Abstract
In Russia, sexual transmission of HIV is increasing and street-based female sex workers (FSW) have a high HIV prevalence, but the role of male clients of FSW in HIV transmission and bridging to the general population has not been studied. Sixty-two male clients completed structured interviews during February-March of 2010 in St. Petersburg Russia. Descriptive analyses focused on condom use with different types of sex partners, substance use, and STI/HIV testing histories. The median lifetime and past 12 month numbers of FSW partners were 10 and 3, respectively. A majority of clients (74%) reported having non-FSW partners during the past 12 months, and nearly half (47%) reported having regular sex partners. Consistent condom use was reported in 61% of relationships with FSW partners and in 43% of relationships with non-FSW partners. A majority of clients (58%) was classified as active or potential bridgers based on having both FSW and non-FSW partners and reporting inconsistent condom use with their non-FSW partners. A majority (61%) also reported concurrent partnerships with FSW and non-FSW partners. Nearly half (48%) of last contacts with FSW partners involved consumption of alcohol by the client. Non-injection and injection drug use in the past 30 days were reported by 15% and 7% of clients, respectively. Twenty-nine percent reported history of an STI and 74% reported a previous HIV test; active/potential bridgers were significantly less likely than unlikely bridgers to have ever been tested for HIV. These data signal the potential for HIV/STI transmission among male clients of street-based FSW in St. Petersburg Russia due to their variety of partner types, sub-optimal condom use, and concurrent partnerships. Larger studies are needed to confirm these findings, further explore the roles of alcohol and drug use, and identify effective strategies and interventions for HIV prevention.
Keywords: HIV, bridging, female sex workers, clients, Russia
Introduction
The Russian social and economic transition in the 1990s that led to open borders and economic collapse gave rise to an injecting drug epidemic that was followed by an increase in street-based female sex work (Aral, St. Lawrence, Dyatlov, & Kozlov, 2005; Atlani, Carael, Brunet, Frasca, & Chaika, 2000). Over 90% of street-based female sex workers (FSW) in St. Petersburg have ever used drugs, with 84% reporting current injection drug use (Tun, Rusakova, Levina, Yakovleva, & Bodanovskaya, 2007). As a result, street-based FSW in St. Petersburg are especially vulnerable to HIV, as evidenced by prevalence reaching 48% in 2003, the last year for which a published estimate is available (WHO, 2004).
Russian HIV surveillance data indicate an increasing proportion of cases attributed to heterosexual transmission among those with a known mode of transmission from 4.1% in 2001 to 35.8% in 2009 (Pokrovsky, Ladnaya, & Buravtsova, 2010). In 2009, the estimated adult HIV prevalence exceeded 1% (UNAIDS/WHO 2010), raising concern about a more generalized epidemic. Recent studies further support the potential for HIV transmission beyond the core group of IDU through sex with non-IDU partners (Niccolai, Shcherbakova, Toussova, Kozlov, & Heimer, 2009). Interventions targeting core groups with high HIV prevalence will have the greatest impact on preventing widespread transmission in countries with early epidemics (Boily, Lowndes, & Alary, 2002; Robinson, Mulder, Auvert, Whitworth, & Hayes, 1999). Given Russia’s late entry to the epidemic (Cohen, 2010), now is a critical time to understand the role of all potential core groups in HIV transmission.
Bridging of HIV is transmission from one segment of the population, typically a high-risk core group, to another. Critical components of bridging include HIV prevalence in the core group, sub-optimal condom use, and sexual mixing patterns with other population groups. These characteristics have been described for male clients of FSW in many countries throughout Africa (Lowndes, Alary, Gnintoungbe, 2000; Gomes do Espirito Santo & Etheredge, 2002; Voeten, Egesah, Ondiege, Varkevisser, & Habbema, 2002; Vuylsteke, Ghys, Traore, Konan, Mah-Bi, Maurice, et al, 2003; Cote, Sobela, & Dzokoto, 2004), Asia (Hor, Detels, Heng, & Mun, 2005; Subramanian, Gupte, Paranjape, Brahmam, Ramakrishnan, Adhikary, et al. 2008; Xu, Wang, Lu, Pu, Zhang, Wong, et al., 2008; Nguyen, Nguyen, Trinh, Mills, & Detels, 2009; Jin, Smith, Chen, Ding, Yao, Wang, et al., 2010), and Latin America (Miller, Mendoza, Krone, Meza, Caceres, Coates, et al., 2004; Couture, Soto, Akom, Labbe, Joseph, & Zunzunegui, 2008; Patterson, Goldenberg, Gallardo, Lozada, Semple, Orozovoch, et al., 2009). In some settings, male clients have been characterized as playing an important role in bridging (Lowndes, 2000; Hor, 2005; Subramanian, 2008; Xu, 2008; Nguyen, 2009; Jin, 2010; Couture, 2008). Though previously considered a “hard to reach” population, male clients are feasible to recruit for research and prevention (Alary & Lowndes, 2004). To the best of our knowledge, no studies have examined the feasibility of recruiting or the potential for HIV/STI bridging of male clients of FSW in Russia.
The overall goals of this pilot study were to: (1) recruit a sample of male clients of street-based FSW in St. Petersburg, Russia and (2) conduct a structured survey about HIV risk behaviors. The varied nature of sex work in St. Petersburg has been well-described (Aral, 2005); in this study we focused on street-based FSW outside the city center and along the suburban commuting routes because they are known to be a more vulnerable population due to younger ages, lower education, less organization, and greater involvement in drug use. The specific aims for our second goal were to collect preliminary data to describe the sociodemographic characteristics of clients, their potential for HIV acquisition and transmission (bridging) based on partner types and condom use, and other HIV risk behaviors including alcohol and drug use, STI history, and HIV testing.
Methods
Formative work
Methods for recruitment and data collection were informed by formative work that included 37 semi-structured interviews with FSW, their clients, and key informants including doctors, policemen and outreach workers. These individuals were identified by the outreach department of the collaborating NGO and through peer referrals. Interviews were tape-recorded and summarized for review and discussion by study investigators prior to the next quantitative phase.
Recruitment and study population
We identified four recruitment methods for male clients that were considered feasible and potentially effective: FSW referral, peer referral (clients of FSW recruiting other clients), street intercept at locations of sex work, and clinician referrals from a city STI clinic. Outreach workers affiliated with the collaborating NGO routinely visit locations of sex work along commuting routes during peak hours to provide condoms, education, health care referrals, and social support. FSW encountered on the outreach van during these the study period (February-March, 2010) were provided the opportunity to recruit their clients for modest compensation of 500 rubles (approximately $17 US). Those who expressed an interest were trained in procedures for recruitment and were provided study coupons to give to their clients. For peer referrals by participating clients, we used a dual incentive system that included reimbursement for participation (500 rubles) as well as an additional reimbursement for successful recruitment of other clients (500 rubles). Street intercept recruitment was conducted in the areas of outreach (five major streets in two districts of the city that lead to the suburbs). Finally, a clinician known to NGO staff through previous projects agreed to act as a recruiter at a city STI clinic. All patients who had a clinic visit with this clinician during the study period were screened for eligibility and offered participation if eligible. Color coded and enumerated coupons were distributed to potential participants and were used to both track recruitment methods and provide reimbursements. Coupons mentioned a study about men’s health and contained contact information including phone numbers for survey staff. Participants chose an interview site that was convenient for them, either the van, STI clinic, or another location mutually agreed upon with the interviewer (e.g. cafés, homes).
The eligibility criterion for participation was self-report of having had sex with a FSW during the previous 12 months. FSW were defined as partners with whom the respondent reported buying sex in exchange for money, drugs, or other compensation. Screening procedures also included general questions about sex work in the area (e.g. locations, prices for services) to verify eligibility. From our formative work, we identified three main categories of male clients of FSW: one-time clients (men who have anonymous, one-time sex with FSW), regular clients (men who pay for sex with the same FSW multiple times), and “sponsors” (men who have more emotional involvement with FSW and who, in addition to paying for sex, may also provide extra money for basic necessities or assistance with living accommodations). These definitions were read to the respondents who then classified their own partners. Although partner types of FSW are dynamic and not always mutually exclusive, we sought to ensure representation of a range by recruiting 25 one-time clients, 25 regular clients, and 10 sponsors. Participants provided written informed consent, and participation was anonymous.
Data collection and survey measures
Participants completed a face-to face structured interview that was developed based on previous research and field experience with this population and formative work described above. The instrument was pilot tested with clients recruited through professional networks of NGO staff. Questions covered the following topics: demographics, substance use, self-reported HIV and STI history, sexual history, and sexual behavior with different types of female sex partners. To collect data about different types of sex partners, we used three different partner-specific modules: one for FSW partners, one for main non-FSW sex partners (wife, girlfriend, or live-in sex partners with whom there was an ongoing romantic relationship), and one for casual non-FSW sex partners (non-spouse, non-romantic partners with whom the respondent had one or more casual sex contacts with limited emotional involvement). Partner-specific data were collected for the last sex partner in each of the following categories: one-time FSW, regular FSW, sponsored FSW, and casual non-FSW partner; partner specific data forms were collected for up to three main non-FSW partners. Partner-specific questions included substance use prior to sex and condom use during vaginal and anal sex. The interview, lasting approximately one hour, was administered by trained outreach workers employed by the collaborating NGO or the clinician at the STI clinic.
Analysis
Means, medians, and proportions were calculated for the sample for demographic, substance use, self-reported HIV/STI history, and sexual history variables. Partner-specific analyses were stratified by FSW and non-FSW sex partners. Numbers of partners, substance use prior to sex with partners, and condom use were summarized. Consistent condom use was determined by responses to the 5-point Likert scale question that referred to the past 12 months: “How often do you use condoms during vaginal sex with this partner?”. Responses of “all the time” were classified as consistent use.
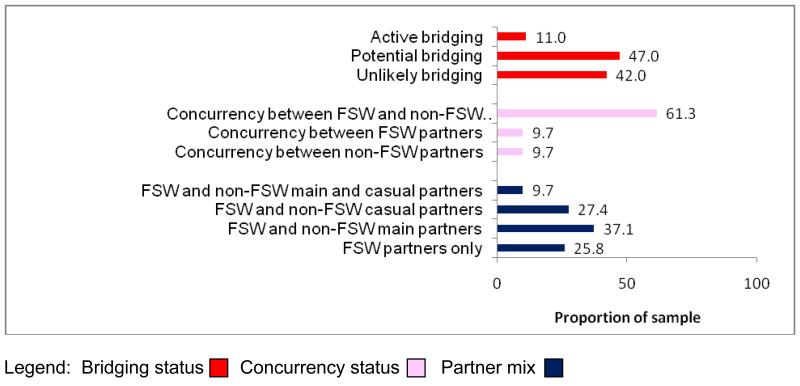
Potential for HIV/STI transmission was described by three different measures: bridging status, concurrency, and partner type mix. Bridging status (Nguyen, 2009) was defined as follows: active bridgers reported inconsistent condom use during vaginal sex with both FSW and non-FSW sex partners, potential bridgers reported consistent condom use with FSW partners and inconsistent condom use with non-FSW partners, and unlikely bridgers reported consistent condom use with FSW and non-FSW sex partners or consistent condom use with FSW and no non-FSW partners. Concurrency (having sex partners that overlap in time) was described with respect to FSW and non-FSW partners. Concurrency was asked directly: for each type of partner the respondent reported having, he was asked if he had other partners and if so which type, during the time he was having a sexual relationship with the previously described partner. Partner type mix described the sample according to whether clients had FSW partners only or FSW and non-FSW partners, including both regular and casual partners. These three measures were neither mutually exclusive nor independent; however, each describes a unique aspect of partnering (condom use with different types of partners, timing of partnerships, and different types of sex partners, respectively).
We conducted chi-square tests for categorical variables and t-tests for normally distributed continuous variables to compare active/potential bridgers to unlikely bridgers. Examined correlates included demographics, substance use, self-reported HIV/STI history, and sex histories including partner types. Variables that were associated with bridging status using the criteria p<0.20 in the unadjusted analyses were entered into a logistic regression model to determine independent associations measured by adjusted odds ratios (aOR) and 95% confidence intervals (CI).
Results
Sixty-two male clients were recruited and interviewed. A total of 67 coupons were distributed to FSW during outreach activities and 35 clients were recruited by this method. A total of 39 coupons were distributed to clients; 21 additional clients enrolled via this method. Two men were recruited directly by street intercept. Four men were recruited by the referring clinician; two additional men who were screened eligible and given study information did not contact staff for participation. None of the examined characteristics were associated with referral method, though active/potential bridgers were somewhat more likely to be recruited by FSW referrals (p=0.06). Forty-five participants contacted study staff to schedule an interview; the remaining 17 men were interviewed at the location of sex work.
Sample characteristics are presented in Table 1. For all analyses, “sponsor” partners were combined with regular FSW partners due to observed similarities and low frequency in our sample. Forty-two percent of clients reported one-time contacts with FSW only, 34% of clients reported contact with regular FSW only, and 24% reported both types of FSW sex partners. Nearly three-quarters of clients (74%) reported having non-FSW partners in the past 12 months, including 12 spouse partners.
Table 1.
Client sociodemographic characteristics and general HIV risk behaviors (n=62 unless otherwise noted)
| n (%)* | |
|---|---|
|
| |
| Age, in years | |
| Mean (SD) | 35.0 (8.5) |
| Median (range) | 34.0 (21-60) |
|
| |
| Citizen and residency status | |
| Citizen | 43 (69.4) |
| Non-citizen, registered | 17 (27.4) |
| Non-citizen, not registered | 2 (3.2) |
|
| |
| Education | |
| General secondary or less | 11 (17.7) |
| Vocational or specialized secondary | 42 (67.7) |
| Higher education | 9 (14.5) |
|
| |
| Employed (n=61) | |
| Yes | 49 (80.3) |
| No | 12 (19.7) |
|
| |
| Employment position (n=49 employed) | |
| Unskilled worker | 8 (16.3) |
| Skilled or service worker | 26 (53.1) |
| Employee, entrepreneur, or freelancer | 13 (26.5) |
| Head | 2 (4.1) |
|
| |
| Income (n=49 employed) | |
| ≤15000 rubles per month (≈USD500) | 9 (18.4) |
| 15001-25000 rubles per month (≈USD500-800) | 25 (51.0) |
| 25001-50000 rubles per month (≈USD800-1500) | 15 (30.6) |
|
| |
| Marital status | |
| Married or domestic partnership | 15 (24.2) |
| Single, never married | 26 (41.9) |
| Widowed, separated, divorced | 21 (33.9) |
|
| |
| Typical alcohol use per week during past 12 months | |
| No alcohol use past 12 months | 5 (8.1) |
| ≤1 occasion | 40 (64.5) |
| 2-3 occasions | 15 (24.2) |
| ≥4 occasions | 2 (3.2) |
|
| |
| Typical amount of alcohol consumed (n=57 consumed alcohol) | |
| 1 beer / 1 glass wine / 2 shots | 10 (17.5) |
| 1.5-2 beers / 2-3 glasses wine / 3-4 shots | 22 (38.6) |
| ≥3 beers / ≥1 bottle wine (0.7L) / ≥ 0.5 L vodka | 25 (43.9) |
|
| |
| Use of non-injection drugs, lifetime | |
| No | 40 (64.5) |
| Yes, but not in past 30 days | 13 (21.0) |
| Yes, in past 30 days | 9 (14.5) |
|
| |
| Use of injection drugs, lifetime | |
| No | 50 (80.6) |
| Yes, but not in past 30 days | 8 (12.9) |
| Yes, in past 30 days | 4 (6.5) |
|
| |
| History of a sexually transmitted infection | |
| Yes | 18 (29.0) |
| No | 44 (71.0) |
|
| |
| Ever had an HIV test | |
| Yes | 46 (74.2) |
| No | 16 (25.8) |
|
| |
| Self-reported HIV status (n=45) | |
| HIV positive | 1 (2.2) |
| HIV negative | 44 (97.8) |
|
| |
| Age at first sex, in years | |
| Mean (SD) | 16.5 (1.9) |
| Median (range) | 16 (13-22) |
|
| |
| Age at first sex with FSW, in years (n=57) | |
| Mean (SD) | 24.3 (6.4) |
| Median (range) | 23 (15-46) |
|
| |
| Lifetime number of sex partners (n=48) | |
| Mean (SD) | 44.3 (51.8) |
| Median (range) | 30 (8-300) |
|
| |
| Lifetime number of FSW sex partners (n=55) | |
| Mean (SD) | 12.3 (11.9) |
| Median (range) | 10 (1-70) |
|
| |
| Total number of sex partners past 12 months (n=62) | |
| Mean (SD) | 5.4 (4.1) |
| Median (range) | 4 (1-20) |
|
| |
| Total number of FSW sex partners past 12 months | |
| Mean (SD) | 3.6 (2.9) |
| Median (range) | 3 (1-14) |
|
| |
| Non-FSW sex partner in past 12 months | |
| Yes | 46 (74.2) |
| No | 16 (25.8) |
n (%) are presented for categorical variables; continuous variables presented as mean (SD) and median (range) are otherwise noted.
Respondents reported data for a total of 126 partners including 77 FSW partners and 49 non-FSW sex partners. Few participants reported anal sex (n=8); thus all analyses were specific for vaginal sex. Alcohol and drug use prior to last sex were reported in 48% and 7% of FSW partnerships, respectively. Consistent condom use and condom use at last sex with FSW partners were reported by 61% and 79%, respectively. Among the 49 non-FSW partnerships, alcohol and drug use prior to last sex were reported by 39% and 4%, respectively. Consistent condom use and condom use at last sex with these partners were reported by 43% and 55%, respectively.
Partnership patterns in past 12 months as described by bridging, concurrency, and partner mix are presented in Figure 1. The proportions of the sample classified as active, potential, and unlikely bridgers were 11%, 47%, and 42%, respectively. Concurrency between FSW and non-FSW partners was reported by 61% of the sample. Approximately one in four of all respondents (26%) reported FSW partners only; the remaining 74% reported having both FSW and non-FSW sex partners including 37% (n=23) who reported FSW and main sex partner, 27% (n=17) who reported FSW and casual sex partner, and 10% (n=6) who reported having FSW, main, and casual sex partners. All variables presented in Table 1 were considered possible correlates of active/potential bridging; we also examined whether type of FSW partner (regular, one-time) and type of non-FSW sex partner (main, casual) were associated with bridging status. Two variables were significantly associated with being an active/potential bridger at p<0.05 in the unadjusted analysis: having never been tested for HIV (81% vs. 50% of ever tested, p=0.03), and having only one-time FSW partners (76% vs. 46% of those with regular FSW partners, p=0.02). Two additional variables, education and employment status, were associated at p<0.20 in unadjusted analyses and were thus included in the final multivariate model. In the final model, no variable was significant at p<0.05; having never been tested for HIV (aOR=4.2, 95% CI=0.9-19.8) and having only one-time FSW partners (aOR=3.0, 95% CI=0.9-9.8) were marginally non-significant (p=0.07 for both).
Figure 1.
Distributions of bridging statusa, concurrencyb, and partner mixc in the past 12 months (n=62)
aDefinitions for bridging status variable are as follows: active bridging - reporting inconsistent condom use during vaginal sex with both FSW and non-FSW partners; potential bridging – reporting consistent condom use during vaginal sex with FSW partners and inconsistent condom use during vaginal sex with non-FSW partners; unlikely bridging – reporting consistent condom use during vaginal sex with FSW and non-FSW partners, or consistent condom use during vaginal sex with FSW and not having a non-FSW sex partner. One participant who reported consistent condom use during vaginal sex with non-FSW partner and inconsistent condom use during vaginal sex with FSW was classified as potential bridging. These categories were mutually exclusive. Participants with missing and “don’t know” responses to condom use questions were classified as inconsistent condom users because consistent condom use could not be verified.
bNot mutually exclusive categories.
cMutually exclusive categories
Discussion
Spread of HIV from high-risk core groups to the general population depends on a number of factors (Lowndes, Renton, Alary, Rhodes, Garnett, & Stimson, 2003), one of which is the sexual behaviors of male clients of FSW in places where FSW have high HIV prevalence. In St. Petersburg Russia, street-based FSW had the alarming HIV prevalence of 48% in 2003 (WHO, 2004), yet the characteristics, HIV risk behaviors, and sexual mixing patterns of their clients have not been studied. Our results indicate that potential for HIV bridging is real and substantial: over half the sample was characterized as active or potential bridgers based on having both FSW and non-FSW sex partners and reporting inconsistent condom use. These findings are similar to results from Vietnam that used the same measure of bridging (Nguyen, 2009). Partner type mix was also substantial: 74% of clients reported having non-FSW sex partners in addition to FSW partners. Similarly high estimates of clients reporting non-FSW partners (>50%) have been reported in other studies from around the world (Alary, 2003; Cote, 2004; Couture, 2008; Jin, 2010; Nguyen, 2009; Subramanian, 2008; Voeten, 2002; Vuylsteke, 2003; Xu, 2008). The high levels of partner type mixing and concurrency (61%) coupled with sub-optimal condom use indicate a pressing need to better understand the context and nature of risk for this potentially important bridging population.
The frequency with which alcohol was consumed prior to last sex with FSW in our sample (48%) was at the high end of the range of estimates reported in other studies (Jin, 2010; Patterson, 2009; Nguyen, 2009). Given the well-established association between alcohol and HIV risk (Kalichman, 2007), this is troublesome, and deserves further study as a possible target for intervention. In the context of sex work, alcohol use also poses the additional risk of violence against women. In the formative phase of this study, several women reported such concerns about drunken clients. The frequency of reported drug use in our sample was higher than estimates from most (Hor, 2005; Jin, 2010; Nguyen, 2009; Xu, 2008) but not all (Patterson, 2009) other studies. Given the current epidemic situation in Russia in which IDU have high HIV incidence and prevalence (Niccolai, 2009; Niccolai, 2010), this is troublesome, and the overlap between sexual and drug related HIV risk among clients of FSW needs to be explored further. Lower rates of testing among active/potential bridgers is also worrisome for HIV transmission to the general population, and future studies should seek to better understand patterns of HIV testing in this population, including testing frequency and motivators.
An important finding of this study was successful recruitment of male clients of FSW in a country experiencing epidemic spread of HIV. Similar to other regions of the world (Alary, 2004), FSW and their clients were willing to participate and welcomed the opportunity to recruit other participants. This was greatly enhanced by the dual incentive structure for recruitment that was used in this study. The most effective methods of recruitment were FSW and peer referrals that produced 90% of our sample. While effective, it should be noted that these methods have potential limitations as well. They may produce biased samples that fail to engage clients who experience greater levels of shame, stigma, or fear related to their behaviors. Future research and programs should be mindful of such sub-groups, and work to identify and engage them in a sensitive, non-coercive, and safe manner.
Sampling in this study was limited to clients of street-based FSW to focus on the potentially high risk for HIV/STI transmission due to high HIV prevalence among these women. Representativeness of our sample may have been limited by selection bias with respect to whom FSW and clients gave coupons and by recruitment in only two districts of the city. Self-report of sensitive information including sexual behaviors is always subject to potential social desirability and under-reporting; however, such an effect would only underestimate the true magnitude of risk. The nature of this pilot study also did not allow us to collect complete data about all aspects of contacts with FSW that may influence transmission dynamics, for example, patterns across different geographic regions. Another potential limitation of this study was our relatively strict definition of “sex work” that may not capture the varied and dynamic nature of sexual partnerships. However, our approach did allow us to quantify risks and behaviors as a starting point toward a greater understanding of HIV risk within different types of partnerships. Despite these limitations, we were successful in obtaining preliminary data to inform future larger studies.
To the best of our knowledge, there are no published estimates of what percent of men in St. Petersburg purchase sex, and it is recognized that this is difficult to estimate (Carael, Slaymaker, Lyerla, & Sarkar, 2006). Unpublished results from a survey of 250 private sector male employees in three Russian cities during 2006-2007 conducted by members of our research team revealed that 26% reported a history of purchasing sex from a FSW. Despite remaining uncertainties about the frequency of this behavior among Russian men, our results suggest that male clients of FSW in Russia may play an important role in HIV/STI bridging to the general population and thus should be the focus of future studies to further elucidate risks and opportunities for intervention. Future studies should also examine HIV/STI prevalence in this population. Preventing further spread of HIV in Russia among core groups and in the general population will require a comprehensive and multi-pronged approach, and including potential bridging populations such as male clients of FSW in these efforts will be a necessary component.
Acknowledgements
We gratefully acknowledge support for this study in the form of funding from the United States National Institutes of Health including R21DA025433 (PI: L Niccolai), D43TW001028 (PI: R Dubrow), and P30NIMH62294 (PI: P Cleary). We also thank Natalia Shuter and Dmitry Sigalov for conduct of interviews, and all participants who gave their time and shared their stories.
References
- Alary M, Lowndes CM. The central role of clients of female sex workers in the dynamics of heterosexual HIV transmission in sub-Saharan Africa. AIDS. 2004;18:945–947. doi: 10.1097/00002030-200404090-00013. [DOI] [PubMed] [Google Scholar]
- Alary M, Lowndes CM, Mukenge-Tshibaka L, Gnintoungbe CAB, Bedard E, Geraldo N, et al. Sexually transmitted infections in male clients of female sex workers in Benin: risk factors and reassessment of the leucocyte esterase dipstick for screening of urethral infections. Sexually Transmitted Infections. 2003;79:388–392. doi: 10.1136/sti.79.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aral SO, Lawrence St., Dyatlov R, Kozlov A. Commercial sex work, drug use, and sexually transmitted infections in St. Petersburg, Russia. Social Science and Medicine. 2005;60:2181–2190. doi: 10.1016/j.socscimed.2004.10.009. J.S. [DOI] [PubMed] [Google Scholar]
- Atlani L, Carael M, Brunet J-B, Frasca T, Chaika N. Social change and HIV in the former USSR: the making of a new epidemic. Social Science & Medicine. 2000;50:1547–1556. doi: 10.1016/s0277-9536(99)00464-5. [DOI] [PubMed] [Google Scholar]
- Boily MC, Lowndes C, Alary M. The impact of HIV epidemic phases on the effectiveness of core group interventions: insights from mathematical models. Sexually Transmitted Infections. 2002;78(Suppl i):i78–i90. doi: 10.1136/sti.78.suppl_1.i78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carael M, Slaymaker E, Lyerla R, Sarkar S. Clients of sex workers in different regions of the word: hard to count. Sexually Transmitted Infections. 2006;82(Suppl i):iii26–iii33. doi: 10.1136/sti.2006.021196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Late for the epidemic: HIV/AIDS in Eastern Europe. Science. 2010;329:160–164. doi: 10.1126/science.329.5988.160. [DOI] [PubMed] [Google Scholar]
- Cote A-M, Sobela F, Dzokoto A. Transactional sex is the driving force in the dynamics of HIV in Accra, Ghana. AIDS. 2004;18:917–925. doi: 10.1097/00002030-200404090-00009. [DOI] [PubMed] [Google Scholar]
- Couture M-C, Soto JC, Akom E, Labbe A-C, Joseph G, Zunzunegui M-V. Clients of female sex workers in Gonaives and St-Marc, Haiti: characteristics, sexually transmitted infection prevalence and risk factors. Sexually Transmitted Diseases. 2008;35:849–855. doi: 10.1097/OLQ.0b013e318177ec5c. [DOI] [PubMed] [Google Scholar]
- Gomes do Espirito Santo ME, Etheredge GD. How to reach clients of female sex workers: a survey “by surprise” in brothels in Dakar, Senegal. Bulletin of World Health Organization. 2002;80:709–713. [PMC free article] [PubMed] [Google Scholar]
- Hor LB, Detels R, Heng S, Mun P. The role of sex worker clients in transmission of HIV in Cambodia. International Journal of STD & AIDS. 2005;16:170–174. doi: 10.1258/0956462053057567. [DOI] [PubMed] [Google Scholar]
- Jin X, Smith K, Chen RY, Ding G, Yao Y, Wang H, et al. HIV prevalence and risk behaviors among male clients of female sex workers in Yunnan, China. Journal of Acquired Immune Deficiency Syndromes. 2010;53:131–135. doi: 10.1097/QAI.0b013e3181b3552a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in Sub-Saharan Africa: systematic review of empirical findings. Prevention Science. 2007;8:141–151. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- Lowndes CM, Renton A, Alary M, Rhodes T, Garnett G, Stimson G. Conditions for widespread heterosexual spread of HIV in the Russian Federation: Implications for research, monitoring and prevention. International Journal of Drug Policy. 2003;14:45–62. [Google Scholar]
- Lowndes CM, Alary M, Gnintoungbe CA, et al. Management of sexually transmitted diseases and HIV prevention in men at high risk: targeting clients and non-paying sexual partners of female sex workers in Benin. AIDS. 2000;14:2523–2534. doi: 10.1097/00002030-200011100-00015. [DOI] [PubMed] [Google Scholar]
- Miller GA, Mendoza W, Krone MR, Meza R, Caceres CF, Coates TJ, et al. Clients of female sex workers in Lima, Peru: a bridge population for sexually transmitted disease/HIV transmission? Sexually Transmitted Diseases. 2004;31:337–342. doi: 10.1097/00007435-200406000-00003. [DOI] [PubMed] [Google Scholar]
- Nguyen NT, Nguyen HT, Trinh HQ, Mills SJ, Detels R. Clients of female sex workers as a bridging population in Vietnam. AIDS and Behavior. 2009;13:881–891. doi: 10.1007/s10461-008-9463-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niccolai LM, Shcherbakova IS, Toussova OV, Kozlov AP, Heimer R. The potential for bridging of HIV transmission in Russian Federation: Sex risk behaviors and HIV prevalence among drug users (DUs) and their non-DU sex partners. Journal of Urban Health. 2009;86:S131–S143. doi: 10.1007/s11524-009-9369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niccolai LM, Verevochkin SV, Toussova OV, White E, Barbour R, Kozlov AP, et al. Estimates of HIV incidence among drug users in St. Petersburg, Russia: Continued growth of a rapidly expanding epidemic. European Journal of Public Health. 2010 doi: 10.1093/eurpub/ckq115. doi:10.1093/eurpub/ckq115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Goldenberg S, Gallardo M, Lozada R, Semple SJ, Orozovoch P, et al. Correlates of HIV sexually transmitted infections, and associated high-risk behaviors among male clients of female sex workers in Tijuana, Mexico. AIDS. 2009;23:1765–1771. doi: 10.1097/QAD.0b013e32832f08a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokrovsky V, Ladnaya N, Buravtsova Y. HIV-infection Informational Bulletin No. 34. Russian Federal AIDS Centre; Moscow: 2010. in Russian. [Google Scholar]
- Robinson NJ, Mulder D, Auvert B, Whitworth J, Hayes R. Type of partnership and heterosexual spread of HIV infection in rural Uganda: results of simulation modeling. International Journal of STD & AIDS. 1999;10:718–725. doi: 10.1258/0956462991913394. [DOI] [PubMed] [Google Scholar]
- Subramanian T, Gupte MD, Paranjape RS, Brahmam GNV, Ramakrishnan L, Adhikary R, et al. HIV, sexually transmitted infections and sexual behavior of male clients of female sex workers in Andhra Pradesh, Tamil Nadu and Maharashtra India: results of a cross-sectional survey. AIDS. 2008;22:S69–S79. doi: 10.1097/01.aids.0000343765.00573.ce. [DOI] [PubMed] [Google Scholar]
- Tun W, Rusakova M, Levina O, Yakovleva A, Bodanovskaya Z. Behavioral Monitoring Survey: Russia 2005. Family Health International; Arlington: 2007. 2007. http://pdf.usaid.gov/pdf_docs/PNADK868.pdf. [Google Scholar]
- UNAIDS. WHO Epidemiological Fact Sheet: Russian Federation 2009 Update. 2010 http://unaids.org/en.regionscountires/countires/russianfederation/
- Voeten HACM, Egesah OB, Ondiege MY, Varkevisser CM, Habbema JDF. Clients of female sex workers in Nyanza Province, Kenya: A core group in STD/HIV transmission. Sexually Transmitted Diseases. 2002;29:444–452. doi: 10.1097/00007435-200208000-00003. [DOI] [PubMed] [Google Scholar]
- Vuylsteke BL, Ghys PD, Traore M, Konan Y, Mah-Bi G, Maurice C, et al. HIV prevalence and risk behaviors among clients of female sex workers in Abidjan, Cote d’Ivoire. AIDS. 2003;17:1691–1694. doi: 10.1097/00002030-200307250-00014. [DOI] [PubMed] [Google Scholar]
- World Health Organization . HIV-related sentinel surveillance among risky populations in the Republic of Azerbaijan. Republic of Moldova and the Russian Federation; 2004. http://www.euro.who.int/Document/E84675.pdf. [Google Scholar]
- Xu JJ, Wang N, Lu L, Pu Y, Zhang GL, Wong M, et al. HIV and STIs in clients and female sex workers in mining regions of Gejiu City, China. Sexually Transmitted Diseases. 2008;35:558–565. doi: 10.1097/OLQ.0b013e318165926b. [DOI] [PubMed] [Google Scholar]