Abstract
INTRODUCTION
Currarino syndrome (CS) is characterized by the triad of anorectal malformations, sacral bone defects, and presacral mass in which an autosomal dominant inheritance has been described. The surgical community has a little no knowledge of CS in adults, apart from, perhaps, a small number of paediatric surgeons. Therefore, we sought to describe this unusual cause of anal fistula.
PRESENTATION OF CASE
A 55-year-old man was referred with an anal fistula. The patient was scheduled for drainage of multiple collections and an anal fistulectomy. Cytological results were confirmed that the cyst was dermoid (and non abscess). One month after surgery, the patient informs us of his CS. MRI was performed and it revealed an anterior sacral mass. It was to decide to realize an exeresis of this mass by coelioscopy. The patient experienced severely constipated and urinary retention. After therapy by Peristeen anal irrigation and self Intermittent catheterization (six times daily), there was a good improvement in symptoms.
DISCUSSION
This is an extremely rare case of CS revealed in an adult. MRI is a sensitive non-invasive diagnostic tool, and could be performed on any patient with long-standing anal fistula.
CONCLUSION
We recommend an early and multidisciplinary approach of CS is suspected in a patient. The surgeon must always be alert to the possibility of pelvic nerves injury during an exeresis of a retrorectal tumour fistulized.
Keywords: Currarino syndrome, Anal fistula, Sacrococcygeal agenesis, Presacral mass, Surgery, Genetic disease
1. Introduction
In most cases, Currarino syndrome is diagnosed in childhood, with most descriptions being found in paediatric literature. It is extremely uncommon for this syndrome to present in adulthood. We describe a man affected by Currarino syndrome who presented with an anal fistula. In over 80% of cases, presentation of Currarino syndrome occurs in infancy or childhood.1 Symptoms such as intractable constipation, urinary retention, incontinence and bowel obstruction in infancy are frequently associated with this presentation.2 There have been reports of the syndrome presenting in adulthood, although these reports are extremely rare. We wish to present this extremely rare case of Currarino syndrome, which is the first one that we have encountered in our practice, along with the accompanying diagnostic and therapeutic issues and a review of the literature.
2. Presentation of case
A 55-year-old man was referred with an anal fistula of the right lower quadrant. His medical history revealed surgery on a knee hygroma, a right inguinal hernia repair, a calcific tendonitis of the rectus femoris, a left capsulitis. There was no history of genitourinary problems. The patient smokes one packet of cigarettes per day and drinks three glasses of wine per day.
Proctology examination revealed a complex anal fistula. In the lithotomy position, this fistula is at the 6 o’clock position with multiple openings. Rectal examination revealed good sphincter tone. No masses were palpable. The rectal mucosa was normal. Colonoscopic examination shows a fistula without any lesion suggestive of ileocolic inflammatory disease. Multiple colonic biopsies were within normal limits with no evidence of inflammatory bowel disease or aganglionosis. MRI of the patient's pelvis and abdomen (Figs. 1 and 2) revealed a perianal fistula with multiple abscesses (grade 2). The MRI showed a left intersphincteric abscess cavity above the primary intersphincteric tract. The enteric entry point is suggested by the medial tract. The fistula is confined by the external sphincter and the ischiorectal fossa is unaffected. MRI also showed a partial sacral agenesis: only the first and second sacral vertebrae are preserved.
Fig. 1.
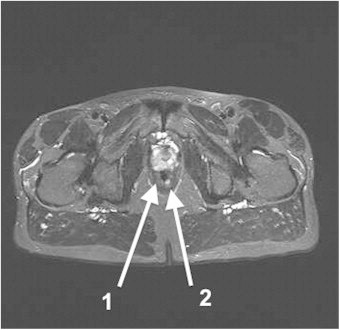
Pelvic MRI before surgery (axial view). (1) Rectum; (2) anal fistula.
Fig. 2.
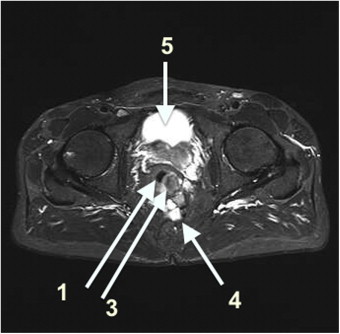
Pelvic MRI before surgery (axial view). (1) Rectum; (3) intramural collection; (4) presacral collection; (5) bladder.
The presumptive diagnosis was complex anal fistula with multiple abscesses. The patient was scheduled for drainage of multiple collections and an anal fistulectomy. We discovered a seborrheic liquid during draining the “abscess”. Cytological results were confirmed that the cyst was dermoid (and non abscess) due to the indication of lipid content. The postoperative period was uncomplicated.
One month after surgery, he experienced persistent fistula. By discussing with the patient about the presence of seborrheic material and not pus, he informs us of his Currarino syndrome. He did not have a severe form. The only symptom is constipation. This syndrome is discovered within the framework of assessment of disease Hirschsprung in him daughter at its birth. For that reason, MRI was performed and it revealed an anterior sacral mass. After a review of the literature, it was decided to realize an exeresis of this mass by coelioscopy. The patient underwent laparoscopy. A transabdominal approach was taken. A monobloc exeresis of the mass was performed without rectal resection despite the very inflammatory peripheral tissues. Microscopically, the cavity of the cyst was not composed of neurogenic elements (glial tissue or meningocele). Endodermal and ectodermal tissues were present in several sections. No malignant histological features were found. Histological results from the samples showed teratoma. Postoperatively, the patient presented with micturition difficulties. Urinary catheterisation has relieved the symptoms.
During the postoperative period, the patient experienced very dark watery diarrhoea what persuaded us that the surgery had been effective and had solved the problem of constipation as described in the literature. Laboratory analysis, including routine serum and urinalysis, coagulation studies and full autoimmune profiles, were all within the normal limits. His endocrine status was within the normal limits. Urinary retention did not respond to medical treatment, the patient underwent cystoscopy. The cystoscopy revealed a posterior extrinsic compression. Therefore a pelvis MRI was performed and it revealed a mega rectosigmoid. The rectum was markedly dilated and no obstructive lesion was identified (Fig. 3). It was therefore a diarrhoea by “overflow “and it was indeed severely constipated. Fearing a Hirschsprung's disease in this patient as described in paediatric cases, the patient underwent radiological investigation. Flexible sigmoidoscopy revealed a markedly distended rectum. The anorectal manometry revealed a lack of a normal recto anal inhibitory reflex consistent with Hirschsprung's disease or megarectum. Additional studies were then performed. The defecography and barium enema were not very informative. The radiologist felt that the mega rectosigmoid was suggestive of Hirschsprung's disease. Full-thickness rectal biopsies demonstrated multiple ganglion cells, suggesting that Hirschsprung's disease was not the correct diagnosis.
Fig. 3.
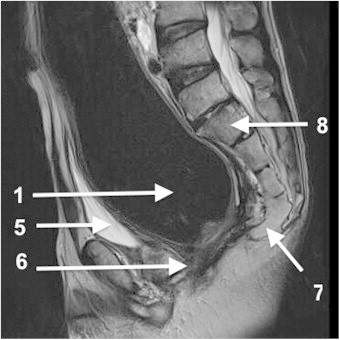
Pelvic MRI after surgery (sagittal view). (1) rectum; (5) bladder; (6) anorectal junction; (7) partial agenesis of the sacrum; (8) S1–S2–S3.
The case was discussed by the multidisciplinary surgical team who decided that biofeedback therapy should be performed. After biofeedback therapy, there was modest improvement in symptoms (constipation). Currently, we decided to pursue a conservative approach and monitor him in the outpatient clinic. The urodynamic tests confirmed nerve damage. After therapy by Peristeen anal irrigation and self Intermittent catheterization (six times daily), there was a good improvement in symptoms.
3. Discussion
In 1981, Currarino et al.3 described a rare congenital complex syndrome, which they named Currarino syndrome, characterized by a sacral bone defect, a congenital hindgut anomaly, and a presacral tumour. Recently, mutations of the HLXB9 gene in chromosome 7 (7q36) were identified as being responsible for Currarino syndrome.4 The phenotypical expression of the gene mutations causing the Currarino triad can vary from asymptomatic to patients presenting with the complete triad.5 Therefore, the number of patients with Currarino syndrome has been underestimated so far. About 50–60% of the reported cases have a family history of triad-associated anomalies.6 The presacral mass associated with the Currarino triad may be a teratoma, hamartoma, neuroenteric cyst, anterior meningocele or a combination of these four items.
A teratoma is a neoplasm originating from primordial germ cells and is derived from all three embryonal germ layers. Sacral agenesis is defined as the congenital absence of the whole or part of the sacrum.
Actually this syndrome could remain asymptomatic in many instances. The presacral mass may be accompanied by central neurological symptoms or local pressure symptoms (constipation, urinary incontinence, sacral anaesthesia, paraesthesia of the lower extremities, disturbance of anal sphincter control etc.). In our review, we did not discover any adults presenting with an anal fistula similar to our patient's. Therefore, we believe that this type of presentation in adults is extremely rare. Lynch and associates found that 16% of patients with Currarino syndrome presented with bowel obstruction in infancy.2 Thus, it is important to note that in our case, the patient claimed to have never had bowel obstruction or unusual weight loss. Patients with Currarino syndrome frequently present with other anomalies including urological disorders: congenital single kidney, hydronephrosis, urinary incontinence, vesicoureteric reflux, voiding dysfunction, duplex ureters and tethered cord.2
A long-lasting anal fistula could imply that there is an associated neural tube anomaly, such as anterior sacral teratoma. Magnetic resonance imaging is a specific and sensitive non-invasive diagnostic tool, and could be performed on any patient with long-standing anal fistula.
Proper treatment of Currarino syndrome varies according to the severity of the case. Decisions on treatment depend on two major aspects: the radiological findings and the neurological symptoms. Given our patient's age at presentation, the presence of an complex anal fistula and the apparent presence of external pressure from the mass, we considered that surgical resection of a presacral mass is indicated. Whatever its nature, surgical resection of a presacral mass is advisable. In our case, a transabdominal approach was taken because the tumour was far above sphincters and we were afraid of aggravating the anorectal malformation and the sacral agenesis by the Kraske procedure. However, when an anterior meningocele is present, a retroperitoneal approach is recommended: a sacral laminectomy or the Kraske procedure. The surgeon must always be alert to the possibility of a communication between the spinal canal and the tumour that could lead to severe neurological complications if not treated correctly.7 Some rare but confirmed cases have been published that document a malignant change to a teratoma.8
In summary, the key features in our patient included a partial agenesis of the sacrum, a presacral tumour (dermoid) and an anal fistula. The anal fistulation and the Currarino Syndrome are unrelated.
The surgeon must always be alert to the possibility of pelvic nerves injury during an exeresis of a retrorectal mass especially in this case: a fistulized tumour with péritumoral tissues very inflammatory The Kraske procedure is it better than surgical resection by transabdominal approach? The surgical community has little to no knowledge of Currarino syndrome in adults, apart from, perhaps, a small number of paediatric surgeons. Affected subjects are at risk of serious complications which lead to significant morbidity and mortality. We recommend an early and multidisciplinary approach if a patient is suspected of having Currarino syndrome. Even when the patient presents with no other symptoms, further examination might be required to exclude the Currarino triad in adults with a long-lasting anal fistula
Conflict of interest
No conflict of interests.
Funding
None.
Ethical approval
Informed consent was obtained from the patient in writing for the publication of this case report and the accompanying images. A copy of the written consent is available for review and can be obtained from the Editor-in-Chief of this journal on request.
Author contributions
Radwan Kassir has contributed in writing this paper.
David Kaczmarek has contributed in data collections.
References
- 1.Kochling J., Pistor G., Marzhauser Brands S., Nasir R., Lanksch W.R. The Currarino syndrome – hereditary transmitted syndrome of anorectal, sacral and presacral anomalies. Case report and review of the literature. Eur J Pediatr Surg. 1996;6:114–119. doi: 10.1055/s-2008-1066487. [DOI] [PubMed] [Google Scholar]
- 2.Lynch S.A., Wang Y., Strachan T., Burn J., Lindsay S. Autosomal dominant sacral agenesis: Currarino syndrome. J Med Genet. 2000;37:561–566. doi: 10.1136/jmg.37.8.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Currarino G., Coln D., Votteler T. Triad of anorectal, sacral, and presacral anomalies. AJR Am J Roentgenol. 1981;137:395–398. doi: 10.2214/ajr.137.2.395. [DOI] [PubMed] [Google Scholar]
- 4.Kochling J., Karbasiyan M., Reis A. Spectrum of mutations and genotypes–phenotype analysis in Currarino syndrome. Eur J Hum Genet. 2001;9:599–605. doi: 10.1038/sj.ejhg.5200683. [DOI] [PubMed] [Google Scholar]
- 5.Emans P.J., Kootstra G., Marcelis C.L., Beuls E.A., van Heurn L.W. The Currarino triad: the variable expression. J Pediatr Surg. 2005;40(August (8)):1238–1242. doi: 10.1016/j.jpedsurg.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 6.Gardner P.A., Albright A.L. Like mother, like son: hereditary anterior sacral meningocele. Case report and review of the literature. J Neurosurg. 2006;104(2 Suppl):138–142. doi: 10.3171/ped.2006.104.2.11. [DOI] [PubMed] [Google Scholar]
- 7.Crétolle C., Zérah M., Jaubert F., Sarnacki S., Révillon Y., Lyonnet S., Nihoul-Fékété C. New clinical and therapeutic perspectives in Currarino syndrome (study of 29 cases) J Pediatr Surg. 2006;41:126–131. doi: 10.1016/j.jpedsurg.2005.10.053. [DOI] [PubMed] [Google Scholar]
- 8.Yates V.D., Wilroy R.S., Whitington L., Simmons J.C.H. Anterior sacral defects: an autosomal dominantly inherited condition. J Pediatr. 1983;102:239–242. doi: 10.1016/s0022-3476(83)80528-9. [DOI] [PubMed] [Google Scholar]


