Abstract
Objective
Toward explicating relations between economic adversity and children’s sleep, we examined associations between multiple indicators of socioeconomic status (SES)/adversity and children’s objectively and subjectively derived sleep parameters; ethnicity was examined as potential moderator.
Methods
Participants were 276 third- and fourth-grade children and their families (133 girls; M age = 9.44 years; SD = .71): 66% European American (EA) and 34% African American (AA). Four SES indicators were used: income-to-needs ratio, perceived economic well-being, maternal education, and community poverty. Children wore actigraphs for 7 nights and completed a self-report measure to assess sleep problems.
Results
Objectively and subjectively assessed sleep parameters were related to different SES indicators, and overall worse sleep was evident for children from lower SES homes. Specifically, children from homes with lower income-to-needs ratios had higher levels of reported sleep/wake problems. Parental perceived economic well-being was associated with shorter sleep minutes and greater variability in sleep onset for children. Lower mother’s education was associated with lower sleep efficiency. Children who attended Title 1 schools had shorter sleep minutes. Ethnicity was a significant moderator of effects in the link between some SES indicators and children’s sleep. AA children’s sleep was more negatively affected by income-to-needs ratio and mother’s education than was the sleep of EA children.
Conclusions
The results advocate for the importance of specifying particular SES and sleep variables used because they may affect the ability to detect associations between sleep and economic adversity.
Keywords: socioeconomic status, sleep, children, health disparity, actigraphy
Sleep is a basic requirement for and determinant of health and well-being across the life span. Specifically in children, low quality and/or short sleep duration are associated with physical health problems including obesity and risk for cardiometabolic disease (Knutson, 2012). A causal role of sleep in these associations has been suggested, with studies showing that sleep problems can affect metabolic and endocrine functioning (Leproult & Van Cauter, 2010). Furthermore, sleep problems have been shown to predict symptoms of anxiety and depression in children (El-Sheikh, Erath, & Keller, 2007), possibly mediated by the deleterious effects of sleep disruptions on prefrontal cortex functioning (Muzur, Pace-Schott, & Hobson, 2002).
Normative child sleep problems such as insufficient or poor sleep quality are common (Dewald, Meijer, Oort, Kerkhof, & Bogels, 2010) yet are not equally distributed in the population. Evidence is accumulating indicating that children of lower socioeconomic status (SES) are at greater risk for nonclinical sleep disturbances and insufficiency than their higher SES counterparts (Gellis, 2011). Given the observed disparities in sleep associated with economic adversity, it has been hypothesized that sleep may be an important mediator of the effects of SES on physical and mental health (Moore, Adler, Williams, & Jackson, 2002). Thus, understanding the childhood roots of “sleep disparity” could have significant clinical and social implications.
Critical to understanding how disparities in health outcomes develop in children from low SES families is a better understanding of the mechanisms and variables through which SES effects are seen. Much of our knowledge of SES-related effects is based on studies that used a single marker of SES such as income as opposed to viewing SES as a complex construct requiring multiple measures. Further, SES measures and ethnicity have been frequently confounded, disallowing clear interpretation. Understanding is also incomplete regarding which aspects of sleep are related to SES. Similar to SES, sleep is a complex, multidimensional construct and is not appropriately captured in a single variable such as duration.
Thus, key scientific questions remain: Do different indicators of SES relate differently to sleep problems in children? Are some facets of sleep more vulnerable to the effects of low SES? Do these relations vary based on ethnicity? In this study, we address these questions through examining associations between multiple indicators of SES and multivariate assessments of children’s sleep obtained via objective and subjective measures; we also assess ethnicity (African [AA] and European American [EA]) as a moderator of effects in the economic adversity-sleep link.
Conceptualizations and Indicators of SES
The operational definition of SES has long been debated because of its multidimensional nature (for review see Hout, 2008). Objective and subjective measures of monetary/wealth resources, economic hardship, class/status, education, and community-level variables (e.g., poverty rates, crime rates) have been used as markers of SES, yet different indicators of SES are not considered interchangeable (Braveman et al., 2005). The measures one chooses to examine SES reflect different underlying conceptualizations that may be associated with different pathways linking SES to children’s health (Bradley & Corwyn, 2002). Thus, the use of multiple indices of SES is imperative for delineating relations between SES and child health. In the study presented here, we utilize four distinct approaches to capturing SES, as detailed below.
First, one traditional approach to conceptualizing SES is based on resources; the notion being that an important component of SES is the availability of material resources. These assets, typically measured via family income and/or income-to-needs ratio, are hypothesized to play a role in determining health status in a family (Adler & Ostrove, 1999). For example, in relation to sleep, families with higher versus lower incomes are likely to live in larger dwellings with sleeping spaces that may be superior (e.g., temperature-controlled, minimized noise) and to have access to better quality health care for conditions that may affect sleep (e.g., asthma, allergies, pain).
A second traditional approach to conceptualizing SES is based on status. For example, the highest level of achieved education is considered an indicator of status within one’s society (Krieger, Williams, & Moss, 1997) and is considered an approximate index of human capital (McLoyd & Ceballo, 1998). Human capital is thought to encompass a diverse set of nonmaterial resources (e.g., skills, knowledge) and includes health literacy. Although maternal education may be considered a more distal influence on children’s sleep, it frequently accounts for a significant amount of SES-related differences in developmental outcomes through mechanisms including competent parenting (Bornstein, Hahn, Suwalsky, & Haynes, 2003). Further, more educated adults sleep longer than their less educated counterparts (Hale, 2005). Thus, mothers with higher levels of education may be more knowledgeable about the importance of sleep, better models of healthy sleep behaviors, and more proactive in facilitating children’s sleep.
In contrast to these objective measures, subjective measures of SES assess perceptions of the family’s current economic situation and may not necessarily align with objective measures (Braveman et al., 2005). As described by the family stress model (Conger, Conger, & Martin, 2010), lower perceived economic well-being may increase overall stress levels within a household. Research testing this model suggests that the caregiver’s perceived economic pressure is the primary predictor of child outcomes because it is responsible for harmful changes in parental mental health and marital and parent–child processes that may mediate the effects of SES on children’s mental health. In turn, evidence has linked children’s sleep problems to these intermediary processes, such as parental depression (El-Sheikh, Kelly, Bagley, & Wetter, 2012), marital conflict (Kelly & El-Sheikh, 2011), and parenting (El-Sheikh, Hinnant, Kelly, & Erath, 2010).
SES can be conceptualized as a community-level (rather than household-level) variable (Krieger et al., 1997), representing aggregate measures of the characteristics of a broader district in which a child lives (Diez Roux, 2001) such as the percentage of people living in poverty. Community-level variables characterize the larger sociocultural milieu and are important from an ecological perspective (Bronfenbrenner, 1986) of development. Low-income neighborhoods with higher levels of violent crime may lower children’s perceptions of neighborhood safety and lead to heightened levels of vigilance, which interfere with initiation and maintenance of sleep (Dahl, 1996). Children in disadvantaged neighborhoods may also be more likely to be exposed to substandard housing conditions and air pollution (Evans, 2004), both of which can affect sleep.
Links Between SES and Children’s Sleep
Children from lower SES homes have shorter sleep duration and poorer sleep quality (Gellis, 2011). Using Census data as a proxy for SES, children residing in zip codes with a median household income below the U.S. average had shorter parent-reported sleep duration (McLaughlin Crabtree et al., 2005). Likewise, Census data on neighborhood disadvantage were related to parent-reported child sleep problems (Spilsbury et al., 2006); null and inconsistent effects have also been reported. Using the Panel Survey of Income Dynamics, family income, but not parental education, was related to shorter sleep duration (Adam, Snell, & Pendry, 2007). A few studies have used actigraphy to measure sleep objectively, thereby avoiding problems with reporter bias and providing more information about sleep quality. Lower parental education (Sadeh, Raviv, & Gruber, 2000) and a composite measure of SES that included education (El-Sheikh, Kelly et al., 2010) were predictive of actigraphy-based poorer sleep in school-age children.
In sum, prior research that has examined SES and children’s sleep has often considered only a single indicator of SES or created composites using multiple indicators of SES (i.e., income and education). Likewise, measurement of sleep has frequently relied on parent report. Thus, there remains uncertainty regarding how various indicators of SES are related to a wide range of children’s objectively and subjectively measured sleep outcomes.
Ethnicity As a Potential Moderator in the SES-Sleep Connection
Significant differences exist in the sleep of AA and EA youth (Gellis, 2011). In comparison to EAs, AA children (McLaughlin Crabtree et al., 2005) have shorter sleep duration and have more variable sleep schedules (Hale, Berger, LeBourgeois, & Brooks-Gunn, 2009). In one of the few studies to use actigraphy, Buckhalt, El-Sheikh, Keller, and Kelly (2009) reported AA children to have shorter sleep duration and poorer sleep quality than EAs. Assessing the effect of SES within the context of ethnicity (Braveman & Barclay, 2009) allows for examining aggregation of risk in children’s sleep and is a focus of the study presented here.
The Current Study
A primary aim was to examine the effects of various indicators of SES on children’s actigraphy-based and self-reported sleep parameters. The inclusion of multiple indicators of objectively (sleep minutes, efficiency, and variability) and subjectively measured sleep (child report) adds substantially to the current literature on the association between sleep and SES and is of importance for a better understanding of sleep regulation (Sadeh, 2008). In addition, the moderating effect of ethnicity on relations between SES and sleep was examined; in initial analyses child gender was examined as a moderator, but no significant effects were found.
Overall, we expected lower SES to be associated with worse sleep in children (i.e., shorter sleep minutes, lower efficiency, more variability in sleep schedule, and higher levels of child-reported sleep problems). We hypothesized that monetary resources and perceived economic well-being would be most strongly related to children’s sleep, reasoning that parental education and community-level SES are more distal influences on children’s development. Further, consistent with an aggregated risk perspective, we expected moderation effects demonstrating that relations between low SES and sleep problems would be stronger for AA than EA children. Given the novelty of this question, no differential hypotheses were proposed regarding sleep parameters most likely affected by SES.
Methods
Participants
Third- and fourth-grade children (N = 282) and their families were recruited from two public school districts (N = 7 schools within one county) in the southeastern United States (rural and semirural towns); we have ongoing collaborations with the schools, which are relatively close to our on-campus laboratory. Data were collected in 2009–2010 during the academic school year excluding major holidays. Most families were reached through letters distributed to schools that were sent home with children. From 2,700 letters sent to families, 314 families who contacted our laboratory fit our inclusion criteria, and of those, approximately 90% participated in the study. Children were excluded if they had been diagnosed with a mental or learning disability or a clinically significant sleep disorder (e.g., apnea). Of the participating families, six mothers reported that their child had a severe chronic illness that may cause pain (e.g., sickle cell) and these children were not included further in analyses. Thus, the final sample for this study was composed of 276 children (133 girls; M age = 9.44 years; SD = .71), 12% of whom had been diagnosed with asthma. Additionally, 22% of participating children took regular medications for conditions such as asthma, attention-deficit hyperactivity disorder, or allergies; asthma and medication status were controlled in analyses. Although participants were drawn from the same community as those in some of our other samples (e.g., Buckhalt et al., 2009), this is the first time we have used this newer, independent sample to address questions pertinent to SES and sleep. Of note, children in this study are exposed to much higher levels of socioeconomic adversity those in our prior samples.
Parents (or guardians) reported during the initial phone contact on family structure, partner status (e.g., married, single), and education level. Because fathers were the respondents in less than 5% of the cases, the term mother will hereafter be used as a proxy for parent/guardian. Most children lived with both of their biological parents (53%; N = 146); 21% (N = 59) lived with one biological parent and a spouse (e.g., step-parent, partner), 21% (N = 57) of children lived in a single-parent home (mostly with the mother), and 14 (5%) lived with other family members. The ethnic composition of the sample was similar to the area from which it was drawn: 66% EA and 34% AA. We oversampled to include EA and AA children across a wide range of socioeconomic backgrounds.
Procedures and Measures
This paper stems from a larger study approved by the university’s institutional review board examining links between sleep and children’s adaptation. Mothers gave consent and children provided assent. Actigraphs were delivered to the child’s home. Parents and children were instructed to place the actigraph on the child’s nondominant wrist just before bedtime and to remove it upon waking for 7 consecutive nights; nightly, a researcher called parents to obtain children’s bed and rise times as well as information on medication use during the past 24 h. After actigraphic assessments (M = 3.50 d; SD = 8.82), children and mothers visited our laboratory. Mothers completed SES-relevant measures, and children reported on their sleep and wake problems via interview with a researcher. Children and mothers received monetary compensation for their own participation.
Monetary Resources
Monetary resources were assessed using the family income-to-needs ratio, a standard measure of a family’s economic situation (U.S. Department of Commerce; www.commerce.gov) that accounts for the number of individuals supported by the family income. Mothers reported annual familial income according to the following categories: (a) $10,000 to $20,000; (b) $20,000 to $35,000; (c) $35,000 to $50,000; (d) $50,000 to $75,000; or (e) more than $75,000. Mean of the familial income range and household size were used in the calculation of income-to-needs ratio. Income-to-needs ratio was computed by dividing family income by the federal poverty threshold for that family size (e.g., in 2010, a family of four with an annual income at or below $22,025 was considered to be living in poverty). Families who received an income-to-needs ratio of 1.0 or less were considered to be living in poverty (31% of the sample), scores greater than 1 but 2 or less were considered to be living near the poverty line (31%), greater than 2 but less than 3 were considered to be of lower middle class (28%), and those with a score of 3 or higher were considered to be of middle class standing (10%).
Perceived Economic Well-Being
Mothers provided information about their family’s economic hardship using three well-established scales (Conger et al., 1992): “can’t make ends meet,” “material needs,” and “financial cutbacks.” Regarding can’t make ends meet, mothers rated how much they agreed with three statements assessing the amount of difficulty the family had in paying their bills each month over the last year. Two of the three questions were on a five-point Likert-type scale; the third was on a four-point scale. Standardized scores were generated for this scale and higher scores were representative of less economic pressure; α = .82 in the current sample. The second indicator (material needs) comprised seven questions assessing how mothers felt about their family’s economic situation (e.g., “My family has enough money to afford the kind of home we would like to have”). Using a five-point scale, mothers rated how much they agreed with each statement. Per the original scale (Conger et al., 1992), lower scores indicate less material needs and more economic well-being; however, we reversed the score to make it compatible with the others and thus in all analyses higher scores represent more economic well-being (α = .92). The final economic well-being indicator (financial cutbacks) comprised 22 statements describing adjustments the family had to make over the last year because of financial need (e.g., using savings to meet daily living expenses). Higher scores were indicative of a better economic situation; α = .86.
Mother Education
Mothers indicated their education level on the basis of the following categories: (a) less than 7th grade, (b) completion of 8th grade, (c) 9th to 11th grade, (d) high-school graduate, (e) partial college or specialized training, (f) bachelor’s degree, or (g) graduate degree. A small percentage (1%) had less than a seventh-grade education, 2% completed eighth grade, 28% graduated from high school, 42% had at least 1 year of college/specialized training, 16% obtained a bachelor’s degree, and 6% completed graduate school. Education was used as a continuous variable (1 through 7) in analyses.
Community-Level Poverty
To assess school-level poverty, Title 1 status of the child’s school system was used. Title 1 is a set of programs developed by the U.S. Department of Education to distribute funds to schools with a high percentage (~40%) of students from low-income families. In this sample, 55% of children were from schools in which the surrounding community was considered to be largely low income. This variable was dummy coded (0, 1) with 1 indicative of attending a Title 1 school.
Actigraphy
The actigraph used was the Octagonal Basic Motionlogger (Ambulatory Monitoring, Inc., Ardsley, NY), which is a small, watch-size device and is widely used in pediatric sleep research (Sadeh, 2007). Raw data were analyzed using the ACTme software and Analysis Software Package (Action W2). The Sadeh algorithm (Sadeh, Sharkey, & Carskadon, 1994), which has established validity with children, was used to calculate the sleep variables in 1-min epochs. Sleep onset times were corroborated by the sleep diary data that were obtained by researchers during the week of actigraphy and are based on established guidelines (Acebo & Caskadon, 2001; unpublished laboratory manual).
Consistent with recommendations (Acebo & Carskadon, 2001), multiple sleep measures were derived. To examine sleep quantity, Sleep Minutes, the total minutes scored as sleep during the sleep period, were derived. Sleep Efficiency, the percentage of epochs scored as sleep between sleep onset and offset, was derived and was a measure of sleep quality. Finally, to assess sleep schedule variability, we examined Variability in Sleep Onset, derived by calculating the variance of Sleep Onset over the course of the week of actigraphy assessment using the mean-centered coefficient of variance statistic (Snedecor & Cochran, 1967). Given the school start times, there was not much variability in time of morning awakenings.
Most children (62%) had actigraphy data for the entire week of assessment. However, because of actigraph malfunctions or forgetting to wear the device, 17% had data for 6 nights, 10% had data for 5 nights, 3% had data for 4 nights, 1% had data for 3 nights, and 7% had no actigraphy data. These rates of valid actigraph data are considered very good (Acebo et al., 1999). Intraclass correlations indicated good night-to-night stability over the week of assessment for Sleep Minutes (α = .85), Sleep Efficiency (α = .90), and Sleep Onset Time (α = .75). Actigraphy variables used in analyses were based on the week’s (or total number of available nights) mean.
Subjective Sleep
Children completed the Children’s Sleep Habits Survey (SHS; Wolfson & Carskadon, 1998), which has demonstrated reliability and validity (e.g., has been validated against sleep diary reports and actigraphy; Wolfson et al., 2003) for school-age children and has been used in many studies to examine children’s sleep (e.g., Acebo & Carskadon, 2002; Buckhalt, El-Sheikh, & Keller, 2007, Buckhalt et al., 2009; El-Sheikh & Buckhalt, 2005). In analyses, we used the Sleep/Wake Problems Scale, which includes 10 items rated from 1 (never) to 5 (every day/night) that measures oversleeping, staying up late at night, and falling asleep at unscheduled times. In this study, α = .64.
Plan of Analysis
First, we fit structural equation models (SEMs) to examine the direct effects of four SES indices on four child sleep outcomes. The SES indices were (a) the observed family income-to-needs ratio; (b) a latent variable composed of the three Conger and colleagues observed scales (Conger et al., 1992, 2002) of can’t make ends meet, material needs, and financial cutbacks, which we term “perceived economic well-being”; (c) the observed variable of mother’s education; and (d) the observed variable of community-level poverty (i.e., enrollment in Title 1 School). The following were our actigraphy-derived sleep measures: (a) sleep minutes, (b) sleep efficiency, and (c) sleep onset variability. Child-reported sleep/wake problems from the SHS were used as the subjectively assessed sleep measure. In all SEM models, we controlled for child age, medication use, asthma, and single-parent status. To reduce outlier effects, data points that exceeded 4 SDs were removed. Specifically, the following data points were removed: one for sleep minutes, five for sleep efficiency, and four for variability of sleep onset.
We simultaneously tested direct effects of each of the socioeconomic indicators on all four of the sleep variables. The only two sleep variables for which residual variance did covary were sleep minutes and sleep efficiency. We next examined whether ethnicity moderated the relations in the aforementioned direct effects models. To do this, we fit a multiple-group model across the two ethnic groups (EA, AA). We used Δχ2 invariance tests to determine whether moderation by ethnicity existed for each direct parameter estimate, one at a time (Muthen & Muthen, 1998–2010). We also tested if the residual variances of the observed sleep variables differed across ethnicity (i.e., were we predicting more variance for EA rather than AA children?) If the Δχ2 invariance test indicated invariance for any set of parameters, they were held invariant as the other parameters were tested.
These analyses were conducted with Mplus (version 6; Muthen & Muthen, 1998–2010). Missing data were not imputed; rather, available data from all 276 participants were used in analyses by using full information maximum likelihood (FIML) estimation with robust standard errors. The proportion of data present to estimate each relation ranged from 91% to 100%. FIML estimation is one of the best methods of dealing with missing data (Acock, 2005). Model fit was assessed by a nonsignificant χ2 statistic, a nonsignificant root mean standard error of approximation (RMSEA) less than .08, and a comparative fit index (CFI) greater than .90.
Results
Preliminary Analyses
Descriptive statistics and correlations among primary study variables are presented in Table 1. Some significant correlations between control and study variables were observed. Child age was negatively related to mother’s education (r = −.23, p < .001). Younger children had longer sleep minutes (r = −.19, p < .01) and reduced sleep efficiency (r = −.14, p < .05). Single-parent status was associated with longer sleep minutes (r = .14, p < .05). Children who took medication were more likely to come from homes with lower income-to-needs ratio (r = −.12, p < .05) and with lower perceived economic well-being (r = −.14, p < .05). Further, medication status was negatively related to sleep efficiency (r = −.15, p < .05). Children with asthma were more likely to come from homes with lower income-to-needs ratio (r = −.14, p < .05). Asthma was also associated with fewer sleep minutes (r = −.19, p < .01) and lower sleep efficiency (r = −.27, p < .01).
Table 1.
Summary of Correlations Among Primary Study Variables, Means, and SDs
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Income-to-needs ratio | — | |||||||||
| 2. Can’t make ends meet | .41** | — | ||||||||
| 3. Material needs | .42** | .69** | — | |||||||
| 4. Financial cuts | .34** | .67** | −.61** | — | ||||||
| 5. Mother’s education | .49** | .23** | −.22** | .13* | — | |||||
| 6. Community povertya | −.07 | −.07 | .11~ | −.06 | .01 | — | ||||
| 7. Sleep minutesb | .18** | .20** | −.18** | .23** | .14* | −.17** | — | |||
| 8. Sleep efficiencyb | .14* | .03 | −.07 | .06 | .17** | −.02 | .73** | — | ||
| 9. Variability sleep onsetb | −.09 | −.19** | .22** | −.15* | .01 | .02 | −.17** | −.02 | — | |
| 10. Sleep/wake problemsc | .20** | −.08 | .15* | −.10 | −.09 | −.04 | −.04 | −.03 | .12 | — |
| Mean | 1.72 | 8.06 | 18.76 | 36.51 | 4.81 | .55 | 457 | 88.79 | .07 | 18.97 |
| SD | 1.04 | 2.86 | 7.07 | 4.96 | 1.08 | .50 | 57 | 6.40 | .12 | 5.23 |
Community poverty was dummy coded as (1) Title 1 school district; (0) not a Title 1 school district.
Actigraphy-based data.
Child-reported data.
p < .10.
p < .05.
p < .01.
Using t tests, we compared EAs and AAs on the various SES and sleep indices. No significant differences between EA and AA children were found on any of the SES parameters, sleep minutes, variability in sleep schedule, or subjective sleep/wake problems. However, statistically significant differences were found indicating that AAs tended to have lower sleep efficiency on average than their EA counterparts. Specifically, for EA and AA children, respectively, means were 89.44 (SD = 5.95) and 87.64 (SD = 7.02), p < .05, for sleep efficiency.
The latent construct of perceived economic well-being was fit in Mplus and showed excellent measurement properties. The three observed measures—can’t make ends meet, material needs, and financial cutbacks—loaded well on the latent variable of perceived economic well-being (r values = .76 to .87); all were coded and analyzed such that higher levels are indicative of a better economic situation.
Socioeconomic Indices as Predictors of Sleep
Below, we report SES indices as predictors of sleep and moderation effects by ethnicity if found. Income-to-needs ratio (model fit: χ2 = 0, df = 0, p = 1; CFI = 1; RMSEA = .00, p = 1) was marginally associated with children’s sleep quantity (β = .10, r = .11, p < .10, R2 = 9.2%) and child-reported sleep/wake problems (β = −.08, r = −.17, p < .01, R2 = 4.3%). Children in homes with fewer monetary resources had marginally less sleep and more reported sleep/wake problems (see Figure 1). The direct effects of income-to-needs ratio on sleep onset variability (test for slopes: Δχ2 = 5.77, Δdf = 1, p < .05; EA: β = .01, r = .08, p > .05, R2 = 8.0%; AA: β = −.03, r = −.25, p < .05) and children’s sleep/ wake problems (test for slopes: Δχ2 = 4.37, Δdf = 1, p < .05; EA: β = −.03, r = −.02, p > .05, R2 = 3.1%; AA: β = −.18, r = −.36, p < .001; R2 = 12.3%) were significantly moderated by ethnicity (model fit: χ2 = 8.2, df = 11, p = .69; RMSEA = .00, p = .87; CFI = 1.00). AA children who are worse off financially had more sleep onset variability and sleep/wake problems than those with more financial resources; no such significant effects were found for EA children.
Figure 1.
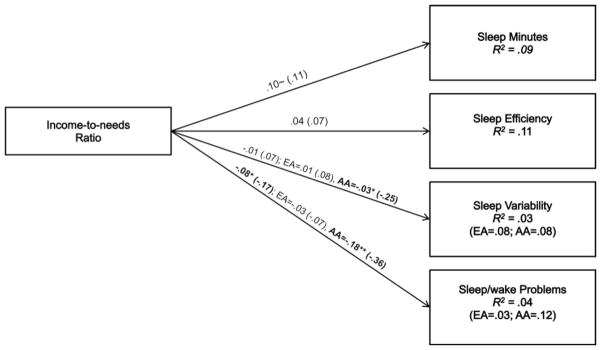
Fitted path model of sleep minutes, sleep efficiency, sleep variability, and sleep/wake problems regressed on income-to-needs ratio and controlled for single-parent household, child age, medications, and asthma. Significant multiple group estimates for EA and AA children representing the moderation by ethnicity are presented following the main effects parameter estimates. Nonstandardized parameter estimates are depicted with estimated correlations in parentheses. ~p < .10. *p < .05. **p < .01.
Economic well-being (model fit: χ2 = 19, df = 16, p = .25; RMSEA = .03, p = .81; CFI = .99; see Figure 2) predicted sleep quantity (β = .26, r = .21, p < .01, R2 = 11.6%) and sleep onset variability (β = −.04, r = −.22, p < .01, R2 = 7.0%) in expected directions. No moderation effects involving ethnicity were observed.
Figure 2.
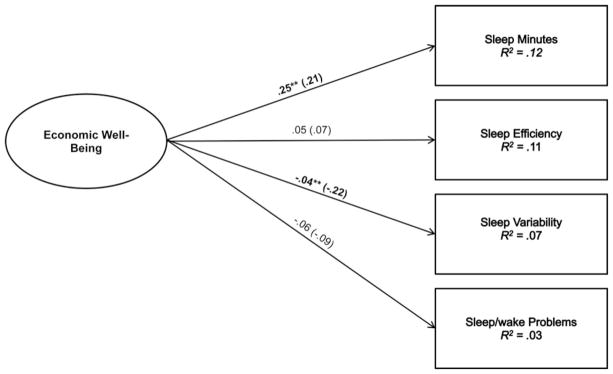
Fitted path model of sleep minutes, sleep efficiency, sleep variability, and sleep/wake problems regressed on the latent construct, economic well-being, and controlled for single-parent household, child age, medications, and asthma. Nonstandardized parameter estimates are depicted with estimated correlations in parentheses. ~p < .10. *p < .05. **p < .01.
Mother’s education (model fit: χ2 = 0, df = 0, p = 1; RMSEA = .00, p = 1; CFI = 1) predicted children’s sleep efficiency (β = .08, r = .14, p < .05, R2 = 12.0%), and this association was moderated by ethnicity (test for slopes: Δχ2 = 10.5, Δdf = 1, p < .05; EA: β = .01, r = .02, p > .05, R2 = 11.2%; AA: β = .17, r = .34, p < .001, R2 = 26.5%; see Figure 3. AA children with educated mothers slept less efficiently than AA children with more educated mothers; this relation was not significant for EA children. Further, ethnicity moderated the effect of mother’s education on sleep quantity (model fit: χ2 = 14.4, df = 11, p = .21; RMSEA = .05, p = .47; CFI = .98; test for slopes: Δχ2 = 3.84, Δdf = 1, p < .05; EA: β = .01, r = .01, p > .05, R2 = 9.0%; AA: β = .20, r = .34, p < .05, R2 = 17.2%). These findings indicate that mother’s education was related to sleep quantity for AA but not EA children.
Figure 3.
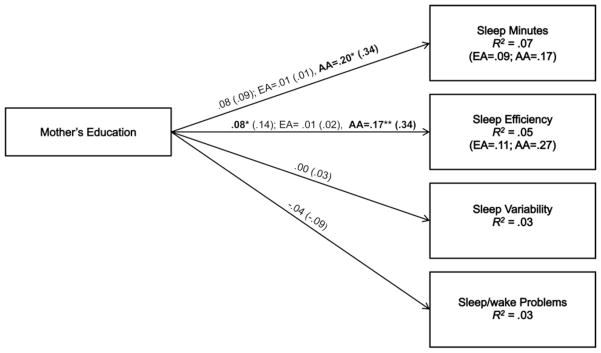
Fitted path model of sleep minutes, sleep efficiency, sleep variability, and sleep/wake problems regressed on mother’s education and controlled for single-parent household, child age, medications, and asthma. Significant multiple group estimates for EA and AA children representing the moderation by ethnicity are presented following the main effects parameter estimates. Nonstandardized parameter estimates are depicted with estimated correlations in parentheses. ~ p < .10. *p < .05. **p < .01.
Finally, community poverty was related to children’s sleep quantity (β = −.32, r = −.17, p < .01, R2 = 11.4%; model fit: χ2 = 0, df = 0, p = 1; RMSEA = .00, p = 1; CFI = 1). Children who attended Title 1 schools slept less (Figure 4; no moderation effects were found).
Figure 4.
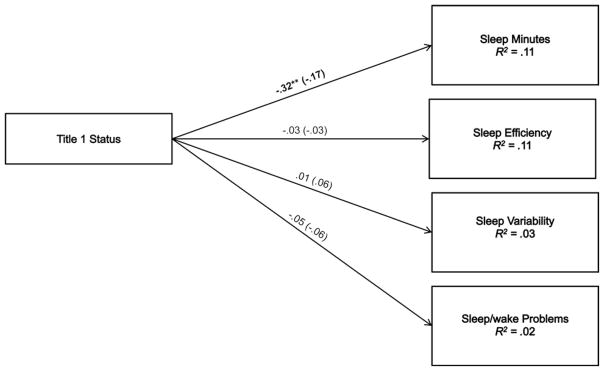
Fitted path model of sleep minutes, sleep efficiency, sleep variability, and sleep/wake problems regressed on the latent construct, economic well-being, and controlled for single-parent household, child age, medications, and asthma. Nonstandardized parameter estimates are depicted with estimated correlations in parentheses. ~ p < .10. *p < .05. **p < .01.
Discussion
Our findings are consistent with the idea that “one size does not fit all” (Braveman et al., 2005) when it comes to measurement of SES in health research and specifically for understanding children’s sleep. Consequently, investigators interested in relations between SES and sleep would benefit from assessments of multiple indicators of SES. To build a cumulative knowledge base regarding the influence of contextual factors on sleep, our findings advocate for the importance of specifying the particular SES variables used because they may relate to the detection of associations. Similar to the conclusions of the authors of a recent meta-analysis regarding the influence of sleep on school performance (Dewald, Meijer, Oort, Kerkhof, & Bogels, 2010), our results also suggest that assessing multiple aspects of sleep through objective and subjective measurement is important for providing a more complete understanding of the influence of SES on children’s sleep.
The questions about differential relationships between various indicators of SES and sleep are not merely methodological because they may also provide insights into different causal pathways that explain the effect of SES on sleep. The SES variables examined include objective (income-to-needs ratio) and subjective (economic well-being) indicators as well as measures of human capital (mother’s education) and community poverty (Title 1 status). Although moderately correlated, these indicators of SES may implicate different processes that affect children’s sleep. Therefore, this study represents an important advance toward illuminating disparities in children’s sleep along socioeconomic lines and developing effective prevention and intervention strategies.
The observed relations between income-to-needs ratio and child-reported sleep problems, and to a lesser extent sleep minutes, may implicate more direct effects of SES on children’s sleep. Investment models, which have been useful in explaining how family income affects child learning outcomes (Yeung, Linver, & Brooks-Gunn, 2002), suggest that a family’s ability to invest in stimulating environments supports children’s development. Similarly, a family’s ability to provide a physical environment that supports the onset and maintenance of sleep (e.g., pillows, beds, temperature control, low noise levels) may explain our findings; of course, this plausible explanation is tentative pending the direct testing of the physical sleep environment. Evaluation of existing programs that provide underprivileged children with concrete resources such as bedding may provide important information about the extent to which improvement in the physical sleeping environment might mitigate the negative effects of SES on sleep.
Consistent with our prediction and the family stress model (Conger, Conger, & Martin, 2010), lower levels of mothers’ perceived economic well-being (only moderately associated with income in our sample) predicted shorter sleep duration and greater variability in sleep onset in children. Given that economic well-being is a correlate and index of family stress, reduced sleep duration and erratic sleep schedules may result from family altercations during the night (e.g., Kelly & El-Sheikh, 2011), problems with the parent–child relationships (El-Sheikh, Hinnant et al., 2010), and disrupted parenting practices including low levels of monitoring and supervision. However, within the framework of family stress, it is not evident why perceived economic well-being was not associated with sleep quality or child-reported sleep problems; previous research cited in the introduction of the study presented here does support links between family stress and these sleep parameters. Testing of the family stress model in relation to children’s sleep may clarify mechanisms through which SES affects this important bioregulatory system and may inform intervention efforts.
Maternal education was positively associated with children’s sleep efficiency. These findings corroborate reported associations between education (Sadeh et al., 2000) and an SES composite that included education (El-Sheikh, Kelly et al., 2010) with an independent sample than that used in the present study with actigraphically assessed poorer sleep in school-age children. Although more distal than monetary resources and subjective economic well-being, it could be that with higher education parents are more aware, more proactive, and better equipped to deal with their children’s sleep problems. Therefore, the associations between parental education and sleep may suggest an important point for intervention to improve children’s sleep. Indeed, if future research finds that higher levels of education are indicative of greater awareness of the importance of sleep for well-being, and greater familiarity with sleep-facilitating conditions and behaviors, then programs that aim to educate parents regarding ways to improve children’s sleep may be particularly helpful. In addition, making sleep hygiene education compulsory in schools may help children improve their sleep; however, recent reviews of such programs suggest that intervention efforts to date have been more successful in increasing knowledge than actually changing sleep behavior (Blunden, Chapman, & Rigney, 2012). Targeting parent and child may be an important innovation to improving the efficacy of sleep education programs.
Finally, although other studies have found links between children’s sleep and neighborhood disadvantage (Spilsbury et al., 2006) using survey data, our study is the first to demonstrate that higher community-level poverty predicts objectively measured shorter sleep duration. Unfortunately, our measure of community poverty (i.e., Title 1 status) only serves as a proxy for environmental risks (e.g., substandard housing, low sense of neighborhood safety) and does not identify the aspects of disadvantaged neighborhoods that lead to reduced sleep in children. It is also possible that children in Title 1 districts are more likely to wake up earlier to accommodate longer busing routes and to be able to receive free breakfast at school (common in this community if the child arrives early). An important avenue for future work would be to identify specific risk factors for poor sleep faced by children in Title 1 districts and then targeting these factors in future interventions.
Ethnicity served as an important moderator of relations between SES and sleep (recall that ethnicity was not associated with any SES index in this sample). Specifically, the income-to-needs ratio of the family was related to AA children’s sleep onset variability and sleep/wake problems, but neither of these relations was significant for EA children. Likewise, the effects of mother’s education on sleep minutes and efficiency were significant only for AA children. These findings are the first demonstration in the literature of interactions between SES and ethnicity in the prediction of children’s objective and subjective sleep and they add to the understanding of the childhood sleep disparities in the United States along socioeconomic and ethnic lines. The results complement a study of young adults showing that relations between perceived social status and subjective sleep quality existed for AA but not EA college students (Goodin, McGuire, & Smith, 2010). One possible explanation for these moderation findings may be that AA children from lower SES backgrounds are under a greater burden of stress by way of being poor and belonging to a minority group (the double jeopardy hypothesis). Explication of the extent to which processes such as perceived discrimination may explain our findings is warranted. Identifying sociocultural variables associated with AA ethnicity known to affect sleep, such as preference for room sharing (Buckhalt et al., 2007), taking naps (e.g., Crosby, LeBourgeois, & Harsh, 2005), and more variable sleep schedules (Hale et al., 2009), would be instrumental in improving sleep-related behaviors amenable to intervention through education. Of course, cultural consideration is critical when one plans such interventions.
Findings should be interpreted within the study’s context and limitations. Although the response rate from the school letters was 12%, raising important questions about potential response bias, this rate is typical for school-based mailings (Ji, Porkony, & Jason, 2004). Our final sample is representative of the community, and 90% of contacted families participated. The sample includes children from rural and semirural communities exposed to high levels of socioeconomic adversity and may not be generalizable to other populations. The exclusion of children with clinically diagnosed sleep problems may attenuate observed associations between SES and sleep problems. In addition, the SHS used for child report of sleep problems demonstrated only marginal internal consistency, possibly explaining why sleep/wake problems were only related to one SES indicator. Further, the observed statistically significant findings do not translate to clinically meaningful effects. Finally, it would be important in future research to gather information on children’s perceptions of family economic well-being given that these may differ from parental perceptions and may have independent effects on children’s sleep.
Exploring the strength of the SES-health association across the life span may expose critical periods when the relation is stronger than others, providing further insights into mechanisms underlying the link (Chen, 2004). Because of the cross-sectional design, our study is unable to reveal the timing of exposure that leads to the observed relations between SES indicators and sleep. For example, the observed associations could be the result of experiences that the child had early in development, even prenatally. It is known that children from low-SES families are more likely to have inadequate neurobehavioral development in utero, to be born prematurely, and to be of low birth weight (McLoyd, 1998); prematurity may be a risk factor for shorter nighttime sleep duration and more active sleep at 12 months (Asaka & Takada, 2010). However, limited evidence exists for the long-term consequences of early adversity on sleep. Longitudinal work is needed to answer important questions about timing of exposure, critical periods, and the possibility of “latent” effects of early adversity on sleep.
A life span approach to understanding the lasting effects of low SES during childhood is critical and underscores the importance of reducing disparities early in development (Hertzman, 1999). Research has consistently found effects of childhood SES on adult health, irrespective of adult SES (Melchior, Moffitt, Milne, Poulton, & Caspi, 2007). Extending this finding to sleep, Tomfohr, Ancoli-Isreal, and Dimsdale (2010) found that retrospectively reported low-SES status during childhood was associated with worse sleep outcomes during adulthood, independent of concurrent SES. In light of the study presented here showing a wide range of effects of SES on objective and subjective sleep parameters during childhood, researchers might start to consider how sleep patterns and sleep-related behaviors established during childhood in the context of disadvantage might function to affect health across the life span. Because sleep and SES are dynamic constructs, issues of chronicity in poverty and sleep problems also need to be considered. Along these lines, interventions during childhood aimed at improving sleep could have long-lasting effects on overall health and well-being for individuals who grow up disadvantaged.
Acknowledgments
This research was supported by National Institutes of Health grant R01-HL093246, awarded to the first author. The authors thank the staff of our research laboratory, most notably Bridget Wingo, for data collection and preparation as well as the school personnel, children, and parents who participated.
Contributor Information
Mona El-Sheikh, Auburn University.
Erika J. Bagley, Auburn University
Margaret Keiley, Auburn University.
Lori Elmore-Staton, Auburn University.
Edith Chen, University of British Columbia.
Joseph A. Buckhalt, Auburn University
References
- Acebo C, Carskadon M. Scoring actigraphy data using ACTION-W2. Providence, RI: Bradley Sleep Center, Brown University; 2001. [Google Scholar]
- Acebo C, Sadeh A, Seifer R, Tzischinsky O, Wolfson AR, Hafer A, Carskadon MA. Estimating sleep patterns with activity monitoring in children and adolescents: How many nights are necessary for reliable measures? Sleep. 1999;22:95–103. doi: 10.1093/sleep/22.1.95. [DOI] [PubMed] [Google Scholar]
- Acock AC. Working with missing values. Journal of Marriage and Family. 2005;67:1012–1028. doi: 10.1111/j.1741-3737.2005.00191.x. [DOI] [Google Scholar]
- Adam EK, Snell EK, Pendry P. Sleep timing and quantity in ecological and family context: A nationally representative time-diary study. Journal of Family Psychology. 2007;21:4–19. doi: 10.1037/0893-3200.21.1.4. [DOI] [PubMed] [Google Scholar]
- Adler NE, Ostrove JM. Socioeconomic status and health: What we know and what we don’t. Annals of the New York Academy of Sciences. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Asaka Y, Takada S. Activity-based assessment of the sleep behaviors of VLBW preterm infants and full-term infants at around 12 months of age. Brain & Development. 2010;32:150–155. doi: 10.1016/j.braindev.2008.12.006. [DOI] [PubMed] [Google Scholar]
- Blunden SL, Chapman J, Rigney GA. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep Medicine Reviews. 2012;16:355–370. doi: 10.1016/j.smrv.2011.08.002. [DOI] [PubMed] [Google Scholar]
- Bornstein MH, Hahn C, Suwalsky JT, Haynes MO. Socioeconomic status, parenting, and child development: The Holling-shead four-factor index of social status and the socioeconomic index of occupations. In: Bornstein MH, Bradley R, editors. Socioeconomic status, parenting and child development, Monographs in parenting series. Mahwah, NJ: Erlbaum; 2003. pp. 29–82. [Google Scholar]
- Bradley RH, Corwyn RF. Socioeconomic status and child development. Annual Review of Psychology. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Braveman P, Barclay C. Health disparities beginning in childhood: A life course perspective. Pediatrics. 2009;124:S163–S175. doi: 10.1542/peds.2009-1100D. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research. JAMA: Journal of the American Medical Association. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a contest for human development: Research perspectives. Developmental Psychology. 1986;22:723–742. doi: 10.1037/0012-1649.22.6.723. [DOI] [Google Scholar]
- Buckhalt JA, El-Sheikh M, Keller P. Children’s sleep and cognitive functioning: Race and socioeconomic status as moderators of effects. Child Development. 2007;78:213–231. doi: 10.1111/j.1467-8624.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- Buckhalt JA, El-Sheikh M, Keller PS, Kelly RJ. Concurrent and longitudinal relationships between children’s sleep and cognitive functioning: The moderating role of parent education. Child Development. 2009;80:875–892. doi: 10.1111/j.1467-8624.2009.01303.x. [DOI] [PubMed] [Google Scholar]
- Chen E. Why socioeconomic status affects the health of children: A psychosocial perspective. Current Directions in Psychological Science. 2004;13:112–115. doi: 10.1111/j.0963-7214.2004.00286.x. [DOI] [Google Scholar]
- Conger RD, Conger KJ, Elder GH, Jr, Lorenz FO, Simons RL, Whitbeck LB. A family process model of economic hardship and adjustment of early adolescent boys. Child Development. 1992;63:526–541. doi: 10.1111/j.1467-8624.1992.tb01644.x. [DOI] [PubMed] [Google Scholar]
- Conger RD, Conger KJ, Martin M. Socioeconomic status, family processes, and individual development. Journal of Marriage and Family. 2010;72:685–704. doi: 10.1111/j.1741-3737.2010.00725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger RD, Wallace LE, Sun Y, Simons RL, McLoyd VC, Brody GH. Economic pressure in African American families: A replication and extension of the Family Stress Model. Developmental Psychology. 2002;38:179–193. [PubMed] [Google Scholar]
- Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2- to 8- year old children. Pediatrics. 2005;115:225–232. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Development and Psychopathology. 1996;8:3–27. doi: 10.1017/S0954579400006945. [DOI] [Google Scholar]
- Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bogels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Medicine Reviews. 2010;14:179–189. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV. Investigating neighborhood and area effects on health. American Journal of Public Health. 2001;91:1783–1789. doi: 10.2105/AJPH.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Buckhalt JA. Vagal regulation and emotional intensity predict children’s sleep problems. Developmental Psychophysiology. 2005;46:307–317. doi: 10.1002/dev.20066. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Erath SA, Keller PS. Children’s sleep and adjustment: The moderating role of vagal regulation. Journal of Sleep Research. 2007;16:396–405. doi: 10.1111/j.1365-2869.2007.00618.x. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Hinnant JB, Kelly RJ, Erath S. Maternal psychological control and child internalizing symptoms: Vulnerability and protective factors across bioregulatory and ecological domains. Journal of Child Psychology and Psychiatry. 2010;51:188–198. doi: 10.1111/j.1469-7610.2009.02140.x. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Kelly RK, Bagley EJ, Wetter EK. Parental depressive symptoms and children’s sleep: The role of family conflict. Journal of Child Psychology & Psychiatry. 2012;53:806–814. doi: 10.1111/j.1469-7610.2012.02530.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Kelly RK, Buckhalt JA, Hinnant JB. Children’s sleep and adjustment over time: The role of socioeconomic context. Child Development. 2010;81:870–883. doi: 10.1111/j.1467-8624.2010.01439.x. [DOI] [PubMed] [Google Scholar]
- Evans GW. The environment of childhood poverty. American Psychologist. 2004;59:77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Gellis L. Children’s sleep in the context of socioeconomic status, race, and ethnicity. In: El-Sheikh M, editor. Sleep and development: Familial and socio-cultural considerations. New York, NY: Oxford University Press; 2011. pp. 219–244. [Google Scholar]
- Goodin BR, McGuire L, Smith MT. Ethnicity moderates the influence of perceived social status on subjective sleep quality. Behavioral Sleep Medicine. 2010;8:194–206. doi: 10.1080/15402002.2010.509193. [DOI] [PubMed] [Google Scholar]
- Hale L. Who has time to sleep? Journal of Public Health. 2005;27:205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. Social and demographic predictors of preschoolers’ bedtime routines. Journal of Developmental and Behavioral Pediatrics. 2009;30:394–402. doi: 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertzman C. The biological embedding of early experience and its effects on health in adulthood. Annals of the New York Academy of Sciences. 1999;896:85–95. doi: 10.1111/j.1749-6632.1999.tb08107.x. [DOI] [PubMed] [Google Scholar]
- Hout M. How class works: Objective and subjective aspects of class since the 1970s. In: Lareau A, Conley D, editors. Social class: How does it work? New York, NY: Russell Sage Foundation; 2008. pp. 25–64. [Google Scholar]
- Ji PY, Porkony SB, Jason LA. Factors influencing middle and high schools’ active parental consent return rates. Evaluation Review. 2004;28:578–591. doi: 10.1177/0193841X04263917. [DOI] [PubMed] [Google Scholar]
- Kelly RJ, El-Sheikh M. Marital conflict and children’s sleep: Reciprocal relations and socioeconomic effects. Journal of Family Psychology. 2011;25:412–422. doi: 10.1037/a0023789. [DOI] [PubMed] [Google Scholar]
- Knutson KL. Does inadequate sleep play a role in vulnerability to obesity? American Journal of Human Biology. 2012;24:361–371. doi: 10.1002/ajhb.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: Concepts, methodologies, and guidelines. Annual Review of Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- Leproult R, Van Cauter E. Role of sleep and sleep loss in hormonal release and metabolism. Endocrine Development. 2010;17:11–21. doi: 10.1159/000262524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin Crabtree V, Beal Korhonen J, Montgomery-Downs HE, Faye Jones V, O’Brien LM, Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep Medicine. 2005;6:319–324. doi: 10.1016/j.sleep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53:185–204. doi: 10.1037/0003-066X.53.2.185. [DOI] [PubMed] [Google Scholar]
- McLoyd VC, Ceballo R. Conceptualizing and assessing economic context: Issues in the study of race and child development. In: McLoyd VC, Steinberg L, editors. Studying minority adolescents: Conceptual, methodological, and theoretical issues. Mahwah, NJ: Lawrence Erlbaum; 1998. pp. 251–278. [Google Scholar]
- Melchior M, Moffitt TE, Milne BJ, Poulton R, Caspi A. Why do children from socioeconomically disadvantaged families suffer from poor health when they reach adulthood? A life-course study. American Journal of Epidemiology. 2007;166:966–974. doi: 10.1093/aje/kwm155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore PJ, Adler NE, Williams DR, Jackson JS. Socioeconomic status and health: The role of sleep. Psychosomatic Medicine. 2002;64:337–344. doi: 10.1097/00006842-200203000-00018. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus users guide. 6. Los Angeles, CA: Muthen & Muthen; 1998–2010. [Google Scholar]
- Muzur A, Pace-Schott E, Hobson JA. The prefrontal cortex in sleep. Trends in Cognitive Sciences. 2002;6:475–481. doi: 10.1016/S1364-6613(02)01992-7. [DOI] [PubMed] [Google Scholar]
- Sadeh A. Consequences of sleep loss or sleep disruption in children. Sleep Medicine Clinics. 2007;2:513–520. doi: 10.1016/j.jsmc.2007.05.012. [DOI] [Google Scholar]
- Sadeh A. Commentary: Comparing actigraphy and parental report as measures of children’s sleep. Journal of Pediatric Psychology. 2008;33:406–407. doi: 10.1093/jpepsy/jsn018. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Developmental Psychology. 2000;36:291–301. doi: 10.1037/0012-1649.36.3.291. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: An empirical test of methodological issues. Sleep. 1994;17:201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- Snedecor GW, Cochran WG. Statistical methods. 6. Ames, IA: Iowa State University Press; 1967. [Google Scholar]
- Spilsbury JC, Storfer-Isser A, Kirchner HL, Nelson L, Rosen CL, Drotar D, Redline S. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. The Journal of Pediatrics. 2006;149:342–347. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- Tomfohr LM, Ancoli-Isreal S, Dimsdale JE. Childhood socioeconomic status and race are associated with adult sleep. Behavioral Sleep Medicine. 2010;8:219–230. doi: 10.1080/15402002.2010.509236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Development. 1998;69:875–887. [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, Martin JL. Evidence for the validity of a sleep habits survey of adolescents. Sleep. 2003;26:213–216. doi: 10.1093/sleep/26.2.213. Retrieved from http://www.journalsleep.org/Default.aspx. [DOI] [PubMed] [Google Scholar]
- Yeung WJ, Linver MR, Brooks-Gunn J. How money matters for young children’s development: Parental investment and family processes. Child Development. 2002;73:1861–1879. doi: 10.1111/1467-8624.t01-1-00511. [DOI] [PubMed] [Google Scholar]


