Abstract
Introduction
Body temperature measurement in children is of clinical relevance. Although rectal measurement is the gold standard, less invasive tools have become available. We aimed to describe the accuracy of tympanic, infrared skin, or temporal artery scan thermometers compared with rectal measurement to reflect core temperature.
Methods
Rectal (Filac 3000; Covidien, Mechelen, Belgium), tympanic (AccuSystem Genius2 Typmanic Infrared Ear Thermometer, Covidien, Mechelen, Belgium), temporal artery scan (Exergen, Exergen Corp, Watertown, Massachusetts), and infrared (ThermoFlash Contactless Medical Electronic Thermometer, Visiomedlab, Paris, France) body temperature measurements were randomly performed and readings were collected once. Temperature readings were described as median and range, and observations were compared with rectal temperature readings (using Wilcoxon, Bland-Altman, sensitivity, and specificity tests). The child’s comfort was assessed by the child, parent, and nurse (using Likert scales) and ease of use was assessed by nurses (using visual analog scale).
Results
Based on observations in 294 (median age = 3.2 years, range = 0.02–17 years) children, the mean difference was 0.49°C (tympanic scan; P < 0.0001), 0.34°C (infrared skin scan; P < 0.0001), and 0°C (temporal artery scan; P = 0.9288), respectively, when compared with rectal temperature readings. Based on visual inspection of Bland-Altman plots, all tools overestimated the temperature at lower body temperature and underestimated the temperature at higher body temperature, resulting in a sensitivity of 22% to 41% and a specificity of 98% to 100% for rectal temperatures above 38°C. The Likert scale scores and the visual analog scale scores for rectal measurement were only slightly higher when compared with the other methods.
Conclusions
All noninvasive techniques underperformed compared with rectal measurement. The temporal artery scan deviations were smallest, but all noninvasive techniques overestimate lower temperatures and underestimate higher temperatures compared with rectal measurement. In our hands, temporal artery scan measurement seems to be second best, but not yet ideal.
Key Words: Bland-Altman, body temperature, infrared skin scan, rectal, temporal artery scan, tympanic scan
Introduction
Medical decisions related to diagnosis, planning of investigations, or subsequent pharmacologic treatment in children are in part driven by body temperature measurement.1–3 In pediatrics, the gold-standard reference to measure core body temperature is by measurement of rectal temperature because this reflects central core temperature. Although this is considered to be the gold standard in many health care systems, it carries its own drawbacks. This includes discomfort, emotional distress, and—although very rare—possible complications such as perforation or transmission of micro-organisms. In a systematic review, axillary instead of rectal recordings resulted in a pooled difference of 0.85°C (−0.2°C to 1.9°C).4,5 In an attempt to avoid the disadvantages of rectal measurement, a range of alternative devices and less noninvasive methods have been introduced, including tympanic,6–11 infrared skin scan,6,12–15 and temporal artery scan16,17 temperature measurement.
A popular alternative for rectal measurement is the tympanic scan thermometer.6–11 This device measures the amount of infrared heat produced by the tympanic membrane of the ear by means of a sensor probe. The tympanic membrane shares its blood supply with the hypothalamus, the thermoregulatory center of the human body. However, this necessitates appropriate application and access to the tympanic membrane. Consequently, the probe needs to be positioned in the auditory external duct in the appropriate angle to the tympanic membrane, which makes it more difficult in young infants or in cases of suspected otitis media, but has indeed been very well validated in, for example, sedated patients or during anesthesia. The infrared skin thermometer is another tool to measure body temperature.6,12–15 A sensor probe measures the amount of infrared emitted heat. Consequently, temperature can be measured without direct contact with the child. Specific advantages of the no-touch technique relate to cross-infections or the possibility to measure without disrupting sleep. Finally, temporal artery scan techniques have been developed.16,17 Temperature is hereby registered by slow scanning the forehead in the temporal artery region and behind the ear by direct skin contact. The thermometer thereby measures the naturally emitted infrared heat form the temporal arterial supply.
Several comparative studies have been performed in either sedated patients9,12 or in specific pediatric subpopulations,9,10,14 commonly by comparing 2 devices.4–6,8,11,13,15–17 In contrast, investigator-driven studies that simultaneously compare different available assessment tools in a heterogeneous group of pediatric populations commonly admitted in a pediatric hospital is limited. In our study, we aimed to evaluate the accuracy and performance of 3 newer tools when compared with what is considered to be the gold standard; that is, rectal temperature measurement, within a real-life clinical setting. Besides the measurement, we also collected some subjective impressions about the child’s comfort (evaluated by the nurse, parent, and child) and the device-specific ease of use (evaluated by the nurse).
Methods
Ethics, enrollment, and clinical study
The study protocol (S 53071) was approved by the ethics board of University Hospitals, Leuven, Belgium. Pediatric patients admitted to different pediatric wards of University Hospitals were included in the study after informed consent of the patients and/or their legal representatives when body temperature assessment was scheduled.
The study protocol had the explicit aim to reflect a real-life assessment. Measurements were collected in every single patient in random order. Using an at-random approach, a rectal body temperature measurement device (Filac 3000; Covidien, Mechelen, Belgium), a tympanic scan thermometer (AccuSystem Genius2 Tympanic Infrared Ear Thermometer; Covidien, Mechelen, Belgium), an infrared skin scan thermometer (ThermoFlash Contactless Medical Electronic Thermometer; Visiomedlab, Paris, France), and a temporal artery scan thermometer (Exergen; Exergen Corp, Watertown, Massachusetts) were used. Measurements were collected consecutively at 1 single time point with a time interval to collect all readings of <5 minutes to avoid physiologic fluctuations.
Measurements were performed according to the product-specific instructions, and nurses were trained before the study on the appropriate use of the different devices. These trainings were formal teaching sessions explaining product-specific issues for appropriate and safe use of the different devices. The presentations and written handout documents were subsequently provided to the nurses and compliance was intermittently verified by a dedicated study nurse (I. van Gorp). Temperature readings in every individual patient were collected at 1 time point, every child was only included once, and device-specific readings were only performed once in every patient. To reflect the heterogeneous character of the study population, children were included at the emergency department, at the outpatient clinic, at the pediatric day surgery unit and on the medical wards.
In addition to the temperature readings, subjective impressions about the child’s comfort (as assessed by the nurse, parent, and child) and the ease of use (assessed by the nurse) were collected. These subjective impressions were quantified based on a Likert scale score (child’s comfort, assessed by the child, parent, and nurse, where 1–5 = very well, well, neutral, poor, and very poor comfort, respectively) or a visual analog scale (VAS) score (ease of use, assessed by the nurse, where 0–10=very good to very poor). The choice for different scores (Likert or VAS) for the assessments of the nurses was to stress the differences between both questions (child’s comfort vs ease of use). These data were collected immediately following temperature readings.
Data analysis and statistics
Temperature readings and Likert scale or VAS scores were reported by median and range. Temperature readings as collected with the different measurement tools were compared (using Wilcoxon test). Considering rectal temperature readings as the reference value, temperature readings were compared with this reference value (differences) and graphed according to the Bland-Altman method. Finally, sensitivity, specificity, positive predictive values, and negative predictive values to detect raised body temperature (37.8°C) and fever (38°C) were calculated based on the same rectal reference measurements. Statistics were analyzed using MedCalc (MedCalc Software, Ostend, Belgium), and P values <0.05 were considered significant.
Results
In total, 294 children with a median age of 3.2 years (range = 0.02–17 years) were included. Temperature readings as recorded for the different measurement tools are listed in Table I. Compared with rectal measurement, the mean differences were 0.49°C (tympanic scan P < 0.0001), 0.34°C (infrared skin scan P < 0.0001), and 0°C (temporal artery scan P = 0.9288), respectively.
Table I.
Temperature readings* and subjective evaluation by nurses, parents, and children related to the child’s comfort or ease of use.
| Temperature measurement device | Median | Range | |
|---|---|---|---|
| Rectal measurement | 37.1 | 35.1–39.5 | |
| Tympanic thermometer | 36.6 | 34.7–39.5 | |
| Infrared skin scan thermometer | 36.7 | 35.0–39.7 | |
| Temporal arterial scan thermometer | 37.1 | 35.6–39.8 | |
| Nurse | Parent | Child | |
| Subjective evaluation, child friendly† | |||
| Rectal measurement | 2 (0-5) | 2 (0-5) | 2 (0-5) |
| Tympanic thermometer | 1 (0-3) | 1 (0-5) | 1 (0-5) |
| Infrared skin scan thermometer | 1 (0-5) | 1 (0-5) | 1 (0-5) |
| Temporal arterial scan thermometer | 1 (0-5) | 1 (0-5) | 1 (0-5) |
| Subjective evaluation, ease of use‡ | |||
| Rectal measurement | 3 (0-7) | ||
| Tympanic thermometer | 2 (0-6) | ||
| Infrared skin scan thermometer | 1 (0-9) | ||
| Temporal arterial scan thermometer | 2 (0-6) |
Values are given in °C.
Based on Likert score of 0–5. Values are given as median (range).
Based on visual analog scale score of 0–10. Values are given as median (range).
Bland-Altman plots (Figures 1–3) confirm these mean differences and also illustrate the temperature-related influence on the magnitude and the direction of the difference between tympanic scan (Figure 1), infrared skin scan (Figure 2), and temporal artery scan (Figure 3), respectively, and the rectal reference value. All nonrectal measurement techniques resulted in a relatively higher result in the setting of a lower rectal body temperature (<37°C), and a relatively lower result in the setting of a higher rectal body temperature (>37.5°C). Thirty-three children showed a rectal body temperature above 37.8°C, of whom 22 had a body temperature above 38°C. Sensitivity, specificity, positive predictive value, and negative predictive value of the other measurement techniques compared with rectal measurement are provided in Table II.
Figure 1.
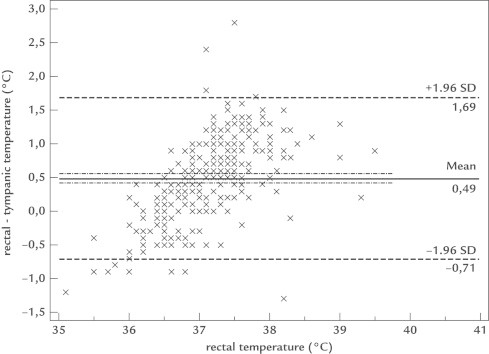
Bland-Altman plot illustrating a mean difference of 0.49°C, with a temperature-related influence on the direction and extent of the difference between rectal or tympanic scan temperature measurement.
Figure 2.
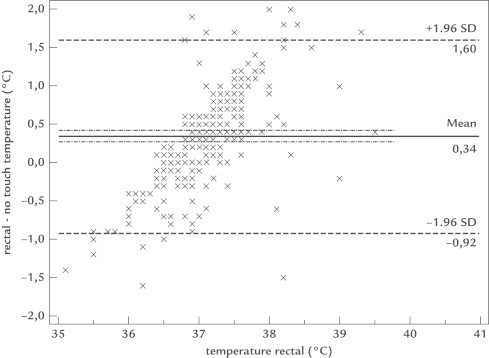
Bland-Altman plot illustrating a mean difference of 0.34°C, with a temperature-related influence on the direction and extent of the difference between rectal or infrared skin scan temperature measurement.
Figure 3.
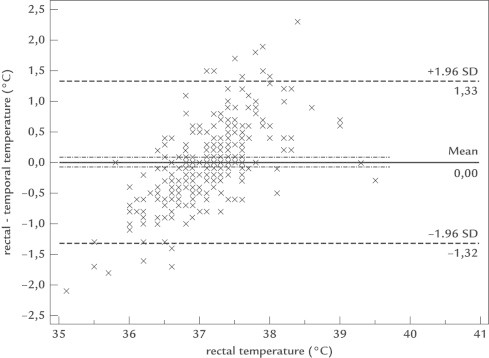
Bland-Altman plot illustrating a mean difference of 0°C, with a temperature-related influence on the direction and extent of the difference between rectal or temporal artery scan temperature measurement.
Table II.
Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of raised body temperature of thermometer types when compared with rectal measurement as reference.*
| Body temperature | Tympanic thermometer | Infrared skin scan thermometer | Temporal artery scan thermometer |
|---|---|---|---|
| Cut off value 37.8°C (n = 33/294) | |||
| Sensitivity | 18 | 18 | 34 |
| Specificity | 99.6 | 99.5 | 94 |
| PPV | 86 | 86 | 42 |
| NPV | 90 | 91 | 92 |
| Cut off value 38°C (n = 22/294) | |||
| Sensitivity | 22 | 27 | 41 |
| Specificity | 100 | 100 | 98 |
| PPV | 100 | 100 | 60 |
| NPV | 94 | 92 | 96 |
Values are given as %.
Table I also provides data on the subjective impression on the child’s comfort as assessed by nurse, parent, and child (Likert scale score) and the ease of use by the nurse (VAS score). Overall, there was good agreement between the different assessors, with a limited difference (median 2 vs median 1) between rectal measurement and the other techniques. Similar trends in differences were observed for ease of use as evaluated by the nurse.
Discussion
In a heterogeneous cohort of 294 children, we documented that the mean difference between tympanic scan, infrared skin scan, and temporal artery scan compared with rectal measurement was 0.49°C, 0.34°C, and 0°C, respectively. Compared with the rectal measurement device, all assessed tools overestimated body temperature at lower body temperature and underestimated at higher body temperature (Figures 1–3), resulting in sensitivity of 22% to 41% and a specificity of 98% to 100% for rectal temperature above 38°C.
A wide range of devices are available to exclude fever or to quantify body temperature in children. Although the multiplicity of modes and sites provides flexibility, it also introduces procedure or device-related variability. Such variability may be of clinical relevance (eg, predictive value to document the presence or absence of fever)1 or of pharmacodynamic relevance (eg, concentration time profile of acetaminophen for fever reduction).3,18 Based on our observations, none of the nonrectal measurement tools performed equal to the reference technique, although temporal artery scan was closest to this reference technique.
Our supportive findings in favor of temporal artery scan as second best confirms earlier observations in cohorts reported by Reynolds et al,16 Batra et al,7 Eyelade et al,9 and Bahorski et al.17 in 52, 100, 36, and 47 children, respectively. In essence, Reynolds et al16 concluded that mean (SD) temporal artery scan measurement (−0.46°C [0.5°C]), but not axillary (−0.93°C [0.49°C]) was sufficiently accurate when compared with rectal measurement in a cohort of 52 children.16 Unfortunately, this was only based on correlation studies; Bland-Altman analysis is obviously more appropriate to compare these measurements.16 More recently, Batra et al7 documented a similar mean difference and similar trends in differences in body temperature readings when rectal measurements were compared with either tympanic scan (0.5; 95% CI, −0.24°C to 1.37°C) or temporal artery scan measurement (0; 95% CI, −0.36°C to 0.3°C) in 100 children. There was a similar trend with an overestimation of noninvasive measurements in the setting of lower rectal temperature, and an underestimation in the setting of higher rectal temperature.7 In the Batra study,7 sensitivity and specificity for a rectal temperature above 38°C were 98% and 98% or 80% and 98% for tympanic scan and temporal artery scan thermometer measurement, respectively.7 Eyelade et al9 confirmed the same Bland-Altman pattern in 36 pediatric patients during general anesthesia: higher in the setting of low temperature and lower in the setting of high temperature before and during (30 and 60 minutes) anesthesia and mean differences of 0.29°C, 0.29°C, and 0.31°C when compared with rectal measurements.9 Finally, Bahorski et al17 reported on differences in rectal measurement versus temporal artery scan method in 47 pediatric patients and described a good correlation (0.86) and no significant difference between both measurements. Unfortunately, only correlations were reported and no Bland-Altman analysis had been performed.17 However, in patients with fever (>38°C; n = 22), temporal artery scan readings were lower in 18 out of 22 patients when compared with rectal measurement, confirming our observations on the affect of body temperature on the extent and direction of the difference (Figure 3).17
The underperformance of tympanic or infrared skin scan thermometers also confirms previous studies.6,8,13 In a recent meta-analysis by Dodd et al,8 the pooled estimates of sensitivity and specificity for tympanic scan thermometry were 63.7% (95% CI, 55.6%–71.8%) and 95.2% (95% CI, 93.5%–96.9%) for the diagnosis of fever (ie, 38°C) when compared with rectal temperature measurement. This means that tympanic scan thermometry would fail to diagnose fever in about one-third of cases.8 Paes et al6 conducted a similar study (rectal reference, tympanic and infrared skin, but no temporal artery scan thermometer in children). Based on observations in 100 children, similar differences (−0.27°C, 95% CI, −1.5°C to 1.05°C) of tympanic or infrared (Thermofocus, Varese, Italy) (−0.26°C, 95% CI, −1.75°C to 1.65°C) scan were documented.6 Sensitivity, specificity, positive predictive value, and negative predictive value for rectal fever (38°C) were 80%, 97%, 91%, and 94% for tympanic and 64%, 96%, 84%, and 89% for an infrared method.6 Finally, Selent et al13 compared 3 different infrared thermal skin detection systems (OptoTherm Thermoscreen, Sewickley, PA; FLIR ThermoVision 360, Boston, MA; and Thermofocus), and documented that sensitivity (compared with 38°C rectal) was between 77% and 84%; specificity was between 79% and 86%.
Although the number of studies that simultaneously compared different available assessment tools in a heterogeneous group of pediatric populations is limited, there were paired or specific subpopulation studies to compare with. In contrast, we were unable to retrieve data on how nurses, parents, and children evaluated these techniques. We found some differences between the different techniques, but the extent of these differences was overall more limited than initially anticipated, irrespective of who evaluated the intervention. Obviously, our study has its limitations. We a priori decided not to include axillary temperature measurement because there was already meta-analytical evidence on the differences when compared with rectal measurement.5 Secondly, the overall number of patients—although quite high when compared with other reported cohorts—could have been higher, or additional recruitment of cases with either fever (38°C)16 or hypothermia9 likely is of benefit to draw additional or firmer conclusions. Finally, the study design aimed to reflect a real-life assessment. This means that measurements were not limited to study nurses only but were performed by the clinical nurses, there was only 1 temperature reading for each device, and all temperature readings were collected at 1 time point with an aimed time interval of <5 minutes. Harmonization was aimed for based on formal training and verified based on intermittent compliance monitoring.
Taking these limitations into account, we documented that the mean difference between tympanic scan, infrared skin scan, and temporal artery scan compared with rectal measurement was 0.49°C, 0.34°C, and 0°C, respectively. All tools overestimated the temperature at lower and underestimated at higher body temperature, resulting in sensitivity of 22% to 41% and a specificity of 98% to 100% for rectal temperature above 38°C. This means that care providers should be aware of the limitations of nonrectal temperature measurement not yet reflected in the specific UK National Institute for Health and Care Excellence guideline on feverish illness in children.1,19 In a screening setting, sensitivity should be higher, whereas in a setting of consecutive measurement (eg, concentration-effect profiles as part of a pharmacologic study), the absolute values and the accuracy of the data will strongly depend on the tool applied. In our hands and based on our population, it seems that temporal artery scan measurement is second best but not optimal when compared with rectal measurement.
Conflicts of Interest
The authors have indicated that they have no conflicts of interest regarding the content of this article.
Acknowledgments
Karel Allegaert’s clinical research is supported by a fundamental clinical investigatorship award (No. 1800214N). The authors thank the parents and children for providing consent and collaboration, and the nurses for their contributions. All authors contributed to the design, the recruitment, the collection of results and the interpretation of the data. All authors contributed to the writing of the final paper.
References
- 1.Davis T. NICE guideline: feverish illness in children—assessment and initial management in children younger than 5 years. Arch Dis Child Educ Pract Ed. 2013;98:232–235. doi: 10.1136/archdischild-2013-304792. [DOI] [PubMed] [Google Scholar]
- 2.Walson P.D., Jones J., Chesney R. Antipyretic efficacy and tolerability of a single intravenous dose of the acetaminophen prodrug propacetamol in children: a randomized, double-blind, placebo-controlled trial. Clin Ther. 2006;28:762–769. doi: 10.1016/j.clinthera.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Allegaert K., van den Anker J. Pharmacokinetics and pharmacodynamics of intravenous acetaminophen in neonates. Expert Rev Clin Pharmacol. 2011;4:713–718. doi: 10.1586/ecp.11.50. [DOI] [PubMed] [Google Scholar]
- 4.Craig J.V., Lancaster G.A., Taylor S. Infrared ear thermometry compared with rectal thermometry in children: a systematic review. Lancet. 2002;360:603–609. doi: 10.1016/S0140-6736(02)09783-0. [DOI] [PubMed] [Google Scholar]
- 5.Craig J.V., Lancaster G.A., Williamson P.R. Temperature measured at the axilla compared with rectum in children and young people: a systematic review. BMJ. 2000;320:1174–1178. doi: 10.1136/bmj.320.7243.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paes B.F., Vermuelen K., Brohet R.M. Accuracy of tympanic and infrared skin thermometers in children. Arch Dis Child. 2010;95:974–978. doi: 10.1136/adc.2010.185801. [DOI] [PubMed] [Google Scholar]
- 7.Batra P., Goval S. Comparison of rectal, axillary, tympanic and temporal artery thermometer in the pediatric emergency room. Pediatr Emerg Care. 2013;29:63–66. doi: 10.1097/PEC.0b013e31827b5427. [DOI] [PubMed] [Google Scholar]
- 8.Dodd S.R., Lancaster G.A., Craig J.V. In a systematic review, infrared ear thermometry for fever diagnosis in children finds poor sensitivity. J Clin Epidemiol. 2006;59:354–357. doi: 10.1016/j.jclinepi.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Eyelade O.R., Orimadegun A.E., Akinyemi O.A. Esophageal, tympanic, rectal and skin temperatures in children undergoing surgery with general anesthesia. J Perianesth Nurs. 2011;26:151–159. doi: 10.1016/j.jopan.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Devrim I., Kara A., Ceyhan M. Measurement accuracy of fever by tympanic and axillary thermometry. Pediatr Emerg Care. 2007;23:16–19. doi: 10.1097/PEC.0b013e31802c61e6. [DOI] [PubMed] [Google Scholar]
- 11.Dew P.L. Is tympanic membrane thermometry the best method for recording temperature in children? J Child Health Care. 2006;10:96–110. doi: 10.1177/1367493506062550. [DOI] [PubMed] [Google Scholar]
- 12.Myny D., de Waele J., Defloor T. Temporal scanner thermometry: a new method of core temperature estimation in ICU patients. Scott Med J. 2005;50:15–18. doi: 10.1177/003693300505000106. [DOI] [PubMed] [Google Scholar]
- 13.Selent M.U., Molinari N.M., Baxter A. Mass screening for fever in children: a comparison of 3 infrared thermal detection systems. Pediatr Emerg Care. 2013;29:305–313. doi: 10.1097/PEC.0b013e3182854465. [DOI] [PubMed] [Google Scholar]
- 14.Fortuna E.L., Carney M.M., Macy M. Accuracy of non-contact infrared thermometry versus rectal thermometry in young children evaluated in the emergency department for fever. J Emerg Nurs. 2010;36:101–104. doi: 10.1016/j.jen.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Chiappini E., Sollai S., Longhi R. Performance of non-contact infrared thermometer for detecting febrile children in hospital and ambulatory settings. J Clin Nurs. 2011;20:1311–1318. doi: 10.1111/j.1365-2702.2010.03565.x. [DOI] [PubMed] [Google Scholar]
- 16.Reynolds M., Bonham L., Gueck M. Are temporal artery temperatures accurate enough to replace rectal temperature measurement in pediatric ED patients? J Emerg Nurs. 2012 Nov 8 doi: 10.1016/j.jen.2012.07.007. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Bahorski J., Repasky T., Ranner D. Temperature measurement in pediatrics: a comparison of the rectal method versus the temporal artery method. J Pediatr Nurs. 2012;27:243–247. doi: 10.1016/j.pedn.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 18.Hopchet L., Kulo A., Rayyan M. Does intravenous paracetamol administration affect body temperature in neonates? Arch Dis Child. 2011;96:301–304. doi: 10.1136/adc.2010.203778. [DOI] [PubMed] [Google Scholar]
- 19.Van den Anker J.N. Optimising the management of fever and pain in children. Int J Clin Pract Suppl. 2013:26–32. doi: 10.1111/ijcp.12056. [DOI] [PubMed] [Google Scholar]


