Abstract
Objective
Coronary artery calcification (CAC) by the Agatston method predicts cardiovascular disease (CVD), but requires cardiac gated computed tomography (CT) scans, a procedure not covered by most insurance providers. An ordinal CAC score (scored 0-12 based on artery number and extent of calcification involvement) can be measured on standard chest CTs. However, the correlation of ordinal and Agatston CAC scores and the relative association with CVD mortality is uncertain, which we sought to determine.
Design
Nested case-control study
Setting
Community-living individuals undergoing “whole body” CT scans for preventive medicine.
Patients
4,544 consecutive patients with CT scans, were followed from 2000-2009. We selected cases who died of CVD (n=57) and age, sex, and CT slice-thickness matched each to 3 controls (N=171).
Interventions
Cardiac gated 3mm chest CTs and non-gated 6mm standard chest CTs.
Main outcome
CVD death over 9 years follow-up.
Results
The intra- and inter-reader kappa for the ordinal CAC score was 0.90 and 0.76 respectively. The correlation of Agatston and ordinal CAC scores was 0.72 (p< 0.001). In models adjusted for traditional CVD risk factors, the odds of CVD death per 1 SD greater CAC was 1.66 (1.03-2.68) using the ordinal CAC score and 1.57 (1.00-2.46) using the Agatston score.
Conclusions
A simple ordinal CAC score is reproducible, strongly correlated with Agatston CAC scores, and provides similar prediction for CVD death in predominantly Caucasian community-living individuals.
Keywords: calcium, cardiovascular diseases, circulation, imaging, epidemiology
INTRODUCTION
In asymptomatic individuals, quantification of coronary artery calcium (CAC) from electron beam computed tomography (EBCT) scans using the Agatston method is predictive of future cardiovascular disease (CVD) events,1-4 and the American College of Cardiology has recommended CAC scoring for patients classified as having “intermediate” risk by Framingham risk score.5 However, cardiac CT scans require a specific protocol that includes ECG synchronization. It scores both the volume and the density of calcium within the coronary arteries and requires dedicated analysis software. Most health insurance providers do not cover CAC measurement for preventive medicine purposes, and therefore they are rarely used in clinical practice.6 In contrast, standard chest CTs are used commonly for a wide range of clinical indications.
A recent study reported a method of CAC scoring that provided a simple ordinal score between 0 and 12 and could be applied to standard chest CT scans. This method relies exclusively on visual assessment of the proportion of the coronary arteries affected by CAC, and does not require ECG gating or special software.7 If the ordinal CAC score proved predictive of future CVD events, it might provide important information on CVD risk in the large numbers of patients that have already had chest CTs for other clinical indications, and might reduce radiation exposure of a second specialized scan. However, to date, this method has only been tested in smokers undergoing CTs for lung cancer screening.7 Thus, the correlation between the ordinal and Agatston CAC scores in the general community is unknown. In addition, whether or not the ordinal CAC score is associated with future CVD events, and whether the strength of association is similar to that obtained by the Agatston method, is unknown in the general population. Therefore, the purpose of this study was to examine the cross-sectional correlation of the ordinal CAC and Agatston scores, and to compare their respective associations with CVD death in community-living individuals. We hypothesized a priori that the ordinal score would be strongly correlated with the Agatston score, and that their respective associations with CVD death would be similar.
METHODS
Participants
Between 2000 and 2003, 4,544 community-living individuals self-referred or were referred by their primary care physician for CT scanning for preventive medicine purposes in San Diego. The CT scan extended from the base of the skull to the pubic symphysis for all participants. The scanning protocol included distinct segments of the neck, heart, lungs, abdomen and pelvis. The CT scans were not obtained as part of a research protocol. Instead, individuals were predominantly self-referred for screening for coronary artery calcification and calcified atherosclerosis in other vascular beds. Participants were followed through 2009. The CT scan extended from the base of the skull to the pubic symphysis for all participants. The canning protocol included distinct segments of the neck, heart, lungs, abdomen, and pelvis. Scans were performed without radiocontrast. The cardiac scan was conducted using ECG gating and 3 mm slice thickness. When lung scans were included, they were not ECG gated, and used 6 mm slice thickness. All scans were performed using the same Imatron C-150 scanner.
We conducted a nested matched case-control study. During follow-up through 2009, 57 individuals died due to CVD. Each CVD death case was individually matched by age (within 5 years), gender, and CT scan thickness (i.e. 3mm EBCT or 6mm lung scan) with 3 living controls using a random number generator to identify a total of 171 controls. Complete covariate information was required for age, BMI, HDL, and total cholesterols for both cases and controls to avoid need for imputation.
Measurements
Imaging
3 millimeter EBCT scans were used for Agatston CAC scoring in all cases and controls. However, many individuals also had 6mm lung scans. When a 6mm lung CT scan was also available (56% of participants), we used the 6mm lung CTs for the ordinal CAC score in the cases and the 3 controls. All CT scans used in this study were non-contrast. The 6mm scans provide less precise information (more volume averaging), and thus, correlations between the ordinal and Agatston CAC score, and associations of the ordinal score with CVD events would likely provide more conservative estimates for the ordinal vs. Agatston CAC scans when using the 6mm lung scans. Moreover, it provided us the opportunity to test whether standard (non-EBCT) chest CTs were equally predictive in comparison to 3mm scans for CAC scoring by the ordinal method. For the remaining 44% of participants and their controls, 6mm lung scans were not available, thus the ordinal score was calculated from the 3 mm cardiac scans. The study was approved by the University of California, San Diego institutional review board.
Agatston scores were calculated on 3mm EBCTs in all individuals. For the EBCT scans, images were electrocardiographically triggered at 40 or 65% of the R-R interval, depending on the subject’s heart rate at a 3 mm CT slice thickness and CAC was scored as described by Agatston et al.8 In brief, atherosclerotic calcification was defined as a plaque area ≥ 1 mm2 with a density ≥130 Hounsfield units (HU). The calcium score per lesion was calculated by multiplying the area of the contiguous pixels by the corresponding density number using the following scale for density (1 = 130 – 199 Hounsfield units, 2 = 200 – 299 HU, 3 = 300 – 399 HU, 4 = ≥ 400 HU).
Ordinal scores were conducted on 6mm lung CTs when available (32 cases and 96 controls [56% of participants]) and otherwise on the 3mm scans. The right coronary artery, left main, left anterior descending, and left circumflex arteries were each given a score of 0-4 for presence and extent of calcium using the methods described by Shemesh, et. al.7 with 0 (none), 1 (< 1/3 of the artery length calcified), 2 (≥ 1/3 to < 2/3 calcified), and 3 (≥ 2/3 calcified). These scores were summed across the 4 arteries, providing a range of possible scores from 0-12.
Ordinal scoring was conducted by a medical student with no previous experience reading chest CTs (K.J.B.). This investigator was trained in scan reading by another investigator with extensive experience in CVD imaging (M.A.A.). After training, nineteen 6mm chest CT scans were chosen at random, and each of the two investigators scored the scans using the ordinal method blinded to the others’ score, the Agatston score, case/control status, and other clinical data. Intra-reader and inter-reader reliability was determined using Cohen’s kappa, and were 0.90 and 0.76, respectively.
Cardiovascular Disease Death
Mortality was ascertained for the participants through 2009. Using the social security death index (SSDI), patients were cross-referenced with study records to confirm identity. Death certificates were obtained and the underlying and contributing causes of death were adjudicated by study physicians with experience in adjudicating CVD outcomes. CVD-specific mortality included myocardial infarction, stroke, congestive heart failure, coronary artery disease, and other vascular diseases. TIA was not included as a CVD event for cases in this study.
Selection of Controls
Each case was matched with 3 controls. Ages were rounded to the nearest year to facilitate the matching- based on age and gender. Random number generation was used to select the age and sex matched controls. Complete covariate information was required for age, BMI, HDL, and total cholesterol for both cases and controls.
Other Measurements
Age and sex were determined by self-report. A questionnaire was used to obtain medical history of diabetes, smoking, and hypertension and cholesterol medication use. Height and weight were measured and body mass index was calculated (in kg/m2). Casual serum lipid and glucose levels were obtained via finger-stick using the Cholestec LDX system. Diabetes was defined as serum glucose >200, or the use of glucose lowering medications. Dyslipidemia was defined as total cholesterol to HDL cholesterol ratio > 5, or the use of cholesterol-lowering medication. Systolic and diastolic blood pressures were obtained after the patient rested for 5 minutes via a standard protocol from a trained technician. Hypertension was defined as systolic pressure >140 mmHg, diastolic >90 mmHg, or the use of anti-hypertensive medications.
Statistical Analysis
We compared differences in demographics, traditional CVD risk factors, Agatston, and ordinal CAC scores between cases and controls using the Chi Square test or Fisher’s Exact test for categorical variables and the Student T-test or Wilcoxon test for continuous variables, as appropriate. Next, we evaluated the correlations between the Agatston and ordinal CAC scores at baseline separately in cases and controls, and then in all participants together. Given right skewed distributions of both CAC scores, Spearman correlations were used.
To examine the functional form of the association of ordinal CAC score with CVD death, we categorized participants into groups (ordinal CAC score 0, 1-3, 4-6, ≥ 7). To provide a comparison with Agatston CAC score, we defined CAC categories using the Agatston score that included similar numbers of participants as in each ordinal CAC category, and we compared odds of CVD death for each CAC category using staged conditional logistic regression models. An initial model was unadjusted. A second model adjusted for age and sex. A final model additionally adjusted for traditional CVD risk factors (age, sex, diabetes, hypertension, total cholesterol to HDL cholesterol ratio, cholesterol lowering medication use, body mass index, and smoking status [current/former/never]).
We added 1 to each CAC score and natural log transformed the distribution (Ln[CAC + 1]) to more closely approximate a normal distribution. We then evaluated a one standard deviation higher Ln CAC score as our primary predictor variable. In companion analysis, we evaluated a dichotomous score of any CAC (Agatston or ordinal score > 0 vs. none). We tested a multiplicative interaction term to determine whether associations of the ordinal score with CVD death differed among persons with 3mm EBCT scans only vs. 6mm standard chest CT scans, and conducted stratified analyses by scan thickness. All statistical analyses were performed using Stata software version 11 (Stata Corp., College Station, Texas).
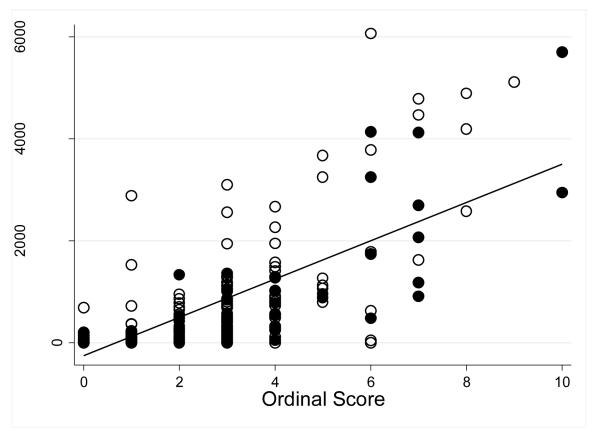
RESULTS
The characteristics of CVD death case and control status are shown in Table 1. Reflecting their use as matching variables, cases and controls were similar by age and sex. The prevalence of hypertension, diabetes, lipid medication use, and smoking were all higher in cases compared to controls. CVD death cases also had higher median Agatston and ordinal scores. The Spearman correlation between the ordinal score and Agatston CAC scores were 0.749 (p < 0.001) in CVD death cases, 0.705 (p < 0.001) in controls, and 0.715 (p < 0.001) when cases and controls were evaluated together (Figure 1).
Table 1.
Baseline Characteristics of CVD Death Cases and Controls.
| The Lifescore Study | |||
|---|---|---|---|
| N |
Cases 57 |
Controls 171 |
P-value |
| Age, years ± SD | 72.3 ± 10.3 | 72.2 ± 9.9 | 0.93 |
| Female n (%) | 15 (26.3%) | 45 (26.3%) | 0.99 |
| Diabetes n (%) | 11 (19.6%) | 3 (1.83%) | 0.01 |
| Hypertension n (%) | 29 (50.9%) | 76 (44.4%) | 0.4 |
| Total Cholesterol, mg/dL ± SD | 195 ± 42 | 209 ± 151 | 0.51 |
| HDL, mg/dL ± SD | 50 ± 20 | 53 ± 18 | 0.35 |
| Cholesterol medication use n (%) | 15 (26.3%) | 24 (14.0%) | 0.03 |
| BMI (kg/m2) ± SD | 26.6 ± 4.2 | 26.5 ± 3.9 | 0.79 |
| Smoking status | 0.11 | ||
| Never | 23 (40.3%) | 88 (51.5%) | |
| Former | 28 (49.1%) | 76 (44.4%) | |
| Current | 6 (10.5%) | 7 (4.1%) | |
| Agatston CAC Score, Median (IQR) | 315 (101, 1024) | 202 (5, 794) | 0.05 |
| Ordinal Score, Median (IQR) | 3 (2, 4) | 2 (1, 3) | 0.01 |
IQR = interquartile range
Figure 1.
Correlation of the Ordinal and Agatston CAC Scores. (Open circles represent CVD death cases, closed circles represent matched controls).
We observed a dose-response relationship between the ordinal score and odds of CVD death (Figure 2). When Agatston scores were grouped into similar sized categories as evaluated using the ordinal score, a similar dose-response relationship was noted comparing the two scoring methods.
Figure 2.
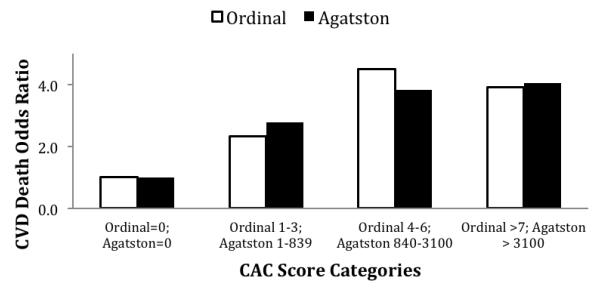
Figure shows unadjusted odds of CVD death by increasing categories of coronary artery calcification, scored by the ordinal and Agatston methods among 57 CVD death cases and 171 age, sex, and CT scan thickness matched controls.
Table 2 shows the associations of the Agatston and ordinal CAC scores with CVD death through a series of multivariable models. In the fully adjusted model, each SD higher Agatston score was associated with a 57% higher odds of CVD death, whereas each SD higher ordinal score was associated with a 66% higher odds; both findings were statistically significant. Point estimates for the odds of CVD death evaluating each score as any CAC vs. none suggested similar strengths of association with CVD death by either score, but neither reached statistical significance. Results were similar irrespective of whether a 3mm EBCT or 6 mm lung scan was used for calculating the ordinal CAC score (p-value for interaction = 0.95).
Table 2.
Association of Agatston and Ordinal CAC Scores with CVD Mortality.
| 0dds Ratio |
95% CI | p-value | |
|---|---|---|---|
| Ln CAC+1 (per SD higher) | |||
| Agatstson | |||
| Unadjusted | 1.62 | 1.11-2.38 | 0.01 |
| Age and Sex Adjusted | 1.61 | 1.10-2.36 | 0.01 |
| Fully adjusted* | 1.57 | 1.00-2.46 | 0.05 |
| Ordinal | |||
| Unadjusted | 1.85 | 1.22-2.81 | < 0.01 |
| Age and Sex Adjusted | 1.86 | 1.23-2.81 | < 0.01 |
| Fully adjusted* | 1.66 | 1.03-2.68 | 0.04 |
| Any CAC vs. None | |||
| Agatston CAC > 0 vs. None | |||
| Unadjusted | 3.05 | 1.01-9.19 | 0.05 |
| Age and Sex Adjusted | 2.94 | 0.97-8.92 | 0.06 |
| Fully adjusted* | 2.23 | 0.67-7.40 | 0.19 |
| Ordinal CAC vs. None | |||
| Unadjusted | 2.32 | 0.93-5.78 | 0.07 |
| Age and Sex Adjusted | 2.44 | 0.97-6.11 | 0.06 |
| Fully adjusted* | 2.38 | 0.81-6.97 | 0.12 |
Adjusted for age, sex, diabetes, hypertension, total/hdl cholesterol ratio, lipid med use, body mass index, and smoking (current, former, never).
DISCUSSION
To our knowledge, this is the first study to compare the ordinal and Agatston CAC score in community-living individuals. We demonstrated that a simple, visually assessed CAC score that determines the extent of coronary calcium on an ordinal scale ranging between 0 and 12 and can be applied to standard chest CTs, had good reproducibility, was strongly correlated with the Agatston score and had similar predictive value for CVD death in community-living individuals. Results were similar when the ordinal CAC score was applied to 6mm non-ECG gated standard lung CT scans and compared to Agatston CAC scores using 3mm EBCT scans. Because lung CTs are done frequently for many clinical indications, these findings suggest that a great wealth of data about future CVD risk may already be available without the need for additional radiation exposure.
The Agatston CAC score is well known to predict future CVD events above and beyond the Framingham risk score.3, 9 However, it requires a dedicated cardiac scan with ECG gating and is not covered by most insurance providers. For example, in 2007, approximately 700,000 CT scans were performed for calcium scoring, while approximately 11 million standard chest CT scans were performed for other clinical indications in the US.10 The ordinal CAC score may provide unique opportunities because it can be applied to standard, non-ECG gated chest CTs. In our experience in this study, it took approximately 2 minutes to read and score each standard chest CT using the ordinal score, which had good to excellent intra- and inter-reader reliability, even with an inexperienced reader. If these results are confirmed, existing chest CT scans could be scored for CAC and would provide important, incremental information for CVD risk stratification. These data could subsequently inform more aggressive risk factor management strategies, including suitability for statin therapy.
A recent high profile study demonstrated that lung-cancer screening using standard chest CTs reduced lung cancer death by 20% and death from any cause by 6.7% compared to chest x-ray screening among smokers.11 This important finding will likely lead to greater use of lung CTs for cancer screening. If so, there will be even greater numbers of chest CTs that could be used to garner information about CVD risk. Additional studies are needed to determine if our results are reproducible in other settings, and to evaluate whether the ordinal score or other modifications12, 13 may have greater reliability, ease of use, and predictive value for future CVD events.
This study is the first to our knowledge to evaluate the ordinal score in community-living individuals. Previous studies have evaluated the association of calcium in thoracic arteries on standard chest CT and abdominal aortic calcification on abdominal CTs used for virtual colonoscopy with CVD events. These studies also found that calcification in these regions were associated with future CVD.12, 13 The ordinal score evaluated here has previously been evaluated in cohorts of smokers who may have greater burden of coronary calcium and higher CVD event risk.7 It is possible that detection of risk in the much larger general population may allow earlier use of appropriate preventive measures, which could lower cardiovascular disease rates.
A key strength of our study is the simultaneous availability of EBCT and chest CT scans and the long-term follow-up for CVD death in a relatively large cohort of community-living individuals. The simultaneous availability of both scans allowed us to compare performance of the ordinal score in 3mm vs. 6mm CTs, to determine the correlation between the CAC scores using the two scoring methods, and to compare their relative strengths of association with CVD death. Our study also has important limitations. The study population was composed of many individuals who self-referred for preventive medicine CT screening, which may limit the generalizability to other populations. Almost all participants were Caucasian, so the ordinal score needs validation in other race/ethnicities. Some study participants had only 3 mm CT scans available for comparison, so the Agatston and ordinal CAC scores were compared on the same CT images in these individuals. While results between the 3 and 6mm scans were comparable, further studies are required to determine the minimal acceptable scan thickness to provide reliable CVD risk information.
In conclusion, we demonstrate that a simple ordinal CAC scoring method is reproducible, strongly correlates with Agatston CAC scores on EBCT scans, and is equally predictive of CVD death in predominantly Caucasian community-living individuals. Thus the 11 million chest CTs done annually in the US may potentially yield valuable information on future risk for cardiovascular events.
ACKNOWLEDGEMENTS
This material is the result of work supported with resources of the VA San Diego Healthcare System. The authors wish to thank Ms. Clydene Nee for administrative support and careful review of this manuscript.
FUNDING SOURCE This study was supported by a grant from the National Heart Lung and Blood Institute (R01HL096851)- Ix; and R01HL116395- Criqui and an American Heart Association Established Investigator Award (14EIA18560026).
Footnotes
DISCLOSURES There are no conflicts of interest to disclose.
REFERENCES
- 1.Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, Flores FR, Callister TQ, Raggi P, Berman DS. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–1870. doi: 10.1016/j.jacc.2006.10.079. [DOI] [PubMed] [Google Scholar]
- 2.Taylor AJ, Bindeman J, Feuerstein I, Cao F, Brazaitis M, O’Malley PG. Coronary calcium independently predicts incident premature coronary heart disease over measured cardiovascular risk factors: mean three-year outcomes in the Prospective Army Coronary Calcium (PACC) project. J Am Coll Cardiol. 2005;46:807–814. doi: 10.1016/j.jacc.2005.05.049. [DOI] [PubMed] [Google Scholar]
- 3.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 4.Budoff MJ, Nasir K, McClelland RL, Detrano R, Wong N, Blumenthal RS, Kondos G, Kronmal RA. Coronary calcium predicts events better with absolute calcium scores than age-sex-race/ethnicity percentiles: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2009;53:345–352. doi: 10.1016/j.jacc.2008.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, Lauer MS, Post WS, Raggi P, Redberg RF, Rodgers GP, Shaw LJ, Taylor AJ, Weintraub WS. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2007;49:378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 6.O’Malley PG, Greenberg BA, Taylor AJ. Cost-effectiveness of using electron beam computed tomography to identify patients at risk for clinical coronary artery disease. Am Heart J. 2004;148:106–113. doi: 10.1016/j.ahj.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 7.Shemesh J, Henschke CI, Shaham D, Yip R, Farooqi AO, Cham MD, McCauley DI, Chen M, Smith JP, Libby DM, Pasmantier MW, Yankelevitz DF. Ordinal scoring of coronary artery calcifications on low-dose CT scans of the chest is predictive of death from cardiovascular disease. Radiology. 2010;257:541–548. doi: 10.1148/radiol.10100383. [DOI] [PubMed] [Google Scholar]
- 8.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr., Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 9.Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, Greenland P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berrington de Gonzalez A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, Land C. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071–2077. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, Marcus PM, Sicks JD. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenland P, Lloyd-Jones D. Time to end the mixed--and often incorrect--messages about prevention and treatment of atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2007;50:2133–2135. doi: 10.1016/j.jacc.2007.05.055. [DOI] [PubMed] [Google Scholar]
- 13.Vehmas T. Visually scored calcifications in thoracic arteries predict death: follow-up study after lung cancer CT screening. Acta Radiol. 2012;53:643–647. doi: 10.1258/ar.2012.120247. [DOI] [PubMed] [Google Scholar]