Abstract
Heterotopic supradiaphragmatic livers are rare. A total of 23 cases of primary supradiaphragmatic livers have been reported in the literature. The clinical presentations of heterotopic supradiaphragmatic liver are variable. The simultaneous detection of intrathoracic accessory liver and pulmonary sequestration is extremely rare, and only one case has previously been reported. It is difficult to make a correct diagnosis preoperatively. We presented a 53-year-old woman with complaints of an intermittent, productive cough and dyspnea for two months that was refractory to medical treatment. She had no previous history of trauma or surgery. A chest radiograph only showed a widening of the mediastinum. Contrast-enhanced computed tomography of the chest revealed a well-circumscribed homogenous soft-tissue mass, approximately 4.35 cm × 2.5 cm × 6.14 cm in size, protruding through the right diaphragmatic crura to the right pleural cavity, attached to the inferior vena cava, esophagus and liver. There was no conclusive diagnosis before surgery. After the operation, we discovered that this patient was the first case of a supradiaphragmatic heterotopic liver, which passed through the inferior vena cava foramen and was coincidentally combined with an intralobar pulmonary sequestration that was found intraoperatively. We discussed its successful management with surgical resection via a thoracic approach and reviewed the published literature.
Keywords: Intrathoracic liver, Pulmonary sequestration, Supradiaphragmatic ectopic liver
Core tip: Heterotopic supradiaphragmatic livers are rare. A total of 23 cases of primary supradiaphragmatic liver have been reported in the literature. The simultaneous detection of intrathoracic accessory liver and pulmonary sequestration is extremely rare. It is difficult to make a correct diagnosis preoperatively. We reported the first case of a supradiaphragmatic heterotopic liver passing through the inferior vena cava foramen that coincidentally combined with intralobar pulmonary sequestration. We discussed the successful operation via a thoracic approach and reviewed the published literature.
INTRODUCTION
Heterotopic supradiaphragmatic livers are exceedingly rare. Abnormally positioned liver tissues have been described, but these are more commonly observed in the abdominal cavity than in the thoracic cavity. This is one of the first examples of a supradiaphragmatic heterotopic liver in the literature[1]. The clinical presentations of heterotopic supradiaphragmatic livers are variable. The simultaneous detection of an intrathoracic accessory liver and pulmonary sequestration was reported as the first and only one case in 2008[2]. The etiology of an introthoracic liver coinciding with pulmonary sequestration is not well known. Herein, we describe the first case of a supradiaphragmatic heterotopic liver passing through the inferior vena cava foramen and coincidentally combined with intralobar pulmonary sequestration.
CASE REPORT
A 53-year-old woman was referred to our center from an outside clinic complaining of intermittent productive cough and dyspnea over the previous 2 mo that was refractory to medical treatment. She denied any previous history of trauma or surgery. There were no positive findings on the physical examination. A chest roentgenogram only showed a widening of the mediastinum. Despite adequate medical treatment, her symptoms persisted. Contrast-enhanced computed tomography (CT) of the chest revealed a well-circumscribed homogenous soft-tissue mass, approximately 4.35 cm × 2.5 cm × 6.14 cm in size, protruding through the right diaphragmatic crura to the right pleural cavity attached to inferior vena cava (IVC), esophagus and liver (Figure 1). There was no pulmonary consolidation or other abnormalities of the bilateral lungs in imaging studies. In addition, the esophagram showed no submucosal lesions. Based upon these imaging findings, the tumor at middle mediastinum and right pleural cavity provoked discussion of a surgical resection.
Figure 1.
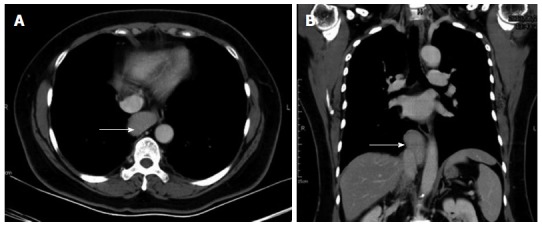
Computed tomography of the patient’s chest showing a well-circumscribed soft-tissue mass (white arrow), approximately 4.35 cm × 2.5 cm × 6.14 cm in size, over the middle mediastinum, with mild compression on the esophagus. A: Sagittal view; B: Transverse view.
Video-assisted thoracoscopic surgery (VATS) through the right chest wall was performed initially, and the operative findings revealed hypoplasia and regional hyperemic changes at the pleural surface of the right lower lobe (RLL) of the lung, with two obvious aberrant vessels from the right hemidiaphragm. After dissecting the visceral pleura and the tense capsule, the inferior pulmonary vein was identified, and a well-defined, red-brown, 7 cm × 4.5 cm × 2 cm solid mass abutting the IVC from the cardiophrenic angle of the right hemidiaphragm was found (Figure 2). Due to the limited area of the sequestrated lung of RLL, a wedge resection with an Endo-GIA staple instrument was performed. Due to the indeterminate nature of the mass and the location close to the IVC, we converted the operation to a right limited thoracotomy. The tumor was biopsied, and the frozen section showed reactive liver tissue with cirrhotic change. Therefore, we resected the tumor, which was extruding from the right pleural cavity, and then repaired the foramen of the IVC. The pathologic report showed liver tissue with chronic inflammation and cirrhotic changes (Figure 3). The patient had a good recovery after the surgery and was discharged home one week later. CT-angiography of the chest was conducted after the surgery to retrospectively evaluate the pulmonary sequestration (Figure 4). The aberrant arteries were identified from the abdominal aorta.
Figure 2.
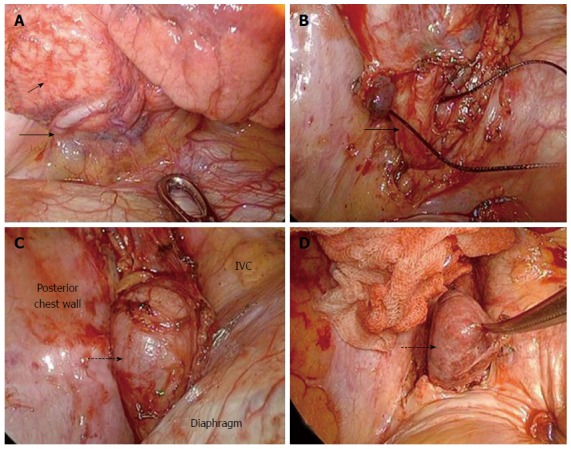
Intraoperative picture. Intraoperative picture showing the exposure of the abnormal lung with hypervascularity at the posterior basal segment (A) (short arrow) and aberrant vessels (B) (long arrow) passing through diaphragm. The mass (C) (dotted arrow), covered by the sac, abutted the inferior vena cava (IVC), posterior chest wall and diaphragm. After dissecting the covering sac, a herniated liver (D) (dotted arrow) was impressed.
Figure 3.
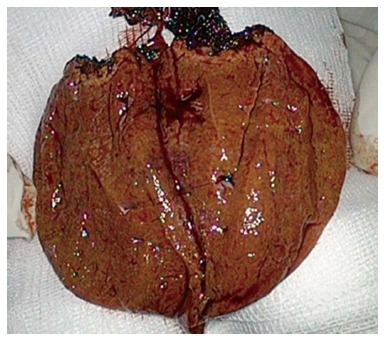
Cutting surface of the resected specimen showed liver tissue with cirrhotic changes.
Figure 4.
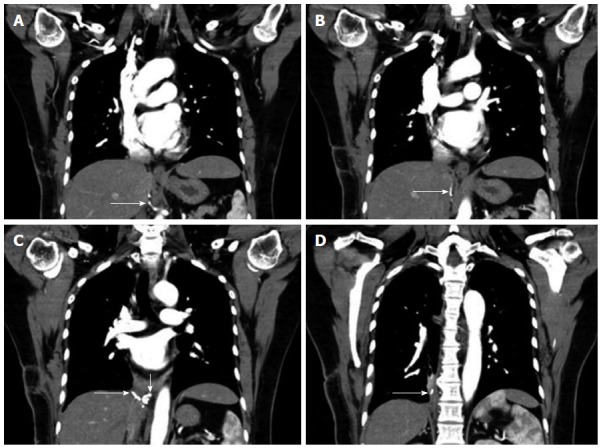
Postoperative computed tomography angiography confirmed the cutting end of the aberrant vessels. A-D: Showed the trend of the aberrant vessel. The remnant aberrant vessel from abdominal aorta (long arrow), engorged aberrant vessels (short arrow).
DISCUSSION
Supradiaphragmatic, intrathoracic liver tissue is very rare. A total of 23 cases of intrathoracic liver have been reported in the literature[1-23]. We introduced a rare case of an accessory liver lobe herniation from the IVC foramen to the right pleural cavity, combined with an intralobar sequestration of the RLL. This is the second case of a simultaneous detection of intrathoracic liver and pulmonary sequestration. The first case was reported in 2008, and the multiple cystic lesions in the right upper lobe, which were thought to constitute a congenital cystic malformation, were in fact an intralobar pulmonary sequestration[2]. However, the sequestrated lung of the above case was not typically located at the lower lobe, and the aberrant vessels were not visible. We found the sequestrated lung during the operation and then followed up with CT angiography to identify the feeding arteries of the sequestrated lung. Table 1 showed that seven cases (7/24, 29%) had diaphragmatic defects, and only the present supradiaphragmatic liver passed through the IVC foramen. There were 18 cases (18/24, 75%) associated with right-side intrathoracic livers. The majority of the intrathoracic ectopic or accessory liver lobes were connected to the orthotopic liver by means of a small pedicle that pierced the diaphragm or passed through a small hiatus[1,9,12,15-17,19,21]. In the presenting case, the caudate liver connected with the main portion of the liver just beneath the IVC. However, the pre-operative CT scan of the chest was not able to demonstrate this clearly, and it was difficult to make appropriate diagnosis before the operation.
Table 1.
Literature review of published cases associated with primary intrathoracic supradiaphragmatic livers
| Ref. | Sex/age | Location of mass | Symptoms | Associated anomalies | Preoperative diagnosis | Surgical procedure | Diaphragm | Histology |
| Hansbrough et al[1] | M/26 yr | Right CP angle | Abdominal pain | None | Mesothelioma | Right thoracotomy | Intact | Atypical cirrhosis |
| Kaufman et al[3] | F/48 yr | Right cardiophrenic angle | None | None | None | Right thoracotomy | Intact | Normal liver |
| Le Roux et al[4] | M/18 yr | Right CP angle | None | None | None | Right thoracotomy | Right diaphragmatic defect | Normal liver |
| Hudson et al[5] | M/21 yr | Right diaphragmatic dome | None | None | Diaphragmatic tumor | Right thoracotomy | Intact | Abundant bile ducts |
| Caron et al[6] | F/26 yr | Right CP angle | Asthenia | None | Benign tumor of the pleura or diaphragm | Right thoracotomy | Intact | Chronic inflammation |
| Sehdeva et al[7] | F/21 yr | Left diaphragmatic dome | Chest pain | None | Pleural or diaphragmatic tumor | Left thoracotomy | Intact | Centrilobular congestion |
| Desvignes et al[8] | F/7 yr | Right cardiophrenic angle | None | Right mirror lung, no scissure | Pulmonary sequestration | Right thoracotomy | Right diaphragmatic defect | Signs of pycnosis |
| Desvignes et al[8] | F/20 yr | Parenchyma of right lower lobe | Hemoptysis | Bochdaleck hernia | Hydatid cyst | Right thoracotomy | Right diaphragmatic defect | Normal liver |
| Lasser et al[9] | M/51 yr | Right thoracic cavity | Chest pain | None | Pleural tumor | Right thoracotomy | - | Hyperplasia |
| Mendoza et al[10] | F/6 mo | Parenchyma of right lower lobe | Respiratory distress | - | Solitary pulmonary mass | Autopsy | Intact | Normal liver |
| Shah et al[11] | F/1 d (36w GA) | Left thoracic cavity | Respiratory distress | - | - | Autopsy | Left diaphragmatic defect | Normal liver |
| Rendina et al[12] | F/19 yr | Right CP angle | None | None | Benign pleural tumor | Right thoracotomy | Intact | Normal liver |
| Shapiro et al[13] | F/1 d (26w GA) | Right diaphragmatic dome | Respiratory distress | - | - | Autopsy | - | Normal liver |
| Iber et al[14] | M/6 yr | Right thoracic cavity | Mild asymmetry of chest | None | Benign pleural tumor | Right thoracotomy | - | - |
| Babu et al[15] | M/17 mo | Right CP angle | Recurrent pneumonia | None | Diaphragmatic hernia with a sequestrated lung or herniated liver | Right thoracotomy | Intact | Normal liver |
| Beiler et al[16] | M/1 d (39w GA) | Left diaphragmatic dome | Respiratory distress | Bochdaleck hernia | Diaphragmatic hernia | Laparotomy | Left diaphragmatic defect | Normal liver |
| Bedii Salman et al[17] | F/6yr | Left thoracic cavity | - | Left diaphragmatic hernia | Left diaphragmatic hernia | Laparotomy | Left diaphragmatic defect | Normal liver |
| Luoma et al[18] | F/full term | Left thoracic cavity | Respiratory distress | Left hydrothorax | Left paramediastinal mass with massive hydrothorax | Left thoracotomy | Intact | Normal liver |
| Chen et al[20] | M/13 mo | Right diaphragmatic dome | Respiratory distress | Repeated pneumonia | Pleural or diaphragmatic tumor | Right thoracotomy | Intact | Normal liver |
| Choi et al[2] | M/3 yr | Right cardiophrenic angle | Cough and fever | Intralobar pulmonary sequestration of right upper lobe | Pulmonary sequestration | Right thoracotomy | Intact | Normal liver |
| Han et al[21] | F/26 yr | Left CP angle | Dry cough | None | Pulmonary sequestration | Left thoracotomy | Intact | Normal liver |
| Wang et al[22] | M/39 yr | Right thoracic cavity | Chest pain | None | A benign tumor of right lung | Right thoracotomy | Intact | Normal liver |
| An et al[23] | F/48 yr | Right cardiophrenic angle | Cough and dyspnea | None | Benign fibrous tumor of the pleura or peripheral lung carcinoid tumor | Right thoracotomy | Intact | Normal liver |
F: Female; M: Male.
Such events are most often found in the vicinity of the liver, such as in the gallbladder, spleen, pancreas, umbilicus, adrenal gland, or omentum, and usually some connective tissue or mesenteric attachment to the liver remains[10]. Very rare cases involving the thoracic cavity can be found. Of those cases reported in the literature, almost all were misdiagnosed, most often as a pulmonary tumor and sometimes as pulmonary sequestration or hydatid cyst[12,21]. The misdiagnosis of such cases often leads to potentially unnecessary or inappropriate thoracotomies and the resection of the ectopic liver tissue. Although heterotopic liver tissue may be acquired secondary to trauma or diaphragmatic hernia repair, previous reports have speculated that this condition mostly represents a developmental defect of the septum transversum[10]. The most probable explanation is the development of an accessory liver lobule, with atrophy or regression of the original connection to the abdominal liver[10]. Retrospectively re-examining the clinical evidence, we found at least two signs implying the possibility of an accessory liver lobe in the thoracic cavity. First, the mass was homogeneous, with a density similar to that of a normal liver. Second, the mass was adjacent to the hemidiaphragm and connected to caudal lobe of liver through a defect of the right crus. An intrathoracic ectopic or accessory liver lobe is rarely of clinical significance[12,16]. Surgery is not always required for such a condition. However, the cases reported were almost always respected because of their inappropriate diagnoses. There were a few cases that did have symptoms, such as chest pain, hemoptysis, or dry cough[12,21], that may or may not have been related to the underlying condition. Such abnormal tissue could lead to further liver pathologies, such as cancer, hepatitis, and tissue ischemia secondary to torsion[21]. To avoid malignant changes in this loco-regional cirrhosis of the liver[24], surgical resection was the first choice for treatment.
Because heterotopic supradiaphragmatic livers are extremely rare and occur at tricky anatomic locations, it is difficult to make an appropriate diagnosis preoperatively. In our case, we also misdiagnosed the liver as a pulmonary sequestration before surgery. The intralobar pulmonary sequestration was found incidentally at the time of the operation because of the engorged aberrant vessels from systemic circulation; it was then divided by stapled Endo-GIA due to the small area of the sequestrated lung of the RLL. The pathological report of the sequestrated lung showed inflammation, mucus accumulation, microcystic changes and dilated lymphatic channels. Pulmonary sequestration is a rare congenital malformation of the lower respiratory tract[25] that consists of a nonfunctioning mass of lung tissue that lacks normal communication with the tracheobronchial tree and receives its arterial blood supply from the systemic circulation[26]. There are intralobar and extralobar forms, the former of which is embedded in a normal lung and the latter, separated from the adjacent lung by its own visceral pleural investment[27]. Misdiagnosis or delayed diagnosis of such pulmonary malformations results in unnecessary treatments and hospitalizations, as well as in frequent, recurrent infectious complications. The definitive treatment for sequestrated lung diseases is surgical resection, which is curative and has low morbidity and mortality rates[28].
In addition, a multi-detector spiral CT scan with multi-planar reconstruction and magnetic resonance imaging can also reveal the location of the mass and its relation to the normal liver parenchyma[19]. Furthermore, with enhanced scanning and hepatic angiography, if the hepatic vessels extend to the mass, the diagnosis of an accessory liver lobe is more definitive[19]. Thoracoscopy is also effective in the diagnosis of the intrathoracic accessory liver lobes in suspected patients, and conveniently, the lesion might be resected with minimally invasive procedures under thoracoscopy, if the connecting pedicle is not too large in size[22]. If an intrathoracic mass is suspected to be a pulmonary or chest wall benign tumor, abnormal liver tissue should enter the scope of a differential diagnosis to avoid potentially unnecessary or inappropriate surgical interventions[22]. Table 1 revealed that 19 cases underwent thoracotomy, and only two had laparotomy. We attempted to use VATS with the removal of the mediastinal tumor at first, but we finally converted to thoracotomy because of the unclear anatomic view and our diminished confidence.
We presented a very interesting case of supradiaphragmatic heterotopic liver coincidentally combined with intralobar pulmonary sequestration. The ectopic liver was the first case to pass through IVC foramen. To our knowledge, these two anatomic abnormalities are congenital and developmental problems and may constitute a specific type of syndrome.
COMMENTS
Case characteristics
A 53-year-old woman was referred to the authors’ center from an outside clinic complaining of intermittent productive cough and dyspnea over the previous 2 mo that was refractory to medical treatment.
Clinical diagnosis
A middle mediastinal tumor was impressed initially.
Differential diagnosis
Differential diagnoses included an esophageal cyst, pulmonary tumor or metastatic mediastinal lesions by computed tomography (CT) imaging before surgery.
Laboratory diagnosis
No laboratory data could help to diagnosis in this case.
Imaging diagnosis
Contrast-enhanced CT of the chest revealed a well-circumscribed homogenous soft-tissue mass, approximately 4.35 cm × 2.5 cm × 6.14 cm in size, protruding through the right diaphragmatic crura to the right pleural cavity attached to inferior vena cava, esophagus and liver.
Pathological diagnosis
The pathologic report showed liver tissue with chronic inflammation and cirrhotic changes.
Treatment
Video-assisted thoracoscopic surgery with wedge resection of right lower lobe of lung through the right chest wall was performed initially, and then converted right limited thoracotomy with resection of intrathoracic liver.
Experiences and lessons
Intrathoracic liver or pulmonary sequestration should be included in differential diagnoses of patient with unknown etiology of mediastinal lesions.
Peer review
This strengths included the first case of a supradiaphragmatic heterotopic liver passing through the inferior vena cava foramen that coincidentally combined with intralobar pulmonary sequestration and literature review in intrathoracic ectopic liver.
Footnotes
P- Reviewers: Gao Y, Julianov A S- Editor: Qi Y L- Editor: A E- Editor: Ma S
References
- 1.Hansbrough ET, Lipin RJ. Intrathoracic accessory lobe of the liver. Ann Surg. 1957;145:564–567. doi: 10.1097/00000658-195704000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi SU, Kim HK, Kim J. Heterotopic supradiaphragmatic liver combined with intralobar pulmonary sequestration. Ann Thorac Surg. 2008;85:1809–1810. doi: 10.1016/j.athoracsur.2007.11.040. [DOI] [PubMed] [Google Scholar]
- 3.Kaufman SA, Madoff IM. Intrathoracic accessory lobe of the liver. Ann Intern Med. 1960;53:403–407. doi: 10.7326/0003-4819-53-2-403. [DOI] [PubMed] [Google Scholar]
- 4.Le Roux BT. Heterotopic intrathoracic liver. Thorax. 1961;16:68–69. [Google Scholar]
- 5.Hudson TR, Brown HN. Ectopic (supradiaphragmatic) liver. J Thorac Cardiovasc Surg. 1962;43:552–555. [PubMed] [Google Scholar]
- 6.Caron J, Bascands J, Cosson R. [Thoracic hepatic lobe] J Chir (Paris) 1970;100:213–226. [PubMed] [Google Scholar]
- 7.Sehdeva JS, Logan WD. Heterotopic (supradiaphragmatic) liver. Ann Thorac Surg. 1971;11:468–471. doi: 10.1016/s0003-4975(10)65484-7. [DOI] [PubMed] [Google Scholar]
- 8.Desvignes G, Mary H, Levasseur P, Aubert A, Petithomme H, Terrazas G, Thevenet A, Merlier M. [A study of two cases of intrathoracic hepatic heterotopia (author’s transl)] Ann Chir Thorac Cardiovasc. 1975;14:177–180. [PubMed] [Google Scholar]
- 9.Lasser A, Wilson GL. Ectopic liver tissue mass in the thoracic cavity. Cancer. 1975;36:1823–1826. doi: 10.1002/1097-0142(197511)36:5<1823::aid-cncr2820360537>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 10.Mendoza A, Voland J, Wolf P, Benirschke K. Supradiaphragmatic liver in the lung. Arch Pathol Lab Med. 1986;110:1085–1086. [PubMed] [Google Scholar]
- 11.Shah KD, Beck AR, Jhaveri MK, Keohane M, Weinberg B, Gerber MA. Infantile hemangioendothelioma of heterotopic intrathoracic liver associated with diaphragmatic hernia. Hum Pathol. 1987;18:754–756. doi: 10.1016/s0046-8177(87)80250-2. [DOI] [PubMed] [Google Scholar]
- 12.Rendina EA, Venuta F, Pescarmona EO, Martelli M, Ricci C. Intrathoracic lobe of the liver. Case report and review of the literature. Eur J Cardiothorac Surg. 1989;3:75–78. doi: 10.1016/1010-7940(89)90015-8. [DOI] [PubMed] [Google Scholar]
- 13.Shapiro JL, Metlay LA. Heterotopic supradiaphragmatic liver formation in association with congenital cardiac anomalies. Arch Pathol Lab Med. 1991;115:238–240. [PubMed] [Google Scholar]
- 14.Iber T, Rintala R. Intrapulmonary ectopic liver. J Pediatr Surg. 1999;34:1425–1426. doi: 10.1016/s0022-3468(99)90028-3. [DOI] [PubMed] [Google Scholar]
- 15.Babu R, Van der Avoirt A. Ectopic intrathoracic liver. Pediatr Surg Int. 2001;17:461–462. doi: 10.1007/s003830000520. [DOI] [PubMed] [Google Scholar]
- 16.Beiler HA, Sergi C, Wagner G, Zachariou Z. Accessory liver in an infant with congenital diaphragmatic hernia. J Pediatr Surg. 2001;36:E7. doi: 10.1053/jpsu.2001.24020. [DOI] [PubMed] [Google Scholar]
- 17.Bedii Salman A. Left-sided congenital diaphragmatic hernia associated with intrathoracic ectopic liver lobule. Eur J Cardiothorac Surg. 2002;21:558–560. doi: 10.1016/s1010-7940(01)01147-2. [DOI] [PubMed] [Google Scholar]
- 18.Luoma R, Raboei E. Supradiaphragmatic accessory liver: a rare cause of respiratory distress in a neonate. J Pediatr Surg. 2003;38:1413–1414. doi: 10.1016/s0022-3468(03)00412-3. [DOI] [PubMed] [Google Scholar]
- 19.Massaro M, Valencia MP, Guzman M, Mejia J. Accessory hepatic lobe mimicking an intra-abdominal tumor. J Comput Assist Tomogr. 2007;31:572–573. doi: 10.1097/01.rct.0000250107.78176.de. [DOI] [PubMed] [Google Scholar]
- 20.Chen F, Heller DS, Bethel C, Faye-Petersen O. Intrathoracic ectopic lobe of liver presenting as pulmonary sequestration. Fetal Pediatr Pathol. 2005;24:155–159. doi: 10.1080/15227950500305520. [DOI] [PubMed] [Google Scholar]
- 21.Han S, Soylu L. Accessory liver lobe in the left thoracic cavity. Ann Thorac Surg. 2009;87:1933–1934. doi: 10.1016/j.athoracsur.2008.10.076. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y, Junlin L, Zhang WG, Chen JH, He Y, Chen JM. Accessory lobe of right liver mimicking a pulmonary tumor in an adult male. Ann Thorac Surg. 2010;89:e9–e10. doi: 10.1016/j.athoracsur.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 23.An J, Han J, Lee KS, Choi YS. Supradiaphragmatic heterotopic liver presenting as a pleural mass: a case report. Tuberc Respir Dis. 2010;69:191–195. [Google Scholar]
- 24.Wong CR, Garcia RT, Trinh HN, Lam KD, Ha NB, Nguyen HA, Nguyen KK, Levitt BS, Nguyen MH. Adherence to screening for hepatocellular carcinoma among patients with cirrhosis or chronic hepatitis B in a community setting. Dig Dis Sci. 2009;54:2712–2721. doi: 10.1007/s10620-009-1015-x. [DOI] [PubMed] [Google Scholar]
- 25.Wei Y, Li F. Pulmonary sequestration: a retrospective analysis of 2625 cases in China. Eur J Cardiothorac Surg. 2011;40:e39–e42. doi: 10.1016/j.ejcts.2011.01.080. [DOI] [PubMed] [Google Scholar]
- 26.Landing BH, Dixon LG. Congenital malformations and genetic disorders of the respiratory tract (larynx, trachea, bronchi, and lungs) Am Rev Respir Dis. 1979;120:151–185. doi: 10.1164/arrd.1979.120.1.151. [DOI] [PubMed] [Google Scholar]
- 27.Stern EJ, Webb WR, Warnock ML, Salmon CJ. Bronchopulmonary sequestration: dynamic, ultrafast, high-resolution CT evidence of air trapping. AJR Am J Roentgenol. 1991;157:947–949. doi: 10.2214/ajr.157.5.1927813. [DOI] [PubMed] [Google Scholar]
- 28.Costa Júnior Ada S, Perfeito JA, Forte V. Surgical treatment of 60 patients with pulmonary malformations: what have we learned? J Bras Pneumol. 2008;34:661–666. doi: 10.1590/s1806-37132008000900005. [DOI] [PubMed] [Google Scholar]


