Abstract
Background:
Glaucomatous Optic Neuropathy (GON) is very common in the glaucoma patients, and impaired effect of glaucoma is measured by the Retinal Nerve Fiber Layer (RNFL) thickness.
Objective:
The study was conducted to find out the mean RNFL thickness, RNFL thickness in different quadrants, Intra-Ocular Pressure (IOP) changes, and visual field changes after filtration surgery in different ages and genders using Optical Coherence Tomography (OCT).
Materials and Methods:
The study was an interventional case-series conducted at the Glaucoma Clinic at the Regional Institute of Ophthalmology at Kolkata from March 2009 to August 2010. Fifty-one eyes of 43 open angle glaucoma patients had been selected for clinical and ophthalmologic evaluation. All the eyes of glaucoma patients who fulfilled the inclusion criteria were registered in the study population. The glaucoma filtration surgery was done in these patients. The RNFL thickness, IOP, visual field changes were measured before and after intervention of filtration surgery. Pre-operative OCT images of RNFL were obtained 0 to 120 days before surgery, and post-operative images were obtained from 60 to 120 days after surgery. Data collected in a standard data collection form included schedule.
Results:
Paired t-test was used. RNFL thickness was (pre-operative: 52.56 ± 17.40, post-operative: 58.48 ± 20.20, P < 0.0001) significantly increased after filtration surgery measured by OCT with significant reduction of IOP (r = - 0.38, P = 0.005) irrespective of age and gender.
Conclusions:
An increase in RNFL thickness was observed after glaucoma filtration surgery that correlated with IOP reduction.
Keywords: Glaucomatous optic neuropathy, optical coherence tomography, retinal nerve fiber layer thickness
Introduction
Glaucoma is a progressive optic neuropathy with characteristic appearance of the optic disc and specific pattern of visual field defect that is associated frequently but not invariably with raised intraocular pressure. As the visual loss is silent, sustained, and often symptomless, it goes unnoticed, undetected, and undiagnosed in many cases. Glaucoma accounts for 12.3 percent of blindness worldwide.[1]
Glaucoma accounts for 7.9 percent of total blindness in India.[2] Primary open angle glaucoma is generally bilateral, but not always symmetric disease characterized by adult onset, IOP >21 mm of Hg, an open angle of normal appearance, glaucomatous optic nerve head changes, and loss of visual field. The most important risk factor for glaucoma is raised intraocular pressure, and other risk factors are advanced age, black race, positive family history, myopia, corneal thickness. The normal range of IOP is 16-21 mm of Hg. Glaucoma is an optic neuropathy characterized by loss of retinal ganglion cells and their axons. Loss of retinal nerve fiber layer precedes measured optic nerve head changes, and visual field damage was observed in 60 percent of eyes approximately six years before any detectable visual field loss in glaucoma. Detection of optic nerve head and retinal nerve fiber layer damage is, therefore, crucial for the early diagnosis and management of glaucoma.[3]
With the above background in mind, this study was conducted to assess changes in Retinal Nerve Fiber Layer (RNFL) thickness, macular thickness, and IOP after filtration surgery.
Materials and Methods
This prospective study was conducted to evaluate the patients at the Glaucoma Clinic at the Regional Institute of Ophthalmology at Kolkata during March 2009 to August 2010. The patients were counseled and informed. Before going through ocular examination, a detailed history was taken. Personal interview was conducted to determine exposure to the risk factors of glaucoma like family history of glaucoma, ocular trauma, past eye surgery, past treatment for glaucoma. History was taken, and general checkup was done to rule out diabetes, anemia, and hypertension. The visual acuity of each eye, both with and without corrections, was noted. Refraction was carried out manually using streak retinoscope followed by subjective corrections. Anterior segment was examined both by diffuse light and slit-lamp. The subjects enrolled in this study were glaucoma patients who underwent filtration surgery. Place of study: Regional Institute of Ophthalmology (RIO) associated with Medical College, Kolkata. Institutional Review Board provided permission to conduct the study. Study population was eyes of patients who attended at out-patient department and Glaucoma Clinic, Regional Institute of Ophthalmology, Kolkata.
Sample design: Established glaucoma patients, who attended the Institute during the study period and were fit for filtration surgery, were taken in the study census population. Inclusion Criteria: All subjects undergone full clinical ophthalmologic evaluation including Snellens chart visual acuity testing, intraocular pressure measurement, slit lamp stereo-bio-microscopy etc., fulfilling the criteria of operability with consent were included. Exclusion Criteria: The patients with extreme age, very sick, unwilling to follow-up examination, failed to provide consent, patients having diabetic retinopathy, age-related macular degeneration, cystoid macular edema, macular dystrophy, central serous retinopathy, patients having advanced cataract, ocular pathology, which can affect visual field, and retinal nerve fiber thickness other than glaucoma were not included in the study.
Case definitions: Diagnosis of glaucoma was based on glaucomatous visual field loss with accompanying optic nerve head abnormality. OCT scan had been obtained 0 to 4 months before and 2 to 4 months after trabeculectomy.
Study design: Prospective, interventional case-series.
Study variables: (a) IOP before and after Glaucoma Surgery, (b) Visual field, (c) Mean Retinal Nerve Fiber Layer (RNFL) thickness from 0-4 months before and 2-4 months after filtration surgery and associated intraocular pressure changes in mm of Hg.
Study tools: Retinoscope, Snellens chart, Gonioscope, direct and indirect Ophthalmoscope, Slit lamp stereo-bio-microscopy by 78D, Goldman Applanation Tonometer, Automated perimeter (Humphrey Field Analyzer II), and Stratus Optical Coherence Tomography (Carl.Ziess-Stratus OCT).
Slit-lamp examination
Detailed examination was done to note the status of conjunctiva, cornea, anterior Chamber, iris, and lens. Any atrophic patch on the iris and signs of exfoliation were noted. Pupillary reaction was noted. The depth of the anterior chamber was assessed by van Herrick method.
Tonometry
The cornea was anesthetized using 0.5 percent proparacaine eye drop. The tear film was stained with sodium fluorescein 2%, and IOP was then measured using an Applanation Tonometer (“Goldmann” model, Haag-Streit, Bern, Switzerland). The IOP was measured three times in quick succession in each eye, and the IOP was taken as the mean of the three readings.
Gonioscopy
Gonioscopy was performed in a routine manner using the Goldmann two-mirror Gonioscope. Gonioscopy was done with adequate illumination with the patient looking straight ahead; special care was taken to ensure that the slit beam did not encroach upon the pupillary area during this procedure. Next, the patient was instructed to look in the direction of the mirror and the angle manipulated open to look for synechiae. If this procedure was unsuccessful or with a doubt about the presence of synechiae, indentation gonioscopy would have been performed using a Sussman four-mirror lens. Drainage angles were graded according to Shaffer's and Spaeth grading.[4] Evidence of angle recession and angle neo-vascularization, any abnormality was carefully noted.
Fundus Examination
Optic disc was examined after dilating each pupil with one drop of a mixture of tropicamide 0.8% and phenylephrine 5%. A + 90D lens (volk) was used at the slit lamp for optic disc biomicroscopy. A ratio of the longest vertical diameter of the cup to the longest vertical diameter of the disc was estimated as the vertical-cup/disc-ratio (VCDR) for each eye.[5] Any asymmetry of the VCDRs (0.2 or more) between two eyes, narrowing of the neuro-retinal rim, any notching at the cup margin, laminar dot sign, vessel overpass, saucerization of the cup, loss of nerve fiber layer, disc pallor, and hemorrhages were noted. Peripapillary atrophy, nasal displacement of the vessels, narrowing of the peripapillary retinal vessels, and baring of the circumlunar vessels were carefully looked for. Disc pallor and disc hemorrhage were noted. A red free light was used to look for any nerve fiber layer defect. Fundus photography (Topcon Retinal camera TRC-50XT) was done routinely, except in subjects where dense cataractous changes prevented visualization of the disc.
Filtration surgery
Filtration surgery which was performed in this study was trabeculectomy, or TRAB- a piece of tissue in the drainage angle of the eye is removed, creating an opening.
Visual field examination
An automated visual field (Humphrey Field Analyzer 30-2 program) analysis was scheduled on the following indications: Intraocular pressure (IOP) >21 mm of Hg, VCDR ≥0.7 in either eye, difference in VCDR >0.2 between the two eyes and/or the presence of glaucomatous features. Unreliable fields[6,7] were repeated during another session. If an advanced field defect precluded a successful 30-2 examination, the macular program or a 10-2 program was used. Field defects considered suggestive of glaucoma included isolated paracentral scotoma, nasal steps of Roenne, Siedel's scotoma, altitudinal defect, temporal wedge, generalized depression of field, arcuate scotoma, and advanced constriction of fields.
Optical coherence tomography:
RNFL thickness around optic disc was determined by OCT 3000 (V4.2.4 Zeiss-Humphrey, Dublin, California, USA). Three circular scans each 3.4 mm diameter centered on optic disc were obtained after full pupillary dilatation, and these measures were averaged by fast RNFL thickness 3.4 programs. The OCT lens was adjusted for the patient's refractive error. The subject was then instructed to fix with the eye being measured on the internal fixation target to bring the optic nerve head with in view of the examiner real time. The Z offset was adjusted to bring the OCT image into view. Polarization was optimized to maximize the reflective signal. The position of the aiming circle was adjusted to match the optic nerve head so that the nerve head scan would acquire an OCT image of an even radius of 1.73 mm around the optic nerve head. Scan quality was monitored by constantly assessing the color coding of the scans, paying particular attention to maximizing the red reflectivity of the retinal pigment epithelial cell layer. The software version used at the time of this study had signal strength of the image 7-10 to set high accuracy image. Three sets of standard scan RNFL measurements were made in quick succession. Each of this scans consisted of 512 A-scan measurements taken in a single circular path around the optic disc with a standard diameter of 3.4 mm in 1.28 sec. The fast scan was obtained; this consists of three successive circular sub-scans around the disc with A-scan measurements at 256 locations per revolution, over a total of 1.92 sec. Although these three scans can be examined separately for research or quality control purposes, they are usually simply averaged to report the thicknesses as a combined set of 768 A-scans in a circle of 3.4 mm diameter around the disc. The testing was supplemented with at least three separate fast scans (each consisting of three circular sub scans) to assess within-session variability of fast scan measurements. For both the fast and standard scan protocols, the subject was repositioned between the scan measurements only when necessary. There was no specific attempt to reposition the subjects between scans done during the same session. The RNFL analysis used an automated computer algorithm to identify the anterior and posterior margins of the band of reflectance representing the RNFL, making the margins with white lines in the visual display. The distance between the margins made up the RNFL thickness. The analysis algorithm reported 17 RNFL thickness values: Mean RNFL thickness around the entire circumference, average thickness within the 4 quadrants (temporal, superior, nasal, inferior), and average thickness in each of 12 clock-hour sectors.[8]
Statistical Analysis: Paired t tests were used to analyze NFL thickness differences on an individual eye basis and to compare findings before and after surgery. Pearson's correlation was used to evaluate the relations between parameters. All analyses were performed with SPSS software (version 17), and P < 0.05 were considered to be statistically significant.
Results
This prospective study was conducted to evaluate 51 eyes of 43 glaucoma patients. Number of male and female patients was 23 (53%) and 20 (47%), respectively, with ratio of male and female 23: 20. Mean age of the patient was 53.93 ± 13.92 years.
In the current study, more scientific, accurate, and reproducible measurement of both pre-operative and post-operative RNFL thickness loss along with ONH (Optic Nerve Head) damage was done by OCT. It had been documented that only arcuate nerve fiber were damaged in early glaucoma and nerve fibers in all quadrants were damaged in advanced glaucoma.
The RNFL thickness changes among the patients of pre-operative and post-operative glaucoma (52.56 ± 17.40 and 58.48 ± 20.20, respectively) cases were statistically significant. The RNFL thickness changes were also significant between male and female patients.
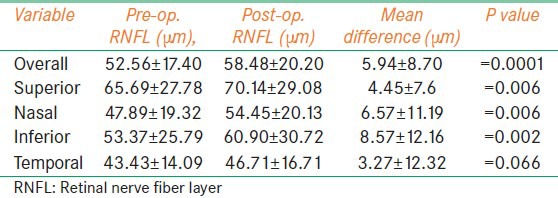
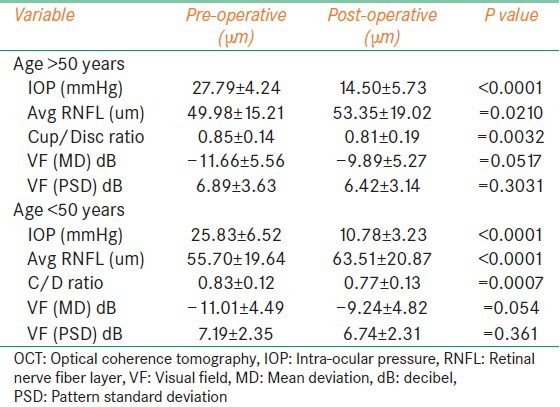
There was an increased RNFL thickness (superior quadrant: 4.45 ± 7.61 μm, nasal quadrant 6.57 ± 11.19 μm, inferior quadrant 7.57 ± 12.16 μm, and temporal quadrant 3.27 ± 12.32 μm) in all quadrants, but more changes were found in nasal quadrant. The improvement was confined to the nasal quadrant and the adjacent RNFL thickness because this area might be least affected by the disease. A significant increase in the RNFL thickness was found in both age groups with significant reduction of intraocular pressure. Both pre-operative and post-operative reliable Visual Field (VF) tests were taken, 36 of the 51 eyes participating in the study. The mean deviation was statistically significant (P = 0.0052). But, pattern standard deviation (PSD) was not statistically significant (P = 0.1600). It has been found that, RNFL thickness changes were more in younger group than in older people. This change might be due to resistance developed to further damage with reduced IOP.
Mean pre-operative IOP (mm of Hg) was 26.90 ± 6.38, and mean post-operative IOP (mm of Hg) was found 12.82 ± 5.08. This was significantly different (P < 0.0001).
The significant correlations between mean RNFL thickness changes and age and mean IOP were found. Using linear regression, the mean RNFL was thicker by 0.42 μm with each mmHg of IOP decrease after surgery.
Some post-operative complications encountered included shallow anterior chamber (4%), choroidal effusion (2%), and post-operative hyphema (4%).
The visual acuity was 6/12 (Snellen's chart) or better in 17 (33%) eyes preoperatively and in 29 (57%) eyes postoperatively among the 51 eyes.
Similarly, it was worse than 6/12 (Snellen's chart) in 34 (67%) eyes preoperatively and in 22 (43%) eyes postoperatively among the 51 eyes. The visual acuity was statistically significant (P = 0.0014). The visual acuity in pre- and post-operative patients in Log Mar scale is 0.5239 ± 0.3197 and 0.4023 ± 0.3770, respectively.
The reliable VF tests were taken for 36 eyes among the 51 eyes pre- and post-operatively.
The pre-operative mean deviation (MD) ± standard deviation (SD) and PSD ± SD were -11.36 ± 5.02 dB and 7.03 ± 3.05 dB, respectively. The post-operative MD ± SD and PSD ± SD were -9.58 ± 4.99 dB and 6.58 ± 2.75 dB, respectively.
The visual field (MD) changes were statistically significant (P = 0.0052). But, the visual field (PSD) was not statistically significant (P = 0.1600).
Mean pre-operative RNFL thickness (μm) was found 52.56 ± 17.40, and mean post-operative RNFL thickness (μm) was found 58.48 ± 20.20, and the difference was statistically significant (P < 0.0001).
The peripapillary RNFL thickness was significantly increased in this study as determined by OCT after glaucoma filtration surgery. The RNFL thickness was significantly increased for the overall measurement and in all quadrants. The mean RNFL thickness was increased in 39 (76%) eyes among the 51 eyes (mean increase 9.17 ± 7.72 μm), and the mean RNFL thickness was decreased in 12 (24%) among the 51 eyes (mean decrease 4.66 ± 3.01 μm). The correlation was found between intraocular pressure and retinal nerve fiber thickness changes (r = - 0.38, P = 0.005).
The RNFL thickness was increased in the superior quadrant of 31 (61%) eyes (4.45 ± 7.61 μm), in the nasal quadrant of 35 (69%) eyes (6.57 ± 11.19 μm), in the inferior quadrant of 29 (57%) eyes (7.57 ± 12.16 μm), and in the temporal quadrant of 28 (54.9%) eyes (3.27 ± 12.32 μm). The RNFL thickness changes were statistically significant in overall as well as in different quadrants after filtration surgery. The RNFL thickness was increased more in nasal quadrant in comparison to other quadrants [Table 1].
Table 1.
RNFL Thickness in different quadrants before and after filtration surgery
The RNFL thickness was significantly increased in both the age groups with significant reduction of intraocular pressure. The mean IOP changes were from 27.79 ± 4.24 mmHg to 14.50 ± 5.73 mmHg (P < 0.0001), and the mean RNFL changes were 49.98 ± 15.21 μm to 53.35 ± 19.02 μm, respectively, (P = 0.0210) in pre- and post-operative patients aged >50 years. For each mmHg reduction of IOP, RNFL thickness increased 0.25 μm.
Similarly, in the patients aged <50 years, the mean IOP changes were from 25.83 ± 6.52 mmHg to 10.78 ± 3.23 mmHg (P < 0.0001) and the mean RNFL changes were from 55.70 ± 19.64 μm to 63.51 ± 20.87 μm (P < 0.0001). For each mmHg of IOP reduction, the RNFL thickness increased by 0.52. Significant optic nerve head and visual field (MD) changes were seen without significant pattern standard deviation (PSD) changes in both the age groups.
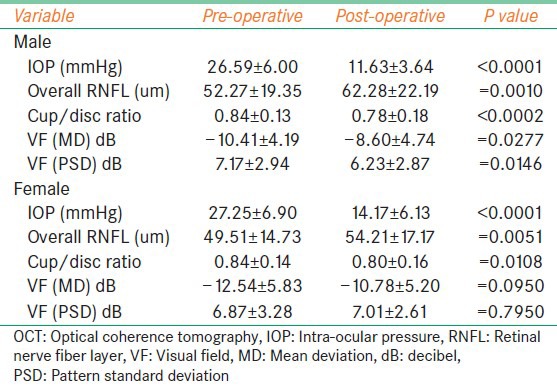
In comparison to older age group, RNFL thickness changes were found more in favor of younger group [Table 2]. The significant RNFL thickness changes were found in both male (P < 0.001) and female (P = 0.0051) patients with IOP changes. Average age of the male and female patients was 50.62 ± 15.65 yrs. and 57.70 ± 10.81 yrs., respectively.
Table 2.
RNFL thickness as measured by OCT according to age
The RNFL thickness was significantly increased in both male and female patients with significant reduction of intraocular pressure. The mean IOP changes were from 26.59 ± 6.00 mmHg to 11.63 ± 3.64 mmHg (P < 0.0001), and the mean RNFL thickness changes were from 52.27 ± 19.35 μm to 62.28 ± 22.19 μm (P = 0.0010) in pre- and post-operative male patients, respectively. With each mmHg reduction of IOP, RNFL thickness increased by 0.49 μm and also significant optic nerve head, visual field (mean deviation), and PSD changes were seen.
Similarly, in female patients, the mean IOP changes were from 27.25 ± 6.90 mmHg to 14.17 ± 6.13 mmHg (P < 0.0001) and the mean RNFL thickness changes were from 49.51 ± 14.73 μm to 54.21 ± 17.17 μm (P = 0.0051). With each mm of Hg of IOP reduction, the RNFL thickness increased by 0.35 μm. There was significant mean RNFL, optic nerve head, visual field (mean deviation) changes seen, except PSD in spite of significant reduction of intraocular pressure [Table 3].
Table 3.
RNFL Thickness as measured by OCT according to gender
Discussion
This study evaluated the RNFL thickness changes, as measured by OCT, after filtration surgery. The OCT scans in this study were performed with a prototype device. A strong correlation between RNFL measurements before and after operation was obtained by a prototype OCT 3000. Three circular scans each 3.4 mm diameter centered on optic disc.
Sogano et al.[9] found a significant decrease in cup volume and an increase in rim area 2 to 6 months after glaucoma surgery. No statistically significant change was observed in that study in relative RNFL height; however, the authors reported that relative RNFL height increased in 7 of 12 eyes, in which IOP was markedly reduced, and the changes in RNFL height were shown by linear regression analysis to be pressure-dependent. In the present study, significant optic disc changes were found in overall, different age groups and male and female patients 2 to 4 month after filtration surgery. There was also significant RNFL thickness changes found with significant reduction of IOP.
Irak et al.[10] found a significant decrease in mean cup area, cup volume, and cup-to-disc area ratio, as well as a significant increase in mean rim area and rim volume after 3 months after filtration surgery, and no significant change was found in RNFL cross-sectional area, but the change was significantly associated (P < 0.01) with the change in IOP.
Lesk et al.[11] reported similar results with the Confocal Scanning Laser Ophthalmoscope (CSLO) evaluation in 17 glaucoma patients 6 months after surgery; however, the correlation with the IOP change did not reach significance.
Kotecha et al.[12] found a significant increase in rim area and rim volume at 2 years after surgery. Segmental analysis showed a significant change in rim volume in the nasal, inferonasal, superonasal, and superotemporal sectors. A significant correlation was reported between changes in the optic disc parameters and reduction of IOP. In comparison to their study, the present study showed significant optic disc changes, which were found in all quadrants but more in nasal followed by inferior quadrant. There was no significant correlation found between mean RNFL thickness and optic nerve head changes (r = - 0.52: P = 7.91).
Topouzis et al.[13] did not find any significant changes in optic nerve head (ONH) parameters 8 months after surgery. This result might be due to the high degree of pre-existing glaucomatous damage (MD, -13.2 dB), because experimental studies[14,15,16] have shown that reversal of damage is more likely to occur in earlier stages of glaucoma.
The physiologic basis of the improvement in ONH appearance and RNFL thickness with IOP reduction is not clear. It has been suggested that IOP reduction results in less posterior bowing of the lamina cribrosa.[17,18] This theory may explain changes in ONH parameters, such as the decrease in cup volume and cup area and the increase in rim volume and rim area. The clinical implications of the ONH topography and RNFL thickness improvement are unclear, although previous studies have shown that there may be an associated improvement of visual function that corresponds to this improvement.[19,20,21,22] and similar findings have been reported by Lesk et al.[11] However, this study noted a significant change in the mean visual field (mean deviation) (P = 0.0052) but did not find mean visual field (pattern standard deviation) after surgery (P = 0.1600).
Ali Aydin et al.[23] found a significant increase in overall mean retinal nerve fiber thickness after surgery (P < 0.0001). Segmental analysis found a significant increase in RNFL thickness in the nasal, superior, and temporal quadrants. Twenty-eight (73.7%) of 38 eyes had an IOP reduction >30%. The mean RNFL thickness increase (0.5 microns/mmHg decrease of IOP) was significantly correlated with the IOP reduction (r = -0.41; P = 0.03). No correlation was found between RNFL thickness changes and age, pre-operative visual field global indices or post-operative change in visual field global indices. Similar changes regarding overall mean RNFL thickness and with segmental analysis found significant increase in inferior quadrant (P = 0.0020) in the present study. Significant correlation was found between RNFL thickness changes and age visual field (MD and PSD) indices.
Chang et al.[24] studied 21 eyes of 21 glaucoma patients who underwent medical or surgical intervention to lower IOP. There was no significant change in the overall RNFL thickness associated with the lowering of IOP (1.02 ± 10.3 μm, P = 0.653). Quadrant analysis did not show any significant change in the RNFL thickness of any of the four quadrants. This might be due to intervention variation in his study.
Raghu et al.[25] studied 17 glaucoma patients who underwent trabeculectomy to lower IOP. There was significant increase in average (P = 0.019), and inferior RNFL (P = 0.038) thickness was observed 1 week after surgery, but no significant change was found in other ONH parameters. The present study showed significant RNFL thickness changes as well as significant optic disc changes, which were found in all quadrants but more in nasal followed by inferior quadrant.
Conclusion
The study showed an increase in RNFL thickness after glaucoma filtration surgery that was correlated with IOP reduction, ages, and gender. The improvement is yet to be evaluated whether these changes have any clinical significance in long-term follow-up.
Strengths of the study: Quantitative measures were done in this study.
Limitations of the study: Large sample size, subsequent follow up, and long-term study was essential to assess clinical significance of changes. More elderly patients and advanced glaucomatous damage of patients were included in this study, and this hinders the generalization in a specific group of patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairement in the year 2002. Bull World Health Organ. 2004;82:844–51. [PMC free article] [PubMed] [Google Scholar]
- 2.National Survey on Blindness and Visual Outcome after Cataract Surgery 2001.-2002 report NPCB, DGHS, MOHFW, GOI [Google Scholar]
- 3.Robert Stamper, Mrc F Lieberman, Michael V Drake. Becker-Shaffer's Diagnosis and Therapy of Glaucoma. 1999;1:4–8. [Google Scholar]
- 4.Clemmensen V. Problems in gonioscopic screening in Greenland. Technique, classification of findings and diagnosis. Acta Ophthalmol. 1971;49:59–64. [PubMed] [Google Scholar]
- 5.Garway-Heath DF. Optic disc assessment in primary open angle glaucoma. Community Eye Health. 1996;9:25–8. [Google Scholar]
- 6.Sommer A, Enger C, Witt K. Screening for glaucomatous visual field loss with automated threshold perimetry. Am J Ophthalmol. 1987;103:681–4. doi: 10.1016/s0002-9394(14)74329-6. [DOI] [PubMed] [Google Scholar]
- 7.Katz J, Sommer A. Screening for glaucomatous visual field loss: The effect of patient reliability. Ophthalmology. 1990;97:1032–7. doi: 10.1016/s0161-6420(90)32467-3. [DOI] [PubMed] [Google Scholar]
- 8.Klein BE, Klein R, Sponsel WE, Franke T, Cantor LB, Martone J, et al. Prevalence of glaucoma. The Beaver Dam Eye Study. Ophthalmology. 1992;99:1499–504. doi: 10.1016/s0161-6420(92)31774-9. [DOI] [PubMed] [Google Scholar]
- 9.Sogano S, Tomita G, Kitazawa Y. Changes in retinal nerve fiber layer thickness after reduction of intraocular pressure in chronic open-angle glaucoma. Ophthalmology. 1993;100:1253–8. doi: 10.1016/s0161-6420(93)31497-1. [DOI] [PubMed] [Google Scholar]
- 10.Irak I, Zangwill L, Garden V, Shakiba S, Weinreb RN. Change in optic disk topography after trabeculectomy. Am J Ophthalmol. 1996;122:690–5. doi: 10.1016/s0002-9394(14)70488-x. [DOI] [PubMed] [Google Scholar]
- 11.Lesk MR, Spaeth GL, Azuara-Blanco A, Araujo SV, Katz LJ, Terebuh AK, et al. Reversal of optic disc cupping after glaucoma surgery analyzed with a scanning laser tomograph. Ophthalmology. 1999;106:1013–8. doi: 10.1016/S0161-6420(99)00526-6. [DOI] [PubMed] [Google Scholar]
- 12.Kotecha A, Siriwardena D, Fitzke FW, Hitchings RA, Khaw PT. Optic disc changes following trabeculectomy: Longitudinal and localisation of change. Br J Ophthalmol. 2001;85:956–61. doi: 10.1136/bjo.85.8.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Topouzis F, Peng F, Kotas-Neumann R, Garcia R, Sanguinet J, Yu F, et al. Longitudinal changes in optic disc topography of adult patients after trabeculectomy. Ophthalmology. 1999;106:1147–51. doi: 10.1016/S0161-6420(99)90248-8. [DOI] [PubMed] [Google Scholar]
- 14.Shirakashi M, Nanba K, Iwata K. Reversal of cupping in experimental glaucoma. Ophthalmologica. 1991;202:194–201. doi: 10.1159/000310198. [DOI] [PubMed] [Google Scholar]
- 15.Shirakashi M, Nanba K, Iwata K. Changes of reversal of cupping in experimental glaucoma. Longitudinal study. Ophthalmology. 1992;99:1104–10. doi: 10.1016/s0161-6420(92)31844-5. [DOI] [PubMed] [Google Scholar]
- 16.Coleman AL, Quigley HA, Vitale S, Dunkelberger G. Displacement of the optic nerve head by acute changes in intraocular pressure in monkey eyes. Ophthalmology. 1991;98:35–40. doi: 10.1016/s0161-6420(91)32345-5. [DOI] [PubMed] [Google Scholar]
- 17.Quigley HA. The pathogenesis of reversible cupping in congenital glaucoma. Am J Ophthalmol. 1977;84:358–70. doi: 10.1016/0002-9394(77)90680-8. [DOI] [PubMed] [Google Scholar]
- 18.Albon J, Purslow PP, Karwatowski WS, Easty DL. Age related compliance of the lamina cribrosa in human eyes. Br J Ophthalmol. 2000;84:318–23. doi: 10.1136/bjo.84.3.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katz LJ, Spaeth GL, Cantor LB, Poryzees EM, Steinmann WC. Reversible optic disk cupping and visual field improvement in adults with glaucoma. Am J Ophthalmol. 1989;107:485–92. doi: 10.1016/0002-9394(89)90492-3. [DOI] [PubMed] [Google Scholar]
- 20.Tsai CS, Shin DH, Wan JY, Zeiter JH. Visual field global indices in patients with reversal of glaucomatous cupping after intraocular pressure reduction. Ophthalmology. 1991;98:1412–9. doi: 10.1016/s0161-6420(91)32118-3. [DOI] [PubMed] [Google Scholar]
- 21.Spaeth GL. The effect of change in intraocular pressure on the natural history of glaucoma: Lowering intraocular pressure in glaucoma can result in improvement of visual fields. Trans Ophthalmol Soc U K. 1985;104:256–64. [PubMed] [Google Scholar]
- 22.Yildirim E, Bilge AH, Ilker S. Improvement of visual field following trabeculectomy for open angle glaucoma. Eye (Lond) 1990;4:103–6. doi: 10.1038/eye.1990.12. [DOI] [PubMed] [Google Scholar]
- 23.Aydin A, Wollstein G, Price LL, Fujimoto JG, Schuman JS. Optical coherence tomography assessment of retinal nerve fiber layer thickness changes after glaucoma surgery. Ophthalmology. 2003;110:1506–11. doi: 10.1016/S0161-6420(03)00493-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang PT, Sekhon N, Budenz DL, Feuer WJ, Park PW, Anderson DR. Effect of lowering intraocular pressure on optical coherence tomography measurement of peripapillary retinal nerve fiber layer thickness. Ophthalmology. 2007;114:2252–8. doi: 10.1016/j.ophtha.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 25.Raghu N, Pandav SS, Kaushik S, Ichhpujani P, Gupta A. Effect of trabeculectomy on RNFL thickness and optic disc parameters using optical coherence tomography. Eye (Lond) 2012;26:1131–7. doi: 10.1038/eye.2012.115. [DOI] [PMC free article] [PubMed] [Google Scholar]


