment for experimental stroke was Chen and associates (Chen et al., 2001). They found that delivering 3 × 106 cells 24 hr post-MCAO significantly improved motor function, as determined with the modified neurological severity score (mNSS) and rotorod tests, while having little effect on infarct size. Since that time there have been a number of reports demonstrating that HUCB cells can repair damaged brain in rodent models of cerebral hypoxia and ischemia. We found that systemic administration of these cells significantly decreases infarct size, and reduces the pro-inflammatory cells and cytokines associated with stroke (Hall et al., 2009; Jiang et al., 2010; Leonardo et al., 2010; Vendrame et al., 2005). Systemic administration is the preferable route, producing more sustained behavioral improvements compared to direct intraparenchymal administration (Willing et al., 2003). This was confirmed by another research group that showed that HUCB cells do not have to enter the CNS to produce their reparative effects (Borlongan et al., 2004). When delivered systemically at 48 hours following MCAO these cells have their optimal effect on decreasing infarct volume and enhancing behavioral recovery (Newcomb et al., 2006; Vendrame et al., 2004). This work has been replicated by other research groups (Boltze et al., 2006; Boltze et al., 2011). Other studies have focused on CD34+ hematopoietic stem cells from HUCB as the active cell type (Boltze et al., 2008; Liu et al., 2006; Taguchi et al., 2004), although both CD34+ and CD34− HUCB cells had similar behavioral effects, but neither were as good as MNC (Boltze et al., 2012). Still others have focused on developing HUCB derived neural cell lines (Kozłowska et al., 2007; Xiao et al., 2005) for the treatment of stroke.
We have routinely employed the mononuclear cell (MNC) fraction of human umbilical cord blood (HUCB) in our studies. It is a mixed population of cells composed predominantly of immature T-cells, B-cells, monocytes, and stem cells. Although we have repeatedly shown the neuroprotective and anti-inflammatory effects of HUCB cells following MCAO, it is unclear which of the cell populations within the MNC is responsible for these effects. All of the major components of the HUCB MNCs are immunologically immature and do not respond to stimulation in the same way mature T cells, B cells or monocytes respond; as such they may passively interfere with the ongoing inflammatory responses that occur after MCAO. Alternatively, their more limited repertoire of responses may skew their responses toward one aspect of the cells’ function. For example, HUCB derived monocytes are not as responsive to stimulation with hepatocyte growth factor (Jiang et al., 2001), interleukin (IL)-4, or granulocyte and macrophage colony stimulating factor (GM-CSF) (Liu et al., 2001) and therefore produce fewer dendritic cells than adult monocytes as well as producing less IL-1β, TNF-α and adhesion molecules (Brichard et al., 2001; Jiang et al., 2001; Le et al., 1997). As we begin to develop a HUCB-based cell therapy for stroke, it becomes even more important to characterize the active component of the cell preparation in order to provide only those cells that are necessary for the anti-stroke effect, thereby enhancing the therapeutic potency and reducing potential adverse reactions. Therefore, in this study, specific cellular components of the HUCB MNC were depleted (monocytes (CD14+), stem cells (CD133+), T-cells (CD2+) or B cells (CD19+)) and the ability of the resulting cell preparations to induce behavioral recovery and minimize infarct size were measured in male Sprague Dawley rats after MCAO. CD133+ stem cells instead of the CD34+ hemtoapoietic stem cell studied by other groups because these cells can give rise to both hematopoietic and non-hematopoietic cells. Moreover, administration of CD14 enriched fractions confirmed the effects of this specific cell population on infarct size.
MATERIALS AND METHODS
Animals
These studies were carried out under the purview of the University of South Florida Institutional Animal Care and Use Committee (protocol #2866, #3472) and adhered to the NIH Guide for the Care and Use of Laboratory Animals. Adult male Sprague Dawley rats (344 ± 5 g at surgery) were group housed in a temperature controlled room with free access to food and water under 12 hour light/dark conditions. All animals underwent MCAO and were then randomly assigned to the experimental conditions. Surgical mortality was 21%. We lost an additional 4 animals because cerebral blood flow did not decrease to criterion. In the first 4 days post-stroke, an additional 19% of animals were either euthanized or died; these animals came from all experimental conditions. Fifty-one animals completed the study with the final number per group as follows: MCAO-only (n=8), HUCB MNC (n=7), adult human peripheral blood mononuclear cells (HPB; n=7), or HUCB depleted of CD2+ T cells (n=6), CD133+ stem cells (n=8), CD19+ B cells (n=7) or CD14 monocytes and macrophage (n=8).
A second cohort of animals was transplanted with enriched HUCB cell fractions. In this study, mortality was 20.5%. Forty-eight animals completed the study with the final number per group as follows: MCAO-only (n=12), HUCB MNC (n=9), CD14+ cells from adult HPB (HPB CD14+; n=10) and CD14+ cells from HUCB (n=17).
Middle Cerebral Artery Occlusion
At the time of surgery, the animals were anesthetized with Isoflurane (2–5% in O2 delivered at 2 liters/min) and the top of the skull exposed. Using a Dremel microdrill, a small hole was drilled through the skull 1 mm posterior and 4 mm lateral to bregma. A hollow guide screw was placed in the hole and a 500 µm fiber optic filament was inserted through the guide until it rested on the surface of the brain. The filament was anchored with super glue. Cerebral blood perfusion was measured with the Moor Instruments Ltd., Flow Laser Doppler using MoorLab Windows-based software.
Once the laser Doppler probe was in place, an incision was made just above the clavicle. Using blunt dissection techniques, the right common carotid artery was exposed and carefully dissected from surrounding tissue. The external carotid was ligated and a 4 cm length of 4.0 monofilament was inserted into the artery and then threaded through the internal carotid to the origin of the right middle cerebral artery (about 25 mm from the point of insertion). Cerebral blood perfusion was again measured. To be included in the study, blood flow had to decrease at least 60% from the baseline recorded prior to occlusion. Once this was established, the monofilament was permanently anchored in place and the incision closed. The screw guide and fiber optic filament were removed from the skull and the incision closed.
Behavioral Testing
Both prior to MCAO surgery and one month post-MCAO, behavioral tests were performed to determine extend of MCAO impairment and HUCB-induced recovery.
Spontaneous Activity
The animals were placed in a Plexiglass box (35 × 20 × 30 cm) surrounded by two tiers of infrared beams (Sanberg et al., 1987) and spontaneous activity measured as previously described (Willing et al., 2003). Locomotor parameters examined were horizontal activity, total distance travelled in the cage, margin distance (distance travelled around the perimeter of the cage) and clockwise rotation. Spontaneous activity was measured hourly during the 12 hour dark phase of the light cycle. Activity is calculated as percent of baseline activity for each animal and then this is averaged across animals in each group. The data are presented as mean ± SEM.
Step test
This test was performed as previously described (Willing et al., 2003). The paws were tested in random order and the data presented as mean ± SEM percent of the number of steps taken during baseline.
HUCB Cell Preparation and Administration
We have previously shown that the optimal time to administer the HUCB cells is 48 hours post-MCAO (Newcomb et al., 2006); we therefore transplanted the cells at this time point post MCAO to all groups except the non-treatment (MCAO only) group. The cells (either HUCB or HPB MNC, obtained commercially from AllCells, LLC), were thawed rapidly at 37°C and transferred slowly into 10 ml of 10mM PBS. The cells were then centrifuged for 10 minutes at 2000 rpm, the supernatant removed and cell viability determined using the trypan blue dye exclusion method. The HPB MNC were used as a cellular control group for the HUCB MNC fraction. In one HUCB group, the whole MNC fraction was injected. For the remaining HUCB groups, the cells then underwent cell sorting prior to administration.
Magnetic Antibody Cell Sorting (MACS)
Cellular Depletion
Magnetic Antibody Cell Sorting (MACS) was used to deplete specific populations of cells from the HUCB mononuclear fraction. First, the HUCB cells were thawed quickly in a 37°C water bath and transferred into 5–10 ml of running buffer plus 100 µl DNase. After determining viability of the cells using the trypan blue dye exclusion method, the sample was centrifuged at 1000 rpm × 10 minutes. The supernatant was removed and the cells resuspended in buffer at a volume of 80 µl/107 cells and incubated for 15 min at 4°C. Antibody conjugated paramagnetic microbeads (20µl/107 cells) were then added to the cells. CD2 labeled beads (cat#130-091-114, Miltenyi Biotech) were used to deplete T cells, CD14 labeled beads (cat# 130-050-201, Miltenyi) to deplete monocytes/macrophage, CD19 (cat# 130-050-301, Miltenyi Biotech) to deplete B cells and CD133 (cat#130-090-853) to deplete stem cells. After incubation, the cells were washed with 10–20× labeling volume of buffer and centrifuged at 1000 rpm for 10 min. The supernatant was removed and the cells resuspended in 500 µl of buffer. Cells were then depleted by passing the cells through a column with a high magnetic field gradient that trapped the paramagnetic beads and the cells they were attached to (AutoMacs Pro). An aliquot of the resulting cell preparation was then analyzed by flow cytometry to determine composition. The cells were placed into 200 µl of flow cytometry buffer (0.02% BSA, 0.05 mM EDTA in PBS) containing Fc-block™ (BD Pharmingen) to reduce non-specific antibody binding. and then incubated in the dark with the designated human antibody for 60 minutes on ice, washed and flow cytometry performed on the BD LSR II flow cytometery system. Control samples matched for each fluorochrome and each antibody isotype were used to set negative staining criteria. Dead cells were excluded using propidium iodide staining. Data were analyzed using BD FACS Diva software (see Table 1)
Table 1.
Efficiency of MACS Depletion
| Cell Type | Antigen | Non-Depleted | Depleted | Percent Depletion |
|---|---|---|---|---|
| T Cell | CD2 | 70.5% | 54.8% | 22.3% |
| Monocyte | CD14 | 57.5 | 0.9% | 99.9% |
| B Cell | CD19 | 52.2% | 6% | 88.5% |
| Stem Cell | CD133 | 3.4% | 1.6% | 52.9% |
Cellular Enrichment
Magnetic Antibody Cell Sorting (MACS) was used to enrich specific populations of cells from the HUCB mononuclear fraction. The HUCB cells were thawed and viability determined as described for cellular depletion. The supernatant was removed and the cells resuspended in buffer at a volume of 80 µl/107 cells and incubated for 15 min at 4°C. Antibody conjugated CD14+ (cat# 130-050-201, Miltenyi)paramagnetic microbeads (20µl/107 cells) were then added to the cells and incubated for 15 min at 4°C. After incubation, the cells were washed with 10–20× labeling volume of buffer and centrifuged at 1000 rpm for 10 min. The supernatant was removed and the cells resuspended in 500 µl of buffer and then passed through a column with a high magnetic field gradient that trapped the paramagnetic bead labeled. The magnetic field gradient was removed, releasing the labeled cells into a new vial with buffer.
Transplantation
Cell concentration was adjusted to 2 × 106 cells/ ml. The rats were anesthetized with Isoflurane (2–5% in O2 delivered at 2 liters/min) and a 30 gauge needle inserted into the lumen of the penile vein. In the negative selection study a single fixed (non-body weight adjusted) dose of cells (1 × 106 cells in 500 µl PBS) was delivered over 5 min. We have previously demonstrated that this is the optimal cell dose in our rodent MCAO model when the HUCB MNCs are delivered 48 hours post-stroke, regardless of body weight (Newcomb et al., 2006; Vendrame et al., 2004). Pressure was applied to the insertion site and the needle removed. In the enrichment experiment, the MNCs were delivered at 1 × 106 cells in 500 µl PBS while the CD14+ cells were delivered at 1.5 × 105 cells in 500 µl PBS, which is equivalent of the approximate number of CD14+ cells present within the 1 × 106 cell dose of MNC fraction.
Tissue Preparation and Immunohistochemistry
After the last behavioral tests, the animals were perfused transcardially with 0.1 M phosphate buffer (PB) until the blood cleared. The animals were then perfused with 4% paraformaldehyde (PFA) in PB, the brain harvested and post-fixed in PFA for 24 hours. The brains were then cryopreserved in 20% sucrose for 24 hours, sectioned at 30 µm on a cryostat and thaw mounted. These slides were stored at −20°C until use.
Nissl Thionin histology
The slides were rehydrated through a series of graded alcohols and then incubated in Nissl Thionin in glacial acetic acid/ 1N NaOH solution for 1.5 min. Distilled water was used to rinse the slides for 2 min before they were dehydrated, cleared in xylene and coverslipped with Permount. Six representative sections equally spaced through the extent of the infarct beginning 1.7mm anterior to bregma and ending 3.3 mm posterior to bregma were chosen for analysis. We measured the area of intact tissue (mm2) in the normal (contralateral) hemisphere and in the damaged hemisphere using the analysis tool in Adobe Photoshop CS4 Extended. These measured areas were summed for both the infarcted and normal hemispheres. Relative infarct size was determined by subtracting the summed areas of intact tissue on the infarcted side of the brain from the summed areas of the contralateral side and was expressed as a percentage of the contralateral hemisphere.
Immunohistochemistry for microglia
In order to examine changes in microglia, two sections were chosen between 0.7mm anterior and 0.3 mm posterior to bregma for analysis. The sections were washed with 0.1M phosphate buffered saline (PBS) before being incubated in 40% methanol 2% H2O2 in PBS for 20 min at room temperature. The sections were washed again and blocked with 10% normal goat serum with 0.03% Triton ×100 in PBS for 1 hour. After blocking, sections were incubated in rabbit anti-Iba-1, which labels ionized calcium binding adaptor molecule 1 present in myeloid cells (1:1000, Wako, cat. #011974) overnight at 4°C. The following day, the sections were washed and then incubated in biotinylated goat anti-rabbit secondary antibody (1:300, Jackson ImmunoResearch) for 1 hour at room temperature. After washing, the sections were incubated in ABC solution (Vector Laboratories) for 1 hour, washed again and then the immunolabeling visualized using DAB (Pierce). The slides were then dried, dehydrated through a graded series of alcohols, cleared in xylene and coverslipped with DPX. The sections were examined on an Olympus BX60 microscope at 20×, the view field aligned to medial edge of the infarct and the image captured with a Magnafire digital camera. The number of IBa1 labeled cells was counted using a semi-automated process with Image-Pro Plus software (Media Cybernetics).
Statistical Analysis
The data are reported as mean ± SEM. Based on a previous study in which we examined the effect of HUCB MNC fractions on cellular content of spleen and circulating lymphocytes (Golden et al., 2012), we had hypothesized that removing specific cellular components of the MNC would negatively affect behavioral recovery and infarct size. For these analyses, we made a priori comparisons with t tests (Prism 5, GraphPad Software, Inc.) corrected for multiple comparisons with the Benjamini-Hochberg procedure (McDonald, 2009). In this statistical procedure the false discovery rate is controlled. The false discovery rate we were willing to accept was 20%. We compared MCAO only group to HPB treated and MNC treated as well as comparing the MNC group with all the groups in which cell populations were depleted. For the enrichment study, the infarct data were analyzed by ANOVA with Neuman-Keuls post-hoc tests. For analysis of IBa1 immunolabeling, analysis of variance was performed followed by Newman-Keuls post-hoc tests. A p value < 0.05 was considered significant.
RESULTS
Removing CD14+ monocytes from the HUCB MNC reversed the behavioral improvement observed with MNC administration
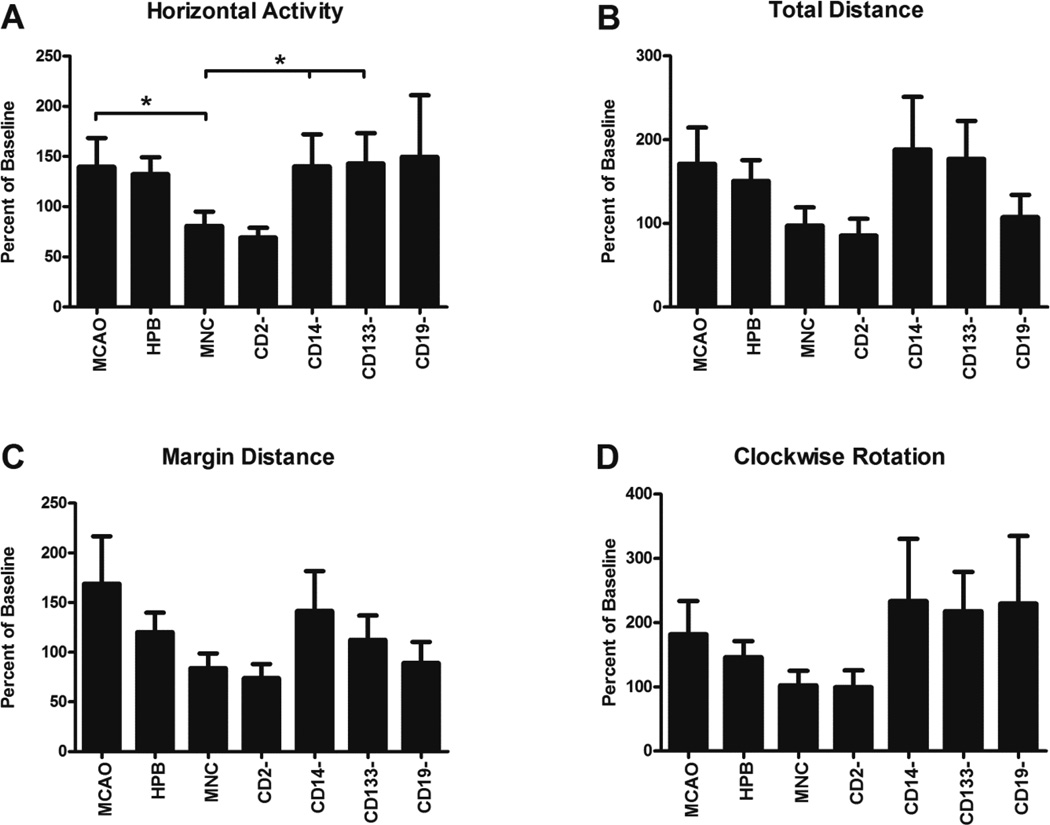
Measurement of spontaneous activity was performed during the 12 hour dark phase of the light cycle when the animals were most active using an automated open field system from Accuscan Instruments. The animals were tested both prior to MCAO and then at 1 month after the surgical procedure. The data are expressed as percent of baseline. In Figure 1, we present activity measured on four parameters – horizontal activity (Figure 1A), total distance traveled in the horizontal plane (Figure 1B), total distance traveled around the outside edges of the test cage (margin distance; Figure 1C) and clockwise rotation (Figure 1D). After MCAO, there was an increase in activity above baseline levels on all measured variables, consistent with previous observations (Block and Schwarz, 1996; Borlongan et al., 1995a; Borlongan et al., 1995b; Newcomb et al., 2006; Poignet et al., 1989; Puurunen et al., 1997; Willing et al., 2002). There were no significant differences between the MCAO group and the HPB group on any parameters. Administration of HUCB MNC reduced horizontal activity significantly (p < 0.05) but only marginally reduced activity on all other parameters examined. Animals that were treated with CD14 depleted MNC were as active as untreated MCAO animals on all activity measures and significantly more active than MNC treated animals (p < 0.05). Removal of the CD133 cells resulted in a significant increase from the amount of horizontal activity observed compared to the MNC group (p <0.05). Removal of the CD19+ B cells produced variable results, tending to increase horizontal activity and clockwise rotation but having little effect on total distance or margin distance.
Figure 1. Depletion of CD14+ and CD133+ cells from HUCB MNC reverses the effect of HUCB MNC on spontaneous activity.
Following baseline recording of spontaneous activity during the dark phase of the light cycle, rats underwent MCAO and then were injected with either HUCB MNC (n=7), or MNC depleted of one of the following cell types; T-cells (CD2−; n=6), monocytes and macrophages (CD14−, n=8), stem cells (CD133−; n=8), B-cells (CD19−; n=7), or human peripheral blood (HPB) MNC (n=7). The negative control was MCAO only (n=8). Measures shown: A) Horizontal activity. B) Total distance traveled. C) Margin distance or the distance traveled along the outside perimeter of the test cage. D) Clockwise rotation. * p< 0.05.
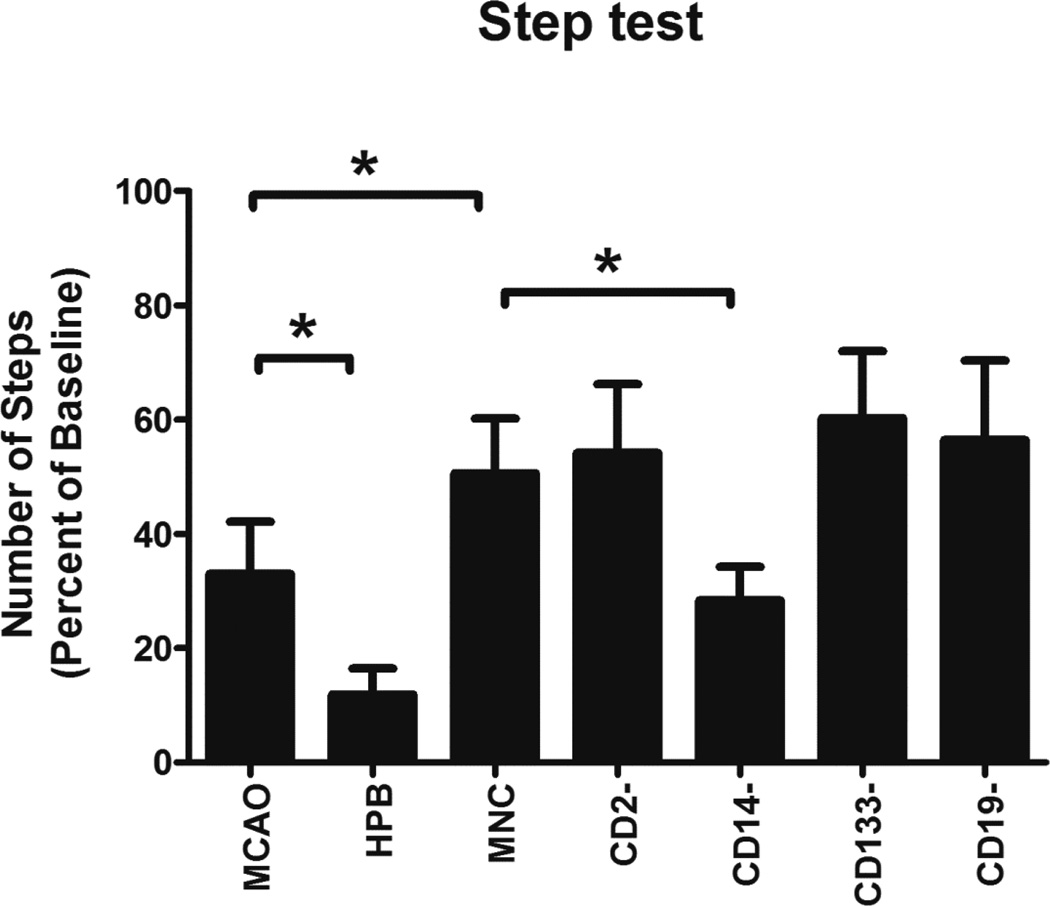
The Step test of motor asymmetry was used to measure function of the contralateral forelimb. After MCAO, the number of steps taken with the contralateral paw in the MCAO only group was 33.0 ± 9.2% of the baseline number of steps (Figure 2). Administering HPB cells actually reduced the number of steps taken even further (11.9 ± 12.2%, p < 0.05 compared to MCAO only). With administration of MNC, the percentage of steps taken marginally improved to 50.6 ± 9.6%. Number of steps taken significantly decreased in the CD14 depleted group (28.4 ± 5.8%) compared to the MNC treated group (p < 0.05). Removal of the CD2, CD133 and CD19 cells from the MNC did not alter performance on the Step test compared to the MNC treated group.
Figure 2. Depletion of CD14+ cells from the HUCB MNC eliminates improved motor function on the Step Test.
The rats were dragged at constant velocity for one meter with their impaired paw in contact with the table top. The number of steps taken was counted prior to MCAO and then 30 days post-MCAO. In the MCAO only group, the rats took less than 40% of the steps with their impaired paw than they had prior to MCAO. Administration of MNC resulted in the rats performing better on this test while removal of the CD14+ cells from the MNC reversed this improvement. * p< 0.05.
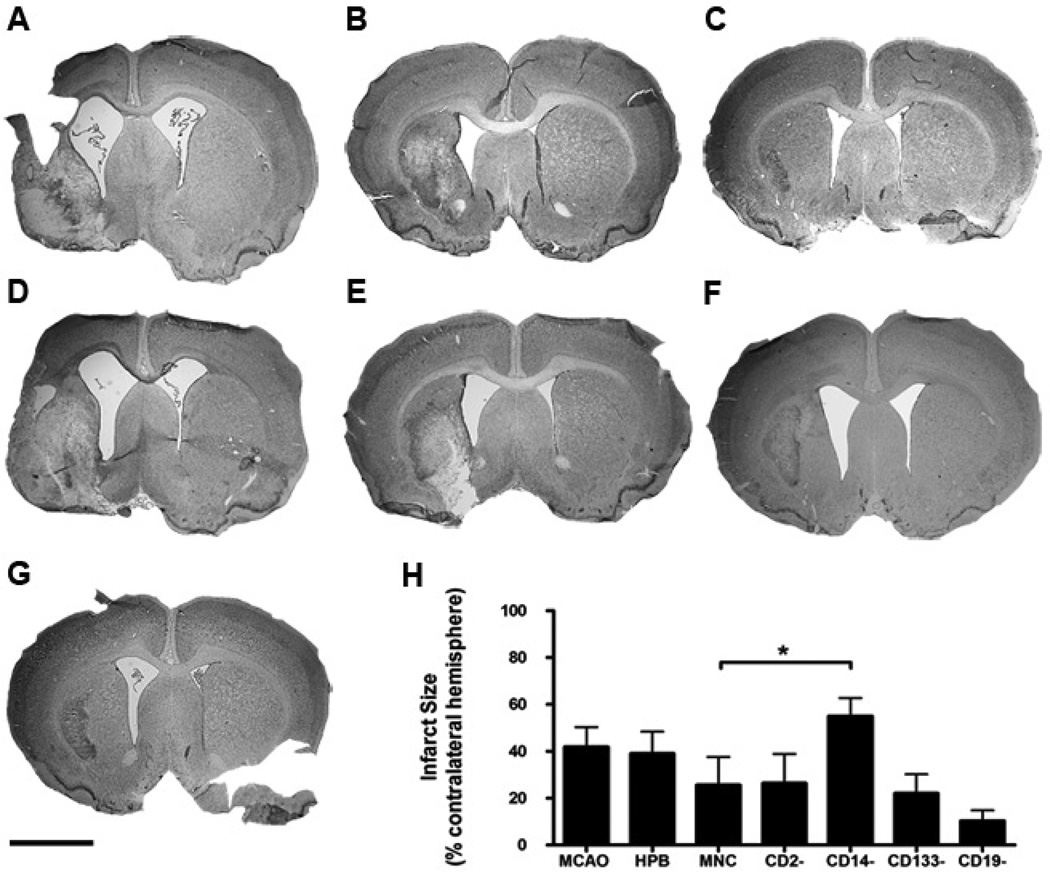
Removal of CD14+ monocytes from the HUCB MNC increased infarct size after MCAO
Infarct size was determined using Nissl Thionin histology (Figure 3). There was extensive damage in the lateral striatum and overlying cortex after MCAO (Figure 3A). Administration of HPB did not reduce infarct size (Figure 3B, 3H). The lateral ventricle in the infarcted hemisphere was enlarged and there was some loss of striatal architecture. Infarcts were visible in all HUCB treated groups (Figure 3C–G); all had ongoing degenerative processes as illustrated with the Nissl Thionin staining and various degrees of ventricular enlargement and loss of tissue. When we analyzed infarct size, there was a significant increase in infarct size in the groups treated with CD14 depleted MNC compared to the group that received the whole MNC fraction (p < 0.05).
Figure 3. CD14+ Cell Depletion increased infarct size after MCAO.
Thionin histology was used to delineate the brain damaged area in cortex and striatum. A) MCAO (n=8). B) Treatment with HPB MNC (n=8). C) HUCB MNC (n=7). D) MNC depleted of CD2 T cells (n=6). E) MNC depleted of CD14 monocytes (n=8). F) MNC depleted of CD133 stem cells (n=8). G) MNC depleted of CD19 B cells (n=7). H) Infarct size calculated from 6 sections equally spaced throughout the extent of the damaged hemisphere (Bregma −1.7 to +3.3). *p< 0.05.
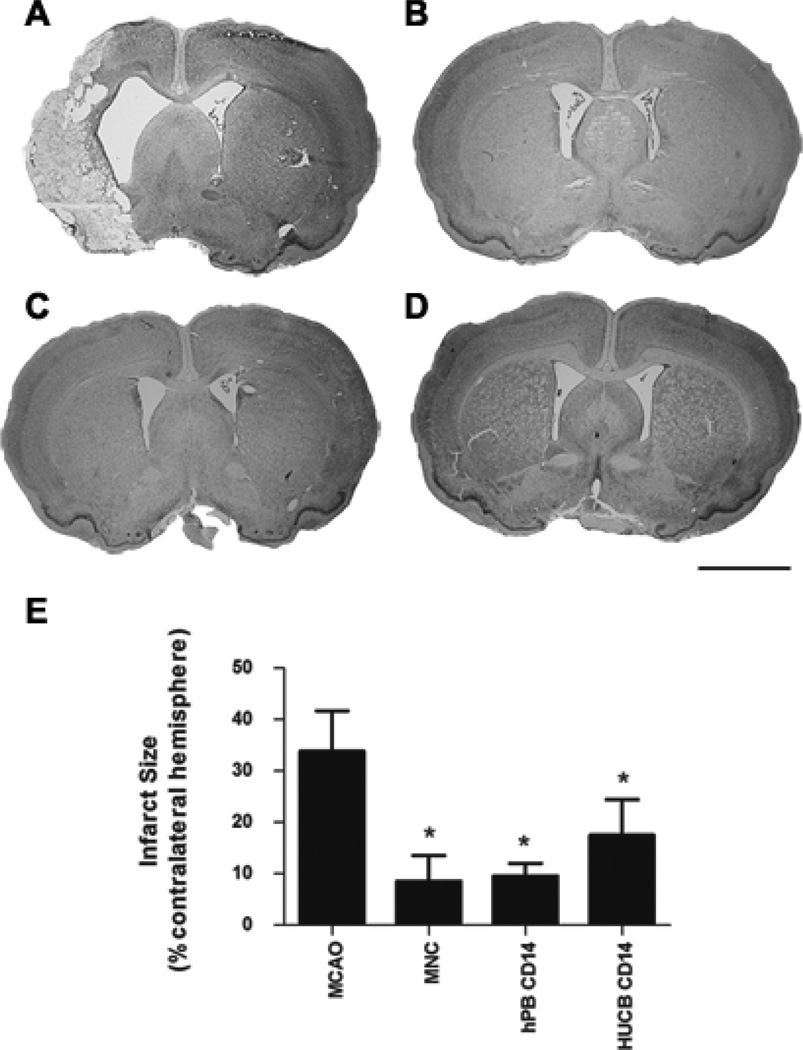
Administration of CD14+ monocytes replicates the effect of HUCB MNC on infarct size after MCAO
To provide further evidence for the role of CD14+ monocytes in the HUCB MNC effects, we injected a cohort of animals with either HUCB MNCs, HUCB CD14+ cells or HPB CD14+ cells (Figure 4). Infarct size was decreased equally in all cell transplant groups and was significantly less infarct size in the MCAO only group. In addition, infarct size in the CD14 antibody group was also significantly decreased.
Figure 4. CD14+ cells from HUCB and HPB Decrease Infarct Size.
A) MCAO. B) Treatment with HUCB MNC. C) HPB CD14+ cells. D) HUCB CD14+ cells. E) Infarct size. Six representative sections equally spaced through the extent of the infarct beginning 1.7mm anterior to bregma and ending 3.3 mm posterior to bregma were stained with thionin. Infarct size was determined with the indirect method. All treated groups had significantly smaller infarcts than the MCAO alone group. *p< 0.05.
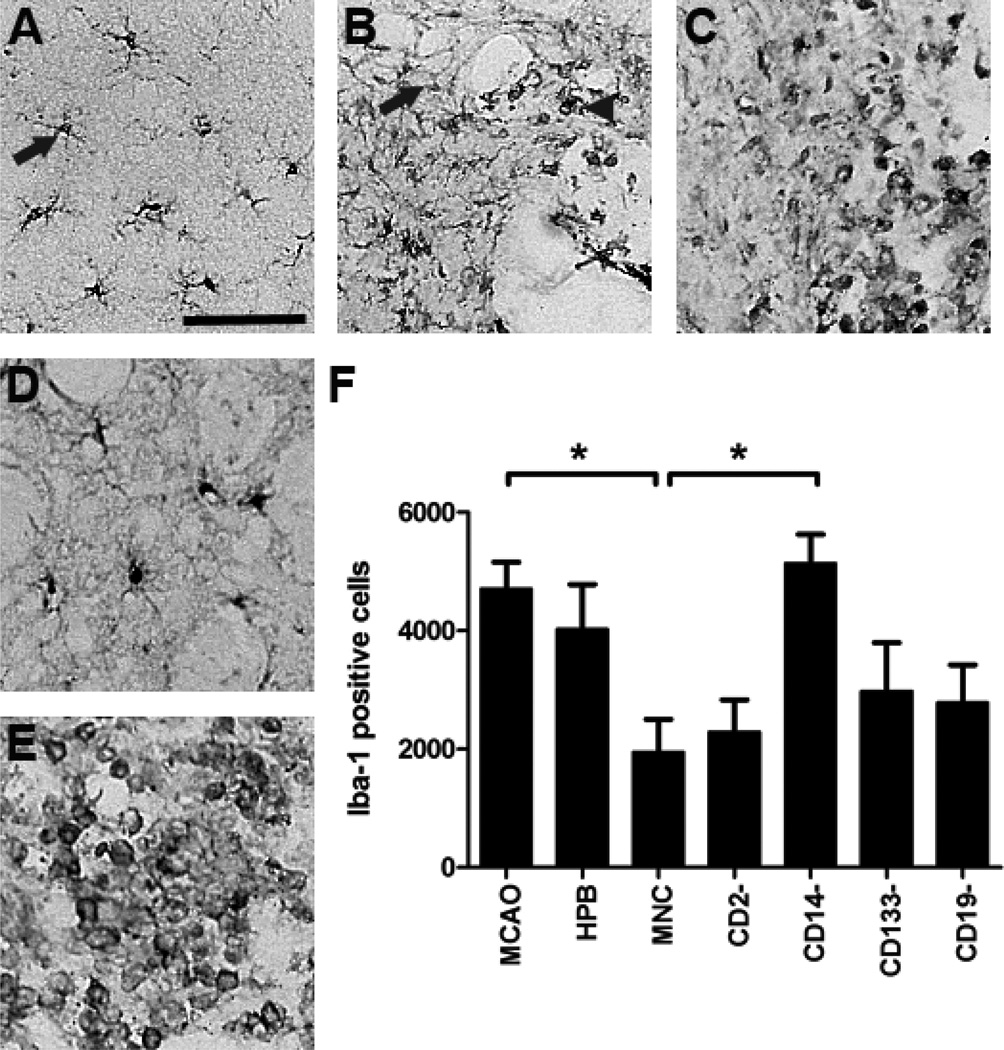
IBa1+ labeling of cells in the infarcted hemisphere
We have previously shown that HUCB MNC modify the inflammatory response to MCAO, as indicated by changes in the number and morphology of myeloid cells (microglia, monocytes or macrophage) (Leonardo et al., 2010) and altered cytokine profile (Vendrame et al., 2005). In this study we used an antibody to IBa1 to determine if there were long term changes in these myeloid cells in response to the MCAO and HUCB treatment. Microglia within the contralateral hemisphere of the untreated MCAO only animals exhibited a resting morphology, with a small cell body and long branching processes (Figure 4A). In the untreated MCAO animals even 30 days post-MCAO, there were many IBa1 positive (+) cells in the border zone around the infarct as well as within the core of the infarct (Figure 5B). The cells in this region exhibited all three “microglial” morphologies – small and ramified (resting), bushy and ramified (partially activated state) or amoeboid (phagocytic/inflammatory state). In the HPB treated animals, there were many amoeboid and bushy ramified microglia within and around the infarct site (Figure 5C). Consistent with the earlier studies, rats treated with HUCB MNC exhibited microglia with a resting phenotype throughout the infarcted hemisphere (Figure 5D). When we examined sections from the CD14 depleted group, however, there was extensive IBa1 immunolabeling and the majority of labeled cells exhibited an amoeboid morphology (Figure 5E). When we quantified the number of labeled cells in the sections, there was a significant effect of treatment (p < 0.008; Figure 5F). When individual comparisons were made using the Newman-Keuls test, there were significantly fewer microglia in the MNC group than in the MCAO only group (p < 0.05). There were also significantly more labeled microglia in the CD14 depleted group than in the MNC group (p < 0.05).
Figure 5. Representative photomicrographs of immunostaining for IBa1 labeled microglia following MCAO.
A) Microglia in the contralateral hemisphere after MCAO exhibited a resting, ramified morphology (arrow). B) Microglia in the ipsilateral hemisphere after MCAO are observed with the infarct core and around the boundaries of the infarct (n=8) and exhibit resting (arrow), ramified and activated (asterisk) and amoeboid (arrowhead). C) HPB MNC (n=7). D) HUCB MNC (n=7). E) MNC depleted of CD14 monocytes (n=8). Scale bar = 50 µm. F) There were significantly fewer microglia in the brain of animals treated with HUCB MNC or MNC depletd of CD2 T cells compared to animals treated with MNC depleted of CD14 monocytes. *p< 0.05.
DISCUSSION
The goal of this study was to determine which subpopulation of MNC HUCB cells is responsible for the ability of the HUCB MNC fraction to decrease infarct size and improve recovery. Using MACS, we depleted the HUCB MNC of monocytes, T cells, B cells or CD133+ stem cells. Depletion of the CD14+ monocytes produced the largest, most consistent decrements in behavioral recovery and increased infarct size. Activity levels and infarct size of the animals treated with monocyte depleted HUCB MNC were similar to that observed in the untreated MCAO group. When animals were treated with enriched fractions of CD14+ cells infarct size decreased to the same extent as with the MNC treated group. These results suggest that HUCB monocytes are the critical cellular component of HUCB MNC fraction that induces recovery after MCAO.
Monocytes repair ischemic damage
There have been three recent reports implicating monocytes in ischemic tissue repair. When CD14+ cells isolated from adult human peripheral blood MNC fraction were injected into the ischemic hind limb of diabetic mice, there was less necrotic muscle and greater arteriolar densities in the treated mice (Awad et al., 2006). In a second study, either CD133+ stem cells or CD11b+ monocytes from mouse bone marrow were injected intravenously (i.v.) or intramuscularly (i.m.) 24 hours after induction of hind limb ischemia (Sanchez-Guijo et al., 2010). Whether delivered i.m. or i.v. both cell types significantly increased blood flow to the ischemic limb as measured by laser Doppler and both increased capillary density as determined using immunohistochemistry for endothelial nitric oxide synthase. Neither cell type integrated into the new blood vessels in the muscle, however, suggesting that the cells may be releasing angiogenic substances. The third study was a clinical trial in which patients with refractory angina received multiple injections of autologous bone marrow MNCs into viable, but ischemic myocardium (Hossne et al., 2009). Patients exhibited significant, progressive improvements in clinical angina classification that were maintained out to 18 months post-transplant as well as reduced ischemia as determined using stress technecium scintigraphy. Improved function was correlated with the monocyte content of the MNC fraction and not lymphocyte or stem cell content.
In all three of these studies, treatment with monocytes, decreased damage. Our results are consistent with these earlier observations since removal of the CD14+ monocytes from the HUCB MNC fraction eliminated the neuroprotective and anti-inflammatory effects of HUCB administration in our permanent MCAO model while administering cord blood derived CD14+ reduced infarct size to a similar degree as the MNC fraction.
The results of these earlier studies also suggest that the therapeutic properties of monocytes may not be limited to the HUCB derived cells, but may be a universal property of monocytes, regardless of their source. Indeed, when we administered CD14+ cells harvested from adult HPB, infarct size was decreased to the same extent as when we administered HUCB MNC or CD14+ cells. However, the HPB MNC did not induce behavioral recovery or have any effect on infarct size, in spite of the fact that monocytes are present in HPB MNC. The explanation for this discrepancy may rest in the interactions of the mononuclear fraction cellular components. Both T and B cells in the adult peripheral blood are fully competent immune cells whereas the HUCB T and B cells are not. While monocytes can inhibit T cell proliferation (Slaney et al., 2011) and present antigen to B cells (Randolph et al., 2008), administering the mixture of fully competent immune cells into the pro-inflammatory environment prevalent after MCAO may mask the protective effects of the monocytes.
CD14+ depleted HUCB Cells Increase MCAO-induced Inflammation
Inflammation begins immediately after the onset of an ischemic stroke and is characterized by an early proliferative response followed by a later pro-inflammatory response. During the early phase, the proliferating microglia secrete insulin-like growth factor one (IGF 1), which is neuroprotective (Kriz, 2006). Indeed, by eliminating microglia or macrophage during this early inflammatory phase, infarct size is increased (Lalancette-Hebert et al., 2007; Smirkin et al., 2010). Similar observations have been made in other models of neurodegeneration; inhibiting tumor necrosis factor alpha (TNFα) during the first week after 6-hydroxydopamine (6-OHDA) treatment produced a larger lesion than inhibiting TNFα beginning 5 days after 6-OHDA (Gemma et al., 2007). Smirkin and associates demonstrated that Iba1+/NG2+ cells observed in the brain during the first 2 days after transient MCAO expressed mRNA for multiple growth factors (Smirkin et al., 2010), which would account for their neuroprotective properties. The later inflammatory response is characterized by the massive influx of peripheral immune cells (mainly macrophage) and the release of pro-inflammatory cytokines. In our MCAO model, we showed that there is a transformation of CD11b+ cells into amoeboid cells and infiltration of isolectin+ cells into infarcted hemisphere that occurs by 72 hours after stroke onset (Leonardo et al., 2010); these cells express matrix metalloproteinase (MMP)-9 and nitric oxide. By administering the HUCB MNCs 48 hours after stroke, we allow the early inflammatory response to proceed while altering the secondary inflammatory response. Indeed, HUCB MNCs decrease the number of CD11b+ cells (microglia, monocytes, and macrophage) within the brain and this decrease is associated with a significant decrease in both mRNA and protein expression of pro-inflammatory cytokines (Vendrame et al., 2005). Further, the HUCB MNCs decrease microglial activation as indicated by a return to resting morphology within 24 hours of administration (Leonardo et al., 2010). In this study we showed that the return to resting morphology in the infarcted hemisphere is maintained out to one month after MCAO. In contrast when the CD14+ monocytes are depleted from the HUCB MNC, there are more Iba-1+ cells within the infarcted hemisphere and they have an amoeboid morphology indicative of a pro-inflammatory, phagocytic function.
The mechanism by which the CD14+ monocytes produce this alteration in microglial or macrophage function in the brain, remains to be elucidated. Adult monocytes can differentiate into macrophage and dendritic cells but they also scavenge toxins, produce cytokines, growth factors, reactive oxygen species, nitric oxide, prostaglandins, complement and proteolytic enzymes (see references (Auffray et al., 2009; Geissmann et al., 2008) for recent reviews) and can function as antigen presenting cells (Van Voorhis et al., 1983). In many respects, monocytes within HUCB are indistinguishable from adult monocytes (Filias et al., 2011; Gille et al., 2009), but they are not stimulated by hepatocyte growth factor (Jiang et al., 2001), produce fewer dendritic cells compared to adult monocytes (Liu et al., 2001) and also produce lower concentrations of pro- and anti-inflammatory cytokines (Brichard et al., 2001; Jiang et al., 2001; Le et al., 1997). A recent report in a model of diabetic retinopathy demonstrated that CD14+ HUCB cells became alternatively activated M2 macrophage that stimulated the resident myeloid cells to also become alternatively activated (Marchetti et al., 2011). Removal of the CD14+ monocytes would remove a significant anti-inflammatory, regenerative signal.
The Role of other MNCs in HUCB induced recovery
Our data in those animals that received the CD133 (stem cell) and CD2 (T cell) depleted HUCB preparations do not allow us to draw any firm conclusions about the role of these cells in HUCB induced recovery after MCAO since the MACS sorting only depleted 52.9% and 22.3% respectively of these cells from the MNC fraction. Removal of the B cells from the MNC fraction was more effective, removing 88.5% of the cells. Even so, the results were equivocal; activity tended to increase on some of the measured parameters but there were no significant increases on the behavioral measures or in infarct size. The lack of effect after B cell removal from the HUCB MNC fraction would suggest that these are not the primary cells involved in HUCB MNC induced repair.
In summary, CD14+ monocytes play a critical role in the ability of HUCB cells to improve functional recovery and reduce infarct size in the permanent MCAO rat model of stroke; removal of these cells from the MNC eliminated the HUCB therapeutic effects while administering CD14+ monocytes alone replicated the HUCB-induced brain repair. The protective effects of the CD14+ monocytes was similar regardless of whether they were harvested from adult blood or cord blood. These results are consistent with other recent studies demonstrating the ability of monocytes to induce tissue repair in multiple models of ischemic tissue injury. Additional studies will be required to determine if monocyte therapeutic effects are a result of direct modulation of inflammatory processes, induction of angiogenesis (see (Sanberg et al., 2010) for a recent review), or activation of other processes.
ACKNOWLEDGEMENTS
This research was supported in part by NINDS RO1NS52839 (AEW). AEW is a consultant and PRS a co-founder of Saneron CCEL Therapeutics, Inc. AEW and PRS are inventors on cord blood patents licensed to Saneron, and a monocyte patent with CryoPraxis, Inc. PRS is also a consultant to CryoPraxis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Auffray C, Sieweke MH, Geissmann F. Blood Monocytes: Development, Heterogeneity, and Relationship with Dendritic Cells. Annual Review of Immunology. 2009;27:669–692. doi: 10.1146/annurev.immunol.021908.132557. [DOI] [PubMed] [Google Scholar]
- Awad O, Dedkov EI, Jiao C, Bloomer S, Tomanek RJ, Schatteman GC. Differential Healing Activities of CD34+ and CD14+ Endothelial Cell Progenitors. Arteriosclerosis, Thrombosis, and Vascular Biology. 2006;26:758–764. doi: 10.1161/01.ATV.0000203513.29227.6f. [DOI] [PubMed] [Google Scholar]
- Block F, Schwarz M. Dextromethorphan reduces functional deficits and neuronal damage after global ischemia in rats. Brain Research. 1996;741:153–159. doi: 10.1016/s0006-8993(96)00916-x. [DOI] [PubMed] [Google Scholar]
- Boltze J, Kowalski I, Förschler A, Schmidt U, Wagner D, Lobsien D, Emmrich J, Egger D, Kamprad M, Blunk J, Emmrich F. The stairway:A novel behavioral test detecting sensomotoric stroke deficits in rats. Artificial Organs. 2006;30:756–763. doi: 10.1111/j.1525-1594.2006.00297.x. [DOI] [PubMed] [Google Scholar]
- Boltze J, Kowalski I, Geiger KD, Reich DM, A G, Buhrle C, Egger D, Kamprad M, Emmrich F. Experimental treatment of stroke in spontaneously hypertensive rats by CD34+ and CD34− cord blood cells. GMS German Medical Sciences. 2008 Doc;3 [PMC free article] [PubMed] [Google Scholar]
- Boltze J, Reich DM, Hau S, Reymann KG, Strassburger M, Lobsein D, Wagner D-C, Kamprad M, Stahl T. Assessment of neuroprotective effects of human umbilical cord blood mononuclear cell subpopulations in vitro and in vivo. Cell Transplant. 2012;21:723–737. doi: 10.3727/096368911X586783. [DOI] [PubMed] [Google Scholar]
- Boltze J, Schmidt UR, Reich DM, Kranz A, Reymann KG, Strassburger M, Lobsien D, Wagner DC, Forschler A, Schabitz WR. Determination of the therapeutic time window for human umbilical cord blood mononuclear cell transplantation following experimental stroke in rats. Cell Transplant. 2011 doi: 10.3727/096368911X589609. [DOI] [PubMed] [Google Scholar]
- Borlongan CV, Cahill DW, Sanberg PR. Locomotor and passive avoidance deficits following occlusion of the middle cerebral artery. Physiology and Behavior. 1995a;58:909–917. doi: 10.1016/0031-9384(95)00103-p. [DOI] [PubMed] [Google Scholar]
- Borlongan CV, Hadman M, Davis Sanberg C, Sanberg PR. CNS entry of peripherally injected umbilical cord blood cells is not required for neuroprotection in stroke. Stroke. 2004;35:2385–2389. doi: 10.1161/01.STR.0000141680.49960.d7. [DOI] [PubMed] [Google Scholar]
- Borlongan CV, Martinez R, Shytle RD, Freeman TB, Cahill DW, Sanberg PR. Striatal Dopamine-Mediated Motor Behavior Is Altered Following Occlusion of the Middle Cerebral Artery. Pharmacology Biochemistry and Behavior. 1995b;52:225–229. doi: 10.1016/0091-3057(95)00108-9. [DOI] [PubMed] [Google Scholar]
- Brichard B, Varis I, Latinne D, Deneys V, de Bruyere M, Leveugle P, Cornu G. Intracellular cytokine profile of cord and adult blood monocytes. Bone Marrow Transplantation. 2001;27:1081–1086. doi: 10.1038/sj.bmt.1703037. [DOI] [PubMed] [Google Scholar]
- Chen J, Sanberg PR, Li Y, Wang L, Lu M, Willing AE, Sanchez-Ramos J, Chopp M. Intravenous administration of human umbilical cord blood reduces behavioral deficits after stroke in rats. Stroke. 2001;32:2682–2688. doi: 10.1161/hs1101.098367. [DOI] [PubMed] [Google Scholar]
- Filias A, Theodorou G, Mouzopoulou S, Varvarigou A, Mantagos S, Karakantza M. Phagocytic ability of neutrophils and monocytes in neonates. BMC Pediatrics. 2011;11:29. doi: 10.1186/1471-2431-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geissmann F, Auffray C, Palframan R, Wirrig C, Ciocca A, Campisi L, Narni-Mancinelli E, Lauvau G. Blood monocytes: distinct subsets, how they relate to dendritic cells, and their possible roles in the regulation of T-cell responses. Immunology and Cell Biology. 2008;86:398–408. doi: 10.1038/icb.2008.19. [DOI] [PubMed] [Google Scholar]
- Gemma C, Catlow B, Cole M, Hudson C, Samec A, Shah N, Vila J, Bachstetter A, Bickford PC. Early inhibition of TNFalpha increases 6-hydroxydopamine-induced striatal degeneration. Brain Research. 2007;1147:240–247. doi: 10.1016/j.brainres.2007.02.003. [DOI] [PubMed] [Google Scholar]
- Gille C, Leiber A, Mundle I, Spring B, Abele H, Spellerberg B, Hartmann H, Poets CF, Orlikowsky TW. Phagocytosis and Postphagocytic Reaction of Cord Blood and Adult Blood Monocyte After Infection with Green Fluorescent Protein-Labeled Escherichia coli and Group B Streptococci. Cytometry Part B. 2009;76B:271–284. doi: 10.1002/cyto.b.20474. [DOI] [PubMed] [Google Scholar]
- Golden JE, Shahaduzzaman M, Wabnitz A, Green S, Womble TA, Sanberg PR, K. R. Pennypacker KR, Willing AE. Human Umbilical Cord Blood Cells Alter Blood and Spleen Cell Populations After Stroke. Translational Stroke Research. 2012 doi: 10.1007/s12975-012-0208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall AA, Leonardo CC, Collier LA, Rowe DD, Willing AE, Pennypacker KR. Delayed Treatments For Stroke Influence Neuronal Death in Rat Organotypic Slice Cultures Subjected to Oxygen Glucose Deprivation. Neurosci. 2009;164:470–477. doi: 10.1016/j.neuroscience.2009.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossne J, N A, Invitti AL, Buffolo E, Azevedo S, de Oliveira JSR, Stolf NG, Cruz LE, Sanberg PR. Refractory angina cell therapy (ReACT) involving autologous bone marrow cells in patients without left ventricular dysfunction: a possible role for monocytes. Cell Transplant. 2009;18:1299–1310. doi: 10.3727/096368909X484671. [DOI] [PubMed] [Google Scholar]
- Jiang L, Womble T, Saporta S, Chen N, Sanberg CD, Sanberg PR, Willing AE. Human Umbilical Cord Blood Cells Depress the Microglial Inflammatory Response in Vitro. Stem Cells and Development. 2010;19:221–227. doi: 10.1089/scd.2009.0170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Q, Azuma E, Hirayama M, Iwamoto S, Kumamoto T, Kobayashi M, Yamamoto H, Sakurai M, Komada Y. Functional immaturity of cord blood monocytes as detected by impaired response to hepatocyte growth factor. Ped. Intl. 2001;43:334–339. doi: 10.1046/j.1442-200x.2001.01420.x. [DOI] [PubMed] [Google Scholar]
- Kern DS, Maclean KN, Jiang H, Synder EY, Sladek JR, Jr, Bjugstad KB. Neural stem cells reduce hippocampal tau and reelin accumulation in aged Ts65Dn Down Syndrome mice. Cell Transplantation. 2011;20:371–379. doi: 10.3727/096368910X528085. [DOI] [PubMed] [Google Scholar]
- Kondziolka D, Wechsler L, Goldstein S, Meltzer C, Thulborn KR, Gebel J, Jannetta P, DeCesare S, Elder EM, McGrogan M, Reitman MA, Bynum L. Transplantation of cultured human neuronal cells for patients with stroke. Neurology. 2000;55:565–569. doi: 10.1212/wnl.55.4.565. [DOI] [PubMed] [Google Scholar]
- Kozłowska H, Jabłonka J, Janowski M, Jurga M, Kossut M, Domańska-Janik K. Transplantation of a Novel Human Cord Blood-Derived Neural-Like Stem Cell Line in a Rat Model of Cortical Infarct. Stem Cells Dev. 2007;16:481–488. doi: 10.1089/scd.2007.9993. [DOI] [PubMed] [Google Scholar]
- Kriz J. Inflammation in ischemic brain injury: timing is important. Crit Rev Neurobiol. 2006;18:145–157. doi: 10.1615/critrevneurobiol.v18.i1-2.150. [DOI] [PubMed] [Google Scholar]
- Lalancette-Hebert M, Gowing G, Simard A, Weng YC, Kriz J. Selective ablation of proliferating microglial cells exacerbates ischemic injury in the brain. Journal of Neuroscience. 2007;27:2596–2605. doi: 10.1523/JNEUROSCI.5360-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le T, Leung L, Carroll WL, Schibler KR. Regulation of Interleukin-10 Gene Expression: Possible Mechanisms Accounting for Its Upregulation and for Maturational Differences in Its Expression by Blood Mononuclear Cells. Blood. 1997;89:4112–4119. [PubMed] [Google Scholar]
- Leonardo C, Hall AA, Collier LA, Ajmo CT, Jr, Willing AE, Pennypacker KR. HUCB cell therapy blocks the morphological change and recruitment of CD11b-expressing, isolectin-binding proinflammatory cells after MCAO. J. Neurosci. Res. 2010;88:1213–1222. doi: 10.1002/jnr.22306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu E, Tu W, Law HKW, Lau Y-L. Decreased yield, phenotypic expression and function of immature monocyte-derived dendritic cells in cord blood. Br. J. Haematol. 2001;113:240–246. doi: 10.1046/j.1365-2141.2001.02720.x. [DOI] [PubMed] [Google Scholar]
- Liu H-Y, Zhang Q-J, Li H-J, Han Z-C. Effect of intracranial transplantation of CD34+ cells derived from human umbilical cord blood in rats with cerebral ischemia. Chinese Medical Journal. 2006;119:1744–1748. [PubMed] [Google Scholar]
- Mampalam TJ, Gonzalez MF, Weinstein P, Sharp FR. Neuronal changes in fetal cortex transplanted to ischemic adult rat cortex. Journal of Neurosurgery. 1988;69:904–912. doi: 10.3171/jns.1988.69.6.0904. [DOI] [PubMed] [Google Scholar]
- Marchetti V, Yanes O, Aguilar E, Wang M, Friedlander D, Moreno S, Storm K, Zhan M, Naccache S, Nemerow G, Siuzdak G, Friedlander M. Differential macrophage polarization promotes tissue remodeling and repair in a model of ischemic retinopathy. Scientific Reports 1. 2011 doi: 10.1038/srep00076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald JH. Handbook of Biological Statistics (2nd ed.) 2nd ed. Baltimore, Maryland: Sparky House Publishing; 2009. [Google Scholar]
- Newcomb JD, Ajmo CT, Davis Sanberg C, Sanberg PR, Pennypacker KR, Willing AE. Timing of cord blood treatment after experimental stroke determines therapeutic efficacy. Cell Transplant. 2006;15:213–223. doi: 10.3727/000000006783982043. [DOI] [PubMed] [Google Scholar]
- Poignet H, Beaughard M, Lecoin G, Massingham R. Functional, behavioral, and histological changes induced by transient global cerebral ischemia in rats: effects of cinnarizine and flunarizine. Journal of Cerebral Blood Flow Metabolism. 1989;9:646–654. doi: 10.1038/jcbfm.1989.92. [DOI] [PubMed] [Google Scholar]
- Puurunen K, Sirvio J, Koistinaho J, Miettinen R, Haapalinna A, Riekkinen P, Sr, Sivenius J. Studies on the Influence of Enriched-Environment Housing Combined With Systemic Administration of an {alpha}2-Adrenergic Antagonist on Spatial Learning and Hyperactivity After Global Ischemia in Rats. Stroke. 1997;28:623–631. doi: 10.1161/01.str.28.3.623. [DOI] [PubMed] [Google Scholar]
- Randolph GJ, Jakubzick C, Qu C. Antigen Presentation by Monocytes and Monocyte-derived Cells. Current Opinions in Immunology. 2008;20:52–60. doi: 10.1016/j.coi.2007.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J Subcommittee, o.b.o.t.A.H.A.S.C.a.S.S. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e1–e192. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanberg PR, Park D-H, Kuzmin-Nichols N, Cruz E, Hossne J, N A, Buffolo E, Willing AE. Monocyte transplantation for neural and cardiovascular ischemia repair. J Cell. Mol. Med. 2010;14:553–563. doi: 10.1111/j.1582-4934.2009.00903.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanberg PR, Zoloty SA, Willis R, Ticarich CD, Rhoads K, Nagy RP, Mitchell SG, Laforest AR, Jenks JA, Harkabus LJ. Digiscan activity: automated measurement of thigmotactic and stereotypic behavior in rats. Pharmacology, Biochemistry & Behavior. 1987;27:569–572. doi: 10.1016/0091-3057(87)90369-8. [DOI] [PubMed] [Google Scholar]
- Sanchez-Guijo FM, Oterino E, Barbado M-V, Carrancio S, Lopez-Holgado N, Muntion S, Hernandez-Campo P, Sanchez-Abarca L-I, Perez-Simon JA, San Miguel J, s F, Bri, on J, s G, del C, izo M-C. Both CD133+ Cells and Monocytes Provide Significant Improvement for Hindlimb Ischemia, Although They do not Transdifferentiate Into Endothelial Cells. Cell Transplant. 2010;19:103–112. doi: 10.3727/096368909X476869. [DOI] [PubMed] [Google Scholar]
- Sladek JR, Bjugstad KB. The future of stem cell applications: Charting the sea of opportunity. Technology and Innovation. 2011;13:63–74. [Google Scholar]
- Slaney CY, Toker A, La Flamme A, Backstrom BT, Harper JL. Naıve blood monocytes suppress T-cell function. A possible mechanism for protection from autoimmunity. Immunology and Cell Biology. 2011;89:7–13. doi: 10.1038/icb.2010.110. [DOI] [PubMed] [Google Scholar]
- Smirkin A, Matsumoto H, Takahashi H, Inoue A, Tagawa M, Ohue S, Watanabe H, Yano H, Kumon Y, Ohnishi T, Tanaka J. Iba1+/NG2+ macrophage-like cells expressing a variety of neuroprotective factors ameliorate ischemic damage of the brain. Journal of Cerebral Blood Flow & Metabolism. 2010;30:603–615. doi: 10.1038/jcbfm.2009.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taguchi A, Soma T, Tanaka H, Kanda T, Nishimura H, Yoshikawa H, Tsukamoto Y, Iso H, Fujimori Y, Stern DM, Naritomi H, Matsuyama T. Administration of CD34+ cells after stroke enhances neurogenesis via angiogenesis in a mouse model. J. Clin. Invest. 2004;114:330–338. doi: 10.1172/JCI20622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonder N, Sorensen T, Zimmer J, Jorgensen MB, Johansen FF, Diemer NH. Neural grafting to ischemic lesions of the adult rat hippocampus. Experimental Brain Research. 1989;74:512–526. doi: 10.1007/BF00247353. [DOI] [PubMed] [Google Scholar]
- Van Voorhis WC, Valinsky J, Hoffman E, Luban J, Hair LS, Steinman RM. Relative efficacy of human monocytes and dendritic cells as accessory cells for T cell replication. J. Exp. Med. 1983;158:174–191. doi: 10.1084/jem.158.1.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vendrame M, Cassady CJ, Newcomb J, Butler T, Pennypacker KR, Zigova T, Davis Sanberg C, Sanberg PR, Willing AE. Infusion of human umbilical cord blood cells in a rat model of stroke dose-dependently rescues behavioral deficits and reduces infarct volume. Stroke. 2004;35:2390–2395. doi: 10.1161/01.STR.0000141681.06735.9b. [DOI] [PubMed] [Google Scholar]
- Vendrame M, Gemma C, de Mesquita D, Collier L, Bickford PC, Davis Sanberg C, Sanberg PR, Pennypacker KR, Willing AE. Anti-inflammatory Effects Of Human Cord Blood Cells In A Rat Model Of Stroke. Stem Cells Dev. 2005;14:595–604. doi: 10.1089/scd.2005.14.595. [DOI] [PubMed] [Google Scholar]
- Willing AE, Lixian J, Milliken M, Poulos S, Zigova T, Song S, Hart C, Sanchez-Ramos J, Sanberg PR. Intravenous versus intrastriatal cord blood administration in a rodent model of stroke. J. Neurosci. Res. 2003;73:296–307. doi: 10.1002/jnr.10659. [DOI] [PubMed] [Google Scholar]
- Willing AE, Nowicki P, Poulos S, Lixian J, Milliken M, Cahill DW, Sanberg PR. Effects of middle cerebral artery occlusion on spontaneous activity and cognitive function in rats. International Journal of Neuroscience. 2002;112:503–516. doi: 10.1080/00207450290025617. [DOI] [PubMed] [Google Scholar]
- Xiao J, Nan Z, Motooka Y, Low WC. Transplantation of a novel cell line population of umbilical cord blood stem cells ameliorates neurological deficits associated with ischemic brain injury. Stem Cells Dev. 2005;14:722–733. doi: 10.1089/scd.2005.14.722. [DOI] [PubMed] [Google Scholar]
- Yang M, Wei X, Li J, Heine LA, Rosenwasser R, Iacovitti L. Changes in Host Blood Factors and Brain Glia Accompanying the Functional Recovery After Systemic Administration of Bone Marrow Stem Cells in Ischemic Stroke Rats. Cell Transplant. 2010;19:1073–1084. doi: 10.3727/096368910X503415. [DOI] [PubMed] [Google Scholar]