Abstract
Pachydermoperiostosis, also known as Touraine-Solente-Golé syndrome/Rosenfeld-Kloepfer syndrome/primary or idiopathic Hypertrophic osteoarthropathy, is an autosomal-dominant/autosomal recessive inherited disorder with variable expression. In its complete form, it is characterized by pachyderma (thickening of the facial skin), skeletal changes (periostosis), excessive sweating (hyperhydrosis), and acropachia (digital clubbing). We report a patient with skeletal symptoms, associated with pachyderma and clubbing of fingers. Radiographs of patient showed periosteosis of distal end of long bones.
We review the characteristic features of this syndrome. The patient required a close follow-up because of complications that might develop on the long-term.
Keywords: Pachydermoperiostosis, Touraine-solente-Golé syndrome, Clubbing of fingers
1. Introduction
Pachydermoperiostosis was first described by Friedreich1 in 1868, who called it ‘Hyperostosis of the entire skeleton’. In 1907, Unna named the term ‘cutis verticis gyrate’ for thick, transversely folded skin of scalp and forehead.2 In 1935, three dermatologists, Touraine, et al,3 recognized this condition as a familial disorder with three forms: complete (periostosis and pachyderma), incomplete (without pachyderma) and the forme fruste (pachydermia with minimal skeletal changes). In 1965, Rimoin4 observed affected persons in successive generations.
As per Borochowitz,5 the diagnosis should only be made when at least two out of a family history, clubbing, hypertrophic skin changes, and bone pain/radiographic changes are present. Other authors have suggested different criteria.6,7 Alfred Vogl, suggested that if an affected person exhibits only one or a few of the features of this syndrome, the diagnosis being confirmed by examination of other family members.8
Jajic estimated the prevalence of the disease is 0.16%.9,10 Symptoms usually appear around puberty, with a male to female ratio of 7:1, and males are severely affected.11 In a review of 68 published families with Pachydermoperiostosis, including 204 patients, Castori et al10 found that 37 families showed autosomal dominant inheritance and autosomal recessive inheritance was suggested in the remaining families. Although an autosomal dominant model with incomplete penetrance and variable expression has been proved, both autosomal recessive and X-linked inheritance have been suggested. The main features are digital clubbing, skin changes (flushing, blanching, hyperhidrosis and hypertrophy) causing coarse facial features with thickening, furrowing and excessive oiliness of the skin of the face and forehead. Bone and joint involvement includes arthritis, arthralgia, periosteal new bone formation, subperiosteal ossification, acro-osteolysis and osteoporosis. Gastric hypertrophy, gastric ulcer and other endocrine abnormalities have been described.
An infantile form has been described which is characterized by early presentation with enlargement and delayed closure of the cranial sutures, patent arterial duct and skin manifestations.11 This condition progresses slowly for a few years and is self-limiting thereafter.12
2. Case report
A 32-year-old male, non-smoker, non-alcoholic presented with bilateral knee joint pain, swelling, reduced range of movements and progressive enlargement of both hands, feet for last 10 years. No history of similar condition in family and consanguinity. No history of trauma and fractures.
On examination, patient had pronounced folds in the area of forehead, between the eyes, in the nasolabial grooves and on the chin (Fig. 1). The development of the patient's skin folds was insidious and progressive. Clubbing of all his fingers and toes (Fig. 2) noted. Patient has effusion of bilateral knee joints and terminal knee flexion is restricted (Fig. 3). Patient has symmetrical enlargement of bilateral forearm and legs (Fig. 4). Patient has profuse sweating and seborrhea (Figs. 1 and 5).
Fig. 1.

Pronounced forehead skin folds, prominent nasolabial folds, and seborrhea.
Fig. 2.

Clubbing of fingers.
Fig. 3.

Bilateral knee joint effusion.
Fig. 4.

Column like swelling of legs with clubbing of toes.
Fig. 5.

Sweating at the ankle.
Laboratory analyses showed normal erythrocyte sedimentation rate, C-reactive protein, random blood sugar and serum calcium. Chest X-ray shows enlarged clavicles with normal lung markings (Fig. 6). Radiograph of Pelvis with both hips showed Osteoporosis of iliac bones, mild decrease in joint space of left hip with marginal osteophytes and Irregular cortical thickening of bilateral femur (Fig. 7). Radiograph of bilateral knee showed mild osteoarthritis with decreased medial joint space, Erlenmeyer flask appearance of femur, subperiosteal bone formation of proximal tibia and fibula (Fig. 8). Radiograph of bilateral ankle showed osteoarthritis of ankle joint with irregular subperiosteal bone formation and cortical thickening of distal tibia, fibula, calcaneum and talus (Fig. 9). Radiograph of bilateral hand showed enlargement of distal ulna and radius, metacarpals, phalanges (Fig. 10). Skull radiograph showed thick bones with enlarged scalp tissue (Fig. 11). CT scan of head showed thick soft tissue and thickened skull bones (Fig. 12). Fundoscopy of eyes showed tortious veins (Fig. 13). Microscopy of skin showed increased sebaceous glands and thickened dermis (Figs. 14 and 15).
Fig. 6.

Enlarged clavicles.
Fig. 7.

Irregular cortical thickening of bilateral femur with mild osteoarthritis of hip joints.
Fig. 8.

Subperiosteal bone formation of bilateral tibia.
Fig. 9.

Subperiosteal bone formation of bilateral distal tibiae and fibulae.
Fig. 10.

Enlarged phalanges and metacarpals.
Fig. 11.

Thick skull bones with enlarged scalp tissue.
Fig. 12.
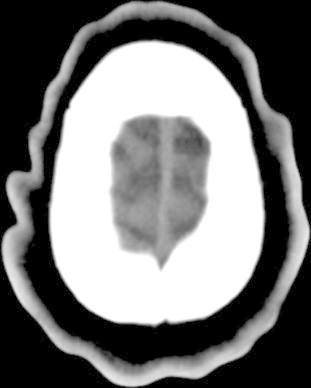
CT scan showing the undulated scalp tissue.
Fig. 13.
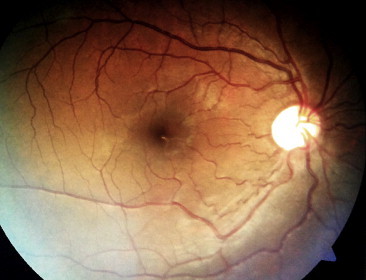
Fundoscopy of eye showing tortious veins.
Fig. 14.
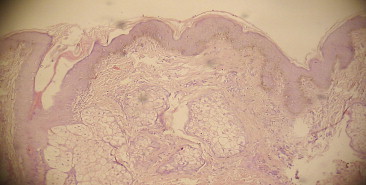
Microscopy finding of skin biopsy with diffuse thickening of dermis (hematoxylin-eosin magnified ×60).
Fig. 15.
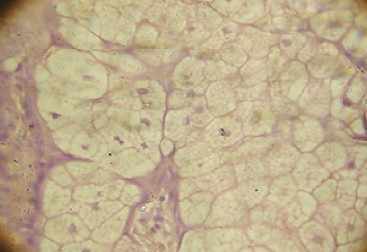
Microscopy showing prominent sebaceous gland.
3. Discussion
The diagnostic criteria for pachydermoperiostosis6,7 are:
Major criteria: pachyderma, periostosis, finger clubbing.
Minor criteria: hyperhidrosis, arthralgia, gastric ulcer, cutis verticis gyrate, blepharoptosis, joint effusion, column-like legs, edema, seborrhea, acne, flushing. Our patient had all three major criteria i.e., hyperostosis, finger clubbing, and pachyderma. Martinez-Lavin 13 proposed the pathology for pachydermoperiostosis is due to increased amount of proliferation of collagen fibers from actively proliferating fibroblasts. Wegrowski14 proposed the pathology for pachydermoperiostosis as dysregulation of the matrix deposits and increased synthesis of decorin protein. These differences are due to difference of stage of disease in the patients.
Some studies explained the role of epidermal growth factor,15 Von Willebrand factor antigen,16 vascular endothelial growth factor,17 and platelet derived growth factor18 in pathogenesis of pachydermoperiostosis. The role of alcohol in pathogenesis of pachydermoperiostosis was proposed by Farrus et al.19
The disease, often hereditary, is transmitted in autosomal dominant form with incomplete penetrance. However, cases have also been described that are transmitted in autosomal recessive form, and also cases with a history of consanguinity. Mutations in the HPGD gene on chromosome 4q34.1 have been found in those with the autosomal recessive form of this condition.20
Pachydermia21—which affects the face and limbs—is the most frequent skin symptom.
The grading of pachyderma is as follows – grade 0:- absence, grade 1:- mild to moderate involvement (cutaneous thickening without puckering), grade 2:- severe (cutaneous thickening and puckering). Patients may also present with seborrhea (90% of cases), acne, folliculitis, dilated pores, hyperhidrosis of the palms and soles (44–67% of cases) may be associated with flushing, thickened eyelids (30–40% of cases), cutis vertices gyrate (24% of cases), and reduced facial and pubic hair.
Digital clubbing is seen in 89% of cases and nail bed capillary microscopy shows slight capillary enlargement and increased tortuosity. Arthritis is seen in 20–40% of cases22 and a joint effusion is seen in 41%. Irregular periosteal ossification affects predominantly the distal ends of long bones seen in 80–97% of patients.
A range of processes (some malignant) has been reported in association with pachydermoperiostosis. These include facial epidermoid carcinoma,23 hypertrophic gastritis, peptic ulcer, gastric adenocarcinoma,24 Crohn disease, and myelofibrosis.25 As a consequence of increased soft tissue bulk and hyperostosis, complications may arise such as ptosis, compression of the nerve endings, hearing problems, kyphosis, arthrosis, osteonecrosis of the femoral head, and carpal tunnel syndrome.
The treatment of pachydermoperiostosis by colchicine, improved the articular symptoms, folliculitis, and pachyderma.26 Rheumatologic symptoms have been improved by intra-venous treatment with pamidronate.27 Isotretinoine showed improvement of the skin symptoms with pachyderma and cutis verticis gyrate.28
Variants of pachydermoperiostosis include Rosenfeld-Kloepfer syndrome (characterized by enlargement of the jaws, especially mandible, and of the hands and feet, nose, lips, tongue, and forehead, along with cutis vertices gyrata and corneal leukoma); Currarino idiopathic osteoarthropathy (an incomplete form of PDP seen in children and adolescents and characterized by the presence of eczema and sutural diastases); and a localized form with only the radiographic features of PDP in the lower extremities.
4. Conclusion
The diagnosis of pachydermoperiostosis is based on the combination of digital clubbing, periostitis and pachyderma with the absence of any cardiovascular, pulmonary, liver, intestinal and mediastinal diseases. It is a rare entity that should be known and differentiated from secondary hypertrophic osteoarthropathy, thyroid acropachy, acromegaly, van Buchem's disease (in which there is absence of clubbing and skin changes), diaphyseal dysplasia (endosteal and periosteal proliferation), syphilitic periostosis and chronic inflammatory rheumatic diseases.29
Conflicts of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Friedrich N. Hyperostose des gesammten skelettes: Virchows. Arch Pathol Anat. 1868;43:83. [Google Scholar]
- 2.Unna P.G. Cutis verticis gyrate. Monastsh PRAKTIS Dermatol. 1907;45:227–233. [Google Scholar]
- 3.Touraine A., Solente G., Gole L. Un syndrome osteodermopathique: la pachydermie plicaturee avec pachyperiostose des extremites. Presse Med. 1935;43:1820–1824. [Google Scholar]
- 4.Rimoin D.L. Pachydermoperiostosis (idiopathic clubbing and periostosis). Genetic and physiologic considerations. New Eng J Med. 1965;272:923–931. doi: 10.1056/NEJM196505062721801. [DOI] [PubMed] [Google Scholar]
- 5.Borochowitz Z., Rimoin D.L. Pachydermoperiostosis. Birth Defects Encyclopaedia. 1990:1349–1350. [Google Scholar]
- 6.Matucci-Cerinic M., Lotti T., Jajic I., Pignone A., Bussani C., Cagnoni M. The clinical spectrum of pachydermoperiostosis. Medicine. 1991;70:208–214. doi: 10.1097/00005792-199105000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Martinez-Lavin M., Pineda C., Valez T. Primary hypertrophic osteoarthropathy. Semin Arthritis Rheum. 1988;17:156–162. doi: 10.1016/0049-0172(88)90017-0. [DOI] [PubMed] [Google Scholar]
- 8.Vogl Alfred, Sidney G. Pachydermoperiostosis. Am J Med. 1962;33:166–187. doi: 10.1016/0002-9343(62)90016-5. [DOI] [PubMed] [Google Scholar]
- 9.Jajic I., Jajic Z. Prevalence of primary hypertrophic osteoarthropathy in selected population. Clin Ex Rheum. 1992;10:73. [Google Scholar]
- 10.Castori M., Sinibaldi L., Mingarelli R., Lachman R.S., Rimoin D.L., Dallapiccola B. Pachydermoperiostosis: an update. Clin Genet. 2005;68:477–486. doi: 10.1111/j.1399-0004.2005.00533.x. [DOI] [PubMed] [Google Scholar]
- 11.Reginato A.J., Shipachasse V., Guerrero R. Familial idiopathic hypertrophic osteoarthropathy and cranial suture defects in children. Skel Radiol. 1982;8:105–109. doi: 10.1007/BF00349574. [DOI] [PubMed] [Google Scholar]
- 12.Martinez-Lavin M. Digital clubbing and hypertrophic osteoarthropathy: a unifying hypothesis. J Rheumatol. 1987;14:6–8. [PubMed] [Google Scholar]
- 13.Martinez-Lavin M. pathogenesis of hypertrophic osteoarthropathy. Clin Exp Rheumatol. 1992;10(suppl 7):49–50. [PubMed] [Google Scholar]
- 14.Wegrowski Z., Gillery P., Serpier H. Alteration of matrix macromolecule synthesis by fibroblasts from a patient with pachydermoperiostosis. J Invest Dermatol. 1996;106:70–74. doi: 10.1111/1523-1747.ep12327267. [DOI] [PubMed] [Google Scholar]
- 15.Bianchi L., Lubrano C., Carrozzo A.M. Pachydermoperiostosis, study of epidermal growth factor and steroid receptors. Br J Dermatol. 1995;132:128–133. doi: 10.1111/j.1365-2133.1995.tb08638.x. [DOI] [PubMed] [Google Scholar]
- 16.Mattuci-Cerinic M., Martinez-Lavin M., Rojo F. Von Willebrand factor antigen in hypertrophic osteoarthropathy. J Rheumatol. 1992;19:765–767. [PubMed] [Google Scholar]
- 17.Silveira L.H., Martinez-Lavin M., Pineda C. Vascular endothelial growth factor and hypertrophic osteoarthropathy. Clin Exp Rheumatol. 2000;18:57–62. [PubMed] [Google Scholar]
- 18.Fonseca C., Martinez-Lavin M., Hernandez-Rodriguez A. Circulating plasma levels of platelet derived growth factor in patients with hypertrophic osteoarthropathy. Clin Exp Rheumatol. 1992;10(suppl 7):72. [Google Scholar]
- 19.Farrus M., Ortiz G., Pou R. Hypertrophic osteopathy and acropachy associated with noncirrhotic alcoholic liver disease. Apropos a case. Aten Primaria. 1989;6:246–248. [PubMed] [Google Scholar]
- 20.Uppal S., Diggle C.P., Carr I.M. Mutations in 15-hydroxyprostaglandin dehydrogenase cause primary hypertrophic osteoarthropathy. Nat Genet. 2008;40:789–793. doi: 10.1038/ng.153. Note: Erratum: Nature Genet. 40: 927 only, 2008. [DOI] [PubMed] [Google Scholar]
- 21.Kabi F., Mkinsi O., Janani S., Raissouni N. Pachydermoperiostosis. A case report. J Intern Med. 2006;27:710–712. doi: 10.1016/j.revmed.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 22.Schumacher H.R., Jr. Hypertrophic osteoarthropathy: rheumatologic manifestations. Clin Exp Rheumatol. 1992;10:35–40. [PubMed] [Google Scholar]
- 23.Lee S.C., Moon H.J., Cho D. Pachydermoperiostosis with cutaneous squamous cell carcinomas. Int J Dermatol. 1998;37:693–696. doi: 10.1046/j.1365-4362.1998.00518.x. [DOI] [PubMed] [Google Scholar]
- 24.Ikeda F., Okada H., Mizuno M. Pachydermoperiostosis associated with juvenile polyps of the stomach and gastric adenocarcinoma. J Gastroenterol. 2004;39:370–374. doi: 10.1007/s00535-003-1304-7. [DOI] [PubMed] [Google Scholar]
- 25.Bachmeyer C., Blum L., Cadranel J.F., Delfraissy J.F. Myelofibrosis in a patient with pachydermoperiostosis. Clin Exp Dermatol. 2005;30:646–648. doi: 10.1111/j.1365-2230.2005.01891.x. [DOI] [PubMed] [Google Scholar]
- 26.Mattuci-Cerinic M., Lotti T., Jajic I. The medical and surgical treatment of finger clubbing and hypertrophic osteoarthropathy. A blind study with colchicine and a surgical approach to finger clubbing reduction. Clin Exp Rheumatol. 1992;10(suupl 7):67–70. [PubMed] [Google Scholar]
- 27.Guyot-Drouot M.H., Solau-Gervais E., Cortet B. Rheumatologic manifestations of pachydermoperiostosis and preliminary experience with bisphosphonates. J Rheumatol. 2000;27:2418–2423. [PubMed] [Google Scholar]
- 28.Beauregard S. Cutis verticis gyrate and pachydermoperiostosis. Several cases in a same family. Initial results of the treatment of pachyderma with isotretinoin. Ann Dermatol Venereol. 1994;121:134–137. [PubMed] [Google Scholar]
- 29.Goyal S, Schwartz RA, Richards GM, Goyal R. Pachydermoperiostosis. Available from: http://www.emedicine.com. [Cited on 2006]. [Updated on 2008 Apr 30].


