Abstract
OBJECTIVE
To develop a framework that describes the most important symptom outcomes for anal incontinence treatment from the patient perspective.
METHODS
A conceptual framework was developed by the Pelvic Floor Disorders Network based on four semi-structured focus groups and confirmed in two sets of 10 cognitive interviews including women with anal incontinence. We explored: 1) Patient preferred terminology for describing anal incontinence symptoms; 2) Patient definitions of treatment “success”; 3) Importance of symptoms and outcomes in the framework; 4) Conceptual gaps (defined as outcomes not previously identified as important). Sessions were conducted according to grounded theory; transcribed, coded, and qualitatively and quantitatively analyzed to identify relevant themes. Content and face validity of the framework was further assessed using cognitive interviews.
RESULTS
Thirty-four women participated in focus groups and 20 in cognitive interviews. Overall, 29 (54%) were aged 60 years or older, 42 (78%) were Caucasian and 10 (19%) had a high school degree or less. Two overarching outcome themes were identified: “Primary Bowel Leakage Symptoms” and “Ancillary Bowel Symptoms”. Subdomains important in Primary Bowel Leakage Symptoms included leakage characteristics (symptom frequency, amount of leakage, symptom bother) and conditions when bowel leakage occurs (predictability, awareness, urgency). Subdomains important under Ancillary Bowel Symptoms included emptying disorders (constipation, obstructed defecation, and wiping issues) and discomfort (pain, burning). New outcomes identified included predictability, awareness, wiping issues, and discomfort.
CONCLUSIONS
Women with anal incontinence desire a wide range of symptom outcomes after treatment. These are captured in our conceptual framework, which can aid clinicians and researchers in assessing anal incontinence..
INTRODUCTION
Female anal incontinence can be a debilitating problem and is associated with medical, social and economic problems.(1–3) In this paper the term anal incontinence is a medical term and accidental bowel leakage (ABL) is a patient perspective term for the involuntary loss of any stool, mucous, fluid or flatus. The prevalence of anal incontinence ranges from 0.5% to 50% (4),(5) and is associated with depression, anxiety, shame and a negative impact on a woman’s quality of life.(2, 6, 7)
Treatments for anal incontinence are primarily aimed at improving symptoms and quality of life. Therefore, the outcomes used by clinicians and researchers to determine treatment “success” should capture the most important and desired outcomes from the patient’s perspective. However, little attention has been given to how to best include the patient voice for anal incontinence outcomes. This results in a limited understanding and assessment of outcomes, which may be most important to patients in clinical trials and the everyday care. Highlighting this, a 2008 National Institutes of Health State of the Science Consensus Conference (8) and large reviews have emphasized the need to develop patient-based anal incontinence symptom severity measures.(9–11)
Qualitative research methods are an important tool to help understand patients’ experiences with a condition and incorporate the patient voice into outcome measures. These methods inform the development of a conceptual framework which helps capture the patient perspective.(12) The objective of this study was to develop a patient-based conceptual framework that captures the range of symptoms experienced and treatment outcomes important to women with anal incontinence.
MATERIALS AND METHODS
A conceptual framework is a theoretical representation which defines the concepts of interest, their interfaces, and possible determinants.(13) It can lend structure, content, coherence and plausibility to concepts being measured. For this framework, we decided a priori to focus on the range of anal incontinence symptoms and symptom outcomes, in line with recommendations from the 2008 NIH Consensus and Cochrane recommendations.(8–11) We did not focus on quality of life in this study because there are existing validated questionnaires for this domain.(14) Although we recognize that anal incontinence symptoms have a negative impact on quality of life we chose to focus on the most pressing gap in the literature at this time: anal incontinence symptoms and symptom severity.
Our initial framework was based on a modified framework for female urinary incontinence.(15) Through literature review we identified 140 symptom items from 23 validated anal incontinence questionnaires, which we coded based on the initial framework. The framework was revised by adding new concepts through this coding process. Previous reviews have described the questionnaires and measures used throughout the process.(16)
We refined our framework using focus groups and cognitive interviews. Participants were recruited from the clinical offices of eight sites in the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Pelvic Floor Disorders Network (PFDN). Focus groups were conducted in July 2012 at 4 PFDN sites: Cleveland Clinic, the University of Alabama at Birmingham, University of California-San Diego and Kaiser Permanente San Diego, and University of New Mexico, Albuquerque, New Mexico. Cognitive interviews were conducted between October 2012-January 2013 at the other 4 PFDN sites: University of Pennsylvania, University of Pittsburgh Medical Center, Duke University Medical Center, and Women and Infants Hospital, Brown Medical School. No one participated in both focus groups and cognitive interviews. All sites received approval through their respective Institutional Review Boards. Details of the study (either focus groups or cognitive interviews) were provided to the subjects and if willing to participate and eligible, informed consent was obtained from the subject. A $75 patient incentive was discussed with subjects at time of consent and paid to participants at the conclusion of each session.
Inclusion criteria included: (1) female, (2) 18 years or older, (3) diagnosed with anal incontinence by a clinician at one of the PFDN sites, (4) bothersome anal incontinence for at least 3 months, (5) able to give informed consent, (6) able to speak, read, and comprehend English. Women were excluded for: (1) stool consistency over the last 3 months that included types 1 (separate hard lumps) or 7 (entirely liquid) on the Bristol Stool Form Scale,(17) or (2) diagnosis of colorectal or anal malignancy, inflammatory bowel disease, recto-vaginal fistula, existing diagnosis of rectal prolapse or history of pelvic floor or abdominal radiation. The Bristol Stool Form Scale classifies stool consistency into seven categories ranging from “Type 1” (separate hard lumps, like nuts) to “Type 7” (watery, no solid pieces, entirely liquid). Types 1–2 generally indicate constipation, Types 3–5 reflect “normal stool”, and Types 6–7 indicate loose stool and diarrhea. Therefore, we excluded women who almost exclusively reported either Type 1 (only hard) or Type 7 (only liquid) as these may represent medical conditions that are transient. Participants could experience a range of stool consistencies. Inclusion and exclusion criteria were the same for focus groups and interviews. Subjects were not required to have any specific evaluation or testing for eligibility.
We used focus group methodology to refine our framework, which allowed us to elicit feedback directly from participants. In brief, a focus group is a qualitative methodology that involves a structured discussion with a small group of 6–12 participants who have a particular condition in common.(18) A trained moderator facilitates the discussion using a guide, which outlines questions, topics, or both to be covered, while also permitting flexibility for the group to reveal insights that may not have been anticipated in the guide. The data from the focus group is collected onto a transcript of the discussion, which is then coded into themes using qualitative analyses. The group allows participants to interact with each other and the resulting group dynamic generally fosters greater discussion than individual interviews.
The 90-minute focus groups were conducted at 4 different sites to provide geographic diversity by an experienced female moderator from the data coordinating center (RTI International). Following the principles of grounded theory, we decided a priori to conduct focus groups iteratively until saturation (in which no new concepts or themes emerged) was reached.(19) Our final number of 4 focus groups is consistent with guidance from Krueger(18) and others suggesting that 3–6 focus groups are generally sufficient for achieving saturation. Each script was reviewed and refined prior to each session and included the following content: 1) Patient-preferred terminology; 2) Patient definitions of treatment “success”; 3) Relevance of symptom and outcomes in framework; 4) Conceptual gaps (defined as themes not previously identified in the working framework).
The transcripts were analyzed using NVivo10, (QSR International, 2012). Two psychometricians from RTI International (CMB and AW) coded data based on categories from the conceptual framework. The transcripts were also reviewed to identify additional common themes using qualitative content analysis.(20) The coding process involved combing the data and marking the text (terms or phrases) with the appropriate sub-theme label. Any emerging themes were discussed and the analytical framework amended accordingly. After the coding was completed a series of thematic charts, or matrices, were set up, each defined relating to a each different unique thematic issue.(21) The coded data from each focus group and each participant was sorted and organized according to the thematic charts. In this way, the data are ordered in a systematic way that is grounded in participants’ own accounts, mapping the women’s experiences, thoughts and opinions. Finally, because the goal of our qualitative research was to provide an opportunity for patients to have direct input, we did not omit themes that were identified as important to participants from our framework.
Cognitive interviews were conducted following analysis of data from focus groups. These one-on-one interviews were aimed primarily at testing new questions that were developed, but we used them also to assess the face and content validity of our framework. As such, the information relevant to our framework is reported here but the full details related to the final questionnaire validation process will be reported elsewhere. Specific to the framework, we asked patients for feedback on whether there were symptoms that were not covered by our framework and whether the symptoms included were relevant.(22) Participants were asked to rank symptoms and outcomes as “not important at all”, “important”, or “very important”. Our objective was to refine the framework to ensure it captured the range of symptoms experienced and treatment outcomes important to women and not necessarily to compare the focus group and interview participants; therefore, statistical comparisons between focus and cognitive interview groups were not performed. In general, 20 iterative interviews are felt to be sufficient to achieve this goal.(23)
Each of the 4 sites conducted 5 interviews to maximize geographic representation. Interviews were conducted by experienced personnel after web-based training to ensure standardization of technique. This was also an iterative process, and after the first 10 interviews, all notes were qualitatively reviewed in a debriefing session with the interviewers, two team members (RGR and VWS), and an RTI survey methodologist (CMB); the items and interview script were then modified as appropriate. An additional 10 interviews were then conducted and findings reviewed in a debriefing session with the protocol team.
Frequencies and percentages of demographic characteristics and responses to the screening questionnaire were analyzed using SAS version 9.3.
RESULTS
Table 1 presents participant demographic and clinical characteristics. Thirty-four of 49 screened, women participated in the focus groups. Eight did not meet eligibility criteria and seven did not attend for unknown reasons. Mean age was 60 ± 12 years. Twenty-nine participants (54%) were aged 60 or older. All of the 20 women recruited for cognitive interviews participated and had a mean age of 62 ± 11 years.
Table 1.
Demographic and Clinical Characteristics of Focus Group and Cognitive Interview Participants
| Characteristic | Focus Groups (n=34) | Cognitive Interviews (n=20) |
|---|---|---|
|
|
||
| Education* | ||
| Less than high school | 1 (3) | 0 (0) |
| High school diploma or equivalent | 7 (21) | 2 (10) |
| Some college | 9 (26) | 10 (50) |
| College degree or higher | 16 (47) | 8 (40) |
| Race and ethnicity* | ||
| Black | 3 (9) | 4 (20) |
| White | 26 (76) | 16 (80) |
| Hispanic | 4 (12) | 0 (0) |
| Bristol Stool Form Scale | ||
| Sausage-shaped but lumpy (Type 2) | 5 (15) | 2 (10) |
| Like sausage or snake with cracks on its surface (Type 3) | 3 (9) | 4 (20) |
| Like a sausage or snake, smooth and soft (Type 4) | 10 (29) | 6 (30) |
| Soft blobs with clear cut edges (Type 5) | 5 (15) | 3 (15) |
| Fluffy pieces with ragged edges, a mushy stool (Type 6) | 9 (26) | 5 (25) |
| Multiple options selected | 2 (6) | 0 (0) |
Data are as n (%) unless otherwise specified.
One participant did not provide information on education, one participant responded “other” for Race.
While participants used a mixture of medical terms and lay language to describe their condition the term “leakage” was preferred to ‘incontinence’. Some women reported that the term “anal” was negative: “… when you say ‘anal’… people shy away from more discussion.” Another group agreed that the term ‘anal’ “shuts people down” and the term “fecal” caused emotional embarrassment. The common use of “bowel” and “leakage” supported the term “accidental bowel leakage” (ABL) as what is most preferred by patients, thus in our framework, the term “bowel leakage” is used.
A refined conceptual framework incorporating our findings is presented in Figure 1. Table 2 presents the themes and abridged remarks from participants supporting the domains in the framework. The two primary domains identified included Primary Bowel Leakage Symptoms and Ancillary Bowel Symptoms.
Figure 1.
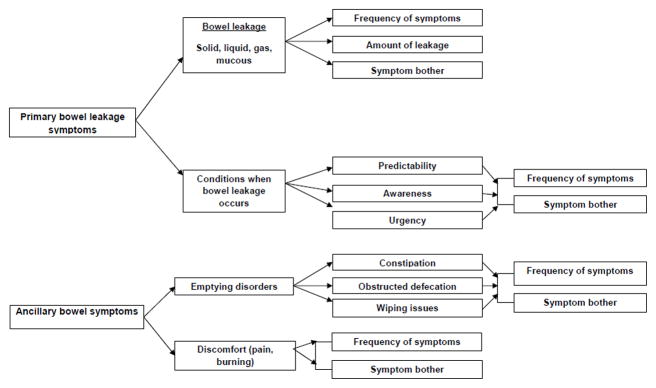
Conceptual framework for bowel leakage symptom outcomes in women
Table 2.
Themes and Sample Quotes From Focus Groups Exploring Symptoms and Outcomes Important to Patients With Accidental Bowel Leakage
| Domains and Sub-domains | Participant Quotes |
|---|---|
| Primary bowel leakage symptoms | |
| Bowel leakage (gas, mucus, liquid, solid) | “One thing diapers do not control is liquid stool and when I have them, liquid stools start coming out, there’s no stopping it..” “I have mucus all day, every day. It’s very annoying. I have my incontinence pad and I stick cotton squares or Kleenex at the crack.” “When I am walking or exercising I feel this boop boop boop – bubbles behind you. And you hope no other walkers are there.” |
| Predictability | “I never know when I’m going to have a bowel movement and that’s the real problem—is the not knowing.” “It’s just this weight of this fear, that it’s coming and I don’t know when.” |
| Awareness | “I don’t even know that it’s coming out.” |
| Urgency | “There’s no controlling [the urge] … when you’re sitting in a car driving home and it starts you can’t squeeze anything tight enough, nothing, you just have to sit in it until you get home and hope the neighbors aren’t out there..” |
| Ancillary bowel symptoms | |
| Constipation | “It’s mainly when I’m constipated and then [bowel leakage] will be days after it.” |
| Obstructed defecation | “Sometimes it’s so soft that it will just not come out…I’ve got a part that just won’t come out so I wipe, and I wipe, and I wipe, and the next time it’s in my panties then”. |
| Wiping and cleanliness | “It’s loose and it keeps coming and you’re wiping and a few minutes later you’re back in the bathroom wiping, or you’ve had an accident that you didn’t know you had.” |
| Discomfort |
Prior to having a bowel movement or leakage: “like someone’s cutting a knife up your rectum.” After having leakage: “the wetness and burning, very uncomfortable. It’s horrible.” |
“Primary Bowel Leakage Symptoms” assesses the presence of leakage symptoms and characteristics that can impact a patient’s perception of the severity including: 1) type of stool leakage; 2) the frequency of occurrence; 3) the amount (volume) of leakage; and 4) a woman’s associated subjective feelings of bother. In addition, other conditions that impacted “how severe” a woman considers her condition included: 1) predictability of ABL; 2) awareness that ABL occurred; and 3) urgency associated with ABL. Because women may not always be aware of the exact etiology of their symptoms, this domain assesses symptoms without causal attribution.
Women commonly discussed the impact of stool consistency, ranging from solid (often described as “pellets”) to liquid (diarrhea and “soft”) and the importance of capturing stool type. “I go from the diarrhea to firm and whether it’s firm, whether it’s loose, whether I’m having the pellets, it’s still incontinence.” In general, liquid or loose stool was considered more problematic than solid stool because it is harder to contain and hide. Many women reported that making stools firmer would represent symptom improvement.
The volume and frequency of leakage were important themes. Leakage volumes tended to be larger with liquid stool types “Woke up one day with huge diarrhea.” Regarding frequency of leakage, participants tended to have fairly severe leakage with the majority experiencing at least weekly and most with daily leakage. Some women did comment on the variability of symptom frequency: “I can be fine for a week, then the next week I can, you know, I can have the floods of the world.” Decreasing both the volume and frequency of leakage were identified as important treatment outcomes to women.
Leakage of mucus and gas were also a consistent theme. While women often did not express embarrassment due to the odor of accidental flatulence, they were bothered if there was sound associated. Other women associated accidental flatulence as a trigger of subsequent leakage of stool: “if I had a gas attack, I have leakage, just a small leakage”. These findings support that it was important to include all types of leakage including mucous and gas in our framework.
We found that many aspects of bowel leakage could contribute to the “bother” of symptoms from an individual patient perspective. For example, type of stool leakage, volume or quantity of leakage, the frequency of leakage events and the impact on a woman’s life all contributed to how bothered a woman may be by the condition, or how “severe” she perceived her condition to be; and in turn how she defined treatment success. In addition, noise and odor associated with bowel leakage (any type) were important contributors of symptom bother. These findings supported the importance of including “bother” as a separate sub-domain.
Women also commonly discussed “conditions when bowel leakage occurs” that could impact the subjective bother or perceived severity of an episode. This included whether participants were aware that leakage had occurred, whether it was predictable, and whether there was urgency associated with the event.
Awareness of when bowel leakage occurred and the inability to distinguish flatus from fecal or mucus material were identified as important concepts that were missing from our preliminary framework. Women referred to the inability to determine when they had leakage and “discovering” fecal material in their pants or underwear and not knowing when the loss had occurred: “I walk my dogs 2 or 3 times a day. I’ll come home and my pants are full and I don’t even know it.” Increased awareness of bowel leakage, fecal smearing, staining, or both were ranked as important aspects of successful treatment because it would allow women to more adequately plan for containment of bowel leakage and bathroom access.
The concept of awareness was linked to the predictability of leakage episodes. While some women reported no warning or sensation with bowel leakage, others found that they were occasionally able to predict when leakage would occur only with atypical warning symptoms such as a “sort of fullness” followed by “a sharp pain,” or “cramping.” When women had difficulty determining the difference between passing gas or fecal material, this contributed to the feeling of unpredictability.
While a few women noticed a pattern to their symptoms (e.g., first thing in the morning, while driving, during sex), the majority reported that they never knew when they would experience leakage. They could suddenly have leakage without warning: “Because you don’t know when it’s going to come. It’s just this weight of this fear, that it’s coming and I don’t know when.” The unpredictability of the symptoms had an impact on their lives, causing them to limit their social interactions or forego some activities they previously enjoyed. Many commented that improving the predictability would at least allow them to plan their daily lives around their condition.
Urgency also impacted how bother a woman felt. Three aspects of urgency associated with bowel leakage included not having enough lead time when an urge to defecate started, the inability to delay an urge, and discomfort associated with urge. “I can’t hold it more than 10 seconds, when it happens”; “…I’d be in [large chain store] and the bathroom’s way in the back and I’ve had to like just take off practically running and still not make it.” Some women reported discomfort when the urge started, although women primarily focused on the inability to suppress a leakage episode when an urge was perceived. Decreasing the associated urgency was also identified as an important treatment outcome. “If I had enough time to make it to the bathroom before it starts to come out, that for me would be a measure of success.”
The second domain in our framework is “Ancillary bowel symptoms”, which includes symptoms that may be ancillary but related to anal incontinence events. These sytmptoms either cause an exacerbation of symptoms, or are related bowel symptoms that may be caused by bowel leakage. Potential exacerbating factors identified included emptying disorders, such as constipation and obstructed defecation, and wiping issues. Symptoms that may be caused by bowel leakage included pain and discomfort that could be either associated with or caused by the leakage, and also potentially wiping issues.
Regarding emptying disorders, several women in the focus groups reported bothersome constipation symptoms: “I am not emptying all the way at one time”. Some women described a relationship between symptoms of constipation and bowel leakage. For example, one stated that “every once in awhile I get so constipated that I cannot go…and then I know for about three days afterwards, I have leakage”. The sensation of obstructed defecation was also frequently discussed, which may be described as difficulty in evacuation or emptying the rectum. This may occur with or without symptoms of constipation. One woman described bowel leakage in the setting of obstructed defecation and soft stools: “sometimes it’s so soft that it will just not come out…I’ve got a part that just won’t come out so I wipe, and I wipe, and I wipe, and the next time it’s in my panties then”.
Feeling unclean and having to wipe repeatedly after bowel movements emerged as important themes. One participant noted “I think the worst part for me is just never feeling clean. I hate not feeling clean.” Participants emphasized difficulty feeling clean and needing to wipe repeatedly after a bowel movement or leakage: “then I’ve got that part that just won’t come out so I wipe and I wipe and I wipe and the next time I see my panties then I go to the bathroom again and the same thing;” As such, it was unclear if this issue represented a manifestation of difficulty with bowel emptying or was directly related to leakage. Nonetheless, improvement in this symptom was commonly endorsed as an important outcome by women.
Many participants described having pain symptoms prior to having an urge to defecate as well as after or as a result of having bowel leakage. Symptoms occurring prior to a bowel movement were described as: “There’s a pressure”, “I don’t like the fullness” and “like someone’s cutting a knife up your rectum.” The most common symptoms described included pain and discomfort that was a result of or occurred after an episode of leakage, causing irritation of the skin: “Just like a child’s bottom when they go to the restroom;” “burning, irritation… anal canal and their rectum gets burned and sore”.
The cognitive interviews supported the comprehensiveness and relevance of our framework. We further explored “discomfort and pain” in interviews. Participants reported 3 “categories” of discomfort including abdominal cramping, rectal pain, and skin irritation from contact with stool. Participants endorsed that all 3 categories of discomfort were important to include in the framework. Therefore, the general construct of “discomfort” remained in our refined framework. No additional themes were identified through the interviews, supporting saturation.
Discussion
Our focus groups provided important information about how women describe their ABL experiences and symptoms and allowed them to prioritize concepts and themes. We also gained a better perspective on patient-preferred terminology for the identified themes. This information is important for clinicians caring for women with this condition, and can facilitate sensitive and appropriate discussion about symptoms and treatment options between clinicians and patients.
Self-reported measures of ABL symptom severity have focused primarily on frequency, coping mechanisms, and impact on quality of life.(24) Our framework identifies other important patient centered aspects that contribute to ABL severity and bother. Our findings that many aspects can moderate a patient’s perception of severity support recommendations from NIH and other authors to develop and include patient-reported outcomes PROs that capture relevant outcomes from the patient perspective.(8) Our findings that the terms “anal” and “fecal” may be problematic from the patient perspective are also in line with previous studies. Although the terms anal incontinence and fecal incontinence FI are medical terms commonly used by health care providers, the term “accidental bowel leakage” may be more patient-friendly and appropriate. In a survey conducted among 1096 US women with fecal incontinence, 71% of the respondents preferred the terminology, “accidental bowel leakage” over “bowel or fecal incontinence”.(25)
Although we intentionally did not focus on the impact of ABL on quality of life, it was clear in this study that ABL has a dramatic impact on women’s lives. Some themes brought up by women included: emotional, social, physical, sexual, and occupational impact, lifestyle adaptation to minimize symptoms, impact on others, stigma, and the management of symptoms. Not only did ABL affect the way women felt about themselves, it also affected how they lived their lives. Specific emotions described included feelings of stress, anxiety, embarrassment, depression, fear and loneliness.
Some of the limitations of this study are inherent to the use of a qualitative focus group and cognitive interview approach. Only women who agreed to participate in these sessions were included in our analysis and their views were incorporated into our framework. Also, we were not able to conduct an in-depth exploration of all identified subdomains. While the impact of ABL on quality of life and functioning was discussed by participants in all groups, we did not examine these constructs in detail given that our primary aim was focused specifically on ABL symptoms. Our framework may also only reflect the participants included and may not be applicable to other excluded conditions. Although the cognitive interview group appears to be more educated, no new themes were identified through the interviews, further supporting comprehensiveness. We emphasize that this framework captures ABL symptoms and contributors without causal attribution. Finally, although the 8 Pelvic Floor Disorders Network sites represent good geographic coverage the number of subjects participating at each site ranged from five to eleven.
The primary strength of our study is that we gained information directly from women suffering from ABL and developed a patient-centered framework for ABL symptoms with face and content validity. This work is critical for advancing patient-centered outcomes research. Because there has been little work thus far in developing a framework, the majority of existing questionnaires may not capture all symptoms and outcomes important to women. However, our work can help guide future development of ABL symptom measures and the design of clinical trials and help keep patient preferences central. More importantly, for clinicians interpreting study findings our framework can improve the transparency of the potential strengths, weaknesses and relevance of outcome measures used by detailing what is most important to patients. Finally, this information is important for clinicians taking care of women because it improves the understanding and recognition of the full breadth and scope of this problem from the patient perspective.
Acknowledgments
Supported by National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development grants K23HD060665 (PI: Sung), and HD054215, HD041261, HD041267, HD069010, HD069013, HD069006, HD054214, HD069025, HD069013 and the NIH Office of Research on Women’s Health.
Footnotes
Presented at the American Urogynecologic Society 34th Annual Scientific Meeting, October 16–19, 2013, Las Vegas, NV.
Financial Disclosure:
Rebecca Rogers is a DSMB Chair for the TRANSFORM trial, sponsored by American Medical Systems. She receives royalties from UpToDate for her chapter on pelvic organ prolapse. Emily Lukacz has been a consultant and received research grants from Renew Medical, Inc., and Pfizer. She has received a research grant from Boston Scientific, has been a consultant to AMS, and she has received a stipend for CME program development from MedEdicus. She has also received: an educational grant from Johnson & Johnson and Ethicon; research grant support from NIH and NICHD; research grant support, travel reimbursement, and honoraria from NIH and NIDDK; research funding from AUGS; and medicolegal expert witness fees from various sources. The other authors did not report any potential conflicts of interest.
References
- 1.Dunivan GC, Heymen S, Palsson OS, von Korff M, Turner MJ, Melville JL, et al. Fecal incontinence in primary care: prevalence, diagnosis, and health care utilization. Am J Obstet Gynecol. 2010 May;202(5):493, e1–6. doi: 10.1016/j.ajog.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bharucha Zinsmeister, Locke Seide, McKeon Schleck, et al. Prevalence and Burden of Fecal Incontinence: A Population-Based Study in Women. Gastroenterology. 2005;129(1):42. doi: 10.1053/j.gastro.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Brown HW, Wexner SD, Segall MM, Brezoczky KL, Lukacz ES. Quality of life impact in women with accidental bowel leakage. International Journal of Clinical Practice. 2012;66(11):1109–16. doi: 10.1111/ijcp.12017. [DOI] [PubMed] [Google Scholar]
- 4.Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213–40. doi: 10.1002/nau.20870. [DOI] [PubMed] [Google Scholar]
- 5.Omotosho TB, Rogers RG. Evaluation and treatment of anal incontinence, constipation, and defecatory dysfunction. Obstet Gynecol Clin North Am. 2009 Sep;36(3):673–97. doi: 10.1016/j.ogc.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Whitehead WE, Borrud L, Goode PS, Meikle S, Mueller ER, Tuteja A, et al. Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology. 2009 Aug;137(2):512–7. 7e1–2. doi: 10.1053/j.gastro.2009.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melville JL, Fan MY, Newton K, Fenner D. Fecal incontinence in US women: a population-based study. Am J Obstet Gynecol. 2005 Dec;193(6):2071–6. doi: 10.1016/j.ajog.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 8.Landefeld CS, Bowers BJ, Feld AD, Hartmann KE, Hoffman E, Ingber MJ, et al. National Institutes of Health state-of-the-science conference statement: prevention of fecal and urinary incontinence in adults. Ann Intern Med. 2008 Mar 18;148(6):449–58. doi: 10.7326/0003-4819-148-6-200803180-00210. [DOI] [PubMed] [Google Scholar]
- 9.Brown SR, Nelson RL. Surgery for faecal incontinence in adults. Cochrane Database Syst Rev. 2007;(2):CD001757. doi: 10.1002/14651858.CD001757.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Norton C, Cody JD, Hosker G. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults. Cochrane Database Syst Rev. 2006;(3):CD002111. doi: 10.1002/14651858.CD002111.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Omar MI, Alexander CE. Drug treatment for faecal incontinence in adults. Cochrane Database Syst Rev. 2013;6:CD002116. doi: 10.1002/14651858.CD002116.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rothman ML, Beltran P, Cappelleri JC, Lipscomb J, Teschendorf B. Patient-reported outcomes: conceptual issues. Value Health. 2007 Nov-Dec;10(Suppl 2):S66–75. doi: 10.1111/j.1524-4733.2007.00269.x. [DOI] [PubMed] [Google Scholar]
- 13.Earp JA, Ennett ST. Conceptual models for health education research and practice. Health Educ Res. 1991 Jun;6(2):163–71. doi: 10.1093/her/6.2.163. [DOI] [PubMed] [Google Scholar]
- 14.Kwon S, Visco AG, Fitzgerald MP, Ye W, Whitehead WE. Validity and reliability of the Modified Manchester Health Questionnaire in assessing patients with fecal incontinence. Dis Colon Rectum. 2005 Feb;48(2):323–31. doi: 10.1007/s10350-004-0899-y. discussion 31–4. [DOI] [PubMed] [Google Scholar]
- 15.Sung VW, Marques F, Rogers RR, Williams DA, Myers DL, Clark MA. Content validation of the patient-reported outcomes measurement information system (PROMIS) framework in women with urinary incontinence. Neurourology and urodynamics. 2011 Apr;30(4):503–9. doi: 10.1002/nau.21048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abrams P, Cardozo L, Khoury S, Wein Ae. Incontinence: Proceedings of the Fourth International Consultation on Incontinence; July 5–8, 2008; Plymouth, United Kingdom: Health Publication Ltd; 2009. pp. 331–412. [Google Scholar]
- 17.Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997 Sep;32(9):920–4. doi: 10.3109/00365529709011203. [DOI] [PubMed] [Google Scholar]
- 18.Krueger RA. Focus groups: A practical guide for applied research. 2. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 19.Strauss AL, Corbin J. Basics of qualitative research: Grounded theory procedures and techniques. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 20.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000 Jan 8;320(7227):114–6. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ritchie J, Lewis J. Qualitative research practice: a guide for social science students and researchers. London: Sage; 2003. [Google Scholar]
- 22.Jabine T, Straf JT, Tourangeau R. Cognitive aspects of survey design: Building a bridge between disciplines. Washington, DC: National Academy Press; 1984. [Google Scholar]
- 23.Emmel N. Sampling and choosing cases in qualitative research: A realist approach. 1. London: SAGE Publications Ltd; 2013. [Google Scholar]
- 24.Rockwood TH. Incontinence severity and QOL scales for fecal incontinence. Gastroenterology. 2004 Jan;126(1 Suppl 1):S106–13. doi: 10.1053/j.gastro.2003.10.057. [DOI] [PubMed] [Google Scholar]
- 25.Brown HW, Wexner SD, Segall MM, Brezoczky KL, Lukacz ES. Accidental bowel leakage in the mature women’s health study: prevalence and predictors. Int J Clin Pract. Nov;66(11):1101–8. doi: 10.1111/ijcp.12018. [DOI] [PubMed] [Google Scholar]


