Abstract
Background:
Cost and environmental pollution are two prime concerns with general anesthesia. We hypothesized that target-controlled (TC) anesthesia drug delivery system also called as end-tidal (ET) control is an effective and safe system that would reduce the cost and also environmental pollution.
Materials and Methods:
We studied 200 patients undergoing laparoscopic abdominal and pelvic surgeries and randomly distributed those in 2 groups of 100 each, TC and manual-controlled (MC) group. We reviewed the two groups in term of consumption of gases, time required to achieve the ET concentration of sevoflurane of 1.5%, maximum inspired concentration of sevoflurane achieved, and number of adjustments required to maintain the depth of anesthesia.
Results:
We found that the consumption of nitrous oxide and sevoflurane was significantly less in TC group than MC group (P < 0.05), oxygen consumption was also less in TC group but not statistically significant. The time required to achieve the desired levels, maximum inspired sevoflurane concentration achieved, and the number of drug delivery adjustments required were statistically significant in TC group (P < 0.05). As the consumption reduced in TC group, the cost of the inhalational anesthesia reduced by approximately Rs. 64/h ($1.12) and thus the environmental pollution.
Conclusion:
We concluded from our study that ET control is a good system for conserving the consumption of gases and thus is efficient as it reduces both the cost and the environmental pollution.
Keywords: End-tidal ET control, inhalational anesthesia, sevoflurane, target control
Introduction
Target-controlled (TC) inhalational anesthesia also called as end-tidal (ET) control is an anesthesia delivery system available in the newer anesthesia machines. It is a modality of anesthesia gas delivery system, where the machine adjusts automatically the anesthetic agent concentration to achieve the desired target levels set by the user. Several machines have emerged with this technology of automatic semiclosed or closed loop control of ET concentration of volatile anesthetic agents, oxygen and nitrous oxide.
We hypothesized that with the use of TC technique, the consumption of gases would reduce, thus effectively reducing the cost and environmental pollution. We conducted this study on AISYS machine (WiproGE Healthcare Pvt. Ltd. 881, Solitare Corporate Park, Ghatkopar – Andheri Link road, Chakala, Andheri (East) Mumbai 400093). The primary outcome measure of this study was to assess the cost-effectiveness of TC versus manual-controlled (MC) inhalational anesthesia with sevoflurane. The secondary outcome was to assess the consumption of oxygen, nitrous oxide, and sevoflurane, time required to achieve ET concentration of sevoflurane (ET sevo) of 1.5%, maximum inspired concentration of sevoflurane achieved (Fi sevo), and number of anesthetic gas delivery adjustments required in both the groups to achieve the ET sevo. We monitored all these patients for depth of anesthesia targeting the entropy values between 40 and 60. Entropy monitoring is not a part of closed loop circuit of TC mechanism in our machine.
A similar study was done by Lortat-Jacob et al.,[1] on Zeus machine that has an automated target control system linked to Bispectral Index (BIS) monitoring. The machine would, thus, adjust the gas delivery depending on the desired target levels of anesthetic agents considering the BIS values.
Mechanism of end tidal control
The ET control is a mechanism in the breathing system, where the desired values of gases are selected and the computerized system adjusts the gas delivery to achieve the targeted levels. Here is the schematic representation of this system in AISYS machine (GE Healthcare) [Figure 1a and b].
Figure 1.
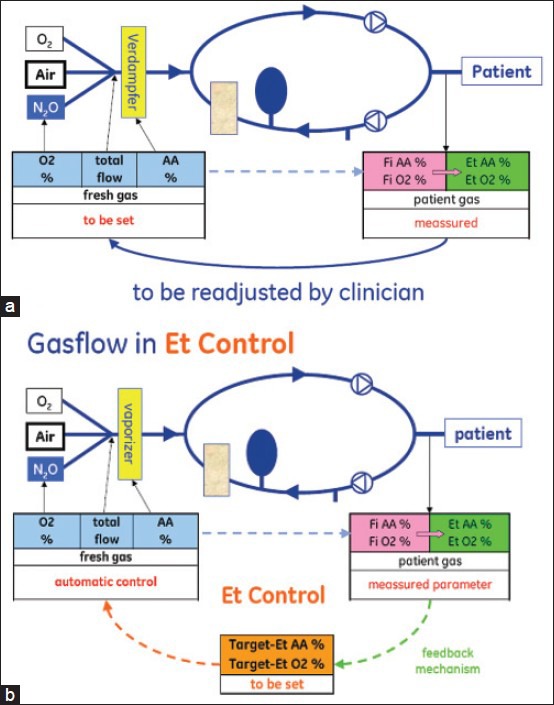
(a) Schematic diagram of the traditional circle system (b) Schematic representation of end-tidal control anesthesia breathing circuit. (The diagrams of Figures 1(a) and (b) are copyrights of GE Healthcare. Permission for publication taken)
The internal anesthesia breathing circuit consists of a gas mixer that controls the amount of oxygen and either air or nitrous oxide delivered to the patient depending on the settings. Selector valves open according to the selection mode. Sensors continuously monitor the gas mixer. Mixed gas exits the mixer and flows to the electronic vaporiser also called as Aladin cassette, where agent vaporization occurs using a conventional bypass flow and free vaporization principle. From here, the common gas with the agent flows through the inflow and outflow valves.
However, the actual agent delivery is controlled by the internal ‘’electronic vaporizer.’’ This device regulates the bypass flow and controls the inflow and outflow valves to achieve the desired output in the fresh gas. Multiple sensors in the gas pathway constantly monitor the flow and pressure to ensure the desired vapor concentration in the fresh gas flow (FGF) even at minimal FGF rates. The consumption of the various inhaled gases is automatically calculated by inbuilt computerized software of the machine.
Materials and Methods
This is a prospective, randomized, single-blinded, single center study of 200 patients undergoing laparoscopic abdominal or pelvic surgeries. This study has been conducted after our hospital ethics committee approval. Patients were included in the study after written informed consent. These patients were randomly allocated to 2 groups of 100 patients each.
Group TC-where the automatic closed loop control of inhalational agent labelled as ‘’Target control’’ was used to achieve the end tidal concentration of sevoflurane.
Group MC-where the manual control of inhalational agent was used to achieve the ET concentration of sevoflurane.
Patients were allocated to the respective groups by chit randomization. Chits were labelled from 1 to 200. Patients were asked to pick the chits. Odd numbers were allocated to Group MC and even to Group TC to which the patients were blinded.
Initially, the sample size was taken randomly. To see the effect of the collected sample size, power calculation was done for the two groups for cost of anesthesia per hour. Standard deviation of 102.41 and power of 0.95 was considered and power and sample size calculation was done with Minitab 16. The clinical difference between the means of 63.81, sample size for each level was 68 with the maximum power of 0.95. Hence, the sample size of 200 patients 100 in each group was adequate for this study.
Inclusion criteria were as follows:
Age: 15-70 years, American Society of Anesthesiologists (ASA) status I and II, surgical procedure of minimum 30 min and maximum of 4 h duration under general anesthesia, patient intubated with endotracheal tube and with controlled ventilation, patients maintained only on sevoflurane and not on any other agents like propofol, midazolam, and sedative infusions.
Exclusion criteria are as follows:
General anesthesia with laryngeal mask airway, face mask, and spontaneous respiration, patients having cardiac, renal, and respiratory diseases, neurological or psychological illness that may interfere with entropy monitoring, ASA III, IV, emergency surgeries, patients having hemodynamic instability intraoperatively, where there is a variation of pulse or blood pressure more than 20% of baseline or entropy values of <40 and >60 in the maintenance period of anesthesia for more than 5 min.
All patients received conventional general anesthesia with preoxygenation with 100% oxygen for 3 min at FGF of 6 L/min. Inj. Propofol 2 mg/kg/intravenous (IV) with inj. rocuronium 0.9 mg/kg/IV was used for induction of anesthesia and tracheal intubation, respectively. Sedation and analgesia was given with inj midazolam 0.03 mg/kg IV and inj. fentanyl 2 μg/kg IV, respectively. After tracheal intubation, both groups were maintained on oxygen: Nitrous oxide combination of 50:50 at FGF of 1.5 L/min with volume-controlled pressure regulated mode of ventilation to maintain EtCO2 values of 35-40 mm Hg. All patients received IV Ringer lactate depending on the starvation status.
In the TC group, the ET control mode was switched on after tracheal intubation. The FGF was set at 1.5 L/min with a combination of oxygen and nitrous oxide in the ratio of 50:50. Sevoflurane delivery was targeted to an ET sevo of 1.5% monitoring the entropy values of 40-60.
In the MC group after tracheal intubation, the FGF was reduced to 1.5 L/min with a combination of oxygen and nitrous oxide in the proportion of 50:50. Sevoflurane was started with a dial setting of 2% and increased every 5 min by 0.5%, till we achieved an ET sevo of 1.5%. Once this concentration was achieved the dial flow settings were titrated by increment or decrement of sevoflurane by 0.5% every 5 min to maintain an ET sevo of 1.5%.
Variables that were monitored are hemodynamic parameters like pulse, blood pressure, oxygen saturation, ET carbon dioxide, train-of-four (TOF), entropy values, ventilatory settings like tidal volume, respiratory rate, airway pressures, ET oxygen, nitrous oxide, and sevoflurane concentrations. We also assessed the time required to achieve ET sevo of 1.5% in minutes after starting sevoflurane, maximum inspired concentration of sevoflurane (Fi sevo), and number of adjustment of dial and flow settings done by the anesthesiologist to maintain the ET sevo of 1.5%.
In the event of persistent tachycardia with hypotension, patients were given bolus of 100-200 mL of ringer lactate. If required rescue analgesia of 25 μg fentanyl IV was given. Bolus of 10 mg inj rocuronium was given as per the TOF values. Inj. paracetamol 1 g IV was given after insertion of the laparoscopy ports. Local instillation of suprahepatic 10 mL 0.5% bupivacaine preclosure of ports and local infiltration with 0.5% bupivacaine of all the surgical ports was done for postoperative pain relief.
At the beginning of skin closure sevoflurane was switched off, 5 min later nitrous oxide was switched off and 100% oxygen was given at 6 L per minute. A total of 5 min after switching on 100% oxygen, consumption of oxygen, nitrous oxide, and sevoflurane was noted. These consumptions are measured by the software of the machine.
All patients were reversed for muscle relaxants with inj. neostigmine 0.05 mg/kg and inj. glycopyrrolate 8 μg/kg IV. Tracheal tube was removed as soon as patient was awake; entropy >90, TOF >0.9, and patient responded to oral commands and were breathing spontaneously [Figure 2].
Figure 2.
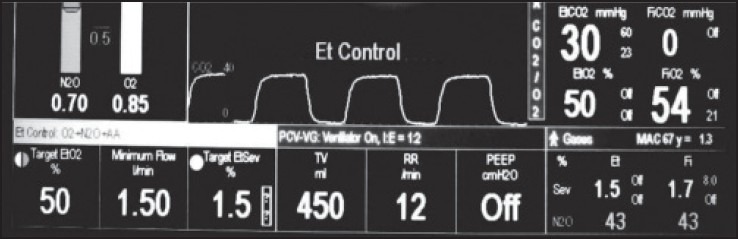
End-tidal control monitor screen
Statistics analysis
The data were managed in Microsoft excel spreadsheet. Correlations among different measurements were assessed using Pearson's correlation coefficients. A P value <0.05 was considered statistically significant. Demographics and general information like count, average, standard deviation, and percentage for various parameters with all permutations and combinations were calculated in Microsoft excels. General linear model [analysis of variance (ANOVA)] is used to investigate and model impact of various parameters with costs like oxygen, nitrous oxide, sevoflurane per minute, maximum Fi sevo, time required for ET sevo to reach 1.5% in minutes and number of gas delivery adjustments between the groups. All specific graphs drawn and all statistical analysis was done using Minitab16.
Results
Among the 200 patients included in the study, none of them were excluded out of the study for any reason. The demographic details of the study group are shown in Table 1.
Table 1.
The demographic details of the study group
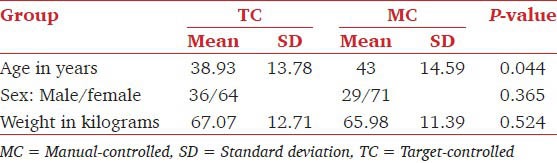
The two groups are similar in demographic details like sex (P value by two proportion test) and weight (P-value by two sample T test). The P < 0.05 shows significant difference for age (P- value by one-way ANOVA) but R-sq value shows the impact is very less which is almost towards nonsignificance [Table 2].
Table 2.
Shows the consumption of oxygen, nitrous oxide, and sevoflurane
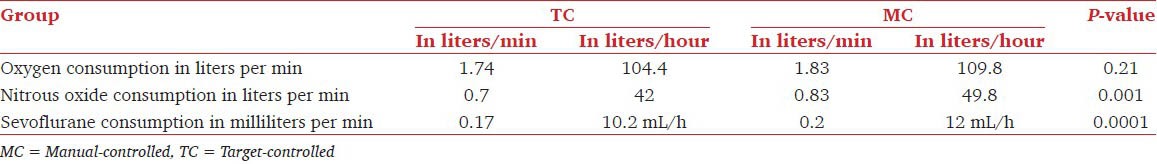
The two groups were compared for consumption of oxygen, nitrous oxide, and sevoflurane. They were statistically significant for nitrous oxide and sevoflurane [Table 3].
Table 3.
Shows the average cost of inhalational anesthesia in the two groups
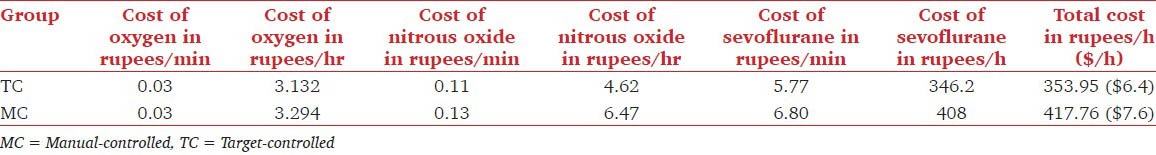
The cost comparison of the two groups showed a statistical significance P-value being 0.0001 [Figure 3].
Figure 3.
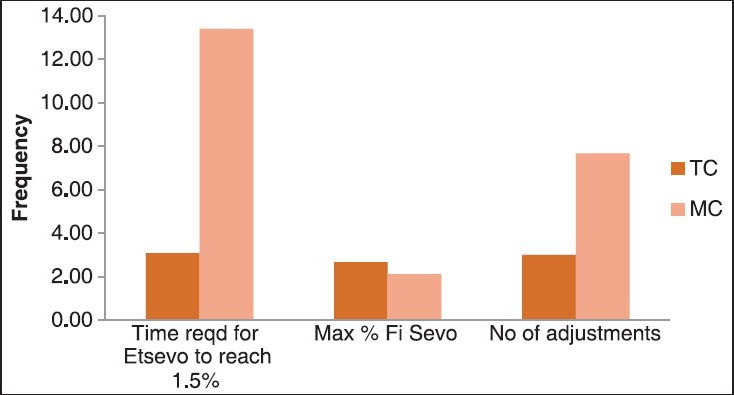
Comparison of average time required to achieve the ET sevo of 1.5%, the average maximum Fi sevo and average number of adjustments done
The results show significant differences in the two groups for average time required to achieve the ET sevo of 1.5% (P value 0.0001), the Fi sevo (P-value 0.0001) and average number of adjustments done (P value 0.0001) [Figure 4].
Figure 4.
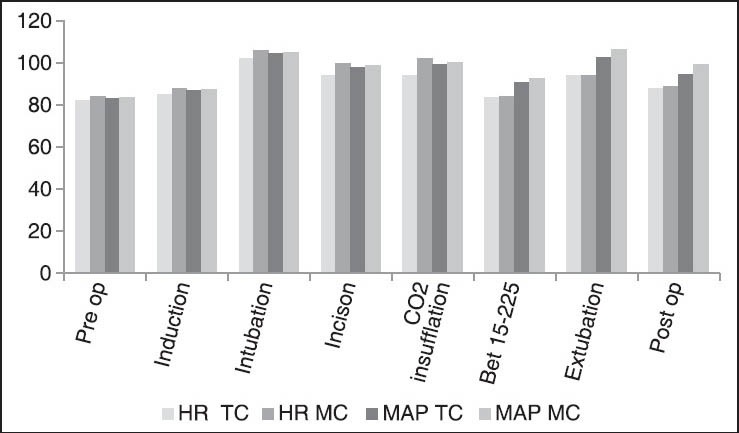
Shows the hemodynamic variability
There were no differences in the hemodynamic parameters like pulse and blood pressure. The ET carbon dioxide, oxygen saturation variability, and entropy values between the two groups are comparable [Figure 5].
Figure 5.
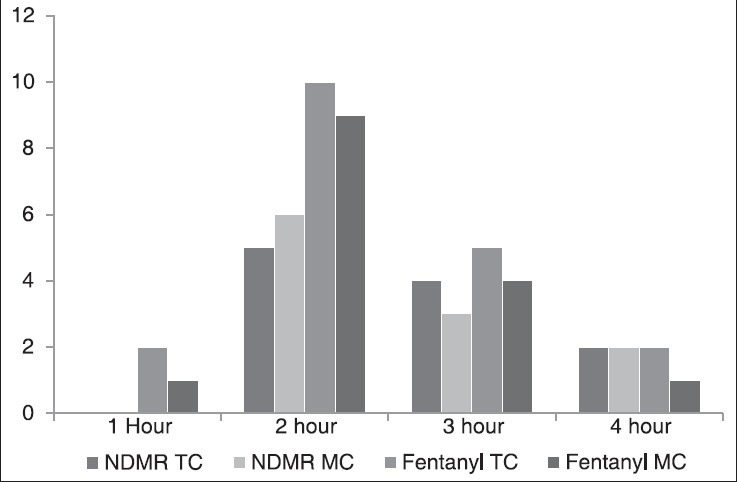
Requirement of NDMRs and fentanyl during the surgeries
There was no differences in the requirement of non depolarising muscle relaxants (NDMRs) and analgesic requirements in both the groups.
Discussion
The use of inhalational anesthetic agents in a semiclosed or a closed circuit leads to rebreathing[2] of the volatile anesthetic agents. This leads to difference in the delivered and inspired concentration of volatile anesthetic agents depending on the FGF. Thus, a high FGF is required at the beginning of the case to enable rapid control of ET anesthetic concentration.[3] This leads to greater flow of gases and thus increases the cost and environmental pollution. A low gas FGF level is acceptable when the ET concentration is stable over a sustained period of time.
The consumption of inhalational agents is not only dependent on the FGF, but also on the relative solubility of the gas. Thus, monitoring of partial pressures of the inhaled agents within the breathing system is desirable.[4] We decided to do this study with ET control at the FGF flow rate of 1.5 L with sevoflurane as the inhalational agent to assess the efficiency of target control anesthesia delivery system versus manual control of anaesthesia delivery.
In our methodology, we titrated the delivery of sevoflurane in MC group by incremental dose of 0.5% after 2% every 5 min to avoid any incidence of hypotension at higher concentrations. We targeted for ET sevo as 1.5% and monitored the depth of anaesthesia and awareness with entropy thus assuring the adequacy of depth of anesthesia.[5] The ET concentration of an inhalational anesthetic closely represents the brain concentration and thus is an indirect measure of depth of anesthesia.[6]
In our study, there was a significant reduction in the consumption of nitrous oxide (0.70 mL/min) and sevoflurane (0.17 mL/min) in TC group as compared with 0.83 and 0.20 mL/min in MC group P value being 0.01 and 0.001, respectively. The oxygen consumption was also reduced from 1.83 L/min in MC group to 1.70 L/min in TC group.
Lortat-Jacob et al.,[1] conducted a study with TC desflurane delivery using a FGF of 1 L using Zeus anesthesia machine in 80 patients. He also monitored the hemodynamic parameters and the desflurane drug delivery was monitored automatically as per BIS results. He had similar results, where oxygen consumption were halved in autocontrol mode 0.07 mL/min from 0.2 mL/min in manual control mode and thus reduced consumption of gases and vapor significantly and was more economical.
We did not find a significant reduction of oxygen consumption as we have included the high FGF at 6 L/min with oxygen in the initial induction phase and also washout phase post surgery.
The calculated approximate cost of inhalational anaesthesia per hour in TC group would be Rs. 354 ($6.4) and for MC group would be Rs.418 ($7.6). Hence, we would be able to save an approximate cost of Rs.64/h ($1.12) of anesthesia given.
The time required for achieving the set target of sevoflurane of 1.5% was significantly less with TC group (3.08 min) than MC group (13.40 m) P value being <0.0001. Lortat-Jacob et al.,[1] had similar time requirement for achieving the ET concentrations of both the groups.
The maximum inspired sevoflurane required was greater in TC group of 2.66% as opposed to 2.11% in the MC group and was statistically significant, P-value being <0.0001. Lortat-Jacob et al.,[1] Struys et al.,[7] and Kennedy et al.,[8] had a similar result in there study, where there was a significant overshoot of inspired concentration in TC group but hemodynamic stability. Inspite of higher inspired sevoflurane concentrations in TC group, there was no evidence of hypotension as these high concentrations were sustained for few minutes till the actual target value was achieved.
Entropy values were monitored throughout the study[5,9] for both the groups and were maintained between 40 and 60 at all times. Locher et al.,[10] studied the effectiveness of automatic control of depth of anaesthesia using BIS with isoflurane administration versus isoflurane via vaporizer that was manually controlled. In the automatic closed loop control with BIS, the drug delivery adjustments were made automatically depending upon the BIS levels and in the manual control, the drug delivery adjustments were made manually depending upon the BIS levels. They found that closed-loop control with BIS using isoflurane can be safely applied clinically and performs significantly better than manual control, even in phases with abrupt changes of stimulation that cannot be foreseen by the control system.
The number of drug delivery adjustments was only three in TC group counted as initial flow settings, the second adjustment after intubation when ET control mode was switched on and the last being switching off the ET control mode. The number of adjustments in the MC group varied from 5 to 12 as greater number of changes in dial flow settings were required to achieve the ET concentrations of sevoflurane. In the study conducted by Lortat-Jacob et al.,[1] the number of drug delivery adjustments per hour was significantly less in autocontrol 7 versus 15 in manual control.
Conclusion
We concluded from our study that ET control is a good system for conserving the consumption of gases and thus is efficient as it reduces both the cost and the environmental pollution.
Acknowledgment
We thank GE Healthcare for providing us with the technical information and the permission for publication of schematic diagrams.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lortat-Jacob B, Billard V, Buschke W, Servin F. Assessing the clinical or pharmaco-economical benefit of target controlled desflurane delivery in surgical patients using Zeus anaesthesia machine. Anaesthesia. 2009;64:1229–35. doi: 10.1111/j.1365-2044.2009.06081.x. [DOI] [PubMed] [Google Scholar]
- 2.Baum JA, Aitkenhead AR. Low-flow anaesthesia. Anaesthesia. 1995;50:37–44. doi: 10.1111/j.1365-2044.1995.tb06189.x. [DOI] [PubMed] [Google Scholar]
- 3.Quenet E, Weil G, Billard V. Which settings to optimize anaesthetics delivery: Fresh gas flow or delivered fraction? Ann Fr Anesth Reanim. 2008;27:900–8. doi: 10.1016/j.annfar.2008.07.097. [DOI] [PubMed] [Google Scholar]
- 4.Coetzee JF, Stewart LJ. Fresh gas flow is not the only determinant of volatile agent consumption: A multi-centre study of low-flow anaesthesia. Br J Anaesth. 2002;88:46–55. doi: 10.1093/bja/88.1.46. [DOI] [PubMed] [Google Scholar]
- 5.Grover VK, Neerja B. Measuring depth of anaesthesia-An overview on currently available monitoring systems. The Indian Anaesthetists’ Forum- October. 2008 [Google Scholar]
- 6.Sieber TJ, Frei CW, Derighetti M, Feigenwinter P, Leibundgut D, Zbinden AM. Model based automatic feedback control versus human control of end-tidal isoflurane concentration using low-flow anaesthesia. Br J Anaesth. 2000;85:818–25. doi: 10.1093/bja/85.6.818. [DOI] [PubMed] [Google Scholar]
- 7.Struys MM, Kalmar AF, De Baerdemaeker LE, Mortier EP, Rolly G, Manigel J, et al. Time course of inhaled anaesthetic drug delivery using a new multifunctional closed-circuit anaesthesia ventilator. In vitro comparison with a classical anaesthesia machine. Br J Anaesth. 2005;94:306–17. doi: 10.1093/bja/aei051. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy RR, French RA, Gilles S. The effect of a model-based predictve display on control of end-tidal sevoflurane concentrations during low-flow anaesthesia. Anesth Analg. 2004;99:1159–63. doi: 10.1213/01.ANE.0000131507.65132.7F. [DOI] [PubMed] [Google Scholar]
- 9.Sandhu K, Dash H. Awareness during anaesthesia. Indian J Anaesth. 2009;53:148–57. [PMC free article] [PubMed] [Google Scholar]
- 10.Locher S, Stadler KS, Boehlen T, Bouillon T, Leibundgut D, Schumacher PM, et al. A new closed loop control system for isoflurane using bispectral index outperforms manual control. Anesthesiology. 2004;101:591–602. doi: 10.1097/00000542-200409000-00007. [DOI] [PubMed] [Google Scholar]


