Abstract
Stressful life events are associated with worsening neurological symptoms and decreased quality of life in multiple sclerosis (MS). Mindful-consciousness can alter the impact of stressful events and has potential to improve health outcomes in MS. This study evaluated the relationship between trait mindfulness and perceived stress, coping, and resilience in people with MS. Quality of life was assessed as a secondary outcome. 119 people with confirmed MS completed the Five-facet Mindfulness Questionnaire, Perceived Stress Scale, Brief Coping Orientation for Problem Experiences, Connor-Davidson Resilience Scale, and the SF-36. Greater trait mindfulness was significantly associated with decreased psychological stress, better coping skills, increased resilience, and higher quality of life. After controlling for confounders, mindfulness accounted for 25% of the variation in perceived stress scores and 44% of the variation in resilience scores. Results support further investigation of mindfulness training to enhance psychological resilience and improve wellbeing for those living with MS.
Introduction
People with multiple sclerosis (MS) have long reported that psychological stress can worsen their symptoms, and studies show that chronic exposure to a wide range of challenging life events is correlated with worsening neurological symptoms in MS and increased lesion burden on brain MRI ((1–4) see (5,6) for excellent reviews). Meta-analyses have found a consistent association between stressful life events and subsequent exacerbation (7,8). While exposure to potentially stressful events is common, not everyone responds with neurological worsening. The response to stress is a dynamic and highly personalized process; innate personality traits, early life experiences, learned cognitive dispositions, and biological factors all influence an individual’s appraisal of potentially stressful events (9). Moreover, studies show that alterations in stress physiology may impact the stress response in MS (see (10,11) for review). Given that the function of the body’s major stress response systems may be altered in MS, it is particularly important to understand specific factors that influence vulnerability to stress in people with MS.
Trait mindfulness is a personality characteristic associated with psychological well-being in other populations (12–15). Broadly conceptualized, mindfulness is a moment-to-moment awareness of one’s present experience in an open, interested, and nonjudgmental way. Being mindful involves paying attention to one’s thoughts and feelings without over-identifying with them, and without responding to them in an automatic or habitual manner. In this way, mindfulness creates distance between one’s perception and response, and enables people to respond to situations more thoughtfully, potentially reducing susceptibility to the effects of stress (16).
To date, no studies have examined mindfulness as a trait characteristic in MS or how it is associated with emotional resilience. To evaluate the relationship between trait mindfulness, stress, and psychosocial correlates in MS, we conducted a cross sectional survey (n=119, any type of MS). Our primary objective was to evaluate the association between mindfulness, perceived stress, coping strategies, and resilience. We hypothesized that those who reported being more mindful in their daily lives (dispositional or trait mindfulness) would also report lower perceived stress, more resilience to challenging situations, and the use of more constructive coping strategies. Because mindfulness is a malleable characteristic, results will inform future interventions to improve resilience and lessen the negative effects of stress in MS.
Materials and Methods
Design, Setting, and Study Participants
Participants were scheduled for one visit to Oregon Health & Science University (OHSU) where they completed several questionnaires. Recruitment began after approval from the Institutional Review Board at OHSU. A convenience sample of men and women were recruited during their outpatient visits to the MS Center at OHSU. The study was also advertised with the National MS Society Oregon Chapter and through MS community events. Inclusion criteria comprised any type of MS, ability to read and write in English, age 18 to 90 years old. Exclusion criteria included a relapse or exacerbation within the previous 90 days. MS diagnosis was confirmed by chart review according to 2010 McDonald criteria (17). Any questions regarding a participant’s diagnosis were discussed with their neurologist. Between December 2011 and February 2013, 119 people with MS were recruited, gave written consent, and completed the study.
Outcome Measures
All questionnaires used in this study are validated patient-reported outcome measures used in clinical trials involving MS and/or other stress-related disorders. Each measure asks participants to rate their feelings or thoughts on a Likert-type scale; responses typically range from 0 (never, not at all) to 4 or 5 (very often, very much so). Primary outcomes included perceived stress, mindfulness, coping, and resilience. Secondary outcomes included quality of life. The following instruments were used:
Perceived Stress Scale (PSS) is a 10-question subjective measure of how unpredictable, uncontrollable, and overloaded respondents find their lives over the previous four weeks (18). Total scores range from 0–40, and higher scores indicate increased levels of perceived stress.
Five Facet Mindfulness Scale (FFMQ) is a 39-item questionnaire that measures five elements of mindfulness: observing, describing, acting with awareness, non-judging, and non-reactivity (19). For this study, a summed score of these five facets was used; higher scores indicate higher levels of mindfulness.
Connor-Davidson Resilience Scale (CD-RISC) is a measurement of one’s ability to successfully cope with challenging situations. The scale draws on a number of resilient characteristics, including patience, tolerance to negative affect, commitment, recognition of limits to control, and adaptability (20). Scores range from 0 100; higher scores indicate higher levels of resilience.
Brief Coping Orientation for Problem Encounters (B-COPE) is a 28-item questionnaire that asks participants to rate their level of agreement with statements regarding how they have been coping with stress in their lives (21). There are 14 subscales that assess different coping strategies, acceptance, humor, planning, emotional support, positive reframing, and self-blame. Each subscale contains 2 questions. There is no “overall score”; each subscale is analyzed separately to identify which strategies subjects rely on. For this study, coping strategies were divided into adaptive and maladaptive strategies a priori. Adaptive strategies include the subscales Acceptance, Humor, Reframing, Emotional Support, Active Coping, Planning, and Instrumental Support. Maladaptive strategies include Denial, Behavioral Disengagement, and Self-Blame. Higher scores on adaptive and maladaptive coping mean greater reliance on those particular strategies.
Medical Outcome Study Short Form – 36 (SF-36) is a generic measure of health-related quality of life comprised of eight subscales (22). Two summary scores are obtained by grouping the eight subscales into either the Mental Health Component Summary (MCS) or the Physical Health Component Summary (PCS); higher scores reflect better quality of life. The SF-36 is widely used in multiple sclerosis trials and its reliability and validity is well supported (23).
Covariates
We examined seven factors that might influence trait mindfulness, perceived stress, or other psychosocial outcomes: age (continuous), gender, education (two categories), MS disease modifying therapy use (yes or no), self-reported disease severity (continuous), stressful life-events (continuous), and type of MS (three categories).
MS includes three disease subtypes: relapsing remitting MS, secondary progressive MS, and primary progressive MS. Relapsing remitting MS is characterized by intermittent neurologic dysfunction that can last for days to weeks but eventually improves. The majority of people with relapsing remitting MS will convert to secondary progressive MS 10–15 years after onset, at which point relapses cease and progressive neurological decline ensues. People with primary progressive MS experience progressive neurological decline from disease onset and typically do not have relapses. We controlled for type of MS because we expect that people with different subtypes will have unique concerns and stressors associated with their diagnosis.
To control for the potential impact of disability on perceived stress (24), self-reported disease severity was generated from a six-point scale ranging from “I have no or minimal MS-related symptoms, no limitations in walking ability, and no limitations on daily activities,” to “I have many severe MS-related symptoms and am restricted to a wheelchair or bed.” We have previously shown that this self-report scale correlates with Expanded Disability Severity Scale scores (r=0.85), a neurologist-rated, objective measure of disease severity (25). The disability scale can be found in the appendix.
Because the experience of recent stressful life events, such as divorce, unemployment, or loss of a loved one are likely to increase one’s level of perceived stress (26), we used the Social Readjustment Rating Scale (SRRS) to control for such interactions (27). The SRRS is a validated checklist of 43 potentially stressful life events. Participants indicate which events they have experienced within the past year. Each event is assigned a value, more stressful events have a higher point value than less stressful events, and a total SRRS score is generated.
Disease modifying therapies (DMTs) reduce the risk of relapse and may have an impact on quality of life (28). DMTs asked about and available for use at the time of this study included: glatiramer acetate, interferon-1b, interferon-1a, natalizumab, fingolimod, and mitoxantrone.
Statistical Analysis
Our hypotheses were that higher levels of mindfulness would be associated with 1) lower levels of perceived stress, 2) higher levels of resilience, 3) the use of more adaptive coping strategies, 4) less use of maladaptive coping strategies, 5) better mental health-related quality of life, and 6) better physical health-related quality of life in people with MS. Mindfulness was designated as the independent predictor variable; perceived stress, resilience, adaptive coping, maladpative coping, mental health related quality of life, and physical health related quality of life as dependent variables. Bivariate Pearson correlation coefficients between mindfulness and dependent variables were generated and linear regression analysis was used to examine these associations. Three models were fitted for each dependent variable: 1) a simple, unadjusted model with mindfulness as the predictor, 2) a model with the covariates age, gender, education, stressful life events, disability, DMT status, and type of MS as the predictors, and 3) model #2 plus the addition of mindfulness. Regression coefficients with 95% confidence intervals and p values were generated for mindfulness, and we used the difference in adjusted R2 between models 2 and 3 to determine how much variance in the dependent variable was explained by mindfulness (noted in the text as ΔR2). No attempts were made to replace missing data. A Bonferroni correction adjusted for multiple analyses; p values less than 0.008 are considered significant. All analyses were performed using STATA version 12.
Results
Sample Size and Participant Characteristics
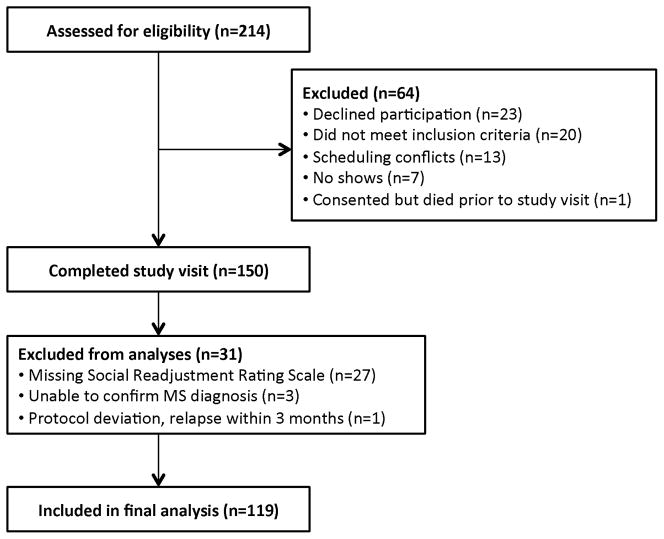
Two hundred fourteen people with MS were approached to participate in this study (Figure 1). Sixty-four people declined to participate or did not meet inclusion criteria; 150 people completed the study visit. The stressful life events checklist (Social Readjustment Rating Scale) was added to the study after the first 27 participants had completed their visits. Because stressful life events were included as a covariate, a SRRS score was required for analysis, and this missing data reduced our final sample size. In addition, four participants were dropped from analysis and some participants were unable to complete all the questionnaires (typically due to survey fatigue). Missing and excluded data resulted in final sample sizes that varied between 116 and 119.
Figure 1.
Study flow diagram.
Demographic data is displayed in Table 1. There were 86 participants (72.27%) who had relapsing remitting MS, 22 (18.49%) with secondary progressive, and 11 (9.24%) with primary progressive disease. The average age of participants was 51.58 ± 12.88 years and ranged from 19 to 81. Ninety-one percent of respondents had at least some college education and 62% had a college degree or higher. Seventy-five people (63%) were using DMTs at the time of the study visit, including glatiramer acetate, interferon-1b, interferon-1a, natalizumab, and fingolimod. The majority of participants (69.75%) were able to walk without aid. Most of the sample comprised individuals who had little to no prior experience with meditation (85.7%). Descriptive data is also presented for those participants who scored in the lowest and highest quartiles of the Perceived Stress Scale. Those respondents with the highest perceived stress scores (PSS ≥ 23, n=33) reported less experience with meditation, higher levels of disability, and fewer years of formal education than those with the lowest perceived stress scores (PSS ≤ 10, n=32). Due to the limited number of respondents in these subanalysis groups, these data should be viewed as descriptive and future studies should confirm results with larger numbers of participants. Mean scores for all outcome questionnaires are presented in Table 2.
Table 1.
Demographic data (n=119).
| Total sample N (%) |
PSS ≤ 10 (lowest quartile) n=32 |
PSS ≥ 23 (highest quartile) n=33 |
|
|---|---|---|---|
| Age (years, sd) | 51.58 ± 12.88 | 52.50 ± 13.52 | 47.55 ± 13.82 |
| Female | 93 (78) | 25 (78) | 28 (85) |
| Using Disease Modifying Therapy* | |||
| Yes | 75 (63) | 19 (60) | 19 (58) |
| No | 44 (37) | 13 (40) | 14 (42) |
| Experience with Meditation | |||
| A lot, regular practice | 17 (14.3) | 8 (25) | 2 (6) |
| Little (less than once a month), or none | 102 (85.7) | 24 (75) | 31 (94) |
| Education | |||
| HS Diploma | 45 (37.8) | 10 (31) | 15 (45) |
| College Grad | 74 (62.2) | 22 (69) | 18 (55) |
| Type of MS | |||
| Relapsing Remitting | 86 (72.3) | 22 (69) | 26 (79) |
| Secondary Progressive | 22 (18.5) | 8 (25) | 2 (6) |
| Primary Progressive | 11 (9.2) | 2 (6) | 5 (15) |
| Disability | |||
| None/minimal | 22 (18.5) | 11 (34) | 4 (12) |
| Mild | 31 (26.1) | 8 (25) | 7 (21) |
| Moderate | 30 (25.2) | 3 (9) | 12 (37) |
| Some support needed to walk | 22 (18.5) | 4 (13) | 7 (21) |
| Walker or two handed crutch | 7 (5.9) | 2 (6) | 3 (9) |
| Unable to walk | 7 (5.9) | 4 (13) | 0 |
| Ethnicity | |||
| Caucasian | 110 (92.4) | 28 (88) | 30 (91) |
| African American | 5 (4.2) | 0 | 0 |
| Other | 4 (2.4) | 4 (12) | 3 (9) |
DMTs used by participants included: glatiramer acetate, interferon-1b, interferon-1a, natalizumab, and fingolimod.
Table 2.
Mean outcome scores.
| Mean | Std Deviation | Respondent Range | |
|---|---|---|---|
| Mindfulness (FFMQ, n=117) | 134.71 | 22.46 | 74 – 182 |
| Perceived Stress (PSS, n=119) | 16.55 | 8.31 | 1 – 34 |
| Resilience (CD-RISC, n=117) | 73.44 | 15.82 | 31 – 97 |
| Maladaptive Coping (B-COPE, n=119) | 9.39 | 3.15 | 6 – 21 |
| Adaptive Coping (B-COPE, n=119) | 38.84 | 7.63 | 22 – 54 |
| Mental Health Quality of Life (SF-36 MCS, n=116) | 47.47 | 12.53 | 13.4 – 69.2 |
| Physical Health Quality of Life (SF-36 PCS, n=116) | 38.46 | 12.31 | 16.2 – 63.6 |
B-COPE: Brief Coping Orientation for Problem Experiences; CD-RISC: Connor-Davidson Resilience Scale; FFMQ: Five-Facet Mindfulness Questionnaire; PSS: Perceived Stress Scale; SF-36 MCS: Mental Health Component Summary Score of SF-36; SF-36 PCS: Physical Health Component Summary Score of SF-36.
Linear regression modeling
Correlation coefficients are presented in Table 3; the results of regression analyses are presented in Table 4. Mindfulness was significantly correlated with all outcomes except for physical health related quality of life (SF-36 PCS), even after adjusting for age, gender, education, disease modifying therapy use, type of MS, stressful life events, and disability status. Adjusted regression analyses indicated that mindfulness accounted for 25% of the variation in perceived stress scores, 44% of the variation in resilience scores, 11% of the variation in adaptive coping strategies and 29% of the variation in maladaptive coping strategies, and 20% of the variation in mental health related quality of life scores (as measured by ΔR2).
Table 3.
Raw correlations for mindfulness, perceived stress, coping, resilience, and quality of life in MS (n=116 – 119)
| Perceived stress | Adaptive coping | Maladaptive coping | Resilience | Mental health QOL | Physical health QOL | |
|---|---|---|---|---|---|---|
| Mindfulness | −0.6* | 0.32* | −0.60* | 0.67* | 0.54* | 0.12 |
| Perceived stress | −0.08 | 0.72* | −0.55* | −0.71* | −0.23┼ | |
| Adaptive coping | −0.19┼ | 0.47* | 0.17 | 0.04 | ||
| Maladaptive coping | −0.58* | −0.68* | −0.21┼ | |||
| Resilience | 0.58* | 0.13 | ||||
| Mental health QOL | −0.04 |
QOL: Quality of life
p < .0001
p < .05
Table 4.
Linear regression analyses of mindfulness predicting psychosocial outcomes.
| Relationship | B | 95% CI | SE | p | Adj. R2 | ΔR2 |
|---|---|---|---|---|---|---|
| Perceived Stress | ||||||
| 1) Mindfulness only | −0.21 | −.27, −.16 | 0.03 | < 0.0001 | 0.31 | |
| 2) Covariates only | 0.19 | |||||
| 3) Covariates + mindfulness | −0.19 | −.25, −.14 | 0.03 | < 0.0001 | 0.44 | 0.25 |
| Resilience | ||||||
| 1) Mindfulness only | 0.47 | .37, .57 | 0.05 | < 0.0001 | 0.44 | |
| 2) Covariates only | 0.01 | |||||
| 3) Covariates + mindfulness | 0.48 | .38, .59 | 0.05 | < 0.0001 | 0.45 | 0.44 |
| Adaptive Coping | ||||||
| 1) Mindfulness only | 0.11 | .05, .17 | 0.03 | < 0.0001 | 0.10 | |
| 2) Covariates only | 0.13 | |||||
| 3) Covariates + mindfulness | 0.12 | .06, .18 | 0.03 | < 0.0001 | 0.24 | 0.11 |
| Maladpative Coping | ||||||
| 1) Mindfulness only | −0.08 | −.10, −.06 | 0.01 | < 0.0001 | 0.35 | |
| 2) Covariates only | 0.08 | |||||
| 3) Covariates + mindfulness | −0.08 | −.10, −.06 | 0.01 | < 0.0001 | 0.37 | 0.29 |
| Mental Health QOL | ||||||
| 1) Mindfulness only | 0.3 | .22, .39 | 0.04 | < 0.0001 | 0.29 | |
| 2) Covariates only | 0.15 | |||||
| 3) Covariates + mindfulness | 0.26 | .17, .35 | 0.04 | < 0.0001 | 0.35 | 0.20 |
| Physical Health QOL | ||||||
| 1) Mindfulness only | 0.07 | −.04, .17 | 0.05 | 0.198 | 0.01 | |
| 2) Covariates only | 0.52 | |||||
| 3) Covariates + mindfulness | 0.05 | −.01, .13 | 0.04 | 0.181 | 0.52 | 0.00 |
- Model 1 is an unadjusted model that includes mindfulness as the predictor variable and perceived stress, resilience, adaptive coping, maladaptive coping, mental health quality of life, or physical health quality of life as the dependent variable.
- Model 2 predicts the dependent variable from the covariates age, gender, education, disease modifying therapy use, type of MS, stressful life events, and disability status.
- Model 3 includes model 2 plus mindfulness as the primary predictor variable.
- B is the unstandardized regression coefficient for mindfulness.
- ΔR2 is the difference between adjusted R2 for models two and three.
Discussion
This is the first study to investigate the relationship between trait mindfulness, perceived stress, and psychosocial outcomes in MS. Those who reported being more mindful in their daily lives were more likely to report lower levels of perceived stress, the use of more constructive coping strategies, increased resilience, and better mental health-related quality of life; and the significance of these relationships was maintained after adjusting for age, gender, education, disability status, DMT use, and type of MS. Our results echo findings from previous studies demonstrating that high trait mindfulness is associated with improved psychological factors in healthy and diseased populations (12,14,15,29) and extend this work by replicating results in MS. Given that the physiology of stress response systems may be altered in MS (10,11), these findings are notable.
Stress and stress-management are important topics for MS research. Current medical management of MS includes disease-modifying and symptomatic therapies, both of which have limitations in compliance due to side effects and cost (30). While DMTs may delay physical progression of MS, they do not completely address the psychosocial challenges faced by those living with chronic illness (30). Many aspects of the disease process are stressful, and several MS studies show that chronic stress can lead to poorer health outcomes (1–4,8,31,32). Notably, Mohr et al. recently demonstrated in a randomized controlled trial that stress-management training had a significant effect on disease activity and reduced the occurrence of new brain lesions in people with relapsing MS (33). Thus, identifying specific factors that may impact the susceptibility to psychological stress in people with MS is essential. While causal relationships cannot be inferred, our data suggest that trait mindfulness may influence stress perception and the response to challenging situations in people who have MS.
Mindfulness may strengthen the stress-response through a relationship with coping. We found that mindfulness was related to type of coping strategy, and participants that reported higher levels of mindfulness were less likely to rely on maladaptive coping strategies such as denial, disengagement, and self-blame, and more likely to utilize adaptive strategies such as information gathering, planning, and seeking out instrumental and social support. Being mindful involves attending to the present moment with acceptance and nonreactivity. Any thoughts, feelings, or sensations that arise are observed with curiosity and allowed to “be.” Acceptance toward painful or unpleasant thoughts and feelings may change the context in which those thoughts and feelings are experienced, and in turn the subjective experience of emotional distress may become less threatening (16). In this way mindfulness may lessen the need to distance oneself from distressing situations and could lead to reductions in the use of avoidant coping strategies like denial or disengagement (16). An attitude of openness and acceptance does not imply that a mindful practice is content with all distressing events; mindfulness should not be confused with complacency. On the contrary, by accepting that a distressing event is happening and observing one’s internal response with curiosity, a mindful person may be empowered to purposefully choose a response or action, rather than react with automatic thought patterns and behaviors. Mindful acceptance can lead to movement and change and in this manner may enhance the use of active, adaptive coping strategies.
Interventions that can improve coping are important for MS. Several studies have found MS patients to disproportionately rely on maladaptive coping strategies, leading to adjustment difficulties, future distress, reduced quality of life, and depressive symptoms (34–38). Alternatively, the use of adaptive strategies by people with MS is related to improved psychological health, including lower levels of depression and better social adjustment (34,39). Few studies have evaluated the ability for mindfulness-based interventions to impact coping style, and our results support future investigation in this area. Because the relationship between mindfulness and maladaptive coping was substantially stronger than mindfulness and adaptive coping, future work should evaluate the ability of mindfulness practice to disengage maladaptive coping strategies as a potential mechanism of action.
Future longitudinal studies should also examine the ability for mindfulness to improve resilience. Several mindfulness-based intervention studies use the term resilience loosely in their reporting, although few, if any, have formally assessed resilience as an outcome. We used the novel CD-RISC to measure resilience in our sample and found a strong correlation with trait mindfulness (r = .67). Qualitatively we found little similarity between questions on the FFMQ and the CD-RISC, suggesting that the strength of the correlation is not due to psychometric overlap but to a genuine relationship that should be further explored.
There are several possible pathways by which mindfulness might improve the capacity for resilience in MS. Being mindful serves to focus awareness on current experience. Observing and attending to the here-and-now may lead to a sense of being fully present during stressful situations with increased clarity and focus for dealing with crisis. By purposefully focusing on the present moment, it is impossible to agonize over what should have happened or anxiously anticipate what might occur. This leads to a “slowing down” of one’s experience, and is often described as room to breathe, or room for choice. In this way, psychologically distressing self-talk is reduced and the mindful brain may be more able to consider a variety of solutions to complex situations.
This study examined trait mindfulness in MS, and while almost everyone has the capacity for self-reflection in this way, people differ in their tendency and ability to sustain mindful-awareness; some are naturally more mindful than others. Mindfulness can be cultivated and enhanced through a variety of factors, including meditation, mind-body practices, and training programs such as mindfulness based-stress reduction (40). Mindfulness-based stress reduction (MBSR) is a formalized program and the most widely researched mindfulness intervention in Western medicine. Participants take part in one class a week for eight weeks in which they are instructed in mindfulness meditation, breath work, yoga postures, self-reflection and awareness. To our knowledge, only one study using mindfulness-based stress reduction has been conducted in MS. Grossman et al. found that MBSR led to significant improvements in depression, anxiety, fatigue, and quality of life (41). In light of these findings, our data support further research of mindfulness training as a stress-management tool for MS. Specifically, investigation of the potential for mindfulness-based interventions to improve coping strategies and enhance resilience in MS is warranted.
This study has limitations. Most participants came from a single center and convenience sampling may have lead to under- or over-representation of certain factors within our sample. Indeed, our participants reported higher levels of education compared to a large North American Research Committee on Multiple Sclerosis (NARCOMS) survey study (N=9107) (42). Even so, education was included as a covariate in our analysis and was not found to significantly impact outcomes. Furthermore, our cross-sectional design does not allow us to determine the direction of the observed relationships. We have predicted mindfulness effects on psychosocial outcomes, but alternative models and explanations should not be ruled out. Despite potential limitations, we found highly significant relationships that warrant further investigation.
Conclusions
Trait mindfulness is significantly associated with decreased psychological stress, a more constructive coping profile, increased resilience, and better quality of life in MS. Whereas some people are naturally mindful, mindfulness is a trait that can be developed and our data support further investigation of mindfulness training to enhance wellbeing and improve the experience of living with MS.
Acknowledgments
Funding
This work was supported by the Oregon Clinical and Translational Research Institute [Grant number UL1 RR024140 from the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health]; the National Center for Complementary and Alternative Medicine of the National Institutes of Health [Grant numbers AT002688 and 2R25AT002878-05A1]; and the Agency for Healthcare Research Quality [Grant number 5T32HS017582-05].
Footnotes
Results of this work were presented at the Symposium for Portland Area Complementary and Alternative Medicine Research annual meeting May 4th, 2013.
Declaration of conflicting interests
The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of this article.
The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Ethical approval
This work was approved by the Institutional Review Board at Oregon Health & Science University, IRB #7989.
Author contributions
Dr. Angela Senders is the principal investigator for this work, she participated in the overall design of the study, conducted the study visits, executed the analysis, and took primary lead in drafting the manuscript. Dr. Douglas Hanes provided statistical support and contributed to the writing of the manuscript drafts. Drs. Lynne Shinto and Vijayshree Yadav are co-investigators, and along with Dennis Bourdette, provided support and mentorship necessary for the success of this work, including critical review of and contributions to the manuscript.
References
- 1.Yamout B, Itani S, Hourany R, et al. The effect of war stress on multiple sclerosis exacerbations and radiological disease activity. J Neurol Sci. 2010 Jan 15;288(1–2):42–4. doi: 10.1016/j.jns.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Golan D, Somer E, Dishon S, et al. Impact of exposure to war stress on exacerbations of multiple sclerosis. Ann Neurol. 2008 Aug;64(2):143–8. doi: 10.1002/ana.21409. [DOI] [PubMed] [Google Scholar]
- 3.Li J, Johansen C, Brønnum-Hansen H, Stenager E, et al. The risk of multiple sclerosis in bereaved parents: A nationwide cohort study in Denmark. Neurology. 2004 Mar 9;62(5):726–9. doi: 10.1212/01.wnl.0000113766.21896.b1. [DOI] [PubMed] [Google Scholar]
- 4.Mohr DC, Goodkin DE, Bacchetti P, et al. Psychological stress and the subsequent appearance of new brain MRI lesions in MS. Neurology. 2000 Jul 12;55(1):55–61. doi: 10.1212/wnl.55.1.55. [DOI] [PubMed] [Google Scholar]
- 5.Lovera J, Reza T. Stress in multiple sclerosis: review of new developments and future directions. Curr Neurol Neurosci Rep. 2013 Nov;13(11):398. doi: 10.1007/s11910-013-0398-4. [DOI] [PubMed] [Google Scholar]
- 6.Mitsonis CI, Potagas C, Zervas I, Sfagos K. The Effects of Stressful Life Events on the Course of Multiple Sclerosis: A Review. International Journal of Neuroscience. 2009 Jan;119(3):315–35. doi: 10.1080/00207450802480192. [DOI] [PubMed] [Google Scholar]
- 7.Artemiadis AK, Anagnostouli MC, Alexopoulos EC. Stress as a Risk Factor for Multiple Sclerosis Onset or Relapse: A Systematic Review. Neuroepidemiology. 2011;36(2):109–20. doi: 10.1159/000323953. [DOI] [PubMed] [Google Scholar]
- 8.Mohr DC, Hart SL, Julian L, et al. Association between stressful life events and exacerbation in multiple sclerosis: a meta-analysis. BMJ. 2004 Mar 27;328(7442):731. doi: 10.1136/bmj.38041.724421.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lecic-Tosevski D, Vukovic O, Stepanovic J. Stress and personality. Psychiatrike. 2011 Dec;22(4):290–7. [PubMed] [Google Scholar]
- 10.Heesen C, Mohr DC, Huitinga I, et al. Stress regulation in multiple sclerosis-current issues and concepts. Multiple Sclerosis. 2007 Jan 29;13(2):143–8. doi: 10.1177/1352458506070772. [DOI] [PubMed] [Google Scholar]
- 11.Gold SM, Mohr DC, Huitinga I, et al. The role of stress-response systems for the pathogenesis and progression of MS. Trends in Immunology. 2005 Dec;26(12):644–52. doi: 10.1016/j.it.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003 Apr;84(4):822–48. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 13.Bränström R, Duncan LG, Moskowitz JT. The association between dispositional mindfulness, psychological well-being, and perceived health in a Swedish population-based sample: Influence of dispositional mindfulness. British Journal of Health Psychology. 2011 May;16(2):300–16. doi: 10.1348/135910710X501683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salmoirago-Blotcher E, Crawford S, Carmody J, et al. Characteristics of Dispositional Mindfulness in Patients With Severe Cardiac Disease. Journal of Evidence-Based Complementary & Alternative Medicine. 2011 Apr 25;16(3):218–25. doi: 10.1177/2156587211405525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carlson LE, Brown KW. Validation of the Mindful Attention Awareness Scale in a cancer population. J Psychosom Res. 2005 Jan;58(1):29–33. doi: 10.1016/j.jpsychores.2004.04.366. [DOI] [PubMed] [Google Scholar]
- 16.Bishop SR, Lau M, Shapiro S, et al. Mindfulness: A Proposed Operational Definition. Clinical Psychology: Science and Practice. 2004;11(3):230–41. [Google Scholar]
- 17.Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011 Feb;69(2):292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983 Dec;24(4):385–96. [PubMed] [Google Scholar]
- 19.Baer RA, Smith GT, Lykins E, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008 Sep;15(3):329–42. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- 20.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 21.Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 22.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–83. [PubMed] [Google Scholar]
- 23.Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992 Jul 18;305(6846):160–4. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Suh Y, Motl RW, Mohr DC. Physical activity, disability, and mood in the early stage of multiple sclerosis. Disability and Health Journal. 2010 Apr;3(2):93–8. doi: 10.1016/j.dhjo.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 25.Shinto L, Yadav V, Morris C, et al. Demographic and health-related factors associated with complementary and alternative medicine (CAM) use in multiple sclerosis. Mult Scler. 2006 Feb;12(1):94–100. doi: 10.1191/1352458506ms1230oa. [DOI] [PubMed] [Google Scholar]
- 26.Myers JK, Lindenthal JJ, Pepper MP, Ostrander DR. Life events and mental status: a longitudinal study. J Health Soc Behav. 1972 Dec;13(4):398–406. [PubMed] [Google Scholar]
- 27.Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res. 1967 Aug;11(2):213–8. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 28.Bermel RA, Weinstock-Guttman B, Bourdette D, et al. Intramuscular interferon beta-1a therapy in patients with relapsing-remitting multiple sclerosis: a 15-year follow-up study. Mult Scler. 2010 May;16(5):588–96. doi: 10.1177/1352458509360549. [DOI] [PubMed] [Google Scholar]
- 29.Bränström R, Duncan LG, Moskowitz JT. The association between dispositional mindfulness, psychological well-being, and perceived health in a Swedish population-based sample. Br J Health Psychol. 2011 May;16(Pt 2):300–16. doi: 10.1348/135910710X501683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zwibel HL, Smrtka J. Improving quality of life in multiple sclerosis: an unmet need. Am J Manag Care. 2011 May;17(Suppl 5):S139–145. Improving. [PubMed] [Google Scholar]
- 31.Ackerman KD, Heyman R, Rabin BS, et al. Stressful life events precede exacerbations of multiple sclerosis. Psychosom Med. 2002 Dec;64(6):916–20. doi: 10.1097/01.psy.0000038941.33335.40. [DOI] [PubMed] [Google Scholar]
- 32.Grant I, Brown GW, Harris T, et al. Severely threatening events and marked life difficulties preceding onset or exacerbation of multiple sclerosis. J Neurol Neurosurg Psychiatr. 1989 Jan;52(1):8–13. doi: 10.1136/jnnp.52.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mohr DC, Lovera J, Brown T, et al. A randomized trial of stress management for the prevention of new brain lesions in MS. Neurology. 2012 Jul 31;79(5):412–9. doi: 10.1212/WNL.0b013e3182616ff9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pakenham KI. Adjustment to multiple sclerosis: application of a stress and coping model. Health Psychol. 1999 Jul;18(4):383–92. doi: 10.1037//0278-6133.18.4.383. [DOI] [PubMed] [Google Scholar]
- 35.Goretti B, Portaccio E, Zipoli V, et al. Coping strategies, psychological variables and their relationship with quality of life in multiple sclerosis. Neurol Sci. 2009 Feb;30(1):15–20. doi: 10.1007/s10072-008-0009-3. [DOI] [PubMed] [Google Scholar]
- 36.Brooks NA, Matson RR. Social-psychological adjustment to multiple sclerosis. A longitudinal study. Soc Sci Med. 1982;16(24):2129–35. doi: 10.1016/0277-9536(82)90262-3. [DOI] [PubMed] [Google Scholar]
- 37.Aarstad AKH, Lode K, Larsen JP, et al. Choice of psychological coping in laryngectomized, head and neck squamous cell carcinoma patients versus multiple sclerosis patients. Eur Arch Otorhinolaryngol. 2011 Jun;268(6):907–15. doi: 10.1007/s00405-010-1417-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hajhashemi A, Vaziripour HD, Baratian H, et al. Recognition of the kind of stress coping in patients of multiple sclerosis. Indian J Psychol Med. 2010 Jul;32(2):108–11. doi: 10.4103/0253-7176.78507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Somer E, Golan D, Dishon S, et al. Patients with multiple sclerosis in a war zone: coping strategies associated with reduced risk for relapse. Mult Scler. 2010 Apr;16(4):463–71. doi: 10.1177/1352458509358714. [DOI] [PubMed] [Google Scholar]
- 40.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York, NY: Delta; 1990. [Google Scholar]
- 41.Grossman P, Kappos L, Gensicke H, et al. MS quality of life, depression, and fatigue improve after mindfulness training: A randomized trial. Neurology. 2010 Sep 27;75(13):1141–9. doi: 10.1212/WNL.0b013e3181f4d80d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Salter AR, Tyry T, Vollmer T, et al. “Seeing” in NARCOMS: a look at vision-related quality of life in the NARCOMS registry. Mult Scler. 2013 Jun;19(7):953–60. doi: 10.1177/1352458512469694. [DOI] [PubMed] [Google Scholar]